Abstract
Objective
We sought to determine clinical and demographic predictors of recovery of left ventricular function for subjects with recent onset cardiomyopathy (ROCM).
Background
While ROCM is a frequent reason for consultation and transplant referral, its prognosis and natural history on contemporary therapy are unknown.
Methods
In the multicenter Intervention in Myocarditis and Acute Cardiomyopathy (IMAC2) study, subjects with a LVEF ≤ 0.40, less than six months of symptoms and an evaluation consistent with idiopathic dilated cardiomyopathy or myocarditis were enrolled, LVEF reassessed at six months, and subjects followed for 4 years. LVEF and event free survival were compared by race, gender, and clinical phenotype.
Results
The cohort of 373 was 38% female, 21% black, with a mean age of 45 ± 14 years. At entry, 91% were receiving ACE inhibitors or ARBs and 82% beta blockers, which increased to 92% and 94% at 6 months. LVEF was 0.24 ± 0.08 at entry and 0.40±0.12 at six months (mean increase 17± 13 EF units). Transplant-free survival at 1, 2 and 4 years was 94, 92 and 88%; survival-free of heart failure hospitalization was 88, 82 and 78%. In analyses adjusted for gender, baseline LVEF, and blood pressure, LVEF at six months was significantly lower in blacks than in non-blacks (p=0.02). LVEDD at presentation was the strongest predictor of LVEF at 6 months (p<0.0001).
Conclusion
Outcomes in recent onset dilated cardiomyopathy are favorable but differ by race. LVEDD by transthoracic echo at presentation was most predictive of subsequent myocardial recovery.
Keywords: cardiomyopathy, myocardial function, outcomes, echocardiography, recovery
Introduction
Idiopathic dilated cardiomyopathy remains an important cause of systolic heart failure and the most common etiology of heart failure in young people referred for cardiac transplantation (1). With a prevalence estimated at 36 cases per one hundred thousand (2), this disorder affects well over 100,000 people in the United States alone. An inflammatory pathogenesis is suspected (3); however, endomyocardial biopsy demonstrates inflammation in only a small subset of patients (4). Treatment with immune modulatory therapy has not proven effective for recent onset cardiomyopathy (5, 6) nor in the subset with cellular myocarditis (7).
Myocardial recovery occurs in one third of subjects with recent onset non-ischemic cardiomyopathy (ROCM), defined as less than six months of cardiac symptoms. Most previous reports (8) in ROCM predate the widespread use of beta blockers, and the prognosis and natural history on contemporary therapy are mostly unknown. We initiated a multicenter investigation of myocardial recovery in subjects with ROCM to determine the demographic and clinical predictors of subsequent left ventricular recovery.
Methods
IMAC2 (Intervention in Myocarditis and Acute Cardiomyopathy 2) was a prospective multicenter investigation of myocardial recovery in subjects with recent onset (“acute”) non-ischemic dilated cardiomyopathy and myocarditis which enrolled subjects at 16 centers (Appendix) from May 2002 through December 2008. All subjects had a LVEF ≤0.40 by echocardiography, and six months of symptoms. Informed consent was obtained from all subjects, and the protocol was approved by the institutional review boards of all participating centers.
Demographic information included self-designated race (white, black, Asian, or other). Subjects underwent angiography or non-invasive screening to exclude coronary artery disease, and a transthoracic echocardiogram to rule out valvular disease. Patients with significant diabetes (requiring therapy with insulin or an oral agent for more than one year), uncontrolled hypertension (diastolic greater than 95 mmHg or systolic > 160 mmHg), suspected alcoholic or tachycardia induced cardiomyopathy, uncorrected thyroid disease, or systemic disorders with associated cardiomyopathy such as lupus erythematosus, hemochromatosis, or sarcoidosis were excluded. Right ventricular endomyocardial biopsy was not required based upon current practice guidelines (9).
LVEF was assessed by transthoracic echocardiogram at entry and six months, and patients followed for up to 48 months. All deaths and hospitalizations were adjudicated by an independent events committee. The primary outcome was change in LVEF from baseline to 6 months. Secondary outcomes included transplant free survival and hospitalization free survival.
Echocardiograms
Echocardiographic studies were reviewed in a blinded fashion by a core laboratory at the University of Pittsburgh. Digital routine grayscale 2-dimensional cine loops were obtained at frame rates of 40 to 90 Hz (mean 60 ± 15 Hz) from standard apical 4-chamber, 2-chamber, and long-axis views. The LV volumes and LVEF were assessed by biplane Simpson’s rule using manual tracing of digital images. LVEDD was assessed in the parasternal long axis view.
