Abstract
Mexican-origin adolescents have a high prevalence of obesity. Research is needed to understand how family context may shape adolescent BMI. This study examined longitudinal associations of family functioning variables with the Centers for Disease Control and Prevention’s modified BMI z-score (BMIaz) in 1,175 Mexican-origin adolescents, and explored interactions with acculturation. Adolescents (50% female, aged 11–13 y in 2005–06) were identified from an ongoing cohort study of Mexican-origin adults in Houston, TX, and were assessed three times from 2005–06 to 2010–11. In multivariate linear mixed models stratified by gender, we assessed longitudinal associations of family cohesion and family conflict with adolescent BMIaz and explored interactions with language acculturation. We disaggregated the between- (mean) and within-person (individual deviation) components of family cohesion and family conflict to assess the effects on BMIaz. Approximately one-third of adolescents were obese at baseline, and BMIaz declined during the study. In girls, higher mean family cohesion and conflict were associated with steeper declines in BMIaz. Parental linguistic acculturation modified the relationship between within-person deviation in family cohesion and BMIaz in girls, such that high parental U.S. acculturation was associated with a stronger inverse association. There were no significant associations in boys. These findings highlight the potential importance of the family context to female adolescent BMI and the promise of addressing family context in obesity-related interventions.
Keywords: Mexican Americans, Adolescent, Obesity, Acculturation, Family Functioning, Family Cohesion, Family Conflict
INTRODUCTION
Adolescent obesity in the U.S. remains a persistent public health concern, with 20% and 21% of boys and girls obese, respectively [1]. The prevalence of obesity is even higher among Hispanics, with 23% of boys and girls obese [1]. Obesity in adolescence tends to persist into adulthood [2], and increases the risk of type 2 diabetes, cardiovascular disease, and certain cancers [3–5]. As such, understanding the factors that affect weight during the vulnerable period of pubertal development is critical to the design of health promotion efforts.
Previous research places growing emphasis on the importance of the family context for adolescent obesity and related behaviors [6, 7]. Family systems theory suggests that family members both influence and are influenced by the actions of others in the family [8]. In this way, the family context helps to shape the formation and maintenance of health behaviors. Indeed, prior research has identified aspects of the family context associated with adolescents’ weight and weight-related behaviors. Parental factors include practices such as modeling health behaviors and providing encouragement and support for health behaviors [9–11], along with general parenting style (i.e., authoritative, authoritarian, permissive, neglectful) [12–15]. Family-level factors such as family functioning, however, are less understood. Family functioning refers to the interactions among family members and how they manage daily routines, communicate, and respond emotionally to each other [16]. Family environments characterized by conflict, a lack of support, and neglect are believed to create conditions ill-suited to support a healthy lifestyle [8]. Although some studies suggest that higher levels of cohesion and lower levels of conflict are associated with healthy weight-related behaviors and outcomes in children and adolescents, particularly girls [16–24], null findings have also been found [22, 25–27]. However, the vast majority of research is based on cross-sectional studies involving predominantly non-Hispanic White participants. There is a need to further study family functioning and adolescent obesity in racial/ethnic minorities using longitudinal data [16, 21]. This research is especially needed in Hispanics, the fastest growing ethnic minority group in the U.S [28].
Acculturation, which refers to the process of cultural change whereby an individual adopts aspects of a new culture [29], may be critical to consider in investigations of family functioning and health outcomes in Hispanic adolescents. Cultural practices of parenting and socialization within the family may modify the relation of family context variables with adolescent obesity [16, 30–34] and previous studies have shown that obesity-related behavior in Hispanic adolescents differ by acculturation level [35, 36]. Family cohesion and conflict, two important family functioning variables, may vary by acculturation [37, 38]. Further, Hispanic families are often comprised of individuals with differing levels of acculturation, which can be a source of familial stress and tension [39, 40], particularly as adolescents seek increasing independence [41]. There is a need to investigate whether acculturation in Hispanic families may modify the relationship between family functioning and adolescent weight outcomes [42–45]. The purpose of this study was twofold: 1) to examine longitudinal associations of two critical dimensions of family functioning (family cohesion and family conflict) with a modified BMI z-score in Mexican-origin adolescents, and 2) to explore the potential moderating effects of adolescent and parent acculturation on these relationships.
METHODS
Study Sample
Participants were members of a prospective cohort study, the Mexican American Tobacco Use in Children (MATCh) study, that examined factors associated with smoking initiation in Mexican-origin adolescents [46]. Participants enrolled when they were 11–13 years of age and were followed until 2011, with in-person assessments conducted in 2005–06 (baseline), 2008–09 (follow-up 1 [F1]) and 2010–11 (follow-up 2 [F2]). MATCh participants were identified from an ongoing adult cohort study, the Mano a Mano Mexican American Cohort Study (MACS) [47]. Recruitment and other details on the MACS cohort can be found elsewhere [47, 48]. Households with age-eligible participants for MATCh were identified from the MACS database and invited to participate. A total of 1,328 of 1,425 households contacted (93%) agreed, and one child from each household enrolled in the study. Bilingual interviewers obtained informed consent from participants’ parents and informed assent from participants. Additional details on MATCh recruitment are described elsewhere [46]. F1 was completed by 1,153 adolescents (87%), and F2 was completed by 1,001 adolescents (75%).
At each assessment, participants completed a survey in English or Spanish, depending on their preference, on a hand-held personal digital assistant. Trained interviewers measured adolescents’ height (to the nearest centimeter) and weight (to the nearest .5 pound) with shoes removed and in light clothing using a portable stadiometer and digital scale, respectively. While only a single measurement of height and weight was taken at baseline, duplicate measures were taken at F1 and F2 and averaged together at each time point. BMI (kg/m2) was then converted to modified BMI z-scores (BMIaz) using age- and gender-specific criteria from the Centers for Disease Control and Prevention [49]. Modified z-scores were developed to address the limitations of traditional BMI z-scores (BMIz), particularly for use with obese and severely obese children, in which the maximum BMIz attainable at a given sex and age is constrained. This can result in poor quantification of z-scores at very high BMI levels, as a wide range of BMIs may correspond with similar BMIz, depending on the age and sex of the child [49–54]. In comparison, BMIaz does not have an upper limit, and the values are not compressed into a fixed range. The modified z-scores correlate more strongly with measures of adiposity in obese and severely obese children and have been recommended for use with these populations in place of BMIz [55, 56]. Demographic (i.e., parents’ education and marital status) and measured height and weight data from the parent enrolled in the MACS were obtained from the MACS database. The Institutional Review Board approved all aspects of this study.
