Abstract
Injustice perception has emerged as a risk factor for problematic musculoskeletal pain outcomes. Despite the prevalence and impact of chronic low back pain (CLBP), no study has addressed injustice appraisals specifically among individuals with CLBP. In addition, despite racial/ethnic disparities in pain, existing injustice research has relied almost exclusively on white/Caucasian participant samples. The current study examined the associations between perceived injustice and pain, disability, and depression in a diverse community sample of individuals with CLBP (N = 137) —51 (37.2%) white, 43 (31.4%) Hispanic, 43 (31.4%) black or African American). Anger variables were tested as potential mediators of these relationships. Controlling for demographic and pain-related covariates, perceived injustice accounted for unique variance in self-reported depression and disability outcomes, but not pain intensity. State and trait anger, and anger inhibition mediated the association between perceived injustice and depression; no additional mediation by anger was observed. Significant racial differences were also noted. Compared with white and Hispanic participants, black participants reported higher levels of perceived injustice related to CLBP, as well as higher depression and pain-related disability. Black participants also reported higher pain intensity than white participants. Current findings provide initial evidence regarding the role of injustice perception specifically in the context of CLBP and within a racially diverse participant sample. Results highlight the need for greater diversity within injustice and CLBP research as well as research regarding socially informed antecedents of injustice appraisals.
Perspective:
Perceived injustice predicted worse outcomes in CLBP, with effects partially mediated by anger. Black participants reported worse pain outcomes and higher injustice perception than their white or Hispanic counterparts. Given racial inequities within broader health and pain-specific outcomes, this topic is critical for CLBP and perceived injustice research.
Keywords: Perceived injustice, chronic low back pain, racial disparities
Within the United States, low back pain (LBP) is a leading cause of pain24,93 and disability,20,33,74 accounting for 52 million of all health care visits.20,93 Although most LBP resolves quickly, ≤ 10% of these patients develop a chronic and disabling pain condition.41 In turn, chronic LBP (CLBP) contributes to annual costs of nearly $300 billion, owing substantially to lost wages and productivity.25,47,93 Despite medical advances,30,50 the cost and incidence of CLBP are steadily increasing.20,36,50
In addition to established cognitive processes—in particular, fearful and catastrophic appraisals of the pain experience78—research has highlighted the deleterious impact of injustice appraisals on musculoskeletal pain and injury outcomes (for review see79,87,94). Pain-related injustice perception is conceptualized as a cognitive appraisal reflecting the severity and irreparability of pain- or injury-related loss, externalized blame, and unfairness.76,79 Elevated injustice perception is associated with greater self-reported pain (eg,9,52,75,82,87,89,95) and disability (eg,52,59,75,76,95,97), symptoms of depression, and post-traumatic stress (eg,32,68,80,87), and worse treatment outcomes, such as after multidisciplinary rehabilitation.68,80,94,96 The salience of injustice appraisals to painful and/or chronic health conditions is not surprising given significant losses, stressors, and disruptions to valued goals that can accompany health impairment.28,56,69,76,94 From a theoretical perspective, chronic pain and injury are thought to violate core social-cognitive assumptions that the world is inherently predictable and fair (ie, Just World Belief).22,46 Injustice perception is likewise conceptualized as a central antecedent to the emotional response of anger67,91; in line with this conceptualization, there is evidence that facets of anger (ie, state, trait, expression, inhibition) serve as mechanisms linking perceived injustice to pain-related outcomes.67,92
Consistent findings across whiplash injury,68 fibromyalgia,62 arthritis,29 pelvic pain,61 and samples comprising varied chronic pain conditions67,91 suggest that injustice perception represents an important risk factor for musculoskeletal pain outcomes. However, although several mixed pain samples have included back complaints (eg,66), no study to date has addressed the role of injustice appraisals specifically among individuals with CLBP. This finding is surprising, given the noted prevalence and impact of CLBP. The existing literature on perceived injustice is further characterized by a striking lack of racial/ethnic diversity, with all but 1 study87 reflecting largely homogenous, primarily white/Caucasian samples (for review, see60,81). Conversely, pain literature documents pronounced racial/ethnic disparities in chronic pain experience and care.1,34 Within the United States, individuals identifying as black/African American endorse more frequent and disabling pain across a number of conditions compared with other racial groups, most notably whites.1,34 Of particular relevance to the current study, substantial literature in the area of Worker’s Compensation finds that African Americans show worse long-term outcomes after a work-related back injury, including greater pain intensity, disability, and emotional distress.15,16,18 This literature likewise identifies systemic racial disparities in the evaluation, treatment, and litigation outcomes, highlighting the potential relevance of injustice appraisal.14,15,17,19,84
Finally, despite growing representation within the U.S. population,39 relatively little is known about the pain experience of Hispanic Americans.40 Such observations underscore mounting recognition of the need for racial/ ethnic diversity within pain research.34
The current study sought to address these limitations by examining the association between perceived injustice and CLBP outcomes (pain intensity, disability, and depressive symptomatology) within a racially diverse sample of individuals with CLBP. Principal aims were to a) characterize perceived injustice, pain, and psychosocial variables within the sample (attending to potential racial differences), b) examine the unique contribution of perceived injustice to CLBP outcomes, and c) replicate the theorized and previously demonstrated role of anger variables (state, trait, inhibition, expression) as mechanisms in the association between injustice appraisal and pain outcomes.67,91,92 Current findings are expected to inform an understanding of the contributors to a uniquely prevalent and disabling pain condition within a racially representative participant sample.
Methods
Participants
Participants were recruited from local community sources in the Southwestern region of the United States. Specifically, recruitment comprised paper advertisements in public settings, newspapers, and online classifieds. Advertisements invited individuals to participate in paid research regarding CLBP. Interested participants were screened by phone to determine study eligibility, at which time they were provided details regarding the study protocol, which involved a self-reported measures component (reported herein) and subsequent physical and cognitive performance assessment (not reported herein). There were no eligibility restrictions with respect to race or ethnicity. Participants were eligible for inclusion if they were ≥ 18 years of age and indicated the presence of LBP for ≥ 6 months, with more than one-half the days in the past 6 months, as well as significant interference of back pain in daily activities.24 Screening likewise determined if LBP was participants’ primary source of perceived limitation/disability; accordingly, potential participants who reported co-occurring medical conditions (eg, nonspinal arthritis, fibromyalgia) that significantly impacted daily function/ mobility and participants who endorsed pregnancy were excluded from the study. Participants completed informed consent and self-report measures included in the current analysis before the initiation of a behavioral testing protocol, as described elsewhere,90 and were compensated $60.00 for completion of the full study protocol. (Note: Although all participants completed the behavioral protocol described in,90 published results reflect only usable data and thus a smaller sample size). Study procedures were reviewed and approved by the University Institutional Review Board at the University of North Texas.
Measures
Demographic Characteristics
In line with the recommended minimum dataset for CLBP,24 participants provided demographic information including gender, age, pain duration, racial identification, educational level, and income. Weight, height, and marital status were also obtained.
Pain Intensity
The average pain intensity over the last 2 weeks was assessed using the Pain Rating Index of the McGill Pain Questionnaire–Short Form (MPQ-SF-PRI6,58). The PRI reflects the summed ratings of 15 adjectives that describe sensory and affective dimensions of pain. Adjectives are ranked on a 4-point scale from 0 (none) to 3 (severe). Scores range from 0 to 45, with higher scores indicating greater pain experience.37 For the current study, Cronbach’s alpha for the MPQ-SF-PRI was .92, indicating a high internal consistency.
Self-Reported Disability
Self-appraised functional status and disability related to back pain was assessed using 2 instruments respectively intended to capture functional limitation owing to CLBP and generalized pain interference across various life domains. The Roland and Morris Disability Questionnaire (RMDQ64) is recommended as a legacy measure in CLBP research24 and assesses specific functional limitations owing to CLBP. The RMDQ consists of 24 items regarding the difficulty of performing various activities of daily living owing specifically to back pain (each item is qualified with the statement “because of my back”; eg, “I avoid heavy jobs around the house because of my back”). Participants respond either yes or no to each item; scores range from 0 to 24, with higher scores indicating greater self-reported functional disability. For the current study, the Cronbach’s alpha was .92, indicating high internal consistency.
The Pain Disability Index (PDI86) was used to assess the degree to which participants perceived themselves to be disabled by pain across 7 areas of daily living: home, social, recreational, occupational, sexual, self-care, and life support activities (eg, sleeping and eating). Participants provide a perceived disability rating for each domain, ranging from 0 (no disability) to 10 (total disability). Scores range from 0 to 70 with higher scores indicative of greater perceived pain-related disability. For the current study, the Cronbach’s alpha was .94, indicating high internal consistency.
