Abstract
Objective
To assess key aspects of transportation and storage of biological therapies (BTs) on the part of the patients, from the time they collect them from the pharmacy up until the moment of administration.
Methods
This was a cross-sectional study in the form of a survey completed by outpatients older than 18 years who were administered BTs. The survey was carried out by the authors between August 2016 and January 2017.
Results
A total of 83 outpatients were interviewed (mean age, 53; standard deviation, 15; 76% female). Sixty percent had rheumatoid arthritis, 24% had psoriatic arthritis, and 16% sustained other rheumatic and inflammatory diseases. Twenty percent had not been informed of the importance of proper refrigeration when they were first prescribed BTs; 77% had acquired the medication at least 7 days before administration; 28% had misplaced the drug in the fridge (65% of them in the freezer); 90% was unaware of the temperature range at which the BT should be kept in the fridge, and only one (1%) of them had once used a thermometer to find out the fridge temperature. Fifty-three percent had suffered frequent power outages the previous summer, 22% had experienced blackouts longer than 48 hours; 37% had taken the BT to another house to avoid wasting it, and four (5%) patients had disposed of the drug due to a prolonged power outage.
Conclusion
Upon prescribing BTs, it is imperative that physicians brief patients on the relevance of suitable transportation and storage methods, and a treatment failure should prompt a thorough assessment of transportation and storage conditions.
Keywords: Transportation, storage, biological therapies
Introduction
To ensure the efficacy of thermolabile drugs, it is the responsibility of manufacturers to indicate the temperature range at which to preserve these drugs in the patient information leaflets (PILs) (1).
The biological therapies (BTs) prescribed in rheumatology are usually costly drugs employed by numerous health care facilities owing to their substantial efficacy in the treatment of rheumatoid arthritis (RA) and other systemic inflammatory disorders, not only by mitigating their symptoms, but also by protecting the patients’ functional status and quality of life, and by halting disease progression (2).
According to the information currently available in the PILs of BTs administered in the field of rheumatology in Argentina (3–10), these drugs require refrigeration at 2 to 8°C; it is essential to avoid exposure to extreme heat and cold; and either the treating physician or the manufacturer should be contacted if the drug is discolored, looks cloudy, or contains particles.
To preclude the alteration of BTs properties, manufacturers, distributors, and pharmacists are bound by law to adhere to standard operating procedures, follow them to the letter, and abide by all the applicable laws with regard to transportation and storage (11).
However, this chain of responsibility has a weak link, namely, when patients or their relatives pick up the drugs from the pharmacist’s. From that moment on, it is vital to implement additional safety measures, sustain them over time, and carry them out accurately to maintain the product stability and prevent treatment efficacy being compromised.
Therefore, the objective of this study was to analyze key aspects of transportation and storage of BTs from the very moment the patient leaves the pharmacy up until they are administered.
Methods
A survey was conducted among outpatients who either were treated in the center or attended the center for the administration of a BT.
Inclusion criteria encompassed patients of over 18 years of age who were using a BT (at least one dose over the last 12 months), and that the PIL contained the statement “must be refrigerated at 2 to 8°C.”
At the time of the survey, the center provided neither a systematic training program for patients nor leaflets about the right way of transporting and storing BTs.