Measures
For this study, we used data from baseline, F1 and F2. BMIaz across the three time points was the dependent variable. Independent variables of interest included family cohesion and family conflict [57] assessed at the same three time points using the Family Life Questionnaire, which was validated in MATCh participants using Confirmatory Factor Analysis [58, 59]. The family cohesion subscale included four items (e.g., “In my family, we really help and support one another”; “We really get along well with each other”), and the family conflict subscale included four items (e.g., “We don’t often fight in my family”; “In my family, we hardly ever lose our tempers”). Response options were on a four-point Likert scale ranging from “strongly disagree” to “strongly agree.” The family conflict subscale was reverse coded so that higher scores indicated higher family conflict. Responses for both subscales were averaged to create a summary score (range 1–4). The family cohesion scale demonstrated very good internal reliability (Cronbach’s alpha=0.83), and the family conflict scale demonstrated lower reliability (Cronbach’s alpha=0.61). The scales were significantly inversely correlated (r=−0.38, −0.45, −0.43, p<0.001 at baseline, F1, and F2, respectively).
Indicators of acculturation included adolescent and parent linguistic acculturation, country of birth, and time in the U.S. Adolescent linguistic acculturation was assessed at baseline, FI, and F2 with the Brief Acculturation Scale for Hispanics [60], a four-item scale that ascertains language used when reading, speaking at home, speaking with friends, and thinking. Responses were averaged to create a summary score. In parents, linguistic acculturation was assessed for the MACS study (at a single time point) with eight items from the Bidimensional Acculturation Scale for Hispanics [61] that inquired about language use, language proficiency, and electronic media preference in English and Spanish, allowing for assessment in two cultural domains (i.e., U.S., Hispanic). Responses were averaged within cultural domain and then dichotomized according to established cut-points [61]. Both domains were combined and categorized to represent a single acculturation variable: high U.S. acculturation (high U.S. score, low Hispanic score); low U.S. acculturation (low U.S. score, high Hispanic score); and bicultural (high U.S. score, high Hispanic score). For both adolescents and parents, country of birth and years in the U.S. were combined into a single variable to reduce collinearity and ease interpretation (see Table 1).
Table 1.
Participant Demographics of 1,175 Mexican-origin adolescents in Houston, TX
| Total Sample N=1175 | Girls N=586 | Boys N=589 | ||
|---|---|---|---|---|
| Adolescent reported | ||||
| Adolescent Age Mean (SD) | Baseline | 12.4 (0.89) | 12.3 (0.87) | 12.4 (0.90) |
| Follow-up 1 | 14.9 (1.00) | 14.8 (1.00) | 14.9 (0.99) | |
| Follow-up 2 | 17.3 (1.08) | 17.3 (1.08) | 17.3 (1.08) | |
| Adolescent modified BMI z-score Mean (SD) | Baseline | 0.86 (1.35) | 0.75 (1.22) | 0.98 (1.45) |
| Follow-up 1 | 0.90 (1.36) | 0.74 (1.12) | 1.05(1.55) | |
| Follow-up 2 | 0.64 1.44) | 0.48 (1.19) | 0.81 (1.64) | |
| Adolescent BMI Mean (SD) | Baseline | 23.0 (5.75) | 22.8 (5.58) | 23.3 (5.90) |
| Follow-up 1 | 25.1 (6.36) | 24.7 (5.84) | 25.5 (6.82) | |
| Follow-up 2 | 25.7 (6.58) | 25.2 (6.29) | 26.2 (6.84) | |
| Adolescent Obese N (%) | Baseline | 373 (32.4) | 160 (27.9) | 213 (36.9) |
| Follow-up 1 | 318 (31.6) | 132 (26.2) | 186 (37.0) | |
| Follow-up 2 | 228 (26.8) | 91 (20.9) | 137 (32.9) | |
| Adolescent linguistic acculturation Mean (SD) | Baseline | 3.5 (0.89) | 3.5 (0.88) | 3.5 (0.90) |
| Follow-up 1 | 3.5 (0.72) | 3.5 (0.68) | 3.5 (0.75) | |
| Follow-up 2 | 3.4 (0.71) | 3.4 (0.68) | 3.4 (0.75) | |
| Adolescent time in the U.S. (baseline) N (%) | <5 years | 87 (7.4) | 44 (7.5) | 43 (7.3) |
| ≥5years | 216 (18.4) | 112 (19.1) | 104 (17.7) | |
| Born U.S. | 872 (74.2) | 430 (73.4) | 442 (75.0) | |
| Family Cohesion Mean (SD) | Baseline | 3.2 (0.48) | 3.2 (0.51) | 3.1 (0.45) |
| Follow-up 1 | 3.1 (0.49) | 3.1 (0.52) | 3.1 (0.45) | |
| Follow-up 2 | 3.2 (0.51) | 3.2 (0.53) | 3.2 (0.49) | |
| Family Conflict Mean (SD) | Baseline | 2.4 (0.55) | 2.4 (0.57) | 2.4 (0.54) |
| Follow-up 1 | 2.4 (0.55) | 2.4 (0.56) | 2.3 (0.54) | |
| Follow-up 2 | 2.3 (0.55) | 2.3 (0.54) | 2.2 (0.55) | |
| Parent reported | Total Sample | Girls | Boys | |
| Parent BMI Mean (SD) Parent education N (%) | -- | 30.1 (6.24) | 30.2 (6.39) | 30.1 (6.09) |
| Less than high school | 759 (64.6) | 376 (64.2) | 383 (65.0) | |
| High school or equivalent | 201 (17.1) | 103 (17.6) | 98 (16.6) | |
| Greater than high school | 215 (18.3) | 107 (18.3) | 108 (18.3) | |
| Married N (%) | -- | 1034 (88.0) | 511 (87.2) | 523 (88.8) |
| Parent time in the U.S. N (%) | < 5years | 118 (10.0) | 57 (9.7) | 61 (10.4) |
| 5–15 years | 471 (40.1) | 244 (41.6) | 227 (38.5) | |
| >15 years | 387 (32.9) | 188 (32.1) | 199 (33.8) | |
| Born U.S. | 199 (16.9) | 97 (16.6) | 102 (17.3) | |
| Parent linguistic acculturation N (%) | Low U.S. Acculturation | 804 (68.4) | 401 (68.4) | 403 (68.4) |
| High U.S. Acculturation | 77 (6.6) | 39 (6.7) | 38 (6.5) | |
| Bicultural | 294 (25.0) | 146 (24.9) | 148 (25.1) | |
Analysis
Analyses assessed longitudinal associations of family functioning variables with adolescent BMIaz. For time-varying predictors of interest (i.e., family cohesion, family conflict), we created two variables to disaggregate the between- (mean) and within-person (or individual deviation) components, an approach used previously in studies of adolescent obesity [62, 63]. The first variable represented the mean value of each time-varying predictor over the three time points for each participant (i.e., between-person differences). The second variable represented the deviation from that mean of each participant (i.e., within-person differences) for each time point [64]. To facilitate interpretation, all continuous variables, except for the within-person family cohesion and family conflict, were centered by subtracting the grand mean of the observed values. Baseline mean-centered age, henceforth referred to as age, served as the index for time.