Statistical analysis
Demographic and clinical characteristics were compared by gender and race (black versus non-black) with continuous variables compared by student t tests and categorical variables compared by use of Fisher’s Exact test. For the analysis of LVEDD and myocardial recovery comparisons were first made based on a simple arbitrary division chosen for clinical utility. Subject were grouped based on LVEDD at presentation into those with minimal dilation: <6.0 cm; moderate dilation: 6.0 to 7.0 cm; and severe dilation: >7.0 cm. Analysis was then repeated using gender specific tertiles. This included use of general linear models and a 1 degree of freedom linear contrast (coded −1, 0, 1) to evaluate whether the extent of myocardial recovery varied monotonically with respect to tertiles of LVEDD. In multivariable analysis, multiple linear regression was used to identify independent predictors of change in LVEF at 6 months (i.e. verified as approximately normally distributed). Covariates were selected by use for stepwise selection (forward) with an entry and retainment p-value of 0.05, and age included irrespective of statistical significance. Prior to assessment of main effects, the interaction between race and both systolic and diastolic blood pressure was examined.
Survival analysis methods were based on 3 endpoints: death, death/transplantation, and a composite endpoint which included death, transplantation and heart failure hospitalization. The Kaplan-Meier method was used to estimate event-free survival and curves compared by log-rank test. In multivariable analysis, Cox regression was used to estimate adjusted hazard ratios for the endpoints death/transplantation, and the composite endpoint. Stepwise selection (forward) was used to identify independent predictors of these endpoints, with race (black, non-black) and diastolic blood pressure (below or above the median of 70 mmHg) combined into 4 groups to yield estimates of interaction effects (due to the significant interaction). The proportional hazards assumption of invariant relative risk was formally tested and found to be upheld for all variables and endpoints assessed with 2 minor exceptions. For risk of death/transplantation, the hazard ratio associated with NYHA functional class 4 was more pronounced in the first year of follow-up; for risk of the composite endpoint, there was an indication that risk increased in a non-proportional manner over follow-up among black patients with diastolic blood pressure < 70 mg/dl at baseline. For these 2 exceptions, separate risk estimates were reported for early follow-up.
Results
The cohort of 373 subjects was 21% (n=80) black, and 38% (n=143) women, including 39 (10%) with peripartum cardiomyopathy. The mean age was 45 ± 14 years, LVEF was 0.24 ± 0.08, symptom duration was 2.2 ± 1.7 months, and % NYHA functional class 1/2/3/4 was 18/46/29/7. Forty four subjects (12%) had an endomyocardial biopsy which revealed inflammation in 15 (4.0 %) and myocarditis in only 10 (2.6%).
Therapy at entry included an ACE inhibitor or ARB in 91%, beta blocker in 82%, aldosterone receptor antagonist in 27%, and loop diuretic in 67% (predominantly furosemide in 96%, mean daily dose 57 ± 43 mg). At entry 28 subjects (7.5%) had an implantable cardiac defibrillator (ICD), 28 (7.5%) were on intravenous inotropic therapy, 3 (0.8%) an intra-aortic balloon pump, and 6 (1.6%) a left ventricular assist device.
