From the Authors:
We welcome the interest shown by Lescoat and colleagues and Khamis and colleagues in our publication (1), and thank the authors for their letters. Although the clinical value of plasma biomarkers is well established in many chronic disease states, we recognize that limitations exist regarding their use in prognostication of outcomes. As alluded to by Lescoat and colleagues, the magnitude of the prognostic effect for individual plasma biomarkers will likely vary across diverse forms of interstitial lung disease (ILD) and at different thresholds. Indeed, circulating plasma biomarker levels may be lower relative to biomarker concentrations within specific organs that are directly involved in tissue repair and homeostasis. Also, the extent of disease activity that typically occurs across multiple extrapulmonary organs, such as those affected in connective tissue disease associated with ILD, may accentuate this variation. With regard to IL-6, it has been suggested that this cytokine has a bidirectional role in the pathogenesis of lung fibrosis. Whereas IL-6 blockade at an early inflammatory stage can accelerate lung fibrosis, blockade at an early fibrotic stage may ameliorate subsequent fibrogenesis (2). These factors could conceivably account for the potentially favorable results that are observed when IL-6 is therapeutically targeted in scleroderma-associated ILD (3). We did find that mean plasma IL-6 levels were nonsignificantly decreased in subjects with enlarged mediastinal lymph nodes (MLNs) in our study, but chose to report median plasma cytokine values in our comparative analyses because these values are less subject to the influence of outliers (1). In both our primary and replication cohorts, the median plasma IL-6 levels did not differ by MLN size (Figure 1) and did not predict mortality risk. We therefore reiterate that we cannot conclude from the data presented in our study that IL-6 might be protective in fibrotic ILD, and agree with Lescoat and colleagues that further study of the blockade of IL-6 in clinical trials is warranted (1).
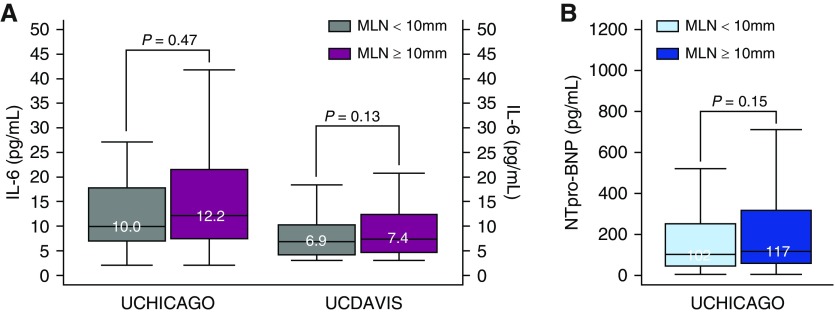
Figure 1.
(A) Box plots depicting IL-6 (pg/ml) levels stratified by MLN size (mm) in patients with ILD within the UCHICAGO (n = 116) and UCDAVIS (n = 118) cohorts. Comparison of cytokine concentrations in patients with MLN < 10 mm and MLN ≥ 10 mm, using the Wilcoxon signed-rank test for matched nonparametric data in 10,000 bootstrap replications to improve precision at the 95% confidence interval level. (B) Box plots depicting NT-proBNP (pg/ml) levels stratified by MLN size (mm) in patients with ILD within the UCHICAGO cohort (n = 628). For clarity, NT-proBNP data points for two subjects (16,116 and 22,812 pg/ml) are not depicted. Group comparisons for unmatched nonparametric data were conducted using the Pearson chi-squared test for equality of the medians between patients with MLN ≥ 10 mm (purple) and MLN < 10 mm (gray). ILD = interstitial lung disease; MLN = mediastinal lymph node; NTpro-BNP = N-terminal pro–B-type natriuretic peptide; UCDAVIS = University of California, Davis; UCHICAGO = University of Chicago.
