Abstract
Background
The management of mentally ill offenders in the community is one of the great challenges imposed on community psychiatry.
Aim
The aim of this study was to analyze the association between sociodemographic, clinical, and psychosocial factors and violent behavior in a sample of outpatients with severe mental disorders.
Method
This was a prospective cohort study with a baseline cross-sectional design used to provide a detailed analysis of patients’ profiles, followed by a longitudinal design to measure aggressive and violent behavior during a 1-year follow-up. Patients with severe mental disorders, with or without a history of violence, were enrolled in four Italian Departments of Mental Health and underwent a comprehensive multidimensional assessment.
Results
The sample included 247 outpatients, for a total of 126 cases and 121 controls. Compared to controls, patients with a history of violence had a greater frequency of lifetime domestic violence, a greater lifetime propensity to misuse substances, and a higher number of compulsory admissions. The forthnightly monitoring during the 1-year follow-up did show statistically significant differences in aggressive and violent behavior rates between the two groups. Verbal aggression was significantly associated with aggression against objects and physical aggression. Moreover, outpatients with an history of violence showed statistically significant higher MOAS scores compared to both residential patients with an history of violence, assessed in the first wave of this project, and all controls.
Conclusions
Patients with a history of violence had specific characteristics and showed a greater occurrence of additional community violence during a 1-year observation period. Our results may assist clinicians in implementing standardized methods of patient assessment and violence monitoring in outpatient mental health services and may prompt improved collaboration between different community services.
Introduction
Several studies have investigated the association between severe mental disorders (SMDs) and violence, many of which focused on psychiatric patients admitted to or discharged from acute inpatient facilities, [1] Residential Facilities (RFs) [2], or Forensic Mental Hospitals (FMHs) [3]; other studies have assessed the risk of violence among outpatients in treatment at mental health services [4,5]. All these studies have identified several variables that may increase the risk of violence, including male gender, a diagnosis of schizophrenia, substance use disorders, and a lifetime history of violence [6]. However, only a few studies prospectively assessed the frequency of aggressive and violent behavior among patients in different treatment settings, such as outpatient care and RFs: the latter in many countries have replaced mental hospitals for long-term care [7,8].
In Italy, very few retrospective studies have been conducted to investigate the clinical and sociodemographic profiles of patients at risk for violence or to assess the frequency and severity of aggressive and violent behavior among psychiatric outpatients [9–11]; none of these studies that have been conducted used standardized multidimensional evaluation tools. This represents a serious problem, especially when considering the current structure and provision of mental healthcare in Italy [12,13], which includes the recent closure of all FMHs [14], with the consequent increase in the number of mentally ill offenders who are in outpatient treatment at ordinary Departments of Mental Health (DMHs).
In this study, we aimed to investigate the prevalence of aggressive and violent behavior in a large sample of outpatients with SMDs and their associated factors. First, we examined the sociodemographic, clinical, and treatment-related characteristics of psychiatric outpatients with SMDs with a history of violence (i.e., cases), compared to controls. Second, we measured aggressive or violent behavior exhibited by outpatients during a 1-year period, using a standardized tool, and analyzed a variety of risk and protective factors. An additional aim was to compare the frequency of aggressive and violent behavior (over a 1-year period) among (a) residential patients (VIORMED-1 Study) assessed in wave 1 of this project [15], (b) outpatients (VIORMED-2 Study), both with a history of violence, and (c) residential and outpatients without any history of violence.
Method
Design overview and participants
The Violence Risk and Mental Disorder (VIORMED-2) is a prospective cohort study, with a baseline cross-sectional comparative design, followed by a 1-year follow-up observation period.
Outpatient recruitment was carried out at four DMHs in Lombardy (Northern Italy). In each of the four DMHs, there are four community mental health centers that provide outpatient care; the participating sites have a catchment area with an average population of 351,400 (±32,366.70) (see S1 Table). The average number of outpatients receiving care is 4,206 (±360.13).
Recruitment started in the second half of 2015 and study participants were then consecutively recruited during six months. Inclusion criteria were a primary psychiatric diagnosis and age between 18 and 65 years. Exclusion criteria included a diagnosis of organic mental disorder, mental retardation, dementia, or sensory deficits.
Cases were recruited first. The selection of these patients was based solely on a comprehensive and detailed documentation (as reported in clinical records) about a history of violent behavior(s). Violent patients had to meet any of the following criteria: (i) to have been admitted at least once to a FMH for any violent acts against people and then discharged; and/or (ii) to have a documented lifetime history of violent acts against people in the last 10 years (as reported in the official clinical records), which caused physical harm to the victim, or having committed armed robbery, pyromania, or sexual violence; these behaviors led to legal prosecution or to arrest. The control group included patients who did not meet any of these three conditions during their lifetime.
All participants provided written informed consent before entering the study. Before signing consent, the treating clinician with the local research assistant provided the potential participant with detailed information about the observational nature of the study, of the study aims and methods. The participant information sheets and consent/assent forms made explicit the voluntary nature of subjects’ involvement and the possibility to withdraw from the study at any time. There were 6 patients who had a legal representative: 3 ‘cases’ and 1 control in Garbagnate; 1 control in Legnano and 1 case in Brescia. In these six cases the informed consent was initially sought from the legal representative, and then from the patient. Even if the legal representative gave consent but the patient refused, that person was not included in the study. Patients were assessed with several standardized instruments within 14 days of recruitment. The purpose of the observation follow-up period, which started once patients had completed baseline assessment, was to measure and quantify patients’ aggressive and violent behavior. Ethical approval was granted by the ethical committee of the coordinating center (IRCCS Saint John of God, Fatebenefratelli; n° 64/2014) and by ethical committees of all other recruiting centers.
Measures and assessments
A specific patient schedule was developed to collect information on selected sociodemographic characteristics, clinical and treatment-related factors, and the history of violence (to be completed for cases only). The Structured Clinical Interview for DSM-IV Axis I (SCID-I) [16] and Axis II (SCID-II) [17] were administered to confirm clinical diagnoses. The global concordance was evaluated by Cohen’s K index, and it was K = 0.93 for Axis I and K = 0.65 for Axis II; the latter value (which, according to Landis and Koch, should be considered substantial) [18] is in the range of Cohen’s k value found in Italy by Maffei et al. [19] in a sample of 231 consecutively admitted in- and outpatients assessed with the SCID-II. Symptom severity and psychosocial functioning were assessed using the Brief Psychiatric Rating Scale-Expanded (BPRS-E) [20], and the Specific Levels of Functioning scale (SLOF) [21].
Aggressiveness, impulsiveness, and hostility were evaluated through a set of self-reported measures, notably (a) the Brown-Goodwin Lifetime History of Aggression (BGLHA) [22], an 11-item questionnaire assessing lifetime aggressive behavior across two stages of life (adolescence and adulthood) by directly asking how many times the aggressive behavior occurred for each item; (b) the Buss-Durkee Hostility Inventory (BDHI) [23], a 75-item questionnaire containing eight subscales (e.g, direct and indirect aggression, irritability, negativism, resentment, suspiciousness, verbal aggression and guilt) and producing an index of inhibition of aggression (a higher score indicating more hostility); and (c) the Barratt Impulsiveness Scale (BIS-11) [24], a 30-item 4-point Likert scale questionnaire that investigates personality and behavioral impulsiveness, with scores ranging from 30 to 120 (a higher score indicating more impulsiveness). The State-Trait Anger Expression Inventory 2 (STAXI-2) [25], which includes 57 items grouped into six scales (state and trait anger, anger directed inside and outside, control and expression of anger) plus an anger expression index and an overall measure of total anger expression (a higher score indicates more anger) evaluated on a 4-point Likert scale, was employed to provide specific measures of anger.