Linear mixed models were used for all analyses, as they account for clustering of observations within individuals, allow for the inclusion of time-invariant and time-varying predictors, model individual-specific associations through the inclusion of random slopes and intercepts, and flexibly accommodate missing data [65]. We used linear mixed models with individual-specific random intercepts and random slopes that were allowed to be correlated. The first set of models regressed BMIaz on the mean and deviation variables for family cohesion and family conflict, age, and interaction terms for family cohesion and conflict by age. Interactions enabled examination of whether the change in BMIaz over time (i.e., as adolescents aged) varied according to family functioning variables. Models were stratified by gender and controlled for adolescents’ and parents’ acculturation, adolescents’ and parents’ time in the U.S., and parents’ marital status, BMI, and education, as well as household size. We did not include income due to considerable missingness (approximately 40%) in the MACS database. Nonsignificant interactions (P≥0.05) were removed, and the models were reassessed. We then ran exploratory models to examine whether associations of family cohesion and family conflict with BMIaz differed by acculturation variables, with interaction terms for each acculturation variable examined in separate models. Only interaction terms that were statistically significant (P<0.05) in these individual models were retained. Analyses were performed using the “lme4” package in the R statistical computing environment (R Version 3.3.2) [66].
RESULTS
The sample included 1,175 adolescents. Of the original 1,328 participants at baseline, 135 had missing parent data, 17 had invalid or missing anthropometric data, and 1 had missing demographic data. Girls who were excluded were more likely to have parents who were low U.S. acculturated than girls who were not excluded (83.3% vs. 68.4%, p=0.04). Boys who were excluded were slightly older at F1 and F2 than boys who were not excluded (14.9 years vs. 14.6 years, p=0.02 at F1; 17.3 years vs 16.8 years, p=0.01 at F2), and were less likely to have married parents (76.4% vs. 88.8%, p=0.02). There were no statistically significant differences in those included and excluded for baseline, F1 and F2 BMIaz, and no significant differences in baseline BMIaz in participants who had missing data at F1 or F2 versus those who had complete follow-up data.
Characteristics of the sample are shown in Table 1. Participants were evenly distributed by gender with a baseline mean age of 12.4 years. The majority of adolescents were born in the U.S. (74.2%), whereas 16.9% of parents were born in the U.S. Among parents, 6.6% were categorized as high U.S. acculturated, 68.6% were high Hispanic acculturated (low U.S. acculturated), and 25% were bicultural. Adolescent BMIaz fluctuated over the study period, with mean values of 0.86, 0.90 and 0.64 at baseline, F1, and F2, respectively.
Main Analyses: Association of family cohesion and conflict with adolescent BMI
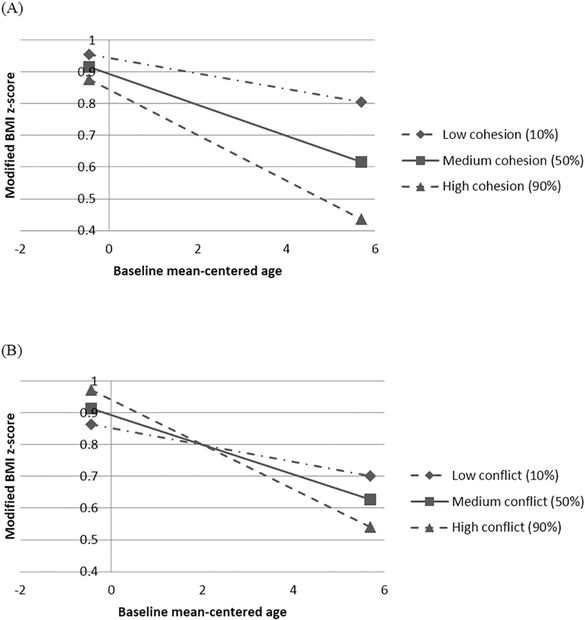
Table 2 presents the results of the primary analyses in girls that tested the main effects of family cohesion and conflict on adolescent BMIaz along with their interactions with age. The deviation of family cohesion was inversely associated with BMIaz such that an adolescent girl whose family cohesion increased by one unit during the study period had an average decrease in BMIaz of 0.09 (P<0.05). The interactions between mean family cohesion and mean family conflict with age were statistically significant, whereas the interactions involving the deviations of these variables with age were not (non-significant interactions were not retained). Results indicate that girls’ BMIaz declined with age, and that higher levels of mean cohesion and mean conflict were associated with steeper declines (Figures 1a and b).
Table 2.
