Abstract
Rationale: In developing countries, poor and rural areas have a high burden of chronic obstructive pulmonary disease (COPD), and environmental pollutants and indoor burning of biomass have been implicated as potential causal exposures. Less is known about the prevalence of COPD in the United States with respect to urban–rural distribution, poverty, and factors that uniquely contribute to COPD among never-smokers.
Objectives: To understand the impact of urban–rural status, poverty, and other community factors on COPD prevalence nationwide and among never-smokers.
Methods: We studied a nationally representative sample of adults in the National Health Interview Survey 2012–2015, with data linkage between neighborhood data from the U.S. Census’s American Community Survey and the National Center for Health Statistics Urban–Rural Classification Scheme. The main outcome was COPD prevalence.
Measurements and Main Results: The prevalence of COPD in poor, rural areas was almost twice that in the overall population (15.4% vs. 8.4%). In adjusted models, rural residence (odds ratio [OR], 1.23; P < 0.001) and census-level poverty (OR, 1.12; P = 0.012) were both associated with COPD prevalence, as were indicators of household wealth. Among never-smokers, rural residence was also associated with COPD (OR, 1.34; P < 0.001), as was neighborhood use of coal for heating (OR, 1.09; P < 0.001).
Conclusions: In a nationally representative sample, rural residence and poverty were risk factors for COPD, even among never-smokers. The use of coal for heating was also a risk factor for COPD among never-smokers. Future disparities research to elucidate contributors to COPD development in poor and rural areas, including assessments of heating sources and environmental pollutants, is needed.
Keywords: COPD, chronic obstructive pulmonary disease, epidemiology, rural health, health disparities
At a Glance Commentary
Scientific Knowledge on the Subject
There is increasing awareness of nationwide disparities in chronic obstructive pulmonary disease (COPD), with a recognized need to better understand the risks for COPD in rural areas. The COPD National Action Plan recently identified the need to conduct surveys designed to investigate geographic urban–rural differences as a major goal. Previous studies have identified differences in smoking rates as a contributor to urban–rural disparities in COPD, but there is a need to understand individual and community factors that increase the risk for developing COPD in the population as a whole and among never-smokers.
What This Study Adds to the Field
This is the first study to report individual, community, and geographic risk factors for COPD in the United States. The study findings demonstrate that living in a rural community and poverty are independent risk factors for COPD among both ever- and never-smokers. The study also demonstrates that community use of coal for heating represents an additional risk factor for COPD among never-smokers. These results suggest that future studies and public health initiatives should investigate household and community-level environmental factors that contribute to COPD prevalence in rural parts of the United States in order to reduce disparities.
Chronic obstructive pulmonary disease (COPD) continues to be a leading cause of morbidity and mortality worldwide (1–3). In the United States, smoking remains the strongest risk factor for development of COPD, although international studies suggest that poverty and indoor air pollution from the burning of biomass may contribute to the burden of COPD worldwide, even among those who do not smoke (4–6). Although significant work has informed our understanding of the international prevalence of COPD, substantial knowledge gaps exist regarding factors that contribute to the regional distribution of COPD in the United States, especially for the estimated 20% of COPD that occurs among never-smokers (7, 8). Beyond smoking, other exposures and risk factors that may contribute to COPD development include exposure to indoor and outdoor pollution, and solid fuel (coal and wood) combustion—exposures that are likely to differ between urban and rural areas (8). Rural COPD has become a recent focus of the NIH and CDC, with a disproportionate increase in prevalence and mortality being observed in isolated rural areas (1, 8, 9). The COPD National Action Plan also recently identified the development of surveys and targeted studies designed to understand urban–rural differences and environmental disparities in COPD as a major goal (10, 11). However, rural individuals in the United States still remain understudied compared with their urban counterparts (12). Due to limited research in rural areas, it has been difficult to separate the impacts of individual factors, and community-level exposures with potential regional variation, in characterizing this COPD disparity in the United States (13–15).
We linked publically available datasets to 1) describe the nationwide prevalence of COPD by urban–rural status and community-level poverty; 2) determine the impact of community and individual factors such as rural residence, community poverty, household heating exposures, and socioeconomic status on COPD prevalence; and 3) describe prevalence and determine risk factors for COPD among never-smokers and current or former smokers. Some of the results from this study have been previously reported in the form of an abstract (16).
Methods
Data Sources and Study Sample
Data were obtained from the National Health Interview Survey (NHIS) for the years 2012–2015. The NHIS is a cross-sectional household interview survey that is conducted annually by the National Center for Health Statistics (NCHS). The survey uses a multistate probability design and covers all 50 states and the District of Columbia. The survey was chosen because it is designed to be representative of the noninstitutionalized population living within the United States. Our study population was limited to adults ≥40 years of age, as COPD is a disease of older adults.
To evaluate the effect of community factors on COPD prevalence, we linked participants’ census tract information to the U.S. Census Bureau’s 2015 American Community Survey (ACS) and to the 2013 NCHS Urban–Rural Classification of Counties. Urbanization was assessed using the 2013 NCHS Urban–Rural Classification, which divides counties into six categories: 1) large metro central, 2) large metro fringe, 3) medium metro, 4) small metro, 5) micropolitan, and 6) noncore. Generally, large metro fringe is thought to be equivalent to suburban, and large metro central is considered urban (17). The nonmetropolitan areas, micropolitan and noncore, are considered rural. We combined these categories for our analysis because relatively few of the participants resided in these areas.
Census tract information is restricted and not available in the public-use NHIS dataset. The NCHS Research Ethics Review Board approved data collection from the NHIS to be linked to census tract information in our study. Analysis of deidentified data from the survey is exempt from the federal regulations for the protection of human research participants. The NCHS Research Ethics Review Board approved the analysis of restricted data through the NCHS Research Data Center in Hyattsville, Maryland.
Outcomes
Our primary outcome was a diagnosis of COPD defined by self-report from the NHIS. Participants were labeled as having COPD by answering “yes” to having COPD, emphysema, or chronic bronchitis. Given the potential for misclassification, in our sensitivity analyses we excluded individuals who reported a current diagnosis of asthma, and removed chronic bronchitis from our definition of COPD.
Census-Level Variables
We also used the ACS to gather census-level exposures that may increase COPD prevalence, including poverty, occupations associated with lung disease (i.e., agricultural), and household heating sources (18). The 2015 ACS provided the percentage of households living below the poverty level in each census tract. We divided census tracts into poor and nonpoor based on a definition of 20% of households residing below the poverty line (19). The ACS also provided data on the primary heating source used by households in each census tract, including the percentage of households using solid fuels (coal and wood) for primary heating. Data regarding census-level occupations were also available from the ACS, which grouped certain occupations together, such as agriculture and mining.