Depressive Symptoms
The Patient Health Questionnaire-9 (PHQ-945) was used to measure depressive symptomatology. The PHQ-9 consists of 10 items and asks participants to indicate the frequency with which they experience each of the 9 symptoms included in the diagnostic criteria for major depression, as well as 1 item regarding any functional difficulty they associate with checked symptoms. Frequency scores range from 0 (not at all) to 3 (nearly every day). Total scores range from 0 to 27, with higher scores indicated greater depressive symptomatology. For the current study, the Cronbach’s alpha was .91, indicating high internal consistency.
Anger
On the State-Trait Anger Expression Inventory-II (STAXI-II72), participants completed the state (STAXI-S; 15 items; α = .97), trait (STAXI-T; 15 items; α = .90), expression (STAXI-Ex; 8 items; α = .84), and inhibition (STAXI-In; 8 items; α = .75) subscales. STAXI-S items reflect the intensity of an individual’s angry feelings at the time of testing; STAXI-T items reflect a person’s general predisposition to become angry. The STAXI-Ex sub-scale assesses how often anger is outwardly expressed and the STAXI-I subscale assesses the frequency with which persons attempt to suppress anger feelings. Items are rated on a 4-point Likert scale, with each item scored from 1 to 4; scores on the STAXI-S and STAXI-T subscales range from 15 to 60, whereas scores on the STAXI-Ex and STAXI-In subscales range from 8 to 32. Greater scores reflect a greater state or trait anger, as well as a greater tendency toward anger expression or inhibition.
Perceived Injustice
The Injustice Experiences Questionnaire (IEQ76) was used to assess perceptions of injustice associated with CLBP. Participants rated the frequency with which they experienced each of 12 thoughts or feelings when reflecting on their chronic pain condition. Items are rated on a scale of 0 (never) to 4 (all of the time). IEQ items broadly reflect the associated factors of severity/irreparability of loss and blame/unfairness. Representative severity/irreparability items include “Most people don’t understand how severe my condition is,” and “My life will never be the same.” Blame/unfairness items include “I am suffering because of someone else’s negligence,” and “It all seems so unfair.” IEQ scores range from 0 to 48, with higher scores indicating higher appraisals of injustice related to CLBP. The IEQ demonstrates strong psychometric properties, including sensitivity to change among individuals with persistent musculoskeletal pain.76,87 The Cronbach’s alpha for IEQ in the current study was .92, indicating high internal consistency.
Pain Catastrophizing
The Pain Catastrophizing Scale78 was used as a standard measure of catastrophic cognition about pain (ie, a general negative orientation toward pain characterized by tendency to magnify, ruminate about, and feel helpless in the face of pain experience). Participants are asked to reflect on painful past experiences and indicate the degree to which they experienced each of 13 thoughts or feelings when in pain using a 5-point scale ranging from 0 (not at all) to 4 (all the time). The Pain Catastrophizing Scale ranged from 0 to 52, with higher scores indicative of higher catastrophic cognition. Internal consistency for the current sample was high (α= .95).
Analytic Plan
Means, standard deviations, and counts were calculated for relevant study variables. Male and female participants as well as individuals who identified as black, white, or Hispanic were compared on all self-report measures. In preparation for subsequent modeling, bivariate correlations and analyses of variance were conducted to examine associations between participants’ IEQ score, anger variables, and outcome variables, as well as interrelationships among measures. Significant findings on analysis of variance were followed by Bonferroni-corrected post hoc comparisons. These analyses provided a method for identifying pertinent covariates for analyses of each dependent variable. Separate multiple linear regression analyses were then conducted to examine the unique/incremental contribution of injustice perception (IEQ) to self-reported pain intensity, depression, and general and functional disability. Pain intensity, disability, and depressive symptoms were also included as covariates when their inclusion was deemed to be theoretically indicated (pain intensity and depression scores as covariates in predicting disability outcomes, pain intensity and disability scores as covariates in predicting depression, depression scores as covariates in predicting pain intensity). Sociodemographic variables that showed significant bivariate association with a given outcome variable were entered into the first block of the regression; pain intensity, depression, disability, and/or pain catastrophizing scores were entered separately into subsequent blocks. IEQ score was entered into the final block of all regression analyses. Post hoc power analyses conducted using G*Power version 3.0.1027 suggested that the current sample was powered to detect regression effect sizes of >.15 (regarding overall regression block effects) and incremental increases in R2 of >.11 at a power level of .80 (with an expected 7 predictors/degrees of freedom during covariate analyses). For all analyses, pairwise exclusion of missing data was used as a means of maximizing the available data for analysis.
For outcome variables that showed a significant direct effect of the IEQ above and beyond relevant covariates/ controls, path modeling was used to examine the mediating effects of the 4 STAXI-II subscales (state, trait, expression, and inhibition). Each potential mediator was tested in a separate model. As part of mediation,49 a direct relationship between predictor and mediator variables was first estimated (a path), as was the effect of the mediator on each outcome above and beyond the effect of the predictor (b path). Mediation was deemed significant if the product of the a and b path coefficients (the ab product) was significant.49 As discussed, covariates that showed significant association with each outcome variable were included in all paths. Mediation effects were estimated using the PROCESS macro.3 All coefficients are presented in their standardized form to allow comparison regarding the relative size of the statistical relationships. The ab product coefficient, like the path estimates, is presented in standardized form (ie, in units of standard deviation). Of note, given the cross-sectional nature of the current data, special caution should be applied in the interpretation of current mediation results.
We also opted to include a set of moderation analyses, examining the role of self-identified racial status as a potential moderator of all examined relationships. This step was taken as a means of describing the potential differences among racial groups but, given the lack of prior research on this topic, these analyses were not guided by specific theory and were instead exploratory in nature. In these models, the categorical variable representing racial status was entered as a predictor along with all other variables of interest (substantive predictors and covariates). In addition, an interaction term was computed as a product of racial status and each predictor (IEQ, anger variables) and was modeled along with effects of identified covariates in predicting each endogenous variable in the model. An example equation is described below:
A significant interaction indicated an omnibus finding regarding potential differences between racial groups in terms of the main effect; in the instance of a significant finding, main effects for each group were then computed.
Results
Participant Characteristics
Participant demographic characteristics are summarized in Table 1. Of the 137 participants who completed self-report measures, 73 were male and 64 were female; 51 (37.2%) identified as white, 43 (31.4%) identified as black or African American, and 43 (31.4%) identified as Hispanic or Latino (although Hispanic technically denotes ethnicity rather than race, existing research and pilot testing with local participants indicated that most individuals identified Hispanic as a racial distinction51; therefore, it is used here to refer to participants’ racial self-identification). Participants ranged from 19 to 70 years of age (M =41.86; SD = 12.2) and duration of CLBP ranged from 6 months to 39 years (M=8.52 years, SD = 7.58). Median income was $10,000 to $20,000; 81.0% of the sample reported earning < $40,000 per year. The overall sample means regarding perceived injustice scores were comparable with prior chronic pain samples.31,67 Similarly, the study means were comparable with prior publications in terms of scores on the RMDQ,21,63 PDI,86 PHQ-9,4 MPQ-PRI,73,83 as well as STAXI subscales.12,13 All variables, with the exception of IEQ, RMDQ, and PHQ-9, included some degree of missing data. The exact counts for valid responses for each variable can be found in Table 1.
Table 1.
Sample Characteristics: Demographic Variables
| CHARACTERISTICS | N (%) OR MEAN ± SD |
|---|---|
| Gender | |
| Female | 64 (46.7) |
| Male | 73(53.3) |
| Age, y | 40.99 ± 12.3 |
| Pain duration y | 8.52 ± 7.6 |
| BMI, kg/m2 | 29.72 ± 9.3 |
| Race | |
| White | 51 (37.2) |
| Black or African American | 43 (31.4) |
| Hispanic or Latino | 43 (31.4) |
| Marital status | |
| Married | 43 (31.4) |
| Separated | 12(8.8) |
| Widowed | 2(1.5) |
| Divorced | 15(10.9) |
| Single | 65 (47.4) |
| Education level | |
| Less than high school | 20(14.6) |
| High school diploma | 18(13.1) |
| Some college (nondegree) | 42 (30.7) |
| Associate’s | 8(5.8) |
| Bachelor’s | 11 (8.0) |
| Graduate/professional | 6 (4.4) |
| Would rather not say | 29(21.2) |
| Missing | 2(2.2) |
| Income, $ | |
| < 10,000 | 49 (35.8) |
| 10,000–19,000 | 33(24.1) |
| 20,000–29,000 | 11 (8.0) |
| 30,000–39,000 | 18(13.1) |
| 40,000–49,000 | 10(7.3) |
| ≥ 50,000 | 16(11.7) |
Female participants reported significantly more pain intensity (t(2, 134) = −2.01, P =.05) and depressive symptoms than male counterparts (t(2, 135) = −2.15, P =.03); female participants also had significantly higher scores on the anger inhibition subscale of the STAXI-II (t(2, 134) = −2.30, P =.02). No other significant gender differences were observed.