At six months, 92% were on ACE inhibitor or ARB, 94% on beta blockers, 20% had an ICD, and the % of subjects NYHA class 1/2/3/4 was 45/44/9/1. The mean LVEF was 0.40±0.12 (n=327) with an increase of 17 ± 13 EF units (n=312). Overall, 70% demonstrated an increase at six months of at least 10 EF units, and 39% an increase of 20 units or greater. Forty percent had an LVEF of 0.45 or greater at six months, and for 25% the LVEF had normalized (0.50 or greater). The % of subjects who normalized differed by gender (men 20%, women 34%, p=0.004) with a trend toward less recovery in blacks (blacks 18%, non-blacks 27%, p=0.14). Combining the demographic factors, an LVEF ≥ 0.50 at 6 months was most likely in white women (38%), least likely in black men (15%), and intermediate in white men (21%) and black women (20%).
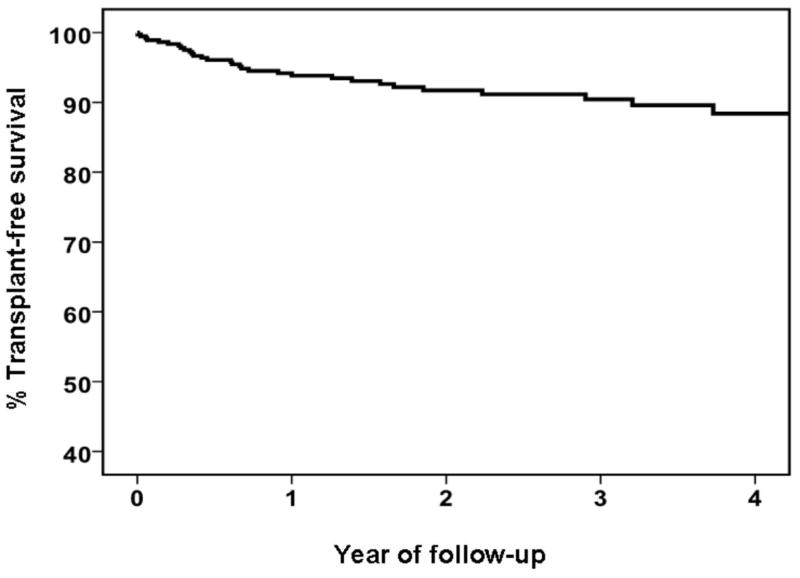
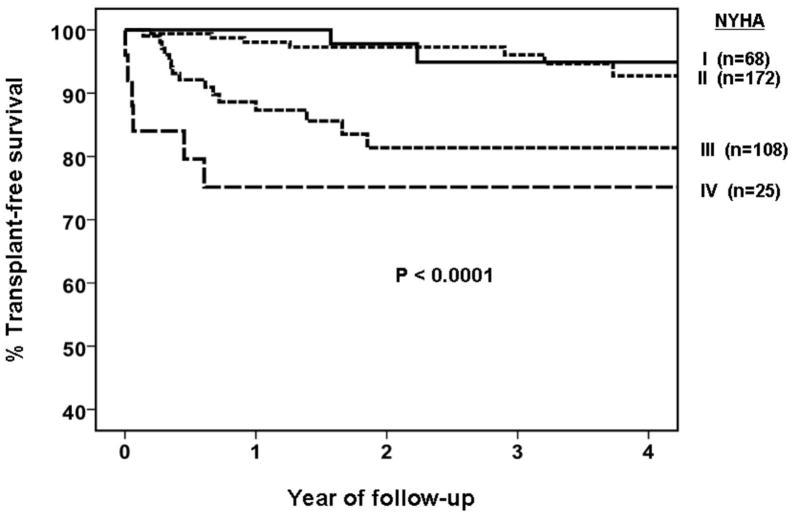
The mean follow-up was 2.2 ± 1.4 years. During follow-up there were 14 deaths (4%), 17 transplants (5%), 45 hospitalizations for heart failure (12%) in the absence of death or transplant, and 62 (17%) hospitalizations for heart failure in aggregate with a survival at 1, 2 and 4 years of 98%,96% and 94%, transplant-free survival of 94%, 92% and 88% (Figure 1A), and survival-free of the composite endpoint of 88%, 82% and 78%. Prognosis was dependent on functional class at presentation, with % transplant free survival at one year for NYHA class 1/2/3/4 of 100/98/87/75 (Figure 1B, p<0.001). A similar finding was evident based on hemodynamic support, as more subjects on intravenous inotropic therapy at entry died (18% versus 3%) or were transplanted (18% versus 4%) during follow up (p<0.001).
Figure 1. Transplant free Survival.
a. Overall Cohort (n=373)
b. Stratified by NYHA Functional Class (for class 1/2/3/4, n=68/172/108/25). Higher functional class is associated with poorer event free survival, p<0.0001.
Gender and outcomes
Myocardial recovery was more evident in women, with a similar baseline LVEF of 0.24±0.08 in women versus 0.23±0.08 in men (p=0.09), and a larger LVEF at 6 months of 0.43±0.12 in women versus 0.39±0.12 in men (p=0.004) (Table 1A). Transplant-free survival was significantly better in women (1, 2 and 4 year % transplant-free survival women=96/96/96; men=93/90/84, p=0.03), driven by a marked difference in survival (p=0.003).
Table 1A.
Demographic and Clinical Characteristics by Gender
| All (N=373) | Men (N=230) | Women (N=143) | p value | |
|---|---|---|---|---|
| Age (years) | 45 ± 14 | 46 ± 14 | 43 ± 14 | 0.01 |
| Black (%) | 21.5 | 19.1 | 25.2 | 0.19 |
| NYHA Class (%1/2/3/4) | 18/46/29/7 | 20/45/27/7 | 15/48/31/6 | 0.53 |
| LVEF baseline | 0.24 ± 0.08 | 0.23 ± 0.08 | 0.24 ± 0.08 | 0.09 |
| LVEF six months | 0.40 ± 0.12 | 0.39 ± 0.12 | 0.43 ± 0.12 | 0.004 |
| BP systolic | 112±19 | 113±20 | 111±17 | 0.27 |
| BP diastolic | 71±13 | 71±13 | 71±13 | 0.97 |
| Heart Rate | 83±17 | 83±17 | 83±16 | 0.86 |
| Therapy at entry | ||||
| ACE Inhibitor (%) | 82.3 | 84.3 | 79.0 | 0.21 |
| Aldosterone receptor antagonist (%) | 27.4 | 29.1 | 24.5 | 0.34 |
| Beta Blocker (%) | 82.0 | 80.9 | 83.9 | 0.49 |
Race and outcomes
The cohort included 80 black subjects (21%) and 293 (79%) non-black (272 white, 9 Asian, and 12 “other”). Medical therapy with ACE inhibitors and beta blockers was comparable (Table 1B). Hydralazine and nitrates were received by 9% of blacks and 2% of non-blacks (p=0.005). The black cohort was younger (range 42±12, non-black 46±14, p=0.02), with higher diastolic blood pressure at entry (mean diastolic blacks 74±13 mm Hg, non-blacks 70±12 mm Hg, p=0.005; systolic blacks 115±19 mm Hg, non blacks 111±19 mm Hg, p=0.10) and heart rate (blacks 87±17 beats per minute 82±17 bpm, p=0.02). Aldosterone receptor antagonist use was greater in blacks (p=0.007), and was driven by utilization in subjects with advanced heart failure (for NYHA class 3 and 4: 53% of blacks on therapy versus 28% of non-blacks, p=0.01).