Participant-Level Variables
The NHIS was used to obtain information on risk factors for COPD at the individual level, including demographics, region of residence, smoking information, and household income-to-poverty ratio. Because of missing data regarding income, multiple imputed income provided by the CDC was used for analyses of household poverty, reported as the income-to-poverty ratio (20). These data were generated by the CDC using multivariate imputation implemented by the module IMPUTE with IVE-ware (www.isr.umich.edu/src/smp/ive) and were analyzed with multiple imputation estimate commands (21). Additional socioeconomic variables provided by the NHIS included home ownership, health insurance status, and education. Health insurance was used as a surrogate for access to healthcare.
Smoking status was obtained from the NHIS, with never-smokers defined as participants who reported smoking less than 100 cigarettes in their lifetime. Smoking exposure was captured as smoking duration (the number of smoking years per participant). Smoking duration is a validated predictor of COPD and was recently noted to be more accurate and predictive of COPD than pack-years (22).
Statistical Analysis
All analyses used the sampling units, survey weights, and strata provided by the NHIS. For participant demographics (Table 1), the Clopper-Pearson method was used to obtain confidence intervals (23). Two primary logistic regression models were used: 1) crude/bivariate analysis and 2) multivariate models adjusted for age, sex, race/ethnicity, region of residence, smoking duration, community poverty, urban–rural status, census-level use of solid fuels in homes, census-level data on the percentage of inhabitants in occupations associated with lung disease, and individual socioeconomic factors. Subgroup analyses were conducted for smokers and never-smokers. Our primary analysis presents the imputed income-to-poverty ratio as a continuous variable. We performed a separate analysis that categorized the income-to-poverty ratio into historically used thresholds (>2.00, 1.00–2.00, and <1.00), as presented in the online supplement (Table E1) (24). All analyses were done using STATA 15/SE. Statistical significance was defined as a P value less than 0.05.
Table 1.
Participant Characteristics
| Characteristic | Overall | Rural |
Nonrural |
||
|---|---|---|---|---|---|
| Poor* (2.7%) | Nonpoor (12.2%) | Poor (13.7%) | Nonpoor (71.3%) | ||
| Overall poverty | 15.7 (14.7–16.7) | ||||
| Age, yr† | 58.4 (58.3–58.6) | 58.9 (58.3–59.7) | 60.2 (59.8–60.6) | 57.7 (57.3–58.0) | 58.2 (58.1–58.4) |
| Male sex | 47.4 (46.9–47.8) | 45.7 (43.6–47.8) | 47.4 (46.1–48.6) | 46.1 (45.0–47.1) | 47.7 (47.1–48.2) |
| Race/ethnicity | |||||
| White | 71.6 (70.9–72.2) | 72.9 (67.5–77.6) | 89.2 (87.1–91.0) | 38.9 (36.5–41.5) | 74.8 (74.1–75.5) |
| Black | 10.9 (10.5–11.4) | 17.3 (13.5–21.9) | 4.7 (3.5–6.2) | 28.7 (26.7–30.8) | 8.3 (7.8–8.8) |
| Hispanic | 11.7 (11.3–12.1) | 5.5 (3.8–7.8) | 3.9 (3.0–5.2) | 27.4 (25.6–29.4) | 10.2 (9.8–10.7) |
| Asian | 5.1 (4.8–5.3) | 1.5 (1.0–2.2) | 1.1 (0.6–1.9) | 3.8 (3.3–4.4) | 6.1 (5.8–6.4) |
| Region | |||||
| Northeast | 18.6 (18.1–19.3) | 5.2 (2.7–9.4) | 11.2 (7.7–16.1) | 17.3 (14.9–19.9) | 20.7 (19.6–21.9) |
| Midwest | 22.4 (21.7–23.0) | 14.9 (10.3–21.0) | 39.3 (34.2–44.8) | 18.1 (15.7–20.8) | 20.5 (19.4–21.7) |
| South | 37.1 (36.3–38.0) | 70.1 (62.8–76.6) | 36.2 (30.5–42.2) | 39.6 (36.5–42.8) | 35.6 (34.1–37.1) |
| West | 21.9 (21.2–22.3) | 9.8 (6.2–15.3) | 13.3 (10.3–16.9) | 25.1 (22.3–28.0) | 23.2 (22.2–24.3) |
| Smoking characteristics | |||||
| Ever-smokers | 43.9 (43.4–44.4) | 50.7 (47.8–53.5) | 49.5 (48.1–51.0) | 46.5 (45.1–47.8) | 42.2 (41.6–42.9) |
| Years smoked (smokers)† | 27.7 (27.5–27.9) | 30.5 (29.8–31.2) | 29.5 (28.9–30.1) | 30.2 (29.7–30.7) | 26.7 (26.4–27.0) |
| Prominent fuel type used in each census tract | |||||
| Coal | 0.1 (0.09–0.14) | 0.5 (0.1–0.9) | 0.3 (0.2–0.4) | 0.02 (0.01–0.03) | 0.09 (0.07–0.11) |
| Wood | 2.2 (2.04–2.45) | 5.6 (3.3–7.8) | 7.3 (6.2–8.5) | 0.6 (0.3–0.9) | 1.60 (1.4–1.7) |
| Insurance status | |||||
| Private insurance | 49.3 (48.6–49.9) | 34.5 (31.3–37.8) | 41.9 (40.0–43.8) | 34.4 (33.0–35.7) | 53.9 (53.2–54.7) |
| No insurance | 9.85 (9.55–10.2) | 13.3 (11.7–15.1) | 9.84 (9.00–10.7) | 17.9 (17.0–18.9) | 8.17 (7.84–8.53) |
| Medicare | 24.0 (25.5–24.5) | 28.2 (25.5–30.1) | 31.1 (30.0–32.3) | 21.4 (20.3–22.5) | 24.5 (23.9–25.1) |
| Medicaid | 6.86 (6.59–7.14) | 14.5 (12.1–18.5) | 7.04 (6.24–7.94) | 15.8 (14.8–16.9) | 4.81 (4.51–5.12) |
| Education | |||||
| Less than high school | 13.9 (13.5–14.3) | 27.1 (24.5–30.0) | 15.7 (14.6–16.9) | 28.5 (27.2–29.8) | 10.3 (9.79–10.7) |
| Home ownership status | |||||
| Owns home | 76.2 (75.6–76.8) | 73.0 (69.3–76.4) | 82.8 (81.5–84.0) | 54.8 (53.0–56.6) | 79.3 (78.5–80.0) |
| COPD prevalence | 8.4 (8.1–8.7) | 15.7 (14.0–17.7) | 12.0 (11.1–13.0) | 10.1 (9.4–10.9) | 7.1 (6.9–7.5) |
Definition of abbreviation: COPD = chronic obstructive pulmonary disease.
