Abstract
Purpose:
To determine whether a bacteriophage antimicrobial-lock technique can reduce bacterial colonization and biofilm formation on indwelling central venous catheters in a rabbit model.
Materials and Methods:
Cuffed central venous catheters were inserted into the jugular vein of female New Zealand White rabbits under image guidance. Catheters were inoculated for 24 hours with broth culture of methicillin-sensitive Staphylococcus aureus. The inoculum was aspirated, and rabbits were randomly assigned to two equal groups for 24 hours: (i) untreated controls (heparinized saline lock), (ii) bacteriophage antimicrobial-lock (staphylococcal bacteriophage K, propagated titer > 108/mL). Blood cultures were obtained via peripheral veins, and the catheters were removed for quantitative culture and scanning electron microscopy.
Results:
Mean colony-forming units (CFU) per cm2 of the distal catheter segment, as a measure of biofilm, were significantly decreased in experimental animals compared with controls (control, 1.2 × 105 CFU/cm2; experimental, 7.6 × 103; P = .016). Scanning electron microscopy demonstrated that biofilms were present on the surface of five of five control catheters but only one of five treated catheters (P = .048). Blood culture results were not significantly different between the groups.
Conclusions:
In a rabbit model, treatment of infected central venous catheters with a bacteriophage antimicrobial-lock technique significantly reduced bacterial colonization and biofilm presence. Our data represent a preliminary step toward use of bacteriophage therapy for prevention and treatment of central venous catheter–associated infection.
Microorganisms that colonize indwelling catheters have the capability to form biofilms on the catheter surface, which are a microbially derived community of cells embedded in a matrix of extracellular polymeric substances that are irreversibly attached to a living or nonliving substratum. These biofilms form a microenvironment that confers increased antimicrobial resistance to the embedded microorganisms via various mechanisms. Biofilm-associated organisms can also elicit disease processes by detachment of individual cells or aggregates of cells resulting in bloodstream infections, by production of endotoxin, or by providing a niche for the development of antibiotic-resistant organisms (1–3).
Approximately 250,000 cases of intravascular catheter-related bloodstream infections occur in the United States each year, resulting in a mortality of 12%−25% with an estimated cost of treatment per episode of approximately $25,000 (4). The standard management of catheter-related infection involves decisions regarding removal of the catheter and the administration of appropriate antibiotics. Catheter removal and eventual replacement raises important practical problems in these patients requiring parenteral nutrition, chemotherapy, and hemodialysis. To avoid catheter removal, strategies for treatment of catheter-related bacteremia with antibiotics administered through the catheter or locked within the catheter lumen have been previously studied (5–7). However, antibiotic catheter salvage protocols, which include systemic antibiotics, are rarely recommended, particularly in the commonly encountered setting of coagulase-positive Staphylococcus species infection owing to a high failure rate of > 30% and the serious risk of contributing to the development of antibiotic-resistant bacteria (6,7). It is widely believed that the high rate of therapy failure is explained in part by the inability of most antibiotics to kill bacteria growing in a biofilm (3,8–15).
Bacteriophages are viruses that infect bacteria and multiply via a lytic cycle in which the phage particle attaches to the host bacterial cell surface, injects its genomic material, and takes over the host metabolic machinery, resulting in intracellular phage multiplication (1,3). Subsequent bacterial cell lysis and liberation of multiple progeny phage complete the phage lytic cycle. Bacteriophages have been used therapeutically for the treatment of infectious diseases in plants, animals, and humans (eg, dysentery, skin infections, lung infections, meningitis, wound infections, osteomyelitis) caused by various organisms, including Staphylococcus, Streptococcus, Escherichia coli, and Pseudomonas aeruginosa (16). Infections now thought to be associated with biofilms, including otitis media, urinary tract infections, periodontitis, and burn infections, have been effectively treated with phage therapy (16–18). Phage therapy could be targeted against multidrug-resistant bacteria with the potential to limit the use of antimicrobial drugs and the spread of antimicrobial resistance (9,15,17–21). Few studies have concentrated on phage application to biofilm control and treatment (19). In vitro investigations suggest that the application of bacteriophages to indwelling medical devices, such as intravascular catheters, could provide a strategy for the reduction in biofilm formation by clinically relevant bacteria such as Staphylococcus (20,21).