Table 1B.
Demographic and Clinical Characteristics by Race
| Non-Black (N=293) | Black (N=80) | p value | |
|---|---|---|---|
| Age (years) | 46 ± 14 | 42 ± 12 | 0.02 |
| Female (%) | 36.5 | 40.0 | 0.19 |
| NYHA Class (%1/2/3/4) | 20/46/26/8 | 11/46/40/3 | 0.02 |
| LVEF baseline | 0.24 ± 0.08 | 0.23 ± 0.08 | 0.33 |
| LVEF six months | 0.41 ± 0.12 | 0.37 ± 0.13 | 0.007 |
| BP systolic | 111±19 | 115±19 | 0.10 |
| BP diastolic | 70±12 | 74±13 | 0.005 |
| Heart Rate | 82±17 | 87±17 | 0.02 |
| Therapy at entry | |||
| ACE Inhibitor (%) | 82.9 | 80.0 | 0.51 |
| Aldosterone receptor antagonist (%) | 23.9 | 40.0 | 0.007 |
| Beta Blocker (%) | 80.5 | 87.5 | 0.19 |
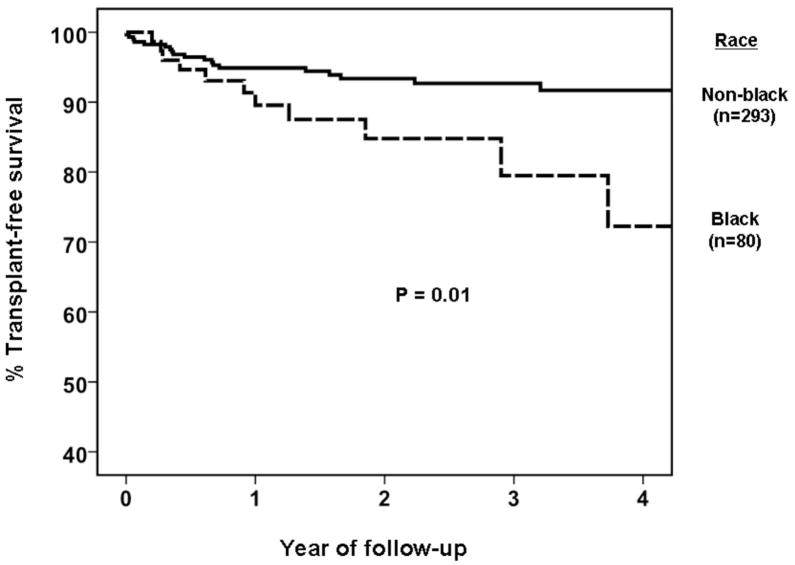
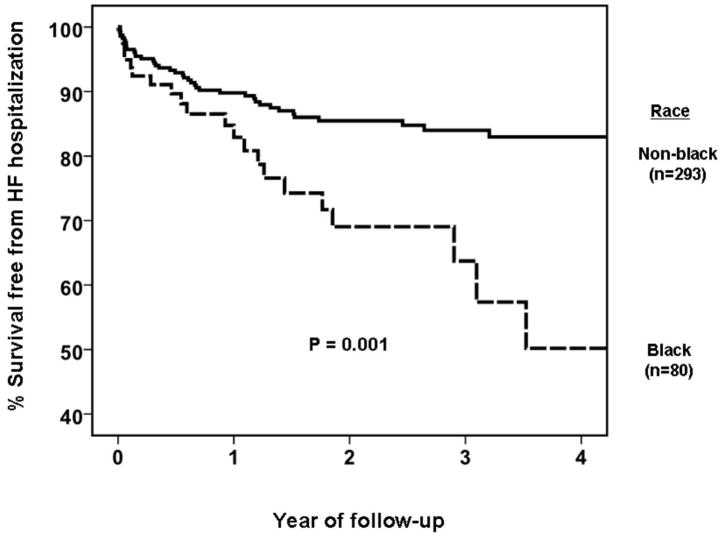
LVEF was similar at baseline (black 0.23±0.08; non-black 0.24±0.08, p=0.33) but lower in blacks at six months (black 0.37±0.13; non-black 0.41±0.12, p=0.007). Clinical outcomes were worse in blacks for transplant-free survival (%1, 2, 4 years black=90/85/72; non-black 95/93/92, p=0.01, Figure 2A) and survival free of the composite endpoint (%1, 2, 4 years black=83/69/50; non-black 90/86/83, p=0.001, Figure 2B). Similar results were observed when the non-black group was restricted to the 272 of 293 (93.5%) subjects with self designated race classified as white (data not shown).
Figure 2. Clinical Outcomes by Race.
a. Transplant free Survival (Blacks n=80 versus non-black, n=293). Event free survival is worse in Blacks, p=0.01.
b. Survival Free from Heart Failure Hospitalization (Blacks n=80 versus non-black, n=293). Event free survival is worse in Blacks, p=0.001.