Racial Differences in Study Variables
No racial differences were observed in terms of participant age, body mass index (BMI), or pain duration. Relative to black and Hispanic participants, a significantly greater proportion of white participants reported income above the sample median (χ2(2, N = 137) = 7.80, P =.02). Similarly, there was a trend in higher educational attainment among white participants, followed by black and subsequently Hispanic participants (χ2(6, N =137) = 76.48, P <.01).
Notable racial differences were observed across study variables and are summarized in Fig 1 and Table 2. Specifically, in comparison with both white and Hispanic counterparts, participants who identified as black or African American reported significantly higher levels of perceived injustice related to CLBP (F(2, 134) = 14.60, P <.001), depressive symptoms (F(2, 134) =4.09, P =.019), general disability (F(2, 119) = 7.11, P =.001), and functional disability related to back pain (F(2, 134) = 13.29, P <.001). Black or African American participants also reported significantly higher levels of pain catastrophizing compared with white and Hispanic participants (F(2, 117) = 5.82, P =.004). Finally, black participants endorsed higher pain intensity (F(2, 134) = 3.09, P =.04) compared with white participants, but did not differ from Hispanic participants on this measure (Figs. 2–4).
Figure 1.
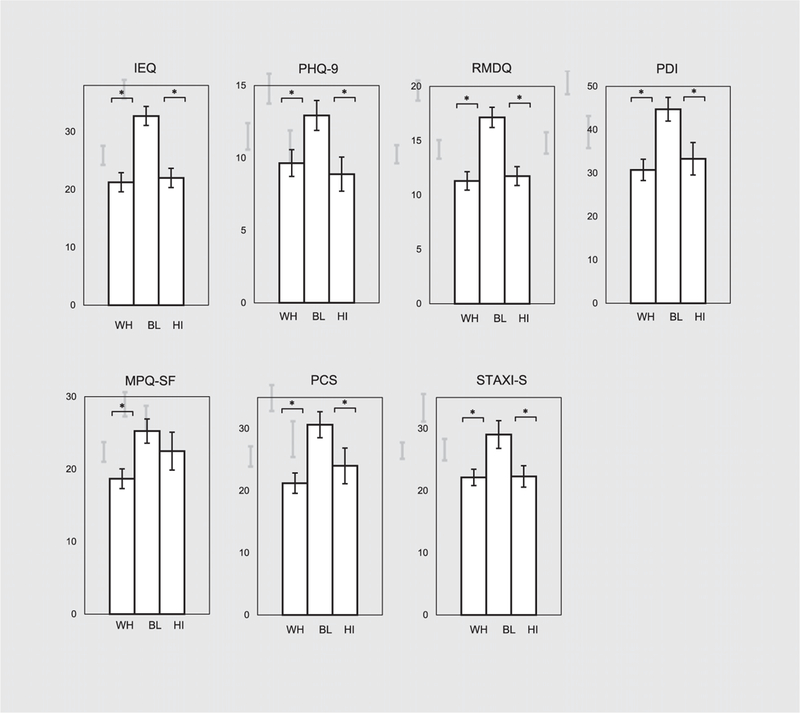
WH, white participants; BL, black/African American participants; HI, Hispanic participants; PCS, Pain Catastrophizing Scale. *P < .05.
Table 2.
Descriptive Statistics for Pain, Disability, and Psychosocial Outcomes
| TOTAL SAMPLE (N= 137) |
RANGE
OF SCORES (MIN-MAX) |
BLACK PARTICIPANTS (N = 43) |
HISPANIC PARTICIPANTS (N = 43) |
WHITE PARTICIPANTS (N = 51) |
|
|---|---|---|---|---|---|
| MPQ-SF-PRI | 21.58 ± 13.05 | 0–45 | 25.25 ± 11.00* | 22.49 ± 17.11 | 18.68 ± 9.59 |
| RMDQ | 13.19 ± 6.53 | 0–24 | 17.14 ± 6.10† | 11.74 ± 5.70 | 11.29 ± 6.04 |
| PDI | 35.79 ± 18.78 | 3–70 | 44.73 ± 17.24† | 33.31 §20.11 | 30.75 ± 17.59 |
| PHQ-9 | 10.29 ± 7.08 | 0–27 | 12.93 ± 6.76† | 8.88 ± 7.73 | 9.65 ± 6.59 |
| PCS | 35.11 ± 13.69 | 2–52 | 30.63 ± 13.25† | 24.00 ± 15.49 | 21.22 ± 11.66 |
| IEQ | 24.81 ± 12.44 | 0–48 | 32.72 ± 10.76† | 22.00 ± 10.90 | 21.25 ± 11.80 |
| STAXI - S | 24.14 ± 11.86 | 0–60 | 29.05 ± 14.44† | 22.30 ± 11.33 | 22.14 ± 9.41 |
| STAXI - T | 18.00 ± 6.82 | 6–40 | 18.83 ± 8.28 | 17.07 ± 6.07 | 17.75 ± 5.34 |
| STAXI - Ex | 15.32 ± 4.97 | 7–32 | 16.55 ± 5.35 | 14.19 § 4.83 | 14.98 ± 4.77 |
| STAXI - In | 19.14 ± 5.09 | 8–32 | 18.52 ± 5.11 | 18.98 ± 5.25 | 17.35 ± 4.98 |
Abbreviation: PCS, Pain Catastrophizing Scale.
Score is significantly greater than white participants at P < .05.
Score is significantly greater than both Hispanic and white participants at P < .05.
Values are mean ± standard deviation unless otherwise noted.
Figure 2.
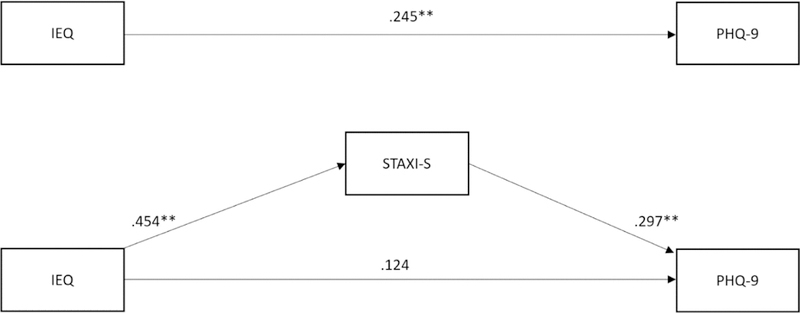
State anger as a cross-sectional mediator of the relationship between perceived injustice and depressive symptoms.
Figure 4.
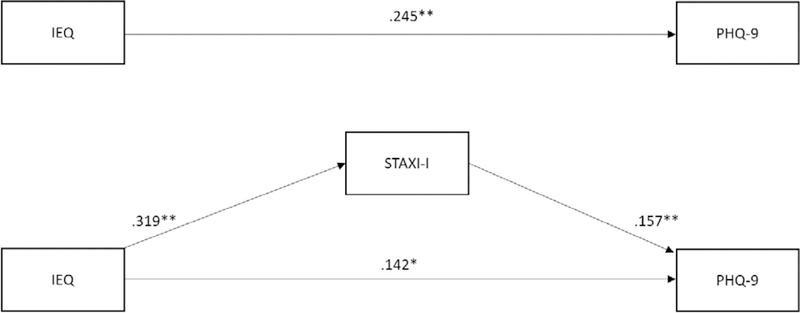
Anger inhibition as a cross-sectional mediator of the relationship between perceived injustice and depressive symptoms.
In terms of anger-related variables, black participants endorsed significantly higher State Anger (F(2, 134) = 4.09, P =.009) than white or Hispanic counterparts; black participants also reported relatively higher levels of anger expression than white or Hispanic participants, but racial differences on this measure did not reach statistical significance (F(2, 134) = 1.28, P =.08). Hispanic and white participants did not differ significantly on any of these study variables.
Bivariate Correlations Among Study Variables
Table 3 shows bivariate correlations among study variables. Age was significantly and positively associated with self-reported pain intensity, perceived injustice (IEQ score), and disability (RMDQ and PDI); age was significantly negatively associated with participants’ scores on the anger expression and anger inhibition subscales of the STAXI-II. Self-reported income was negatively associated with pain intensity, perceived injustice, disability (RMDQ and PDI), depression, and pain catastrophizing. Higher income was associated with lower scores on the STAXI-II-S subscale. Finally, participants’ BMI showed significant positive association with pain intensity, perceived injustice, and disability. Perceived injustice showed moderate to strong positive correlations with pain intensity (r =.52), disability (r =.68 and r =.72 for the RMDQ and PDI, respectively), pain catastrophizing (r =.62), and depression (r =.64), as well as each of the anger subscales (r =.33, r =.50, r =.26, and r =.34, for state, trait, expression, and inhibition, respectively). Of note, self-reported income was positively skewed and a log transformation was conducted. All correlations followed the same pattern and were of similar levels of significance when the log-transformed versus original data were used, and we present the nontransformed data in the remainder of the manuscript for ease of interpretation.
