Abstract
Background:
Sacroiliac joint pain is increasingly recognized as a cause of low back pain. We compared the safety and effectiveness of minimally invasive sacroiliac joint arthrodesis using triangular titanium implants and conservative management in patients with chronic sacroiliac joint pain.
Methods:
This study was a prospective, multicenter randomized controlled trial of adults with chronic sacroiliac joint pain assigned to either conservative management or sacroiliac joint arthrodesis with triangular titanium implants. The study end points included self-rated low back pain (visual analog scale [VAS]), back dysfunction (Oswestry Disability Index [ODI]), and quality of life. Ninety percent of subjects in both groups completed the study.
Results:
Between June 6, 2013, and May 15, 2015, 103 subjects were randomly assigned to conservative management (n = 51) or sacroiliac joint arthrodesis (n = 52). At 2 years, the mean low back pain improved by 45 points (95% confidence interval [CI], 37 to 54 points) after sacroiliac joint arthrodesis and 11 points (95% CI, 2 to 20 points) after conservative management, with a mean difference between groups of 34 points (p < 0.0001). The mean ODI improved by 26 points (95% CI, 21 to 32 points) after sacroiliac joint arthrodesis and 8 points (95% CI, 2 to 14 points) after conservative management, with a mean difference between groups of 18 points (p < 0.0001). Parallel improvements were seen in quality of life. In the sacroiliac joint arthrodesis group, the prevalence of opioid use decreased from 56% at baseline to 33% at 2 years (p = 0.009), and no significant change was observed in the conservative management group (47.1% at baseline and 45.7% at 2 years). Subjects in the conservative management group, after crossover to the surgical procedure, showed improvements in all measures similar to those originally assigned to sacroiliac joint arthrodesis. In the first 6 months, the frequency of adverse events did not differ between groups (p = 0.664). By month 24, we observed 39 severe adverse events after sacroiliac joint arthrodesis, including 2 cases of sacroiliac joint pain, 1 case of a postoperative gluteal hematoma, and 1 case of postoperative nerve impingement. The analysis of computed tomographic (CT) imaging at 12 months after sacroiliac joint arthrodesis showed radiolucencies adjacent to 8 implants (4.0% of all implants).
Conclusions:
For patients with chronic sacroiliac joint pain due to joint degeneration or disruption, minimally invasive sacroiliac joint arthrodesis with triangular titanium implants was safe and more effective throughout 2 years in improving pain, disability, and quality of life compared with conservative management.
Level of Evidence:
Therapeutic Level I. See Instructions for Authors for a complete description of levels of evidence.
Low back pain is the number-1 contributor to global health burden in terms of years lived with disability1. Chronic low back pain is the most common specific reason for prescribed opioid use2 and has contributed to marked increases in opioid abuse3. Finding effective solutions for chronic low back pain is a critical agenda item for health-care professionals worldwide.
Pain from the sacroiliac joint has long been recognized as a potential source of chronic low back pain, playing a role in 15% to 30% of patients with chronic low back pain4-6. Also, the sacroiliac joint is implicated in up to 40% of patients with new-onset low back pain after lumbar arthrodesis7.
The effectiveness of nonsurgical treatments for chronic sacroiliac joint pain remains unclear. Periarticular radiofrequency ablation and periarticular corticosteroid injections are supported only by short-term evidence; to our knowledge, no long-term, high-quality evidence supports these treatments’ effectiveness. Open surgical arthrodesis of the sacroiliac joint can be achieved through multiple approaches8. With the advent of minimally invasive approaches, open arthrodesis of the sacroiliac joint has decreased in usage. The most studied minimally invasive sacroiliac joint arthrodesis device, triangular titanium implants, has evidence support from randomized trials9,10, a multicenter single-arm trial11, prospective case series12-15, and comparative case series16-18. We conducted a randomized trial of minimally invasive sacroiliac joint arthrodesis compared with conservative management, previously reporting short-term outcomes10. Herein, we report 2-year results.
Materials and Methods
iMIA (iFuse Implant System Minimally Invasive Arthrodesis; SI-BONE) is a prospective, open-label, multicenter randomized controlled trial conducted at 9 European centers. Local ethics committees approved the protocol prior to study initiation. The trial was registered at ClinicalTrials.gov (NCT01741025). One-year results for iMIA were published previously19. Details on the study design are presented in the Appendix. In brief, subjects with clinically relevant pain originating from the sacroiliac joint were randomized to either conservative management or sacroiliac joint arthrodesis (Fig. 1). Subjects had scheduled follow-up visits to 24 months after randomization. Assessments, described previously, included changes in low back pain (visual analog scale [VAS] for pain), leg pain, active straight leg raise for the affected side20, Oswestry Disability Index (ODI)21, EuroQoL EQ-5D22, and Zung Depression Scale23. In the sacroiliac joint arthrodesis cohort, computed tomographic (CT) scans were conducted immediately postoperatively and at 12 months.
