Watch a video presentation of this article
Watch the interview with the author
Abbreviations
- BF
bridging fibrosis
- CLN
centrilobular necrosis
- IH
interface hepatitis
- P/R
preservation/reperfusion
- PT
portal tract
- VOI
venous outflow impairment
Necrosis, also referred to as cell death, is a process in which viable cells become nonviable, resulting in dissolution of the cell contents. Under physiological conditions it is a well‐regulated process that leads to replacement of individual effete cells. However, under pathological conditions, necrosis is often the end result of various forms of tissue injury.
Necrosis is a common finding in acute and chronic liver diseases, and with persistence of the underlying cause, it is followed by progressive fibrosis. Thus, the extent and pattern of necrosis is an important part of the information obtained from a liver biopsy performed during a patient's clinical evaluation. Although this information may be stated descriptively in the pathology report, it is often incorporated into a histological “grade” that also takes into consideration the degree of inflammation. The extent of necrosis is a continuum, ranging from individual cell necrosis to massive hepatic necrosis.1 The role of the pathologist is to evaluate the pattern and extent of necrosis in the context of other morphological changes, with the goal of suggesting one or more possible underlying causes.
The aim of this review is to describe the patterns and etiological correlations of necrosis that result from liver injury. For the purpose of this review, the changes will be mainly described in the context of a classic lobule, with reference to the corresponding acinar zones where applicable.
Patterns of Necrosis
Apoptosis (Individual Cell Necrosis)
Apoptosis is a term used to describe death of individual cells. Under physiological conditions it is a well‐regulated, slow process that leads to cell renewal and tissue remodeling. In pathological conditions, the process is less controlled and often more rapidly progressive (pathological apoptosis). In the liver it is commonly seen in various forms of hepatitis and is usually associated with other findings, such as inflammation, feathery degeneration, and lobular disarray. A cell undergoing apoptosis is variably referred to as “apoptotic body,” “acidophil body,” or “Councilman body” (Fig. 1).
Figure 1.
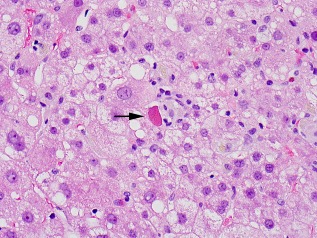
Apoptotic (acidophil) body (arrow). Note the condensation and dark staining of the cytoplasm and absence of nucleus.
Spotty and Focal Necrosis
Spotty necrosis is a term used to describe necrosis of minute clusters of hepatocytes, usually in association with lymphocytes (Fig. 2). Necrosis involving larger groups of hepatocytes within a lobule may be referred to as focal necrosis. These terms describe a continuum of lobular injury and are often used to describe lobular changes in hepatitis.
Figure 2.
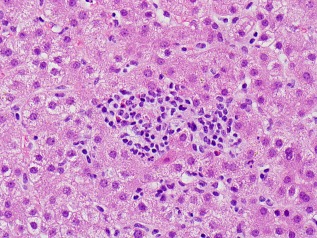
Spotty necrosis. Several adjacent hepatocytes are absent and replaced by inflammatory cells.
Zonal Necrosis
Zonal necrosis refers to necrosis involving a particular zone of the acinus, such as centrilobular (acinar zone 3) necrosis resulting from ischemic or drug‐related injury (Fig. 3). With more severe injury, necrosis may become confluent involving more than one zone within the lobule and/or extend zonally from one lobule to another adjacent lobule. The latter is termed “bridging necrosis” and can occur in various forms, such as central‐central or portal‐portal bridging necrosis.
Figure 3.
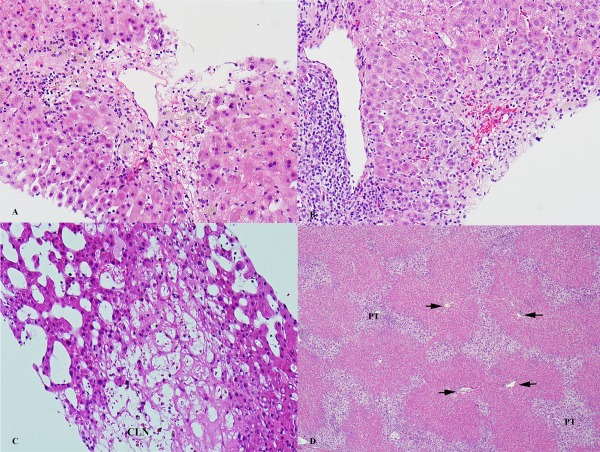
Examples of zonal necrosis. (A) Bland CLN necrosis caused by ischemia. (B) Drug‐induced hepatitis with portal inflammation and CLN. (C) Venous outflow impairment with sinusoidal dilatation and CLN. (D) Massive hepatic necrosis, with involvement of all three zones and only sparse remaining periportal hepatocytes. Foci of confluent necrosis across multiple lobules are present. Arrows point to the central veins.
Piecemeal necrosis (more currently called “interface hepatitis” [IH]) is a relatively common type of necrosis seen in hepatitis. It is characterized by inflammation extending from the portal tract (PT) into the periportal zone, with necrosis of periportal hepatocytes and disruption of the limiting plate. The limiting plate is a layer of hepatocytes surrounding the portal tact. In chronic hepatitis, this pattern of injury is an indicator of activity and is usually followed by fibrosis (Fig. 4).
Figure 4.