Left Ventricular End diastolic Diameter (LVEDD) and Myocardial Recovery
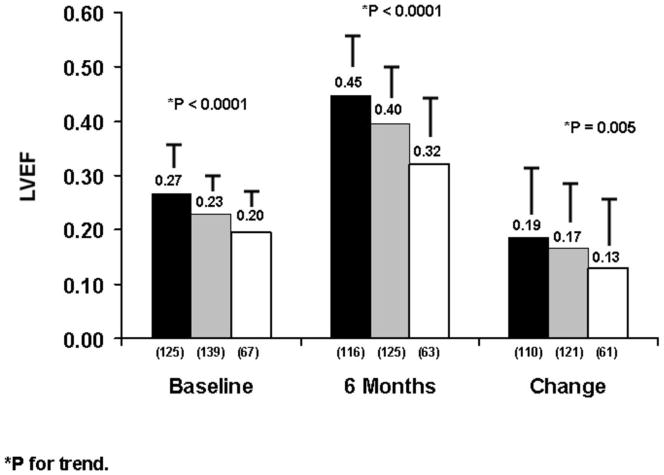
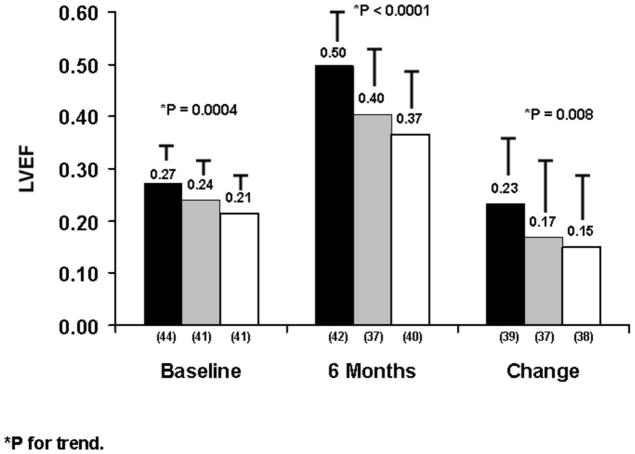
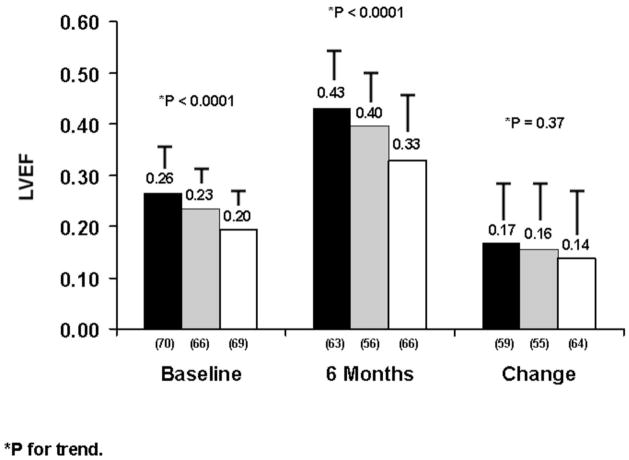
Overall the mean LVEDD was 6.3±1.0 cm. When dividing subjects into those with minimal (group 1, LVEDD<6.0cm n=125) moderate (group 2, 6.0 to 7.0cm, n=139) or severe dilation (group 3, >7.0 n=67), LVEF at baseline (groups 1/2/3=0.27±0.08/0.23±0.08/0.20±0.07, p<0.0001), LVEF at six months (0.45±0.11/0.40±0.11/0.32±0.12 p<0.0001), and change in LVEF (0.19±0.12/0.17±0.13/0.13±0.13, p=0.005), were all greatest for group 1, intermediate for group 2 and lowest for group 3 (Figure 3A). This analysis was repeated using gender specific tertiles, and similar association of smaller LVEDD with greater recovery was evident for both women (Figure 3B) and men (Figure 3C).
Figure 3. Myocardial Recovery By Left Ventricular End Diastolic Diameter (LVEDD).
a. Entire cohort: black=LVEDD<6.0cm, gray 6.0 to 7.0 cm, white>7.0 cm, LVEF entry (p<0.0001), LVEF six months (p<0.0001), LV change (p=0.005) all significantly greater with smaller LVEDD.
b. Women: black=LVEDD≤5.5cm, gray 5.6 to 6.1 cm, white>6.1 cm, LVEF entry (p=0.0004), LVEF six months (p<0.0001), LV change (p=0.008).
c. Men: black=LVEDD≤ 6.1cm, gray 6.2 to 6.9 cm, white>6.9 cm, LVEF entry (p<0.0001), LVEF six months (p<0.0001), LV change (p=0.37).
Note: Label on each bar represents mean LVEF for the subset. Error bar represents standard deviation.
