Abstract
Rationale:
South Africa continues to experience new HIV infections, with the highest risk among Black Africans living in poor communities. Most HIV prevention interventions target women or men separately and only a small number target couples jointly.
Objective:
This study examines varying strategies to engage women and men around HIV prevention and improved couple interactions.
Methods:
The study comprises three arms: (1) a couple-based intervention delivered to women and men jointly; (2) women and men both offered a gender-focused intervention that is delivered to them separately; and (3) an intervention offered to women only and their male partners receive standard HIV testing and counseling (comparison arm). Between June 2010 and April 2012, men were identified in and around drinking establishments in a large disadvantaged community in Cape Town and asked to participate in the study if they drink regularly, had recent unprotected sex with their partner, and have a female partner who was willing to participate in the study.
Results:
A total of 299 couples completed the baseline assessment and 276 were included in the analysis of sexual risk, partner communication, conflict resolution, and gender norm outcomes at baseline and six-month follow-up. Couples that participated in the couple-level intervention and couples where both partners received the intervention separately had better couple-level gender norms than couples in the comparison arm (women only receive intervention). Further, couples in the couple-level intervention and the both partners exposed separately arms were more likely to have the man only report consistent condom use than neither partner report consistent condom use than couples in the comparison arm.
Conclusion:
Community-based HIV prevention intervention programs need to consider strategies to engage women and men and, if feasible, reach both partners jointly. Couple-level interventions are promising to improve gender norms and subsequently improve health outcomes, including reduced HIV risk among women, men, and couples.
Keywords: South Africa, Couple, HIV prevention, Gender norms, Sexual risk behavior, Partner communication, Couple conflict
Introduction
South Africa is experiencing a generalized heterosexual HIV epidemic, with HIV prevalence highest among Black Africans living in poor communities (Shaikh et al., 2006; Shisana et al., 2014). These communities also have high, problematic rates of gender-based violence and alcohol use (Kalichman et al., 2005) and gender norms that accept and expect that men will have multiple sex partners (Sawyer et al., 2006) and support men’s violent behavior (Mthembu et al., 2014). Each of these factors contributes to high HIV transmission (Browne & Wechsberg, 2010; Chersich & Rees, 2010; Shuper et al., 2010).
In South Africa, more than 60% of new HIV infections are transmitted through sexual contact of heterosexual couples (Case et al., 2012). At all ages, women have higher rates of HIV in South Africa than men (Dworkin et al., 2013; Shisana et al., 2014; Wechsberg et al., 2014). One factor that increases women’s risk of HIV acquisition is greater biological risk of infection on a per sex act basis (Deller et al., 2015). Importantly, beyond the greater biological risk among women, there are also cultural, social, and economic factors that put women at greater risk of HIV. For example, women who are poor may exchange sex for money, may have sex with partners that are much older than them, or are under the influence of alcohol; each of these scenarios can increase the likelihood of having unprotected sex and/or experience of gender-based violence and increase a woman’s risk of HIV (Deller et al., 2015; Chersich & Rees, 2010; Mthembu et al., 2014). Moreover, even within a woman’s established partnership, if she or her partner are using alcohol or other drugs, there is risk of partner violence and non-use of condoms (Chersich & Rees, 2010).
To reduce HIV transmission, condom use has been emphasized as a major component of HIV prevention, especially in high HIV prevalence settings. This includes condom use within main partnerships and/or condom use within other partnerships. Many couples are HIV discordant (Curran et al., 2012), and in partnerships where both partners are HIV negative the potential for extra-couple partnerships makes consistent condom use important (Chemaitelly et al., 2014).
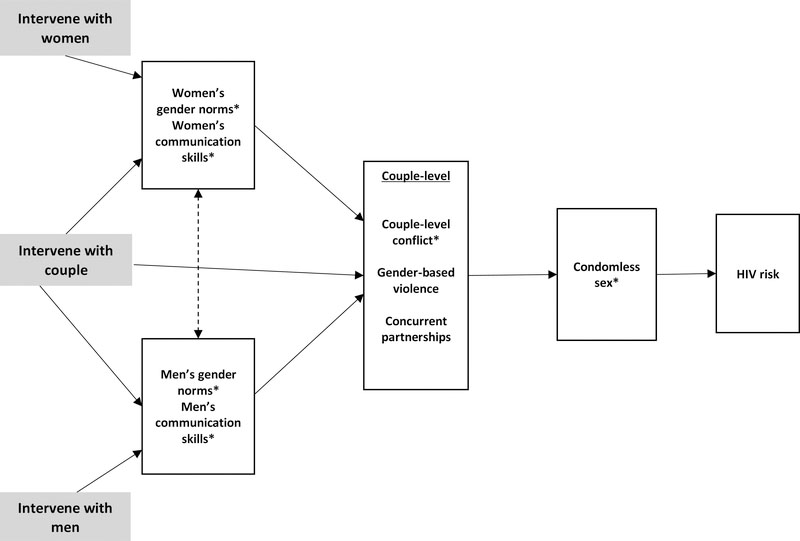
Given the importance of men to condom use and to the spread of HIV in South Africa and elsewhere, it is important to develop interventions targeted both to men and women, rather than just one member of the dyad, which typically is the woman (Karney, et al., 2010; Conroy et al. 2016). Programs that simply target women fail to recognize that in many cases, women lack the ability to negotiate condom use, especially if her partner has been drinking or has more economic and physical power in the relationship. Women-centered programs have typically addressed couple-level behaviors by encouraging the participant to talk to her partner about condom use (Karney et al., 2010). In a conceptual framework shown in Figure 1, programs that engage only the woman or only the man can influence gender norms and communication skills of each individual; these programs have an underlying expectation that each individual will influence his/her partner (the dotted line). By affecting individual-level norms and communication skills, this may lead to improved couple-level behaviors such as conflict resolution, reduced gender-based violence and reduced concurrent partnerships. These couple-level behaviors are related to condom use and subsequently HIV risk. An alternative approach is to engage both members of the partnership either through separate interventions or as a part of a couple-level program (Karney et al., 2010). In this case, both partners’ norms and communication skills are influenced, and this can lead to communal coping and improved behaviors of the couple (Lewis et al., 2006). What is still an outstanding research question is whether intervening with both partners separately or as a couple leads to better outcomes? In particular, reaching both partners jointly may lead more directly to behavior change as new skills gained can be role-played within the intervention and both partners are aware of what the other has learned about communication, problem-solving, risk-taking and prevention (see Figure 1). Alternatively, reaching both partners separately may ensure that both partners are learning about the importance of behavior change but in an environment that is safe to examine gender norms in more depth without feeling the pressure from one’s partner. This study examines the advantage of reaching both partners under the two varying scenarios.
Figure 1.