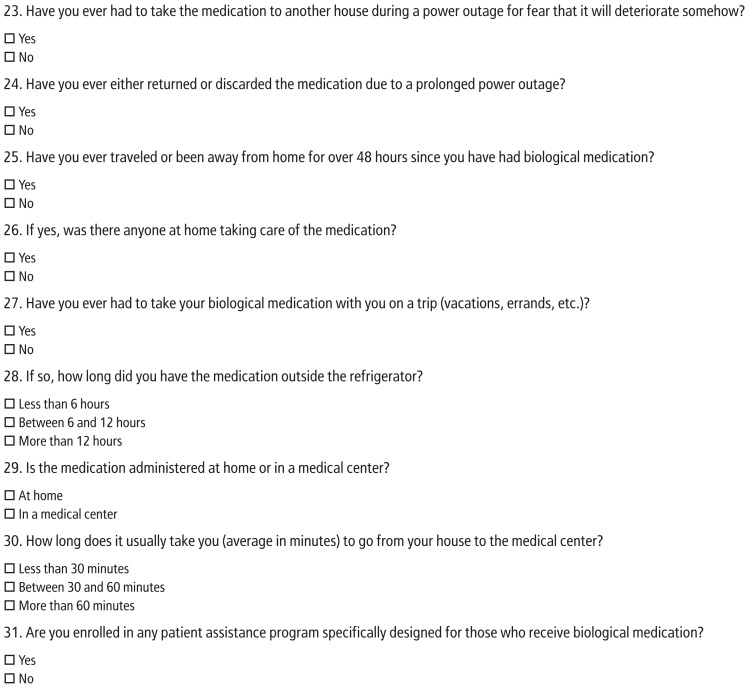
The survey comprised 31 questions about the transportation and storage of BTs from the time of collection from the pharmacy up until the moment they were administered. The questionnaire was designed by the authors and consisted of both multiple-choice and two-point close-ended questions. The original Spanish survey was translated into English and is herein submitted as supplementary material (Appendix 1).
Each survey was conducted by the authors during interviews with the patients when they visited the center. The survey was carried out between August 2016 and January 2017. The study was granted approval by the Bioethics Committee, and every patient signed an informed consent form.
Descriptive statistics were employed for the general analysis, and Student’s t-test was employed to compare means. The Mann-Whitney U test and the Kruskal–Wallis test were applied to compare medians where appropriate. Nominal variables were analyzed by means of either the chi-square test or Fisher’s exact test where applicable. A p<0.05 in the two-tailed test was considered statistically significant. The Epi Info version 3.5.4. was used for the statistical analysis.
Results
A total of 83 patients were interviewed. Their demographic features are shown in Table 1. Sixty-four percent were undergoing treatment with a BT for the first time. Forty-eight percent were enrolled in a patient assistance program.
Table 1.
Epidemiological Characteristics of the Population Surveyed
| N | 83 |
| Female | 63 (76%) |
| Average Age (Standard Deviation) | 53 years old (15) |
| Lived in Buenos Aires City | 30 (36%) |
| Level of Education | |
| Primary | 32 (39%) |
| Secondary | 35 (42%) |
| University | 16 (19%) |
Sixty percent of the patients who answered the survey had a diagnosis of RA, 24% had psoriatic arthritis, 6% sustained ankylosing spondylitis, 5% underwent juvenile idiopathic arthritis, 2% suffered from systemic lupus erythematosus, 1.5% had ulcerative colitis, and 1.5% had Takayasu arteritis.
Patients received the following medications: abatacept, adalimumab, certolizumab, etanercept, golimumab, infliximab, rituximab, tocilizumab, and ustekinumab.
Had patients been fully informed of the importance of proper transportation and storage of the drug? No, 20% acknowledged that the first time they were handled a BT, they had not been made aware of the relevance of its correct preservation. With regard to those patients who did not know the importance of proper transportation and storage, the proportion of females was 73% vs. 88% in the other group (p=0.2). Both groups had the same level of education (the median was secondary school; p=0.6), and no differences were observed regarding the place of residence (35% lived in the Autonomous City of Buenos Aires or CABA vs. 36% in other group; p=0.9). The number of respondents who did not know the importance of proper transportation and storage was 17% among patients enrolled in a patient assistance program vs. 23% among those who did not participate in these programs (p=0.7).
Are patients usually administered the BT immediately after collecting it from the pharmacy? No, 77% collected the drug more than 7 days before administration; 31% requested acquaintances or relatives to procure the BT for them, but they were well-informed about the impact of refrigeration during transportation except in two cases. It took 25% of the respondents over an hour to get home from the pharmacy, and although they received the BT in a cooler with ice packs, except in five cases, 71% had not been informed of the time frame to keep BT in this condition.