Aggressive and violent behavior exhibited by patients during the 1-year follow-up were rated every fifteen days with the Modified Overt Aggression Scale (MOAS) [26], for a total of 24 MOAS evaluations for each patient. All MOAS evaluators (treating clinicians and other mental health staff, and family relatives) were very familiar with the patients and had daily, or very frequent, contact with them. The MOAS includes four aggression subdomains: verbal, against objects, against self, and physical-interpersonal. A score from 0 to 4 is assigned: 0 indicating no aggressive behavior and higher scores showing increasing severity. The score in each category is multiplied by a factor assigned to that category, which is 1 for verbal aggression, 2 for aggression against objects, 3 for aggression against self, and 4 for aggression against other people. The total weighted score for each evaluation ranges from 0 (no aggression) to 40 (maximum grade of aggression); since there were 24 ratings during a 1-year period, the individual MOAS total score for that time period ranged from 0 to 960. We will subsequently refer to the weighted MOAS total score (our primary outcome) simply as the MOAS score.
Treatment compliance was rated with the Medication Adherence Rating Scale (MARS), a 10-item self-report questionnaire validated in patients with psychosis [27].
Statistical analyses
To compare categorical data, a χ2 test or the exact Fisher’s test, whenever appropriate (n<5 in any cell), were used. For quantitative data, ANOVA or a nonparametric Mann Whitney test were used. The normality assumption was verified by visual inspection of the variable distribution through QQ-plots and box plots in addition to Shapiro-Wilk and Kolmogorov-Smirnov tests.
For the BPRS-E, an exploratory factor analysis was used to identify the main scale domains. Factor extraction was performed by varimax rotation, and the number of factors was determined through Kaiser’s criterion (i.e., eigenvalue ≥1) and through visual inspection of the screen plot. Factor loadings with the highest value (among extracted factors) were considered to contribute sufficiently to the overall variability accounted for in each factor.
Monitoring of aggressive and violent behavior was carried out by analyzing MOAS scores across all 24 evaluations, and their trends were estimated with the smoothing-splines method [28]. Given the non-Gaussian distribution of the MOAS scores (skewed and zero-inflated distribution), generalized estimating equation models (GEE) with tweedie distribution and log-link function were used to analyze MOAS repeated measurements.
Finally, the analyses of predictive factors for violence were performed by adopting generalized linear models (GLMs) with tweedie distribution and log-link function (MOAS score—total and subscales—used as the dependent variable and all other measurements as independent ones). Model goodness of fit was evaluated by Akaike information criterion (AIC: the lower value indicates a better model). The beta coefficients are reported as exponential reparameterization of the standardized ones for easier interpretation.
All tests were two-tailed with statistical significance set at p = 0.05. All data were coded and analyzed using the Statistical Package for Social Science (SPSS, version 21 for Windows Chicago, Illinois 69606, USA), and R: A language and environment for statistical computing (R Core Team, 2015), R Foundation for statistical Computing, Vienna, Austria.
Results
Sample
To estimate the minimum sample size based on significant change (baseline-follow-up) differences in the MOAS Total Score between violent and control groups we relied on two studies (Margari et al. [26] and Mauri et al. [29]), indicating that it was necessary to enroll 232 patients (116 cases and 116 controls). However, our main aim was to recruit a larger sample to prevent possible dropouts, so that at the end of the recruitment period (6 months) we enrolled 15 more patients (10 cases and 5 controls). Among the 274 patients who were asked to join the study, 27 (9.8%) refused; therefore, the total study sample included 247 outpatients with a primary diagnosis of SMDs: 126 of them had a lifetime history of violence (i.e., cases) and 121 had no such history (i.e., controls). The two groups did not differ in age, gender, nationality, marital status, or occupation. Compared to the controls, the cases had a lower educational level (X2 = 4.3, p = 0.038), spent more time doing nothing (more than 3 hours per day; X2 = 7.9, p = 0.005), and had received less social support during the past year (X2 = 4.0, p = 0.046). Regarding a lifetime history of violence, the proportion of participants who had witnessed or were involved in at least one episode of domestic violence was higher among cases (X2 = 20.2, p < 0.001). The sociodemographic information is presented in Table 1.
Table 1. Socio-demographic characteristics of patients with an history of violence and controls.
| Violent group | Controls | Test* | p-value | |||
|---|---|---|---|---|---|---|
| N = 126 | % | N = 121 | % | |||
| Gender | ||||||
| Male | 103 | 81.7 | 90 | 74.4 | 1.96 | 0.161 |
| Female | 23 | 18.3 | 31 | 25.6 | ||
| Nationality | ||||||
| Italian | 121 | 96.0 | 119 | 98.3 | 1.20 | 0.240 |
| Others | 5 | 4.0 | 2 | 1.7 | ||
| Age | ||||||
| 18–35 | 20 | 15.9 | 25 | 20.8 | 2.80 | 0.247 |
| 36–50 | 70 | 55.6 | 54 | 45.0 | ||
| 51+ | 36 | 28.6 | 41 | 34.2 | ||
| Marital status | ||||||
| Married or cohabiting | 51 | 40.5 | 47 | 38.8 | 0.07 | 0.793 |
| Single | 75 | 59.5 | 74 | 61.2 | ||
| Education | ||||||
| Low level | 82 | 65.1 | 63 | 52.1 | 4.31 | 0.038 |
| Medium-high level | 44 | 34.9 | 58 | 47.9 | ||
| Occupation | ||||||
| Employed | 52 | 41.6 | 60 | 50.4 | 1.91 | 0.167 |
| Unemployed | 73 | 58.4 | 59 | 49.6 | ||
| Economic independence | ||||||
| Yes | 54 | 44.3 | 55 | 47.0 | 0.18 | 0.670 |
| No | 68 | 55.7 | 62 | 53.0 | ||
| Social support in the last year | ||||||
| Present | 86 | 72.3 | 94 | 83.2 | 3.97 | 0.046 |
| Not present | 33 | 27.7 | 19 | 16.8 | ||
| Time spent doing nothing | ||||||
| Less than 3 h per day | 46 | 37.4 | 66 | 55.5 | 7.94 | 0.005 |
| More than 3 h per day | 77 | 62.6 | 53 | 44.5 | ||
| Episodes of violence in family | ||||||
| Yes | 40 | 34.2 | 11 | 9.6 | 20.21 | <0.001 |
| No | 77 | 65.8 | 103 | 90.4 | ||
* Chi-squared test or Exact Fisher’s test (when n <5 in at least one cell).
The most frequent primary diagnoses included schizophrenia spectrum disorders (up to 41.3%) and personality disorders (up to 28.1%). The mean duration of illness was 17.7 years (SD = 10.5) for the violent group and 16.0 years (SD = 10.0) for the control group (F = 1.8, p = 0.186). The mean age of patients at their first contact with mental health services was 28.6 years (SD = 10.4) for the violent group and 29.8 years (SD = 11.5) for the control group (F = 0.7, p = 0.396). Cases had a higher number of past compulsory admissions to psychiatric hospital wards (X2 = 19.8, p < 0.001) and were less able to collaborate with treating clinicians during the previous year (X2 = 5.1, p = 0.023). With regard to lifetime substance use disorders, higher comorbid rates were found among cases compared to controls (X2 = 8.3, p = 0.004), while there were no between-group differences in alcohol misuse (X2 = 2.1, p = 0.145). The groups did not differ even in recent substance use disorders over the previous 12 months as reported by treating clinicians. No statistical differences were observed regarding medication (present/absent) or the presence/absence of symptoms during the previous 2 years. Clinical and treatment-related characteristics are reported in Table 2.