Conceptual framework of interventions with individuals versus couples and the effects on individual and couple-level HIV-related outcomes
Note: Starred items are the focus of this analysis
Three recent systematic reviews of HIV interventions—one focusing on heterosexual men in low- and middle-income countries (LMIC) (Townsend et al., 2013) and the other two focusing on heterosexual couple-based interventions (LaCroix et al., 2013)—demonstrate gaps in knowledge of how to affect men, women, and the couple’s behaviors related to HIV risk-taking. Among the 19 male-focused interventions in LMIC examined, less than half of the reviewed interventions increased condom use; these studies also yielded mixed effects on intimate partner violence (Townsend et al., 2013). In one review of couples, among the 29 couple-based interventions examined, only eight interventions were in Africa (LaCroix et al., 2013). These interventions showed increases in condom use with exposure to couple-based programming (LaCroix et al., 2013). Likewise, a systematic review by Crepaz and colleagues (2015) demonstrated that couple-based interventions are more effective than individual-level interventions at promoting protective sex. This provides empirical evidence that couple-based interventions can be more effective than individual level interventions just as interdependence theory would suggest (Lewis et al 2006; Rogers et al. 2016). A gap identified by one of these reviews is a need for future research that examines the efficacy of couple-level interventions on gender norms (LaCroix et al., 2013). Of note, among the African couple-level studies, only a small number examined couple-level outcomes; the remaining examined outcomes at the individual participant (male and/or female) level (LaCroix et al., 2013; Crepaz et al., 2015).
Evaluating couple-level programs by focusing on the behaviors of individuals in the couple fails to recognize that each partner influences the behaviors of the other either directly or indirectly (Karney et al., 2010; Kenny et al., 2006; Lewis et al., 2006). An alternative way to determine the effect of couple-level programming is to examine couple-level outcomes that account for joint attitudes or behaviors as reported by both partners (Karney et al., 2010; Kenny et al., 2006). These dyadic models also permit an assessment of whether one partner is less responsive to the intervention than the other. The present study compares the effects of intervening with both male and female partners in a couple jointly, intervening with the male and female partners separately, or intervening with only the female partner on couple-reported condom use, communication, conflict, and gender norms.
Method
This study was conducted in a large Black African community outside of the city center of Cape Town, South Africa. All study materials were reviewed and approved by the Institutional Review Board at RTI International and Stellenbosch University Faculty of Health Sciences granted ethical approval for the study. The study used a geographically cluster-randomized three-arm design to compare the effects of different strategies of intervening with couples on reductions in alcohol use, HIV risk, and IPV.
For this study, the target group was men who use alcohol and their female main partners. The intervention targeted men as the index case as this was an identified gap in earlier HIV prevention efforts. To identify this target group of men, project staff drove and walked through the community and geocoded the location of bars, taverns, and shebeens (i.e., informal drinking establishments) using handheld global positioning system (GPS) devices (Wechsberg et al., 2014). The GPS files were imported into ArcView and overlaid on a Google Earth map of the community.
To be eligible for the study, men had to be between 18 and 35 years of age, Black African, live in the study community, report drinking alcohol in a shebeen in the past three months and visiting shebeens often, been with their partner for at least a year; planning to stay with their partner for at least a year; not planning to get pregnant in the next year, report unprotected sex with their main partner in the past three months, and have a female partner who was also willing to be enrolled in the study (Wechsberg et al., 2016). Both the male and female partners were screened for eligibility separately and at the same time to avoid coercion. After screening of both partners by gender-matched project staff, the outreach team regrouped to determine eligibility and consistent responses from both partners to confirm that they were in a stable relationship. Given the fluidity of partnerships in South Africa (Crankshaw et al., 2016), a focus was put on including stable couples in this study rather than less stable couples. For this study, the definition of being in a stable relationship was that both partners had to separately report that they had been together for at least a year and they both had to plan on remaining in the partnership for another year. Recruitment for the study occurred between June 2010 and April 2012.
Interventions
This study had three arms that implemented different interventions. In the first arm, which is considered the comparison study arm, women received the Women’s Health CoOp (WHC) intervention and their male partners received HIV testing and counseling (HTC). Men in the comparison arm were offered HTC to ensure that they received some type of intervention at enrollment; these men did not receive any targeted behavior-change intervention besides counseling and testing. The WHC is an evidence-based behavioral intervention that, in previous studies, reduced sex risk behaviors among South African women who use drugs (Wechsberg et al., 2013). The WHC is a two session, four module program with seven core elements: (a) education on risk reduction strategies; (b) extensively trained peer interventionists; (c) skills training for risk reduction; (d) role-playing on negotiating safe sex and communication skills; (e) development of action plans to meet personalized goals; (f) HIV testing; and (g) referrals for other health services, as needed (Wechsberg et al., 2015a). In the second arm, women received the WHC and their male partners received a version adapted with elements from the Men as Partners program (Peacock & Levack, 2004), called the Men’s Health CoOp (MHC). The MHC was also delivered as a two-session, four module program and addressed similar risk reduction and communication skills as the WHC adapted from materials from the Men as Partners program (Wechsberg et al., 2015a). The MHC also included developing an action plan. In the third intervention arm, couples received the Couples Health CoOp (CHC), which is adapted using the WHC and other evidence-based programs for couples (El-Bassel et al., 2003; Wechsberg et al., 2015a). The CHC was also delivered as a two-session, four module program with couple-level role playing of risk reduction and communication skills and development of a joint action plan. The WHC/MHC/CHC all included behavior change strategies focused on couple communication, speaker-listener engagement, role play and rehearsal, and action plan development. Details of the content of the intervention and delivery mechanisms can be found elsewhere (Wechsberg et al., 2015a). Of note, for the comparison arm and one of the intervention arms, women and men received the intervention separately; whereas in the CHC arm, the intervention was delivered to couples in joint sessions.
The main study outcome effects for women and men separately were reported in detail previously (Wechsberg et al., 2016). In brief, at six-month follow-up, the couple-level intervention (CHC) significantly reduced men’s alcohol use, increased men’s reported consistent condom use, and reduced men’s reported number of unprotected sex acts, as compared with the comparison arm (Wechsberg et al., 2016). No differences were found between the separate implementation (WHC/MHC) and CHC arms for men’s outcomes and no differences were found for women across the arms on alcohol use, consistent condom use, and number of unprotected sex acts (women were exposed to an intervention in all arms: the WHC in the first and second arms and the couples’-level version in the CHC arm). In another analysis focused specifically on women, study authors demonstrated that women in the CHC arm compared to the comparison arm had increased relationship control and positive gender norms supporting female autonomy and women in the WHC/MHC compared to the CHC had greater relationship equity (Minnis et al., 2015b). The present study extends these earlier findings by examining the effect of the separate men’s and women’s intervention approach (WHC/MHC arm) compared with the couple-level intervention arm (CHC) and the comparison arm (WHC/HTC) on couple-level sex behavior, communication, conflict, and gender norm outcomes. Of note, each of the study outcomes is examined separately since we lack the statistical power to examine some outcomes (e.g., communication and norms) as mediators.