Table 3.
Associations Between Study Variables
| VARIABLE | N | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Age | 134 | — | ||||||||||||
| 2. Income | 137 | −.05 | — | |||||||||||
| 3. BMI, kg/m2 | 133 | .20* | −.02 | — | ||||||||||
| 4. Pain duration, y | 136 | .29† | −.07 | −.01 | — | |||||||||
| 5. MPQ-SF-PRI | 136 | .18* | −.21* | .18* | −.00 | — | ||||||||
| 6. IEQ | 137 | .23† | −.25† | .24† | .14 | .52† | — | |||||||
| 7. RMDQ | 137 | .29† | −.27† | .28† | .12 | .53† | .68† | — | ||||||
| 8. PDI | 120 | .35† | −.25† | .21* | .07 | .72† | .72† | .75† | — | |||||
| 9. PHQ-9 | 137 | .11 | −.27† | .13 | .12 | .55† | .64† | .60† | .63† | — | ||||
| 10. PCS | 120 | .16† | −.25† | .08 | .08 | .61† | .62† | .63† | .71† | .64† | — | |||
| 11. STAXI - T | 136 | −.16‡ | −.11 | .03 | −.06 | .28† | .33† | .25† | .34† | .56† | .40† | — | ||
| 12. STAXI – S | 136 | −.03 | −.20* | .05 | .01 | .44† | .50† | .49† | .54† | .63† | .57† | .71† | — | |
| 13. STAXI - Ex | 136 | −.24† | −.01 | .12 | −.11 | .20* | .26† | .15† | .24† | .35† | .34† | .74† | .54† | — |
| 14. STAXI - In | 136 | −.180* | −.11 | .11 | −.07 | .32† | .33† | .30† | .35† | .38† | .39† | .54† | .41† | .54† |
Abbreviation: PCS, Pain Catastrophizing Scale.
P < .05.
P < .01.
P < .10.
Prediction of CLBP Outcomes by IEQ and Mediation by Anger Variables
The Association Between Anger and Perceived Injustice
As a first condition of mediation, the relationship between IEQ score and each of the mediators (STAXI-II subscales) was tested (a path). The IEQ scores showed a significant relationship with the STAXI-S scores (β =.453, P <.001, total model r2 =.262), above and beyond inclusion of relevant covariates (income and race). The IEQ was also a significant predictor of STAXI-T (β =.268, P <.001, total model r2 =.113), above and beyond the effects of race. The IEQ significantly predicted STAXI-In scores (β =.319, P <.001, total model r2 =.132) above and beyond the effects of study covariates (income, race, and gender), as well as STAXI-Ex scores (β =.259, P =.009, total model r2 =.074), above and beyond the effects of age, BMI, race, and income.
Depression
Multiple linear regression analyses were used to examine the unique/incremental contribution of injustice perception to each outcome variable (Table 4). When entered into the final block of the analysis, perceived injustice scores significantly contributed an additional 2.8% variance to the model (FΔ = 7.04, P <.01) above and beyond the contribution of sociodemographic variables (gender, race, and income), pain intensity scores, disability scores, and catastrophizing (accounting for 12.8%, 23.8%, 11.2%, and 6.0% of variance in PHQ-9 scores, respectively).
Table 4.
Regression Analyses
| OUTCOME VARIABLE | N | R2CHANGE | FΔ | β | T |
|---|---|---|---|---|---|
| Depression (PHQ-9) | |||||
| Step 1 | 118 | .13 | 5.64* | ||
| Gender | .21† | 2.43 | |||
| Race | .12 | 1.33 | |||
| Income | −.31* | −3.50 | |||
| Step 2 | .24 | 42.88* | .51* | 6.55 | |
| MPQ-SF PRI | |||||
| Step 3 | .11 | 24.28* | .41* | 4.92 | |
| RMDQ | |||||
| Step 4 | .06 | 14.70* | .35* | 3.83 | |
| PCS | |||||
| Step 5 | .03 | 7.04* | .25* | 2.65 | |
| IEQ | |||||
| Functional disability (RMDQ) | |||||
| Step 1 | 116 | .21 | 5.76* | ||
| Age | .24* | 2.76 | |||
| Gender | .05 | .60 | |||
| Race | .03 | .33 | |||
| Income | −.27* | −3.06 | |||
| BMI | .23 | 2.62 | |||
| Step 2 | .17 | 30.52* | .45* | 5.53 | |
| MPQ-SF-PRI | |||||
| Step 3 | .11 | 24.02* | .42* | 4.90 | |
| PHQ-9 | |||||
| Step 4 | .06 | 13.22* | .34* | 3.64 | |
| PCS | |||||
| Step 5 | .05 | 13.41* | .33* | 3.66 | |
| IEQ | |||||
| Disability (PDI) | |||||
| Step 1 | 116 | .22 | 6.09* | ||
| Age | .33* | 3.79 | |||
| Gender | .13 | 1.52 | |||
| Race | −.03 | −.39 | |||
| Income | −.23* | −2.65 | |||
| BMI | .14 | 1.61 | |||
| Step 2 | .36 | 95.02* | .65* | 9.75 | |
| MPQ-SF-PRI | |||||
| Step 3 | .07 | 23.36* | .34* | 4.83 | |
| PHQ-9 | |||||
| Step 4 | .05 | 18.35* | .33* | 4.28 | |
| PCS | |||||
| Step 5 | .04 | 18.23* | .30* | 4.27 | |
| IEQ | |||||
| Pain intensity (MPQ-SF-PRI) | |||||
| Step 1 | 116 | .14 | 3.50* | ||
| Age | .17 | 1.84 | |||
| Gender | .20† | 2.21 | |||
| Race | −.06 | −.66 | |||
| Income | −.20† | −2.18 | |||
| BMI | .13 | 1.46 | |||
| Step 2 | .22 | 37.46* | .51* | 6.12 | |
| PHQ-9 | |||||
| Step 3 | .09 | 17.41* | .40* | 4.17 | |
| PCS | |||||
| Step 4 | .01 | 1.13 | .11 | 1.06 | |
| IEQ | |||||
Abbreviation: PCS, Pain Catastrophizing Scale.
P < .01.
P < .05.
For the mediation analysis (Figures 2–4), a significant direct effect on PHQ-9 scores was found for STAXI-S (β =.297, P <.001, total model r2 =.628), STAXI-T (β =.312, P <.001, total model r2 =.651), STAXI-In (β =.157, P =.024, total model r2 =.590), and STAXI-Ex scores (β =.127, P =.049, total model r2 =.585) above and beyond that of the predictor (IEQ score) and covariates (b path). When mediation analyses were conducted, only STAXI-S (standardized ab =.135, P <.05), STAXI-T scores (standardized ab = .084, P < .05), and STAXI-In (standardized ab =.050, P < .05) were found to mediate the relationship between IEQ and PHQ-9 scores, above and beyond the effect of covariates.
Disability
Injustice perception scores significantly contributed 5.1% of variance to self-reported functional disability (RMDQ) scores (FΔ = 13.41, P < .01). The effect of IEQ was significant, above and beyond the effects of associated sociodemographic variables (age, race, gender, income, BMI), pain intensity, depressive symptoms, and pain catastrophizing scores (which accounted for 20.6%, 17.2%, 11.2%, and 5.6% of variance in the RMDQ scores, respectively). Similarly, IEQ scores were found to significantly account for an additional 4.3% of variance in general disability (PDI) ratings (FΔ = 18.23, P < .01). These effects occurred above and beyond the effects of sociodemographic variables (age, race, gender, income, BMI), as well as pain intensity, depressive symptoms, and pain catastrophizing, which accounted for 21.5%, 36.4%, 7.4%, and 5.0% of the variance in PDI scores, respectively.
Controlling for the effects of IEQ and relevant covariates, there was no association observed between RMDQ scores and the STAXI-II subscales: STAXI-S (β =.038, P =.66, total model r2 =.632), STAXI-T (β = −.095, P =.21, total model r2 =.637), STAXI-Ex (β = −.118, P =.08, total model r2 =.642), or STAXI-In scores (β = −.002, P =.98, total model r2 =.631). Similarly, PDI scores were not found to be significantly associated with any of the STAXI-II subscales above and beyond the effects of the IEQ and covariates: STAXI-S (β =.076, P =.37, total model r2 =.724), STAXI-T (β =.076, P =.24, total model r2 =.719), STAXI-Ex (β =.019, P =.75, total model r2 =.716), or STAXI-In scores (β =.025, P =.70, total model r2 =.716). None of the STAXI subscales were found to significantly mediate the relationships between the IEQ and either the RMDQ or PDI, above and beyond the effects of study covariates (P > .05 in all cases).
Pain Intensity
When entered into the final block of multiple regression analyses, perceived injustice scores did not significantly contribute variance to the prediction of pain intensity (MPQ-SF-PRI) scores (FΔ = 14.41, P =.13), above and beyond the effects of associated sociodemographic variables (age, race, gender, income, BMI), depressive symptoms, and pain catastrophizing scores (which accounted for 13.6%, 21.9%, and 8.9% of variance in MPQ-SF-PRI scores, respectively).