Table 2. Baseline clinical characteristics of patients with an history of violence and controls.
| Violent group (N = 126) |
Controls (N = 121) |
Test* | p-value | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | ||||||
| Illness duration (Years) | 17.73 | 10.52 | 15.99 | 9.98 | 1.76 | 0.186 | |||
| Age of first contact with DMHs (Years) | 28.63 | 10.36 | 29.81 | 11.48 | 0.72 | 0.396 | |||
| N | % | N | % | Test* | p-value | ||||
| Primary diagnosis by the treating clinician | |||||||||
| Schizophrenia | 52 | 41.3 | 52 | 43.0 | 34.20 | 0.331 | |||
| Personality disorder | 47 | 37.3 | 34 | 28.1 | |||||
| Bipolar disorder | 13 | 10.3 | 14 | 11.6 | |||||
| Anxiety/Mood disorders | 14 | 11.1 | 21 | 17.4 | |||||
| Current comorbidity with substance use disorders | |||||||||
| Alcohol | 9 | 7.3 | 4 | 3.3 | 2.44 | 0.295 | |||
| Other substances | 13 | 10.5 | 17 | 14.0 | |||||
| None | 102 | 82.3 | 100 | 82.6 | |||||
| Lifetime alcohol use disorders | |||||||||
| Yes | 39 | 31.0 | 27 | 22.7 | 2.12 | 0.145 | |||
| No or occasional | 87 | 69.0 | 92 | 77.3 | |||||
| Lifetime substance use disorders | |||||||||
| At least one | 47 | 37.9 | 25 | 21.0 | 8.31 | 0.004 | |||
| None | 77 | 62.1 | 94 | 79.0 | |||||
| Alcohol use disorder in the last 12 months | |||||||||
| Yes | 38 | 30.2 | 30 | 24.8 | 0.89 | 0.345 | |||
| No | 88 | 69.8 | 91 | 75.2 | |||||
| Misuse of at least one substance in the last 12 months | |||||||||
| Yes | 19 | 15.2 | 12 | 9.9 | 1.56 | 0.212 | |||
| No | 106 | 84.8 | 109 | 90.1 | |||||
| Lifetime compulsory admissions | |||||||||
| None | 66 | 54.1 | 88 | 72.7 | 19.81 | <0.001 | |||
| 1–3 | 40 | 32.8 | 33 | 27.3 | |||||
| ≥4 | 16 | 13.1 | 0 | 0.0 | |||||
| Access rate to outpatient community services | |||||||||
| 1 time per month | 89 | 70.6 | 72 | 59.5 | 3.37 | 0.066 | |||
| Less than 1 time per month | 37 | 29.4 | 49 | 40.5 | |||||
| Capability of collaboration in the last year | |||||||||
| Collaborating | 106 | 89.1 | 115 | 96.6 | 5.13 | 0.023 | |||
| Non-collaborating | 13 | 10.9 | 4 | 3.4 | |||||
| Psychopharmacological treatment | |||||||||
| Yes | 115 | 92.0 | 115 | 95.0 | 0.94 | 0.334 | |||
| No | 10 | 8.0 | 6 | 5.0 | |||||
| Psychopathological symptoms (last 2 years) | |||||||||
| Absent | 78 | 67.8 | 80 | 67.8 | 0.00 | 0.996 | |||
| Persistent | 37 | 32.2 | 38 | 32.2 | |||||
DMHs = Departments of Mental Health
* ANOVA for continuous variables; Chi-square test or Fisher’s exact test (n<5 in at least one cell) for categorical variables.
History of violence
Cases committed a large number of violent offenses, including physical aggression (87.2%), stalking (3.2%), sexual violence (2.4%), armed robbery (1.6%), murder (1.6%), attempted murder (0.8%), and other violent acts (3.2%). In more than one-fourth of cases, violent behavior was committed in the presence of psychotic symptoms, and in 20.5% of the instances the offenders were under the influence of alcohol. The history of violence was more frequently due to an episode of impulsive violence (92.4%). Victims of violence were more frequently the patients’ parents or partners (respectively 28.0% and 24.6%), followed by clinical staff (6.8%), patients’ friends (6.8%), other relatives (6.8%), other patients (2.5%), or others (24.6%). The large majority of patients (88.8%) recognized their acts as violent, while the remaining 11.2% denied the violent nature of the offenses. Almost one-fourth (23.4%) of the violent patients were arrested for the violent offenses; 72.8% of patients already had a diagnosis of SMD at the time of their violent offense, and 67.5% were under care at the local DMH. Cases obtained higher scores on the BGLHA (mean score: 40.4, SD = 12.4 for cases vs. 33.6, SD = 9.7 for controls; p < 0.001) (Table 3).
Table 3. Baseline assessment: clinician-administered assessment tools and self-reports.
| Violent group (N = 126) | Controls (N = 121) | Test* | p-value | |||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | |||
| BPRS-E | ||||||
| Affect-Anxiety | 11.17 | 4.11 | 10.70 | 4.19 | –0.73 | 0.463 |
| Activation | 11.67 | 4.75 | 9.55 | 3.09 | –3.81 | <0.001 |
| Negative Symptoms | 5.48 | 3.15 | 5.26 | 2.72 | –0.57 | 0.572 |
| Psychotic Symptoms | 12.38 | 5.47 | 10.88 | 3.50 | –1.16 | 0.247 |
| Total score | 41.01 | 11.75 | 36.85 | 8.89 | –2.43 | 0.015 |
| SLOF | ||||||
| Physical functioning | 24.13 | 1.44 | 24.25 | 1.34 | 0.83 | 0.406 |
| Self-care | 33.24 | 3.14 | 33.37 | 3.12 | 0.44 | 0.663 |
| Interpersonal relationships | 23.90 | 5.94 | 24.93 | 5.63 | 1.46 | 0.143 |
| Social acceptability/adjustment | 23.69 | 4.03 | 26.96 | 2.70 | 6.81 | <0.001 |
| Activities | 48.51 | 7.39 | 49.80 | 6.02 | 1.03 | 0.303 |
| Work skills | 21.51 | 6.57 | 23.16 | 6.11 | 1.91 | 0.056 |
| BGLHA | ||||||
| Total score | 40.38 | 12.44 | 33.59 | 9.68 | –3.91 | <0.001 |
| BIS-11 | ||||||
| Attentional impulsiveness | 15.40 | 4.32 | 14.51 | 3.80 | –1.47 | 0.142 |
| Motor impulsiveness | 22.64 | 4.86 | 21.37 | 4.55 | –1.85 | 0.064 |
| Non-planning impulsiveness | 27.21 | 5.38 | 26.42 | 5.38 | –1.21 | 0.228 |
| Total score | 64.81 | 11.56 | 62.10 | 10.41 | –1.62 | 0.105 |
| BDHI | ||||||
| Assault | 4.58 | 2.61 | 4.43 | 2.45 | 0.17 | 0.683 |
| Indirect aggression | 4.62 | 2.25 | 4.56 | 1.73 | 0.05 | 0.822 |
| Irritability | 4.11 | 2.60 | 4.00 | 2.29 | 0.09 | 0.759 |
| Negativism | 2.63 | 1.57 | 2.31 | 1.54 | 2.02 | 0.157 |
| Resentment | 3.90 | 1.98 | 3.89 | 2.35 | 0.00 | 0.976 |
| Suspicion | 4.13 | 2.38 | 4.28 | 2.62 | 0.15 | 0.702 |
| Verbal aggression | 6.61 | 2.82 | 6.25 | 2.49 | 0.82 | 0.367 |
| Guilt | 4.88 | 2.33 | 4.36 | 2.33 | 2.26 | 0.135 |
| Total score | 35.58 | 14.58 | 34.62 | 12.57 | 0.19 | 0.665 |
| STAXI-2 | ||||||
| State anger | 33.44 | 200.23 | 31.47 | 17.68 | –0.29 | 0.770 |
| Feeling angry | 24.48 | 23.79 | 25.67 | 23.39 | –0.10 | 0.919 |
| Feel like expressing anger verbally | 24.58 | 24.46 | 24.42 | 21.88 | –0.23 | 0.818 |
| Feel like expressing anger physically | 23.32 | 23.44 | 23.73 | 22.26 | –0.04 | 0.969 |
| Trait anger | 32.97 | 19.42 | 29.07 | 16.02 | –1.29 | 0.197 |
| Angry temperament | 25.42 | 23.82 | 23.87 | 21.12 | –1.43 | 0.153 |
| Angry reaction | 25.38 | 23.34 | 23.14 | 19.14 | –0.72 | 0.474 |
| Anger expression-out | 30.14 | 20.99 | 26.17 | 16.41 | –1.74 | 0.083 |
| Anger expression-in | 30.93 | 19.96 | 31.77 | 19.14 | 0.15 | 0.878 |
| Anger control-out | 27.91 | 13.61 | 33.00 | 15.37 | 2.72 | 0.006 |
| Anger control-in | 31.20 | 15.47 | 35.05 | 16.63 | 2.06 | 0.040 |
| Anger expression index | 46.45 | 16.83 | 39.91 | 15.15 | –2.84 | 0.005 |
BDHI = Buss-Durkee Hostility Inventory; BGLHA = Brown-Goodwin Lifetime History of Aggression; BIS-11 = Barratt Impulsiveness Scale; BPRS-E = Brief Psychiatric Rating Scale; SLOF = Specific Levels Of Functioning; STAXI-2 = Scale State-Trait Anger Expression Inventory 2.