Analytic sample
A total of 299 couples participated in the initial enrollment and data collection (the full sample was 300; however, one man was missing relevant demographic information at baseline). By six-month follow-up, 267 couples completed participation and data collection; this comprised the analytic sample for this study. A small number of enrolled couples were dropped because they were missing at six-month follow-up (n=32) and, as appropriate, they were dropped if they were missing the relevant outcome variables. As shown in Table 1, there were few differences between the full sample enrolled and the reduced sample, which dropped couples with missing follow-up information; this suggests that missing data was at random. For this analysis, the sample comprised three groups of couples: couples in the comparison arm (n=84); couples in the WHC/MHC arm (n=85); and couples in the CHC arm (n=98). Table 1 demonstrates that randomization was effective at creating three groups similar on demographic factors.
Table 1.
Demographic characteristics of sample of couples included in Western Cape Couples Health CoOp Study by time and study arm, Cape Town, South Africa, 2010–2012
| Characteristic | Baseline Full Couples Sample (n=299) | Follow-up Couples Sample (n=267) | Follow-up Sample |
||
|---|---|---|---|---|---|
| Comparison (n=84) | WHC/MHC (n=85) | CHC (n=98) | |||
| Baseline mean age (Women) | 24.21 | 24.39 | 25.12 | 24.78 | 23.43 |
| Baseline mean age (Men) | 26.14 | 26.15 | 26.46 | 27.06 | 25.08† |
| Couple age | |||||
| Man 5+ years older than woman | 24.41 | 23.22 | 21.43 | 28.24 | 20.41 |
| Man within 4 years of woman (+/− 4 years) | 68.56 | 68.91 | 69.05 | 64.71 | 72.45 |
| Man 5+ years less than woman | 7.02 | 7.87 | 9.52 | 7.06 | 7.14 |
| Couple education | |||||
| Both no high school | 8.03 | 7.87 | 11.90 | 9.41 | 3.06 |
| Both some high school | 23.08 | 24.34 | 14.29 | 25.88 | 31.63 |
| Man less education than woman | 32.78 | 32.96 | 36.90 | 31.76 | 30.61 |
| Man more education than woman | 27.76 | 27.72 | 28.57 | 23.53 | 30.61 |
| Both more than high school | 8.36 | 7.12 | 8.33+ | 9.41 | 4.08 |
| Relationship to main partner (as reported by woman) | |||||
| Not living together | 72.74 | 70.04 | 70.24 | 70.59 | 69.39 |
| Married/cohabiting | 27.26 | 29.96 | 29.76 | 29.41 | 30.61 |
| % with running water (reported by woman) | 45.15 | 47.19 | 47.62 | 52.94 | 41.84 |
Note: Women in the comparison and WHC/MHC arms had the Women’s Health CoOp (WHC); Men’s Health CoOp (MHC); Couples Health CoOp (CHC). Significance testing controls for clustering using svy commands in Stata.
Indicates significant difference between WHC/MHC and CHC groups (p ≤ 0.05).
Indicates significant difference between Comparison and CHC groups (p ≤ 0.05).
Outcome measures
This study focuses on outcomes that are relevant at the couple level and examines all outcomes at the couple level at baseline and six-month follow-up. This means that all variables represent a comparison of the responses from the woman and man in the partnership. Outcomes examined include consistent condom use, partner communication, partner conflict, and gender norms.
Consistent condom use was based on whether each partner said that the number of times she or he used a condom in the past month with her/his main partner (i.e., the other partner of the dyad) was the same as the number of times he or she had sex in the past month with her/his main partner. The following categories were created: neither partner reported consistent condom use in the past month; only the woman reported consistent condom use in the past month; only the male partner reported consistent condom use in the past month; and both partners reported consistent condom use in the past month. Notably, in some cases, the woman or man was missing information on the number of sex acts and/or number of times a condom was used in the past month. For these couples, we coded the responses (at baseline or six-month follow-up) based only on the partner that had the information (i.e., these cases will fall in the neither, woman-only, or man-only categories).
Partner communication around HIV risk was based on two separate items: whether the woman and man reported at baseline and six-month follow-up that they had asked their partner in the past six months to use a condom; and if in the past six months they asked their partner how many partners he or she has had. For both questions, we created four categories: neither asked, woman only asked, man only asked, and both asked.
For the conflict variable, women and men were asked if they ever had an argument or conflict with their partner; and if so, when was the last time. For those who ever experienced a lifetime argument or conflict, they were recoded as experiencing a recent argument or conflict if they reported that the last time was within the past three months. A joint outcome was created with four categories: neither reported conflict in the past three months, woman only reported conflict in the past three months, man only reported conflict in the past three months, and both reported conflict in the past three months.
Finally, the gender norms outcome was created based on three statements where a respondent was asked if he or she agrees, partially agrees, or does not agree. The statements were (1) “A man needs other women even if things with his main partner/wife are fine,” (2) “A woman should tolerate violence in order to keep her family together,” and (3) “I would be angry if my partner asked me to use a condom.” Those who responded that they disagree were coded as one on each item. The responses were summed and the score was recoded as dichotomous such that if a person disagreed with all statements (a score of 3) he or she was coded as having positive gender norms (coded 1); all others were coded as zero. A joint couple-level outcome was created: neither the man nor the woman reported positive gender norms, woman only reported positive gender norms, man only reported positive gender norms, both the man and the woman reported positive gender norms.
Analyses
We used cross-tabulations with Pearson’s F-tests to determine if the intervention and comparison groups differed at baseline and endline on the study outcomes, and controlled for the clustered design. For the multivariate analyses, since each of the outcomes had four response options, multinomial logistic regression was used to assess intervention effects. All multivariate results controlled for the couple’s age, the couple’s education, the relationship status (as reported by the woman), and whether there was running water in the household (as reported by the woman) and adjusted for study clustering using the svy commands in Stata statistical software. (See Table 1 for the classification of these control variables.) The models included the baseline level of the outcome (e.g., consistent condom use at baseline or gender norms at baseline). The analyses were restricted to couples with full information for each of the outcomes at baseline and six-month follow-up. Of note, multiple imputation was used to examine the results with full information and the results did not differ significantly; where differences are observed, they are noted in the text.
Results
Table 1 presents the descriptive characteristics of the study sample; few differences are observed between the baseline sample of couples surveyed (n=299) and the matched sample with follow-up information (n=267). In the matched sample, the average age among women is 24 years and the men are slightly older at 26 years. Two-thirds of women and men are within a similar age group (i.e., within four years of one another) and for about a quarter of the couples the man is five or more years older than the woman). For more than 50% of the couples there is a distinction in the education levels between the partners; in about half of these cases, the woman is more educated than the man and in the other half, the man is more educated than the woman. A majority of couples are not living together; in only about 30% of the cases did the woman report that she lives with her main partner. Finally, a little less than half of the women report having running water in the house; this is not surprising given the study setting, a targeted large disadvantaged community in Cape Town. Overall, randomization resulted in few demographic differences between the three study arms. The only distinctions found were that the men in the CHC arm were significantly younger than the men in the WHC/MHC arm (25.08 years vs. 27.06 years, respectively; p<0.05) and there were couple level education differences between the comparison group and the CHC group.