Above and beyond the effects of IEQ and covariates in the model, there was not a significant relationship between MPQ-SF-PRI scores and any of the STAXI-II subscales: STAXI-S (β =.109, P =.15, total model r2 =.537), STAXI-T (β = −.054, P =.44, total model r2 =.531), STAXI- In (β =.000, P =.99, total model r2 =.528), or STAXI-Ex scores (β = −.020, P =.75, total model r2 =.528). None of the STAXI subscales were found to significantly mediate the relationships between the IEQ and MPQ-SF-PRI, above and beyond the effects of study covariates (P > .22 in all cases).
Moderation by Race
Given consistent racial differences in study outcome variables, self-reported racial status was tested as a moderator for the observed associations between perceived injustice and self-reported pain intensity, disability, and depression. Subsequent analyses showed that racial status did not moderate the association between IEQ and MPQ-SF-PRI scores (β =.256, P =.31), PHQ-9 scores (β = −.067, P =.81), RMDQ scores (β =.109, P =.62), or PDI scores (β =.103, P =.63).
For anger variables, racial status was found to moderate the relationship between perceived injustice and STAXI-T scores (β = −.472, P =.033); this interaction suggested a relatively stronger relationship between IEQ scores and STAXI-T scores in black or African American participants (β =.469, P < .001) compared with white (β =.173, P =.16) and Hispanic participants (β =.379, P =.014). Race did not moderate the relationship between IEQ and other subscales of the STAXI-II (P > .06 in all cases).
Discussion
The current study is the first to examine the association between perceived injustice and physical and psychological outcomes specifically in the context of CLBP. It is likewise the first to examine these relationships within a racially diverse participant sample. Current findings are consistent with existing studies showing a positive association between injustice perception and pain, depression, and disability across a number of chronic pain conditions,67,76,77 as well as in acute trauma and rehabilitation settings.11,60,80,87 Perceived injustice accounted for unique variance in cross-sectional prediction of disability and depression when controlling for significant sociodemographic factors and major psychosocial contributors to CLBP (ie, depression and catastrophizing). Specific focus on CLBP and CLBP outcomes was integral to the current study. Given its ubiquity and impact within the United States and worldwide, CLBP is recognized as a unique target of empirical inquiry,2 guided by specific research standards (ie, National Institutes of Health Task Force on Research Standards for Chronic Low Back Pain24). However, despite burgeoning literature on the deleterious impact of injustice appraisals in mixed chronic pain samples (which often reference back pain/injury), no studies have replicated these effects specifically in a CLBP context. The current findings provide an empirical foundation for future CLBP research by demonstrating the incremental value of injustice beliefs within this population.
Recent research has increasingly focused on mechanisms of action that may drive the effects of perceived injustice. Theoretical literature suggests that perceived injustice is a key cognitive antecedent to the experience of anger.91 Current findings and previous studies support a robust positive association between perceived injustice and anger variables.67,75,88,91 In line with previous studies,66,67,92 anger variables in the current study mediated the relationship between perceived injustice and depressive symptoms, but did not extend to measures of self-reported disability or pain intensity.67 These findings suggest that there may be other mechanisms (eg, behavioral avoidance, treatment nonadherence) that more closely correspond with functional outcomes, but are inadequately explained by emotional factors such as anger. Although not measured directly, the observed mediation effects may reflect the potential of anger to disrupt meaningful social relationships and contribute to greater distress, conflict, and isolation, ultimately undermining psychological adjustment.67,75 In line with this, anger expression was found to mediate the association between pain-related injustice perception and impaired therapeutic alliance among individuals receiving multidisciplinary rehabilitation for chronic musculoskeletal pain.70 Notably, in the current study anger expression emerged as the only STAXI subscale that did not mediate depression outcomes. These differential findings may be due to critical sample differences (ie, participants in the current sample reported substantially longer pain duration than rehabilitation patients).
In addition to anger, acceptance has emerged as a potential mechanism of perceived injustice outcomes.10,31,52 Contrasted with efforts to avoid or solve persistent pain,26 pain acceptance refers to engaging in value-driven activity with the goal of living a fulfilling life despite continued pain experience.26,54 Conceptually, acceptance stands in contrast with injustice perception, characterized by emphasis on loss and irreparability31; in line with this, acceptance and injustice perception are negatively correlated in the literature (eg,62). In a recent study of a mixed pain sample,10 acceptance was found to function in parallel to anger as in mediating the effects of perceived injustice on pain, disability, and opioid prescription. Future studies examining mechanisms of action in injustice appraisal should consider the inclusion of acceptance and anger to replicate and extend current findings.
A central aim of the current study was to characterize the current sample with respect to pain and psychosocial outcomes. Echoing earlier findings of race disparities in work-related LBP,15,16,18,85 as well as other chronic pain conditions,1,34 black participants in the current study reported significantly more pain, disability, pain catastrophizing, and depression than their white or Hispanic counterparts. Critically, black participants endorsed significantly greater perceived injustice with respect to CLBP than either white or Hispanic participants. This observation is notable because, to date, the vast majority of the literature has addressed pain-related injustice appraisals in predominantly or exclusively Caucasian samples. The finding of higher injustice perception among black participants is consistent with differences identified by Trost et al (87) among individuals discharged from severe trauma hospitalization; to our knowledge, this is the only other study to collect injustice appraisals from a racially diverse participant sample. Although current analyses examining potential moderation by race were largely nonsignificant (it is probable that the relatively stronger relationship between IEQ and trait anger scores would not have survived post hoc adjustments for multiple comparisons), these finding represent an initial step in highlighting the unequal distribution and potential impact of pain-related injustice perception across racial groups.
In the same vein, current findings offer tentative insight regarding factors that may contribute to the development and maintenance of pain-specific injustice appraisals. Substantial research testifies to the deleterious health impact of broader social inequities or injustice experiences (eg, racial discrimination, unfair hierarchical treatment, low social status23,35,42,43). For instance, the Perceived Unfairness Model42 defines repeated exposure to unjust societal experiences as a distinct form of stress, ultimately shaping poorer health prognoses among African Americans. However, despite clear evidence of the destructive impact of discriminatory experiences,5,42,44 studies have yet to examine the interface of such societal- and individual-level inequities with injustice appraisals regarding a specific pain condition like CLBP. For example, it is plausible that, in the context of back injury, a lifetime history of race-related injustice experiences8 may reinforce pain-related injustice appraisals and ultimately contribute to worse pain- and disability-specific outcomes. In line with the potential impact of existing sociodemographic factors, CLBP injustice appraisals were negatively associated with socioeconomic indicators like income (which also showed difference between black and white participants), potentially reflecting the greater burden of physical injury and disability on individuals with lower financial resources.48,65 These findings again highlight the broader sociocultural context within which injustice appraisals arise and the increasingly recognized role of social and interpersonal processes within injustice literature.55,57,60,61,75 Recent findings of the negative association between perceived injustice and patient-provider interactions70 is perhaps particularly relevant here given evidence of racial inequities in pain treatment1,14,19,34,84 and mistrust of the medical establishment within minority communities.36,71
Limitations and Future Directions
As noted, our findings are taken from a cross-sectional dataset, and the proposed mediation model is limited in this respect. We are not able to state definitively that the proposed variables follow a causal or temporal order as they are represented in our model; there is reasonable argument that these factors may more appropriately be considered mutually influential. Individuals in pain may become more disabled or more depressed, and may thus experience more anger or appraise their pain experience as more unjust. We urge replication of our findings within larger CLBP samples that may reflect greater racial and socioeconomic diversity, as well as extension of our findings in longitudinal and intervention studies that may better delineate the temporal and causal relationships between these variables. For example, whereas our analyses suggest the presence of both potential moderators and mediators in examining the role of injustice appraisal and anger across racial groups, our relatively limited sample size did not facilitate sufficient power to estimate moderated mediation models; this approach would likely be appropriate for future, larger studies. Similarly, results of post hoc power analysis suggested that our sample may have been underpowered to detect subtler effects in our regression and mediation analyses, particularly with presence of missing data on some variables that further reduced sample size for analysis. Thus, although our analysis yielded several significant effects, our non-significant findings should be interpreted with this caution in mind.
In terms of future directions, the incremental contribution of IEQ scores to CLBP outcomes above and beyond other pain-relevant factors suggest that nonbiological treatment approaches to CLBP may benefit from inclusion of individuals, pain-related injustice appraisals alongside traditional cognitive-behavioral targets, namely catastrophic and fearful appraisals. In addition to individual-level intervention, observed racial differences suggest the potential utility of systems-level interventions that address possible antecedents to elevated injustice appraisals both within medical contexts (eg, provider education7,38) and broader social structures. Further, given the critical importance of identifying potential risk factors that contribute to the transition from acute to chronic pain status in back injury,77 a longitudinal perspective—currently largely absent within the perceive injustice literature—would be particularly valuable with this population. Additionally, recent studies have linked higher injustice perception with a greater likelihood of opiate use and maintenance9,69; given that 25% of individuals with CLBP report aberrant medication use,53 it may be particularly important to examine the role of injustice appraisals in the natural course of treatment for patients with CLBP.