* Mann-Whitney test for BPRS-E, SLOF, BGLHA, BIS, STAXI-2; ANOVA for BDHI.
Psychopathology
The exploratory factor analysis of the BPRS-E suggested a four-factor structure named affect-anxiety, activation, negative symptoms and psychotic symptoms (S2 Table). This BPRS-E structure was similar to the previously published [30]. Cases showed higher symptom severity than controls (Table 3). We found a statistically significant difference in the BPRS-E total score between the two groups (mean score: 41.0, SD = 11.7 for cases vs. 36.9, SD = 8.9 for controls; p = 0.015) and different scores in the BPRS-E activation subdomain (mean score: 11.7, SD = 4.8 for cases vs. 9.6, SD = 3.1 for controls; p < 0.001).
Psychosocial functioning and treatment compliance
Although cases had lower scores on all SLOF domains, a statistically significant difference was found for the social acceptability subscale (mean score: 23.7, SD = 4.0 for the violent group vs. 27.0, SD = 2.7 for controls; p < 0.001) (Table 3).
With regard to treatment compliance, patients with an history of violence had a significantly lower MARS average score (6.87, SD = 2.31) compared to controls (7.51, SD = 1.73) (t-test = -2.06, p = 0.041).
Impulsiveness and anger
We did not find any differences between groups in the BDHI and BIS-11 scores. A statistically significant difference was found on two STAXI-2 subscales and for the Anger Expression Index: (i) anger control-out (mean score: 27.9, SD = 13.6 for the violent group vs. 33.0, SD = 15.4 for the control group; p = 0.006); (ii) anger control-in (mean score: 31.2, SD = 15.5 for the violent group vs. 35.1, SD = 16.6 for the control group; p = 0.040); (iii) Anger Expression Index (mean score: 46.5, SD = 16.8 for the violent group vs. 39.9, SD = 15.2 for the control group; p = 0.005). The mean total scores (including subscale scores) for the BDHI, BIS-11, and STAXI-2 in both groups are shown in Table 3.
Aggressive and violent behavior during the 1-Year follow-up
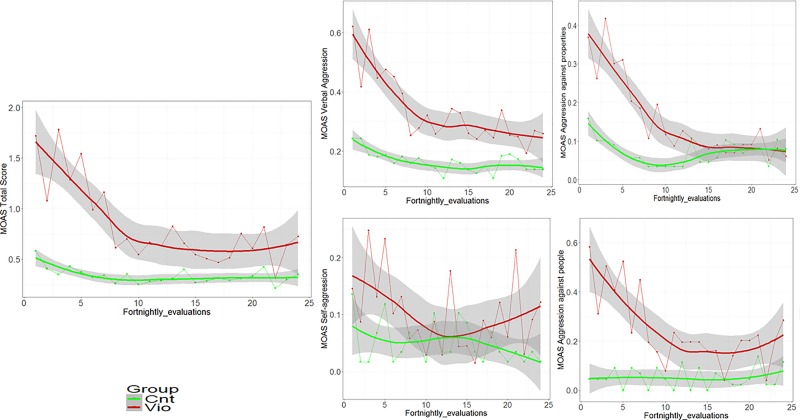
Fifteen patients (11 cases and 4 controls) had more than two missing MOAS and so were not considered in these analyses. Patients with up to two missing MOAS evaluations were computed by the moving average estimation method. Compared to controls, cases displayed statistically greater scores on the MOAS total score (mean = 25.7, SD = 36.3 for the violent group and mean = 8.4, SD = 17.4 for controls; U = -4.7, p < 0.001). The MOAS subratings were also higher for the violent group when compared to controls. This was true for MOAS verbal aggression (mean = 10.2, SD = 12.1 vs. mean = 4.8, SD = 8.5; U = -4.1, p < 0.001), MOAS aggression against objects (mean = 4.7, SD = 8.4 vs. mean = 1.7, SD = 5.6; U = -3.9, p < 0.001), MOAS physical aggression (mean = 7.4, SD = 17.0 vs. mean = 1.0, SD = 5.0; U = -5.1, p < 0.001), and MOAS self-aggression (mean = 3.3, SD = 10.8 vs. mean = 0.8, SD = 3.9; U = -1.8, p = 0.067). Since the specific interest of this study was aggressive and violent behavior, we focused only on the first three subscales. Cases showed a quickly decreasing trend on MOAS scores, while controls had an almost stable trend (see Fig 1). Moreover, trends were statistically different between cases and controls for MOAS total scores. For the verbal and physical aggression scores and MOAS aggression against objects, cases showed a different trend (confidence bands do not overlap) only up to the thirteenth observation.
Fig 1. Longitudinal evaluation of MOAS Total and subscales scores during follow-up in cases and controls.
Trend estimated through Smoothing Spline functions with corresponding 95% confidence bands.
A longitudinal evaluation of the MOAS subscales was performed through generalized estimating equation (GEE) with an interaction effect between time (from 1 to 24 evaluations) and group, and showed significantly different trajectories for aggression against objects (p = 0.002) and physical aggression (p = 0.006), but not for verbal aggression (p = 0.191) (see S3 Table).
Further analyses for gender-specific differences in the frequency of aggressive and violent behavior, measured by the total MOAS, showed no significant differences between males and females (see S1 Fig).
Predictors of aggressive and violent behavior
With regard to the relationship between the three subscales, verbal aggression was a significant predictor of aggression against objects (p < 0.001) and of interpersonal violence (p < 0.001), while aggression against objects was a significant predictor (p < 0.001) of interpersonal violence.
Generalized Linear Models with MOAS total score as a dependent variable and clinical and socio-demographic features, group and their interaction as independent variables were applied to detect which MOAS predictors had different effect in the two study groups. In order to quantify these differentiated (between the two groups) effects (evaluated by beta coefficients) we computed GLMs for the two groups separately.Results showed that the negativism score of the BDHI was the best (in terms of AIC) predictor of violent behavior (p = 0.039, AIC = 1195.3). A lower MOAS total score was predicted by higher levels of negativism (which in this instrument evaluates oppositive and conflictual behaviors) among cases (βcases = 0.81).
Other predictors of the MOAS total score included the SLOF social acceptability score (p < 0.001, AIC = 1521.0), with higher total MOAS scores predicted by lower levels of social acceptability among both cases and controls (but with different strength between groups: βcases = 0.92, βcontrols = 0.75). Both MOAS verbal aggression and MOAS aggression against objects were inversely associated with the SLOF social acceptability score (respectively, p = 0.002, AIC = 1272.0, βcases = 0.91, βcontrols = 0.77; and p = 0.012, AIC = 700.5, βcases = 0.89, βcontrols = 0.71). MOAS physical aggression was predicted by BDHI total score (p = 0.036, AIC = 325.7), with higher strength in controls with respect to cases (βcases = 0.98, βcontrols = 1.11). An inverse association was found between MOAS physical aggression and SLOF social acceptability (p = 0.012, AIC = 556.5), in controls only (βcontrols = 0.69). Table 4 shows all risk and protective factors for violent behavior (recorded during the follow-up period) with a significant different effect between the two study groups.