Data are given as percentages (95% confidence intervals) unless otherwise indicated.
“Poor” was defined as ≥20% of households living below the poverty line.
Means (95% confidence intervals).
Results
Population Characteristics
Data from a total of 90,334 adults above the age of 40, collected between 2012 and 2015, were analyzed (Table 1). In our dataset, 14.9% of the participants resided in rural counties, 15.7% resided in poor census tracts, and 43.9% were current or former smokers. Among smokers, the mean smoking duration was 27.7 years. The estimated national prevalence of COPD, as estimated from our sample, was 8.4% (8.1–8.7%), with a prevalence of 4.3% (4.1–4.6%) among never-smokers and 13.5% (13.0–14.0%) among current or former smokers; 23.2% of the participants with COPD were never-smokers.
Association of Rural Residence and Indicators of Poverty with COPD Prevalence
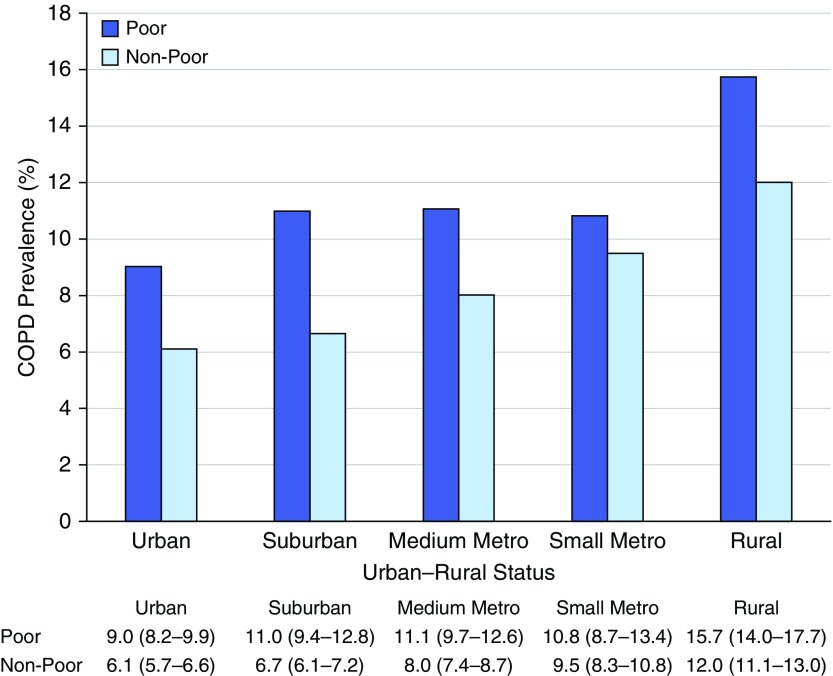
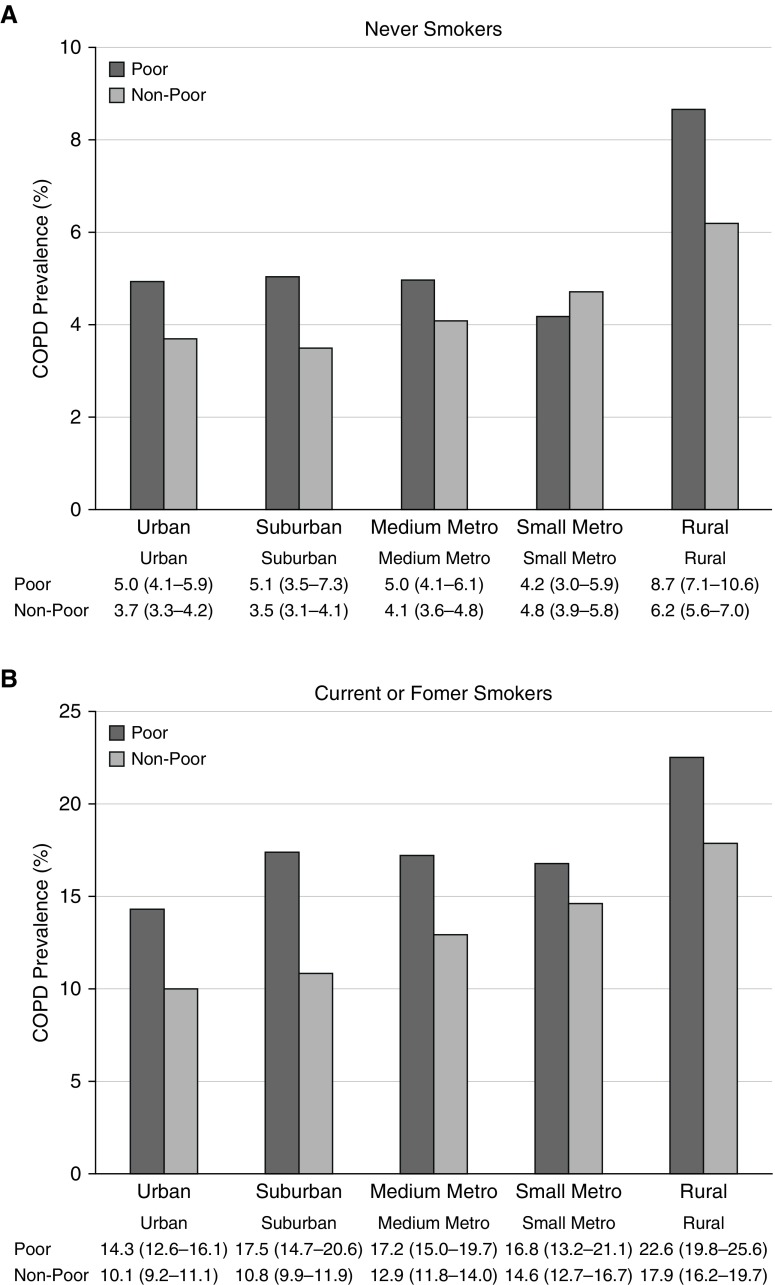
The prevalence of COPD varied across regions. Overall, we found the highest prevalence of COPD in rural regions, at 12.7% (11.8–13.7%), with a higher estimated prevalence in rural, poor communities. Specifically, in rural, poor communities the prevalence was 15.7% (14.0–17.7%), compared with 12.0% (11.1–13.0%) in rural, nonpoor communities. The lowest prevalence was seen in urban, nonpoor communities, at 6.1% (5.7–6.6%) (Figure 1). This pattern was consistent for the subgroup of never-smokers, with an overall COPD prevalence of 4.4% (4.1–4.6%), compared with 8.7% (7.1–10.6%) in rural, poor communities (Figure 2).
