Lung cancer is the leading cause of cancer-related mortality in the United States and worldwide.1–4 In 2011, it is estimated that 156,900 deaths (85,600 in men, 71,300 in women) from lung cancer will occur in the United States.4 Five-year survival rates for lung cancer are only approximately 15.6%, partly because most patients have advanced-stage lung cancer at initial diagnosis (http://seer.cancer.gov/statfacts/html/lungb.html).5
These facts, combined with the success of screening in improving outcomes in cervical, colon, and breast cancers, have been the impetus for studies to develop an effective lung cancer screening test.6,7 Ideally, effective screening will lead to earlier detection of lung cancer (before patients have symptoms and when treatment is more likely to be effective) and will decrease mortality.8 Currently, most lung cancer is diagnosed clinically when patients present with symptoms (such as cough, chest pain, weight loss); unfortunately, patients with these symptoms usually have advanced lung cancer.
Early detection of lung cancer is an important opportunity for decreasing mortality. Considerable interest has been shown in developing screening tools to detect early-stage lung cancer. Recent data support using spiral (helical) low-dose computed tomography (LDCT) of the chest to screen select patients who are at high risk for lung cancer (http://www.cancer.gov/clinicaltrials/noteworthy-trials/nlst).8
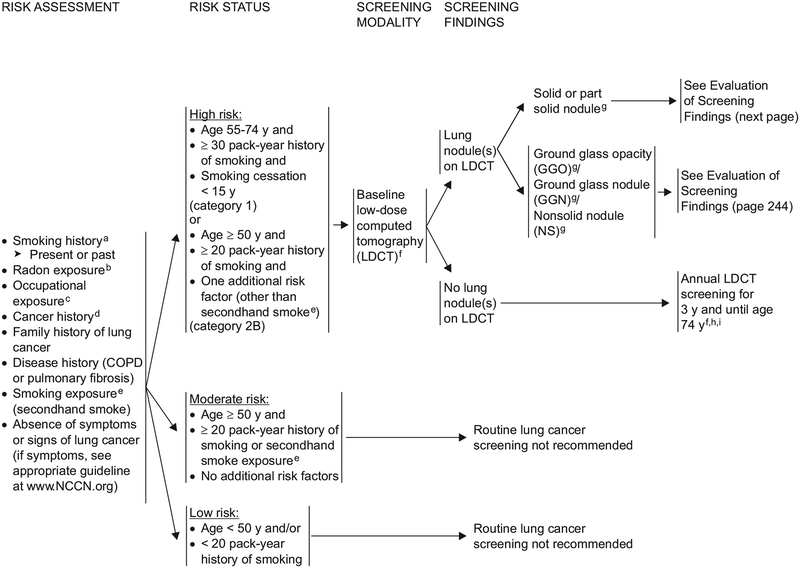
The NCCN Lung Cancer Screening Panel developed this new screening guideline in 2011 based on the current body of evidence.8 These guidelines 1) describe risk factors for lung cancer; 2) recommend criteria for selecting high-risk individuals for screening; 3) provide recommendations for evaluation and follow-up of nodules found during screening; 4) discuss the accuracy of LDCT screening protocols and imaging modalities; and 5) discuss the benefits and risks of screening.
Screening for Non–Small Cell Lung Cancer
Most lung cancers (85%) are classified as non–small cell lung cancer (NSCLC); small cell lung cancer occurs in 13% to 15% of patients (see the NCCN Clinical Practice Guidelines in Oncology ([NCCN Guidelines] for NSCLC and Small Cell Lung Cancer, available online at www.NCCN.org). Thus, these guidelines mainly refer to detection of NSCLC. Other types of cancer can metastasize to the lungs (e.g., breast cancer), and there are also less common cancers of the lung or chest (e.g., malignant pleural mesothelioma, thymic carcinoma). Lung cancer screening may also detect other noncancerous conditions of the thorax (e.g., aortic aneurysm, coronary artery calcification) and tumors or benign disease outside of the chest (e.g., renal cell carcinoma, adrenal adenoma).
The goal of screening is to detect disease at a stage when it is not causing symptoms and when treatment is most successful. Screening should benefit the individual by increasing life expectancy and increasing quality of life. The rate of false-positive results should be low to prevent unnecessary additional testing. The large fraction of the population without the disease should not be harmed (low risk), and the screening test should not be so expensive that it places an onerous burden on the health care system. Thus, the screening test should: 1) improve outcome; 2) be scientifically validated (e.g., have acceptable levels of sensitivity and specificity); and 3) be low risk, reproducible, accessible, and cost effective.
Perhaps the most difficult aspect of lung cancer screening is addressing the moral obligation. As part of the Hippocratic oath, physicians promise to first “do no harm.”9 The dilemma is that if lung cancer screening is beneficial but physicians do not use it, they are denying patients effective care. However, if lung cancer screening is not effective, then patients may be harmed from overdiagnosis, increased testing, invasive testing or procedures, and the anxiety of a potential cancer diagnosis. Debates from mammography and prostate cancer screening may provide additional insight for lung cancer screening, especially regarding the problem of overdiagnosis (see Randomized Trials on this page).10
CT as Part of a Screening Program
Lung cancer screening with CT should be part of a program of care and should not be performed in isolation as a free-standing test. Given the high percentage of false-positive results and the downstream management that ensues for many patients, the risks and benefits of lung cancer screening should be discussed with the individual before a screening LDCT scan is performed. It is recommended that institutions performing lung cancer screening use a multidisciplinary approach that may include specialties such as radiology, pulmonary medicine, internal medicine, thoracic oncology, and thoracic surgery. Management of downstream testing and follow-up of small nodules are imperative and may require the establishment of administrative processes to ensure adequate follow-up.
Randomized Trials
Disease-specific mortality (number of cancer deaths relative to number of individuals screened) is considered the ultimate test of screening effectiveness and the only test that is without bias.11 Randomized controlled screening trials are essential for determining whether cancer screening decreases disease-specific mortality. Nonrandomized trials are subject to biases that may cause an apparent increase in survival (e.g., lead-time bias, length-time bias) (http://www.cancer.gov/newscenter/qa/2002/nlstqaQA).
If lung cancer is detected through screening before symptoms occur, then the lead time in diagnosis equals the length of time between screening detection and when the diagnosis otherwise would have occurred, either as a result of symptoms or other imaging. Even if early treatment had no benefit, the survival of the screened person is increased simply by the addition of the lead time. Length-time bias refers to the tendency of the screening test to detect cancers that take longer to become symptomatic, possibly because they are slower-growing and perhaps indolent cancers. Survival (the number of individuals who are alive after detection and treatment of disease relative to the number of individuals diagnosed with the disease) has often been reported but is subject to these biases.7 For further discussion of randomized and nonrandomized screening trials, see Benefits of Lung Cancer Screening on page 253.
In the 1960s and 1970s, several randomized trials assessed whether chest radiographs could improve lung cancer survival. Many of these studies were flawed in their design or power, and all were negative.12 More recently, studies have focused on the more sensitive modality of helical LDCT–based lung cancer screening studies (see also section on Benefits of Lung Cancer Screening on page 253). However, analyses of some lung cancer screening studies using LDCT scans suggest that overdiagnosis (i.e., diagnosis of “cancer” that would never be life-threatening) and false-positive screening tests are significant concerns.13–15 Thus, although LDCT scanning may be a better screening test for lung cancer, it also has limitations (see Risks of Lung Cancer Screening on page 256).
Multiple ongoing randomized trials are assessing LDCT screening for lung cancer among high-risk groups, including 1) the National Lung Screening Trial (NLST), sponsored by the NCI7; and 2) the Dutch Belgian randomized lung cancer screening trial (NELSON).16 In November 2010, preliminary results from the NLST suggested that LDCT screening decreases disease-specific mortality, and the now-published results show that LDCT yields a decrease in lung cancer–specific mortality of 20% (95% CI, 6.8–26.7; P = .004) and in all-cause mortality of 7% (95% CI, 1.2–13.6; P = .02) when compared with chest radiograph alone.8
High-Risk Individuals
An essential goal of any lung cancer screening protocol is to identify the populations that are at a high risk for developing the disease. Although smoking tobacco is a well-established risk factor for lung cancer, other environmental and genetic factors also seem to increase risk. This section reviews the currently known risk factors for the development of lung cancer to identify high-risk populations that should be targeted for screening. Note that high-risk individuals who are recommended for screening do not have any symptoms suggestive of lung cancer (e.g., cough, chest pain, weight loss).
Tobacco Smoke
Active Tobacco Use:
Tobacco smoking is a major modifiable risk factor in the development of lung cancer, and accounts for 85% of all lung cancer–related deaths.1,6 The causal relationship between tobacco smoking and lung cancer was first reported in 1939. Since then, the risk of developing lung cancer from smoking tobacco has been firmly established. Tobacco smoke contains more than 4500 compounds, and more than 50 of these are known carcinogens that increase the risk of cancerous mutations at the cellular level, especially among individuals with a genetic predisposition. A dose–response relationship exists between smoking tobacco and the risk of developing lung cancer; however, there is no risk-free level of tobacco exposure (http://cancercontrol.cancer.gov/tcrb/monographs/7/m7_6.pdf). The relative risk (RR) for lung cancer is approximately 20-fold higher1,17 for smokers than for nonsmokers. Cessation of tobacco smoking decreases the risk of lung cancer.18 However, even reformed former smokers have a higher risk of lung cancer compared with never-smokers (http://cancercontrol.cancer.gov/tcrb/monographs/8/index.html). As a result, current or past history of tobacco smoking is considered a risk factor for the development of lung cancer, irrespective of the magnitude of exposure and the time since smoking cessation.
In the algorithm, individuals (aged 55–74 years) with a 30 or more pack-year history of smoking tobacco are selected as the highest-risk group for lung cancer and are recommended for screening (category 1) based on criteria for entry into the NLST.7,8 Pack-years of smoking history is defined as the number of packs of cigarettes smoked every day multiplied by the number of years of smoking. Individuals with a 30 pack-year smoking history who quit smoking less than 15 years ago are still in this highest-risk group.
Exposure to Second-Hand Smoke:
The relationship between lung cancer and exposure to second-hand smoke (also known as environmental tobacco smoke, passive smoke, and involuntary smoke) was first suggested in epidemiologic studies published in 1981.19 Since then, several studies and pooled RR estimates suggest that second-hand smoke causally increases the risk for lung cancer among nonsmokers (http://www.surgeongeneral.gov/library/secondhandsmoke/factsheets/factsheet6.html).20 However, the NCCN Lung Cancer Screening Panel does not consider second-hand smoke to be an independent risk factor, because the association is either weak or variable. Thus, second-hand smoke does not confer a great enough risk for exposed individuals to be considered for lung cancer screening in these guidelines.
A pooled analysis of 37 published studies found an estimated RR of 1.24 (95% CI, 1.13–1.36) for adult nonsmokers who live with a smoker.21 A pooled estimate from 25 studies found an RR of 1.22 (95% CI, 1.13–1.33) for lung cancer risk from exposure to second-hand smoke at the workplace.20 The pooled estimate for 6 studies suggests a dose–response relationship between number of years of second-hand smoke exposure and lung cancer risk.20 The data are inconsistent for second-hand smoke exposure during childhood and subsequent lung cancer risk in adulthood. For childhood tobacco smoke exposure, pooled RR estimates for the development of lung cancer were 0.93 (95% CI, 0.81–1.07) for studies conducted in the United States, 0.81 (95% CI, 0.71–0.92) for studies conducted in European countries, and 1.59 (95% CI, 1.18–2.15) for studies conducted in Asian countries.20
Occupational Exposure
Approximately 150 agents are classified as known or probable human carcinogens (IARC 2002). The 8 agents that are identified specifically as carcinogens targeting the lungs are arsenic, chromium, asbestos, nickel, cadmium, beryllium, silica, and diesel fumes.22–25 These agents are listed in order of their presumed risk.22 The calculated mean RR for development of lung cancer is 1.59 for individuals in the United States who have a known occupational exposure to these agents.22,25 Among those who are exposed to these carcinogens, smokers have a greater risk for lung cancer than nonsmokers.26
Residential Radon Exposure
Radon (a gaseous decay product of uranium-238 and radium-226) has been implicated in the development of lung cancer.27 The risk of lung cancer from occupational exposure among uranium miners is well established.28 However, the risk associated with residential radon is uncertain. A meta-analysis in 1997 of 8 studies yielded an estimated RR of 1.14 (95% CI, 1.0–1.3).29 However, a 2005 meta-analysis of 13 studies (using individual patient data) reported a linear relationship between the amount of radon detected in a home and the risk of developing lung cancer.30 Among those exposed to radon, smokers have a greater risk for lung cancer than nonsmokers.30
Cancer History
Evidence shows an increased risk of new primary cancers among patients who survive lung cancer, lymphomas, cancers of the head and neck, or smoking-related cancers (e.g., esophageal cancer). Patients who survive small cell lung cancer have a 3.5-fold increase in the risk for developing a new primary cancer (predominantly NSCLC).31
The risk for subsequent lung cancers is increased in patients who continue to smoke and who have been previously treated with either chest irradiation or alkylating agents. Patients previously treated with chest irradiation have a 13-fold increase in risk for developing new primary lung cancer, and those previously treated with alkylating agents have an estimated RR of 9.4. In patients previously treated for Hodgkin’s lymphoma, the RR for new primary lung cancer is 4.2 if previously treated with alkylating agents, and 5.9 if previously treated with 5 Gy or more of radiation therapy.32
In patients with head and neck cancers, subsequent new primary lung cancer may occur synchronously or metachronously. New primary tumors are seen in approximately 9% of patients. Most of these tend to be squamous cell cancers and a third of them occur in the lung. However, data do not suggest that previous treatment for head and neck cancers increases the risk of subsequent new primary lung cancer independent of tobacco exposure.33,34
Evidence suggests that patients who are successfully treated (i.e., cured) for an initial smoking-related lung cancer and who stop smoking will have a decreased risk of a subsequent smoking-related cancer compared with those who continue smoking.35
Family History of Lung Cancer
Several studies have suggested an increased risk for lung cancer among first-degree relatives of patients with lung cancer, even after adjustment for age, gender, and smoking habits.36,37 A meta-analysis of 28 case-control studies and 17 observational cohort studies showed an RR of 1.8 (95% CI, 1.6–2.0) for individuals with a sibling/parents or a first-degree relative with lung cancer.38 The risk is greater in individuals with multiple affected family members or who had a cancer diagnosis at a young age.