Table 2 presents the outcomes at baseline and six-month follow-up by the study intervention arm and shows the number of observations with complete information on the outcome at each time period. As mentioned earlier, each of the outcomes was coded as neither partner, woman only, man only, or both partners. At baseline, with the exception of consistent condom use, there were no differences in the outcomes by study condition. Overall, at baseline, among most of the couples, neither partner reported consistent condom use (ranges from 70% to 78%). Differences were observed across the three arms (p=0.046) such that at baseline, men in the CHC arm reported less condom use (man only reported is 5.2%) than in the other arms. By six-month follow-up, there is an increase in reported consistent condom use in all three arms. At follow-up, the CHC arm has significantly higher reported consistent condom use by both partners (26%) and men only (25%) than the comparison arm (19% and 9%, respectively; p<0.05).
Table 2.
Relevant outcomes by intervention group at baseline and 6-month follow-up for sample with full information on outcome at both time points
| Baseline | 6-month Follow-up | |||||||
|---|---|---|---|---|---|---|---|---|
| Comparison | WHC/MHC | CHC | p-value* | Comparison | WHC/MHC | CHC | p-value* | |
| Reported consistent condom use in past montha | (n=79) | (n=84) | (n=96) | 0.046 | (n=79) | (n=84) | (n=96) | 0.129 |
| Neither report use | 69.62 | 75.00 | 78.13 | 40.51 | 33.33 | 29.17 | ||
| Woman only | 8.86 | 4.76 | 15.63 | 31.65 | 26.19 | 19.79 | ||
| Man only | 18.99 | 17.86 | 5.21 | 8.86 | 21.43 | 25.00 | ||
| Both report use | 2.53+ | 2.38 | 1.04† | 18.99+ | 19.05 | 26.04 | ||
| In past 6 months, asked partner to use condom | (n=78) | (n=77) | (n=94) | 0.574 | (n=78) | (n=77) | (n=94) | 0.093 |
| Neither | 19.23 | 19.48 | 22.34 | 10.26 | 6.49 | 6.38 | ||
| Woman only | 25.64 | 33.77 | 24.47 | 35.90 | 22.08 | 17.02 | ||
| Man only | 20.51 | 22.08 | 27.66 | 7.69 | 23.38 | 21.28 | ||
| Both | 34.62 | 24.68 | 25.53 | 46.15+ | 48.05 | 55.32 | ||
| In past 6 months, asked partner how many sexual partners she or he had | (n=78) | (n=77) | (n=94) | 0.427 | (n=78) | (n=77) | (n=94) | 0.256 |
| Neither | 21.79 | 23.38 | 27.66 | 11.54 | 15.58 | 6.38 | ||
| Woman only | 37.18 | 37.66 | 26.60 | 35.90 | 18.18 | 25.53 | ||
| Man only | 14.10 | 19.48 | 24.47 | 11.54 | 19.48 | 23.40 | ||
| Both | 26.92 | 19.48 | 21.20 | 41.03 | 46.75 | 44.68 | ||
| Reported partner conflict in past 3 months | (n=76) | (n=76) | (n=94) | 0.734 | (n=76) | (n=76) | (n=94) | 0.362 |
| Neither report | 15.79 | 17.11 | 11.70 | 31.58 | 35.53 | 27.66 | ||
| Woman only | 23.68 | 17.11 | 19.15 | 39.47 | 21.05 | 39.36 | ||
| Man only | 26.32 | 23.68 | 31.91 | 13.16 | 19.74 | 13.83 | ||
| Both | 34.21 | 42.11 | 37.23 | 15.79 | 23.68 | 19.15 | ||
| Positive gender normsb | (n=83) | (n=83) | (n=98) | 0.471 | (n=83) | (n=83) | (n=98) | 0.000 |
| Neither has positive norms | 30.12 | 22.89 | 17.35 | 26.51 | 13.25 | 16.33 | ||
| Woman only | 32.53 | 36.14 | 45.92 | 38.55 | 39.76 | 20.41 | ||
| Man only | 15.66 | 14.46 | 11.22 | 21.69 | 9.64 | 9.18 | ||
| Both have positive norms | 21.69 | 26.51 | 25.51 | 13.25+ | 37.35 | 54.08† | ||
Note:
Pearson F-test p-value controlling for clustering.
Some couples with missing data from one partner were recoded based on available information.
Gender norms coded based on three questions, see text for details. MHC=Men’s Health CoOp; CHC=Couples Health CoOp.
Indicates significant difference between WHC/MHC and CHC arms (p ≤ 0.05).
Indicates significant difference between Comparison and CHC arms (p ≤ 0.05).
For couple communication, at baseline there was no difference by arm in asking the partner to use a condom or asking the partner how many sexual partners she or he has had. At six-month follow-up, the percentage of couples where both partners said they asked their partner about condom use or other sexual partners increased in all three arms. At follow-up, the CHC arm had significantly higher reported communication about condoms by both partners and men only than the comparison arm (p<0.05). For example at follow-up, for 55.3% of couples in the CHC both partners reported asking to use condoms and for 21.3% of couples the man only reported asking to use condoms; the respective values for the comparison arm were 46.2% and 7.7%. Of note, reported discussion of condom use (or discussion of other sexual partners, or consistent condom use, or conflict) may differ between partners because of multiple reasons including: a) reporting bias such that one partner chooses to not report the behavior when it happened; b) one partner thinking she/he discussed something when the other did not perceive the discussion to have taken place; or c) differential memory of events. With the data available, we cannot know why there are some behaviors with differing reports by partners for joint behaviors such as condom discussion and condom use.
In more than 80% of couples at baseline, one or both partners reported partner conflict in the past three months. No difference was observed by arm. At six-month follow-up, recent partner conflict had declined; however, the decline was observed in all arms, with no significant differences by arm.
The last outcome presented in Table 3 is gender norms. Having positive gender norms at baseline did not differ by arm, and for about a quarter of couples, both partners reported positive gender norms. At baseline, a third or more of women reported having positive gender norms when their partner did not report the same. At six-month follow-up, there were improvements in positive gender norms at the couple level (e.g., both partners report positive norms) particularly in the WHC/MHC and CHC arms. The difference across all three arms was significant (p≤0.001) and significant differences (p<0.05) between the CHC and the comparison arm and between the CHC and the WHC/MHC arm were also found. Given the extensive attention paid to equitable gender norms as part of the CHC/WHC/MHC, it is not surprising to see these norms change; behavior change, however takes longer to observe.
Table 3.