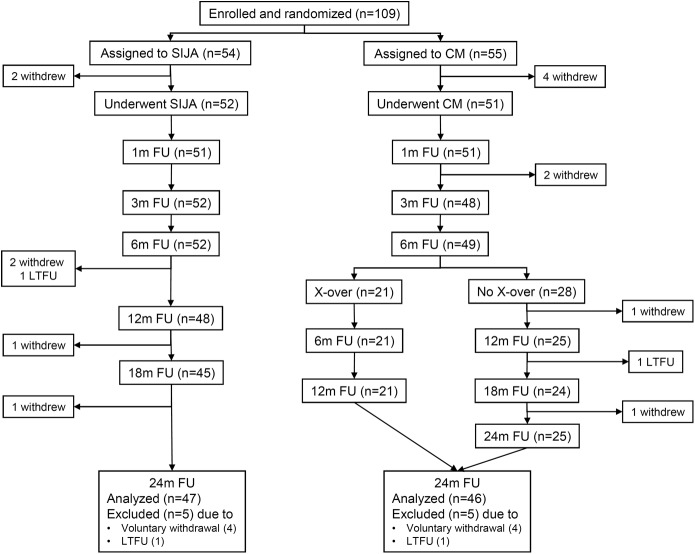
Fig. 1.
Patient flow. SIJA = sacroiliac joint arthrodesis, CM = conservative management, FU = follow-up, m = month, X-over = crossover, and LTFU = lost to FU.
Statistical Analysis
The minimum sample size was 40 subjects in each group, providing a power of 80% to identify a difference of 20 VAS points in sacroiliac joint pain with the assumption of a standard deviation of 35 points. Accounting for expected loss to follow-up, the trial’s sample size was inflated to 50 per group. T tests and repeated-measures analysis of variance were used to compare continuous variables. Ordinal end points were analyzed using the Wilcoxon test, logistic or proportional-odds logistic regression, or the McNemar test for paired observations. Poisson regression was used to compare the number of adverse events per subject across groups. The primary end point used an as-available data analysis approach without missing data imputation. The impact of crossover from conservative management to sacroiliac joint arthrodesis was investigated using a last-observation-carried-forward approach, substituting the last observation prior to crossover for subsequent values. Repeated-measures analysis of variance was used to compare all post-treatment change scores across the following subgroups: age, pain duration, relation to pregnancy, sex, body mass index (BMI), prior lumbar arthrodesis, use of opioids, and smoking. All statistical analyses were performed using R (The R Foundation)24. All study data were 100% source-verified.
Results
Between June 6, 2013, and May 15, 2015, 109 qualified subjects were enrolled; of these, 6 (4 assigned to conservative management and 2 assigned to sacroiliac joint arthrodesis) withdrew before any intervention, leaving 103 participating subjects (Fig. 1). Baseline characteristics are displayed in Table I. The mean baseline low back pain scores were 77.7 points in the sacroiliac joint arthrodesis group and 73.0 points in the conservative management group (p = 0.06).
TABLE I.
Baseline Characteristics of Enrolled and Randomized Subjects
| Conservative Management (N = 51) | Sacroiliac Joint Arthrodesis (N = 52) | P Value* | |
| Age† (yr) | 46.7 (23 to 69) | 49.4 (27 to 70) | 0.210 |
| Female sex‡ | 37 (72.5%) | 38 (73.1%) | 0.999 |
| Pain duration† (yr) | 4.5 (0.45 to 23) | 4.9 (0.58 to 44) | 0.777 |
| BMI† (kg/m2) | 27.6 (16 to 44) | 26.5 (18 to 42) | 0.355 |
| Smoking‡ | 0.044 | ||
| Current | 16 (31.4%) | 23 (44.2%) | |
| Former | 8 (15.7%) | 14 (26.9%) | |
| Never | 27 (52.9%) | 15 (28.8%) | |
| Pain syndrome‡ | |||
| Pain began in peripartum period | 3 (5.9%) | 6 (11.5%) | 0.488 |
| Radiates down leg | 40 (78.4%) | 42 (80.8%) | 0.811 |
| Pain in groin | 36 (70.6%) | 31 (59.6%) | 0.303 |
| Pain sitting | 38 (74.5%) | 42 (80.8%) | 0.486 |
| Pain rising | 40 (78.4%) | 48 (92.3%) | 0.055 |
| Pain walking | 42 (82.4%) | 43 (82.7%) | 0.999 |
| Pain climbing stairs | 41 (80.4%) | 41 (78.8%) | 0.999 |
| Pain descending stairs | 29 (56.9%) | 33 (63.5%) | 0.549 |
| Prior treatment‡ | |||
| Prior physical therapy | 27 (52.9%) | 32 (61.5%) | 0.429 |
| Prior prolotherapy | 0 (0%) | 0 (0%) | 0.999 |
| Prior corticosteroid sacroiliac joint injections | 38 (74.5%) | 37 (71.2%) | 0.825 |
| Prior radiofrequency ablation§ | 6 (11.8%) | 11 (21.2%) | 0.289 |
| Work status‡ | 0.792 | ||
| Working normal hours | 3 (5.9%) | 5 (9.6%) | |
| Working with limitations | 12 (23.5%) | 13 (25.0%) | |
| Not working due to lower back pain | 27 (52.9%) | 23 (44.2%) | |
| Not working due to other reason | 2 (3.9%) | 1 (1.9%) | |
| Retired | 7 (13.7%) | 10 (19.2%) | |
| Ambulatory status‡ | 0.295 | ||
| Ambulatory without assistance | 46 (90.2%) | 42 (80.8%) | |
| Ambulatory with assistance | 3 (5.9%) | 8 (15.4%) | |
| Cannot walk | 2 (3.9%) | 2 (3.8%) | |
| History of prior lumbar arthrodesis‡ | 19 (37.3%) | 18 (34.6%) | 0.839 |
The Fisher test was used to determine p values for nominal variables, and the t test was used to determine p values for continuous variables.