Multivariable Analyses
Independent predictors of LVEF at 6 months follow-up are provided in rank order in Table 2a. A smaller LVEDD at baseline was associated with higher LVEF at 6 months (p<0.0001), independent of gender (p=0.75). Higher systolic blood pressure at baseline was also associated with LVEF at 6 months (p=0.001), whereas black race (p=0.02) and higher NYHA class (p=0.04) were associated with lower LVEF at 6 months. These associations occurred independent of baseline LVEF which was included as a covariate and was not associated with LVEF at 6 months (p=0.32). In total, the 7 variables included in the multiple linear regression model explained 25% of the variation in LVEF at 6 months. The interaction between race and systolic blood pressure (p=0.96), as well as diastolic pressure (p=0.63), was not statistically significant (data not shown) indicating that the effect of race was independent of baseline blood pressure. Similar results were observed when the outcome (dependent) variable was absolute change in LVEF between baseline and 6 months (Table 2b).
Table 2a.
Predictors of LVEF at 6 Months (n=292).
| Variable | T-value | Standardized Coefficient | Semi-partial2 correlation | P-value |
|---|---|---|---|---|
| LVEDD | −6.98 | −0.41 | 0.13 | <0.0001 |
| Systolic BP | 3.30 | 0.18 | 0.03 | 0.001 |
| Black race | −2.39 | −0.12 | 0.01 | 0.02 |
| NYHA | −2.10 | −0.11 | 0.01 | 0.04 |
| Age | −1.25 | −0.07 | 0.004 | 0.21 |
| Baseline LVEF | 1.00 | 0.06 | 0.003 | 0.32 |
| Female gender | 0.32 | 0.02 | 0.0003 | 0.75 |
Adjusted R2 = 0.25.
Table 2b.
Predictors of Change in LVEF at 6 Months (n=292).
| Variable | T-value | Standardized Coefficient | Semi-partial2 correlation | P-value |
|---|---|---|---|---|
| Baseline LVEF | −10.91 | −0.59 | 0.28 | <0.0001 |
| LVEDD | −6.98 | −0.39 | 0.11 | <0.0001 |
| Systolic BP | 3.30 | 0.17 | 0.03 | 0.001 |
| Black race | −2.39 | −0.12 | 0.01 | 0.02 |
| NYHA | −2.10 | −0.11 | 0.01 | 0.04 |
| Age | −1.25 | −0.06 | 0.004 | 0.21 |
| Female gender | 0.32 | 0.02 | 0.0002 | 0.75 |
Adjusted R2 = 0.32.
Predictors of death/transplantation and the composite endpoint are provided in Table 3. As seen, NYHA functional class 4 (adjusted hazard ratio=9.41) and black race (adjusted hazard ratio=2.78) were associated with a significantly higher risk of death/transplantation over 4-year follow-up. In contrast, female gender (adjusted hazard ratio=0.34) was associated with a significantly lower risk of death/transplantation. Compared to white patients with diastolic blood pressure ≥70 mg/dl at baseline, black patients with diastolic blood pressure >70 mg/dl has an estimated 5-fold higher risk of death/transplantation. Results were generally consistent for the broader outcome of risk of the composite endpoint, however, black patients were at higher risk than white patients irrespective of baseline diastolic blood pressure.
Table 3.
Predictors of Death/Transplantation and Heart Failure (HF) Hospitalization.
| Predictor | Death/Transplantation (n=373) | HF Hospitalization (n=373) | ||||
|---|---|---|---|---|---|---|
| Adj. HR | 95% CI | P-value | Adj. HR | 95% CI | P-value | |
| NYHA Class | ||||||
| 2 (versus 1) | 1.19 | 0.25–5.71 | 0.83 | 1.04 | 0.43 – 2.48 | 0.94 |
| 3 (versus 1) | 4.16 | 0.93–18.63 | 0.06 | 1.52 | 0.62 – 3.74 | 0.36 |
| 4 (versus 1) | 9.41a | 1.83–48.32 | 0.007b | 3.50 | 1.22 – 10.02 | 0.02c |
| Age (per 10 years) | 0.77 | 0.59–1.01 | 0.06 | 0.85 | 0.70 – 1.04 | 0.12 |
| Female gender | 0.34 | 0.14–0.83 | 0.02 | 0.57 | 0.32 – 0.99 | 0.05 |
| Heart rate (per 10 beats) | --- | --- | --- | 1.21 | 1.03–1.43 | 0.02 |
| Race and Diastolic BPd | ||||||
| White, DBP < 70 mg/dl | 2.07 | 0.79–5.43 | 0.14 | 1.85 | 0.97–3.53 | 0.06 |
| Black, DBP < 70 mg/dl | 2.11 | 0.41–10.84 | 0.38 | 3.65 | 1.51–8.82 | 0.004e |
| Black, DBP ≤ 70 mg/dl | 4.97 | 1.69–14.60 | 0.004 | 2.94 | 1.37–6.32 | 0.006 |
Adj.: Adjusted; HR: hazard ratio; CI: Confidence interval; NYHA: New York Heart Association; BP: blood pressure.
The estimated adjusted hazard ratio in the first 2-years of follow-up was 18.2 (95% CI: 2.13–155.5) indicating higher risk early in follow-up compared to the average risk estimate of 9.41 estimated for the entire follow-up period.
The p-value for NYHA class as an ordered variable was <0.0001.
