Watch a video presentation of this article
Watch the interview with the author
Abbreviations
- 2D
two‐dimensional
- MR
magnetic resonance
- MRI
magnetic resonance imaging
- MRE
magnetic resonance elastography
- pSWE
point shear wave elastography
- SWE
shear wave elastography
- TE
transient elastography
- US
ultrasound
What Is Elastography?
Elastography encompasses imaging techniques that noninvasively estimate tissue elasticity and related mechanical properties through the application of external forces. Elasticity reflects the ability of tissue to deform and resume its normal shape under an applied stress and relates to tissue stiffness. Tissue stiffness in turn reflects tissue composition and structure. In the liver, tissue stiffness has been shown to be elevated with advanced fibrosis and to correlate with the stage of fibrosis.1
Why Elastography?
In the pediatric population, the major causes of chronic liver disease are fatty liver disease, hepatitis (infectious, autoimmune, or drug‐related), genetic diseases (α‐1 antitrypsin deficiency, cystic fibrosis, biliary atresia, Wilson's disease, and storage disorders), and congestive hepatopathy.2, 3 Liver fibrosis is an important pathological and pathogenic feature of each of these conditions, and the assessment of fibrosis is often necessary for prognosis, risk stratification, clinical decision making, and disease severity monitoring. Because of the cost, need for sedation, and risk associated with biopsy, noninvasive methods to assess liver fibrosis such as elastography are needed.4
Elasticity Imaging
Tissue stiffness can be estimated by imaging with either ultrasound (US) or magnetic resonance imaging (MRI). US‐based elastography techniques include strain‐based imaging, transient elastography (TE), and shear wave elastography (SWE). MRI measures tissue stiffness with magnetic resonance elastography (MRE). Other than strain‐based imaging, which has largely been abandoned in the liver, all of these techniques (TE, SWE, and MRE) estimate tissue stiffness by measuring the speed (and sometimes other characteristics) of a shear wave traversing the tissue.
Ultrasound Elastography
US shear wave examinations are performed by placing a probe in the intercostal space. TE induces shear waves in the liver with a mechanical actuator, which vibrates on the skin surface. SWE transmits focused push pulses into the tissue, which in turn induces lateral shear waves. The two main implementations of SWE are point shear wave elastography (pSWE), which measures stiffness (or sometimes shear wave speed) at a single point in the tissue, and 2D SWE, which generates a color map of tissue stiffness or shear wave speed over a defined area of interest within which multiple measurements can be made (Fig. 1).
Figure 1.
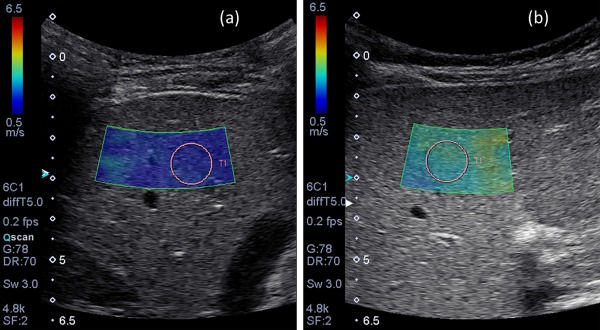
(A) Normal 2D SWE US examination in a 5‐year‐old boy with hepatitis C. Mean shear wave speed was 1.3 m/second. (B) Abnormal 2D SWE US examination in a 2‐year‐old boy with progressive familial intrahepatic cholestasis. Mean shear wave speed in this patient was 2.8 m/second.
TE is available on a dedicated, nonimaging device manufactured by a single manufacturer (Fibroscan; Echosens). By comparison, SWE is available on conventional clinical US scanners. Individual vendors use proprietary technology, and limited data are available on measurement reproducibility across scanner models.
Among US‐based techniques, the greatest body of literature exists for TE. Studies in pediatric patients with chronic liver disease have shown TE to be reliable in distinguishing stages of liver fibrosis.5 A meta‐analysis of TE that included 57 studies found the sensitivity and specificity of diagnosing liver fibrosis to be 81% and 88%, respectively.6 The main disadvantage of TE is that it does not produce anatomic images, so the precise location of the measurements is not known. TE is also limited in the setting of ascites because the shear wave is not reliably transmitted to the liver.7pSWE and two‐dimensional (2D) SWE techniques differ from TE in that the user is provided with images of the liver (grayscale for pSWE and color stiffness maps for 2D SWE) in which a region of interest can be placed. Pediatric studies of SWE have shown significant positive correlations between liver histological fibrosis score and mean shear wave speed measured by SWE.8 One unique application of SWE in the pediatric population is the differentiation of biliary atresia from other forms of neonatal cholestasis (Fig. 2).9 SWE has been shown to provide reasonable discriminatory value in this setting. One limitation of SWE is that both pSWE and 2D SWE sample only small areas of the liver and therefore have some risk for sampling error.