Figure 1.
Prevalence of chronic obstructive pulmonary disease (COPD) by urban–rural status. This figure demonstrates the estimated national prevalence of COPD by poverty and urban–rural status. Prevalence is displayed below, with 95% confidence intervals. “Poor community” was defined as a census tract with ≥20% of households living below the poverty line.
Figure 2.
Prevalence of chronic obstructive pulmonary disease (COPD) by urban–rural status among (A) never-smokers and (B) current or former smokers. This figure demonstrates the estimated national prevalence of COPD by poverty and urban–rural status for both smokers and never-smokers. Prevalence is displayed below, with 95% confidence intervals. Note that the scales differ between A and B. “Poor community” was defined as a census tract with ≥20% of households living below the poverty line.
Living in a rural tract remained predictive for COPD prevalence even in adjusted models that controlled for region of residence, age, sex, race, smoking status, indicators of household wealth, education, community poverty, health insurance, census-level occupational distribution, and solid fuel use (odds ratio [OR], 1.23; P < 0.001) (Table 2). This association was present among never-smokers (OR, 1.34; P < 0.001) and current or former smokers (OR, 1.19; P = 0.031) (Table 3).
Table 2.
Individual- and Community-Level Predictors of Chronic Obstructive Pulmonary Disease
| Crude Model |
Adjusted Model* |
|||||
|---|---|---|---|---|---|---|
| Odds Ratio | 95% CI | P Value | Odds Ratio | 95% CI | P Value | |
| Census tract characteristics | ||||||
| Urban–rural status | ||||||
| Urban | Reference |
|||||
| Suburban | 1.04 | 0.93–1.16 | 0.51 | 0.97 | 0.87–1.07 | 0.51 |
| Medium metro | 1.30 | 1.17–1.44 | <0.001 | 1.02 | 0.92–1.14 | 0.69 |
| Small metro | 1.48 | 1.28–1.44 | <0.001 | 1.05 | 0.91–1.21 | 0.49 |
| Rural | 2.01 | 1.80–2.23 | <0.001 | 1.23 | 1.09–1.40 | <0.001 |
| Census-level poverty | ||||||
| Community poverty | 1.46 | 1.35–1.57 | <0.001 | 1.12 | 1.03–1.22 | 0.012 |
| Regions | ||||||
| Northeast | Reference |
|||||
| Midwest | 1.35 | 1.21–1.50 | <0.001 | 1.20 | 1.06–1.36 | 0.003 |
| South | 1.32 | 1.19–1.47 | <0.001 | 1.27 | 1.14–1.41 | <0.001 |
| West | 0.87 | 0.78–0.98 | 0.023 | 1.01 | 0.89–1.14 | 0.91 |
| Census tract fuel use† | ||||||
| Wood | 1.01 | 1.01–1.02 | <0.001 | 1.00 | 0.99–1.00 | 0.23 |
| Coal | 1.07 | 1.04–1.11 | <0.001 | 1.03 | 0.98–1.08 | 0.28 |
| Occupation category‡ | ||||||
| Agriculture, mining | 1.02 | 1.01–1.03 | 0.002 | 1.00 | 1.00–1.01 | 0.64 |
| Construction | 1.02 | 1.01–1.03 | 0.001 | 1.00 | 0.99–1.01 | 0.94 |
| Manufacturing | 1.02 | 1.01–1.02 | <0.001 | 1.00 | 1.00–1.01 | 0.131 |
| Individual characteristics | ||||||
| Demographics | ||||||
| Age, per 10-yr increase | 1.32 | 1.29–1.35 | <0.001 | 1.04 | 1.00–1.07 | 0.039 |
| Smoking duration | 1.04 | 1.04–1.05 | <0.001 | 1.04 | 1.03–1.04 | <0.001 |
| Race | ||||||
| White | Reference |
|||||
| Black | 0.87 | 0.79–0.95 | 0.002 | 0.68 | 0.61–0.75 | <0.001 |
| Asian | 0.29 | 0.24–0.36 | <0.001 | 0.44 | 0.35–0.54 | <0.001 |
| Hispanic | 0.47 | 0.42–0.53 | 0.017 | 0.49 | 0.43–0.57 | <0.001 |
| Insurance status | ||||||
| Private insurance | Reference |
|||||
| No insurance | 1.62 | 1.42–1.84 | <0.001 | 1.07 | 0.92–1.23 | 0.38 |
| Medicare | 3.14 | 2.89–3.41 | <0.001 | 1.83 | 1.65–2.03 | <0.001 |
| Medicaid | 5.06 | 4.59–5.58 | <0.001 | 2.76 | 2.44–3.11 | <0.001 |
| Education | ||||||
| College and beyond | Reference |
|||||
| High school graduate | 1.62 | 1.49–1.75 | <0.001 | 1.04 | 0.96–1.14 | 0.33 |
| Less than high school | 2.13 | 1.96–2.31 | <0.001 | 1.16 | 1.05–1.29 | 0.003 |
| Home ownership status | ||||||
| Owns home | Reference |
|||||
| Other arrangement (rented) | 1.54 | 1.43–1.65 | <0.001 | 1.18 | 1.09–1.27 | <0.001 |
| Household poverty§ | 1.20 | 1.18–1.22 | <0.001 | 1.08 | 1.06–1.10 | <0.001 |
Definition of abbreviation: CI = confidence interval.
Bold values are statistically significant.
Adjusted for urban–rural status, community wealth, region, census-level occupational distribution, census-level fuel use, race, age, sex, smoking duration, household poverty, home ownership, education, and insurance type.
Per 1% increase in census tract residents using this fuel type as their primary source of heating.
Per 1% increase in census tract residents employed in this occupation.
Per one-unit decrease in household income-to-poverty ratio.