The p-value for NYHA class as an ordered variable was 0.01.
The referent group is white, DBP ≤ 70 mg/dl; the white classification includes all races self-reported other than black.
The estimated adjusted hazard ratio in the first years of follow-up was 1.76 (95% CI: 0.47–6.65) indicating lower risk early in follow-up compared to the average risk estimate of 3.65 estimated for the entire follow-up period.
Discussion
Recent onset dilated cardiomyopathy remains a challenging diagnosis for patients and clinician alike, which frequently results in referral to tertiary centers. The current study demonstrates there is substantial improvement in LVEF evident for the majority of subjects over the first six months. Despite concerns, the short-term the prognosis is favorable, with a transplant-free survival of 88% at 4 years.
The dynamic nature of recent onset cardiomyopathy has long been recognized, and the percent of patients normalizing their ejection fraction (25%) in the current series does not differ significantly from previous investigations (4,6,8). However the percentage of subjects experiencing at least moderate recovery of LV function, i.e. 10 EF units or more, has improved dramatically from one third in older series (4,8), to one half in the previous IMAC trial (6) to nearly 70% of subjects in the current cohort. Given the impact of beta blockers in chronic non-ischemic cardiomyopathy (10,11), the widespread improvements in LVEF in the current investigation can be attributed in part to their extensive use in this cohort.
An inflammatory pathogenesis is postulated for subjects with “reversible” cardiomyopathy, in which the recovery ensues when the inflammatory event resolves (12). Indeed, for subjects with histological confirmation of lymphocytic myocarditis the mean LVEF at 6 months was 0.49±0.08. While myocardial inflammation may be a potential marker of reversibility, additional methodologies including cardiac magnetic resonance (cMR) and novel peripheral biomarkers may be more effective than endomyocardial biopsy at delineating reversible inflammatory myocarditis (13).
Women had better outcomes than men in terms of LVEF at 6 months and transplant-free survival. A similar trend towards better recovery in women was seen in the first IMAC trial. Analysis of myocardial gene expression in that trial demonstrated that activation of apoptotic pathways was inversely associated with recovery (14) and that this activation was less evident in women. The recovery of LVEF in the current study is consistent with investigations in chronic heart failure in which women generally have better outcomes than their male counterparts (15).
Self-identified black subjects demonstrated less recovery and markedly worse transplant-free survival. The impact of race in recent onset cardiomyopathy again parallels findings in chronic heart failure (16). It has been long been recognized that hypertension is more prevalent in blacks as an etiology of heart failure. Though multivariate analysis did not suggest racial differences by race could be attributed to blood pressure, this was based a single baseline measurement, and does not address the potential impact of chronic hypertension. Whether outcomes by race reflect a differential genomic response to therapy or other socioeconomic variables will require further analysis.
In terms of the initial assessment, LVEDD was most predictive as less LV enlargement at presentation predicted a greater LVEF at 6 months. In a recent analysis of subjects supported with a left ventricular assist device, myocardial recovery occurred in 12 % of subjects overall, but 33% of subjects with LVEDD less than 6.0 cm (17). Smaller LV size is likely a marker of a more reversible cardiac pathology and LVEDD remains a simple standard echo measure routinely reported which can provide immediate clinical guidance in predicting recovery potential.
A limitation of this study is the overall low number of “hard” events in the analysis (i.e. death/transplantation). The net consequence of this is relatively imprecise estimates of long-term risk of death/transplantation and HF hospitalization. This limitation should be kept in mind when interpreting the relative predictive value of individual variables.
Contemporary heart failure therapy has changed the natural history of recent onset cardiomyopathy from a rapidly progressive disorder to a more manageable condition with an overall favorable prognosis. Indeed, the majority of subjects have significant improvements in LVEF during the first six months. Recognition of this recovery potential is essential and advanced therapies such as cardiac transplant should not be undertaken until clinicians observe the early clinical course to determine the degree of recovery. While these results are encouraging, outcomes remain heterogeneous, and in particular recovery and survival were poorer in black subjects. The basis for these apparent racial differences is unknown, and additional investigation is required to delineate the biologic and genomic determinants of myocardial recovery in recent onset cardiomyopathy.