Girls’ Longitudinal Model Predicting Adolescent modified BMI z-score
| Model 1a | Model 2b | |||||
|---|---|---|---|---|---|---|
| Variables | β | (SE) | 95% CI | β | (SE) | 95% CI |
| Adolescent age | −0.05*** | 0.01 | −0.06, −0.03 | −0.05*** | 0.01 | −0.06, −0.03 |
| Family Cohesion | ||||||
| Deviation | −0.09* | 0.04 | −0.16, −0.01 | −0.05 | 0.05 | −0.14, 0.04 |
| Mean | −0.10 | 0.13 | −0.35, 0.16 | −0.10 | 0.13 | −0.36, 0.15 |
| Mean × Age | −0.04* | 0.02 | −0.09, −0.01 | −0.04* | 0.02 | −0.08, −0.01 |
| Family Conflict | ||||||
| Deviation | 0.03 | 0.03 | −0.04, 0.09 | 0.02 | 0.03 | −0.04, 0.09 |
| Mean | 0.08 | 0.13 | −0.16, 0.32 | 0.08 | 0.13 | −0.16, 0.33 |
| Mean × Age | −0.04* | 0.02 | −0.08, −0.01 | −0.04* | 0.02 | −0.08, −0.01 |
| Interactions between Family Cohesion X Acculturation | ||||||
| Deviation X Parent Low U.S. Acculturation (Ref) | -- | -- | -- | -- | ||
| Deviation X Parent High U.S. Acculturation | -- | -- | −0.35* | 0.14 | −0.63, −0.07 | |
| Deviation X Parent Bicultural | -- | -- | −0.04 | 0.08 | −0.20, 0.12 | |
Notes:
Model controlled for household size, parent marital status, parent BMI, parent education, parent acculturation, adolescent age (shown in the table) and adolescent acculturation;
Model controlled for household size, parent marital status, parent BMI, parent education and adolescent age (shown in the table);
p<0.05;
p<0.01;
p<.001; this study was conducted in Houston, TX from 2005–06 to 2010–11
Figure 1. Interactions of age and family functioning variables on girl’s modified BMI z-score.
(A) BMI z-score trajectories for girls with low, medium, and high levels of mean family cohesion*(B) BMI z-score trajectories for girls with low, medium, and high levels of mean family conflict** We used the 10th, 50th and 90th percentiles mean conflict to represent the low, medium and high levels of family conflict, respectively; this study was conducted in Houston, TX from 2005–06 to 2010–11
In boys, BMIaz also declined with age, yet no significant relationships were observed between any measure of family functioning and adolescent BMIaz (Table 3).
Table 3.
Boys’ Longitudinal Model Predicting Adolescent modified BMI z-score
| Model 1 | |||
|---|---|---|---|
| Variables | β | (SE) | 95% CI |
| Age | −0.03** | 0.01 | −0.05, −0.01 |
| Family Cohesion | |||
| Deviation | −0.03 | 0.05 | −0.13, 0.07 |
| Mean | −0.10 | 0.17 | −0.42, 0.23 |
| Family Conflict | |||
| Deviation | 0.01 | 0.04 | −0.07, 0.09 |
| Mean | −0.17 | 0.15 | −0.47, 0.13 |
Notes: Model controlled for household size, parent marital status, parent BMI, parent education, parent acculturation, adolescent age and adolescent acculturation;
p<.001; ; this study was conducted in Houston, TX from 2005–06 to 2010–11
Exploratory Analyses: Moderating effect of acculturation
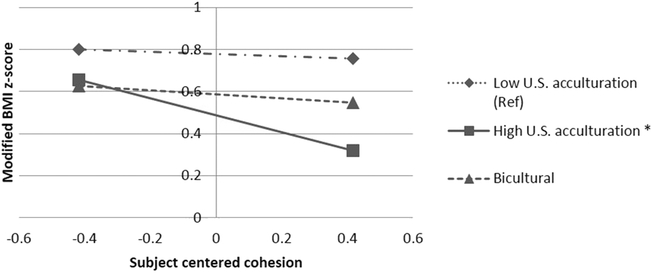
In girls, parental linguistic acculturation modified the relationship between within-person deviation in family cohesion and BMIaz such that high parental U.S. acculturation was associated with a stronger inverse association (Figure 2a). A one-unit increase in family cohesion during the study period was associated with a decrease of 0.40 in BMIaz in a girl whose parents were highly U.S. acculturated and a decrease of 0.052 and 0.095 in BMIaz in a girl whose parents were low-acculturated and bicultural, respectively. Adolescent acculturation variables and adolescent and parent time in the U.S were not significant effect modifiers.
Figure 2. Interaction of deviations in within-person family cohesion and parent’s linguistic acculturation on girl’s modified BMI z-score.
* Interaction effect is significant at P<0.05; this study was conducted in Houston, TX from 2005–06 to 2010–11
There were no significant interactions between any family functioning and acculturation variables in boys.
DISCUSSION
In this study, we observed significant longitudinal associations between family functioning variables and adolescent girls’ BMIaz. Specifically, higher levels of mean family cohesion and mean family conflict over the study were each associated with steeper declines in BMIaz. Additionally, associations of within-person increases in family cohesion with BMIaz varied in magnitude, according to parental linguistic acculturation. These longitudinal findings highlight the potential importance of the family’s social and cultural contexts to adolescent girls’ BMI.
Our finding that both mean and within-person deviations in family cohesion were inversely associated with BMIaz in girls is consistent with the literature. Previous studies have generally found that higher levels of family cohesion are associated with better dietary habits [17, 67–69], higher physical activity [70, 71], and lower BMI in adolescents [72, 73]. The longitudinal design of our study and the focus on a Mexican-origin population bolster the evidence that family cohesion can affect adolescent BMI, at least among girls. Surprisingly, mean family conflict was also inversely associated with BMIaz in girls. This differs from previous studies [16, 22, 74, 75] and underscores the need for further research in this population. While the reasons for this association are unclear, the effects of family interactions including teasing and pressure to lose weight on girls’ emotional health, body image, and weight-related behaviors warrant further investigation [76, 77].
In contrast to girls, Mexican-origin adolescent boys’ BMI may not be strongly affected by family cohesion and family conflict. Although some studies have observed significant associations with family functioning [16], our findings are consistent with other studies [18, 23, 24] and may indicate that other aspects of the family context, such as parent BMI [78–80], parenting style [15], or consistent family meals together [81], have more influence on adolescent boys’ BMI. Similarly, family conflict in boys may be more strongly related to other risk factors such as smoking and alcohol use [58, 82, 83].
This study was unique in its assessment of possible interactions between family functioning and acculturation variables. Parental U.S. acculturation was an effect modifier with significant interactions in girls involving the within-person deviations in family cohesion. The inverse association between the within-person deviation in family cohesion and BMIaz was much stronger in girls whose parents were highly U.S. acculturated relative to those who were less acculturated or bicultural. Although this study did not allow for the examination of mechanisms underlying these relationships, the literature may offer some insight. First, poverty is strongly associated with increased risk of obesity in children and adolescents [84] and is more concentrated among less acculturated Hispanics. For Hispanic girls with less acculturated parents, this may offset positive influences of family cohesion on adolescent weight outcomes. Second, acculturation may be associated with parents’ body image perception of their children, which could have implications for children’s actual weight status [85]. Research has found that low-income Hispanic mothers and mothers in Mexico prefer their children to have a heavier body shape [86]. If such traditional beliefs are more prevalent among bicultural and low U.S. acculturated parents, this may contribute to the differential associations of family cohesion with adolescent weight outcomes observed. Although speculative, this offers potential pathways for further investigation.