Although no high-penetrance inherited syndrome has been described for lung cancer (either small cell lung cancer or NSCLC), several groups have identified genetic loci that may be associated with an increased risk of developing lung cancer. The Genetic Epidemiology of Lung Cancer Consortium conducted a genome-wide linkage analysis of 52 families who had several first-degree relatives with lung cancer. Linkage disequilibrium was shown on chromosome 6, localizing a susceptibility locus influencing lung cancer risk to 6q23–25.39 Subsequently, 3 groups performed genome-wide association studies in patients with lung cancer and matched controls. They found a locus at 15q24–25 associated with an increased risk of lung cancer, nicotine dependence, and peripheral artery disease.40–42 It was noted that subunits of the nicotinic acetylcholine receptor genes are localized to this area (CHRNA5, CHRNA3, and CHRNB4). Other investigators recently found that a variant at 15q24/25 is associated with spirometric bronchial obstruction and emphysema as assessed with CT.43 Patients with classic familial cancer susceptibility syndromes (such as retinoblastoma, Li-Fraumeni syndrome) have a substantially increased risk for lung cancer if they also smoke tobacco.44–46
History of Lung Disease in the Patient
Chronic Obstructive Pulmonary Disease:
A history of chronic obstructive pulmonary disease (COPD) is associated with lung cancer risk,47–53 and this association may be largely caused by smoking. Yang et al.54 found that COPD accounts for 12% of lung cancer cases among heavy smokers. However, even after statistical adjustment, evidence suggests that the association between COPD and lung cancer may not be entirely caused by smoking.55 For example, 1) family history of chronic bronchitis and emphysema is associated with increased risk of lung cancer, and 2) COPD is associated with lung cancer among never-smokers.54–56 Yang et al.54 found that COPD accounts for 10% of lung cancer cases among never-smokers. Koshiol et al.55 found that when they restricted their analyses to adenocarcinoma (which is more common among nonsmokers, particularly women), COPD was still associated with an increased risk of lung cancer.
Pulmonary Fibrosis:
Patients with diffuse pulmonary fibrosis seem to be at a higher risk for lung cancer even after age, gender, and a history of smoking are taken into consideration (RR, 8.25; 95% CI, 4.7–11.48).57,58 Among patients with a history of exposure to asbestos, those who develop interstitial fibrosis are at a higher risk of developing lung cancer than those without fibrosis.59
Hormone Replacement Therapy
Whether hormone replacement therapy (HRT) use affects the risk of lung cancer in women is currently unclear. More than 20 studies have been published and the results have been inconsistent. Most of the currently available information comes from case-control and cohort studies. Cumulatively, these studies are variable; they have found associations ranging from an increased risk of lung cancer, no effect on risk, and a protective effect against lung cancer risk. However, in a large randomized controlled study,60 no increase in the incidence of lung cancer was found among postmenopausal women treated with estrogen plus progestin HRT, but deaths from lung cancer (especially NSCLC) were higher among patients receiving HRT.
Selection of High-Risk Individuals for Screening
Well-known risk factors exist for the development of lung cancer, especially smoking tobacco. Results from the recently concluded NLST support screening select individuals who are at high risk for lung cancer.8 The NCCN Lung Cancer Screening Panel recommends that high-risk individuals should be screened; however, moderate- and low-risk individuals should not be screened currently. Patients are selected for the different risk categories using the NLST inclusion criteria, nonrandomized studies, and/or observational studies. Based on the available data, the NCCN Lung Cancer Screening Panel recommends using the following criteria to determine whether individuals are at high, moderate, or low risk for lung cancer.
High-Risk Individuals
The NCCN Lung Cancer Screening Panel recommends lung cancer screening using helical LDCT for individuals with the following high-risk factors:
Age 55 to 74 years; 30 or more pack-year history of smoking tobacco; and, if former smoker, have quit within 15 years (category 1).7,8 Some high-risk individuals in the NLST also had COPD and other risk factors. This is a category 1 recommendation because these individuals are selected based on the NLST inclusion criteria.7,8 An NCCN category 1 recommendation is based on high-level evidence (i.e., randomized controlled trial) and uniform consensus among panel members. Annual screening is recommended for these high-risk individuals until they are 74 years of age based on the NLST.8 However, uncertainty exists about the appropriate duration of screening and the age at which screening is no longer appropriate.
Age 50 years or older, 20 or more pack-year history of smoking tobacco, and one additional risk factor (category 2B).61 This is a category 2B recommendation, because these individuals are selected based on nonrandomized studies and observational data.61 These additional risk factors were previously described and include cancer history, lung disease history, family history of lung cancer, radon exposure, and occupational exposure. Note that the NCCN Lung Cancer Screening Panel does not currently believe that exposure to second-hand smoke is an independent risk factor, because the data are either weak or variable (see Exposure to Second-Hand Smoke on page 248).
Moderate-Risk Individuals
NCCN defines moderate-risk individuals as those aged 50 years or older and have a 20 or more pack-year history of smoking tobacco or second-hand smoke exposure but no additional lung cancer risk factors.61 The NCCN Lung Cancer Screening Panel does not recommend lung cancer screening for these moderate-risk individuals. This is a category 2A recommendation based on nonrandomized studies and observational data.
Low-Risk Individuals
NCCN defines low-risk individuals as those younger than 50 years and/or with a smoking history of fewer than 20 pack-years.61 The NCCN Lung Cancer Screening Panel does not recommend lung cancer screening for these low-risk individuals. This is a category 2A recommendation based on nonrandomized studies and observational data.
Accuracy of LDCT Protocols and Imaging Modalities
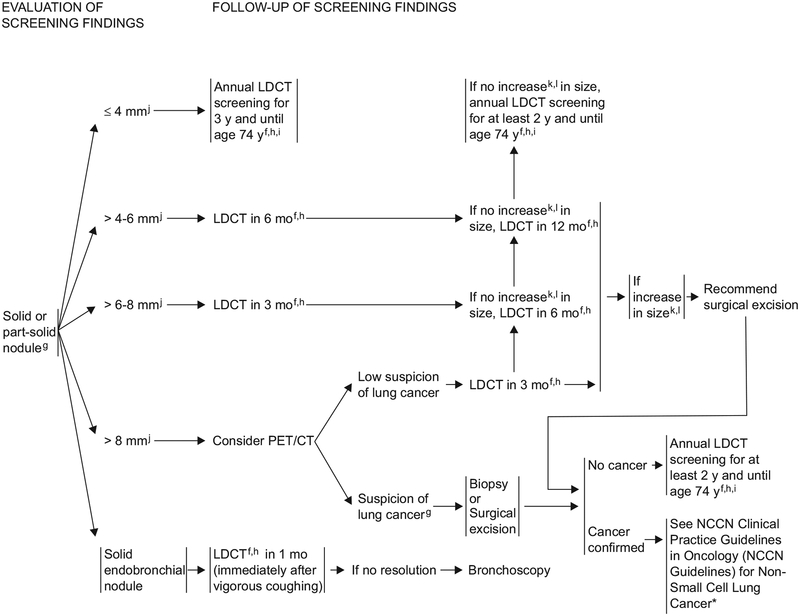
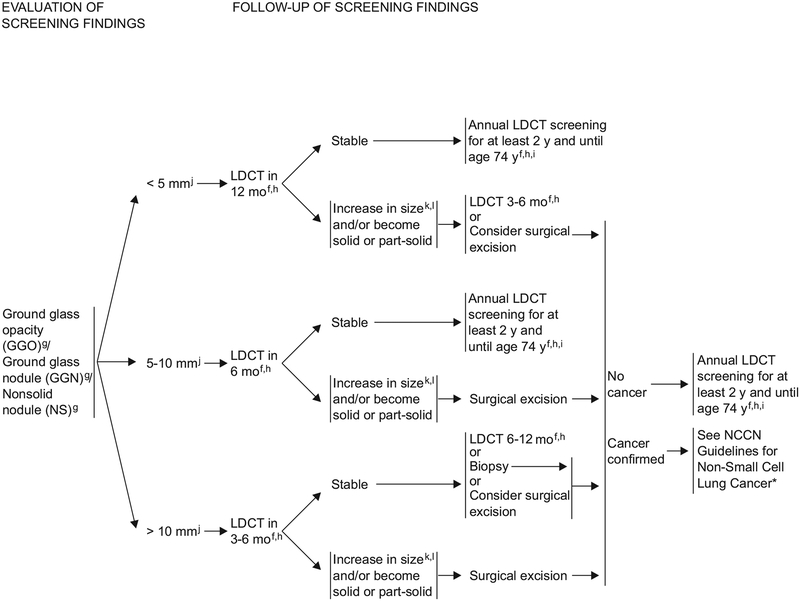
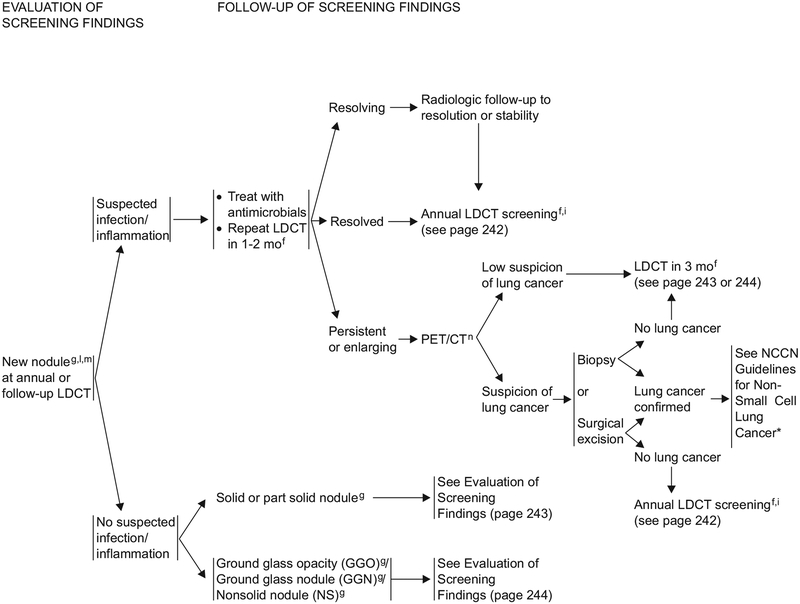
As shown in the algorithm, LDCT is recommended for detecting noncalcified nodules that may be suspicious for lung cancer depending on their type and size (e.g., solid, part-solid, and ground glass nodules). Li et al.62 found that the prevalence of malignancy was as follows: ground glass opacities (GGOs; 59%), mixed GGOs and solid (48%), and solid (11%). GGOs have the highest incidence of malignancy; 75% of persistent GGOs are cancer.63 However, the GGOs are mainly adenocarcinoma in situ (AIS) or minimally invasive adenocarcinoma (MIA), formerly known as bronchioloalveolar carcinomas (BAC), which have 100% 5-year disease-free survival if completely resected.63,64 Solid and part-solid nodules are more likely to be invasive and faster-growing cancers, factors that are reflected in the increased suspicion and follow-up of these nodules.14
Helical multidetector CT (MDCT) of the chest has made it possible to detect very small lung nodules, both benign and malignant. The ability to acquire thinner slices, the use of maximum intensity projection (MIP) or volume-rendered (VR) images, and computer-aided diagnosis (CAD) software have increased the sensitivity of small-nodule detection.65–74 The use of thinner images has also improved the characterization of small lung nodules.75
For lung cancer screening, LDCT without intravenous contrast is currently recommended instead of standard-dose CT to decrease the dose of radiation. Although there is no strict definition of LDCT of the chest, it is usually considered to be approximately 10% to 30% of standard-dose CT. In most cases, LDCT has been shown to be as accurate as standard-dose CT for detecting solid pulmonary nodules, although nodule detection with LDCT may be limited in larger patients.76,77 However, LDCT seems to be less sensitive for detecting very low-density non-solid nodules or GGOs.78 Decreasing the radiation dose does not significantly affect the measurement of nodule size when using 1-mm thick slices.79 These low-dose scans require radiologists to assess images that are much noisier than they are currently used to seeing. Studies suggest that some variation occurs in interpretation of LDCT scans among radiologists.80,81
Recent LDCT lung cancer screening studies using MDCT have reported that lung cancer mortality is decreased when compared with unscreened cohorts or those receiving chest radiographs.8,82 However, studies using multidetector LDCT screening for lung cancer in high-risk patients have applied various different protocol algorithms for detection and follow-up of pulmonary nodules/lesions (http://www.ielcap.org/professionals/docs/ielcap.pdf).7,83–89 These protocols have been based on the positive relationships among 1) nodule size and/or nodule consistency/density and likelihood of malignancy; 2) nodule size and tumor stage; and 3) tumor stage and survival. They also take into account the average growth rate of lung cancer (i.e., doubling time).61,90–96 Most of these protocols recommend dynamic contrast-enhanced CT and/or PET/CT be considered for nodules that are at least 7 to 10 mm, because these technologies have been shown to increase specificity for malignancy.97–101 In the workup of pulmonary nodules detected with CT in a high-risk lung cancer screening population, the roles of contrast-enhanced CT and PET/CT are still in evolution.102,103
Optimally, these lung cancer screening methods will maximize detection of early-stage lung cancer and minimize false-positive results, unnecessary invasive procedures, radiation exposure, and cost. In at least one medical center, improvement in CT equipment and change in screening protocol have been shown to increase early lung cancer detection, decrease the surgery rate, and improve cancer-specific survival.104 Strict adherence to a screening protocol may also significantly reduce unnecessary biopsies.105
Currently, the most accurate protocol for lung cancer detection using LDCT is difficult to determine because of differing patient populations, methodologies, lengths of follow-up, and statistical analyses among lung cancer screening studies. Recent LDCT screening programs (with multiple years of follow-up) report that 65% to 85% of their detected lung cancers are stage I.88,101 The I-ELCAP (International Early Lung Cancer Action Program) and NLST are the largest recent series examining lung cancer detection using LDCT in high-risk patients (see Benefits of Lung Cancer Screening 253).7,61 Differences in screening algorithms or recommended diagnostic pathways between these studies are summarized in Table 1 (available online, in these guidelines, at www.NCCN.org [MS-19]).7,61
In 2005, the Fleischner Society published guidelines for the management of small pulmonary nodules detected on LDCT scans.106 Most radiologists in the United States are aware of these guidelines and/or work in a practice that uses them.107 However, these recommendations do not specifically address the management of part-solid or nonsolid pulmonary nodules. Although understanding of the histology and behavior of nonsolid and part-solid nodules has changed recently, interim guidelines for the assessment and management of subsolid nodules were recently proposed.14
Because of the familiarity and/or acceptance of the Fleischner Society guidelines among radiologists, pulmonologists, and thoracic surgeons, these same principles have been incorporated into the NCCN recommendations for lung cancer screening. The NCCN recommendations in the algorithm are an adaptation of the Fleischner Society guidelines, proposed guide lines for subsolid nodules by Godoy, NLST data, and the I-ELCAP protocol guidelines (http://www.ielcap.org/professionals/docs/ielcap.pdf).14,106 The currently proposed NCCN recommendations are less aggressive (i.e., less-frequent LDCT) than the I-ELCAP protocol for the workup of baseline and new solid and part-solid nodules 6 mm or smaller. However, the NCCN recommendations are slightly different (i.e., consider PET/CT and/or contrast-enhanced CT) from the I-ELCAP protocol (see Table 1, available online, in these guidelines, at www.NCCN.org [MS-19]) in the evaluation of solid and part-solid nodules larger than 8 mm, because the NCCN Guidelines recommend considering short-term assessment with PET/CT (to increase nodule specificity) rather than longer-term assessment with LDCT.