Table 3.
Predictors of Chronic Obstructive Pulmonary Disease among Current or Former Smokers versus Never-Smokers*
| Current or Former Smokers |
Never-Smokers |
|||||
|---|---|---|---|---|---|---|
| Odds Ratio | 95% CI | P Value | Odds Ratio | 95% CI | P Value | |
| Urban–rural status | ||||||
| Urban | Reference |
|||||
| Suburban | 0.96 | 0.85–1.10 | 0.61 | 0.96 | 0.80–1.15 | 0.68 |
| Medium metro | 1.03 | 0.90–1.18 | 0.64 | 1.01 | 0.84–1.20 | 0.94 |
| Small metro | 1.06 | 0.90–1.25 | 0.49 | 1.05 | 0.84–1.32 | 0.66 |
| Rural | 1.19 | 1.02–1.39 | 0.031 | 1.34 | 1.09–1.63 | <0.001 |
| Census-level poverty | ||||||
| Community poverty | 1.13 | 1.02–1.26 | 0.028 | 1.10 | 0.95–1.29 | 0.20 |
| Regions | ||||||
| Northeast | Reference |
|||||
| Midwest | 1.14 | 0.98–1.32 | 0.079 | 1.33 | 1.08–1.64 | 0.007 |
| South | 1.20 | 1.06–1.37 | 0.005 | 1.41 | 1.16–1.72 | 0.001 |
| West | 0.97 | 0.84–1.12 | 0.65 | 1.09 | 0.88–1.35 | 0.41 |
| Community fuel use† | ||||||
| Wood | 0.99 | 0.99–1.00 | 0.23 | 1.00 | 0.99–1.01 | 0.70 |
| Coal | 1.00 | 0.93–1.06 | 0.93 | 1.09 | 1.05–1.13 | <0.001 |
| Household poverty‡ | 1.07 | 1.05–1.10 | <0.001 | 1.08 | 1.05–1.11 | <0.001 |
Definition of abbreviation: CI = confidence interval.
Bold values are statistically significant.
Adjusted for urban–rural status, community wealth, region, census-level occupational distribution, census-level fuel use, race, age, sex, home ownership, education, and insurance type.
Per 1% increase in census tract residents using this fuel type as their primary source of heating.
Per one-unit decrease in household income-to-poverty ratio.
Both individual socioeconomic status and community poverty were associated with COPD prevalence. At the individual level, a one-unit decrease in the household income-to-poverty ratio was associated with an 8% increase in the odds of having COPD (P < 0.001). Other markers of individual wealth, including a college education and home ownership, were also independently protective against COPD. Community poverty was independently associated with COPD (OR, 1.12; P = 0.012) even after measures of individual household wealth were taken into account (Table 2).
Association of Region of Residence and Community-Level Exposures with COPD Prevalence
Residence in the South and Midwest were associated with increased COPD prevalence in our multivariate models (ORs, 1.20 [P = 0.003] and 1.27 [P < 0.001], respectively). This relationship persisted for both current or former smokers and never-smokers.
Sold fuel use was reported at the census tract level. Use of solid fuels for heating appeared to be more common in rural census tracts: 0.5% (0.1–0.9%) used coal as the primary heating source in rural, poor census tracts, as opposed to 0.02% (0.01–0.03%) in nonrural, poor census tracts. In rural, poor tracts, 5.6% (3.3–7.8%) used wood as the primary heating source, and 0.6% (0.3–0.9%) used wood as the primary heating source in nonrural, poor tracts. In the analysis of never-smokers, there was a significant association for coal combustion in multivariate models (OR, 1.09; P < 0.001), such that a 1% increase in the number of homes using coal as the primary heating source could be linked to a 9% increase in the odds of having COPD, for never-smokers in that census tract. This relationship was unique to never-smokers and was not significant among the overall population or in our model of current or former smokers.
In our crude models, increases in census-level employment in agriculture, construction, or mining occupations were associated with an increased odds of COPD development, although the effect size was relatively small. None of these relationships were significant in our adjusted model (Table E1).
Individual Factors
Other individual demographics, including age, smoking duration, and race, were associated with a diagnosis of COPD. Black and Hispanic participants were less likely to report a diagnosis of COPD (ORs, 0.68 [P < 0.001] and 0.49 [P < 0.001], respectively). Participants with Medicaid insurance (OR, 2.76; P < 0.001) and Medicare (OR, 1.83; P < 0.001) were also more likely to carry a diagnosis of COPD than those with private insurance.
Discussion
Our study shows that the greatest burden of COPD in the United States is found in rural areas, with the prevalence of COPD in rural, poor communities being nearly double that in the general population. Community and household indicators of poverty were both associated with COPD prevalence. These associations were demonstrated for never-smokers with COPD, as well as current and former smokers. The results of this study demonstrate an urban–rural disparity that is compounded by several socioeconomic factors.
These findings address the research priorities outlined in the COPD National Action Plan and extend recent reports of urban–rural COPD disparities to include an evaluation of multiple risk factors at the individual, household, and community levels. Our study demonstrates an association between living in a rural environment and the development of COPD, which persists even when controlling for socioeconomic factors, and exposures that are more common in rural areas (heating with solid fuels, as well as agricultural and mining occupations) (25, 26). Poverty and rural residence represent important risk factors that jointly increase the prevalence of COPD. The combined effects of poverty and shifting demographics may partially contribute to the urban–rural disparity characterized in this study. A previous publication described the “suburbanization of poverty,” noting that the greatest growth in poverty has occurred in suburban and rural areas (27).
COPD is also a disease that represents exposure to risk factors over a lifetime, and these risk factors are often mediated by poverty and geographic exposures. Low-income communities historically have had a higher prevalence of people exposed to indoor and outdoor air pollution, poor nutritional status, low birth weight, and childhood respiratory infections—all factors that may be associated with an increased prevalence of COPD and poor lung function (28–31). Lack of access to healthcare and health education is also likely to contribute to the increased prevalence of COPD in rural and poor areas (32). Our findings suggested that insurance status was associated with COPD prevalence, but inferences are limited by the cross-sectional nature of the analysis and the fact that insurance status is a complex and imperfect surrogate for access to care, as it also represents age, socioeconomic status, and other factors.