Notably, BMIaz declined between F1 and F2 in both boys and girls, although BMI continued to increase. While this contrasts with national trends [1, 87, 88], other studies have documented declines in BMIaz and obesity during the latter teenage years [89, 90]. The reasons for the decline are not clear but may pertain to growth patterns, pubertal maturation [91], body dissatisfaction, social pressures to lose weight [92], and possibly regression to the mean over time [93]. Importantly, the high baseline prevalence of obesity indicates that gains in adiposity took place prior to adolescence.
Future research and practice
Results from this study have implications for the design of culturally appropriate family-based interventions in Mexican-origin adolescent girls. Few interventions targeting obese Hispanic adolescents have intervened upon family system components [94], yet family cohesion may be important to focus on through activities and counseling that promote support and bonding among family members. Although family cohesion may be less relevant for adolescent Mexican-origin boys, other actionable variables within the family environment can be considered, such as instrumental support from parents or the family’s food culture [95]. Interventions should also consider levels of acculturation within the family [96]. Further research is needed to better explicate the longitudinal relationships between family functioning, acculturation, and adolescent weight outcomes in understudied populations such as Mexican-origin adolescents.
Strengths and Limitations
This study had several limitations. First, the purpose of the MATCh study was to examine smoking initiation in Mexican-origin adolescents, and thus it was not designed or powered to test associations of family functioning with BMIaz. Nonetheless, the study presented an opportunity to expand the research of an understudied population to include investigation in this new area, recognizing the limitations of this approach. Further research is needed to better elucidate the pathways linking family cohesion and conflict with adolescent weight-related outcomes to inform obesity prevention efforts in this population. Second, the lower internal reliability (α=0.61) of the family conflict subscale may indicate a need for further refinement of this measure in this population. Third, we tested multiple interaction terms, making it possible that the significant interaction between family functioning and parental linguistic acculturation was due to chance alone. Because of the exploratory nature of these analyses, we did not adjust for multiple comparisons [97]. Fourth, the findings observed here may not generalize to other Hispanic subgroups or to adolescents of a different race/ethnicity. Fifth, in this study we used the modified BMI z-score developed by the CDC to overcome recognized limitations of BMIz that hinder valid correlations with adiposity in severely obese children [49, 98]. However, the most appropriate measure for tracking BMI over time remains unclear and may depend on the population studied and degree of obesity [99]. Finally, our results showed small to moderate effect sizes on BMIaz. Thus, other factors likely exert a stronger effect, such as attitudes towards and support for weight-related health behaviors, access to healthy foods, and opportunities for physical activity. Despite these limitations, this study has several important strengths. This study capitalized on two large, linked, and unique datasets of an understudied population of Mexican-origin adolescents and their parents. We were able to examine repeated measures of key predictor and outcome variables over a six-year period, with high participation rates across all time points. We disaggregated the effects of family cohesion and family conflict into between- and within-person components. This facilitated understanding of the longitudinal, independent contributions of the mean values and deviations of family functioning.
Conclusion
This study lends evidence to the body of work aimed at understanding the potential effects of family functioning on adolescent weight outcomes, particularly in Mexican-origin youth. Our results suggest that family cohesion, family conflict, and parental language acculturation are important variables to consider in examinations of family influences on adolescent girls’ weight outcomes.
Acknowledgements
Disclaimer: The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Cancer Institute or the National Institutes of Health.
This work was supported by the National Cancer Institute [Cancer Center Support Grant P30 CA016672, R01CA105203 and K07 CA126988], the American Cancer Society [MRSG-13–145-01], and the UTHealth School of Public Health Cancer Education and Career Development Program through a National Cancer Institute/National Institutes of Health Grant [R25CA57712], and the Department for Health Promotion & Prevention Research. The Mexican American Cohort Study receives funds collected pursuant to the Comprehensive Tobacco Settlement of 1998, and appropriated by the 76th legislature to The University of Texas M. D. Anderson Cancer Center, from the Caroline W. Law Fund for Cancer Prevention, and by the Duncan Family Institute for Cancer Prevention and Risk Assessment.
Dr. Heredia and Dr. Strong conceived of the research question, developed the analytic strategy, and drafted the manuscript. Drs. Wilkinson, Bondy, and Forman were involved in directing the implementation of the parent studies, including quality assurance and control, and reviewed and edited the manuscript. Drs. Christie and Wang conducted the analyses and assisted with the methods and results sections, as well as the tables and figures. Drs. Daniel and Zhao are currently involved with the parent studies and reviewed and edited the manuscript.