Figure 2.
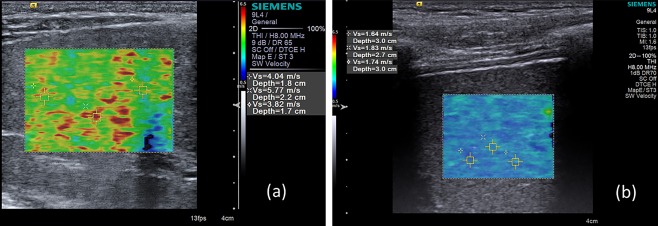
Two infants with persistent jaundice. (A) Elastogram generated with 2D SWE in one of the infants shows marked liver stiffening and heterogeneity. Further work‐up established a diagnosis of biliary atresia. (B) Elastogram in the other infant shows only mild stiffening without heterogeneity. Further work‐up established a diagnosis of neonatal hepatitis.
Magnetic Resonance Elastography
MRE uses low‐frequency (60‐Hz) sound waves to induce shear waves in the liver, visualizes the shear waves by tracking tissue displacement using a modified phase‐contrast sequence, and measures the speed of the propagating wave with specialized software called an inversion algorithm. The sound waves are generated by a subwoofer (“active driver”) outside the scan room and are transmitted to a plastic disk (“passive driver”) secured by an elastic band over the right lower anterior chest wall (Fig. 3). Identical MRE hardware and inversion algorithms are now available on scanners manufactured by the three major magnetic resonance (MR) vendors.
Figure 3.
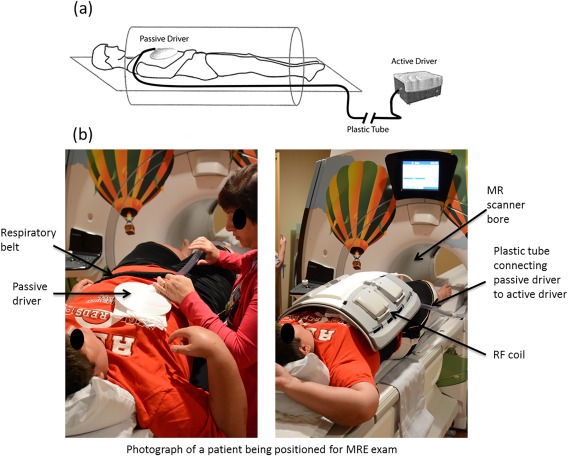
(A) Schematic diagram of patient set up with MRE hardware. The active driver is placed in the MR equipment room and is connected to the passive driver by a plastic tube. (B) Photograph of a patient being positioned for liver MRE study.
Most patients can feel the vibrations generated by the disk but do not find them uncomfortable. To prepare pediatric patients for the sensation of the hepatic vibrations, our child life specialists use a vibrating passive driver simulator to acquaint the child with the sensation of the vibrations.10
MRE can be achieved in between one and four breath holds depending on the sequence used. We have successfully performed awake MRE examinations on children as young as 4 months of age (Fig. 4), but sedation may be required for very young or developmentally delayed children.
Figure 4.
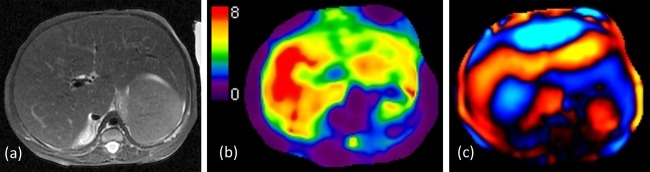
Four‐month‐old girl with a history of hemophagocytic lymphohistiocytosis. (A) Axial T2‐weighted image showing an enlarged but smoothly contoured liver. (B) Representative elastogram at the same level showing yellow and red regions of elevated liver stiffness (mean 5.5 kPa). (C) The propagating wave has a long wavelength, reflecting elevated stiffness.