The purpose of this study was to evaluate bacteriophage antimicrobial therapy for treatment of Staphylococcus aureus central venous catheter–related infections in a leporine model. A secondary objective was to investigate whether bacteriophage antimicrobial therapy could reduce catheter-related bloodstream infections in a leporine model.
MATERIALS AND METHODS
Animal Model and Catheter Insertion Technique
This study was approved by the Duke University institutional animal care and use committee. Intramuscular anesthesia with ketamine (70 mg/kg body weight) and xylazine (7 mg/kg body weight) was administered to 10 female New Zealand White rabbits weighing 3–4 kg. General anesthesia was maintained with isoflurane via an endotracheal tube. After the surgical sites were shaven and prepared in usual sterile fashion, a surgical cutdown was performed over the right internal jugular vein. The vein was accessed with a 22-gauge needle under direct visualization. An 0.018-inch guide wire was inserted through the needle, which was exchanged for a micropuncture sheath (Cook, Inc, Bloomington, Indiana). A 5-F peel-away sheath (Bard Access Systems, Salt Lake City, Utah) was inserted over a 0.025-inch guide wire. The exit site was created in an intrascapular location, and a single-lumen 4.2-F Broviac catheter with polyethylene cuff (Bard Access Systems) was tunneled to the access site and inserted via the peel-away sheath (Figs 1, 2). The catheter tip was positioned in the right atrium using fluoroscopic guidance.
Figure 1.
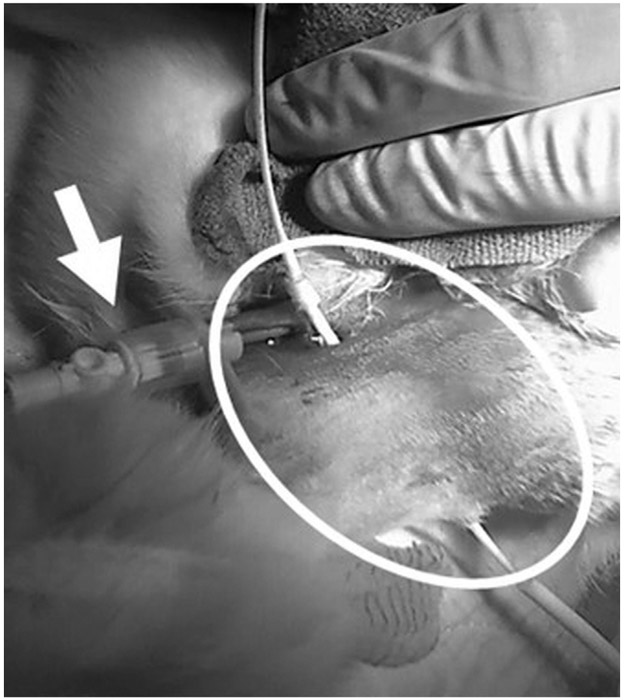
Intraoperative photograph of a female New Zealand White rabbit after insertion of the peel-away sheath (arrow) into the right internal jugular vein and interscapular subcutaneous tunneling of the 4.2-F catheter from the venotomy to the skin exit site (circle).
Figure 2.