Never-smokers with COPD are another important population that is increasing but remains understudied in the United States. Our study was able to evaluate individual and community-wide risk factors for COPD in a nationally representative population of never-smokers. Approximately 23% of our participants with COPD were never-smokers, similar to the 20% that has been estimated in prior studies (33). In our analysis, many of the risk factors associated with COPD prevalence were similar between never-smokers and participants with a smoking history, with the notable exception that neighborhood-level solid fuel use for heating was associated with increased COPD prevalence among never-smokers. International studies have suggested that solid fuel combustion may be associated with an increased prevalence of COPD in low- and middle-income countries, with minimal exposure to tobacco smoke, but some notable studies have produced conflicting results (5, 34). Few studies to date have investigated solid fuel use and COPD development in the United States, and the studies that did include sites in the United States were limited in their sample of the U.S. population and did not focus solely on never-smokers (35). A Canadian study in a population more comparable to ours suggested that the use of solid fuels was a risk factor for COPD among women without a smoking history, but not for ever-smokers (36). Similarly, in our study, although it was not a significant factor for the population as a whole, the use of coal for heating was strongly associated with a diagnosis of COPD among never-smokers. It is possible that solid fuel use has a detrimental effect on the population as a whole, but the impact of household pollution from solid fuel use might be more apparent in never-smokers, where exposure to tobacco is not a competing risk factor. Although the overall use of solid fuel was low, our dataset suggests a disproportionate use of coal and wood fuel for heating among the rural groups. With these results, we now demonstrate a risk factor for nonsmokers in the United States that is more common in rural areas (37).
Previous studies have also suggested that the urban–rural disparities observed for chronic disease in the United States may be related not only to smoking and indoor air pollutants but also to occupational and agricultural exposures in rural communities (38). COPD prevalence has been linked to both crop farming and coal mining, both of which are more common in rural areas (39). However, our study did not show a significant association between increases in agricultural or mining occupations at the census level and COPD prevalence. This analysis was further limited because the ACS groups multiple occupation groups together (including agriculture, mining, and forestry), which constrained our ability to evaluate these exposures individually. Future studies should focus on environmental factors that contribute to the higher prevalence of COPD in rural communities, looking at occupation and household exposures at the individual level rather than the census level to better delineate these effects (40).
Race also proved to be a significant factor in our analysis. Minority groups (black, Hispanic, and Asian) were less likely to report a diagnosis of COPD in our analysis. With this dataset, we were not able to determine whether this was related to susceptibility factors or disparities in screening for COPD among different racial groups. Previous studies looking at the association between racial disparities and COPD prevalence have yielded mixed results (41, 42). African Americans have been described to be at increased risk for early-onset COPD; however, our study focused on older adults and may not have captured this effect (43).
Limitations
There are limitations to our study. One major limitation is that the NHIS relies on self-reported diagnoses of COPD. Historically, COPD has been underreported, with estimates based on spirometry data indicating that COPD prevalence may be double that suggested by self-reported data (44). The underreporting of COPD may in fact underestimate the disparities reported in our analyses. The problem of self-reporting is also not unique to our study and is a limitation of large-scale estimates of COPD prevalence. We did perform multiple sensitivity analyses to limit the risk of misclassification, and in our alternative definitions for COPD the relationships observed between rural residence and COPD persisted (Table E2). A limitation to our model of nonsmokers was a lack of information about second-hand smoke exposure, and a potential for underreporting of smoking exposure among participants. Other household air pollutants and exposures, such as coal use for heating, were also reported at the census tract level rather than for individual participants with household measurements. These data were also cross-sectional, and we were unable to measure other potential risk factors such as early-childhood infections, geographic mobility, changes in access to care, and duration of residence in rural tracts over time. We countered many of these limitations by having robust data from the NHIS that allowed us to measure individual poverty and markers of socioeconomic status.
Our analysis has several strengths, including the NHIS’s careful design, which provides a robust representation of the entire U.S. population. Our dataset allowed us to capture individuals living in rural parts of the United States, who have remained understudied in clinical research and environmental monitoring campaigns (45, 46). The combination of NHIS and Census data allowed us to analyze both community-wide and individual factors that contribute to COPD prevalence nationwide. The ACS additionally allowed us to uniquely link robust data on heating practices and occupations to health outcomes. Our use of the NCHS Urban Rural Classification of Counties was an additional strength and gave us the ability to move beyond a dichotomized classification of urban versus rural, which previous studies relied on, and distinctly consider suburban and small and medium metropolitan areas (9). Finally, the large-scale nature of this analysis allowed us to investigate the association between COPD and rural residency and poverty throughout the United States.
Conclusions
In a nationally representative sample of the U.S. population, living in a rural area, community poverty, and indicators of household wealth were significant risk factors associated with higher COPD prevalence. Among individuals with COPD who reported never smoking, living in a community with coal use as a primary heating source was an additional risk factor, suggesting that indoor air pollution is a risk factor that is especially relevant for this population. Future disparities research should focus on designing local cohorts to better understand the unique risk factors within rural and poor populations that contribute to the development of COPD, including environmental monitoring to capture indoor air pollution (such as solid fuel combustion). These research efforts will be essential for developing strategies to reduce the burden of COPD and eliminate disparities in disadvantaged rural populations between both ever- and never-smokers. Although these efforts will not reduce the importance of tobacco cessation initiatives, the results they provide can be used to develop policies targeted at decreasing the burden of COPD nationwide.
Supplementary Material
Footnotes
Supported by grants from the National Institute on Minority Health and Health Disparities/NIH (P50MD010431), National Institute of Environmental Health Sciences/NIH (F32 ES029786-01 and R21ES025840), Environmental Protection Agency (R836150), and NHLBI/NIH (5T32HL007534).
Author Contributions: C.A.K., E.C.M., and R.D.P. contributed to study design and data acquisition and analysis. L.M.P. and N.N.H. contributed to authorship of the manuscript and interpretation of results. M.C.M. contributed to study design, data analysis, interpretation of results, and authorship of the manuscript. S.R. contributed to study design, data analysis, and interpretation of results, and drafted the manuscript.
This article has an online supplement, which is accessible from this issue’s table of contents at www.atsjournals.org.
Originally Published in Press as DOI: 10.1164/rccm.201807-1374OC on November 2, 2018
Author disclosures are available with the text of this article at www.atsjournals.org.