The values are given as the mean, with the range in parentheses.
The values are given as the number of patients, with the percentage in parentheses.
This is radiofrequency ablation of the lateral branches of the sacral nerve root.
Of the subjects who underwent sacroiliac joint arthrodesis, 7 had bilateral pain and underwent staged bilateral sacroiliac joint arthrodesis, 11 had bilateral pain but underwent only unilateral sacroiliac joint arthrodesis, 6 with initial unilateral pain underwent bilateral sacroiliac joint arthrodesis, and the remainder underwent unilateral sacroiliac joint arthrodesis for unilateral pain. All but 1 case used 3 implants on the treated side (Table II); in the remaining subject, 4 implants were used on the treated side. The median hospital length of stay was 3 days (range, 1 to 28 days). Subjects assigned to conservative management underwent a mean of 25 physical therapy sessions over the first 6 months. Two subjects in the conservative management group underwent sacroiliac joint corticosteroid injections and 1 subject underwent sacroiliac joint corticosteroid injection and radiofrequency ablation as deviations from the investigational protocol.
TABLE II.
Description of Operative Characteristics (Index Side Only) and Conservative Management
| Study Group | Value |
| Sacroiliac joint arthrodesis (n = 52) | |
| Time from enrollment to surgery* (days) | 18 (1 to 82) |
| No. of implants† | |
| 3 | 51 (98.1%) |
| 4 | 1 (1.9%) |
| Procedure duration* (min) | 54 (19 to 107) |
| Fluoroscopy time* (min) | 2.1 (1.0 to 4.0) |
| Hospital length of stay* (days) | 3 (1 to 28) |
| Conservative management (n = 51) | |
| Physical therapy sessions† | |
| 1 | 1 (2.0%) |
| 2 to 4 | 2 (3.9%) |
| 5 to 10 | 1 (2.0%) |
| 11 to 15 | 9 (17.6%) |
| >15 | 38 (74.5%) |
| Cognitive behavioral therapy sessions† | |
| 0 | 27 (52.9%) |
| 1 | 1 (2.0%) |
| 2 to 5 | 7 (13.7%) |
| 6 to 10 | 10 (19.6%) |
| 11 to 15 | 3 (5.9%) |
| >15 | 3 (5.9%) |
The values are given as the median, with the range in parentheses.
The values are given as the number of patients, with the percentage in parentheses.
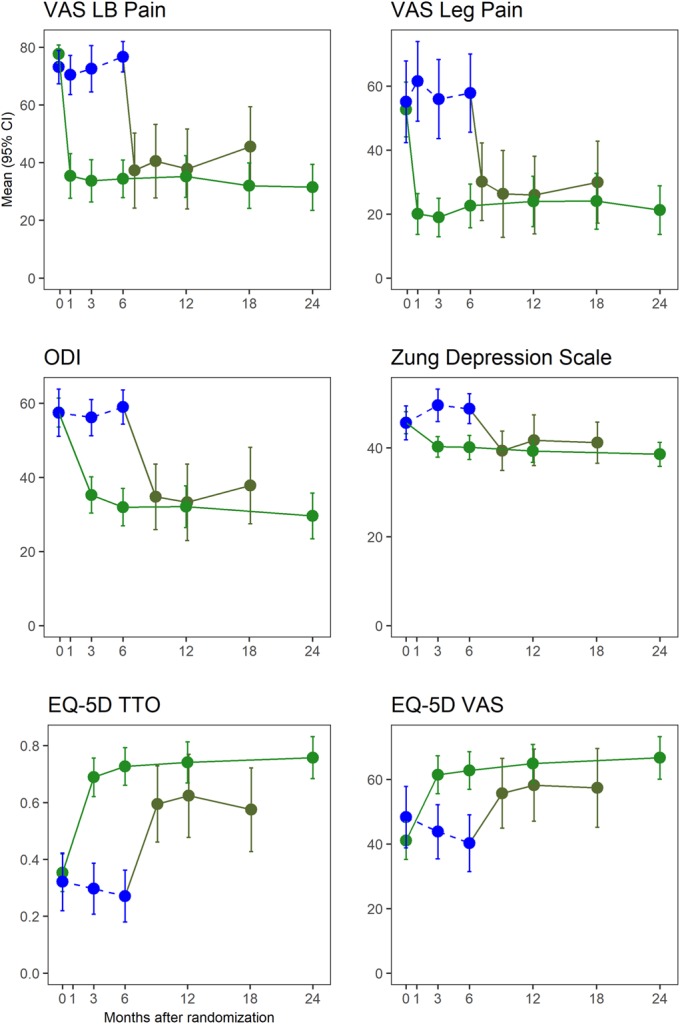
Low back pain improvement at 6 months was significantly larger in the sacroiliac joint arthrodesis group (43.3 points) compared with conservative management (5.7 points), a difference of 38 points (p < 0.0001) (Fig. 2). Improvement in low back pain after sacroiliac joint arthrodesis persisted at 24 months; the mean improvement was 45.3 points (95% confidence interval [CI], 37 to 54 points), 34 points higher than the conservative management group (p < 0.0001). Improvements in leg pain paralleled those seen in low back pain, with minimal improvements in the conservative management group (by 1.4 points at 6 months and 7.7 points at 24 months) and large improvements (by 30 points at 6 months and 32 points at 24 months) in the sacroiliac joint arthrodesis group. In the conservative management group, the mean ODI improved minimally at 6 months (by 5.6 points) and 24 months (by 8 points); in contrast, the mean ODI