The NCCN definition of nodule growth is 1) an increase in mean diameter of 2 mm or more for nodules 15 mm or smaller or in the solid portion of a part-solid nodule when compared with the baseline scan, or 2) an increase of 15% in mean diameter if the nodule is 15 mm or more when compared with the baseline scan. Mean diameter is the mean of the longest diameter of the nodule and its perpendicular diameter when compared with the baseline scan. This definition of nodule growth is based on intraobserver and interobserver variability when measuring small pulmonary nodules, and on the minimum change in diameter that can be reliably detected using conventional methods (excluding volumetric analysis software).108 This definition of nodule growth is simplified compared with the formula used by I-ELCAP (see Table 1, available online, in these guidelines, at www.NCCN.org [MS-19]), which requires nodule growth of 1.5 to 3.0 mm in mean diameter for nodules 3 to 15 mm, depending on their diameter. The NCCN definition of nodule growth should also result in fewer false-positive diagnoses compared with the NLST suggested definition of nodule growth (≥ 10% increase in nodule diameter).8
Currently, the NCCN recommendations do not take into consideration other possibly relevant nodule features, such as proximity to the pleura or fis-sure.109–111 Currently, the topics of nodule volumetric analysis and/or calculations of tumor doubling time have not been addressed. In some cases, it may be appropriate to perform standard-dose CT with or without intravenous contrast for follow-up or further evaluation of lung or mediastinal abnormalities detected on screening LDCT.
The recommended LDCT acquisition parameters in these NCCN Guidelines (see Table 2, available online, in these guidelines, at www.NCCN.org [MS-20–21]) are similar to many of the recent and ongoing lung cancer screening studies using low-dose MDCT. Use of MIP, VR, and/or CAD software is highly recommended in addition to evaluation of conventional axial images for increased sensitivity of small nodule detection. A detector collimation of 1.5 mm or less is necessary for optimal use of these 3-dimensional applications. For accurate nodule volumetric analysis, some radiologists feel that a detector collimation of 1 mm or less is needed. Measurement and evaluation of small nodules are more accurate and consistent on 1-mm thick images compared with 5-mm images.75 There may be a similar but less-pronounced benefit in evaluating nodules on 1-mm reconstructed images after detecting them on 2.5- to 3.0-mm thick slices. Because slice thickness, reconstruction algorithms, and postprocessing filters affect nodule size measurement, the same technical parameters should be used for each screening LDCT. Ultra-low-dose chest CT currently produces lower sensitivity for nodule detection, especially in larger patients.77 However, new LDCT technologies may soon make it possible to significantly decrease the radiation dose without compromising nodule detection and evaluation.112–115
Benefits of Lung Cancer Screening
This section summarizes current information about the possible or projected benefits of screening for lung cancer using helical LDCT scans, including 1) decreased lung cancer mortality, or improvement in other oncologic outcomes, 2) quality-of life benefits from screening and early detection (compared with standard clinical detection), 3) cost-effectiveness of screening, and 4) detection of disease, other than lung cancer, that requires treatment.
Oncology Outcomes
After a clinical diagnosis of NSCLC, survival is directly related to stage at diagnosis.5 Although patients with earliest-stage disease (IA) may have a 5-year survival rate of approximately 75% with surgery, the outcomes quickly decrease with increasing stage (e.g., 5-year survival is 71% for stage IB; 58% for IIA; 49% for IIB; and < 25% for stages III and IV).116 Note that staging for NSCLC was recently revised in January 2010 (see the NCCN Guidelines for NSCLC, available online at www.NCCN. org).117 Although it is intuitively appealing to conclude that earlier detection of disease will improve outcome, screen-detected lung cancers may have a different natural history from that of clinically detected cancers,118,119 and an apparent improvement in survival from early detection itself (lead-time bias). Pathology results of resected lung cancers detected through prior screening trials suggest that screening increases the detection of indolent cancer. However, randomized trial data from the NLST show that LDCT screening decreases lung cancer mortality.8
Nonrandomized Trials:
Of the single-armed screening studies (i.e., nonrandomized), the I-ELCAP study is the largest. It included 31,567 high-risk patients from around the world, all of whom were to be screened with baseline and annual LDCT scans analyzed centrally in New York.61 In the I-ELCAP study, Henschke et al.61 reported that a high percentage of stage I cancers (85%) were detected using LDCT, with an estimated 92% actuarial 10-year survival rate for stage I cancers resected within 1 month of diagnosis (62% of all cancers detected). The authors noted that 8 participants with clinical stage I cancer who opted not to undergo treatment all died within 5 years, findings similar to those of published medical literature examining the natural history of stage I NSCLC.120 They concluded that annual helical LDCT screening can detect lung cancer that is curable. Important caveats about I-ELCAP include that it was not randomized, the median follow-up time was only 40 months, and fewer than 20% of the subjects were observed for more than 5 years. Given the limited follow-up, the 10-year survival estimates may have been overstated.
A study by Bach et al.121 raised concern that LDCT screening may lead to overdiagnosis of indolent cases without substantially decreasing the number of advanced cases or the overall attributable deaths from lung cancer. However, although overdiagnosis did occur with LDCT in the NLST, the magnitude was not large when compared with radiographic screening (83 vs. 17 stage IA BAC, also known as AIS or MIA).8,64,122 Data from the ELCAP suggest that baseline CT scans find more indolent cancers, and subsequent annual scans find more rapidly growing cancers.123
Another recent analysis of 7995 participants in the NY-ELCAP single-arm screening trial (the precursor to the I-ELCAP) compared the observed death rate from lung cancer among ELCAP subjects with that seen in participants in large cancer prevention cohort studies who were not undergoing prescribed lung cancer screening with LDCT scans.82 The analysis was adjusted for age, gender, and smoking status, and suggested a significant reduction in deaths from lung cancer of 40% to 60% among the screened cohort.
Randomized Trials:
To address the concerns of bias and overdiagnosis from single-arm screening (i.e., nonrandomized) studies, the NCI launched the NLST in 2002.7 The NLST was a prospective, randomized lung cancer screening trial comparing annual LDCT scan with annual chest radiograph for 3 years; this trial was designed to have 90% power to detect a 21% decrease in the primary end point of lung cancer–specific mortality in the screened group. The investigators enrolled 53,454 high-risk participants aged 55 to 74 years who had smoking history of at least 30 pack-years. If subjects were no longer smoking tobacco, they had to have quit within the previous 15 years. All screening examinations were completed by mid-2007, and the study mandated a Data Safety Monitoring Board (DSMB) that met twice annually to evaluate follow-up information. In October 2010, the DSMB concluded that sufficient information was available to assess the primary outcome of the study. A NCI press release about the NLST findings was issued in November 2010. The NLST results were recently published and showed a substantial reduction in lung cancer–specific mortality and a reduction in all-cause mortality (http://www.cancer.gov/newscenter/pressreleases/2011/NLSTprimaryNEJM).8
The NLST participants were similar to a United States census population of heavy smokers in terms of gender, but the NLST population was generally younger, better educated, and less likely to be current smokers. Subjects in both the LDCT screening and chest radiograph screening arms were very compliant (> 90%) with their designated screening tests. The screening tests were deemed positive if there was a finding that was suspicious for lung cancer (i.e., suspicious nodule).7 Overall, 24% of the LDCT scans and 7% of the chest radiographs performed were positive screens, an imbalance that was expected based on prior data. In each of the 3 years of screening, positive LDCT scan screens were determined to be actual lung cancer cases (i.e., true-positive) 4%, 2%, and 5% of the time, compared with 6%, 4%, and 7% for positive chest radiographs.
Based on the published NLST results, 356 participants died of lung cancer in the LDCT arm and 443 participants died of lung cancer in the chest radiograph arm.8 Thus, LDCT screening yielded a 20% reduction in lung cancer–specific mortality. In addition, a 7% improvement was seen in all-cause mortality. These results are impressive, and the NLST represents the first randomized study showing an improvement in either disease-specific or overall mortality when using a lung cancer screening program. The NLST results indicate that to prevent one death from lung cancer, 320 high-risk individuals must be screened with LDCT. The NLST results will likely change medical practice in the United States. Results of the NELSON trial are anxiously awaited to ensure the NLST findings are validated in a separate cohort; further analysis of the NLST, including comparative effectiveness modeling, is underway.
The 20% reduction in mortality from LDCT screening (compared with chest radiograph) may actually be greater in clinical practice, because chest radiographs are not currently recommended for lung cancer screening as standard practice (by either the American Thoracic Society or the American College of Chest Physicians).124 In addition, if annual lung screening is continued for more than 3 years, this increased screening may yield mortality reductions of more than 20% (which was reported by the NLST after annual lung screening for only 3 years). Recent findings suggest that showing the benefit of breast cancer screening requires follow-up of at least 20 years.125
Quality of Life
The NLST assessed quality of life among participants at the time of each annual screening study, but these results are not yet available. Possible quality-of-life benefits from early lung cancer detection (as opposed to detection at the time of clinical symptoms) include 1) reduction in disease-related morbidity, 2) reduction in treatment-related morbidity, 3) alterations in health affecting lifestyles, and 4) reduction in anxiety and psychological burden.
Reduction in Disease-Related Morbidity:
It is a reasonable assumption that the disease-related symptom burden would be decreased in patients whose lung cancer is detected early (via screening) compared with late (via clinical presentation). Most patients whose lung cancer is detected early are asymptomatic, and detection is often either incidental or part of a screening protocol.7 Historically, most patients with lung cancer presented with symptoms of the disease (including cough, dyspnea, hemoptysis, pain, weight loss, and cachexia), and thus their lung cancer was detected clinically. An important analysis of the NLST quality-of-life data will be to assess the 2 cohorts for differences in the types of symptoms experienced at the time of lung cancer diagnosis to see if screening truly can decrease the lung cancer symptom burden.
Reduction in Treatment-Related Morbidity:
Patients with early-stage lung cancer primarily are treated surgically, sometimes with adjuvant chemo-therapy, whereas those with more advanced disease are treated with a combination of chemotherapy and radiation, or chemotherapy alone (see the NCCN Guidelines for NSCLC, available online at www.NCCN.org).126,127 Patients with early-stage lung cancer who undergo an R0 resection have increased survival compared with those with more advanced disease who undergo definitive chemoradiation therapy.128 However, few data have been published comparing the treatment burden of surgery versus chemoradiation therapy. It seems reasonable to assume that a patient with stage I lung cancer requiring a lobectomy alone probably has less treatment-related morbidity than a patient with stage III lung cancer requiring combined-modality therapy (i.e., chemotherapy, radiation, and a possible lung resection).129 However, this has not been shown.