References
- 1.Croft JB, Wheaton AG, Liu Y, Xu F, Lu H, Matthews KA, et al. Urban-rural county and state differences in chronic obstructive pulmonary disease—United States, 2015. MMWR Morb Mortal Wkly Rep. 2018;67:205–211. doi: 10.15585/mmwr.mm6707a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Menezes AMB, Victora CG, Perez-Padilla R. The PLATINO project: methodology of a multicenter prevalence survey of chronic obstructive pulmonary disease in major Latin American cities. BMC Med Res Methodol. 2004;7:1–7. doi: 10.1186/1471-2288-4-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Burney P, Jithoo A, Kato B, Janson C, Mannino D, Nizankowska-Mogilnicka E, et al. Burden of Obstructive Lung Disease (BOLD) Study. Chronic obstructive pulmonary disease mortality and prevalence: the associations with smoking and poverty—a BOLD analysis. Thorax. 2014;69:465–473. doi: 10.1136/thoraxjnl-2013-204460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kurmi OP, Semple S, Simkhada P, Smith WC, Ayres JG. COPD and chronic bronchitis risk of indoor air pollution from solid fuel: a systematic review and meta-analysis. Thorax. 2010;65:221–228. doi: 10.1136/thx.2009.124644. [DOI] [PubMed] [Google Scholar]
- 5.Siddharthan T, Grigsby MR, Goodman D, Chowdhury M, Rubinstein A, Irazola V, et al. Association between household air pollution exposure and chronic obstructive pulmonary disease outcomes in 13 low- and middle-income country settings Am J Respir Crit Care Med 2018197611–620.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Po JYT, FitzGerald JM, Carlsten C. Respiratory disease associated with solid biomass fuel exposure in rural women and children: systematic review and meta-analysis. Thorax. 2011;66:232–239. doi: 10.1136/thx.2010.147884. [DOI] [PubMed] [Google Scholar]
- 7.Peña VS, Miravitlles M, Gabriel R, Jiménez-Ruiz CA, Villasante C, Masa JF, et al. Geographic variations in prevalence and underdiagnosis of COPD: results of the IBERPOC multicentre epidemiological study. Chest. 2000;118:981–989. doi: 10.1378/chest.118.4.981. [DOI] [PubMed] [Google Scholar]
- 8.Salvi SS, Barnes PJ. Chronic obstructive pulmonary disease in non-smokers. Lancet. 2009;374:733–743. doi: 10.1016/S0140-6736(09)61303-9. [DOI] [PubMed] [Google Scholar]
- 9.Burkes RM, Gassett AJ, Ceppe AS, Anderson W, O’Neal WK, Woodruff PG, et al. SPIROMICS Investigators. Rural residence and COPD exacerbations: analysis of the SPIROMICS cohort. Ann Am Thorac Soc. [online ahead of print] 27 Mar 2018; DOI: 10.1513/AnnalsATS.201710-837OC. [Google Scholar]
- 10.Mushtaq A. COPD and rural health in the USA. Lancet Respir Med. 2018;6:330–331. doi: 10.1016/S2213-2600(18)30142-5. [DOI] [PubMed] [Google Scholar]
- 11.Kiley JP, Gibbons GH. COPD national action plan: addressing a public health need together. Chest. 2017;152:698–699. doi: 10.1016/j.chest.2017.08.1155. [DOI] [PubMed] [Google Scholar]
- 12.Jackson BE, Coultas DB, Suzuki S, Singh KP, Bae S. Rural-urban disparities in quality of life among patients with COPD. J Rural Health. 2013;29:s62–s69. doi: 10.1111/jrh.12005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Buist AS, McBurnie MA, Vollmer WM, Gillespie S, Burney P, Mannino DM, et al. BOLD Collaborative Research Group. International variation in the prevalence of COPD (the BOLD Study): a population-based prevalence study. Lancet. 2007;370:741–750. doi: 10.1016/S0140-6736(07)61377-4. [DOI] [PubMed] [Google Scholar]
- 14.Buist AS, Vollmer WM, Sullivan SD, Weiss KB, Lee TA, Menezes AMB, et al. The burden of obstructive lung disease initiative (BOLD): rationale and design. COPD. 2005;2:277–283. [PubMed] [Google Scholar]
- 15.Lamprecht B, Vanfleteren LE, Studnicka M, Allison M, McBurnie MA, Vollmer WM, et al. BOLD Collaborative Research Group. Sex-related differences in respiratory symptoms: results from the BOLD study. Eur Respir J. 2013;42:858–860. doi: 10.1183/09031936.00047613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Raju S, Corinne AK, Matsui EC, Drummond MB, Hansel NN, Wise RA, et al. The impact of poverty and rural residence on chronic obstructive pulmonary disease (COPD) prevalence: a nationwide analysis [abstract] Am J Respir Crit Care Med. 2015;191:A3904. [Google Scholar]
- 17.Ingram DD, Franco SJ. 2013 NCHS urban-rural classification scheme for counties. Vital Health Stat 2. 2014;(166):1–73. [PubMed] [Google Scholar]
- 18.Ryu JY, Sunwoo YE, Lee SY, Lee CK, Kim JH, Lee JT, et al. Chronic obstructive pulmonary disease (COPD) and vapors, gases, dusts, or fumes (VGDF): a meta-analysis. COPD. 2015;12:374–380. doi: 10.3109/15412555.2014.949000. [DOI] [PubMed] [Google Scholar]
- 19.Keet CA, McCormack MC, Pollack CE, Peng RD, McGowan E, Matsui EC. Neighborhood poverty, urban residence, race/ethnicity, and asthma: Rethinking the inner-city asthma epidemic. J Allergy Clin Immunol. 2015;135:655–662. doi: 10.1016/j.jaci.2014.11.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Schenker N, Raghunathan TE, Chiu P-L, Makuc DM, Zhang G, Cohen AJ. Multiple imputation of missing income data in the National Health Interview Survey. J Am Stat Assoc. 2006;101:924–933. [Google Scholar]
- 21.Rubin DB. Multiple imputation for nonresponse in surveys. J Market Res. 1989;137(4) [Google Scholar]
- 22.Bhatt SP, Kim Y, Harrington KF, Hokanson JE, Lutz SM, Cho MH, et al. Smoking duration alone provides stronger risk estimates of chronic obstructive pulmonary disease than pack-years. Thorax. 2018;73:414–421. doi: 10.1136/thoraxjnl-2017-210722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Puza B, O’Neill T. Generalised Clopper-Pearson confidence intervals for the binomial proportion. J Stat Comput Simul. 2006;76:489–508. [Google Scholar]
- 24.Pleis JR, Cohen RA. Impact of income bracketing on poverty measures used in the National Health Interview Survey’s Early Release Program: preliminary data from the 2007 NHIS. 2007 Available from: https://www.cdc.gov/nchs/data/nhis/income.pdf.