Abbreviations
- BMI
Body Mass Index
- MATCh
Mexican American Tobacco Use in Children
- MACS
Mano a Mano Mexican American Cohort Study
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest Statement: The authors declare that there are no conflicts of interest
References
- 1.Ogden CL, et al. , Trends in obesity prevalence among children and adolescents in the United States, 1988–1994 through 2013–2014. JAMA 2016. 315(21): p. 2292–2299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Herman KM, et al. , Tracking of obesity and physical activity from childhood to adulthood: the Physical Activity Longitudinal Study. Int J Pediatr Obes, 2009. 4(4): p. 281–8. [DOI] [PubMed] [Google Scholar]
- 3.Biro FM and Wien M, Childhood obesity and adult morbidities. Am J Clin Nutr, 2010. 91(5): p. 1499s–1505s. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Freedman DS, et al. , Cardiovascular risk factors and excess adiposity among overweight children and adolescents: the Bogalusa Heart Study. J Pediatr, 2007. 150(1): p. 12–17 e2. [DOI] [PubMed] [Google Scholar]
- 5.World Cancer Research Fund / American Institute for Cancer Research, Food, Nutrition, Physical Activity, and the Prevention of Cancer: a Global Perspective. 2007, AICR: Washington, DC. [Google Scholar]
- 6.Crossman A, Sullivan DA, and Benin M, The family environment and American adolescents’ risk of obesity as young adults. Social science & medicine, 2006. 63(9): p. 2255–2267. [DOI] [PubMed] [Google Scholar]
- 7.Gruber KJ and Haldeman LA, Using the family to combat childhood and adult obesity. Prev Chronic Dis, 2009. 6(3): p. A106. [PMC free article] [PubMed] [Google Scholar]
- 8.Broderick CF, Understanding Family Process: Basics of Family Systems Theory. 1993, Newbury Park, CA: Sage Publications. [Google Scholar]
- 9.Rhee K, Childhood Overweight and the Relationship between Parent Behaviors, Parenting Style, and Family Functioning. The ANNALS of the American Academy of Political and Social Science, 2008. 615(1): p. 11–37. [Google Scholar]
- 10.Pearson N, Biddle SJ, and Gorely T, Family correlates of fruit and vegetable consumption in children and adolescents: a systematic review. Public Health Nutr, 2009. 12(2): p. 267–83. [DOI] [PubMed] [Google Scholar]
- 11.Trost SG, et al. , Evaluating a model of parental influence on youth physical activity. Am J Prev Med, 2003. 25(4): p. 277–82. [DOI] [PubMed] [Google Scholar]
- 12.Berge JM, A review of familial correlates of child and adolescent obesity: what has the 21st century taught us so far? Int J Adolesc Med Health, 2009. 21(4): p. 457–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Olvera N and Power TG, Brief report: parenting styles and obesity in Mexican American children: a longitudinal study. J Pediatr Psychol, 2010. 35(3): p. 243–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sleddens EF, et al. , General parenting, childhood overweight and obesity-inducing behaviors: a review. Int J Pediatr Obes, 2011. 6(2–2): p. e12–27. [DOI] [PubMed] [Google Scholar]
- 15.Berge JM, et al. , Parenting style as a predictor of adolescent weight and weight-related behaviors. Journal of Adolescent Health, 2010. 46(4): p. 331–338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Halliday J, et al. , The relationship between family functioning and child and adolescent overweight and obesity: a systematic review. International Journal of Obesity, 2014. 38(4): p. 480–493. [DOI] [PubMed] [Google Scholar]
- 17.Franko DL, et al. , What’s love got to do with it? Family cohesion and healthy eating behaviors in adolescent girls. International journal of eating disorders, 2008. 41(4): p. 360–367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mendelson BK and White DR, Adolescents’ weight, sex, and family functioning. International Journal of Eating Disorders, 1995. 17(1): p. 73–79. [DOI] [PubMed] [Google Scholar]
- 19.Zeller MH, et al. , Controlled study of critical parent and family factors in the obesigenic environment. Obesity, 2007. 15(1): p. 126–126. [DOI] [PubMed] [Google Scholar]
- 20.Bigman G, et al. , Family Cohesion and Moderate-to-Vigorous Physical Activity Among Mexican Origin Adolescents: A Longitudinal Perspective. J Phys Act Health, 2015. 12(7): p. 1023–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hooper LM, et al. , The Fit Families pilot study: preliminary findings on how parental health and other family system factors relate to and predict adolescent obesity and depressive symptoms. Journal of Family Therapy, 2014. 36(3): p. 308–336. [Google Scholar]
- 22.Hooper LM, Burnham JJ, and Richey R, Select parent and family system correlates of adolescent current weight status: A pilot study. The Family Journal, 2009. 17(1): p. 14–21. [Google Scholar]
- 23.Berge JM, et al. , Family functioning: associations with weight status, eating behaviors, and physical activity in adolescents. Journal of adolescent health, 2013. 52(3): p. 351–357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Haines J, et al. , Family functioning and quality of parent-adolescent relationship: cross-sectional associations with adolescent weight-related behaviors and weight status. International Journal of Behavioral Nutrition and Physical Activity, 2016. 13(1): p. 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hasenboehler K, et al. , Family structure, body mass index, and eating behavior. International Journal of Eating Disorders, 2009. 42(4): p. 332–338. [DOI] [PubMed] [Google Scholar]
- 26.Stradmeijer M, et al. , Family functioning and psychosocial adjustment in overweight youngsters. Int J Eat Disord, 2000. 27(1): p. 110–4. [DOI] [PubMed] [Google Scholar]
- 27.Gibson LY, et al. , The role of family and maternal factors in childhood obesity. Medical Journal of Australia, 2007. 186(11): p. 591. [DOI] [PubMed] [Google Scholar]
- 28.Ennis SR, Rios-Vargas M, and Albert NG, The Hispanic population: 2010 (2010 Census Briefs C2010BR-04). Washington, DC: US Census Bureau; 2011. [Google Scholar]
- 29.Lara M, et al. , Acculturation and Latino health in the United States: a review of the literature and its sociopolitical context. Annu. Rev. Public Health, 2005. 26: p. 367–397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Parke RD and R. Buriel, Socialization in the family: Ethnic and ecological perspectives Handbook of child psychology, 1998. [Google Scholar]
- 31.Kitzman-Ulrich H, et al. , The integration of a family systems approach for understanding youth obesity, physical activity, and dietary programs. Clinical child and family psychology review, 2010. 13(3): p. 231–253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rollins BY, Belue RZ, and Francis LA, The beneficial effect of family meals on obesity differs by race, sex, and household education: the national survey of children’s health, 2003–2004. Journal of the American Dietetic Association, 2010. 110(9): p. 1335–1339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sen B, Frequency of family dinner and adolescent body weight status: evidence from the national longitudinal survey of youth, 1997. Obesity, 2006. 14(12): p. 2266–2276. [DOI] [PubMed] [Google Scholar]