Conclusions
The current study examined an increasingly recognized psychological risk factor in the context of a highly prevalent pain condition and within a racially diverse participant sample. Findings support the contribution of injustice appraisals to functional and psychosocial outcomes among individuals with CLBP, above and beyond sociodemographic and psychosocial contributors. Findings add to the growing literature on racial disparities in injustice appraisals in musculoskeletal pain and injury. The current findings highlight the relative dearth of research addressing health-related injustice beliefs within minority populations and the need for prospective designs regarding injustice appraisals in CLBP.
Figure 3.
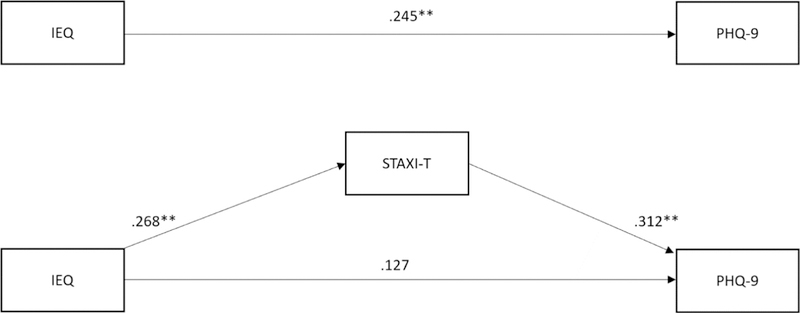
Trait anger as a cross-sectional mediator of the relationship between perceived injustice and depressive symptoms.
Acknowlegment
The authors acknowledge the International Association for the Study of Pain (IASP) Early Career Grants Program and NIH/NIMHD Grant R01MD010441 for their support of this study.
Footnotes
Disclosures: The authors have no disclosures of any additional funding or any relationships that might lead to a conflict of interest.
References
- 1.Anderson KO, Green CR, Payne R: Racial and ethnic disparities in pain: Causes and consequences of unequal care. J Pain 10:1187–1204, 2009 [DOI] [PubMed] [Google Scholar]
- 2.Andersson GBJ: Epidemiological features of chronic low-back pain. Lancet 354:581–585, 1999 [DOI] [PubMed] [Google Scholar]
- 3.Andrew H The PROCESS macro for SPSS and SAS. Columbus, OH: The Ohio State University; 2016. [Google Scholar]
- 4.Bener A, Verjee M, Dafeeah EE, Falah O, Al-Juhaishi T, Schlogl J, Sedeeq A, Khan S: Psychological factors: Anxiety, depression, and somatization symptoms in low back pain patients. J Pain Res 6:95–101, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Brondolo E, Brady Ver Halen N, Pencille M, Beatty D, Contrada RJ: Coping with racism: A selective review of the literature and a theoretical and methodological critique. J Behav Med 32:64–88, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Burckhardt CS, Jones KD: Adult measures of pain: The McGill Pain Questionnaire (MPQ), Rheumatoid Arthritis Pain Scale (RAPS), Short-Form McGill Pain Questionnaire (SF-MPQ), Verbal Descriptive Scale (VDS), Visual Analog Scale (VAS), and West Haven-Yale Multidisciplinary Pain Inventory (WhYMPI). Arthritis Care Res 49, 2003 [Google Scholar]
- 7.Burgess D, van Ryn M, Dovidio J, Saha S: Reducing racial bias among health care providers: Lessons from social-cognitive psychology. J Gen Intern Med 22:882–887, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Burgess D, Grill J, Noorbaloochi S, Griffin JM, Ricards J, van Ryn M, Partin MR: The effect of perceived racial discrimination on bodily pain among older African American men. Pain Med 10:1341–1352, 2009 [DOI] [PubMed] [Google Scholar]
- 9.Carriere JS, Martel M-O, Kao M- C, Sullivan MJ, Darnall BD: Pain behavior mediates the relationship between perceived injustice and opioid prescription for chronic pain: A Collaborative Health Outcomes Information Registry study. J Pain Res 10:557–566, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Carriere JS, Sturgeon JA, Yakobov E, Kao M- C, Mackey SC, Darnall BD: The impact of perceived injustice on painrelated outcomes: A combined model examining the mediating roles of pain acceptance and anger in a chronic pain sample. Clin J Pain 34(8):739–747, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Carriere JS, Thibault P, Adams H, Milioto M, Ditto B, Sullivan MJL: Expectancies mediate the relationship between perceived injustice and return to work following whiplash injury: A 1-year prospective study. Eur J Pain 21:1234–1242, 2017 [DOI] [PubMed] [Google Scholar]
- 12.Carson JW, Keefe FJ, Goli V, Fras AM, Lynch TR, Thorp SR, Buechler JL: Forgiveness and chronic low back pain: A preliminary study examining the relationship of forgiveness to pain, anger, and psychological distress. J Pain 6:84–91, 2005 [DOI] [PubMed] [Google Scholar]
- 13.Carson JW, Keefe FJ, Lynch TR, Carson KM, Goli V, Fras AM, Thorp SR: Loving-kindness meditation for chronic low back pain: Results from a pilot trial. J Holist Nurs 23:287–304, 2005 [DOI] [PubMed] [Google Scholar]
- 14.Chibnall JT, Tait RC: Disparities in occupational low back injuries: Predicting pain-related disability from satisfaction with case management in African Americans and Caucasians. Pain Med 6:39–48, 2005 [DOI] [PubMed] [Google Scholar]
- 15.Chibnall JT, Tait RC: Legal representation and dissatisfaction with workers, compensation: Implications for claimant adjustment. Psychol Inj Law 3:230–240, 2010 [Google Scholar]
- 16.Chibnall JT, Tait RC: Long-term adjustment to work-related low back pain: Associations with socio-demographics, claim processes, and post-settlement adjustment. Pain Med 10:1378–1388, 2009 [DOI] [PubMed] [Google Scholar]
- 17.Chibnall JT, Tait RC, Andresen EM, Hadler NM: Clinical and social predictors of application for social security disability insurance by Workers, Compensation claimants with low back pain. J Occup Environ Med 48:733–740, 2006 [DOI] [PubMed] [Google Scholar]
- 18.Chibnall JT, Tait RC, Andresen EM, Hadler NM: Race and socioeconomic differences in post-settlement outcomes for African American and Caucasian Workers’ Compensation claimants with low back injuries. Pain 114:462–472, 2005 [DOI] [PubMed] [Google Scholar]
- 19.Chibnall JT, Tait RC, Andresen EM, Hadler NM: Race differences in diagnosis and surgery for occupational low back injuries. Spine 31:1272–1275, 2006 [DOI] [PubMed] [Google Scholar]
- 20.Courtney-Long E, Carroll D, Zhang Q, Stevens A, Griffin- Blake S, Armour B, Campbell V: Prevalence of disability and disability type among adults—United States, 2013, mMwR. Morbid Mortal Wkly Rep 64:777–783, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Crombez G, Vlaeyen JW, Heuts PH, Lysens R: Pain-related fear is more disabling than pain itself: Evidence on the role of pain-related fear in chronic back pain disability. Pain 80:329–339, 1999 [DOI] [PubMed] [Google Scholar]
- 22.Dalbert C: Belief in a just world,. In: Leary MR, Hoyle RH, eds. Handbook of Individual Differences in Social Behavior, Guilford Press, NY, NY: 2009. p. 288–297 [Google Scholar]
- 23.De Vogli R, Ferrie JE, Chandola T, Kivimaki M, Marmot MG: Unfairness and health: Evidence from the Whitehall II Study. J Epidemiol Community Health 61:513–518, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Deyo RA, Dworkin SF, Amtmann D, Andersson G, Borenstein D, Carragee E, Carrino J, Chou R, Cook K, DeLitto A, Goertz C, Khalsa P, Loeser J, Mackey S, Panagis J, Rainville J, Tosteson T, Turk D, Von Korff M, Weiner DK: Focus article report of the NIH task force on research standards for chronic low back pain. Clin J Pain 30:701–712, 2014 [DOI] [PubMed] [Google Scholar]
- 25.Dieleman JL, Baral R, Birger M, Bui AL, Bulchis A, Chapin A, Hamavid H, Horst C, Johnson EK, Joseph J, Lavado R, Lomsadze L, Reynolds A, Squires E, Campbell M, DeCenso B, Dicker D, Flaxman AD, Gabert R, Highfill T, Naghavi M, Nightingale N, Templin T, Tobias MI, Vos T, Murray CJL: US spending on personal health care and public health, 1996–2013. JAMA 316:2627–2646, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Eccleston C, Crombez G: Worry and chronic pain: A misdirected problem solving model. Pain 132:233–236, 2007 [DOI] [PubMed] [Google Scholar]
- 27.Faul F, Erdfelder E, Lang A-G, Buchner A: G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods 39:175–191, 2007 [DOI] [PubMed] [Google Scholar]
- 28.Ferrari R: A prospective study of perceived injustice in whiplash victims and its relationship to recovery. Clin Rheumatol 34:975–979, 2015 [DOI] [PubMed] [Google Scholar]