Multivariate multinomial logistic regression coefficients (standard errors) examining couple’s reported asking partner the number of partners she or he has at 6-month follow-up interview
| Woman only reports asking vs. Neither partner reports asking | Man only reports asking vs. Neither partner reports asking | Both partners report asking vs. Neither partner reports asking | Both partners report asking vs. Man only reports asking | Both partners report asking vs. Woman only reports asking | |
|---|---|---|---|---|---|
| Baseline report of asking partner how many partners she or he has had | |||||
| Neither report (REF) | --- | --- | --- | --- | --- |
| Woman only reports | −0.20 (0.45) | −0.11 (0.69) | −0.10 (0.47) | 0.01 (0.50) | 0.11 (0.40) |
| Man only reports | −0.31 (0.73) | 0.30 (0.75) | 0.33 (0.56) | 0.03 (0.57) | 0.64 (0.47) |
| Both report | 2.06 (1.01)* | 2.45 (1.09)* | 2.51 (0.95)* | 0.06 (0.60) | 0.45 (0.39) |
| Intervention condition | |||||
| Comparison (REF) | --- | --- | --- | --- | --- |
| WHC/MHC | −0.79 (0.64) | 0.52 (0.55) | 0.15 (0.74) | −0.37 (0.68) | 0.94 (0.55)+ |
| CHC | 0.48 (0.76) | 1.67 (0.50)** | 1.00(0.65) | −0.66(0.56) | 0.52 (0.54) |
Note:
p ≤ 0.10
p ≤ 0.05
p ≤ 0.01
p ≤ 0.001.
Number of couples = 248. MHC=Men’s Health CoOp; CHC=Couples Health CoOp. Model controls for couple-level age, education, living arrangement, and whether there is running water in the house.
Tables 3–7 present the multivariate multinomial logistic regression results for five outcomes at six-month follow-up. To simplify the presentation of the results, control variables including couple age, couple education, living arrangement, and having running water in the house are not shown. All multivariate models control for baseline experience on the relevant outcome.
Table 7.
Multivariate multinomial logistic regression coefficients (standard errors) of consistent condom use with main partner among couples at 6-month follow-up interview
| Woman only reports consistent use vs. Neither partner reports consistent use | Man only reports consistent use vs. Neither partner reports consistent use | Both partners report consistent use vs. Neither partner reports consistent use | Both partners report consistent use vs. Man only reports consistent use | Both partners report consistent use vs. Woman only r eports consistent use | |
|---|---|---|---|---|---|
| Baseline consistent condom use | |||||
| One/both report consistent use (REF) | --- | --- | --- | --- | --- |
| Neither report consistent use | −0.01 (0.39) | −0.14 (0.34) | −0.06 (0.36) | 0.08 (0.40) | −0.04 (0.38) |
| Intervention condition | |||||
| Comparison (REF) | --- | --- | --- | --- | --- |
| WHC/MHC | 0.08 (0.43) | 1.17 (0.54)* | 0.37 (0.57) | −0.80 (0.61) | 0.29 (0.46) |
| CHC | −0.08 (0.45) | 1.40 (0.52)* | 0.83 (0.48)+ | −0.58 (0.51) | 0.91 (0.53)+ |
Note:
p ≤ 0.10
p ≤ 0.05
p ≤ 0.01
p ≤ 0.001.
Number of couples = 259. MHC=Men’s Health CoOp; CHC=Couples Health CoOp. Model controls for couple-level age, education, living arrangement, and whether there is running water in the house.
In Table 3, couples in the CHC arm were more likely than those in the comparison arm to have men only report that they asked their partner about the number of sexual partners compared with neither partner asking about sexual partners. There were no differences in couple communication about sex partners by study arm in the other comparisons. This is not unexpected given the bivariate results presented earlier. That said, couples where both partners reported asking about the number of partners at baseline were significantly more likely to be in the woman only, man only or both partners asked about sexual partners groups than in the neither partner asked group at six-month follow-up, compared with couples where neither partner asked about partners at baseline. Note that the baseline effects were attenuated in the imputed models whereby both reporting asking at baseline was only significantly (p≤0.05) associated with both partners asking at follow-up (vs. neither).
Table 4 presents the results on communication about condom use in the last six months. Couples in the CHC arm were more likely to have men only report discussing condom use compared with couples in the comparison group who were more likely to be in the group where neither partner reported asking. A similar effect was found for asking to use condoms for couples in the WHC/MHC arm compared with the comparison arm. Further, the coefficients in the comparison between both partners reported asking to use a condom compared to the man only asking to use a condom were negative, indicating that those couples where the men were exposed to a program (either WHC/MHC or CHC), were significantly more likely to have the man only report asking for condom use than both partners reporting asking to use a condom compared to the comparison group. (Note that for this comparison, the effect of the CHC did not attain significance at p≤0.10 in the imputed results). Finally, couples in the CHC arm compared with the comparison arm were more likely to have both partners report asking to use a condom than the woman only asking to use condoms.
Table 4.
Multivariate multinomial logistic regression coefficients (standard errors) of reported asking partner to use a condom among couples at 6-month follow-up interview
| Woman only reports asking to use a condom vs. Neither partner reports asking | Man only reports asking to use a condom vs. Neither partner reports asking | Both partners report asking to use a condom vs. Neither partner reports asking | Both partners report asking to use a condom vs. Man only reports asking | Both partners report asking to use a condom vs. Woman only reports asking | |
|---|---|---|---|---|---|
| Baseline reported asking to use a condom | |||||
| Neither report asking to use a condom (REF) | --- | --- | --- | --- | --- |
| Woman only reports asking | 0.01 (0.77) | −0.58 (0.97) | 0.81 (0.73) | 1.39 (0.64)* | 0.80 (0.59) |
| Man only reports asking | 0.57 (0.86) | 0.91 (0.92) | 1.38 (0.88) | 0.47 (0.54) | 0.81 (0.70) |
| Both report asking to use a condom | 1.14 (0.65)+ | 1.20 (0.73) | 1.45 (0.59)* | 0.25 (0.54) | 0.31 (0.51) |
| Condition | |||||
| Comparison (REF) | --- | --- | --- | --- | --- |
| WHC/MHC | 0.20 (0.61) | 1.90 (0.79)* | 0.70 (0.83) | −1.20 (0.53)* | 0.50 (0.54) |
| CHC | 0.00 (0.63) | 1.79 (0.80)* | 0.97 (0.72) | −0.82 (0.45)+ | 0.97 (0.42)* |
Note:
p ≤ 0.10
p ≤ 0.05
p ≤ 0.01
p ≤ 0.001.
Number of couples = 248. MHC=Men’s Health CoOp; CHC=Couples Health CoOp. Model controls for couple-level age, education, living arrangement, and whether there is running water in the house.