Studies in adult patients have shown that MRE can discriminate patients with moderate and severe fibrosis from those with mild fibrosis with a sensitivity of 86% and specificity of 85%.11 Pediatric studies, however, are more limited, although early results are promising. In a study of 35 pediatric patients with mixed chronic liver disease, Xanthakos et al.1 showed that a cutoff stiffness value of 2.71 kPa provided 88% sensitivity and 85% specificity for detecting moderate liver fibrosis.
Confounding Effects
To get accurate liver stiffness measurements, elastography must be performed after an interval of fasting to avoid elevated liver stiffness values caused by postprandial increased portal venous flow.12 For children, we recommend nothing by mouth for 4 or more hours before the examination.10
Other causes of elevated liver stiffness not due to fibrosis include hepatic congestion and inflammation.3, 13 These processes, which can precede or coexist with fibrosis in patients with congenital heart disease and inflammatory hepatopathies, can confound prediction of liver fibrosis on the basis of elastography (Fig. 5).
Figure 5.
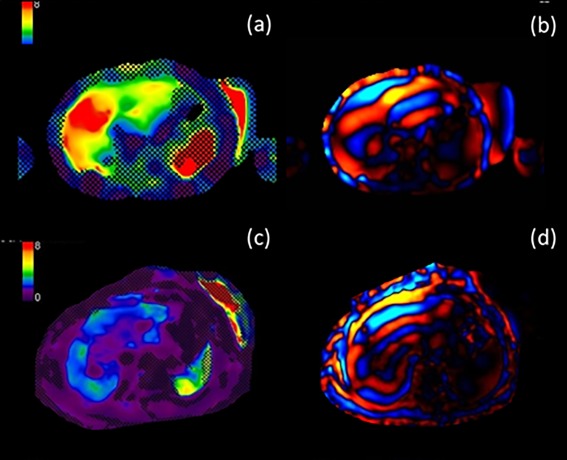
Eight‐year‐old girl with autoimmune hepatitis. (A) Baseline elastogram with red, orange, and yellow areas showing elevated liver stiffness (mean, 5.5 kPa). (B) The propagating wave has a long wavelength. (C) Elastogram obtained in the same patient 2 years later after treatment with steroids shows blue and green areas reflective of reduced liver stiffness (mean, 2.1 kPa). (D) Wavelength is now normal.
Advantages and Limitations: Ultrasound Elastography Versus Magnetic Resonance Elastography
Although both US and MRI can be used to measure hepatic stiffness, each modality has relative advantages and limitations. US‐based elastography is readily available, portable, relatively inexpensive, and does not require sedation. The volume of tissue interrogated, however, is small, and US‐based techniques may not perform as well in the setting of severe obesity that accompanies fatty liver disease (Fig. 6).14 MRE samples a much larger area of the liver, providing a more global assessment of liver stiffness less subject to sampling error. MRE thus provides reproducible results and is not as limited in obesity.15, 16 The disadvantages of MRE, however, are that it is more expensive and less readily available as compared with US, and it may require sedation in pediatric patients.
Figure 6.
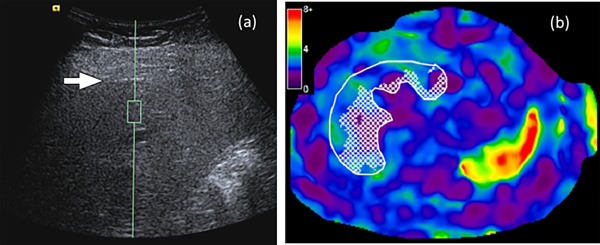
Sixteen‐year‐old girl with nonalcoholic fatty liver disease and a body mass index of 34 kg/m2. (A) On grayscale image, the liver is poorly visualized with only the liver capsule subtly apparent (arrow). The sample region of interest (green box) is within the liver parenchyma. Mean shear wave speed by pSWE was 3.1 m/second (markedly elevated and suggestive of end‐stage liver disease). (B) MR elastogram image shows green, blue, and purple in the liver reflective of a liver stiffness of 2.3 kPa (normal). The discordance between SWE and MRE in this case probably reflects the technical difficultly of SWE in obese adolescents, in whom liver visualization with ultrasound may be inadequate.