Table 4. Predictors of aggressive and violent behavior: generalized linear models (GLMs) with interaction effect between variables and groups (all sample), and corresponding GLMs for the two groups.
| All sample | Case patients group | Control group | ||
|---|---|---|---|---|
| p-value | AIC | βcases | βcontrols | |
| Total MOAS | ||||
| BDHI Negativism | 0.039 | 1195.3 | 0.81** | 1.08 |
| SLOF Social acceptability/adjustment | <0.001 | 1521.0 | 0.92** | 0.75** |
| BPRS-E Total Score | 0.019 | 1547.3 | 1.01 | 1.06** |
| Lifetime misuse of substances (No vs Yes) | <0.001 | 1554.5 | 0.91 | 0.18** |
| Time spent doing nothing | 0.008 | 1570.1 | 0.51** | 1.43 |
| BPRS-E Activation | 0.001 | 1575.5 | 1.05** | 1.23** |
| Age | 0.014 | 1576.7 | 0.98** | 0.94** |
| Primary diagnosis | 0.023 | 1578.4 | # | # |
| Familiarity with psychiatric illness (Yes vs No) | 0.063 | 1583.8 | 1.60** | 0.81 |
| Comorbidity with alcohol/substances misuse | 0.028 | 1588.9 | # | # |
| Illness duration | 0.005 | 1592.3 | 1.00 | 0.95** |
| Misuse of alcohol in the last 12 months (No vs Yes) | 0.003 | 1593.3 | 1.04 | 0.33** |
| MOAS verbal aggression | ||||
| SLOF Social acceptability/adjustment | 0.002 | 1272.0 | 0.91** | 0.77** |
| BPRS-E Total Score | 0.018 | 1295.6 | 1.01 | 1.06** |
| Lifetime misuse of substances (No vs Yes) | <0.001 | 1307.1 | 0.89 | 0.25** |
| BPRS-E Activation | 0.008 | 1321.5 | 1.06** | 1.19** |
| Age | 0.011 | 1329.5 | 0.99 | 0.95** |
| Misuse of alcohol in the last 12 months (No vs Yes) | 0.003 | 1332.9 | 0.95 | 0.31** |
| Comorbidity with alcohol/substances misuse | 0.038 | 1334.3 | $ | $ |
| BPRS-E Psychotic Symptoms | 0.046 | 1334.8 | 1.00 | 1.09** |
| Illness duration | 0.023 | 1339.1 | 1.00 | 0.96** |
| MOAS aggression against objects | ||||
| SLOF Social acceptability/adjustment | 0.012 | 700.5 | 0.89** | 0.71** |
| Lifetime misuse of substances (No vs Yes) | 0.001 | 707.4 | 1.40 | 0.16** |
| Illness duration | 0.047 | 720.3 | 0.99 | 0.92** |
| Time spent doing nothing | 0.023 | 721.1 | 0.59 | 3.00* |
| Misuse of alcohol in the last 12 months (No vs Yes) | 0.056 | 722.8 | 0.90 | 0.24** |
| MOAS self-aggression | ||||
| BDHI Indirect Aggression | 0.025 | 246,5 | 0.98 | 1.99** |
| STAXI Feel like expressing anger physically | 0.036 | 339,7 | 1.03** | 0.97 |
| STAXI Feeling angry | 0.035 | 340,3 | 1.03** | 0.97 |
| STAXI Feel like expressing anger verbally | 0.048 | 340,6 | 1.03** | 0.97 |
| STAXI Anger control-in | 0.045 | 340,9 | 1.04** | 0.97 |
| Familiarity with psychiatric illness (Yes vs No) | 0.005 | 360,3 | 4.67** | 0.12** |
| Occupation (Yes vs No) | 0.014 | 361,3 | 5.96** | 0.34 |
| MOAS physical aggression | ||||
| BDHI Total Score | 0.036 | 325.7 | 0.98 | 1.11* |
| STAXI Anger Expression Index | 0.046 | 510.0 | 1.00 | 1.06** |
| Lifetime misuse of substances (No vs Yes) | 0.001 | 549.1 | 0.91 | 0.03** |
| Age of first contact with DMHs | 0.001 | 553.3 | 0.97 | 0.71** |
| SLOF Social acceptability/adjustment | 0.012 | 556.5 | 0.99 | 0.69** |
| Misuse of alcohol in the last 12 months (No vs Yes) | 0.039 | 563.8 | 0.53 | 0.06** |
| BPRS-E Activation | 0.017 | 566.2 | 1.05 | 1.40** |
| Primary diagnosis | 0.024 | 568.0 | £ | £ |
| Time spent doing nothing | 0.051 | 568.2 | 0.31** | 2.02 |
| Illness duration | 0.029 | 570.3 | 1.03 | 0.92* |
BDHI = Buss-Durkee Hostility Inventory; BPRS-E = Brief Psychiatric Rating Scale; MOAS = Modified Overt Aggression Scale; SLOF = Specific Levels of Functioning; STAXI-2 = Scale State-Trait Anger Expression Inventory 2.
p value: significance of the interaction term; AIC: Akaike Information Criterion of the GLM; βcases βcontrols: estimates of the variable effect in the two groups separately.
* Tendency towards significance (p≤0.1) of the beta coefficient
** Significance (p<0.05) of the β coefficient.
# Among cases, patients with a personality disorder are more violent than other diagnostic groups (p<0.048); among controls, patients with personality disorders are more violent than patients with schizophrenia (p<0.001). Among cases, there are no significant differences between patients with and without comorbidity of alcohol/substance abuse. Among controls, patients with a comorbidity of alcohol/substance abuse are more violent than patients who do not use alcohol and substances.
$ Among cases, there are no significant differences in verbal aggression between patients with and without comorbidity of alcohol/substance abuse. Among controls, patients with a comorbidity of alcohol/substance abuse are more verbally violent than patients who do not use alcohol and substances.
£ Among cases, there are no significant differences among different diagnostic groups; among controls, patients with personality disorders are more violent than patients with schizophrenia (p<0.047).
Additionally, univariate GLMs (without considering the group distinction between cases and controls) were performed to analyze factors associated with the MOAS scores. The best predictor of new aggressive and violent behavior(s) was the BDHI suspicion score (p = 0.030, AIC = 1156.1, β = 1.14), followed by the BGLHA total score (p = 0.002, AIC = 1208.9, β = 1.05).
Furthermore, we found different factors associated with the MOAS domains. MOAS verbal aggression was predicted by the BDHI suspicion score (p = 0.038, AIC = 991.5, β = 1.11), whereas MOAS aggression against objects was predicted by the STAXI Anger Expression Index and STAXI trait anger (respectively, p = 0.014, AIC = 665.9, β = 1.03; and p = 0.038, AIC = 676.0, β = 1.02). Only the BGLHA total score predicted MOAS physical aggression (p = 0.018, AIC = 443.7, β = 1.10). The full list of the factors associated with the MOAS scores is shown in S4 Table.
Violence and hospital admission
During the 1-year follow-up, 23 patients (16 with an history of violence, 7 controls) were hospitalized in general hospital psychiatric wards. We compared the last MOAS score prior to hospitalization with the previous four scores (two months) and with the MOAS score immediately after discharge. As shown in Supporting Information S2 Fig, there were no statistically significant differences between the MOAS scores at these different timepoints, suggesting that in our cases, hospital admission was not due to an increase in aggressive and violent behavior (S2 Fig).
Patients with an history of violence in different treatment settings
In the first wave of this project [15], we evaluated 139 patients living in RFs, 82 violent and 57 control subjects. We did not find any statistically significant differences in aggressive behavior rates between the two groups during the 1-year follow-up. Our conclusion was that patients with a history of violence in RFs, where treatment and clinical supervision are available, do not show higher rates of aggression and violence compared to patients with no lifetime history of violence.
Therefore, we decided to compare the two samples (residential and outpatients) from waves 1 and 2 to establish whether staying in a RF for patients with a history of violence has a protective effect from the risk of violent behavior. To do this, we merged the two control samples (patients with and without a history of violence), while we kept the two case samples (outpatients and residential patients) with a history of violence separated. The results of this analysis are shown in Fig 2.
Fig 2. Longitudinal evaluation of MOAS Total score during the 1-year follow-up in three different clinical groups.