Is the BT duly stored in the patient’s fridge? No, 28% misplaced the drug, 65% of them in the freezer. Improper storage was similar between the patients enrolled in a patient assistance program and those who were not (30% vs. 26%; p=0.8).
With regard to patients who stored the drugs improperly versus those who did so suitably, (a) the proportion of females was 87% vs. 72% (p=0.2); (b) the amount of patients who lived in CABA was 52% vs. 30% (p=0.1); and (c) the number of patients who were receiving a BT for the first time was 70% vs. 62% (p=0.7), respectively. On the other hand, patients who stored the drugs incorrectly had lower median education (p=0.04).
Ninety percent of the respondents did not know the temperature range at which to keep BTs in the fridge, and two out of eight patients who knew the temperature range answered incorrectly. The number of patients who knew the storage temperature range was similar in those enrolled in a patient assistance program and those who were not (7.5% vs. 7%; p=0.9). Only one patient used a fridge thermometer to control the appliance temperature.
Is there another crucial point as to BT storage at home? Yes, 53% of the 83 patients had experienced frequent power outages in summer (once a week or once a day); out of these, 59% were on a weekly basis. Forty percent of the 83 patients had a power outage of over 12 hours, 28% of over 24 hours, and 22% of over 48 hours. Out of 83 patients, 37% took the BT to another house to avoid wasting it, and four disposed of it due to a prolonged blackout. Twenty-nine percent was away from home for over 48 hours during which the BT was in the fridge, and in five cases, they had not assigned another person to take care of the drug during their absence.
Is the BT removed from the fridge only for its immediate administration? No, 46% of the respondents traveled to a center, half of them for over an hour, carrying the BT. Only 10% of the patients took their BT with them on vacation.
Discussion
According to a 2007 publication, in the United States, there were over 1,000 reports due to improper storage of medications that require refrigeration (12). Thus, upon prescribing a BT, physicians are obliged to take into account not only the well-known safety and efficacy considerations, but also whether it is feasible for their patients to transport and store the medication properly since they are required to apply the same standard operating procedures distributors implement from the moment BTs leave the pharmaceutical company until the time of delivery to the pharmacist’s (13). However, several research papers show that patients do not store BTs within the indicated temperature range.
In a study published in 2008, 36 patients prescribed with thermolabile drugs were offered to validate transportation and storage conditions by means of a thermal sensor attached to the product packaging. In 69.4% of the cases, median temperatures during transportation were 8–25°C with maximum trip times of 198 minutes, and in 25% of the cases, the median temperature was higher than 25°C with minimum trip times of 27 minutes and maximum trip times of 45 minutes. All these patients failed to comply with the specified temperature range (14).
In addition, an observational, prospective study published in Spain in 2010 assessed conservation conditions of two BTs in the homes of 60 patients. The study revealed that 58.3% kept the medication within incorrect temperature ranges (15). Deviations were higher when the fridge was older: fridges older than 5 years were considered a risk factor for inadequate storage (Relative Risk, 1.68; 95% confidence interval 1.04–2.71; p=0.02).
Furthermore, a 2016 prospective, multicenter, observational study carried out in eight hospitals in the Netherlands evaluated 255 patients who were administered different BTs. After an average follow-up of 105 days, only 6.7% of the total stored all the packages of BTs within the recommended temperature range (16).
It is noteworthy that information as to acceptable temperature deviations once patients are in charge of BTs storage is scarce. Temperature fluctuations increase the formation of protein aggregates, thus affecting the product quality (17). Laboratories that produce BTs advise communication with the manufacturer if any irregularity in the cold chain maintenance is detected.
In a study published in 2004, a systematic review on the stability of thermolabile medications was performed. In addition to examining PILs, the manufacturing laboratory was contacted either via e-mail or phone. According to the authors, while etanercept (Enbrel) and infliximab (Remicade) may be kept at 25°C for up to 24 hours, rituximab (Mabthera) remains stable for up to 18 days at temperatures of approximately 30°C and 1 day at −20°C (18).