improved rapidly in the sacroiliac joint arthrodesis group by 26 points (95% CI, 21 to 32 points) at 24 months. At 6 months, 79% (41 of 52) of subjects in the sacroiliac joint arthrodesis group had an improvement in low back pain by at least 20 VAS points compared with 22% (11 of 49) of subjects in the conservative management group. Twenty-four months after sacroiliac joint arthrodesis, 79% (37 of 47) had at least a 20-point improvement compared with 24% (11 of 46) in the conservative management group. Threshold 24-month improvements for the ODI occurred in 64% (30 of 47) in the sacroiliac joint arthrodesis group compared with 24% (11 of 46) in the conservative management group. Similar patterns were observed for the EQ-5D time trade-off, with large changes in the sacroiliac joint arthrodesis group at 6 months (0.37 point) and 24 months (0.39 point) and smaller changes in the conservative management group at 6 months (0.09 point) and 24 months (0.15 point). The mean Zung Depression Scale score showed no improvement in the conservative management group and a 5.3-point improvement in the sacroiliac joint arthrodesis group at 6 months, and this difference persisted at 24 months. All across-group comparisons reported here had p values of <0.001. Subgroup analysis showed the following in the sacroiliac joint arthrodesis group at 6 months. Current smokers had a somewhat smaller decrease in VAS low back pain (38 points) compared with former smokers (52 points) and those who had never smoked (43 points); current smokers also had a somewhat smaller decrease in the ODI (21 points) compared with former smokers (29 points) and those who had never smoked (30 points). Baseline opioid users also had somewhat smaller ODI responses (22 points) compared with non-users (28 points) but similar VAS low back pain reduction. The reduction in VAS low back pain was larger in patients with higher baseline back pain scores; similarly, ODI improvements were larger in those with higher baseline scores.
Fig. 2.
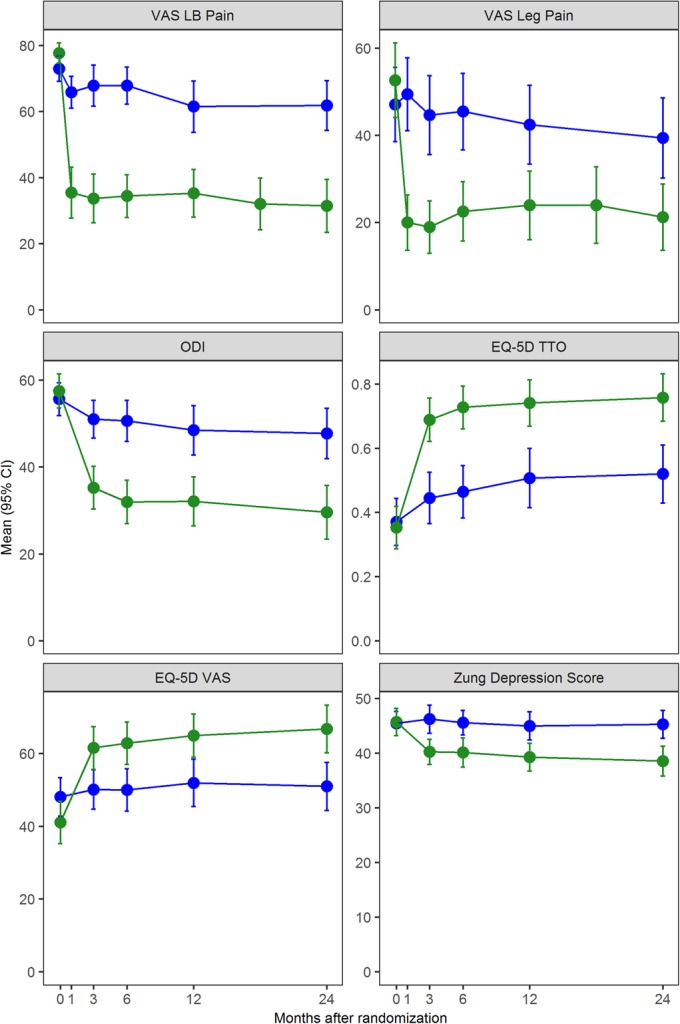
Change in VAS low back (LB) pain, VAS leg pain, ODI, EQ-5D time trade-off (TTO), EQ-5D VAS, and Zung Depression Scale scores. Blue indicates the conservative management group, and green indicates the sacroiliac joint arthrodesis group. The last-observation-carried-forward method was used to estimate values after crossover. The values shown are the mean. The error bars indicate the 95% CI.
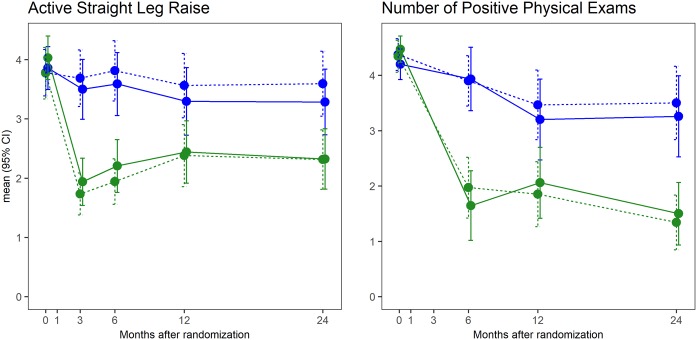
The active straight leg raise showed no significant improvement in the conservative management group but large improvements after sacroiliac joint arthrodesis (p < 0.0001 compared with baseline and p < 0.0001 compared with conservative management) (Fig. 3). Superior improvement in the number of positive physical examination findings was also observed (p < 0.0001). The proportion of subjects using opioids decreased in the sacroiliac joint arthrodesis group from 56% at baseline to 33% at 24 months (McNemar p = 0.009) but was constant in the conservative management group (p = 1) (Fig. 4).