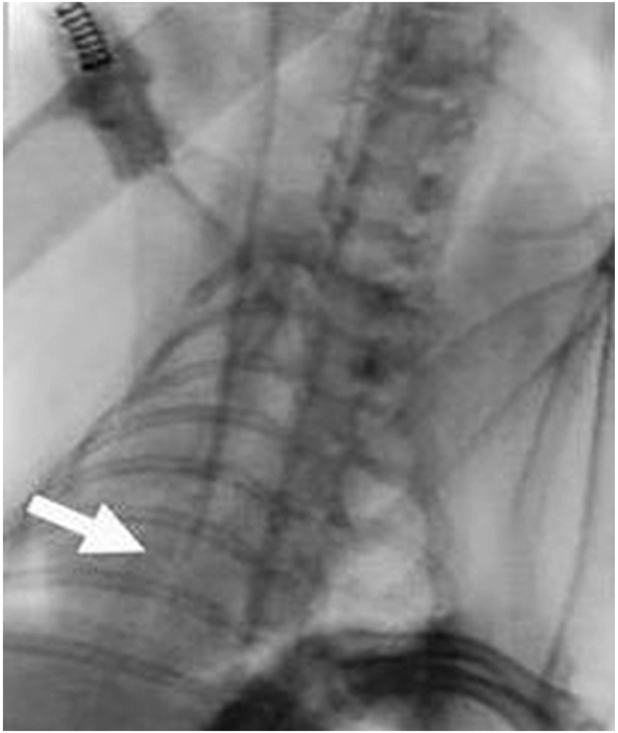
Anteroposterior and lateral intraoperative fluoroscopic images of a New Zealand White rabbit after percutaneous intrascapular tunneled line insertion. Catheter tip (arrow) projects over the right atrium.
Microorganisms and Culture Conditions
S. aureus 46106, a methicillin-susceptible isolate from an abdominal wound that was negative for toxic shock syndrome toxin and Panton-Valentine leucocidin, was obtained from the U.S. Centers for Disease Control and Prevention Clinical and Environmental Laboratory Branch culture collection. This strain was used for growing biofilms in the rabbit catheter model. Cultures were stored at —71 °C and subcultured on trypticase soy agar containing 5% sheep’s blood (blood agar) (BD Diagnostics, Franklin Lakes, New Jersey) overnight. Viable cultures were grown in Brain Heart Infusion Broth (BD Diagnostics) at 37°C with shaking to obtain a cell suspension equivalent to a 0.5 MacFarland standard (108 colony-forming units [CFU]/mL) on the day of use. S. aureus Phage K and its host strain S. aureus (ATCC 19685) were obtained from ATCC (Manassas, Virginia). Phage K was propagated using the soft agar overlay technique (22). Crude high-titer phage broth cultures were prepared according to Adams (23) using Brain Heart Infusion Broth supplemented with 3 mmol/L magnesium chloride and 4 mmol/L calcium chloride (added as MgCl2 • 6H2O and CaCl2 • 2H2O). Phage broth cultures were diluted in heparinized saline (1:10 dilution) and filter sterilized (0.2 μm) before use.
Catheter Inoculation
After placement, catheters were filled with 0.3 mL of a 108 CFU/mL log phase culture of S. aureus 46106. The inoculum was locked in the lumen of the indwelling catheter and remained in place for 24 hours. After 24 hours, the inoculum was carefully withdrawn from all catheters by aspiration. Experimental design was based on prior work with bacteriophage K and clinical S. aureus strain (19,21).
Experimental Approach
The 10 rabbits were randomly assigned to treatment or control arms. After 24 hours of bacterial inoculation, five control-arm animal catheters were locked with 0.3 mL of heparinized saline, and five experimental-arm catheters were locked with 0.3 mL of a 108 plaque-forming units/mL solution of bacteriophage K, prepared as described earlier, for 24 hours. After 24 hours of lock treatment, blood cultures were obtained from each treated and control animal via peripheral ear veins and analyzed using the BACTEC 9000 System (BD Diagnostics) reporting presence of bacteremia, species, and antibiotic sensitivity profile. All rabbits were euthanized by intravenous injection of sodium thiopental (Euthasol euthanasia solution; Virbac, Fort Worth, Texas). Catheters were removed for microbiologic evaluation using aseptic technique, clamped on each end to prevent dehydration of biofilms in the catheter lumen, and processed to recover microorganisms from the luminal surfaces using a previously published method (21). Briefly, the outer surface of the catheters was disinfected with 0.525% sodium hypochlorite, rinsed in sodium thiosulfate, and air dried in a biologic safety cabinet. A 1-cm section was cut from the distal end of the catheter, rinsed gently in sterile phosphate-buffered saline, and bisected lengthwise using a sterile scalpel. Each half of the catheter section was placed into a tube containing 10 mL of phosphate-buffered saline and subjected to three alternating 30-second cycles of water bath sonication (45 kHz, Branson Sonicator; Branson Ultrasonics Corporation, Danbury, Connecticut) and vortexing. The resulting biofilm suspension was diluted in Butterfield Phosphate Buffer (Hardy Diagnostics, Santa Maria, California), and the dilution plated on blood agar, incubated for 48 hours at 37°C, and counted using standard microbiology technique.