Lescoat and colleagues also raise the important issue of chronic heart failure, which may be prevalent in ILD and should be carefully considered when evaluating the impact of novel indices on assessment of clinical outcomes such as hospitalization and mortality. Because it is possible that cardiac disease may at least in part causally mediate the link between MLN enlargement and ILD outcomes (4, 5), we explored the association of NT-proBNP (N-terminal pro–B-type natriuretic peptide) levels with MLN enlargement in our outcome analyses. We found that including this cardiac biomarker in our prognostic models did not significantly alter the predictive value of MLN for all-cause mortality or hospitalization. Furthermore, plasma NT-proBNP levels did not differ with MLN enlargement and lacked a strong correlation with MLN diameter (Figure 1).
We also agree with Khamis and colleagues, who, along with Lescoat and colleagues, wondered about the potential role of inhalational exposures in the etiopathogenesis of MLN enlargement and ILD. Perhaps the lung’s activity as an immunologic organ and the associated enlarged MLNs reflect ongoing inflammation from active immunologic responses to anthracosis and other dust-related environmental exposures. Indeed, the average MLN diameters in smokers within our cohort were larger than those observed in never smokers. As astutely outlined by Khamis and colleagues, patients with various ILDs commonly have inorganic and organic environmental exposures that may impact outcomes. Although our prognostic models adjusted for duration of exposure to inhalational tobacco use, other unmeasured environmental exposures could potentially contribute to disease progression in pulmonary fibrosis. As such, it is certainly possible that MLN enlargement may be a biomarker of ongoing occupational or environmental exposure. Although these exposures may play a causal role, our study was not designed to assess causality, and thus we are unable to ascertain the potential etiologies for the observed MLN enlargement. In addition, it should be noted that many of our patients with ILD had MLNs of unremarkable size, which suggests that enlarged MLNs are not a required precursor to ILD development, and therefore the relationship between prior environmental exposures and enlarged MLN size is unclear. Future investigations should systematically assess the cytologic characteristics of enlarged MLNs and evaluate the enlargement in the context of dose and temporal relationships with occupational and environmental exposures.
Altogether, we concur with Lescoat and colleagues and Khamis and colleagues in the realization that beyond prognostication, our study constitutes a crucial first step toward elucidating the role of MLNs in disease etiopathogenesis and refining the current classification of ILD.
Footnotes
Supported by NIH R21AI126031, NIH K23HL138190, NIH R01AI125644, and NIH R01HL130796.
Originally Published in Press as DOI: 10.1164/rccm.201811-2208LE on January 17, 2019.
Author disclosures are available with the text of this letter at www.atsjournals.org.
References
- 1.Adegunsoye A, Oldham JM, Bonham C, Hrusch C, Nolan P, Klejch W, et al. Prognosticating outcomes in interstitial lung disease by mediastinal lymph node assessment: an observational cohort study with independent validation. Am J Respir Crit Care Med. doi: 10.1164/rccm.201804-0761OC. [online ahead of print] 14 Sep 2018; DOI: 10.1164/rccm.201804-0761OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kobayashi T, Tanaka K, Fujita T, Umezawa H, Amano H, Yoshioka K, et al. Bidirectional role of IL-6 signal in pathogenesis of lung fibrosis. Respir Res. 2015;16:99. doi: 10.1186/s12931-015-0261-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Khanna D, Denton CP, Jahreis A, van Laar JM, Frech TM, Anderson ME, et al. Safety and efficacy of subcutaneous tocilizumab in adults with systemic sclerosis (faSScinate): a phase 2, randomised, controlled trial. Lancet. 2016;387:2630–2640. doi: 10.1016/S0140-6736(16)00232-4. [DOI] [PubMed] [Google Scholar]
- 4.Dalleywater W, Powell HA, Hubbard RB, Navaratnam V. Risk factors for cardiovascular disease in people with idiopathic pulmonary fibrosis: a population-based study. Chest. 2015;147:150–156. doi: 10.1378/chest.14-0041. [DOI] [PubMed] [Google Scholar]
- 5.Ngom A, Dumont P, Diot P, Lemarié E. Benign mediastinal lymphadenopathy in congestive heart failure. Chest. 2001;119:653–656. doi: 10.1378/chest.119.2.653. [DOI] [PubMed] [Google Scholar]