Fig. 3.
Change in functional test (active straight leg raise test) by treatment and time (left) and the number of positive physical examination signs (right). Blue indicates the conservative management group, and green indicates the sacroiliac joint arthrodesis group. The solid line indicates the right sacroiliac joint affected, and the dotted line indicates the left sacroiliac joint affected. The last-observation-carried-forward method was used to estimate values after crossover. The values shown are the mean. The error bars indicate the 95% CI.
Fig. 4.
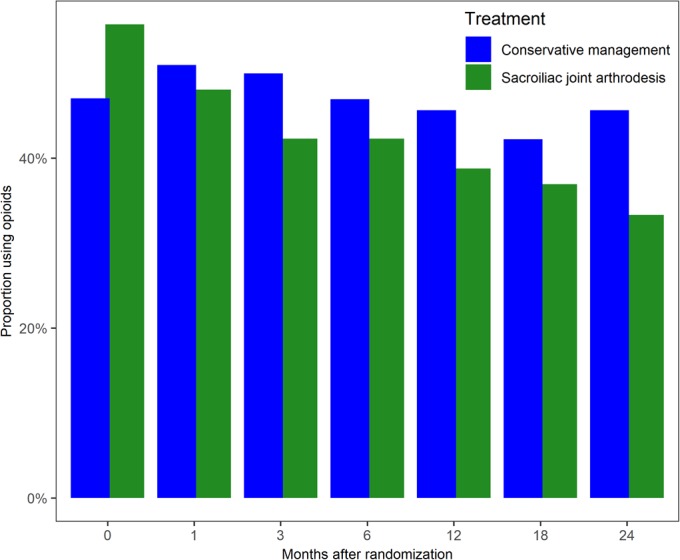
Proportion of subjects reporting opioid use in the past 2 weeks by treatment and study visit. Blue indicates the conservative management (CM) group, and green indicates the sacroiliac joint arthrodesis (SIJA) group.
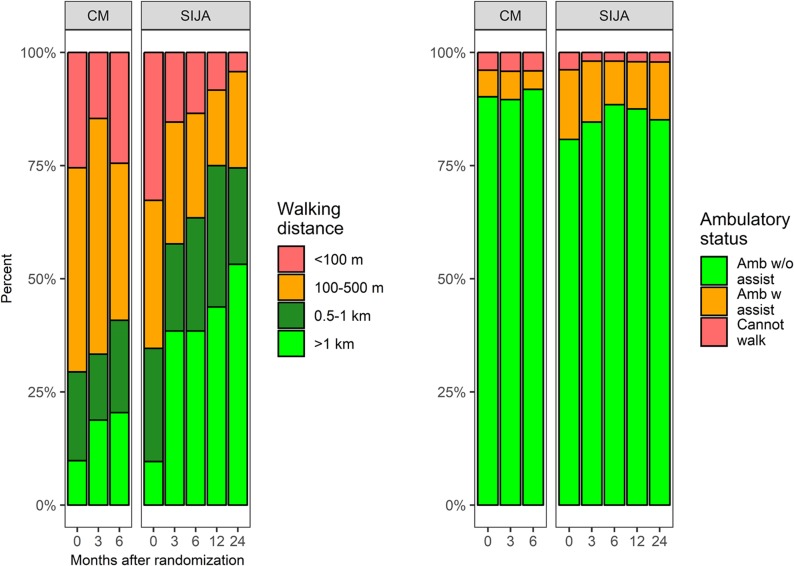
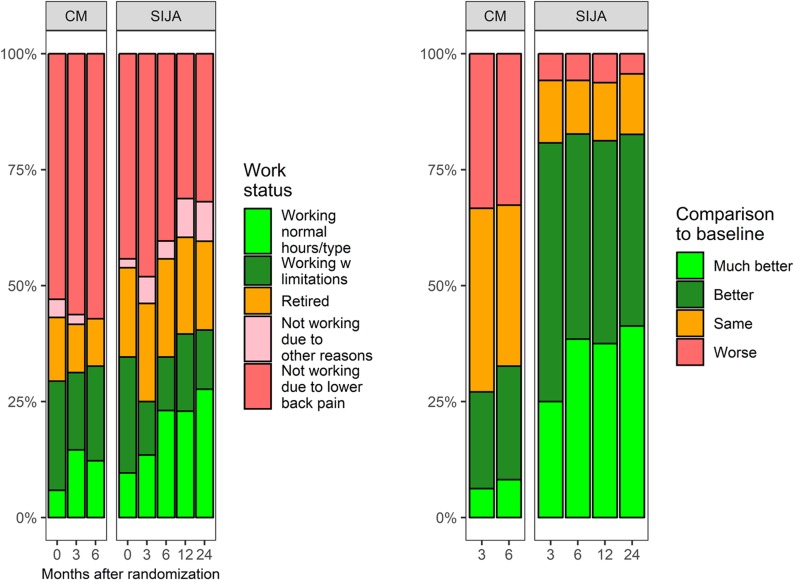
Additional outcomes, such as walking distance, global comparison with baseline, and overall satisfaction, were superior after sacroiliac joint arthrodesis compared with conservative management (Figs. 5-A, 5-B, and 5-C). In subjects in the sacroiliac joint arthrodesis group, work status improved significantly over time (p = 0.001).