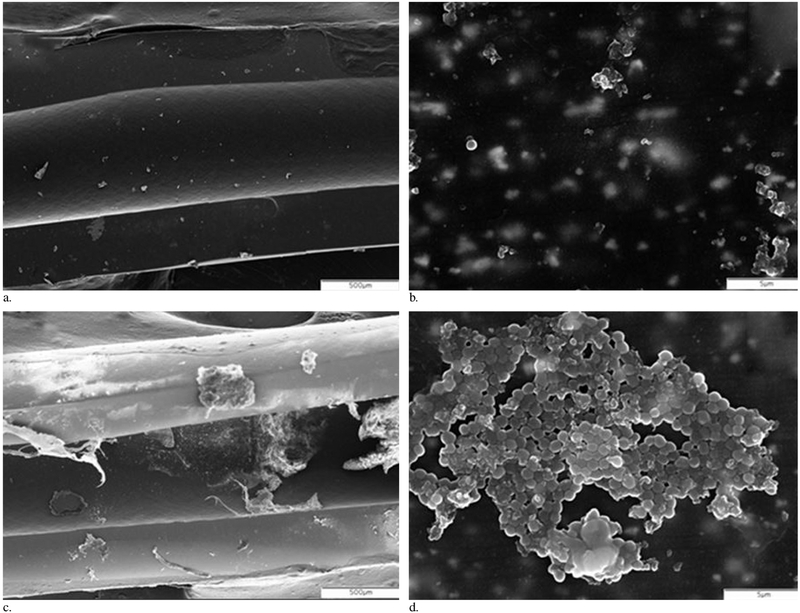
Scanning Electron Microscopy of Catheter Segments
Adjacent catheter segments were also collected for examination using scanning electron microscopy (SEM). Catheter segments were opened to expose the lumen, fixed in 2% glutaraldehyde, and dehydrated for SEM. The fixed and dehydrated catheter segments were sputter coated with gold-palladium (60/40) and viewed under a Philips XL30 scanning electron microscope (FEI Company, Hillsboro, Oregon). Subjective assessment of biofilm burden was based on nonquantitative evaluation of SEM images from each of the catheter segments by a pathologist blinded to the experimental design. Images were graded as either positive for biofilm (presence of biofilm cells on the catheter surface) or negative (absence of biofilm cells on the catheter surface).
Statistical Analysis
All statistical tests were performed using SPSS version 19 (IBM, Armonk, New York). Mean plate counts (as log10 CFU per cm2) for treated and untreated catheter sections were compared using the Mann-Whitney U test. Results from blood cultures and qualitative SEM biofilm analyses were compared between the groups with the Fisher exact test (two-tailed). A P value < 0.05 was considered statistically significant.
RESULTS
All 10 rabbits survived the catheter insertion, inoculation, and treatment protocol. After intraluminal inoculation with S. aureus and a subsequent catheter lock solution consisting of heparinized saline for 24 hours, analysis of catheter tips from these control animals revealed a mean of 1.2 × 105 CFU/cm2 (range, 2.7 × 104—3.6 × 105 CFUcm2; SE, 6.3 × 104 CFU/cm2). In comparison, catheter tips from catheters that were treated with a catheter lock solution consisting of bacteriophage K for 24 hours had a mean of 7.6 × 103 CFU/cm2 (range, 0–3.46 × 104 CFU/cm2; SE, 6.7 × 103 CFU/cm2); this was significantly lower than the control group (P = .016) (Fig 3).