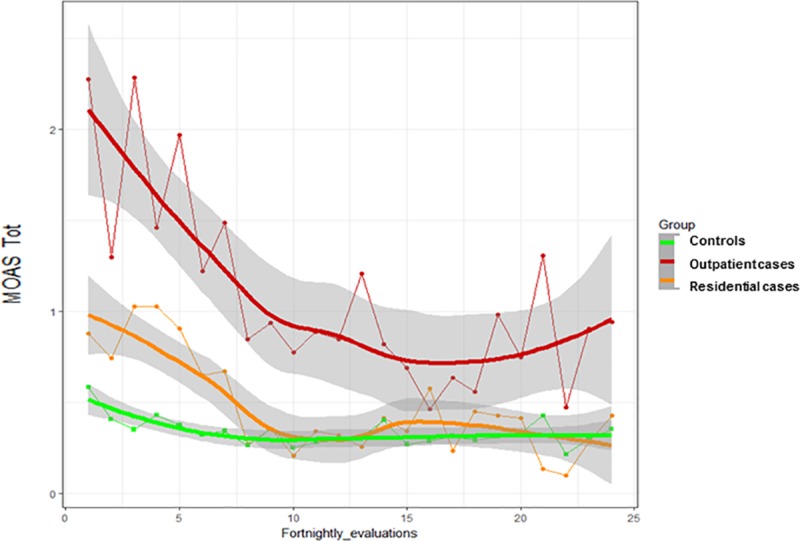
Trend estimated through Smoothing Spline functions with corresponding 95% confidence bands.
Compared to both controls and residential cases, outpatient cases displayed statistically greater scores on the MOAS total score when compared to both controls and residential cases (mean = 25.7 SD = 36.3 for outpatient cases, mean = 11.4 SD = 18.0 for residential cases and mean = 8.1 SD = 17.1 for all controls; K = 32.7, p<0.001).
Discussion
A recent Italian law (81/2014) enacted a significant reorganization of the forensic system, with the closure of the six FMHs, the opening of new small-scale high-security units, and a consequent transfer of many patients with SMD who had offended, or are at risk of offending, to ordinary DMHs (including RFs managed by these services). This change has prompted a deeper investigation into the risk of aggressive and violent behavior among patients in treatment at DMHs. To our knowledge, this is the first Italian study, and one of very few internationally, to use a large set of standardized multidimensional evaluation tools and to prospectively examine the frequency and severity of aggressive and violent behavior in outpatients with SMDs.
Previous studies examining the link between SMDs and violence have produced mixed findings [1,31]. Several factors have been suggested to explain this heterogeneity, such as different study designs, assessment tools, type of outcome(s), settings of care, and the specific national mental health policies and programmes, making it difficult to make comparisons and interpret results [6,32–34].
Our study demonstrates that outpatients with SMDs who have an history of serious violence are more likely to show higher levels (in terms of frequency and severity) of aggressive and violent behavior as compared to patients who do not have such a history, and this raises important clinical problems in terms of prevention and management.
Are outpatients with a history of violence more likely to commit violent acts?
Our findings show that outpatients with a lifetime history of violence under care in Italian DMHs had more frequent and more severe episodes of aggression and violence compared to controls. This is in line with Italian retrospective studies on outpatients conducted after the reform of Law 81/2014 [9,10]. On the other hand, this finding is at odds with the results of the first wave of the VIORMED project, in which 82 patients living in RFs with an history of violence were compared to 57 patients with no such history. In these settings, with 24-hour cover, the difference in the frequency of aggressive and violent behavior between patients with and without a history of violence was negligibile [15]. Living in a controlled environment, with compliance granted and no possibility of substance use disorders, may have a preventive effect on aggressive and violent behavior, while life in the community, where treatment compliance is not warranted and there is a greater risk of substance use disorders, has a potential detrimental effect on the risk of recurrence. Indeed, this finding was confirmed when comparing the MOAS total scores among outpatient cases, residential cases, and all controls: while residential cases, living in a controlled environment, did not show higher scores compared to all controls, from both settings, outpatient cases displayed the highest rates of aggressive and violent behavior. To our knowledge, this is the first time ever that a study with the same prospective design compared patients with an history of violence treated in different setting, and shows a marked difference in behavioral patterns associated with different regimes of care (with higher or lower protection).
What predicts violence?
We identified several predictive and protective factors for community violence. Social acceptability was a predictor of nonaggressive behavior, indicating that better social acceptability is associated with lower MOAS scores among both cases and controls. With specific regard to physically aggressive behavior, higher levels of anger expression did predict aggressive behavior, while hostility was predictive only among controls. Other predictors of aggressive and violent behavior that we found in our study (i.e., lifetime substance use disorders, early age at the first contact with DMHs, longer illness duration) are in line with findings from previous studies on Italian cohorts [9].
Finally, patients who showed higher levels of verbal aggression were more likely to commit physical aggression against objects or against other people, and patients who showed higher levels of aggression against objects were more likely to commit aggression against other people. This sequence seems to compose a ‘continuum’ in the occurrence of aggressive and violent behavior and offers important elements for prevention: if a patient shows increasing levels of verbal aggression, or of aggression against objects, this may indicate the need for appropriate interventions to prevent an escalation to more severe forms of violence against other people.
Clinical differences between patients with or without violence history
Unlike previous studies on outpatient cohorts [31], we did not find any differences in many functional areas between outpatients with or without a lifetime history of physical interpersonal violence. Furthermore, at variance with some studies [35], but not other studies [9] done in outpatient samples, our cases had more severe psychopathological symptoms, as rated with the BPRS-E, compared to controls. Possible explanations for these divergent results may be related to the use of different assessment tools and to the different time elapsed from the index violent behavior. On the other hand, there is consensus in the literature concerning the association between a lifetime history of violence, a history of domestic violence, a lifetime use of substances, and a history of compulsory admissions [6].
Impulsiveness and anger
With regard to impulsiveness, unlike previous findings [36,37], we found no differences between the two groups when rated by the BIS. Although there were differences in BGHA scores, the BDHI scores among cases were similar to those found in a study conducted among male prisoners [38]. Findings on angry feelings showed that compared to controls, cases had lower anger-control, with less ability to calm or cool down. This is in line with previous findings showing a negative association between the STAXI-2 anger control subscale and aggression [39].
How to manage violent patients in the community
This study provides useful indications for planners and clinicians who have the relevant task of planning and managing services which currently have also to care for mentally ill offenders in Italy. While patients with a history of interpersonal violence are effectively managed in RFs [15], where treatment and clinical supervision are granted, our study shows that outpatients living in the community still pose a higher risk of reiteration of aggressive and violent behavior as compared to patients with no history of violence. It is doubtful whether current mental health services in Italy are well equipped to cope with these relevant clinical needs: despite the approval of the new law reorganizing the care for mentally ill offenders, no plans for specific training programmes of mental health workers have been developed, and residency programmes for psychiatrists in training are equally insufficient to meet these training needs; as a consequence many services are inadequately equipped to well manage difficult clinical situations raised by patients with serious histories of violence, as recognized by several authors; the relationships with judicial institutions and forensic services are equally problematic [40–42].
At the same time an active collaboration between mental health services and addiction services (which is of paramount relevance given the importance of substance use disorders as a primary risk factor for aggressive and violent behavior) is often missing, and new strategies of collaborative work involving different treatment agencies have to be developed. It will be necessary to set up appropriate monitoring systems to well understand the main unmet needs of this difficult-to-treat clinical population and identify the clinical skills which mental health workers have to learn to well manage these patients.
Acute hospitalizations and violent behavior
During the 1-year follow-up, 23 patients (16 with an history of violence, 7 controls) were hospitalized in general hospital psychiatric wards: based on MOAS scores in the periods prior to hospitalization and after discharge, we did not find any association between hospital admission and reports of increased violent behavior. In a large survey of almost 3,000 acute patients admitted to Italian general hospital psychiatric wards, violence against people was among factors contributing to admission for a substantial proportion of hospitalized patients: this occurred in 19.3% of patients with a diagnosis of schizophrenia, 13.5% of patients with bipolar disorders, and 19.3 for patients with personality disorders or substance use disorders [43]. Given the small number of patients acutely admitted in our study, it is difficult to generalize our results, and specific investigations about the role of aggressive and violent behavior in triggering hospital admissions are warranted.