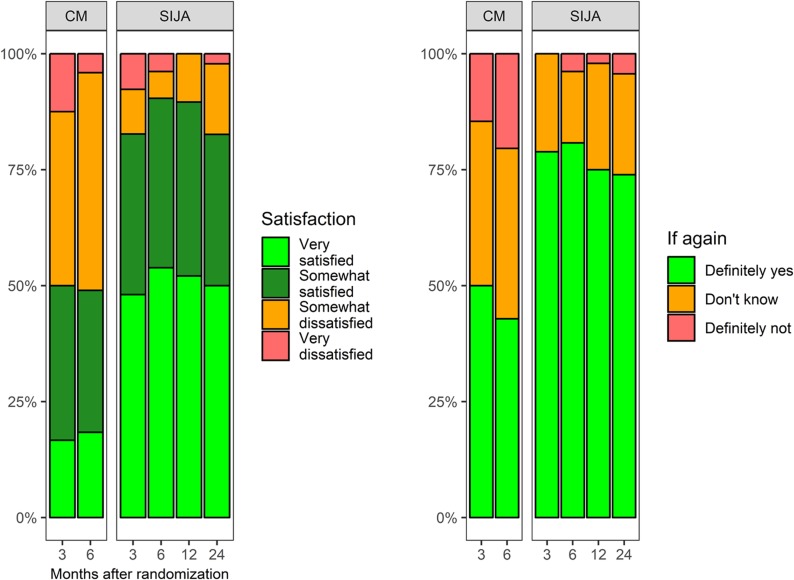
Figs. 5-A, 5-B, and 5-C Bar graphs showing outcomes after conservative management (CM) and sacroiliac joint arthrodesis (SIJA). The last-observation-carried-forward method was used to estimate values after crossover.
Fig. 5-A.
Change in walking distance and ambulatory status.
Fig. 5-B.
Change in work status and comparison with baseline.
Fig. 5-C.
Change in satisfaction and desirability of having a surgical procedure again by treatment and follow-up visit.
Crossover
In the conservative management group, there was no early crossover to sacroiliac joint arthrodesis. After the 6-month visit, 21 subjects (43%) in the conservative management group crossed over to sacroiliac joint arthrodesis. Crossover subjects had similar baseline characteristics compared with subjects who did not cross over, with the exception of more leg pain and a higher proportion of opioid use (30% compared with 5%). Subjects who crossed over had higher 6-month low back pain, leg pain, and ODI scores compared with subjects who did not cross over. Additionally, subjects who crossed over at 6 months had almost no mean improvement in pain and the ODI by 6 months. In contrast, subjects who did not cross over had modest improvements in back pain and the ODI by 6 months. After crossover to sacroiliac joint arthrodesis, improvements in pain, disability, and quality of life were similar to those observed in subjects originally assigned to sacroiliac joint arthrodesis (Fig. 6).
Fig. 6.
Change in VAS low back (LB) pain, VAS leg pain, ODI, Zung Depression Scale, EQ-5D time trade-off (TTO), and EQ-5D VAS scores including subjects who crossed over from conservative management to sacroiliac joint arthrodesis. Green indicates the subjects initially assigned to sacroiliac joint arthrodesis, blue indicates subjects assigned to the conservative management group prior to crossover, and gray indicates conservative management subjects who crossed over to surgical treatment with the sacroiliac joint arthrodesis group after the 6-month visit. The values shown are the mean. The error bars indicate the 95% CI.
Adverse Events
During the first 6 months (200 days), 20 adverse events occurred in 16 subjects in the sacroiliac joint arthrodesis group and 17 adverse events occurred in 15 subjects in the conservative management group (Table III). The rate of events prior to 6 months was similar across groups: 0.33 in the sacroiliac joint arthrodesis group compared with 0.38 in the conservative management group (p = 0.6644).
TABLE III.
Adverse Events by Relationship to Study Device, Severity, Treatment, and Timing
| Conservative Management Event Severity† | Sacroiliac Joint Arthrodesis Event Severity† | ||||||
| Probably or Definitely Related to Study Device or Procedure | Event Timing* | Mild | Moderate | Severe | Mild | Moderate | Severe |
| No | ≤6 months | 3 | 3 | 11 | 2 | 2 | 12 |
| >6 months | 2 | 10 | 15 | 4 | 7 | 23 | |
| Yes | ≤6 months | 0 | 0 | 0 | 0 | 0 | 4 |
| >6 months | 1 | 1 | 1 | 0 | 0 | 0 | |
| All events | All | 6 | 14 | 27 | 6 | 9 | 39 |
The time of 6 months corresponds to 200 days after assignment either to conservative management or sacroiliac joint arthrodesis.
The values are given as the number of adverse events.