The NLST found that 40% of the cancers detected in the CT-screening group were stage IA, 12% were stage IIIB, and 22% were stage IV.8 Conversely, 21% of the cancers detected in the chest radiograph group were stage IA, 13% were stage IIIB, and 36% were stage IV. These results suggest that LDCT screening decreases the number of cases of advanced lung cancer, and therefore may decrease treatment-related morbidity. Lung cancer screening may reduce the number of patients who require pneumonectomy for treatment of lung cancer, which will reduce treatment-related morbidity and mortality. Several series have shown that pneumonectomy is performed in only 1% of cases of lung cancer diagnosed in CT screening programs, in contrast to the 20% to 30% rate of pneumonectomy in symptom-detected cases.130–133
Alterations in Health That Affect Lifestyles:
The process of lung cancer screening itself has been suggested to increase smoking cessation rates. Conversely, it has also been suggested that negative results on a lung cancer screening test may provide a false sense of security to smokers and result in higher smoking rates. Neither hypothesis has been supported by any substantial evidence. A nonrandomized screening study reported that smoking cessation rates were higher when more follow-up LDCT scans were ordered for abnormal findings, regardless of ultimate diagnosis of cancer, suggesting that patients became “scared” into quitting.134 In a controlled study, however, smoking abstinence rates were similarly higher than expected in both screened and unscreened arms. This result suggests that the positive effect on smoking cessation was likely unrelated to the screening test results and may reflect a higher desire to be healthy among volunteers participating in screening clinical trials.135
Smokers, including those undergoing lung cancer screening, should always be encouraged to quit smoking tobacco (http://www.smokefree.gov/).136 Programs using behavioral counseling combined with medications that promote smoking cessation (approved by the FDA) can be very useful (see Quick Reference Guide for Clinicians: Treating Tobacco Use and Dependence; http://www.surgeongeneral.gov/tobacco/tobaqrg.htm).
Reduction in Anxiety and Psychological Burden:
As with mammogram screening for breast cancer, whether lung cancer screening causes anxiety or improves overall quality of life has been a topic of discussion. The randomized NELSON screening study recently published health-related quality-of-life data from 733 participants. In the short term, recipients of an indeterminate result from the LDCT scan experienced increased distress, whereas relief was experienced after a negative baseline screening examination.137 After 2 years of follow-up, data from the NELSON trial suggest that lung screening did not adversely affect quality of life.138 However, further longitudinal studies are needed to determine the long-term effect. Patients’ attitudes toward risk in their life (risk perception) also greatly affect their anxiety when undertaking cancer screening examinations.139 Little definitive research is available to support or refute effects on quality of life from lung cancer screening.
Cost-Effectiveness
Only a small number of preliminary cost–benefit analyses have been performed with respect to lung cancer screening, and many are based on modeled predictive systems because randomized clinical trials have been completed only recently.140 In fact, a current fundamental flaw with cost–benefit analyses for lung cancer screening is that because the true benefit of screening requires more years of follow-up and more years of screening to realize the full potential, this crucial factor in prior analyses has been arbitrarily assigned or assumed.125 The types of assumptions made can significantly affect the conclusions of the analysis. Furthermore, many cost–benefit analyses do not adequately represent the detrimental effects of false-positive test results on screening. For a person undergoing lung cancer screening with 2 sequential annual examinations, the cumulative risk of a false-positive test result was 33%.141 The economic effect of false-positive cancer screening results has been estimated to be at least $1000 per incident.142
The original ELCAP study constructed a decision analysis model from its data.143 The investigators documented that diagnostic procedure costs and hospital/physician costs in the first year after the diagnosis of lung cancer proportionally increased with increasing stage. Because they detected primarily early-stage cancers, they estimated that a baseline screening LDCT scan could increase survival by 0.1 year at an incremental cost of approximately $230 (this study was published in 2003). The incremental cost per life-year gained ratio is also very sensitive to the fraction of the patients screened and found to have early-stage disease; the higher the percentage of patients found with early-stage disease, the lower the incremental cost ratio.144 The emerging NSLT data must be carefully examined to ascertain the proportion of patients diagnosed with early-stage disease, their comparative mortality and morbidity, and the associated costs. Additional studies to examine other cohorts at risk will also be helpful in future cost-effectiveness analysis models.
Risks of Lung Cancer Screening
Lung cancer screening with LDCT has inherent risks and benefits. These risks must be understood to determine whether screening is beneficial. The possible or projected risks of screening for lung cancer using LDCT scans include 1) false-positive results, leading to unnecessary testing, unnecessary invasive procedures (including surgery), increased cost, and decreased quality of life because of mental anguish; 2) false-negative results, which may delay or prevent diagnosis and treatment because of a false sense of good health; 3) futile detection of small aggressive tumors (which have already metastasized, preventing meaningful survival benefit from screening); 4) futile detection of indolent disease (i.e., overdiagnosis), which would never have harmed the patient who subsequently undergoes unnecessary therapy; 5) indeterminate results, leading to additional testing; 6) radiation exposure; and 7) physical complications from diagnostic workup. Patients with several comorbid conditions may be at greater risk than those with few or none.
False-Positive Results
Lung cancer screening studies (which have included only high-risk populations) have found a high rate of noncalcified nodules larger than 4 mm on LDCT screening, with false-positive rates ranging from 10% to 43%.132,141,145–148 In the NLST, the false-positive rate was 96.4% for the CT screening group.8 The cumulative risk of a false-positive result was 33% for a person undergoing lung cancer screening with 2 sequential annual examinations.141 These results then require follow-up, which may include surveillance with chest LDCT scans, percutaneous needle biopsy, or even surgical biopsy. Each of these procedures has its own risks and potential harms.149 Approximately 7% of individuals with a false-positive result will undergo an invasive procedure (typically bronchos-copy).141 However, in the NLST, the rate of major complications after an invasive procedure was very low (only 0.06%) after workup for a false-positive result in the CT screening group.8
The NCCN lung cancer screening protocol may avoid much of the most-invasive follow-up for noncalcified nodules that are detected on baseline screening with LDCT (see the algorithm). The NCCN protocol uses the NLST and I-ELCAP protocols/recommendations (see Table 1, available online, in these guidelines, at www.NCCN.org [MS-19]) and the Fleischner Society guidelines and is based on expert opinion from the NCCN panel members.150 However, even repeat chest LDCT scanning is associated with risk for 1) increased radiation exposure; 2) increased cost of follow-up scans and clinic visits; and 3) ongoing anxiety to the individual, who must wait for the results of repeat chest LDCT scans. Bach et al.121 also provide insight into the potential harms of LDCT screening, which results in a 3-fold increase in lung cancer diagnosis and a 10-fold increase in lung cancer surgery, this representing substantial psychological and physical burdens. Although the I-ELCAP investigators reported a surgical mortality rate of only 0.5% (when surgery is performed by board certified thoracic surgeons at cancer centers), the average surgical mortality rate for major lung surgery across the United States is 5%, and the frequency of serious complications is greater than 20%.151 These potential harms associated with thoracic surgery151–153 mandate that the effectiveness of LDCT screening be accurately assessed.
False-Negative Results
Sone et al.154 published 2 reports on lung cancers missed at screening.155,156 Of the 88 lung cancers diagnosed, 32 were missed on 38 LDCT scans; 23 from detection errors (with a mean size of 9.8 mm) and 16 from interpretation errors (with a mean size of 15.9 mm). Detection errors included 1) subtle lesions (91%) appearing as GGOs; and 2) lesions (83%) that were overlapped with, obscured by, or similar in appearance to normal structures (such as blood vessels). Interpretation errors (87%) were seen in patients who had underlying lung disease, such as tuberculosis, emphysema, or fibrosis.
The second report revealed that 84% of missed cancers in that database were subsequently detected using an automated lung nodule detection method. The CAD method involved the use of gray-level thresholding techniques to identify 3-dimensionally contiguous structures with the lungs, which were possible nodule candidates. The problem is that CAD systems are not universally deployed, and the success of detecting disease can vary greatly among radiologists. The variability and success of CAD and volumetric analysis systems may also affect the success of screening trials. Although these issues are partly being addressed through NCI-sponsored programs (such as the RIDER and PAR 08–225 programs), the range in variability at various centers, particularly outside of academic institutions, may lead to significant differences in results compared with those published from clinical trials. False-negative results from a screening test may provide an individual patient with a false sense of security, causing a patient to per haps ignore symptoms that may have otherwise led to more evaluation.
Futile Detection of Small Aggressive Tumors
Early detection using lung cancer screening may not be beneficial if a small tumor is very aggressive and has already metastasized, with a loss of opportunity for effective treatment. Studies show that a 5-mm lung cancer has undergone approximately 20 doublings yielding 108 cells, whereas patient death typically occurs with a tumor burden of 1012 cells.157 Even small tumors may have already metastasized. Studies have also shown that metastases can occur at the time of angiogenesis, when lesions are approximately 1 to 2 mm.158 Human tumors grown in nude mouse models can shed 3 to 6 million cells per gram of tissue every 24 hours,159 providing the potential for early metastasis.
However, the NLST trial results show that lung cancer screening is effective in select high-risk patients.8 The data from this trial show that detecting and treating lung lesions lead to a reduction in lung cancer–specific mortality. Therefore, the likelihood of futile therapy in patients with screen-detected tumors is much less, albeit not zero. However, because the natural history of lung cancer is heterogeneous and not completely predictable or linear,160 the potential remains for futile treatment in patients with an aggressive tumor that is already incurable at the time of screening diagnosis.
Futile Detection of Indolent Disease
Although lung cancer specialists generally have a strong opinion of the uniform fatality of untreated lung cancer, recent studies of some low-grade lung cancers (i.e., BAC) show a potential for prolonged survival in some patients with NSCLC, even without therapy.161,162 Note that a new lung adenocarcinoma classification has recommended that the term BAC should not be used anymore. Newly defined entities of AIS and MIA, which are likely to present as ground glass nodules (GGN), should have 100% 5-year disease-free survival rate if completely resected.64,161 A greater percentage of the lepidic pattern (formerly BAC pattern), which corresponds with the ground glass component in a part-solid nodule, is correlated with a more favorable prognosis.64,161,162
Furthermore, experience in lung cancer screening has raised the question of increased identification of indolent tumors in the screened population.121,163 These indolent tumors may not cause symptoms or cancer mortality; therefore, patients do not benefit from screening and subsequent workup and treatment. A percentage of these patients will be exposed to the risk, morbidity, and mortality of surgical resection that, in retrospect, will not increase their life expectancy. As the newly defined entities of AIS and MIA (formerly BAC) with excellent survival have been separated from overtly invasive adenocarcinomas, the potential exists to learn how to minimize surgical intervention for pure GGNs through CT screening studies and long-term follow-up.64
Bach et al.121 found an increase in the number of patients with lung cancer detected through screening, yet no evidence of a decline in the number of deaths from lung cancer. Their nonrandomized study raised concern that LDCT screening may lead to overdiagnosis of indolent cases and to the morbidity of treatment, without a survival benefit. However, the recent randomized NLST found that LDCT does decrease lung cancer mortality.8
Quality of Life
What effect a lung cancer screening trial will have on the quality of life (see Benefits of Lung Cancer Screening on page 253) is not fully known. A study by van den Bergh et al.164 found no measured adverse effects, although approximately half of the participants reported discomfort while waiting for the results. However, others have reported significant personal and physical quality-of-life issues from screening tests (http://health.usnews.com/usnews/health/articles/030519/19diagnosis.htm). Several studies (including the NLST and NELSON trial) will be measuring quality-of-life issues.137,138 Recent data from the NELSON trial suggest that lung screening did not adversely affect quality of life.138 False-positive and indeterminate results may decrease quality of life because of mental anguish and additional testing.
Unnecessary Testing
Any lung cancer screening program will result in additional testing. In a report by Croswell et al.165 (from the Prostate, Lung, Colorectal, and Ovarian trial), the cumulative risk of having one false-positive result was 60% for men and 49% for women. The cumulative risk of undergoing an invasive diagnostic procedure prompted by the false-positive test was 29% for men and 22% for women. The NLST is a carefully supervised, randomized, controlled trial. In a less-controlled environment, the rate of additive studies may be higher. Sistrom et al.166 reviewed the recommendations for additional imaging in more than 5.9 million radiology reports; they reported additional imaging of 35.8% for chest LDCT. The issue of incidental findings on screening examinations is problematic, and some organizations are attempting to address the issue, but regional and physician variations remain.167
Radiation Exposure With LDCT
Current MDCT scanners provide a significantly enhanced capability for detecting small nodules through allowing thinner slice images. Using low-dose techniques, the mean effective radiation dose is 1.4 mSv (SD, 0.5 mSv) compared with an average of 7 mSv for conventional CT.168 However, the radiation dose of LDCT is 10 times that of chest radiography.
There may be even more reason to be concerned about use of chest LDCT scans for lung cancer screening, because these individuals, who are already at high risk for lung cancer, may experience adverse effects from increased radiation exposure. In fact, the effects of repeated exposure to radiation at regular intervals are not known. Brenner169 estimated a 1.8% increase in lung cancer cases if 50% of all current and former smokers in the United States between 50 and 75 years of age were to undergo annual LDCT scans for lung cancer screening. However, lower doses of radiation are now used for LDCT scans and these lower doses may be less dangerous.170 The risk of radiation exposure over long periods will have to be considered when screening guidelines are developed, especially when recommending how frequently the scans should be performed.