An updated guide published in Spain in 2014 broadens the scope of information on drug stability outside the temperature range set in the PILs for etanercept (Enbrel), infliximab (Remicade), adalimumab (Humira), and rituximab (Mabthera) (19).
In accordance with the etanercept PIL available on the manufacturer’s website in the United States (www.enbrel.com), even though the medication has to be kept in the fridge at a temperature between 2 and 8°C, it is possible to preserve it at room temperature for up to 14 days (20).
In an effort to ascertain whether there was any kind of supplementary information about stability aside from the temperatures indicated in the PIL, the authors contacted every Argentine laboratory that manufactures the BTs included in this study via e-mail.
The authors were provided with additional data about etanercept (Enbrel), and an article by Shannon et al. (21) published in 2017 asserts that all the presentation forms of this medication maintained stability during 1 month when kept at temperatures of 25°C±2°C, which in their opinion afforded greater flexibility and increased patients’ comfort.
The authors were also supplied with a new version of the infliximab (Remicade) PIL approved on 07/31/2017, which claims the drug may be stored at temperatures as high as 30°C for one single period of 6 months (information received from Janssen Laboratory via e-mail).
The manufacturing laboratories of abatacept (Orencia), golimumab (Simponi), and ustekinumab (Stelara) also sent further data from their archives via e-mail. The information implied that the stability of these BTs can be maintained outside the established temperature range, but in every case it was clearly stated that this material should be considered “off-label,” and that it is the physicians’ responsibility to employ the product in compliance with the instructions on the PIL approved in the country where they practice medicine.
Consequently, although it is likely that some BTs tolerate certain temperature deviations without being affected in terms of stability, it is possible that the product properties deteriorate if the product is frozen or submitted to extreme temperatures.
It should be highlighted that the weather in CABA and its outskirts is extremely hot in summer, with average maximum temperatures of 30°C, and peaks of 32.5°C, as registered in 2013 (22). According to a report by the Argentine Ministry of Energy, during the 2015–2016 summer, an average of 89,284 households a day had power outages due to glitches in the electricity network of the metropolitan area, and during the 2016–2017 summer season, although power cuts experienced a 13% decrease, they affected 77,551 households. In both cases, the average power outage lasted 2 hours (23).
This study has the following limitations: As the surveyed patients attended a public hospital, the sample is not representative of all patients treated with BTs. Also, as all the patients were treated in one center, differences in patients’ training may be found if other centers are considered. However, the difficulties brought on by power outages have been sustained by the whole population of CABA and its outskirts in the last few years. On the other hand, the temperatures to which medications were submitted were not measured. Therefore, it is likely that deviations are lower than suspected. At any rate, four patients claimed to have discarded the BT because of a prolonged power outage. As mentioned before, although it is possible that some BTs remain stable at room temperature for some time, some patients keep them in the freezer.
The data were retrospectively collected, and there was no formal training in every case. Thus, it is impossible to differentiate patients who did not receive information from those who did, but either did not understand it or did not remember it correctly.
In addition, although one half of the patients mentioned they were part of a patient assistance program at the time of the survey, it was not confirmed that they were participating when they were administered the BT for the first time.
In summary, every effort should be made to ensure the proper transportation and storage of the BTs on the part of the patient, and new monitoring mechanisms should be devised. The authors advocate the creation of some sort of systematic training program, and the distribution of pre-printed material, leaflets, and photographs for patients who are administered BTs, mainly aimed at those who receive the drugs for the first time and have a lower level of formal education. We also encourage physicians to ask patients whether they have had difficulty transporting and storing the BT, especially during the first visits after the onset of therapy. Clinical failure upon administering BTs, particularly in the summertime, should prompt rheumatologists to perform a thorough assessment of transportation and storage conditions.
Appendix 1. HOW DO YOU TRANSPORT AND STORE YOUR BIOLOGICAL MEDICATION?