By 24 months, 39 events occurred in the sacroiliac joint arthrodesis group that were rated as severe. Of these, only 4 were probably or definitely related to the study device or procedure: 2 cases of increased sacroiliac joint pain, 1 case of gluteal hematoma, and 1 case of implant-related nerve root impingement causing radicular pain that resolved after a revision surgical procedure. Severe events unrelated to the device or procedure included 14 events in the low back (e.g., disc herniation, lumbar facet pain), 3 events in the hip (e.g., trochanteric bursitis), 10 events in the pelvis (primarily sacroiliac joint or contralateral sacroiliac joint pain), and 8 events unrelated to the pelvis, spine, or hip. In the conservative management group, 27 severe adverse events were observed, of which only 1 was related to a study procedure. In this case, the subject had gluteal and leg pain after a crossover sacroiliac joint arthrodesis; CT showed implant loosening and the pain experienced by the subject responded to a repeat diagnostic sacroiliac joint block. A revision surgical procedure was performed with implant removal and intra-articular arthrodesis via a posteroinferior approach using screws.
Radiographic Analysis
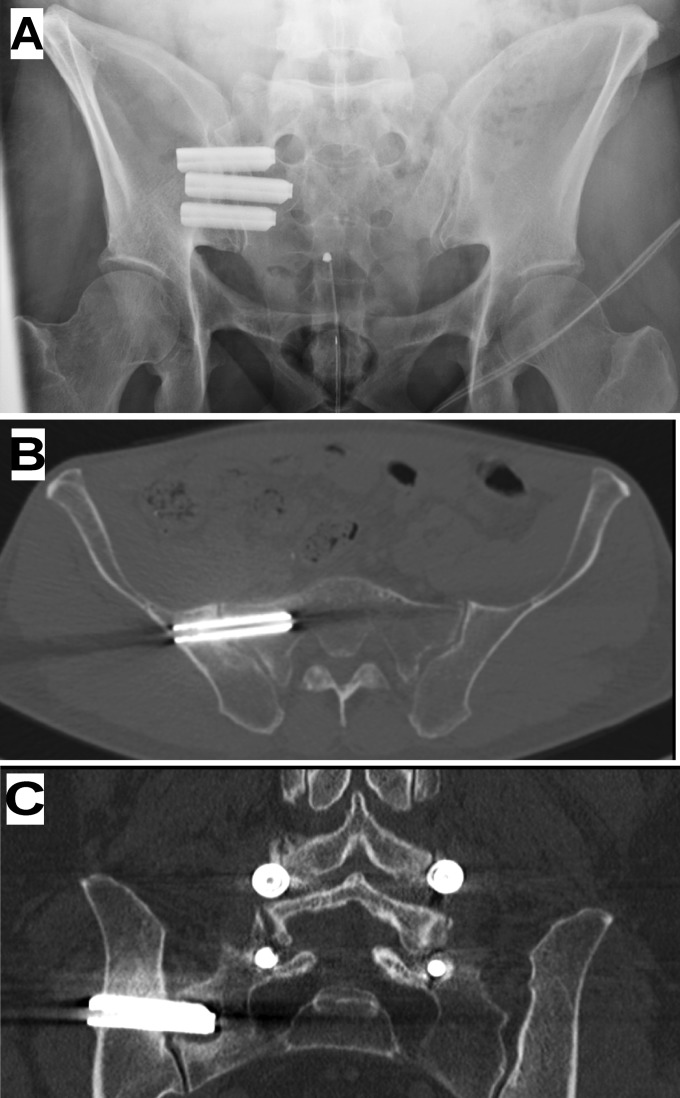
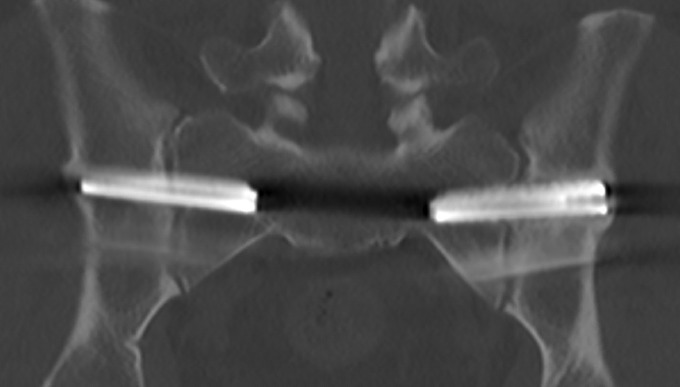
Forty-three of 52 subjects in the sacroiliac joint arthrodesis group had an evaluable 12-month CT scan, providing information on 35 right sides and 31 left sides with a total of 198 implants. Representative CT imaging is shown in Figure 7. According to the independent radiologist reader, the following observations were made. There was no evidence of implant breakage or migration. Breaches (i.e., penetration of cortical margins) occurred in 17 (8.6%) of 198 implants, including 7 breaches into a sacral foramen. Breaches were more commonly observed in the caudal-most implant (11 cases).
Fig. 7.
Imaging of typical configuration of implants. Fig. 7-A Inlet-view pelvic radiograph. Fig. 7-B A 12-month CT image from a different subject showing no radiolucencies around the first implant. Fig. 7-C A 12-month CT image from another subject showing radiolucency around the second implant in the sacrum.