Increased Cost
Many are concerned about the effect of lung cancer screening on medical resources, including the cost of LDCT screening and additional testing. For each LDCT screen for lung cancer, the Medicare reimbursement rate is approximately $300 in the United States (http://www.cancer.gov/newscenter/pressreleases/2011/NLSTFastFacts). Therefore, with the number of high-risk individuals eligible for lung cancer screening at approximately 7 million (using NLST data), the annual cost in the United States would be about $2.1 billion.8
Helical LDCT screening will lead to false-positive results, detection of indeterminate nodules, and detection of potential disease other than lung cancer. In the NLST, although 24.2% of the LDCT scans were positive, most were false-positive (96.4%). In 2004, the economic effect of false-positive cancer screening results was estimated to be at least $1000 per incident.142 Therefore, a conservative estimate of the costs of workup after 1 year for only the false-positive results would be $1.63 billion (7 million × 24.2% = 1.694 million × 96.4% = 1.633 × $1000). This estimate does not include costs of workup for other potential abnormalities detected during screening, such as cardiac and upper abdominal pathology. Of individuals with a false-positive result, approximately 7% will undergo an invasive procedure (typically bronchoscopy).141
Limiting screening to only high-risk patients not only helps avoid unnecessary risks in individuals with a lower risk of cancer but also is important for keeping the screening program cost-effective. “Pre-screening” based on age, smoking history, appropriate medical history, family history, and occupational history is important to determine which patients are high risk.
Lack of well-defined guidelines can lead to overuse of screening. Excessive screening and/or interpretations of studies by unskilled individuals may occur without strict guidelines (as with mammography). Other factors, such as the interval at which screening should be performed, will also affect calculations of cost. In the recent screening studies using helical LDCT, 23% of the ELCAP and 69% of the 1999 Mayo Clinic study had at least one indeterminate nodule. Depending on the size and characteristics of the indeterminate nodule, further evaluation may include serial follow-up LDCT, dynamic contrast-enhanced nodule densitometry, PET, or biopsy. False-positive results also lead to additional unnecessary testing and increased cost. The financial burden, potential complications from invasive procedures, and psychological effect of investigating these indeterminate and false-positive lesions are not fully understood.
Lung screening also leads to detection of disease other than lung cancer, such as infection; coronary artery calcification; and renal, adrenal, and liver lesions. Although detection of other diseases may frequently provide a clinical benefit to the patient, certainly costs will be further increased with additional testing and treatment.
Cost-Effectiveness
The cost-effectiveness of lung cancer screening is also important to consider. LDCT imaging is more expensive than many other screening programs, and therefore it is important to validate the effectiveness first. Each LDCT screen for lung cancer costs approximately $300 (http://www.cancer.gov/news-center/pressreleases/2011/NLSTFastFacts). In contrast, a mammogram costs $80 to $150. Several cost analyses of LDCT lung cancer screening have been undertaken, but all have some limitations because they used simulation modeling.144,171,172 The Mahadevia study concluded that false-positive results are a major obstacle to LDCT screening and may prevent it from being cost-effective.171 However, Wisnivesky et al.143 have argued that LDCT lung cancer screening is potentially highly cost-effective and that the cost-effectiveness ratios are not different from those of other screening programs. The NLST cost-effectiveness evaluation will be extremely beneficial in understanding this issue.
Summary
Lung cancer screening with LDCT is a complex and controversial topic, with inherent risks and benefits. Results from the large, prospective, randomized NLST show that lung cancer screening with LDCT can decrease lung cancer–specific mortality by 20% and even decrease all-cause mortality by 7%.8 The NLST results indicate that to prevent one death from lung cancer, 320 high-risk individuals must be screened with LDCT. However, the NLST findings have not been replicated yet in a separate cohort. Further analysis of the NLST is underway, including comparative effectiveness modeling. The cost-effectiveness and true benefit-to-risk ratio for lung cancer screening still must be determined. At some point, an acceptable level of risk will have to be deemed appropriate for the benefits of screening.
The NCCN Lung Cancer Screening Panel recommends helical LDCT screening for select patients at high risk for lung cancer based on the NLST results, nonrandomized studies, and observational data. These guidelines discuss in detail the criteria for determining which patients are at high risk, and the algorithm provides recommendations for evaluating and following-up nodules detected on LDCT screening (e.g., solid and part-solid nodules).
Smokers should always be encouraged to quit smoking tobacco (http://www.smokefree.gov/). Programs using behavioral counseling combined with medications that promote smoking cessation (approved by the FDA) can be very useful (see Treating Tobacco Use and Dependence: Quick Reference Guide for Clinicians; http://www.surgeongeneral.gov/tobacco/tobaqrg.htm).
When considering lung cancer screening, it is important to have a full understanding of all risks and benefits related to screening with LDCT. As policies for implementing lung screening programs are designed, a focus on multidisciplinary programs (incorporating primary care doctors, pulmonologists, radiologists, thoracic surgeons, medical oncologists, and pathologists) will be helpful to optimize decision-making and minimize interventions for patients with benign lung disease.
Individual Disclosures for the NCCN Guidelines Panel for Lung Cancer Screening
| Panel Member | Clinical Research Support | Advisory Boards, Speakers Bureau, Expert Witness, or Consultant | Patent, Equity, or Royalty | Other | Date Completed |
|---|---|---|---|---|---|
| George A. Eapen, MD | None | None | None | None | 17/20/11 |
| David S. Ettinger, MD | None | Boehringer Ingelheim GmbH; Eli Lilly and Company; Genentech, Inc.; and Biodesix | None | None | 6/13/11 |
| Lifang Hou, MD, PhD | None | None | None | None | 9/9/11 |
| David M. Jackman, MD | None | Genentech, Inc.; and Foundation Medicine, Inc. | None | None | 7/20/11 |
| Ella Kazerooni, MD | None | None | None | None | 7/21/11 |
| Donald Klippenstein, MD | None | None | None | None | 3/28/11 |
| Rudy P. Lackner, MD | None | None | None | None | 7/26/11 |
| Lorriana Leard, MD | None | None | None | None | 9/9/11 |
| Ann N.C. Leung, MD | None | None | None | None | 3/15/11 |
| Pierre P. Massion, MD | None | None | None | None | 9/9/11 |
| Bryan F. Meyers, MD, MPH | Pending | ||||
| Reginald F. Munden, MD, DMD, MBA | None | None | None | None | 7/20/11 |
| Gregory A. Otterson, MD | Abraxis Oncology; Boehringer Ingelheim GmbH; Celgene Corporation; Eli Lilly and Company; Genentech, Inc.; Pfizer Inc.; and Pharmacyclics, Inc. | Abraxis Bioscience, Inc.; and Genentech, Inc. | None | None | 6/21/11 |
| Kimberly Peairs, MD | None | None | None | None | 7/15/11 |
| Sudhakar Pipavath, MD | GE Healthcare | None | None | None | 11/19/10 |
| Christie Pratt-Pozo, MA, DHSc | None | None | None | None | 9/9/11 |
| Chakravarthy Reddy, MD | None | None | None | None | 11/9/11 |
| Mary E. Reid, PhD | None | None | None | None | 7/26/11 |
| Arnold J. Rotter, MD | None | None | None | None | 7/21/11 |
| Matthew B. Schabath, PhD | None | None | None | None | 3/31/11 |
| Lecia V. Sequist, MD, MPH | None | None | None | None | 12/7/10 |
| Betty C. Tong, MD, MHS | None | None | None | None | 7/22/11 |
| William D. Travis, MD | None | None | None | None | 7/26/11 |
| Michael Unger, MD, FCCP | None | None | None | None | 9/12/11 |
| Douglas E. Wood, MD | None | None | None | None | 4/5/11 |
| Stephen C. Yang, MD | None | None | None | None | 5/26/11 |
NCCN Clinical Practice Guidelines in Oncology for Lung Cancer Screening
Key Words
NCCN Clinical Practice Guidelines, NCCN Guidelines, lung cancer, screening, LDCT, smoking, carcinogen, tobacco (JNCCN 2012;10:240–265)
NCCN Categories of Evidence and Consensus
Category 1: Based upon high-level evidence, there is uniform NCCN consensus that the intervention is appropriate.
Category 2A: Based upon lower-level evidence, there is uniform NCCN consensus that the intervention is appropriate.
Category 2B: Based upon lower-level evidence, there is NCCN consensus that the intervention is appropriate.
Category 3: Based upon any level of evidence, there is major NCCN disagreement that the intervention is appropriate.
All recommendations are category 2A unless otherwise noted.
Clinical trials: NCCN believes that the best management for any cancer patient is in a clinical trial. Participation in clinical trials is especially encouraged.
Please Note
The NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®) are a statement of consensus of the authors regarding their views of currently accepted approaches to treatment. Any clinician seeking to apply or consult the NCCN Guidelines® is expected to use independent medical judgment in the context of individual clinical circumstances to determine any patient’s care or treatment. The National Comprehensive Cancer Network® (NCCN®) makes no representation or warranties of any kind regarding their content, use, or application and disclaims any responsibility for their applications or use in any way.
© National Comprehensive Cancer Network, Inc. 2012, All rights reserved. The NCCN Guidelines and the illustrations herein may not be reproduced in any form without the express written permission of NCCN.
Disclosures for the NCCN Guidelines Panel for Lung Cancer Screening
At the beginning of each NCCN Guidelines panel meeting, panel members disclosed any financial support they have received from industry. Through 2008, this information was published in an aggregate statement in JNCCN and online. Furthering NCCN’s commitment to public transparency, this disclosure process has now been expanded by listing all potential conflicts of interest respective to each individual expert panel member.
Individual disclosures for the NCCN Lung Cancer Screening Panel members can be found on page 265. (The most recent version of these guidelines and accompanying disclosures, including levels of compensation, are available on the NCCN Web site at www.NCCN.org.)
These guidelines are also available on the Internet. For the latest update, visit www.NCCN.org.
aSmokers should always be encouraged to quit smoking (http://www.smokefree.gov/).
bDocumented high radon exposure.
cAgents that are identified specifically as carcinogens targeting the lungs: silica, cadmium, asbestos, arsenic, beryllium, chromium, diesel fumes, and nickel.
dThere is increased risk of developing new primary lung cancer among survivors of lung cancer, lymphomas, cancers of the head and neck, or smoking-related cancers.
eIndividuals exposed to secondhand smoke have a highly variable exposure to the carcinogens, with varying evidence for increased risk after this variable exposure. Therefore, secondhand smoke is not independently considered a risk factor for lung cancer screening.
fAll screening and follow-up CT scans should be performed at low dose (100–120 kVp and 40–60 mAs or less), unless evaluating mediastinal abnormalities or lymph nodes, for which standard-dose CT with IV contrast might be appropriate.
gWithout benign pattern of calcification, fat in nodule as in hamartoma, or features suggesting inflammatory etiology. When multiple nodules are present and occult infection or inflammation is a possibility, an added option is a course of a broad-spectrum antibiotic with anaerobic coverage, followed by low-dose CT 1–2 mo later.
hIf new nodule at annual or follow-up LDCT, see page 245. New nodule is defined as ≥ 3 mm in mean diameter
iThere is uncertainty about the appropriate duration of screening and the age at which screening is no longer appropriate.
jMean diameter is the mean of the longest diameter of the nodule and its perpendicular diameter when compared with the baseline scan.
kFor nodules ≤ 15 mm: increase in mean diameter ≥ 2 mm in any nodule or in the solid portion of a part solid nodule compared with baseline scan. For nodules ≥ 15 mm: increase in mean diameter of ≥ 15% compared with baseline scan.
lRapid increase in size should raise suspicion of inflammatory etiology or malignancy other than NSCLC.
mNew nodule is defined as ≥ 3 mm in mean diameter.
nPET-CT for lesions ≥ 8 mm.
*To view the most recent version of these guidelines, visit the NCCN Web site at www.NCCN.org.
RISKS/BENEFITS OF LUNG CANCER SCREENING
RISKS
Futile detection of small aggressive tumors or indolent disease
- Quality of life
- Anxiety of test findings
Physical complications from diagnostic workup
False-positive results
False-negative results
Unnecessary testing
Radiation exposure
Cost
BENEFITS
Decreased lung cancer mortality
- Quality of life
- Reduction in disease-related morbidity
- Reduction in treatment-related morbidity
- Improvement in healthy lifestyles
- Reduction in anxiety/psychosocial burden
Cost-effectiveness
Footnotes
The NCCN guidelines staff have no conflicts to disclose.
Clinical trials: NCCN believes that the best management of any cancer patient is in a clinical trial. Participation in clinical trials is especially encouraged. All recommendations are category 2A unless otherwise indicated.
Contributor Information
Douglas E. Wood, University of Washington/Seattle Cancer Care Alliance.
George A. Eapen, The University of Texas MD Anderson Cancer Center.
David S. Ettinger, The Sidney Kimmel Comprehensive Cancer Center at Johns Hopkins.
Lifang Hou, Robert H. Lurie Comprehensive Cancer Center of Northwestern University.
David M. Jackman, Dana-Farber/Brigham and Women’s Cancer Center.
Ella Kazerooni, University of Michigan Comprehensive Cancer Center.
Donald Klippenstein, H. Lee Moffitt Cancer Center & Research Institute.
Rudy P. Lackner, UNMC Eppley Cancer Center at The Nebraska Medical Center.
Lorriana Leard, UCSF Helen Diller Family Comprehensive Cancer Center.
Ann N. C. Leung, Stanford Comprehensive Cancer Center.
Pierre P. Massion, Vanderbilt-Ingram Cancer Center.