Figure 3.
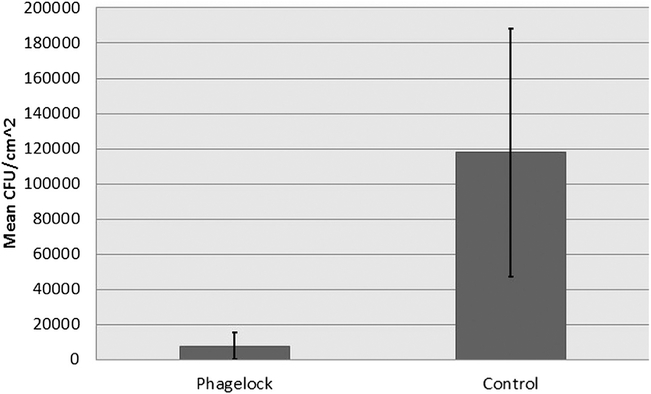
Mean CFU/cm2 of experimental bacteriophage-treated and control groups (n = 5 per group; P = .016).
SEM analysis of the catheter segments demonstrated qualitative reduction of biofilm in treated catheter segments compared with untreated controls (five of five controls with biofilm present, one of five experimental catheter segments with biofilm present, P — .048) (Fig 4a–d). Blood culture results were not significantly different between the control and experimental groups (three of five positive vs four of five positive, P — 1.0). Positive blood cultures in all instances confirmed the presence of methicillin-sensitive S. aureus.
Figure 4.
Representative SEM images of distal catheter segments. Experimental catheter segment is shown under 40× (a) and 4,000× (b) and demonstrates no visible bacterial cells or biofilm matrix. Control catheter segment image reveals biofilm-coated catheter segment at both 40× (c) and 4,000× (d).
DISCUSSION
The broad objective of this research was to investigate further an alternative antimicrobial therapy for salvage treatment of long-term central venous catheter–related infection using bacteriophage. We demonstrated in an animal model a significant decrease in S. aureus biofilm formation on the intraluminal surface of indwelling central venous catheters treated with a bacteriophage lock compared with untreated controls. Prior studies by Curtin and Donlan (21) and Fu et al (20) demonstrated in in vitro models 99.9%–99.99% reductions of bacteria on catheters pretreated with bacteriophage; later, Lungren et al (19) demonstrated > 99% reduction of biofilm on treated catheter surface material using bacteriophage in vitro. However, the clinical significance of this prior in vitro work is unclear. Phage therapy involves the targeted application of bacteriophages that, on encounter with specific pathogenic bacteria, can infect and kill them. To be successful, phage therapy must deliver sufficient phage density in the vicinity of the target bacteria to achieve bacterial clearance (24,25). For this reason, the antimicrobial “lock” strategy used in the present study as a treatment for indwelling central venous catheter infections has a high likelihood of delivering satisfactorily high concentrations of phage to the target in vivo. In view of the more challenging environment in the animal model, the 94% reduction in biofilm formation in the present study is noteworthy. Examination by SEM also confirmed qualitative reduction of biofilm in treated catheter segments.
Bacteriophage K, used in the present study, is a polyvalent Staphylococcus phage and is capable of lysing 10 different Staphylococcus epidermidis strains and 9 different Staphylococcus species including a vancomycin-resistant S. aureus strain and several methicillin-resistant S. aureus strains (26–29). Our study used bacteriophage K titers in a bacteriophage lock in the lumen of colonized catheters with concentrations of > 108 plaque-forming units/mL. We are unaware of other studies that have investigated the use of bacteriophage K in an animal model, and it is currently unknown whether varying phage concentrations would lead to a more or less effective therapeutic response. Further work is needed to delineate an ideal dwell time, concentration, and systemic response to therapy. At the present time, it is virtually unknown how phage will interact when exposed to the intravenous environment in humans, and research is needed to understand what is likely to be a complex biologic interaction.