Limitations
This study has a number of limitations. First, the duration of the observation period limited to one year may have reduced the possibility to detect new aggressive and violent episodes and, hence, to identify long-term predictors of such behavior. Second, the MOAS assessment was based on that reported by the patients’ treating clinicians, case managers, or family members and not based on a direct 24-hour observation. Thus, our results might have underestimated the occurrence of aggressive and violent behavior among outpatients, in particular because MOAS was not used to evaluate each individual aggressive episode. In any event, the limited period of observation for each MOAS rating (two weeks) makes it unlikely that relevant episodes of aggression or violence remained undetected.
Conclusions
Our data show that outpatients with a history of violence are more aggressive than patients with no lifetime violent behavior. The management of mentally ill offenders in the community is one of the great challenges imposed on community psychiatry. Indeed, more intensive care, as found in RFs, where treatment is granted and prevention of significant substance use disorders is avoided, is associated with a substantial decrease in the frequency and severity of aggressive and violent behavior even among people with a history of violence.
Violence by the mentally ill has a profound detrimental effect on public opinion, is associated with stigma and discrimination, and places a great burden on family members, who are often the victims of such violence. Risk assessment plays a key role in the prevention and/or decrease of violent behavior [44,45]. This process is preliminary and linked to an accurate diagnosis, which defines the target population [46], and it has to be integrated with local base information [33]. Better prediction also means better prevention by developing more appropriate treatments tailored to the psychopathological dimensions associated with violence (e.g., impulsivity, hostility). If community psychiatry can prevent the violence associated with mental disorders, the full integration of patients and their families will be much easier.
Supporting information
(DOCX)
(DOCX)
(DOCX)
(DOCX)
Trend estimated through Smoothing Spline functions with corresponding 95% confidence bands.
(TIF)
Longitudinal evaluation of MOAS Total score (n = 23 outpatients).
(TIF)
(XLSX)
Acknowledgments
Acknowledgments are due to the following Clinicians who have provided a valuable collaboration: Paola Artioli, M.D., Monica Bonfiglio, M.D., Silvia Bonomi, M.D., Stefania Borghetti, M. D, Giulia Brambilla, M.D., Paolo Cacciani, M.D., Pierluigi Castiglioni, M.D., Giorgio Cerati, M.D., Andrea Cesareni, M.D., Fabio Consonni, M. M.D., Giacomo Deste, M.D., Emanuela Ferrari, M.D., Giulia Gamba, M.D., Antonio Musazzi, M.D., Roberta Paleari, M.D., Rosa Perrone, M.D., Monica Petrachi, M.D., Francesco Restaino, M.D., Enrico Rossella, M.D., Daniele Salvadori, M.D., Jacopo Santambrogio, M.D., Giuseppina Secchi, M.D., Joyce Severino, M.D., Valentina Stanga, M.D., Bruno Travasso, M.D., Alessandra Vecchi, M.D.
Data Availability
All data are available as a Supporting Information file in Excel format.
Funding Statement
The VIORMED-2 (Violence Risk and Mental Disorder 2) project was funded by the Health Authority of Regione Lombardia, Italy, grant CUP E42I14000280002 for “Disturbi mentali gravi e rischio di violenza: uno studio prospettico in Lombardia” with Decreto D.G. Salute N.6848, date 16.7.2014.
References
- 1.Iozzino L, Ferrari C, Large M, Nielssen O, de Girolamo G. Prevalence and Risk Factors of Violence by Psychiatric Acute Inpatients: A Systematic Review and Meta-Analysis. Li S, editor. PLoS One. 2015;10: e0128536 10.1371/journal.pone.0128536 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bulgari V, Ferrari C, Pagnini F, de Girolamo G, Iozzino L. Aggression in mental health residential facilities: A systematic review and meta-analysis. Aggress Violent Behav. 2018;41: 119–127. [Google Scholar]
- 3.Fazel S, Fimińska Z, Cocks C. Patient outcomes following discharge from secure psychiatric hospitals: Systematic review and meta-analysis. Br J Psychiatry. 2016;208: 17–25. 10.1192/bjp.bp.114.149997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Appelbaum PS, Robbins PC, Monahan J. Violence and delusions: Data from the MacArthur Violence Risk Assessment Study. Am J Psychiatry. 2000;157: 566–572. 10.1176/appi.ajp.157.4.566 [DOI] [PubMed] [Google Scholar]
- 5.Chang WC, Chan SSI, Hui CLM, Chan SKW, Lee EHM, Chen EYH. Prevalence and risk factors for violent behavior in young people presenting with first-episode psychosis in Hong Kong: A 3-year follow-up study. Aust New Zeal J Psychiatry. 2015;49: 914–922. [DOI] [PubMed] [Google Scholar]
- 6.Witt K, van Dorn R, Fazel S. Risk Factors for Violence in Psychosis: Systematic Review and Meta-Regression Analysis of 110 Studies. PLoS One. 2013;8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rueve ME, Welton RS. Violence and mental illness. Psychiatry. 2008;5: 34–48. [PMC free article] [PubMed] [Google Scholar]
- 8.Stuart H. Violence and mental illness: an overview. World Psychiatry. 2003;2: 121–124. [PMC free article] [PubMed] [Google Scholar]
- 9.Amore M, Tonti C, Esposito W, Baratta S, Berardi D, Menchetti M. Course and Predictors of Physical Aggressive Behaviour after Discharge from a Psychiatric Inpatient Unit: 1 Year Follow-up. Community Ment Health J. 2013;49: 451–456. 10.1007/s10597-012-9530-1 [DOI] [PubMed] [Google Scholar]
- 10.Pinna F, Tusconi M, Dessì C, Pittaluga G, Fiorillo A, Carpiniello B. Violence and mental disorders. A retrospective study of people in charge of a community mental health center. Int J Law Psychiatry. Elsevier Ltd; 2016;47: 122–128. 10.1016/j.ijlp.2016.02.015 [DOI] [PubMed] [Google Scholar]
- 11.Catanesi R, Carabellese F, Guarino D. Analisi del comportamento violento in una popolazione di pazienti psichiatrici in Puglia e Basilicata. Criminol Clin. 2007;1: 63–80. [Google Scholar]
- 12.de Girolamo G, Bassi M, Neri G, Ruggeri M, Santone G, Picardi A. The current state of mental health care in Italy: problems, perspectives, and lessons to learn. Eur Arch Psychiatry Clin Neurosci. 2007;257: 83–91. 10.1007/s00406-006-0695-x [DOI] [PubMed] [Google Scholar]
- 13.Picardi A, Lega I, Candini V, Dagani J, Iozzino L, de Girolamo G. Monitoring and Evaluating the Italian Mental Health System. J Nerv Ment Dis. 2014;202: 451–459. 10.1097/NMD.0000000000000144 [DOI] [PubMed] [Google Scholar]
- 14.Barbui C, Saraceno B. Closing forensic psychiatric hospitals in Italy: a new revolution begins? Br J Psychiatry. 2015;206: 445–446. 10.1192/bjp.bp.114.153817 [DOI] [PubMed] [Google Scholar]
- 15.de Girolamo G, Buizza C, Sisti D, Ferrari C, Bulgari V, Iozzino L, et al. Monitoring and predicting the risk of violence in residential facilities. No difference between patients with history or with no history of violence. J Psychiatr Res. 2016;80: 5–13. 10.1016/j.jpsychires.2016.05.010 [DOI] [PubMed] [Google Scholar]
- 16.First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Patient Edition (SCID-I/P). New York, NY: Biometrics Research. New York State Psychiatric Institute; 2002. [Google Scholar]