- 25.Rogalsky DK, Mendola P, Metts TA, Martin WJ., II Estimating the number of low-income americans exposed to household air pollution from burning solid fuels. Environ Health Perspect. 2014;122:806–810. doi: 10.1289/ehp.1306709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Doney BC, Henneberger PK, Humann MJ, Liang X, Kelly KM, Cox-Ganser JM. Occupational exposure to vapor-gas, dust, and fumes in a cohort of rural adults in Iowa compared with a cohort of urban adults. MMWR Surveill Summ. 2017;66:1–5. doi: 10.15585/mmwr.ss6621a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Howell AJ, Timberlake JM. Racial and ethnic trends in the suburbanization of poverty in US metropolitan areas, 1980–2010. J Urban Aff. 2014;36:79–98. [Google Scholar]
- 28.Shaheen SO, Barker DJP, Holgate ST. Do lower respiratory tract infections in early childhood cause chronic obstructive pulmonary disease? Am J Respir Crit Care Med. 1995;151:1649–1651. doi: 10.1164/ajrccm/151.5_Pt_1.1649. discussion 1651–1652. [DOI] [PubMed] [Google Scholar]
- 29.Edwards CA, Osman LM, Godden DJ, Campbell DM, Douglas JG. Relationship between birth weight and adult lung function: controlling for maternal factors. Thorax. 2003;58:1061–1065. doi: 10.1136/thorax.58.12.1061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Misra P, Srivastava R, Krishnan A, Sreenivaas V, Pandav CS. Indoor air pollution-related acute lower respiratory infections and low birthweight: a systematic review. J Trop Pediatr. 2012;58:457–466. doi: 10.1093/tropej/fms017. [DOI] [PubMed] [Google Scholar]
- 31.da Silva LFF, Saldiva SRDM, Saldiva PHN, Dolhnikoff M Bandeira Científica Project. Impaired lung function in individuals chronically exposed to biomass combustion. Environ Res. 2012;112:111–117. doi: 10.1016/j.envres.2011.10.012. [DOI] [PubMed] [Google Scholar]
- 32.Singh GK, Siahpush M. Widening rural-urban disparities in all-cause mortality and mortality from major causes of death in the USA, 1969-2009. J Urban Health. 2014;91:272–292. doi: 10.1007/s11524-013-9847-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lamprecht B, McBurnie MA, Vollmer WM, Gudmundsson G, Welte T, Nizankowska-Mogilnicka E, et al. OLD Collaborative Research Group. COPD in never smokers; results from the population-based burden of obstructive lung disease study. Chest. 2011;139:752–763. doi: 10.1378/chest.10-1253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Burney P, Kato B, Janson C, Mannino D, Studnicka M, Tan W, et al. Burden of Obstructive Lung Disease (BOLD) Study. Chronic obstructive pulmonary disease mortality and prevalence: the associations with smoking and poverty: a BOLD analysis—authors’ reply. Thorax. 2014;69:869–870. doi: 10.1136/thoraxjnl-2014-205474. [DOI] [PubMed] [Google Scholar]
- 35.Amaral AFS, Patel J, Kato BS, Obaseki DO, Lawin H, Tan WC, et al. BOLD Collaborative Research Group. Airflow obstruction and use of solid fuels for cooking or heating: BOLD results Am J Respir Crit Care Med [online ahead of print] 12 Sep 2017; DOI: 10.1164/rccm.201701-0205OC [DOI] [PMC free article] [PubMed]
- 36.Tan WC, Sin DD, Bourbeau J, Hernandez P, Chapman KR, Cowie R, et al. CanCOLD Collaborative Research Group. Characteristics of COPD in never-smokers and ever-smokers in the general population: results from the CanCOLD study. Thorax. 2015;70:822–829. doi: 10.1136/thoraxjnl-2015-206938. [DOI] [PubMed] [Google Scholar]
- 37.Hu G, Zhou Y, Tian J, Yao W, Li J, Li B, et al. Risk of COPD from exposure to biomass smoke: a metaanalysis. Chest. 2010;138:20–31. doi: 10.1378/chest.08-2114. [DOI] [PubMed] [Google Scholar]
- 38.Graber JM, Stayner LT, Cohen RA, Conroy LM, Attfield MD. Respiratory disease mortality among US coal miners; results after 37 years of follow-up. Occup Environ Med. 2014;71:30–39. doi: 10.1136/oemed-2013-101597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Eduard W, Pearce N, Douwes J. Chronic bronchitis, COPD, and lung function in farmers: the role of biological agents. Chest. 2009;136:716–725. doi: 10.1378/chest.08-2192. [DOI] [PubMed] [Google Scholar]
- 40.Abrams TE, Vaughan-Sarrazin M, Fan VS, Kaboli PJ. Geographic isolation and the risk for chronic obstructive pulmonary disease-related mortality: a cohort study. Ann Intern Med. 2011;155:80–86. doi: 10.7326/0003-4819-155-2-201107190-00003. [DOI] [PubMed] [Google Scholar]
- 41.Fuller-Thomson E, Chisholm RS, Brennenstuhl S. COPD in a population-based sample of never-smokers: interactions among sex, gender, and race. Int J Chronic Dis. 2016;2016:5862026. doi: 10.1155/2016/5862026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Martin A, Badrick E, Mathur R, Hull S. Effect of ethnicity on the prevalence, severity, and management of COPD in general practice. Br J Gen Pract. 2012;62:e76–e81. doi: 10.3399/bjgp12X625120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Foreman MG, Zhang L, Murphy J, Hansel NN, Make B, Hokanson JE, et al. COPDGene Investigators. Early-onset COPD is associated with female gender, maternal factors, and African American Race in the COPDGene study. Am J Respir Crit Care Med. 2011;184:414–420. doi: 10.1164/rccm.201011-1928OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Mannino DM, Buist AS. Global burden of COPD: risk factors, prevalence, and future trends. Lancet. 2007;370:765–773. doi: 10.1016/S0140-6736(07)61380-4. [DOI] [PubMed] [Google Scholar]
- 45.Miranda ML, Edwards SE, Keating MH, Paul CJ. Making the environmental justice grade: the relative burden of air pollution exposure in the United States. Int J Environ Res Public Health. 2011;8:1755–1771. doi: 10.3390/ijerph8061755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Behringer B, Friedell GH. Appalachia: where place matters in health. Prev Chronic Dis. 2006;3:A113. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.