Summary
Liver elastography is an accurate, noninvasive method for assessing hepatic fibrosis in adults. Validation in children is emerging. As both US‐ and MR‐based technologies mature, they will likely be complementary examinations in the pediatric population.
Potential conflict of interest: Nothing to report.
REFERENCES
- 1. Xanthakos SA, Podberesky DJ, Serai SD, Miles L, King EC, Balistreri WF, et al. Use of magnetic resonance elastography to assess hepatic fibrosis in children with chronic liver disease. J Pediatr 2014;164:186‐188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Ovchinsky N, Moreira RK, Lefkowitch JH, Lavine JE. Liver biopsy in modern clinical practice: a pediatric point‐of‐view. Adv Anat Pathol 2012;19:250‐262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Serai SD, Wallihan DB, Venkatesh SK, Ehman RL, Campbell KM, Sticka J, et al. Magnetic resonance elastography of the liver in patients status‐post fontan procedure: feasibility and preliminary results. Congenit Heart Dis 2014;9:7‐14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Towbin AJ, Serai SD, Podberesky DJ. Magnetic resonance imaging of the pediatric liver: imaging of steatosis, iron deposition, and fibrosis. Magn Reson Imaging Clin N Am 2013;21:669‐680. [DOI] [PubMed] [Google Scholar]
- 5. Behairy Bel S, Sira MM, Zalata KR, Salama el‐SE, Abd‐Allah MA. Transient elastography compared to liver biopsy and morphometry for predicting fibrosis in pediatric chronic liver disease: does etiology matter? World J Gastroenterol 2016;22:4238‐4249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Geng XX, Huang RG, Lin JM, Jiang N, Yang XX. Transient elastography in clinical detection of liver cirrhosis: a systematic review and meta‐analysis. Saudi J Gastroenterol 2016;22:294‐303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Jeong WK, Lim HK, Lee HK, Jo JM, Kim Y. Principles and clinical application of ultrasound elastography for diffuse liver disease. Ultrasonography 2014;33:149‐160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Dillman JR, Heider A, Bilhartz JL, Smith EA, Keshavarzi N, Rubin JM, et al. Ultrasound shear wave speed measurements correlate with liver fibrosis in children. Pediatr Radiol 2015;45:1480‐1488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Leschied JR, Dillman JR, Bilhartz J, Heider A, Smith EA, Lopez MJ. Shear wave elastography helps differentiate biliary atresia from other neonatal/infantile liver diseases. Pediatr Radiol 2015;45:366‐375. [DOI] [PubMed] [Google Scholar]
- 10. Serai SD, Towbin AJ, Podberesky DJ. Pediatric liver MR elastography. Dig Dis Sci 2012;57:2713‐2719. [DOI] [PubMed] [Google Scholar]
- 11. Yin M, Talwalkar JA, Glaser KJ, Manduca A, Grimm RC, Rossman PJ, et al. Assessment of hepatic fibrosis with magnetic resonance elastography. Clin Gastroenterol Hepatol 2007;5:1207‐1213.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Yin M, Talwalkar JA, Glaser KJ, Venkatesh SK, Chen J, Manduca A, et al. Dynamic postprandial hepatic stiffness augmentation assessed with MR elastography in patients with chronic liver disease. AJR Am J Roentgenol 2011;197:64‐70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Wallihan DB, Podberesky DJ, Marino BS, Sticka JS, Serai S. Relationship of MR elastography determined liver stiffness with cardiac function after Fontan palliation. J Magn Reson Imaging 2014;40:1328‐1335. [DOI] [PubMed] [Google Scholar]
- 14. Trout AT, Dillman JR, Xanthakos S, Kohli R, Sprague G, Serai S, et al. Prospective assessment of correlation between US acoustic radiation force impulse and MR elastography in a pediatric population: dispersion of US shear‐wave speed measurement matters. Radiology 2016;281:544‐552. [DOI] [PubMed] [Google Scholar]
- 15. Serai SD, Yin M, Wang H, Ehman RL, Podberesky DJ. Cross‐vendor validation of liver magnetic resonance elastography. Abdom Imaging 2015;40:789‐794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Trout AT, Serai S, Mahley AD, Wang H, Zhang Y, Zhang B, et al. Liver stiffness measurements with MR elastography: agreement and repeatability across imaging systems, field strengths, and pulse sequences. Radiology 2016;281:793‐804. [DOI] [PubMed] [Google Scholar]