Catheter-related infection can occur via numerous routes, including intraluminal contamination from infusates and handling, extraluminal tracking of microorganisms along the outer surface of the catheter into the bloodstream, and hematogenous seeding from a distant source (30). Our in vivo experiment employed a model of intraluminal colonization with bacteriophage lock therapy 24 hours after initial inoculation. The effective use of bacteriophage therapy relies on employing a bacteriophage specific for the bacterial strain being targeted. Although the specific bacteriophage can be generated or obtained when the responsible bacterial strain has been identified, a more practical approach may involve the use of a “cocktail” of a variety of bacteriophages against the most common, or perhaps the most virulent, organisms. Although this strategy could potentially treat the catheter lumen, it does not address the outer surface of the catheter and the bloodstream, both of which are frequently involved in catheter-related infection. With our experimental model, bloodstream seeding likely occurs during or very soon after catheter lumen inoculation. It is not surprising that we did not find a reduction in bacteremia with the bacteriophage lock therapy considering that the quantity and technique chosen for bacteriophage treatment was designed solely for treatment of the catheter lumen. This study is a preliminary step toward the development of a new strategy for treating central venous catheter infections because bacteriophage therapy has never been reported, to our knowledge, for an intravascular surface.
This study has additional limitations. The small sample size may limit a broad generalization of the findings, although statistical significance was achieved. The biofilm in this work was artificially composed entirely of a single strain of S. aureus. However, we chose bacteriophage K because it has a broad spectrum of lytic activity, particularly against the organisms most commonly found in device-associated infections. Further work is needed to investigate effectiveness of phage therapy on polymicrobial biofilms. With this study design, there is the potential for sampling error because only 1 cm of distal intravenous catheter was sampled for analysis, and it is possible that alternative catheter segment sampling strategies would yield different results. Nonetheless, this protocol was in keeping with standard of care for the management and speciation of indwelling central line infections. We did not compare varying phage lock catheter dwell times, concentration of phage, or, more importantly, the rabbit antibody response after exposure to phage therapy. Based on prior literature, it is possible that phage lock therapy may lead to decreased effectiveness over time secondary to the immune response and subsequent clearance (26–29). Further work is needed to investigate this and other important aspects of this therapeutic strategy.
In conclusion, treatment of central venous catheter S. aureus infection with a bacteriophage antimicrobial-lock technique significantly reduced bacterial colonization and biofilm presence in a leporine model. Although evidence supporting the use of phages for the treatment of device-associated biofilms in humans is lacking, this and other recent studies involving the interaction of phage and biofilms have shown phages to have promise as an alternative therapy for biofilm-associated infection. Further investigation is warranted.
Acknowledgments
The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of the U.S. Centers for Disease Control and Prevention (CDC). This study was funded in part by grants from the Society of Interventional Radiology (SIR) and the American Society for Parenteral and Enteral Nutrition (ASPEN).
ABBREVIATIONS
- CFU
colony-forming unit
- SEM
scanning electron microscopy
Footnotes
None of the authors have identified a conflict of interest.
Contributor Information
Matthew P. Lungren, Department of Radiology, Stanford University Medical Center, 725 Welch Road, Room 1690 MC 5913, Palo Alto, CA 94304.
Rodney M. Donlan, Centers for Disease Control and Prevention, Atlanta, Georgia.
Ravi Kankotia, Interventional Radiology Translational Research Laboratory, Department of Radiology, Duke University Medical Center, Durham, North Carolina..
Ben E. Paxton, Interventional Radiology Translational Research Laboratory, Department of Radiology, Duke University Medical Center, Durham, North Carolina..
Irene Falk, Interventional Radiology Translational Research Laboratory, Department of Radiology, Duke University Medical Center, Durham, North Carolina..