Supplementary Material
Acknowledgments
Investigation supported by NHLBI contracts HL075038, HL086918, and HL69912
Abbreviations
- LVEF
left ventricular ejection fraction
- LVEDD
left ventricular end diastolic diameter
- ACE
angiotensin converting enzyme
- ARB
angiotensin receptor blocker
- ROCM
recent onset cardiomyopathy
- IMAC
Intervention in Myocarditis and Acute Cardiomyopathy
- NYHA
New York Heart Association
Footnotes
Clinical Trial Title: Genetic Modulation of Left Ventricular Recovery in Recent Onset Cardiomyopathy Registration number:NCT00575211 URL:http://clinicaltrials.gov/ct2/show/study/NCT00575211
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Taylor DO, Stehlik J, Edwards LB, et al. Registry of the International Society for Heart and Lung Transplantation: Twenty-sixth Official Adult Heart Transplant Report-2009. J Heart Lung Transplant. 28:1007–1022. doi: 10.1016/j.healun.2009.08.014. [DOI] [PubMed] [Google Scholar]
- 2.Codd MB, Sugrue DD, Gersh BJ, Melton LJ., 3rd Epidemiology of idiopathic dilated and hypertrophic cardiomyopathy. A population-based study in Olmsted County, Minnesota, 1975–1984. Circulation. 1989 Sep;80(3):564–72. doi: 10.1161/01.cir.80.3.564. [DOI] [PubMed] [Google Scholar]
- 3.Cooper LT, Virmani R, Chapman NM, et al. National Institutes of Health-sponsored workshop on inflammation and immunity in dilated cardiomyopathy. Mayo Clin Proc. 2006 Feb;81(2):199–204. doi: 10.4065/81.2.199. [DOI] [PubMed] [Google Scholar]
- 4.Dec GW, Palacios IF, Fallon JT, et al. Active myocarditis in the spectrum of acute dilated cardiomyopathies. N Engl J Med. 1985;312(14):885–890. doi: 10.1056/NEJM198504043121404. [DOI] [PubMed] [Google Scholar]
- 5.Parrillo JE, Cunnion RE, Epstein SE, et al. A prospective, randomized, controlled trial of prednisone for dilated cardiomyopathy. N Engl J Med. 1989;321:1061–1068. doi: 10.1056/NEJM198910193211601. [DOI] [PubMed] [Google Scholar]
- 6.McNamara DM, Holubkov R, Starling RC, et al. for the IMAC Investigators. A Controlled Trial of Intravenous Immune Globulin in Recent Onset Dilated Cardiomyopathy. Circulation. 2001;103(18):2254–2259. doi: 10.1161/01.cir.103.18.2254. [DOI] [PubMed] [Google Scholar]
- 7.Mason JW, O’Connell JB, Herskowitz A, et al. A clinical trial of immunosuppressive therapy for myocarditis. N Engl J Med. 1995;333:269–275. doi: 10.1056/NEJM199508033330501. [DOI] [PubMed] [Google Scholar]
- 8.Steimle AE, Stevenson LW, Fonarow GC, Hamilton MA, Moriguchi JD. Prediction of improvement in recent onset cardiomyopathy after referral for heart transplantation. J Am Coll Cardiol. 1994;23(3):553–559. doi: 10.1016/0735-1097(94)90735-8. [DOI] [PubMed] [Google Scholar]
- 9.Cooper LT, Baughman KL, Feldman AM, et al. The role of endomyocardial biopsy in the management of cardiovascular disease: a scientific statement from the American Heart Association, the American College of Cardiology, and the European Society of Cardiology. Circulation. 2007 Nov 6;116(19):2216–33. doi: 10.1161/CIRCULATIONAHA.107.186093. [DOI] [PubMed] [Google Scholar]
- 10.Packer M, Bristow MR, Cohn JN, et al. The effect of carvedilol on morbidity and mortality in patients with chronic heart failure. N Engl J Med. 1996;334:1349–1355. doi: 10.1056/NEJM199605233342101. [DOI] [PubMed] [Google Scholar]
- 11.Bristow MR, Gilbert EM, Abraham WT, et al. Carvedilol produces dose-related improvements in left ventricular function and survival in subjects with chronic heart failure. MOCHA Investigators. Circulation. 1996 Dec 1;94(11):2807–16. doi: 10.1161/01.cir.94.11.2807. [DOI] [PubMed] [Google Scholar]
- 12.Cooper LT., Jr Myocarditis. N Engl J Med. 2009 Apr 9;360(15):1526–38. doi: 10.1056/NEJMra0800028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Friedrich MG, Sechtem U, Schulz-Menger J, et al. Cardiovascular magnetic resonance in myocarditis: A JACC White Paper. J Am Coll Cardiol. 2009 Apr 28;53(17):1475–87. doi: 10.1016/j.jacc.2009.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sheppard R, Bedi M, Kubota K, et al. Myocardial Expression of Fas and Recovery of Left Ventricular Function in Patients with Recent-onset Cardiomyopathy. Journal of the American College of Cardiology. 2005;46(6):1036–42. doi: 10.1016/j.jacc.2005.05.067. [DOI] [PubMed] [Google Scholar]
- 15.Hsich EM, Piña IL. Heart failure in women: a need for prospective data. J Am Coll Cardiol. 2009 Aug 4;54(6):491–8. doi: 10.1016/j.jacc.2009.02.066. [DOI] [PubMed] [Google Scholar]
- 16.Yancy CW, Strong M. The natural history, epidemiology, and prognosis of heart failure in African Americans. Congest Heart Fail. 2004 Jan-Feb;10(1):15–8. doi: 10.1111/j.1527-5299.2004.02026.x. [DOI] [PubMed] [Google Scholar]
- 17.Simon MA, Primack BA, Teuteberg J, et al. Left Ventricular Remodeling and Myocardial Recovery on Mechanical Circulatory Support. J Cardiac Fail. 2009 doi: 10.1016/j.cardfail.2009.10.018. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.