- 29.Ferrari R: Perceived injustice in fibromyalgia and rheumatoid arthritis. Clin Rheumatol 33:1501–1507, 2014 [DOI] [PubMed] [Google Scholar]
- 30.Freburger JK, Holmes GM, Agans RP, Jackman AM, Darter JD, Wallace AS, Castel LD, Kalsbeek WD, Carey TS: The rising prevalence of chronic low back pain. Arch Intern Med 169:251–258, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gagnon J, Martel M-E, Dionne F, Scott W, Alencar Abaide Balbinotti M: Perceived injustice and chronic pain acceptance: Are we measuring two separate constructs or opposite poles of the same dimension? Saude e Desenvolvimento Humano 4:1, 2016 [Google Scholar]
- 32.Giummarra MJ, Cameron PA, Ponsford J, Ioannou L, Gibson SJ, Jennings PA, Georgiou-Karistianis N: Return to work after traumatic injury: Increased work-related disability in injured persons receiving financial compensation is mediated by perceived injustice. J Occup Rehabil 27:173–185, 2017 [DOI] [PubMed] [Google Scholar]
- 33.Global Burden of Disease Study 2013 Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990–2013: Asystematic analysis for the Global Burden of Disease Study 2013. Lancet 386:743–800, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Green CR, Anderson KO, Baker TA, Campbell LC, Decker S, Fillingim RB, Kaloukalani DA, Lasch Ke, Myers C, Tait RC: The unequal burden of pain: Confronting racial and ethnic disparities in pain. Pain Med 4:277–294, 2003 [DOI] [PubMed] [Google Scholar]
- 35.Hadler NM, Tait RC, Chibnall JT: Back pain in the workplace. JAMA 297:1594–1596, 2007 [DOI] [PubMed] [Google Scholar]
- 36.Halbert CH, Armstrong K, Gandy OH, Shaker L: Racial differences in trust in health care providers. Arch Intern Med 166:896–901, 2006 [DOI] [PubMed] [Google Scholar]
- 37.Hawker GA, Mian S, Kendzerska T, French M: Measures of adult pain: Visual analog scale for pain (vas pain), Numeric Rating Scale for Pain (NRS PAIN), McGill Pain Questionnaire (MPQ), Short-Form McGill Pain Questionnaire (SF-MPQ), Chronic Pain Grade Scale (CPGS), Short Form-36 Bodily Pain Scale (SF-36 BPS), and Measure of Intermittent and Constant Osteoarthritis Pain (ICOAP). Arthritis Care Res 63, 2011. [DOI] [PubMed] [Google Scholar]
- 38.Hirsh AT, Hollingshead NA, Ashburn-Nardo L, Kroenke K: The interaction of patient race, provider bias, and clinical ambiguity on pain management decisions. J Pain 16:558–568, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.United States Census Bureau. The Hispanic Population: 2010. [Google Scholar]
- 40.Hollingshead NA, Ashburn-Nardo L, Stewart JC, Hirsh AT: The pain experience of Hispanic Americans: A critical literature review and conceptual model. J Pain 17:513–528, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hoy D, Brooks P, Blyth F, Buchbinder R: The epidemiology of low back pain. Best Pract Res Clin Rheumatol 24:769–781, 2010 [DOI] [PubMed] [Google Scholar]
- 42.Jackson B, Kubzansky LD, Wright RJ: Linking perceived unfairness to physical health: The perceived unfairness model. Rev Gen Psychol 10:21–40, 2006 [Google Scholar]
- 43.Kivimaki M, Vahtera J, Elovainio M, Virtanen M, Siegrist J: Effort-reward imbalance, procedural injustice and relational injustice as psychosocial predictors of health: Complementary or redundant models? Occupational and environmental medicine 64:659–665, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Krieger N: Embodying inequality: A review of concepts, measures, and methods for studying health consequences of discrimination. Int J Health Serv 29:295–352, 1999 [DOI] [PubMed] [Google Scholar]
- 45.Kroenke K, Spitzer RL, Williams JB: The PHQ-9: Validity of a brief depression severity measure.. J Gen Intern Med 16:606, 2001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lerner MJ, Miller DT: Just world research and the attribution process: Looking back and ahead. Psychol Bull 85:1030–1051, 1978 [Google Scholar]
- 47.Ma VY, Chan L, Carruthers KJ: Incidence, prevalence, costs, and impact on disability of common conditions requiring rehabilitation in the United States: Stroke, spinal cord injury, traumatic brain injury, multiple sclerosis, osteoarthritis, rheumatoid arthritis, limb loss, and back pain. Arch Phys Med Rehabil 95:986–995, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.MacKenzie EJ, Morris JA, Jurkovich GJ, Yasui Y, Cushing BM, Burgess AR, DeLateur BJ, McAndrew MP, Swiontkowski MF: Return to work following injury: The role of economic, social, and job-related factors. Am J Public Health 88:1630–1637, 1998 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.MacKinnon DP, Lockwood CM, Hoffman JM, West SG, Sheets V: A comparison of methods to test mediation and other intervening variable effects. Psychol Meth 7:83, 2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Mafi JN, McCarthy EP, Davis RB, Landon BE: Worsening trends in the management and treatment of back pain. JAMA Intern Med 173:1573–1581, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.The Many Dimensions of Hispanic Identity. An M Pew Research Center’s Social & Demographic Trends Project 2015. Available at: http://www.pewsocialtrends.org/2015/06/11/chapter-7-the-many-dimensions-of-hispanic-racial-identity/. Accessed May 31, 2018.
- 52.Martel M, Dionne F, Scott W: The mediating role of pain acceptance in the relation between perceived injustice and chronic pain outcomes in a community sample. Clin J Pain 33:509–516, 2017 [DOI] [PubMed] [Google Scholar]
- 53.Martell BA, O’Connor PG, Kerns RD, Becker WC, Morales KH, Kosten TR, Fiellin DA: Systematic review: Opioid treatment for chronic back pain: Prevalence, efficacy, and association with addiction. Ann Intern Med 146:116–127, 2007 [DOI] [PubMed] [Google Scholar]
- 54.McCracken LM: Learning to live with the pain: Acceptance of pain predicts adjustment in persons with chronic pain. Pain 74:21–27, 1998 [DOI] [PubMed] [Google Scholar]
- 55.McParland J, Hezseltine L, Serpell M, Eccleston C, Stenner P: An investigation of constructions of justice and injustice in chronic pain: A Q-methodology approach. J Health Psychol 16:873–883, 2011 [DOI] [PubMed] [Google Scholar]
- 56.McParland JL, Eccleston C: “It’s not fair”: Social justice appraisals in the context of chronic pain. Curr Dir Psychol Sci 22:484–489, 2013 [Google Scholar]
- 57.McParland JL, Eccleston C, Osborn M, Hezseltine L: it’s not fair: An interpretative phenomenological analysis of discourses of justice and fairness in chronic pain. Health 15:459–474, 2010 [DOI] [PubMed] [Google Scholar]
- 58.Melzack R: The short-form McGill pain questionnaire. Pain 30:191–197, 1987 [DOI] [PubMed] [Google Scholar]
- 59.Miller MM, Scott EL, Trost Z, Hirsh AT: Perceived injustice is associated with pain and functional outcomes in children and adolescents with chronic pain: A preliminary examination. J Pain 17(11):1217–1226, 2016 [DOI] [PubMed] [Google Scholar]
- 60.Monden KR, Trost Z, Scott W, Bogart KR, Driver S: The unfairness of it all: Exploring the role of injustice appraisals in rehabilitation outcomes. Rehabil Psychol 61:44–53, 2016 [DOI] [PubMed] [Google Scholar]
- 61.Paquet M, Bois K, Rosen NO, Mayrand MH, Charbonneau-Lefebvre V, Bergeron S: Why us? Perceived injustice is associated with more sexual and psychological distress in couples coping with genito-pelvic pain. J Sex Med 13:79–87, 2016 [DOI] [PubMed] [Google Scholar]
- 62.Rodero B, Luciano JV, Montero-Marin J, Casanueva B, Palacin JC, Gili M, del Hoyo YL, Serrano-Blanco A, Garcia-Campayo J: Perceived injustice in fibromyalgia: Psychometric characteristics of the Injustice Experience Questionnaire and relationship with pain catastrophising and pain acceptance. J Psychosom Res 73:86–91, 2012 [DOI] [PubMed] [Google Scholar]
- 63.Roland M, Fairbank J: The Roland-Morris Disability Questionnaire and the Oswestry Disability Questionnaire. Spine 25:3115–3124, 2000 [DOI] [PubMed] [Google Scholar]