Diana Christensen, Interventional Radiology Translational Research Laboratory, Department of Radiology, Duke University Medical Center, Durham, North Carolina..
Charles Y. Kim, Interventional Radiology Translational Research Laboratory, Department of Radiology, Duke University Medical Center, Durham, North Carolina..
REFERENCES
- 1.Kay MK, Erwin TC, McLean RJ, Aron GM. Bacteriophage ecology in Escherichia coli and Pseudomonas aeruginosa mixed-biofilm communities. Appl Environ Microbiol 2011; 77:821–829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ferreira JA, Carr JH, Starling CE, de Resende MA, Donlan RM. Biofilm formation and effect of caspofungin on biofilm structure of Candida species bloodstream isolates. Antimicrob Agents Chemother 2009; 53: 4377–384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cicalini S, Palmieri F, Petrosillo N. Clinical review: new technologies for prevention of intravascular catheter-related infections. Crit Care 2004; 8: 157–162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Umscheid CA, Mitchell MD, Doshi JA, Agarwal R, Williams K, Brennan PJ. Estimating the proportion of healthcare-associated infections that are reasonably preventable and the related mortality and costs. Infect Control Hosp Epidemiol 2011; 32:101–114. [DOI] [PubMed] [Google Scholar]
- 5.Schoot RA, van Dalen EC, van Ommen CH, van de Wetering MD. Antibiotic and other lock treatments for tunnelled central venous catheter-related infections in children with cancer. Cochrane Database Syst Rev 2013; 6:CD008975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.O’Horo JC, Silva GL, Safdar N. Anti-infective locks for treatment of central line-associated bloodstream infection: a systematic review and meta-analysis. Am J Nephrol 2011; 34:415–422. [DOI] [PubMed] [Google Scholar]
- 7.Maya ID, Carlton D, Estrada E, Allon M. Treatment of dialysis catheter-related Staphylococcus aureus bacteremia with an antibiotic lock: a quality improvement report. Am J Kidney Dis 2007; 50:289–295. [DOI] [PubMed] [Google Scholar]
- 8.Krishnasami Z, Carlton D, Bimbo L, et al. Management of hemodialysis catheter-related bacteremia with an adjunctive antibiotic lock solution. Kidney Int 2002; 61:1136–1142. [DOI] [PubMed] [Google Scholar]
- 9.Snaterse M, Ruger W, Scholte Op Reimer WJ, Lucas C. Antibiotic-based catheter lock solutions for prevention of catheter-related bloodstream infection: a systematic review of randomised controlled trials. J Hosp Infect 2010; 75:1–11. [DOI] [PubMed] [Google Scholar]
- 10.Hockenhull JC, Dwan K, Boland A, et al. The clinical effectiveness and cost-effectiveness of central venous catheters treated with anti-infective agents in preventing bloodstream infections: a systematic review and economic evaluation. Health Technol Assess 2008; 12:1–154, iii–iv, xi–xii. [DOI] [PubMed] [Google Scholar]
- 11.Vuong C, Kocianova S, Yao Y, Carmody AB, Otto M. Increased colonization of indwelling medical devices by quorum-sensing mutants of Staphylococcus epidermidis in vivo. J Infect Dis 2004; 190:1498–1505. [DOI] [PubMed] [Google Scholar]
- 12.Capdevila JA, Gavalda J, Fortea J, et al. Lack of antimicrobial activity of sodium heparin for treating experimental catheter-related infection due to Staphylococcus aureus using the antibiotic-lock technique. Clin Microbiol Infect 2001; 7:206–212. [DOI] [PubMed] [Google Scholar]
- 13.Bassetti S, Hu J, D’Agostino RB Jr, Sherertz RJ. Prolonged antimicrobial activity of a catheter containing chlorhexidine-silver sulfadiazine extends protection against catheter infections in vivo. Antimicrob Agents Chemother 2001; 45:1535–1538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.van de Wetering MD, van Woensel JB. Prophylactic antibiotics for preventing early central venous catheter Gram positive infections in oncology patients. Cochrane Database Syst Rev 2007(1):CD003295. [DOI] [PubMed] [Google Scholar]