Table 5 demonstrates that controlling for baseline gender norms of the couple, couples in the WHC/MHC and the CHC arms were significantly more likely than couples in the comparison arm to both report positive gender norms at six-month follow-up than neither partner reporting positive gender norms at follow-up. Further, assignment to study arms that exposed men to interventions (WHC/MHC and CHC) was also linked to both partners reporting positive gender norms, compared with just the woman or just the man reporting positive gender norms; in these comparisons, there was a significantly bigger effect of the CHC than the WHC/MHC. It is notable that the WHC/MHC and CHC do not increase the likelihood that the couple will be in the only one partner has positive norms category versus the neither partner has positive gender norms category. Notably, couples where both partners have a high school education or higher were the most likely to have either one partner or both partners report positive gender norms at six-month follow-up, compared with couples with no education, controlling for baseline gender norms. Further, couples where the male partner was younger than the female partner by five or more years were less likely to have one partner or both partners report positive gender norms.
Table 5.
Multivariate multinomial logistic regression coefficients (standard errors) of equitable gender norms among couples at 6-month follow-up interview
| Woman only reports positive norms vs. Neither partner reports positive norms | Man only reports positive norms vs. Neither partner reports positive norms | Both partners report positive norms vs. Neither partner reports positive norms | Both partners report positive norms vs. Man only reports positive norms | Both partners report positive norms vs. Woman only reports positive norms | |
|---|---|---|---|---|---|
| Baseline gender norms | |||||
| Neither positive (REF) | --- | --- | --- | --- | --- |
| Woman only positive | 1.12 (0.48)* | 1.02 (0.40)* | 0.69 (0.36)+ | −0.33 (0.39) | −0.43 (0.56) |
| Man only positive | 1.58 (0.64)* | 0.61 (0.77) | 1.45 (0.51)** | 0.84 (0.69) | −0.13 (0.62) |
| Both positive | 0.83 (0.53) | 0.18 (0.58) | 0.61 (0.45) | 0.44 (0.54) | −0.22 (0.47) |
| Intervention condition | |||||
| Comparison (REF) | --- | --- | --- | --- | --- |
| WHC/MHC | 0.56 (0.52) | −0.25 (0.68) | 1.66 (0.55)** | 1.91 (0.58)** | 1.10 (0.45)* |
| CHC | −0.24 (0.44) | 0.46 (0.55) | 1.98 (0.46)*** | 2.44 (0.46)*** | 2.22 (0.40)*** |
Note:
p ≤ 0.10
p ≤ 0.05
p ≤ 0.01
p ≤ 0.001.
Gender norms coded based on three questions, see text for details. Number of couples = 264. MHC=Men’s Health CoOp; CHC=Couples Health CoOp. Model controls for couple-level age, education, living arrangement, and whether there is running water in the house.
Table 6 presents the multivariate results of reported conflict in the last three months. Couples in the WHC/MHC arm compared to the comparison arm were more likely at six-month follow-up to have both members report conflict than the woman only report conflict. No other differences were found across the comparisons and intervention groups.
Table 6.
Multivariate multinomial logistic regression coefficients (standard errors) of reported conflict in last three months among couples at 6-month follow-up interview
| Woman only reports conflict vs. Neither partner reports conflict | Man only reports conflict vs. Neither partner reports conflict | Both partners report conflict vs. Neither partner reports conflict | Both partners report conflict vs. Man only reports conflict | Both partners report conflict vs. Woman only reports conflict | |
|---|---|---|---|---|---|
| Baseline reported conflict | |||||
| Neither report conflict (REF) | --- | --- | --- | --- | --- |
| Woman only reports conflict | 0.73 (0.70) | 0.12 (0.64) | 0.47 (0.76) | 0.35 (0.70) | −0.26 (0.79) |
| Man only reports conflict | 0.10 (0.62) | −0.35 (0.65) | −0.05 (0.56) | 0.29 (0.72) | −0.16 (0.67) |
| Both report conflict | 0.52 (0.57) | −0.76 (0.56) | −0.08 (0.63) | 0.68 (0.72) | −0.60 (0.73) |
| Intervention condition | |||||
| Comparison (REF) | --- | --- | --- | --- | --- |
| WHC/MHC | −0.72 (0.52) | 0.46 (0.50) | 0.38 (0.58) | −0.07 (0.65) | 1.11 (0.47)* |
| CHC | 0.12 (0.49) | 0.36 (0.71) | 0.34 (0.61) | −0.03 (0.64) | 0.22 (0.46) |
Note:
p ≤ 0.10
p ≤ 0.05
p ≤ 0.01
p ≤ 0.001.
Number of couples = 246. MHC=Men’s Health CoOp; CHC=Couples Health CoOp. Model controls for couple-level age, education, living arrangement, and whether there is running water in the house.
Finally, Table 7 presents the couple-level outcome on consistent condom use. For consistent condom use, couples in the CHC arm were more likely to be in the group where the man only reports consistent condom use than neither partner reports consistent condom use, as compared with couples in the comparison arm. Likewise, for couples in the WHC/MHC arm compared to the comparison arm there was greater consistent condom use reported by the man only than neither partner reporting condom use.
Discussion
Prior HIV prevention programs often target just one member of a dyad, usually the woman, ignoring that much of HIV risk, especially in South Africa, involves heterosexual relations and the behaviors of the woman and her partner (Karney et al., 2010; Conroy et al., 2016). Programs that intervene with just one partner to change gender norms, communication skills, and promote condom use are assuming that participants will engage their partners to influence behaviors at the couple level. This may be a strong assumption, especially in a context like South Africa where there are high rates of gender-based violence and alcohol use (Kalichman et al., 2005) and traditional gender norms that accept men having the power in relationships and expecting men to have multiple sex partners (Sawyer et al., 2006). In these contexts, it is important to engage the men, and even better, engage both women and men. This study was unique as it examined the advantages of engaging women and men and whether engaging them jointly or separately has added benefit over just engaging women.
Further, among earlier studies that have evaluated couple-level interventions, many examine outcomes at the individual level (LaCroix et al., 2013; Crepaz et al., 2015; Minnis et al., 2015b; Wechsberg et al., 2016; El-Bassel et al., 2003; Kraft et al., 2007). This approach ignores that partners can affect one another and that interventions may be more effective for one partner than another (Lewis et al., 2006; Karney et al., 2010). By examining a joint outcome, it is possible to examine differential effects on both members of the couple.
This study begins to address these issues by examining the effect of varying strategies of engaging women and men around HIV prevention and improved couple interactions, and demonstrates distinctions by whether both partners are engaged individually (e.g., women receive the WHC and men receive the MHC) or jointly (couple receives CHC). Notably, couples exposed to the CHC had more positive gender norms at six-month follow-up, such that both partners had positive norms, as compared with neither partner or only one partner having positive norms in the comparison group. Further, assignment to the WHC/MHC was also found to be related to improved gender norms among couples, as compared with neither partner or only one partner having positive gender norms. Finally, assignment to the CHC and WHC/MHC were related to both partners having positive gender norms, as compared with only one partner having positive gender norms; however, the effect was bigger for couples in the CHC arm. These gender effects suggest the importance of engaging both partners to attain positive gender norms at the couple level. The interventions offered (WHC, MHC, and CHC) all included extensive empowerment and communication skills building activities and messages. These approaches were targeting changing gender norms and behaviors, however, only norms were significantly affected across all groups in the six-month follow-up period. These improvements in positive gender norms in the WHC/MHC and CHC arms may ultimately translate into decreases in having multiple sex partners, increases in condom use, and reductions in IPV. However, it would require a much larger sample size and a longer follow-up period to confirm these potential effects.