- 17.First MB, Gibbon M, Spitzer RL, Williams JBW, Benjamin S. Structured Clinical Interview for DSM-IV Axis II Personality Disorders (SCID-II). Washington, D.C.: American Psychiatric Press, Inc; 1997. [Google Scholar]
- 18.Landis JR, Koch GG. The Measurement of Observer Agreement for Categorical Data. Biometrics. 1977;33: 159 [PubMed] [Google Scholar]
- 19.Maffei C, Fossati A, Agostoni I, Barraco A, Bagnato M, Deborah D, et al. Interrater Reliability and Internal Consistency of the Structured Clinical Interview for DSM-IV Axis II Personality Disorders (SCID-II), Version 2.0. J Pers Disord. 1997;11: 279–284. [DOI] [PubMed] [Google Scholar]
- 20.Ventura J, Green MF, Shaner A, Liberman RP. Training and quality assurance with the Brief Psychiatric Rating Scale: “The drift busters.” Int J Methods Psychiatr Res. 1993;3: 221–244. [Google Scholar]
- 21.Montemagni C, Rocca P, Mucci A, Galderisi S, Maj M. Italian version of the “Specific Level of Functioning.” J Psychopathol. 2015;21: 287–296. [Google Scholar]
- 22.Brown GL, Goodwin FK, Ballenger JC, Goyer PF, Major LF. Aggression in humans correlates with cerebrospinal fluid amine metabolites. Psychiatry Res. 1979;1: 131–139. [DOI] [PubMed] [Google Scholar]
- 23.Buss AH, Durkee A. An inventory for assessing different kinds of hostility. J Consult Psychol. 1957;21: 343–349. [DOI] [PubMed] [Google Scholar]
- 24.Barratt ES. Factor analysis of some psychometric measures of impulsiveness and anxiety. Psychol Rep. 1965;16: 547–554. 10.2466/pr0.1965.16.2.547 [DOI] [PubMed] [Google Scholar]
- 25.Spielberger CD, Johnson EH, Russell SF, Crane RJ, Jacobs GA, Worden TJ. The experience and expression of anger: Construction and validation of an anger expression scale. Anger Hostility Cardiovasc Behav Disord. 1985; 5–30. [Google Scholar]
- 26.Margari F, Matarazzo R, Cassacchia M, Roncone R, Dieci M, Safran S, et al. Italian validation of MOAS and NOSIE: A useful package for psychiatric assessment and monitoring of aggressive behaviours. Int J Methods Psychiatr Res. 2005;14: 109–118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fond G, Boyer L, Boucekine M, Aden LA, Schürhoff F, Tessier A, et al. Validation study of the Medication Adherence Rating Scale. Results from the FACE-SZ national dataset. Schizophr Res. 2017;182: 84–89. 10.1016/j.schres.2016.10.023 [DOI] [PubMed] [Google Scholar]
- 28.Ramsay JO, Silverman BW. Functional data analysis (2nd ed). New York: Springer-Verlag; 2005. [Google Scholar]
- 29.Mauri MC, Rovera C, Paletta S, De Gaspari IF, Maffini M, Altamura AC. Aggression and psychopharmacological treatments in major psychosis and personality disorders during hospitalisation. Prog Neuro-Psychopharmacology Biol Psychiatry. 2011;35: 1631–1635. [DOI] [PubMed] [Google Scholar]
- 30.Dazzi F, Shafer A, Lauriola M. Meta-analysis of the Brief Psychiatric Rating Scale–Expanded (BPRS-E) structure and arguments for a new version. J Psychiatr Res. 2016;81: 140–151. 10.1016/j.jpsychires.2016.07.001 [DOI] [PubMed] [Google Scholar]
- 31.Swanson JW, Swartz MS, Van Dorn RA, Elbogen EB, Wagner HR, Rosenheck RA, et al. A national study of violent behavior in persons with schizophrenia. Arch Gen Psychiatry. 2006;63: 490–499. 10.1001/archpsyc.63.5.490 [DOI] [PubMed] [Google Scholar]
- 32.Brucato G, Appelbaum PS, Lieberman JA, Wall MM, Feng T, Masucci MD, et al. A Longitudinal Study of Violent Behavior in a Psychosis-Risk Cohort. Neuropsychopharmacology. 2018;43: 264–271. 10.1038/npp.2017.151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Singh JP, Fazel S, Gueorguieva R, Buchanan A. Rates of violence in patients classified as high risk by structured risk assessment instruments. Br J Psychiatry. 2014;204: 180–187. 10.1192/bjp.bp.113.131938 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Coid JW, Ullrich S, Bebbington P, Fazel S, Keers R. Paranoid Ideation and Violence: Meta-analysis of Individual Subject Data of 7 Population Surveys. Schizophr Bull. 2016;42: 907–915. 10.1093/schbul/sbw006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Langeveld J, Bjørkly S, Auestad B, Barder H, Evensen J, ten Velden Hegelstad W, et al. Treatment and violent behavior in persons with first episode psychosis during a 10-year prospective follow-up study. Schizophr Res. 2014;156: 272–276. 10.1016/j.schres.2014.04.010 [DOI] [PubMed] [Google Scholar]
- 36.Dolan M, Fullam R. Behavioural and psychometric measures of impulsivity in a personality disordered population. J Forens Psychiatry Psychol. 2004;15: 426–450. [Google Scholar]
- 37.Evans L, Ioannou M, Hammond L. A predictive model of criminality in civil psychiatric populations. J Crim Psychol. 2015;5: 1–12. [Google Scholar]
- 38.Carli V, Jovanovi N, Podle A, Roy A, Rihmer Z, Maggi S, et al. The role of impulsivity in self-mutilators, suicide ideators and suicide attempters—A study of 1265 male incarcerated individuals. 2010;123: 116–122. 10.1016/j.jad.2010.02.119 [DOI] [PubMed] [Google Scholar]
- 39.Lievaart M, Franken IHA, Hovens JE. Anger Assessment in Clinical and Nonclinical Populations: Further Validation of the State-Trait Anger Expression Inventory-2. J Clin Psychol. 2016;72: 263–278. 10.1002/jclp.22253 [DOI] [PubMed] [Google Scholar]
- 40.Ferracuti S, Pucci D, Trobia F, Alessi MC, Rapinesi C, Kotzalidis GD, et al. Evolution of forensic psychiatry in Italy over the past 40 years (1978–2018). Int J Law Psychiatry. 2019;62: 45–49. 10.1016/j.ijlp.2018.10.003 [DOI] [PubMed] [Google Scholar]
- 41.Capuzzi E, Pini E, Malerba MR, Cova F, Lax A, Mauri S, et al. Factors associated with referrals to high security forensic services among people with severe mental illness and receiving inpatient care in prison. Int J Law Psychiatry. 2019;62: 90–94. 10.1016/j.ijlp.2018.11.003 [DOI] [PubMed] [Google Scholar]
- 42.De Luca V, Pompili PM, Paoletti G, Bianchini V, Franchi F, Lombardi M, et al. The reform of Italian forensic psychiatric hospitals and its impact on risk assessment and management. Int J Risk Recover. 2018;1. [Google Scholar]
- 43.Preti A, Rucci P, Santone G, Picardi A, Miglio R, Bracco R, et al. Patterns of admission to acute psychiatric in-patient facilities: A national survey in Italy. Psychol Med. 2009;39: 485–496. 10.1017/S0033291708003607 [DOI] [PubMed] [Google Scholar]
- 44.van de Sande R, Nijman HLI, Noorthoorn EO, Wierdsma AI, Hellendoorn E, van der Staak C, et al. Aggression and seclusion on acute psychiatric wards: effect of short-term risk assessment. Br J Psychiatry. 2011;199: 473–478. 10.1192/bjp.bp.111.095141 [DOI] [PubMed] [Google Scholar]
- 45.van der Veeken FCA, Lucieer J, Bogaerts S. Routine Outcome Monitoring and Clinical Decision-Making in Forensic Psychiatry Based on the Instrument for Forensic Treatment Evaluation. Dang Y, editor. PLoS One. 2016;11: e0160787 10.1371/journal.pone.0160787 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Coid JW, Ullrich S, Kallis C, Keers R, Barker D, Cowden F, et al. The relationship between delusions and violence: Findings from the East London first episode psychosis study. JAMA Psychiatry. 2013;70: 465–471. 10.1001/jamapsychiatry.2013.12 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
(DOCX)
(DOCX)
(DOCX)
Trend estimated through Smoothing Spline functions with corresponding 95% confidence bands.
(TIF)
Longitudinal evaluation of MOAS Total score (n = 23 outpatients).
(TIF)
(XLSX)
Data Availability Statement
All data are available as a Supporting Information file in Excel format.