- 34.Olvera N and Power TG, Brief report: parenting styles and obesity in Mexican American children: a longitudinal study. Journal of pediatric psychology, 2010. 35(3): p. 243–249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gordon-Larsen P, et al. , Acculturation and overweight-related behaviors among Hispanic immigrants to the US: the National Longitudinal Study of Adolescent Health. Social science & medicine, 2003. 57(11): p. 2023–2034. [DOI] [PubMed] [Google Scholar]
- 36.Liu J, et al. , Acculturation, physical activity, and obesity among Hispanic adolescents. Ethnicity & health, 2009. 14(5): p. 509–525. [DOI] [PubMed] [Google Scholar]
- 37.Baer JC and Schmitz MF, Ethnic differences in trajectories of family cohesion for Mexican American and Non-Hispanic White adolescents. Journal of Youth and Adolescence, 2007. 36(4): p. 583–592. [Google Scholar]
- 38.Miranda AO, E. D., and M. Firpo-Jimenez, Differences in family cohesion, adaptability, and environment among Latino families in dissimilar stages of acculturation. The Family Journal, 2000. 8: p. 341–50. [Google Scholar]
- 39.Romero AJ and Roberts RE, Stress within a bicultural context for adolescents of Mexican descent. Cultural Diversity and Ethnic Minority Psychology, 2003. 9(2): p. 171. [DOI] [PubMed] [Google Scholar]
- 40.Martinez CR, Effects of differential family acculturation on Latino adolescent substance use. Family Relations, 2006. 55(3): p. 306–317. [Google Scholar]
- 41.Wagner KD, et al. , The role of acculturation, parenting, and family in Hispanic/Latino adolescent substance use: Findings from a qualitative analysis. Journal of Ethnicity in Substance Abuse, 2008. 7(3): p. 304–327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Niemeier BS, Hektner JM, and Enger KB, Parent participation in weight-related health interventions for children and adolescents: a systematic review and meta-analysis. Preventive medicine, 2012. 55(1): p. 3–13. [DOI] [PubMed] [Google Scholar]
- 43.McLean N, et al. , Family involvement in weight control, weight maintenance and weight-loss interventions: a systematic review of randomised trials. International journal of obesity, 2003. 27(9): p. 987–1005. [DOI] [PubMed] [Google Scholar]
- 44.Branscum P and M.w Sharma, A systematic analysis of childhood obesity prevention interventions targeting Hispanic children: lessons learned from the previous decade. Obesity Reviews, 2011. 12(5): p. e151–e158. [DOI] [PubMed] [Google Scholar]
- 45.Golan M and Crow S, Targeting parents exclusively in the treatment of childhood obesity: Long-Term results. Obesity research, 2004. 12(2): p. 357–361. [DOI] [PubMed] [Google Scholar]
- 46.Wilkinson AV, et al. , Correlates of susceptibility to smoking among Mexican origin youth residing in Houston, Texas: a cross-sectional analysis. BMC Public Health, 2008. 8: p. 337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Chow WH, et al. , Cohort Profile: The Mexican American Mano a Mano Cohort. Int J Epidemiol, 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wilkinson AV, et al. , Effects of nativity, age at migration, and acculturation on smoking among adult Houston residents of Mexican descent. Am J Public Health, 2005. 95(6): p. 1043–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Centers for Disease Control & Prevention, Modified z-scores in the CDC growth charts Homepage of Centers for Disease Control and Prevention.[Online]. Available:(4 July 2013), 2017. [Google Scholar]
- 50.Freedman DS, et al. , Longitudinal changes in BMI z-scores among 45 414 2–4-year olds with severe obesity. Ann Hum Biol, 2017. 44(8): p. 687–692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Freedman DS, et al. , The Limitations of Transforming Very High Body Mass Indexes into z-Scores among 8.7 Million 2- to 4-Year-Old Children. J Pediatr, 2017. 188: p. 50–56.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Freedman DS, et al. , BMI z-Scores are a poor indicator of adiposity among 2- to 19-year-olds with very high BMIs, NHANES1999–2000 to 2013–2014. Obesity (Silver Spring), 2017. 25(4): p. 739–746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Berkey CS and Colditz GA, Adiposity in adolescents: change in actual BMI works better than change in BMI z score for longitudinal studies. Ann Epidemiol, 2007. 17(1): p. 44–50. [DOI] [PubMed] [Google Scholar]
- 54.Cole TJ, et al. , What is the best measure of adiposity change in growing children: BMI, BMI %, BMI z-score or BMI centile? Eur J Clin Nutr, 2005. 59(3): p. 419–25. [DOI] [PubMed] [Google Scholar]
- 55.Freedman DS and Berenson GS, Tracking of BMI z Scores for Severe Obesity. Pediatrics, 2017. 140(3). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Chambers M, et al. , Growth Tracking in Severely Obese or Underweight Children. Pediatrics, 2017. 140(6). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Foxcroft DR and Lowe G, Adolescent drinking, smoking and other substance use involvement: links with perceived family life. Journal of adolescence, 1995. 18(2): p. 159–177. [Google Scholar]
- 58.Rajesh V, et al. , Smoking initiation among Mexican heritage youth and the roles of family cohesion and conflict. Journal of Adolescent Health, 2015. 57(1): p. 24–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Rajesh V, Parental influence on adolescent smoking initiation among Mexican origin youth. 2011, The University of Texas School of Public Health. [Google Scholar]
- 60.Norris A, Ford K, and Bova C, Psychometrics of a brief acculturation scale for Hispanics in a probability sample of urban Hispanic adolescents and young adults. 1996. [Google Scholar]
- 61.Marín G and Gamba RJ, A new measurement of acculturation for Hispanics: The Bidimensional Acculturation Scale for Hispanics (BAS). Hispanic Journal of Behavioral Sciences, 1996. 18(3): p. 297–316. [Google Scholar]
- 62.Laska MN, et al. , Longitudinal associations between key dietary behaviors and weight gain over time: transitions through the adolescent years. Obesity (Silver Spring), 2012. 20(1): p. 118–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Stevens J, et al. , Objectively assessed associations between physical activity and body composition in middle-school girls: the Trial of Activity for Adolescent Girls. Am J Epidemiol, 2007. 166(11): p. 1298–305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Howard AL, Leveraging Time-Varying Covariates to Test Within-and Between-Person Effects and Interactions in the Multilevel Linear Model. Emerging Adulthood, 2015: p. 2167696815592726. [Google Scholar]
- 65.Gibbons RD, Hedeker D, and DuToit S, Advances in analysis of longitudinal data. Annu Rev Clin Psychol, 2010. 6: p. 79–107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.R Core Team, R: A language and environment for statistical computing. 2015, R Foundation for Statistical Computing: Vienna, Austria. [Google Scholar]