The CHC and WHC/MHC intervention was also found to be related to greater men’s communication on condom use and men’s reported consistent condom use compared to neither partner reporting communication on condom use or reporting consistent condom use than couples in the comparison arm. These are positive outcomes related to engaging men and couples in these gender-focused interventions. Notably, because the comparison arm had the WHC, this study demonstrates strong effects on men’s reported discussion and consistent condom use when men are engaged as part of the program either separately or as part of a couple, rather than women being engaged alone (comparison arm). The findings are consistent with interdependence theory and communal coping approaches. According to these dyadic models, couple-level interventions may work by enhancing communal coping or have a direct effect on one member’s behavior (Lewis et al 2006). In this instance, the intervention appears to have had a direct effect on men’s behavior rather through communal coping. Of note, men are more likely to report the behaviors at follow-up, however, comparable increases are not found in women’s reported behaviors. This may reflect either over-reporting by men or under-reporting by women. With the data available we cannot determine whether one partner is more reliable than the other. That said, men’s higher reported consistent condom use, whether true or not, may reflect changing norms and expectations for consistent condom use which could be a precursor to behavior change over the longer term.
This study extends previous work that examined the effect of the WHC/MHC and CHC (Wechsberg et al., 2016; Minnis et al., 2015b) by assessing outcomes at the couple level. Prior studies have demonstrated effects of the CHC and MHC on heavy alcohol use, consistent condom use, and unprotected sex among men, with no additional effect among women because all women were exposed to some form of an intervention (either WHC or CHC) across the groups (Wechsberg et al., 2016). Further, an analysis of the three intervention arms on women’s reported relationship power, communication and violence demonstrated that women in the CHC arm compared to the WHC arm had increased relationship control and positive gender norms supporting female autonomy and women in the WHC/MHC compared to the CHC had greater relationship equity (Minnis et al., 2015b). Similarly, other studies of couple-based programming often examine outcomes at the individual partner level or at both the couple level and individual level (Harvey et al., 2009; LaCroix et al., 2013; Crepaz et al., 2015). Common outcomes in these studies are condom use and partner concurrency (LaCroix et al., 2013); however, gaps have been identified in understanding the role of couple-based programming on gender roles (LaCroix et al., 2013). This was a strength of the current study that examined the effect of the couple-based intervention and the separate women’s and men’s intervention on positive gender norms and found strong significant effects at the couple level.
Limitations
The relatively small sample reduces statistical power for detecting small differences. Nevertheless, the WHC/MHC and CHC arms performed better than the comparison arm on gender norms of the couple and the WHC/MHC and CHC arms performed better for men’s reported condom use discussion and consistent condom use. Also, the outcomes rely on self-reported data, which is subject to social desirability and recall errors. Nonetheless, prior reviews concluded that the reliability and validity of self-reports of sex behaviors are acceptable (Darke, 1998; Weinhardt et al., 1998). There is also a potential bias with the measure of consistent condom use. In this study, consistent condom use is defined based on sexual behaviors in the last month with the main partner (number of times had sex and number of times used a condom). This measure does not capture whether each partner had outside partners which affects the need for consistent condom use. This is a limitation of this study. Further, this study is based on secondary data and therefore it was limited by the timeframe within which the questions were asked. Thus, some questions referred to the last month (consistent condom use) and others to the last three months (conflict) or last six months (discussion of condom use). While these time frames vary, each captures what is feasible to measure and present possible changes that might be seen at six-month follow-up. Additionally, because to be part of this study, men had to report drinking alcohol and having unprotected sex with their main partner, the results may not be generalizable to men who do not drink or to single men. Finally, this study was conducted in one large Black African community in Cape Town, South Africa, and may not generalize to other communities. However, the overall eligibility attributes make the men and couples in this study important for HIV prevention interventions to reduce HIV in South Africa.
Conclusion
Intervening with both partners in a couple had a greater impact on gender attitudes and men’s reported condom discussion and use than intervening with only the woman, which has been the focus of many previous HIV prevention interventions. Further, intervening with both partners jointly and not just as part of separate interventions had the strongest effect on positive gender norms. Future research will need to assess the cost and cost-effectiveness and the logistical feasibility of intervening with both partners jointly and men and women separately, instead of only the woman since engaging both partners adds challenges with recruitment and follow-up (Karney et al., 2010). Research will also need to consider pre-exposure prophylaxis (PrEP) and ARV treatment goals for HIV serodiscordant or concordant negative or concordant positive couples because couple-level biobehavioral interventions will be considered a more comprehensive toolkit.
Acknowledgements
This research was supported by the U.S. National Institutes of Health, National Institute on Alcohol Abuse and Alcoholism (NIAAA) grant R01 AA018076. The views and conclusions are those of the authors and do not necessarily reflect the views of NIAAA. The funding agency had no role in the research design; in the collection, analysis, and interpretation of the data; in the writing of this article, or in the decision to submit the article for publication. The authors would like to thank Jeffrey Novey for editorial assistance.