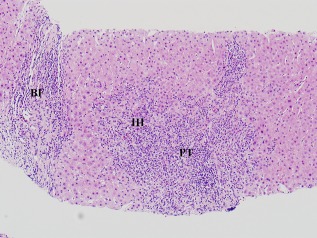
Interface hepatitis (IH) in a case of autoimmune hepatitis. The inflammatory infiltrate extends from the portal tract (PT) into the lobule, with destruction of the limiting plate of hepatocytes. Bridging fibrosis (BF) is also present.
Confluent Necrosis
Confluent necrosis describes necrosis involving multiple lobules. The process may be localized in conditions such as localized ischemic injury or as collateral injury with targeted treatment for tumors (e.g., transarterial chemotherapy or radioembolization). A more generalized severe injury results in necrosis of most or the entire liver parenchyma, referred to as submassive and massive hepatic necrosis, respectively (Fig. 3D). The latter can be most optimally diagnosed in allograft livers removed for acute liver failure or in livers removed during autopsy. Causes of massive or submassive necrosis usually include drug toxicity (e.g., acetaminophen), acute viral or autoimmune hepatitis, acute allograft failure, and fulminant Wilson's disease. In cases with confluent necrosis in which viable tissue remains, there is a striking proliferation of neocholangioles (ductules) as a reactive process, which over time is followed by fibrous scarring.
Diseases and Patterns of Necrosis
Although the patterns of necrosis are not entirely specific, they can be important clues for the underlying cause (Table 1). Additional findings such as the degree and type of inflammation may be helpful in narrowing the differential diagnoses.1, 2, 3
Table 1.
Patterns of Necrosis in Liver Disease
| Pattern of Necrosis | Description | Underlying Cause |
|---|---|---|
| Apoptosis (apoptotic body, acidophil body, or Councilman body) | Necrosis of single cells | Hepatitis (viral, autoimmune, drug) |
| Focal/spotty | Necrosis involving small clusters of hepatocytes | Hepatitis (viral, autoimmune, drug) |
| Zonal necrosis | ||
| Centrilobular | Necrosis around central vein (acinar zone 3) | Ischemia, drugs, VOI, P/R injury |
| Periportal (IH/piecemeal necrosis) | Necrosis of periportal zone (acinar zone 1) | Hepatitis (viral, autoimmune, drug) |
| Confluent necrosis | ||
| Localized (multilobular) necrosis | Necrosis of a part of the liver | Localized ischemia, transarterial embolization treatment |
| Submassive/massive necrosis | Subtotal/total hepatocellular necrosis (often with prominent ductular reaction) | Hepatitis (viral, autoimmune, drug), acute allograft failure, fulminant Wilson's disease |
Abbreviations: P/R, preservation/reperfusion; VOI, venous outflow impairment.
Viral hepatitides can be associated with all the patterns of necrosis described earlier, with mild cases showing apoptosis, spotty necrosis, and mild piecemeal necrosis, and more severe cases showing centrilobular, bridging, and confluent necrosis. Features unique to the cause may be present, such as ground‐glass cytoplasmic change with hepatitis B and viral cytopathic changes with herpes simplex virus, cytomegalovirus, and adenovirus. The type and extent of necrosis is also variable in autoimmune hepatitis; in typical untreated chronic autoimmune hepatitis there is prominent IH with many plasma cells.4
Ischemic liver injury causes centrilobular necrosis (CLN; often called “centrilobular dropout”) in mild or early cases, and confluent necrosis in more severe cases. CLN can also be seen with severe venous outflow impairment, resulting from stasis and ischemic injury; in these cases, other findings of venous outflow impairment are present, such as sinusoidal dilatation, congestion, and hemorrhage.
Drug‐induced liver injury may vary morphologically, depending on the inciting drug, with patterns of injury including bland cholestasis, cholestatic hepatitis, inflammatory hepatitis, granulomatous hepatitis, steatosis/steatohepatitis, and zonal or confluent necrosis.5 Acetaminophen is a drug well‐known for necrosis in the liver, with the extent of necrosis ranging from centrilobular to massive necrosis, the latter requiring liver transplantation. Other common drugs associated with necrosis include isoniazid, ketoconazole, nitrofurantoin, methyldopa, and fluoroquinolones.
After transplantation, necrosis in the allograft may result from preservation/reperfusion injury, acute nonfunction, rejection, ischemia, and hepatitis, with the extent and pattern of necrosis depending on the severity of the underlying cause.
In summary, necrosis in a liver specimen is an indicator of acute or ongoing injury. The pattern and extent of necrosis is often helpful toward determining or confirming the underlying cause and severity of liver injury.
Potential conflict of interest: Nothing to report.
REFERENCES
- 1. Ludwig J, Batts K. Practical Liver Biopsy Interpretation: Diagnostic Algorithms. 2nd ed. Chicago: ASCP Press; 1998. [Google Scholar]
- 2. Lefkowitch JH. Scheuer's Liver Biopsy Interpretation. 8th ed. Saunders Elsevier; 2010. [Google Scholar]
- 3. Lefkowitch JH. Liver biopsy assessment in chronic hepatitis. Arch Med Res 2007;38:634‐643. [DOI] [PubMed] [Google Scholar]
- 4. Manns MP, Czaja AJ, Gorham JD, Krawitt EL, Mieli‐Vergani G, Vergani D, et al. Diagnosis and management of autoimmune hepatitis. Hepatology 2010;51:2193‐2213. [DOI] [PubMed] [Google Scholar]
- 5. Fisher K, Vuppalanchi R, Saxena R. Drug‐induced liver injury. Arch Pathol Lab Med 2015;139:876‐887. [DOI] [PubMed] [Google Scholar]