Bryan F. Meyers, Siteman Cancer Center at Barnes-Jewish Hospital and Washington University School of Medicine.
Reginald F. Munden, The University of Texas MD Anderson Cancer Center.
Gregory A. Otterson, The Ohio State University Comprehensive Cancer Center – James Cancer Hospital and Solove Research Institute.
Kimberly Peairs, The Sidney Kimmel Comprehensive Cancer Center at Johns Hopkins.
Sudhakar Pipavath, University of Washington/Seattle Cancer Care Alliance.
Christie Pratt-Pozo, H. Lee Moffitt Cancer Center & Research Institute.
Chakravarthy Reddy, Huntsman Cancer Institute at the University of Utah.
Mary E. Reid, Roswell Park Cancer Institute.
Arnold J. Rotter, City of Hope Comprehensive Cancer Center.
Matthew B. Schabath, H. Lee Moffitt Cancer Center & Research Institute.
Lecia V. Sequist, Massachusetts General Hospital Cancer Center.
Betty C. Tong, Duke Cancer Institute.
William D. Travis, Memorial Sloan-Kettering Cancer Center.
Michael Unger, Fox Chase Cancer Center.
Stephen C. Yang, The Sidney Kimmel Comprehensive Cancer Center at Johns Hopkins.
References
- 1.U.S. Department of Health and Human Services. The Health Consequences of Smoking: A Report of the Surgeon General. Atlanta: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2004. [Google Scholar]
- 2.Thun MJ, Henley SJ, Burns D, et al. Lung cancer death rates in lifelong nonsmokers. J Natl Cancer Inst 2006;98:691–699. [DOI] [PubMed] [Google Scholar]
- 3.Jemal A, Bray F, Center MM, et al. Global cancer statistics. CA Cancer J Clin 2011;61:69–90. [DOI] [PubMed] [Google Scholar]
- 4.Siegel R, Ward E, Brawley O, Jemal A. Cancer statistics, 2011: the impact of eliminating socioeconomic and racial disparities on premature cancer deaths. CA Cancer J Clin 2011;61:212–236. [DOI] [PubMed] [Google Scholar]
- 5.Goldstraw P, Crowley J, Chansky K, et al. The IASLC Lung Cancer Staging Project: proposals for the revision of the TNM stage groupings in the forthcoming (seventh) edition of the TNM classification of malignant tumours. J Thorac Oncol 2007;2:706–714. [DOI] [PubMed] [Google Scholar]
- 6.Jemal A, Thun MJ, Ries LA, et al. Annual report to the nation on the status of cancer, 1975–2005, featuring trends in lung cancer, tobacco use, and tobacco control. J Natl Cancer Inst 2008;100:1672–1694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Aberle DR, Berg CD, Black WC, et al. The National Lung Screening Trial: overview and study design. Radiology 2011;258:243–253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Aberle DR, Adams AM, Berg CD, et al. Reduced lung-cancer mortality with low-dose computed tomographic screening. N Engl J Med 2011;365:395–409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lee CI, Forman HP. CT screening for lung cancer: implications on social responsibility. AJR Am J Roentgenol 2007;188:297–298. [DOI] [PubMed] [Google Scholar]
- 10.Welch HG, Black WC. Overdiagnosis in cancer. J Natl Cancer Inst 2010;102:605–613. [DOI] [PubMed] [Google Scholar]
- 11.Hulka BS. Cancer screening. Degrees of proof and practical application. Cancer 1988;62:1776–1780. [DOI] [PubMed] [Google Scholar]
- 12.Humphrey LL, Johnson M, Teutsch S. Lung cancer screening: an update for the U.S. Preventive Services Task Force. Available at: http://www.ncbi.nlm.nih.gov/books/NBK42872/. Accessed January 9, 2012. [PubMed]
- 13.Reich JM. A critical appraisal of overdiagnosis: estimates of its magnitude and implications for lung cancer screening. Thorax 2008;63:377–383. [DOI] [PubMed] [Google Scholar]
- 14.Godoy MC, Naidich DP. Subsolid pulmonary nodules and the spectrum of peripheral adenocarcinomas of the lung: recommended interim guidelines for assessment and management. Radiology 2009;253:606–622. [DOI] [PubMed] [Google Scholar]
- 15.Black WC. Computed tomography screening for lung cancer: review of screening principles and update on current status. Cancer 2007;110:2370–2384. [DOI] [PubMed] [Google Scholar]
- 16.van Iersel CA, de Koning HJ, Draisma G, et al. Risk-based selection from the general population in a screening trial: selection criteria, recruitment and power for the Dutch-Belgian randomised lung cancer multi-slice CT screening trial (NELSON). Int J Cancer 2007;120:868–874. [DOI] [PubMed] [Google Scholar]
- 17.Smoking-attributable mortality, years of potential life lost, and productivity losses—United States, 2000–2004. MMWR Morb Mortal Wkly Rep 2008;57:1226–1228. [PubMed] [Google Scholar]
- 18.Peto R, Darby S, Deo H, et al. Smoking, smoking cessation, and lung cancer in the UK since 1950: combination of national statistics with two case-control studies. BMJ 2000;321:323–329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Garfinkel L Time trends in lung cancer mortality among nonsmokers and a note on passive smoking. J Natl Cancer Inst 1981;66:1061–1066. [DOI] [PubMed] [Google Scholar]
- 20.U.S. Department of Health and Human Services. The Health Consequences of Involuntary Exposure to Tobacco Smoke: A Report of the Surgeon General. Atlanta, GA: U.S. Departmsnt of Health and Human Services, Centers for Disease Control and Prevention, Coordinating Center for Health Promotion, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2006. [Google Scholar]
- 21.Hackshaw AK, Law MR, Wald NJ. The accumulated evidence on lung cancer and environmental tobacco smoke. BMJ 1997;315:980–988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Driscoll T, Nelson DI, Steenland K, et al. The global burden of disease due to occupational carcinogens. Am J Ind Med 2005;48:419–431. [DOI] [PubMed] [Google Scholar]
- 23.Nelson DI, Concha-Barrientos M, Driscoll T, et al. The global burden of selected occupational diseases and injury risks: methodology and summary. Am J Ind Med 2005;48:400–418. [DOI] [PubMed] [Google Scholar]
- 24.Nurminen M, Karjalainen A. Epidemiologic estimate of the proportion of fatalities related to occupational factors in Finland. Scand J Work Environ Health 2001;27:161–213. [DOI] [PubMed] [Google Scholar]
- 25.Steenland K, Loomis D, Shy C, Simonsen N. Review of occupational lung carcinogens. Am J Ind Med 1996;29:474–490. [DOI] [PubMed] [Google Scholar]
- 26.Reid A, de Klerk NH, Ambrosini GL, et al. The risk of lung cancer with increasing time since ceasing exposure to asbestos and quitting smoking. Occup Environ Med 2006;63:509–512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.El Ghissassi F, Baan R, Straif K, et al. A review of human carcinogens—part D: radiation. Lancet Oncol 2009;10:751–752. [DOI] [PubMed] [Google Scholar]
- 28.Leuraud K, Schnelzer M, Tomasek L, et al. Radon, smoking and lung cancer risk: results of a joint analysis of three European case-control studies among uranium miners. Radiat Res 2011;176:375–387. [DOI] [PubMed] [Google Scholar]
- 29.Lubin JH, Boice JD Jr. Lung cancer risk from residential radon: meta-analysis of eight epidemiologic studies. J Natl Cancer Inst 1997;89:49–57. [DOI] [PubMed] [Google Scholar]
- 30.Darby S, Hill D, Auvinen A, et al. Radon in homes and risk of lung cancer: collaborative analysis of individual data from 13 European case-control studies. BMJ 2005;330:223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tucker MA, Murray N, Shaw EG, et al. Second primary cancers related to smoking and treatment of small-cell lung cancer. Lung Cancer Working Cadre. J Natl Cancer Inst 1997;89:1782–1788. [DOI] [PubMed] [Google Scholar]
- 32.Travis LB, Gospodarowicz M, Curtis RE, et al. Lung cancer following chemotherapy and radiotherapy for Hodgkin’s disease. J Natl Cancer Inst 2002;94:182–192. [DOI] [PubMed] [Google Scholar]
- 33.Jones AS, Morar P, Phillips DE, et al. Second primary tumors in patients with head and neck squamous cell carcinoma. Cancer 1995;75:1343–1353. [DOI] [PubMed] [Google Scholar]
- 34.Atabek U, Mohit-Tabatabai MA, Raina S, et al. Lung cancer in patients with head and neck cancer. Incidence and long-term survival. Am J Surg 1987;154:434–438. [DOI] [PubMed] [Google Scholar]
- 35.Richardson GE, Tucker MA, Venzon DJ, et al. Smoking cessation after successful treatment of small-cell lung cancer is associated with fewer smoking-related second primary cancers. Ann Intern Med 1993;119:383–390. [DOI] [PubMed] [Google Scholar]
- 36.Jonsson S, Thorsteinsdottir U, Gudbjartsson DF, et al. Familial risk of lung carcinoma in the Icelandic population. JAMA 2004;292:2977–2983. [DOI] [PubMed] [Google Scholar]
- 37.Li X, Hemminki K. Familial multiple primary lung cancers: a population-based analysis from Sweden. Lung Cancer 2005;47:301–307. [DOI] [PubMed] [Google Scholar]
- 38.Matakidou A, Eisen T, Houlston RS. Systematic review of the relationship between family history and lung cancer risk. Br J Cancer 2005;93:825–833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bailey-Wilson JE, Amos CI, Pinney SM, et al. A major lung cancer susceptibility locus maps to chromosome 6q23–25. Am J Hum Genet 2004;75:460–474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Thorgeirsson TE, Geller F, Sulem P, et al. A variant associated with nicotine dependence, lung cancer and peripheral arterial disease. Nature 2008;452:638–642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hung RJ, McKay JD, Gaborieau V, et al. A susceptibility locus for lung cancer maps to nicotinic acetylcholine receptor subunit genes on 15q25. Nature 2008;452:633–637. [DOI] [PubMed] [Google Scholar]
- 42.Amos CI, Wu X, Broderick P, et al. Genome-wide association scan of tag SNPs identifies a susceptibility locus for lung cancer at 15q25.1. Nat Genet 2008;40:616–622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lambrechts D, Buysschaert I, Zanen P, et al. The 15q24/25 susceptibility variant for lung cancer and chronic obstructive pulmonary disease is associated with emphysema. Am J Respir Crit Care Med 2010;181:486–493. [DOI] [PubMed] [Google Scholar]
- 44.Hwang SJ, Cheng LS, Lozano G, et al. Lung cancer risk in germline p53 mutation carriers: association between an inherited cancer predisposition, cigarette smoking, and cancer risk. Hum Genet 2003;113:238–243. [DOI] [PubMed] [Google Scholar]
- 45.Sanders BM, Jay M, Draper GJ, Roberts EM. Non-ocular cancer in relatives of retinoblastoma patients. Br J Cancer 1989;60:358–365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Fletcher O, Easton D, Anderson K, et al. Lifetime risks of common cancers among retinoblastoma survivors. J Natl Cancer Inst 2004;96:357–363. [DOI] [PubMed] [Google Scholar]
- 47.Mayne ST, Buenconsejo J, Janerich DT. Previous lung disease and risk of lung cancer among men and women nonsmokers. Am J Epidemiol 1999;149:13–20. [DOI] [PubMed] [Google Scholar]
- 48.Samet JM, Humble CG, Pathak DR. Personal and family history of respiratory disease and lung cancer risk. Am Rev Respir Dis 1986;134:466–470. [DOI] [PubMed] [Google Scholar]
- 49.Alavanja MC, Brownson RC, Boice JD Jr, Hock E. Preexisting lung disease and lung cancer among nonsmoking women. Am J Epidemiol 1992;136:623–632. [DOI] [PubMed] [Google Scholar]
- 50.Wu-Williams AH, Dai XD, Blot W, et al. Lung cancer among women in north-east China. Br J Cancer 1990;62:982–987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Gao YT, Blot WJ, Zheng W, et al. Lung cancer among Chinese women. Int J Cancer 1987;40:604–609. [DOI] [PubMed] [Google Scholar]
- 52.Brenner AV, Wang Z, Kleinerman RA, et al. Previous pulmonary diseases and risk of lung cancer in Gansu Province, China. Int J Epidemiol 2001;30:118–124. [DOI] [PubMed] [Google Scholar]
- 53.Skillrud DM, Offord KP, Miller RD. Higher risk of lung cancer in chronic obstructive pulmonary disease. A prospective, matched, controlled study. Ann Intern Med 1986;105:503–507. [DOI] [PubMed] [Google Scholar]
- 54.Yang P, Sun Z, Krowka MJ, et al. Alpha1-antitrypsin deficiency carriers, tobacco smoke, chronic obstructive pulmonary disease, and lung cancer risk. Arch Intern Med 2008;168:1097–1103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Koshiol J, Rotunno M, Consonni D, et al. Chronic obstructive pulmonary disease and altered risk of lung cancer in a population-based case-control study. PLoS One 2009;4:e7380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Turner MC, Chen Y, Krewski D, et al. Chronic obstructive pulmonary disease is associated with lung cancer mortality in a prospective study of never smokers. Am J Respir Crit Care Med 2007;176:285–290. [DOI] [PubMed] [Google Scholar]