- 67.Welsh EM, French SA, and Wall M, Examining the relationship between family meal frequency and individual dietary intake: does family cohesion play a role? Journal of nutrition education and behavior, 2011. 43(4): p. 229–235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Cromley T, et al. , Parent and family associations with weight-related behaviors and cognitions among overweight adolescents. Journal of Adolescent Health, 2010. 47(3): p. 263–269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Mellin AE, et al. , Unhealthy behaviors and psychosocial difficulties among overweight adolescents: the potential impact of familial factors. Journal of adolescent health, 2002. 31(2): p. 145–153. [DOI] [PubMed] [Google Scholar]
- 70.Ornelas IJ, Perreira KM, and Ayala GX, Parental influences on adolescent physical activity: a longitudinal study. The International Journal of Behavioral Nutrition and Physical Activity, 2007. 4(1): p. 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Bigman G, et al. , Family Cohesion and Moderate-to-Vigorous Physical Activity Among Mexican Origin Adolescents: A Longitudinal Perspective. Journal of physical activity & health, 2015. 12(7). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Beck S and Terry K, A comparison of obese and normal-weight families’ sychological characteristics. The American Journal of Family Therapy, 1985. 13(3): p. 55–59. [Google Scholar]
- 73.Banis HT, et al. , Psychological and social adjustment of obese children and their families. Child: care, health and development, 1988. 14(3): p. 157–173. [DOI] [PubMed] [Google Scholar]
- 74.Hanson CL, et al. , Family relations, coping styles, stress, and cardiovascular disease risk factors among children and their parents. Family Systems Medicine, 1990. 8(4): p. 387. [Google Scholar]
- 75.Hernandez DC and Pressler E, Gender disparities among the association between cumulative family-level stress & adolescent weight status. Preventive medicine, 2015. 73: p. 60–66. [DOI] [PubMed] [Google Scholar]
- 76.Toro J, et al. , Eating disorders and body image in Spanish and Mexican female adolescents. Social psychiatry and psychiatric epidemiology, 2006. 41(7): p. 556–565. [DOI] [PubMed] [Google Scholar]
- 77.Ata RN, Ludden AB, and Lally MM, The effects of gender and family, friend, and media influences on eating behaviors and body image during adolescence. Journal of Youth and Adolescence, 2007. 36(8): p. 1024–1037. [Google Scholar]
- 78.Butte NF, et al. , Metabolic and behavioral predictors of weight gain in Hispanic children: the Viva la Familia Study. The American journal of clinical nutrition, 2007. 85(6): p. 1478–1485. [DOI] [PubMed] [Google Scholar]
- 79.Elder JP, et al. , Individual, Family, and Community Environmental Correlates of Obesity in Latino Elementary School Children*. Journal of School Health, 2010. 80(1): p. 20–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Lin B, Huang C, and French S, Factors associated with women’s and children’s body mass indices by income status. International Journal of Obesity, 2004. 28(4): p. 536–542. [DOI] [PubMed] [Google Scholar]
- 81.Taveras EM, et al. , Family dinner and adolescent overweight. Obesity, 2005. 13(5): p. 900–906. [DOI] [PubMed] [Google Scholar]
- 82.Baer PE, et al. , Stress, coping, family conflict, and adolescent alcohol use. Journal of behavioral medicine, 1987. 10(5): p. 449–466. [DOI] [PubMed] [Google Scholar]
- 83.Bray JH, et al. , Developmental, family, and ethnic in influences on adolescent alcohol usage: A growth curve approach. Journal of Family Psychology, 2001. 15(2): p. 301. [DOI] [PubMed] [Google Scholar]
- 84.Rogers R, et al. , The relationship between childhood obesity, low socioeconomic status, and race/ethnicity: lessons from Massachusetts. Childhood Obesity, 2015. 11(6): p. 691–695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Olvera N, Suminski R, and Power TG, Intergenerational perceptions of body image in Hispanics: Role of BMI, gender, and acculturation. Obesity, 2005. 13(11): p. 1970–1979. [DOI] [PubMed] [Google Scholar]
- 86.Contento IR, Basch C, and Zybert P, Body image, weight, and food choices of Latina women and their young children. Journal of nutrition education and behavior, 2003. 35(5): p. 236–248. [DOI] [PubMed] [Google Scholar]
- 87.Kimm SY, et al. , Obesity development during adolescence in a biracial cohort: the NHLBT Growth and Health Study. Pediatrics, 2002. 110(5): p. e54. [DOI] [PubMed] [Google Scholar]
- 88.Gordon-Larsen P, et al. , Five-year obesity incidence in the transition period between adolescence and adulthood: the National Longitudinal Study of Adolescent Health. Am J Clin Nutr, 2004. 80(3): p. 569–75. [DOI] [PubMed] [Google Scholar]
- 89.Araujo J, et al. , Longitudinal changes in adiposity during adolescence: a population-based cohort. BMJ Open, 2014. 4(6): p. e004380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Popkin BM and Udry JR, Adolescent obesity increases significantly in second and third generation U.S. immigrants: the National Longitudinal Study of Adolescent Health. J Nutr, 1998. 128(4): p. 701–6. [DOI] [PubMed] [Google Scholar]
- 91.Loomba-Albrecht LA and Styne DM, Effect of puberty on body composition. Curr Opin Endocrinol Diabetes Obes, 2009. 16(1): p. 10–5. [DOI] [PubMed] [Google Scholar]
- 92.Calzo JP, et al. , The development of associations among body mass index, body dissatisfaction, and weight and shape concern in adolescent boys and girls. J Adolesc Health, 2012. 51(5): p. 517–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Cockrell Skinner A, Goldsby TU, and Allison DB, Regression to the Mean: A Commonly Overlooked and Misunderstood Factor Leading to Unjustified Conclusions in Pediatric Obesity Research. Child Obes, 2016. 12(2): p. 155–8. [DOI] [PubMed] [Google Scholar]
- 94.Kitzman-Ulrich H, et al. , An adolescent weight-loss program integrating family variables reduces energy intake. Journal of the American Dietetic Association, 2009. 109(3): p. 491–496. [DOI] [PubMed] [Google Scholar]
- 95.Heredia NI, et al. , Association of parental social support with energy balance-related behaviors in low-income and ethnically diverse children: a cross-sectional study. BMC public health, 2016. 16(1): p. 1182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Miranda AO, et al. , Latino families: The relevance of the connection among acculturation, family dynamics, and health for family counseling research and practice. The Family Journal, 2006. 14(3): p. 268–273. [Google Scholar]
- 97.Schochet PZ, Technical Methods Report: Guidelines for Multiple Testing in Impact Evaluations. NCEE 2008–4018 National Center for Education Evaluation and Regional Assistance, 2008. [Google Scholar]
- 98.Chambers M, et al. , Growth Tracking in Severely Obese or Underweight Children. Pediatrics, 2017: p. e20172248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Kelly AS and Daniels SR, Rethinking the Use of Body Mass Index z-Score in Children and Adolescents with Severe Obesity: Time to Kick It to the Curb? J Pediatr, 2017. 188: p. 7–8. [DOI] [PubMed] [Google Scholar]