- 15.Miedzybrodzki R, Fortuna W, Weber-Dabrowska B, Gorski A. Phage therapy of staphylococcal infections (including MRSA) may be less expensive than antibiotic treatment. Postepy Hig Med Dosw (Online) 2007; 61:461–65. [PubMed] [Google Scholar]
- 16.Weber-Dabrowska B, Mulczyk M, Gorski A. Bacteriophage therapy of bacterial infections: an update of our institute’s experience. Arch Immun Ther Exp (Warsz) 2000; 48:547–551. [PubMed] [Google Scholar]
- 17.Weber-Dabrowska B, Dabrowski M, Slopek S. Studies on bacteriophage penetration in patients subjected to phage therapy. Arch Immun Ther Exp (Warsz) 1987; 35:563–568. [PubMed] [Google Scholar]
- 18.Slopek S, Weber-Dabrowska B, Dabrowski M, Kucharewicz-Krukowska A. Results of bacteriophage treatment of suppurative bacterial infections in the years 1981-1986. Arch Immun Ther Exp (Warsz) 1987; 35:569–583. [PubMed] [Google Scholar]
- 19.Lungren MP, Christensen D, Kankotia R, Falk I, Paxton BE, Kim CY. Bacteriophage K for reduction of biofilm on central venous catheter material. Bacteriophage 2013; 3:e26825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fu W, Forster T, Mayer O, Curtin JJ, Lehman SM, Donlan RM. Bacteriophage cocktail for the prevention of biofilm formation by Pseudomonas aeruginosa on catheters in an in vitro model system. Antimicrob Agents Chemother 2010; 54:397–04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Curtin JJ, Donlan RM. Using bacteriophages to reduce formation of catheter-associated biofilms by Staphylococcus epidermidis. Antimicrob Agents Chemother 2006; 50:1268–1275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Obuchowski M, Stopa M. Quick and efficient method for recovering of bacteriophages from soft agar after their propagation by the plate lysate technique. Acta Biochim Pol 1993; 40:98–99. [PubMed] [Google Scholar]
- 23.Adams MH. The stability of bacterial viruses in solutions of salts. J Gen Physiol 1949; 32:579–594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Abedon ST, Kuhl SJ, Blasdel BG, Kutter EM. Phage treatment of human infections. Bacteriophage 2011; 1:66–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kutter E, De Vos D, Gvasalia G, et al. Phage therapy in clinical practice: treatment of human infections. Curr Pharm Biotechnol 2010; 11:69–86. [DOI] [PubMed] [Google Scholar]
- 26.Kutter E, Sulakvelidze A. Bacteriophages Biology and Applications. Boca Raton, FL: CRC Press; 2005. [Google Scholar]
- 27.O’Flaherty S, Ross RP, Meaney W, Fitzgerald GF, Elbreki MF, Coffey A. Potential of the polyvalent anti-Staphylococcus bacteriophage K for control of antibiotic-resistant staphylococci from hospitals. Appl Environ Microbiol 2005; 71:1836–1842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Scholl D, Rogers S, Adhya S, Merril CR. Bacteriophage K1-5 encodes two different tail fiber proteins, allowing it to infect and replicate on both K1 and K5 strains of Escherichia coli. J Virol 2001; 75:2509–2515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cerca N, Oliveira R, Azeredo J. Susceptibility of Staphylococcus epidermidis planktonic cells and biofilms to the lytic action of staphylococcus bacteriophage K. Lett Appl Microbiol 2007; 45:313–317. [DOI] [PubMed] [Google Scholar]
- 30.Miller DL, Balter S, Dixon RG, et al. Quality improvement guidelines for recording patient radiation dose in the medical record for fluoroscopically guided procedures. J Vasc Interv Radiol 2012; 23:11–18. [DOI] [PubMed] [Google Scholar]