- 57.Turner-Warwick M, Lebowitz M, Burrows B, Johnson A. Cryptogenic fibrosing alveolitis and lung cancer. Thorax 1980;35:496–499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Hubbard R, Venn A, Lewis S, Britton J. Lung cancer and cryptogenic fibrosing alveolitis. A population-based cohort study. Am J Respir Crit Care Med 2000;161:5–8. [DOI] [PubMed] [Google Scholar]
- 59.Hughes JM, Weill H. Asbestosis as a precursor of asbestos related lung cancer: results of a prospective mortality study. Br J Ind Med 1991;48:229–233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Chlebowski RT, Schwartz AG, Wakelee H, et al. Oestrogen plus progestin and lung cancer in postmenopausal women (Women’s Health Initiative trial): a post-hoc analysis of a randomised controlled trial. Lancet 2009;374:1243–1251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Henschke CI, Yankelevitz DF, Libby DM, et al. Survival of patients with stage I lung cancer detected on CT screening. N Engl J Med 2006;355:1763–1771. [DOI] [PubMed] [Google Scholar]
- 62.Li F, Sone S, Abe H, et al. Malignant versus benign nodules at CT screening for lung cancer: comparison of thin-section CT findings. Radiology 2004;233:793–798. [DOI] [PubMed] [Google Scholar]
- 63.Kim HY, Shim YM, Lee KS, et al. Persistent pulmonary nodular ground-glass opacity at thin-section CT: histopathologic comparisons. Radiology 2007;245:267–275. [DOI] [PubMed] [Google Scholar]
- 64.Travis WD, Brambilla E, Noguchi M, et al. International association for the study of lung cancer/american thoracic society/european respiratory society international multidisciplinary classification of lung adenocarcinoma. J Thorac Oncol 2011;6:244–285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Fischbach F, Knollmann F, Griesshaber V, et al. Detection of pulmonary nodules by multislice computed tomography: improved detection rate with reduced slice thickness. Eur Radiol 2003;13:2378–2383. [DOI] [PubMed] [Google Scholar]
- 66.Valencia R, Denecke T, Lehmkuhl L, et al. Value of axial and coronal maximum intensity projection (MIP) images in the detection of pulmonary nodules by multislice spiral CT: comparison with axial 1-mm and 5-mm slices. Eur Radiol 2006;16:325–332. [DOI] [PubMed] [Google Scholar]
- 67.Kawel N, Seifert B, Luetolf M, Boehm T. Effect of slab thickness on the CT detection of pulmonary nodules: use of sliding thin-slab maximum intensity projection and volume rendering. AJR Am J Roentgenol 2009;192:1324–1329. [DOI] [PubMed] [Google Scholar]
- 68.Peloschek P, Sailer J, Weber M, et al. Pulmonary nodules: sensitivity of maximum intensity projection versus that of volume rendering of 3D multidetector CT data. Radiology 2007;243:561–569. [DOI] [PubMed] [Google Scholar]
- 69.Park EA, Goo JM, Lee JW, et al. Efficacy of computer-aided detection system and thin-slab maximum intensity projection technique in the detection of pulmonary nodules in patients with resected metastases. Invest Radiol 2009;44:105–113. [DOI] [PubMed] [Google Scholar]
- 70.Jankowski A, Martinelli T, Timsit JF, et al. Pulmonary nodule detection on MDCT images: evaluation of diagnostic performance using thin axial images, maximum intensity projections, and computer-assisted detection. Eur Radiol 2007;17:3148–3156. [DOI] [PubMed] [Google Scholar]
- 71.Rubin GD, Lyo JK, Paik DS, et al. Pulmonary nodules on multi-detector row CT scans: performance comparison of radiologists and computer-aided detection. Radiology 2005;234:274–283. [DOI] [PubMed] [Google Scholar]
- 72.Fraioli F, Bertoletti L, Napoli A, et al. Computer-aided detection (CAD) in lung cancer screening at chest MDCT: ROC analysis of CAD versus radiologist performance. J Thorac Imaging 2007;22:241–246. [DOI] [PubMed] [Google Scholar]
- 73.Sahiner B, Chan HP, Hadjiiski LM, et al. Effect of CAD on radiologists’ detection of lung nodules on thoracic CT scans: analysis of an observer performance study by nodule size. Acad Radiol 2009;16:1518–1530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Das M, Muhlenbruch G, Heinen S, et al. Performance evaluation of a computer-aided detection algorithm for solid pulmonary nodules in low-dose and standard-dose MDCT chest examinations and its influence on radiologists. Br J Radiol 2008;81:841–847. [DOI] [PubMed] [Google Scholar]
- 75.Lee HY, Goo JM, Lee HJ, et al. Usefulness of concurrent reading using thin-section and thick-section CT images in subcentimetre solitary pulmonary nodules. Clin Radiol 2009;64:127–132. [DOI] [PubMed] [Google Scholar]
- 76.Kubo T, Lin PJ, Stiller W, et al. Radiation dose reduction in chest CT: a review. AJR Am J Roentgenol 2008;190:335–343. [DOI] [PubMed] [Google Scholar]
- 77.Lee JY, Chung MJ, Yi CA, Lee KS. Ultra-low-dose MDCT of the chest: influence on automated lung nodule detection. Korean J Radiol 2008;9:95–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Funama Y, Awai K, Liu D, et al. Detection of nodules showing ground-glass opacity in the lungs at low-dose multidetector computed tomography: phantom and clinical study. J Comput Assist Tomogr 2009;33:49–53. [DOI] [PubMed] [Google Scholar]
- 79.Hein PA, Romano VC, Rogalla P, et al. Linear and volume measurements of pulmonary nodules at different CT dose levels— intrascan and interscan analysis. Rofo 2009;181:24–31. [DOI] [PubMed] [Google Scholar]
- 80.Singh S, Pinsky P, Fineberg NS, et al. Evaluation of reader variability in the interpretation of follow-up CT scans at lung cancer screening. Radiology 2011;259:263–270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Gierada DS, Pilgram TK, Ford M, et al. Lung cancer: interobserver agreement on interpretation of pulmonary findings at low-dose CT screening. Radiology 2008;246:265–272. [DOI] [PubMed] [Google Scholar]
- 82.Henschke CI, Boffetta P, Gorlova O, et al. Assessment of lung-cancer mortality reduction from CT screening. Lung Cancer 2011;71:328–332. [DOI] [PubMed] [Google Scholar]
- 83.van Klaveren RJ, Oudkerk M, Prokop M, et al. Management of lung nodules detected by volume CT scanning. N Engl J Med 2009;361:2221–2229. [DOI] [PubMed] [Google Scholar]
- 84.Lopes Pegna A, Picozzi G, Mascalchi M, et al. Design, recruitment and baseline results of the ITALUNG trial for lung cancer screening with low-dose CT. Lung Cancer 2009;64:34–40. [DOI] [PubMed] [Google Scholar]
- 85.Pedersen JH, Ashraf H, Dirksen A, et al. The Danish randomized lung cancer CT screening trial—overall design and results of the prevalence round. J Thorac Oncol 2009;4:608–614. [DOI] [PubMed] [Google Scholar]
- 86.Menezes RJ, Roberts HC, Paul NS, et al. Lung cancer screening using low-dose computed tomography in at-risk individuals: the Toronto experience. Lung Cancer 2010;67:177–183. [DOI] [PubMed] [Google Scholar]
- 87.Veronesi G, Bellomi M, Scanagatta P, et al. Difficulties encountered managing nodules detected during a computed tomography lung cancer screening program. J Thorac Cardiovasc Surg 2008;136:611–617. [DOI] [PubMed] [Google Scholar]
- 88.Infante M, Cavuto S, Lutman FR, et al. A randomized study of lung cancer screening with spiral computed tomography: three-year results from the DANTE trial. Am J Respir Crit Care Med 2009;180:445–453. [DOI] [PubMed] [Google Scholar]
- 89.Swensen SJ, Jett JR, Hartman TE, et al. Lung cancer screening with CT: Mayo Clinic experience. Radiology 2003;226:756–761. [DOI] [PubMed] [Google Scholar]
- 90.Henschke CI, Yankelevitz DF, Naidich DP, et al. CT screening for lung cancer: suspiciousness of nodules according to size on baseline scans. Radiology 2004;231:164–168. [DOI] [PubMed] [Google Scholar]
- 91.Henschke CI, Yankelevitz DF, Miettinen OS. Computed tomographic screening for lung cancer: the relationship of disease stage to tumor size. Arch Intern Med 2006;166:321–325. [DOI] [PubMed] [Google Scholar]
- 92.Steele JD, Buell P. Asymptomatic solitary pulmonary nodules. Host survival, tumor size, and growth rate. J Thorac Cardiovasc Surg 1973;65:140–151. [PubMed] [Google Scholar]
- 93.Galante E, Reduzzi D, Gallus G, et al. The growth rate in the interpretation of the natural history of lung cancer. Tumori 1984;70:427–432. [DOI] [PubMed] [Google Scholar]
- 94.Usuda K, Saito Y, Sagawa M, et al. Tumor doubling time and prognostic assessment of patients with primary lung cancer. Cancer 1994;74:2239–2244. [DOI] [PubMed] [Google Scholar]
- 95.Arai T, Kuroishi T, Saito Y, et al. Tumor doubling time and prognosis in lung cancer patients: evaluation from chest films and clinical follow-up study. Japanese Lung Cancer Screening Research Group. Jpn J Clin Oncol 1994;24:199–204. [PubMed] [Google Scholar]
- 96.Weiss W, Boucot KR, Cooper DA. The histopathology of bronchogenic carcinoma and its relation to growth rate, metastasis, and prognosis. Cancer 1970;26:965–970. [DOI] [PubMed] [Google Scholar]
- 97.Swensen SJ, Viggiano RW, Midthun DE, et al. Lung nodule enhancement at CT: multicenter study. Radiology 2000;214:73–80. [DOI] [PubMed] [Google Scholar]
- 98.Yi CA, Lee KS, Kim BT, et al. Tissue characterization of solitary pulmonary nodule: comparative study between helical dynamic CT and integrated PET/CT. J Nucl Med 2006;47:443–450. [PubMed] [Google Scholar]
- 99.Christensen JA, Nathan MA, Mullan BP, et al. Characterization of the solitary pulmonary nodule: 18F-FDG PET versus nodule-enhancement CT. AJR Am J Roentgenol 2006;187:1361–1367. [DOI] [PubMed] [Google Scholar]
- 100.Schillaci O, Travascio L, Bolacchi F, et al. Accuracy of early and delayed FDG PET-CT and of contrast-enhanced CT in the evaluation of lung nodules: a preliminary study on 30 patients. Radiol Med 2009;114:890–906. [DOI] [PubMed] [Google Scholar]
- 101.Bastarrika G, Garcia-Velloso MJ, Lozano MD, et al. Early lung cancer detection using spiral computed tomography and positron emission tomography. Am J Respir Crit Care Med 2005;171:1378–1383. [DOI] [PubMed] [Google Scholar]
- 102.Ashraf H, Dirksen A, Loft A, et al. Combined use of positron emission tomography and volume doubling time in lung cancer screening with low-dose CT scanning. Thorax 2011;66:315–319. [DOI] [PubMed] [Google Scholar]
- 103.Ohno Y, Koyama H, Matsumoto K, et al. Differentiation of malignant and benign pulmonary nodules with quantitative first-pass 320-detector row perfusion CT versus FDG PET/CT. Radiology 2011;258:599–609. [DOI] [PubMed] [Google Scholar]
- 104.Liu X, Liang M, Wang Y, et al. The outcome differences of CT screening for lung cancer pre and post following an algorithm in Zhuhai, China. Lung Cancer 2011;73:230–236. [DOI] [PubMed] [Google Scholar]
- 105.CT screening for lung cancer: diagnoses resulting from the New York Early Lung Cancer Action Project. Radiology 2007;243:239–249. [DOI] [PubMed] [Google Scholar]
- 106.MacMahon H, Austin JHM, Gamsu G, et al. Guidelines for management of small pulmonary nodules detected on CT scans: a statement from the Fleischner Society. Radiology 2005;237:395–400. [DOI] [PubMed] [Google Scholar]
- 107.Eisenberg RL, Bankier AA, Boiselle PM. Compliance with Fleischner Society guidelines for management of small lung nodules: a survey of 834 radiologists. Radiology 2010;255:218–224. [DOI] [PubMed] [Google Scholar]
- 108.Revel MP, Bissery A, Bienvenu M, et al. Are two-dimensional CT measurements of small noncalcified pulmonary nodules reliable? Radiology 2004;231:453–458. [DOI] [PubMed] [Google Scholar]
- 109.Hanaoka T, Sone S, Takayama F, et al. Presence of local pleural adhesion in CT screening-detected small nodule in the lung periphery suggests noncancerous, inflammatory nature of the lesion. Clin Imaging 2007;31:385–389. [DOI] [PubMed] [Google Scholar]
- 110.Ahn MI, Gleeson TG, Chan IH, et al. Perifissural nodules seen at CT screening for lung cancer. Radiology 2010;254:949–956. [DOI] [PubMed] [Google Scholar]
- 111.Xu DM, van der Zaag-Loonen HJ, Oudkerk M, et al. Smooth or attached solid indeterminate nodules detected at baseline CT screening in the NELSON study: cancer risk during 1 year of follow-up. Radiology 2009;250:264–272. [DOI] [PubMed] [Google Scholar]
- 112.Bankier AA, Tack D. Dose reduction strategies for thoracic multidetector computed tomography: background, current issues, and recommendations. J Thorac Imaging 2010;25:278–288. [DOI] [PubMed] [Google Scholar]
- 113.Lee TY, Chhem RK. Impact of new technologies on dose reduction in CT. Eur J Radiol 2010;76:28–35. [DOI] [PubMed] [Google Scholar]