Footnotes
Ethics Committee Approval: Ethics committee approval was received for this study from the Bioethics Committee of the Ramos Mejia Hospital.
Informed Consent: Written informed consent was obtained from patients who participated in this study.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept - M.A.S.; Design - G.S.; Supervision - E.K., G.S.; Resources - M.A.S., C.A., J.A.A., D.A., G.S., E.K.; Materials - M.A.S., C.A., J.A.A., D.A., G.S., E.K.; Data Collection and/or Processing - M.A.S., C.A., J.A.A., D.A., G.S., E.K.; Analysis and/or Interpretation - M.A.S., C.A., J.A.A., D.A., G.S., E.K.; Literature Search - M.A.S., C.A., J.A.A., D.A., G.S., E.K.; Writing Manuscript - M.A.S., C.A., J.A.A., D.A., G.S., E.K.; Critical Review - M.A.S., C.A., J.A.A., D.A., G.S., E.K.
Conflict of Interest: The authors have no conflict of interest to declare.
You can reach the appendix of this article at doi.org/10.5152/eurjrheum.2019.18182
Financial Disclosure: The authors declared that this study has received no financial support.
References
- 1.Allegra JR, Brennan J, Lanier V, Lavery R, Markenzie B. Storage temperatures of out-of-hospital medications. Acad Emerg Med. 1999;6:1098–103. doi: 10.1111/j.1553-2712.1999.tb00110.x. [DOI] [PubMed] [Google Scholar]
- 2.Tutuncu Z, Kavanaugh A. Anti-cytokine Therapies. In: Firestein Gary S, Gabriel Sherine E, McInnes Iain B, O’Dell James R., editors. Kelley & Firestein’s Textbook of Rheumatology. Tenth Edition. Elsevier; Philadelphia: 2017. pp. 999–1019. [DOI] [Google Scholar]
- 3.ANMAT. Humira/Humira Pen/Adalimumab. 2015. [Accessed 30, 01, 2018]. Available from: URL: http://www.anmat.gov.ar/boletin_anmat/febrero_2015/Dispo_1711-15.pdf.
- 4.ANMAT. Cimzia/Certolizumab pegol. 2013. [Accessed 30, 01 2018]. Available from: URL. http://www.anmat.gov.ar/boletin_anmat/diciembre_2013/Dispo_7564-13.pdf.
- 5.ANMAT. Enbrel/ Etanercept. 2016. [Accessed 30.01.2018]. Available from: URL: http://www.anmat.gov.ar/boletin_anmat/Abril_2016/Dispo_3722-16.pdf.
- 6.ANMAT. Simponi/Golimumab. 2015. [Accessed 30.01.2018]. Available from: URL: http://www.anmat.gov.ar/boletin_anmat/septiembre_2015/Dispo_7207-15.pdf.
- 7.ANMAT. Remicade/Infliximab. 2013. [Accessed 30.01.2018]. Available from: URL: http://www.anmat.gov.ar/boletin_anmat/abril_2013/Dispo_2093-13.pdf.
- 8.ANMAT. Mabthera/Rituximab. 2012. [Accessed 30.01.2018]. Available from: URL: http://www.anmat.gov.ar/boletin_anmat/junio_2012/Dispo_3563-12.pdf.
- 9.ANMAT. Actemra/Tocilizumab. 2015. [Accessed 30.01.2018]. Available from: URL: http://www.anmat.gov.ar/boletin_anmat/septiembre_2015/Dispo_7858-15.pdf.
- 10.ANMAT. Stelara/Ustekinumab. 2015. [Accessed 30.01.2018]. Available from: URL: http://www.anmat.gov.ar/boletin_anmat/enero_2015/Dispo_0101-15.pdf.
- 11.Regulación de la cadena de Frio de los medicamentos. Medicamentos Ley 26492. 2009. [Accessed 30.01.2018]. Available from: URL: http://www.anmat.gov.ar/webanmat/Legislacion/Medicamentos/Ley_26492_cadenafrio.pdf.