References
- Browne FA, & Wechsberg WM (2010). The intersecting risks of substance use and HIV risk among substance-using South African men and women. Current Opinion in Psychiatry, 23, 205–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Case KK, Ghys PD, Gouws E, Eaton JW, Borquez A, Stover J, Cuchi P, Abu-Raddad LJ, Garnett GP, Hallett TB (2012). Understanding the modes of transmission model of new HIV infection and its use in prevention planning. Bulletin of the World Health Organization, 90, 831–838A. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chemaitelly H, Awad SF, Shelton JD, & Abu-Raddad LJ (2014). Sources of HIV incidence among stable couples in sub-Saharan Africa. Journal of the International AIDS Society, 17, 18765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chersich MF, & Rees HV (2010). Causal links between binge drinking patterns, unsafe sex and HIV in South Africa: its time to intervene. International Journal of STD and AIDS, 21, 2–7. [DOI] [PubMed] [Google Scholar]
- Conroy AA, McGrath N, Van Rooyen H, Hosegood V, Johnson MO, Fritz K, Marr A, Ngubane T & Darbes LA (2016). Power and the association with relationship quality in South African couples: implications for HIV/AIDS interventions. Social Science & Medicine. 153:1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crankshaw TL, Voce A, Butler LM, & Darbes L (2016). Expanding the relationship contxt for couple-based HIV prevention: elucidating women’s perspectives on non-traditional sexual partnerships. Social Science & Medicine. 166: 169–176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crepaz N, Tungol-Ashmon MV, Vosburgh HW, Baack BN, Mullins MM (2015). Are couple-based interventions more effective than interventions delivered to individuals in promoting HIV protective behaviors? A meta-analysis. AIDS Care, 27, 1361–1366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curran K, Baeten JM, Coates TJ, Kurth A, Mugo NR, & Celum C (2012). HIV-1 prevention for HIV-1 serodiscordant couples. Current HIV/AIDS Reports, 9, 160–170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Darke S (1998). Self-report among injecting drug users: a review. Drug and Alcohol Dependence, 51, 253–263; discussion 267–258. [DOI] [PubMed] [Google Scholar]
- Dellar RC, Dlamini S, Abdool Karim Q (2015). Adolescent girls and young women: key populations for HIV epidemic control. Journal of the International AIDS Society, 18, 64–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dworkin SL, Hatcher AM, Colvin C, & Peacock D (2013). Impact of a gender-transformative HIV and antiviolence program on gender ideologies and masculinities in two rural, South African communities. Men and Masculinities, 16, 181–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- El-Bassel N, Witte SS, Gilbert L, Wu E, Chang M, Hill J, et al. (2003). The efficacy of a relationship-based HIV/STD prevention program for heterosexual couples. American Journal of Public Health, 93, 963–969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harvey SM, Kraft JM, West SG, Taylor AB, Pappas-Deluca KA, & Beckman LJ (2009). Effects of a health behavior change model--based HIV/STI prevention intervention on condom use among heterosexual couples: a randomized trial. Health Education and Behavior, 36, 878–894. [DOI] [PubMed] [Google Scholar]
- Kalichman SC, Simbayi LC, Kaufman M, Cain D, Cherry C, Jooste S, et al. (2005). Gender attitudes, sexual violence, and HIV/AIDS risks among men and women in Cape Town, South Africa. Journal of Sex Research, 42, 299–305. [DOI] [PubMed] [Google Scholar]
- Karney BR, Hops H, Redding CA, Reis HT, Rothman AJ, Simpson JA (2010). A framework for incorporating dyads in models of HIV prevention. AIDS Behavior, 14, S189–S203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kenny DA, Kashy DA, Cook WL (2006). Dyadic Data Analysis. New York: The Guilford Press. [Google Scholar]
- Kraft JM, Harvey SM, Thorburn S, Henderson JT, Posner SF, Galavotti C (2007). Intervening with couples: assessing contraceptive outcomes in a randomized pregnancy and HIV/STD risk reduction intervention trial. Women’s Health Issues, 17, 52–60. [DOI] [PubMed] [Google Scholar]
- LaCroix JM, Pellowski JA, Lennon CA, & Johnson BT (2013). Behavioural interventions to reduce sexual risk for HIV in heterosexual couples: a meta-analysis. Sexually Transmitted Infections, 89, 620–627. [DOI] [PubMed] [Google Scholar]
- Lewis MA, McBride CM, Pollak KI, Puleo E, Butterfield RM, Emmons KM. (2006). Understanding health behavior change among couples: an interdependence and communal coping approach. Social Science & Medicine. 62, 1369–80. [DOI] [PubMed] [Google Scholar]
- Minnis AM, Doherty IA, Kline TL, Zule WA, Myers B, Carney T, Wechsberg WM (2015). Relationship power, communication, and violence among couples: results of a cluster-randomized HIV prevention study in a South African township. International Journal of Women’s Health. 7: 517–525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mthembu J, Simbayi L, Onoya D, Jooste S, Mehlomakulu V, Mwaba K, et al. (2014). Sexism, intimate partner violence and risk behavior amongst men in a South African township Violence and Gender, 1, 53–59. [Google Scholar]
- Peacock D, & Levack A (2004). The men as partners program in South Africa: Reaching men to end gender-based violence and promote sexual and reproductive health. International Journal of Men’s Health, 3, 173–188. [Google Scholar]
- Rogers AJ, Achiro L, Bukusi EA, Hatcher AM, Kwena Z, Musoke PL, Turan JM, Weke E, Darbes LA (2016). Couple interdependence impacts HIV-related health behaviors among pregnant couples in southwestern Kenya: a qualitative analysis. Journal of the International AIDS Society, 19, 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sawyer KM, Wechsberg WM, & Myers BJ (2006). Cultural similarities and differences between a sample of Black/African and Coloured women in South Africa: convergence of risk related to substance use, sexual behavior, and violence. Women and Health, 43, 73–92. [DOI] [PubMed] [Google Scholar]
- Shaikh N, Abdullah F, Lombard CJ, Smit L, Bradshaw D, & Makubalo L (2006). Masking through averages--intraprovincial heterogeneity in HIV prevalence within the Western Cape. South African Medical Journal, 96, 538–543. [PubMed] [Google Scholar]
- Shisana O, Ramlagan S, Rehle T, Mbelle N, Simbayi LC, Zuma K, et al. (2014). South African National HIV Prevalence, Incidence and Behaviour Survey, 2012. Cape Town: HSRC Press. [Google Scholar]
- Shuper PA, Neuman M, Kanteres F, Baliunas D, Joharchi N, & Rehm J (2010). Causal considerations on alcohol and HIV/AIDS--a systematic review. Alcohol and Alcoholism, 45, 159–166. [DOI] [PubMed] [Google Scholar]
- Townsend L, Mathews C, & Zembe Y (2013). A systematic review of behavioral interventions to prevent HIV infection and transmission among heterosexual, adult men in low-and middle-income countries. Prevention Science, 14, 88–105. [DOI] [PubMed] [Google Scholar]
- Wechsberg WM, Doherty IA, Myers B, Morgan-Lopez AA, Emanuel A, Carney T, et al. (2014). Contextualizing gender differences and methamphetamine use with HIV prevalence within a South African community. International Journal on Drug Policy, 25, 583–590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wechsberg WM, El-Bassel N, Carney T, Browne FA, Myers B, & Zule WA (2015). Adapting an evidence-based HIV behavioral intervention for South African couples. Substance Abuse Treatment Prevention Policy, 10, 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wechsberg WM, Jewkes R, Novak SP, Kline T, Myers B, Browne FA, et al. (2013). A brief intervention for drug use, sexual risk behaviours and violence prevention with vulnerable women in South Africa: a randomised trial of the Women’s Health CoOp. BMJ Open, 3(5). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wechsberg WM, Zule WA, El-Bassel N, Doherty IA, Minnis AM, Novak SD, et al. (2016). The male factor: outcomes from a cluster randomized field experiment with a couples-based HIV prevention intervention in a South African township. Drug and Alcohol Dependence, 161, 307–315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weinhardt LS, Forsyth AD, Carey MP, Jaworski BC, & Durant LE (1998). Reliability and validity of self-report measures of HIV-related sexual behavior: progress since 1990 and recommendations for research and practice. Archives of Sexual Behavior, 27, 155–180. [DOI] [PMC free article] [PubMed] [Google Scholar]