- 64.Roland M, Morris R: A study of the natural history of low-back pain. Part II: Development of guidelines for trials of treatment in primary care. Spine 8:145–150, 1983 [DOI] [PubMed] [Google Scholar]
- 65.Sacks GD, Hill C, Rogers JSO: Insurance status and hospital discharge disposition after trauma: Inequities in access to postacute care. J Trauma 71:1011–1015, 2011 [DOI] [PubMed] [Google Scholar]
- 66.Scott W, Sullivan M: Perceived injustice moderates the relationship between pain and depressive symptoms among individuals with persistent musculoskeletal pain. Pain Res Manag 17:335–340, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Scott W, Trost Z, Bernier E, Sullivan MJ: Anger differentially mediates the relationship between perceived injustice and chronic pain outcomes. Pain 154:1691–1698, 2013 [DOI] [PubMed] [Google Scholar]
- 68.Scott W, Trost Z, Milioto M, Sullivan MJ: Barriers to change in depressive symptoms after multidisciplinary rehabilitation for whiplash: The role of perceived injustice. Clin J Pain 31:145–151, 2015 [DOI] [PubMed] [Google Scholar]
- 69.Scott W, Trost Z, Milioto M, Sullivan MJ: Further validation of a measure of injury-related injustice perceptions to identify risk for occupational disability: A prospective study of individuals with whiplash injury. J Occup Rehabil 23:557–565, 2013 [DOI] [PubMed] [Google Scholar]
- 70.Scott W, Milioto M, Trost Z, Sullivan MJL: The relationship between perceived injustice and the working alliance: A cross-sectional study of patients with persistent pain attending multidisciplinary rehabilitation. Disabil Rehabil 1–9 [DOI] [PubMed] [Google Scholar]
- 71.Shavers VL, Lynch CF, Burmeister LF: Racial differences in factors that influence the willingness to participate in medical research studies. Ann Epidemiol 12:248–256, 2002 [DOI] [PubMed] [Google Scholar]
- 72.Speilberger C: Manual for the State-Trait Anger Expression Inventory. Odessa, FL, Psychological Assessment Resources,, 1988 [Google Scholar]
- 73.Spinhoven P, Ter Kuile M, Kole-Snijders AMJ, Hutten Mansfeld M, Den Ouden D-J, Vlaeyen JWS: Catastrophizing and internal pain control as mediators of outcome in the multidisciplinary treatment of chronic low back pain. Eur J Pain 8:211–219, 2004 [DOI] [PubMed] [Google Scholar]
- 74.The state of US Health, 1990–2016: Burden of diseases, injuries, and risk factors among US states. US Burden of Disease Collaborators. JAMA 319:1444–1472, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Sturgeon JA, Carriere JS, Kao M-CJ, Rico T, Darnall BD, Mackey SC: Social disruption mediates the relationship between perceived injustice and anger in chronic pain: A collaborative health outcomes information registry study. Ann Behav Med 50:802–812, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Sullivan MJ, Adams H, Horan S, Maher D, Boland D, Gross R: The role of perceived injustice in the experience of chronic pain and disability: Scale development and validation. J Occup Rehabil 18:249–261, 2008 [DOI] [PubMed] [Google Scholar]
- 77.Sullivan MJ, Adams H, Martel MO, Scott W, Wideman T: Catastrophizing and perceived injustice: Risk factors for the transition to chronicity after whiplash injury. Spine (Phila Pa 1976) 36:S244–S249, 2011 [DOI] [PubMed] [Google Scholar]
- 78.Sullivan MJ, Bishop SR, Pivik J: The Pain Catastrophizing Scale: Development and validation. Psychol Assess 7:524,1995 [Google Scholar]
- 79.Sullivan MJ, Scott W, Trost Z: Perceived injustice: A risk factor for problematic pain outcomes. Clin J Pain 28:484–488, 2012 [DOI] [PubMed] [Google Scholar]
- 80.Sullivan MJ, Thibault P, Simmonds MJ, Milioto M, Cantin AP, Velly AM: Pain, perceived injustice and the persistence of post-traumatic stress symptoms during the course of rehabilitation for whiplash injuries. Pain 145:325–331, 2009 [DOI] [PubMed] [Google Scholar]
- 81.Sullivan MJ, Yakobov E, Scott W, Tait R: Perceived injustice and adverse recovery outcomes. Psychol Inj Law 7:325–334, 2014 [Google Scholar]
- 82.Sullivan MJL, Adams H, Yakobov E, Ellis T, Thibault P: Psychometric properties of a brief instrument to assess perceptions of injustice associated with debilitating health and mental health conditions. Psychol Inj Law 9:48–54, 2016 [Google Scholar]
- 83.Sullivan MJL, Thibault P, Andrikonyte J, Butler H, Catchlove R, Lariviere C: Psychological influences on repetition-induced summation of activity-related pain in patients with chronic low back pain. Pain 141:70–78, 2009 [DOI] [PubMed] [Google Scholar]
- 84.Tait RC, Chibnall JT: Management of occupational low back pain: A case study of the Missouri workers, compensation system. Psychol Inj Law 9:298–312, 2016 [Google Scholar]
- 85.Tait RC, Chibnall JT: Workers, Compensation claimants with low back pain: The role of dissatisfaction in the transition to disability. Psychol Inj Law 9:16–22, 2016 [Google Scholar]
- 86.Tait RC, Chibnall JT, Krause S: The Pain Disability Index: Psychometric properties. Pain 40:171–182, 1990 [DOI] [PubMed] [Google Scholar]
- 87.Trost Z, Agtarap S, Scott W, Driver S, Guck A, Roden-Foreman K, Reynolds M, Foreman ML, Warren AM: Perceived injustice after traumatic injury: Associations with pain, psychological distress, and quality of life outcomes 12 months after injury. Rehabil Psychol 60:213–221, 2015 [DOI] [PubMed] [Google Scholar]
- 88.Trost Z, Monden KR, Buelow M, Boals A, Scott W: Perceived injustice predicts intention to litigate: Findings from a spinal cord injury sample. Psychol Inj Law 9:31–40, 2016 [Google Scholar]
- 89.Trost Z, Scott W, Buelow MT, Nowlin L, Turan B, Boals A, Monden KR: The association between injustice perception and psychological outcomes in an inpatient spinal cord injury sample: The mediating effects of anger. Spinal Cord 55:898–905, 2017 [DOI] [PubMed] [Google Scholar]
- 90.Trost Z, Van Ryckeghem D, Scott W, Guck A, Vervoort T: The effect of perceived injustice on appraisals of physical activity: An examination of the mediating role of attention bias to pain in a chronic low back pain sample. J Pain 17:1207–1216, 2016 [DOI] [PubMed] [Google Scholar]
- 91.Trost Z, Vangronsveld K, Linton SJ, Quartana PJ, Sullivan MJ: Cognitive dimensions of anger in chronic pain. Pain 153:515–517, 2012 [DOI] [PubMed] [Google Scholar]
- 92.Trost Z, Scott W, Buelow M, Boals A, Monden KR: The association between injustice perception and psychological outcomes in an inpatient spinal cord injury sample: The mediating effects of anger. Spinal Cord 55:898–905, 2017 [DOI] [PubMed] [Google Scholar]
- 93.3rd ed. Rosemont IL, United States Bone and Joint Initiative, 2014. Available at http://www.boneandjointburden.org
- 94.Yakobov E, Scott W, Stanish W, Dunbar M, Richardson G, Sullivan M: The role of perceived injustice in the prediction of pain and function after total knee arthroplasty. Pain 155:2040–2046, 2014 [DOI] [PubMed] [Google Scholar]
- 95.Yakobov E, Scott W, Stanish WD, Tanzer M, Dunbar M, Richardson G, Sullivan MJL: Reductions in perceived injustice are associated with reductions in disability and depressive symptoms after total knee arthroplasty. Clin J Pain 34:415–420, 2018 [DOI] [PubMed] [Google Scholar]
- 96.Yakobov E, Scott W, Tanzer M, Stanish W, Dunbar M, Richardson G, Sullivan M: Validation of the Injustice Experiences Questionnaire adapted for use with patients with severe osteoarthritis of the knee. J Arthritis 3:2, 2014 [Google Scholar]
- 97.Yamada K, Adachi T, Mibu A, Nishigami T, Motoyama Y, Uematsu H, Matsuda Y, Sato H, Hayashi K, Cui R, Takao Y, Shibata M, Iso H: Injustice Experience Questionnaire, Japanese version: Cross-cultural factor-structure comparison and demographics associated with perceived injustice. PLoS ONE 11, 2016:e0160567 [DOI] [PMC free article] [PubMed] [Google Scholar]