- 12.Cohen V, Jellinek SP, Teperikidis L, Berkovits E, Goldman WM. Room-temperature storage of medications labeled for refrigeration. Am J Health Syst Pharm. 2007;64:1711–5. doi: 10.2146/ajhp060262. [DOI] [PubMed] [Google Scholar]
- 13.European Commission. Information from European Union Institutions, Bodies, Offices and Agencies. Guidelines of 5 November 2013 on Good Distribution Practice of Medicinal Products for Human Use. 2013. [Accessed 30.01.2018]. (2013/c 343/01). Available from: URL: https://ec.europa.eu/health/sites/health/files/files/eudralex/vol1/2013_c343_01/2013_c343_01_en.pdf.
- 14.Marco Garbayo JL, Cuellar Monreal MJ, Pérez Castelló I, Castelló Escrivá A, Muelas Tirado J, Pelegrí Sebastià. Cold chain for the storage of heat-labile drugs in the home. Pharmaceutical Care. 2008;10:40–3. [Google Scholar]
- 15.Cuéllar MJ, Marco JL, Pérez-Castelló I, Castelló Escrivá A. Quality of storage of thermolabile drugs in patients’ homes. Rev Calid Asist. 2010;25:64–9. doi: 10.1016/j.cali.2009.09.001. [DOI] [PubMed] [Google Scholar]
- 16.Vlieland ND, Helga Gardarsdottir, Bouvy ML, Egberts TCG, van den Bemt Bart The majority of patients do not store their biologic disease-modifying antirheumatic drugs within the recommended temperature range. Rheumatology (Oxford) 2016;55:704–9. doi: 10.1093/rheumatology/kev394. [DOI] [PubMed] [Google Scholar]
- 17.Carpenter JF, Randolph TW, Jiskoot W, Crommelin DJ, Middaugh CR, Winter G, et al. Overlooking subvisible particles in therapeutic protein products: gaps that may compromise product quality. J Pharm Sci. 2009;98:1201–5. doi: 10.1002/jps.21530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cuervas-Mons Vendrell M, Fernández Prieto M, Sánchez Sánchez MT, Maestre Fullana MA, Abad Lecha E, Salvador Palacios A, et al. Potential validity of thermolabile drugs outside the preservation conditions recommended by the manufacturer. Farm Hosp. 2004;28:440–4. [PubMed] [Google Scholar]
- 19.Ricote-Lobera I, Ortiz-Martín B, Fraile-Gil S, Santos-Mena B, Hidalgo-Correas FJ, García-Díaz B. Thermolabile drugs stability faced with an accidental interruption in the cold chain. Farm Hosp. 2014;38:169–92. doi: 10.7399/fh.2014.38.3.1164. [DOI] [PubMed] [Google Scholar]
- 20.Medication Guide. [Accesed 14.01.2018]. Available from: URL: http://pi.amgen.com/~/media/amgen/repositorysites/pi-amgen-com/enbrel/enbrel_mg.pdf.
- 21.Shannon E, Daffy J, Jones H, Paulson A, Vicik SM. Etanercept (Enbrel®) alternative storage at ambient temperature. Clin Pharmacol. 2017;9:87–99. doi: 10.2147/CPAA.S131832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Estadística y Censos. Buenos Aires Ciudad. Temperatura media máxima y minima (°C) Ciudad de Buenos Aires. Enero 1991/diciembre 2017. 2018. [Accesed 09.07.18]. Available from: URL: https://www.estadisticaciudad.gob.ar/eyc/?p=27702.
- 23.Ministerio de Energía y Minería. Presidencia de la Nación. Desempe-o del sistema de distribución eléctrica (Edenor y Edesur) 2017. [Accesed 15.01.18]. Available from: URL: https://www.minem.gob.ar/prensa/26104/desempeno-del-sistema-de-distribucion-electrica-edenor-y-edesur.