- 114.Pontana F, Pagniez J, Flohr T, et al. Chest computed tomography using iterative reconstruction vs filtered back projection (Part 1): evaluation of image noise reduction in 32 patients. Eur Radiol 2011;21:627–635. [DOI] [PubMed] [Google Scholar]
- 115.Pontana F, Duhamel A, Pagniez J, et al. Chest computed tomography using iterative reconstruction vs filtered back projection (Part 2): image quality of low-dose CT examinations in 80 patients. Eur Radiol 2011;21:636–643. [DOI] [PubMed] [Google Scholar]
- 116.Rami-Porta R, Ball D, Crowley J, et al. The IASLC Lung Cancer Staging Project: proposals for the revision of the T descriptors in the forthcoming (seventh) edition of the TNM classification for lung cancer. J Thorac Oncol 2007;2:593–602. [DOI] [PubMed] [Google Scholar]
- 117.Edge SB, Byrd DR, Compton CC. AJCC Cancer Staging Manual, 7th ed New York: Springer; 2010. [Google Scholar]
- 118.Flieder DB, Vazquez M, Carter D, et al. Pathologic findings of lung tumors diagnosed on baseline CT screening. Am J Surg Pathol 2006;30:606–613. [DOI] [PubMed] [Google Scholar]
- 119.Hall FM. Identification, biopsy, and treatment of poorly understood premalignant, in situ, and indolent low-grade cancers: are we becoming victims of our own success? Radiology 2010;254:655–659. [DOI] [PubMed] [Google Scholar]
- 120.Raz DJ, Zell JA, Ou SH, et al. Natural history of stage I non-small cell lung cancer: implications for early detection. Chest 2007;132:193–199. [DOI] [PubMed] [Google Scholar]
- 121.Bach PB, Jett JR, Pastorino U, et al. Computed tomography screening and lung cancer outcomes. JAMA 2007;297:953–961. [DOI] [PubMed] [Google Scholar]
- 122.Sox HC. Better evidence about screening for lung cancer. N Engl J Med 2011;365:455–457. [DOI] [PubMed] [Google Scholar]
- 123.Carter D, Vazquez M, Flieder DB, et al. Comparison of pathologic findings of baseline and annual repeat cancers diagnosed on CT screening. Lung Cancer 2007;56:193–199. [DOI] [PubMed] [Google Scholar]
- 124.Foy M, Yip R, Chen X, et al. Modeling the mortality reduction due to computed tomography screening for lung cancer. Cancer 2011;117:2703–2708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Tabar L, Vitak B, Chen TH, et al. Swedish two-county trial: impact of mammographic screening on breast cancer mortality during 3 decades. Radiology 2011;260:658–663. [DOI] [PubMed] [Google Scholar]
- 126.Molina JR, Yang P, Cassivi SD, et al. Non-small cell lung cancer: epidemiology, risk factors, treatment, and survivorship. Mayo Clin Proc 2008;83:584–594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Spira A, Ettinger DS. Multidisciplinary management of lung cancer. N Engl J Med 2004;350:379–392. [DOI] [PubMed] [Google Scholar]
- 128.Manser R, Wright G, Hart D, et al. Surgery for early stage non-small cell lung cancer. Cochrane Database Syst Rev 2005:CD004699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Albain KS, Swann RS, Rusch VW, et al. Radiotherapy plus chemotherapy with or without surgical resection for stage III non-small-cell lung cancer: a phase III randomised controlled trial. Lancet 2009;374:379–386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Crestanello JA, Allen MS, Jett JR, et al. Thoracic surgical operations in patients enrolled in a computed tomographic screening trial. J Thorac Cardiovasc Surg 2004;128:254–259. [DOI] [PubMed] [Google Scholar]
- 131.Grannis FW. Can we avert the need for pneumonectomy by screening for lung cancer? Eur J Cardiothorac Surg 2004;25:296. [DOI] [PubMed] [Google Scholar]
- 132.Henschke CI, McCauley DI, Yankelevitz DF, et al. Early Lung Cancer Action Project: overall design and findings from baseline screening. Lancet 1999;354:99–105. [DOI] [PubMed] [Google Scholar]
- 133.Sone S, Nakayama T, Honda T, et al. Long-term follow-up study of a population-based 1996–1998 mass screening programme for lung cancer using mobile low-dose spiral computed tomography. Lung Cancer 2007;58:329–341. [DOI] [PubMed] [Google Scholar]
- 134.Townsend CO, Clark MM, Jett JR, et al. Relation between smoking cessation and receiving results from three annual spiral chest computed tomography scans for lung carcinoma screening. Cancer 2005;103:2154–2162. [DOI] [PubMed] [Google Scholar]
- 135.Ashraf H, Tonnesen P, Holst Pedersen J, et al. Effect of CT screening on smoking habits at 1-year follow-up in the Danish Lung Cancer Screening Trial (DLCST). Thorax 2009;64:388–392. [DOI] [PubMed] [Google Scholar]
- 136.Taylor KL, Cox LS, Zincke N, et al. Lung cancer screening as a teachable moment for smoking cessation. Lung Cancer 2007;56:125–134. [DOI] [PubMed] [Google Scholar]
- 137.van den Bergh KA, Essink-Bot ML, Borsboom GJ, et al. Short-term health-related quality of life consequences in a lung cancer CT screening trial (NELSON). Br J Cancer 2010;102:27–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.van den Bergh KA, Essink-Bot ML, Borsboom GJ, et al. Long-term effects of lung cancer computed tomography screening on health-related quality of life: the NELSON trial. Eur Respir J 2011;38:154–161. [DOI] [PubMed] [Google Scholar]
- 139.Bunge EM, van den Bergh KA, Essink-Bot ML, et al. High affective risk perception is associated with more lung cancer-specific distress in CT screening for lung cancer. Lung Cancer 2008;62:385–390. [DOI] [PubMed] [Google Scholar]
- 140.Castleberry AW, Smith D, Anderson C, et al. Cost of a 5-year lung cancer survivor: symptomatic tumour identification vs proactive computed tomography screening. Br J Cancer 2009;101:882–896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Croswell JM, Baker SG, Marcus PM, et al. Cumulative incidence of false-positive test results in lung cancer screening: a randomized trial. Ann Intern Med 2010;152:505–512. [DOI] [PubMed] [Google Scholar]
- 142.Lafata JE, Simpkins J, Lamerato L, et al. The economic impact of false-positive cancer screens. Cancer Epidemiol Biomarkers Prev 2004;13:2126–2132. [PubMed] [Google Scholar]
- 143.Wisnivesky JP, Mushlin AI, Sicherman N, Henschke C. The cost-effectiveness of low-dose CT screening for lung cancer: preliminary results of baseline screening. Chest 2003;124:614–621. [DOI] [PubMed] [Google Scholar]
- 144.Chirikos TN, Hazelton T, Tockman M, Clark R. Screening for lung cancer with CT: a preliminary cost-effectiveness analysis. Chest 2002;121:1507–1514. [DOI] [PubMed] [Google Scholar]
- 145.Diederich S, Wormanns D, Semik M, et al. Screening for early lung cancer with low-dose spiral CT: prevalence in 817 asymptomatic smokers. Radiology 2002;222:773–781. [DOI] [PubMed] [Google Scholar]
- 146.Gohagan JK, Marcus PM, Fagerstrom RM, et al. Final results of the Lung Screening Study, a randomized feasibility study of spiral CT versus chest X-ray screening for lung cancer. Lung Cancer 2005;47:9–15. [DOI] [PubMed] [Google Scholar]
- 147.Kaneko M, Eguchi K, Ohmatsu H, et al. Peripheral lung cancer: screening and detection with low-dose spiral CT versus radiography. Radiology 1996;201:798–802. [DOI] [PubMed] [Google Scholar]
- 148.Swensen SJ, Jett JR, Hartman TE, et al. CT screening for lung cancer: five-year prospective experience. Radiology 2005;235:259–265. [DOI] [PubMed] [Google Scholar]
- 149.Wiener RS, Schwartz LM, Woloshin S, Welch HG. Population-based risk for complications after transthoracic needle lung biopsy of a pulmonary nodule: an analysis of discharge records. Ann Intern Med 2011;155:137–144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Henschke CI, Yip R, Yankelevitz DF, Miettinen OS. Computed tomography screening for lung cancer: prospects of surviving competing causes of death. Clin Lung Cancer 2006;7:323–325. [DOI] [PubMed] [Google Scholar]
- 151.Bach PB, Cramer LD, Schrag D, et al. The influence of hospital volume on survival after resection for lung cancer. N Engl J Med 2001;345:181–188. [DOI] [PubMed] [Google Scholar]
- 152.Silvestri GA, Handy J, Lackland D, et al. Specialists achieve better outcomes than generalists for lung cancer surgery. Chest 1998;114:675–680. [DOI] [PubMed] [Google Scholar]
- 153.Stephan F, Boucheseiche S, Hollande J, et al. Pulmonary complications following lung resection: a comprehensive analysis of incidence and possible risk factors. Chest 2000;118:1263–1270. [DOI] [PubMed] [Google Scholar]
- 154.Sone S, Takashima S, Li F, et al. Mass screening for lung cancer with mobile spiral computed tomography scanner. Lancet 1998;351:1242–1245. [DOI] [PubMed] [Google Scholar]
- 155.Li F, Sone S, Abe H, et al. Lung cancers missed at low-dose helical CT screening in a general population: comparison of clinical, histopathologic, and imaging findings. Radiology 2002;225:673–683. [DOI] [PubMed] [Google Scholar]
- 156.Armato SG, Li F, Giger ML, et al. Lung cancer: performance of automated lung nodule detection applied to cancers missed in a CT screening program. Radiology 2002;225:685–692. [DOI] [PubMed] [Google Scholar]
- 157.DeVita VT Jr, Young RC, Canellos GP. Combination versus single agent chemotherapy: a review of the basis for selection of drug treatment of cancer. Cancer 1975;35:98–110. [DOI] [PubMed] [Google Scholar]
- 158.Folkman J Seminars in Medicine of the Beth Israel Hospital, Boston. Clinical applications of research on angiogenesis. N Engl J Med 1995;333:1757–1763. [DOI] [PubMed] [Google Scholar]
- 159.Swartz MA, Kristensen CA, Melder RJ, et al. Cells shed from tumours show reduced clonogenicity, resistance to apoptosis, and in vivo tumorigenicity. Br J Cancer 1999;81:756–759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Patz EF, Black WC, Goodman PC. CT screening for lung cancer: not ready for routine practice. Radiology 2001;221:587–591. [DOI] [PubMed] [Google Scholar]
- 161.Yoshizawa A, Motoi N, Riely GJ, et al. Impact of proposed IASLC/ATS/ERS classification of lung adenocarcinoma: prognostic subgroups and implications for further revision of staging based on analysis of 514 stage I cases. Mod Pathol 2011;24:653–664. [DOI] [PubMed] [Google Scholar]
- 162.Russell PA, Wainer Z, Wright GM, et al. Does lung adenocarcinoma subtype predict patient survival?: a clinicopathologic study based on the new international association for the study of lung cancer/american thoracic society/european respiratory society international multidisciplinary lung adenocarcinoma classification. J Thorac Oncol 2011;6:1496–1504. [DOI] [PubMed] [Google Scholar]
- 163.Jett JR, Midthun DE. Commentary: CT screening for lung cancer—caveat emptor. Oncologist 2008;13:439–444. [DOI] [PubMed] [Google Scholar]
- 164.van den Bergh KA, Essink-Bot ML, Bunge EM, et al. Impact of computed tomography screening for lung cancer on participants in a randomized controlled trial (NELSON trial). Cancer 2008;113:396–404. [DOI] [PubMed] [Google Scholar]
- 165.Croswell JM, Kramer BS, Kreimer AR, et al. Cumulative incidence of false-positive results in repeated, multimodal cancer screening. Ann Fam Med 2009;7:212–222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Sistrom CL, Dreyer KJ, Dang PP, et al. Recommendations for additional imaging in radiology reports: multifactorial analysis of 5.9 million examinations. Radiology 2009;253:453–461. [DOI] [PubMed] [Google Scholar]
- 167.Berland LL, Silverman SG, Gore RM, et al. Managing incidental findings on abdominal CT: white paper of the ACR incidental findings committee. J Am Coll Radiol 2010;7:754–773. [DOI] [PubMed] [Google Scholar]
- 168.Larke FJ, Kruger RL, Cagnon CH, et al. Estimated radiation dose associated with low-dose chest CT of average-size participants in the National Lung Screening Trial. AJR Am J Roentgenol 2011;197:1165–1169. [DOI] [PubMed] [Google Scholar]
- 169.Brenner DJ. Radiation risks potentially associated with low-dose CT screening of adult smokers for lung cancer. Radiology 2004;231:440–445. [DOI] [PubMed] [Google Scholar]
- 170.Mascalchi M, Belli G, Zappa M, et al. Risk-benefit analysis of X-ray exposure associated with lung cancer screening in the Italung-CT trial. AJR Am J Roentgenol 2006;187:421–429. [DOI] [PubMed] [Google Scholar]
- 171.Mahadevia PJ, Fleisher LA, Frick KD, et al. Lung cancer screening with helical computed tomography in older adult smokers: a decision and cost-effectiveness analysis. JAMA 2003;289:313–322. [DOI] [PubMed] [Google Scholar]
- 172.Marshall D, Simpson KN, Earle CC, Chu C. Potential cost-effectiveness of one-time screening for lung cancer (LC) in a high risk cohort. Lung Cancer 2001;32:227–236. [DOI] [PubMed] [Google Scholar]