Five implants (2.5%) showed radiolucency along a single side and 3 implants (1.5%) showed radiolucency along all 3 sides; none of these patients had clinical signs attributable to radiolucency. The majority of implants showed bone apposition to the implants on both the sacral and iliac sides of the sacroiliac joint (Fig. 8). Intra-articular fusion with bridging of trabeculae from ilium to sacrum was not commonly observed. The mean implant engagement length (length from the distal end of the implant to the lateral sacral cortex) was approximately 25 to 28 mm for the first (cranial) implant and progressively decreased to 7 to 11 mm for the caudal-most implant (Table IV). There was no significant relationship between total implant engagement length and clinical responses.
Fig. 8.
A 12-month CT image depicting bilateral implants with bone apposition along the entire length of the superior and inferior sides of both implants. Also, there is bone overgrowth at the outer iliac cortex (the left side is greater than the right side), suggesting complete implant integration into the ilium. However, there is little bone apposition along the implants within the joint.
TABLE IV.
Postoperative Engagement Length by Implant Number, View, and Side Measured in Subjects Undergoing Sacroiliac Joint Arthrodesis
| Implant Number | View (Side*) | No of Patients | Engagement Length† (mm) |
| 1 (superior) | Axial (anterior) | 64 | 27.3 ± 5.5 (16 to 41) |
| Axial (posterior) | 64 | 23.5 ± 6.1 (5 to 35) | |
| Coronal (superior) | 63 | 27.9 ± 5.2 (15 to 44) | |
| Coronal (inferior) | 63 | 25 ± 5.5 (13 to 42) | |
| 2 | Axial (anterior) | 64 | 19.2 ± 5.3 (9 to 36) |
| Axial (posterior) | 64 | 16 ± 5.2 (4 to 30) | |
| Coronal (superior) | 63 | 18.7 ± 5.1 (7 to 32) | |
| Coronal (inferior) | 63 | 16.3 ± 5 (7 to 28) | |
| 3 | Axial (anterior) | 63 | 16.1 ± 5.7 (5 to 36) |
| Axial (posterior) | 59 | 13.2 ± 5.9 (0 to 26) | |
| Coronal (superior) | 62 | 15.6 ± 5.9 (1 to 33) | |
| Coronal (inferior) | 61 | 14.1 ± 5.6 (0 to 32) | |
| 4 (caudal) | Axial (anterior) | 1 | 11 |
| Axial (posterior) | 1 | 8 | |
| Coronal (superior) | 1 | 10 | |
| Coronal (inferior) | 1 | 7 |
The sides are determined as the anterior side of the implant on an axial view, the posterior side of the implant on an axial view, the superior side of the implant on a coronal view, and the inferior side of the implant on a coronal view.
The values for implants 1 to 3 are given as the mean and the standard deviation, with the range in parentheses; the values for implant 4 are given as the mean.
Discussion
The results of this randomized controlled trial support sacroiliac joint arthrodesis with lateral transarticular placement of triangular titanium implants as a safe and effective treatment for chronic sacroiliac joint pain unresponsive to conservative management. Subjects undergoing sacroiliac joint arthrodesis experienced sustained improvements in multiple patient-reported parameters, including low back and leg pain, disability, and quality of life, as well as modest improvements in depression scores. Improvements were also seen in walking distance and work status. A unique feature of our study is the assessment of physical function, including the active straight leg raise test and repeat physical examination maneuvers that stress the sacroiliac joint, both of which showed improvements after sacroiliac joint arthrodesis but not after conservative management. In addition, similar improvements in key parameters occurred in conservative management subjects who crossed over to sacroiliac joint arthrodesis. In contrast, conservative management provided little, if any, net improvement in any of these parameters, including pain, disability, quality of life, depression scores, ability to perform the active straight leg raise test, or number of positive physical examination maneuvers. These findings provide evidence of the intermediate-term superiority of sacroiliac joint arthrodesis over continued conservative treatments in a patient population with debilitating chronic sacroiliac joint pain.
Although all study patients had undergone at least 6 months of conservative management prior to enrollment, with persistence of pain and disability, only a small portion of conservative management subjects experienced improvements in pain during the study. Of interest, patients in the conservative management group who experienced a clinically important improvement in low back pain by 6 months showed improvement starting as early as the first 3 months. This finding suggests that the conservative management treatment effect can be judged relatively quickly. Also, the proportion of subjects with opioid use decreased only after sacroiliac joint arthrodesis but not after conservative management. Because low back pain is a frequent trigger for long-term opioid use, our results support the view that the current discussion on the detrimental epidemiological impact of opioid use ought to include alternatives to conservative management that may help to decrease the demand for opioids.
Subgroup analysis showed that current smokers had somewhat smaller low back pain and ODI improvements after sacroiliac joint arthrodesis compared with nonsmokers. However, smokers still derived clinically important benefits from the procedure. These results are consistent with a pooled analysis of data from the current study and 2 U.S. studies25.
Radiographic analysis, based on 12-month CT scans, showed no evidence of device migration or breakage. Breaches (i.e., the presence of some aspect of the implant outside of the sacral cortex on CT scan) were mostly not associated with clinical symptoms, with the exception of 1 subject with post-placement radicular pain that improved on surgical implant repositioning. Breach was more common in implants placed more caudally, confirming that caudal implant placement is more technically challenging. Symptomatic breaches typically manifest with immediate postoperative new neuropathic pain; in our study, late (12-month) CT scans did not show any breaches associated with new or recurrent symptoms. Radiolucencies occurred at a low frequency; no radiolucency seen by the independent radiologist was associated with new or recurrent symptoms. In 2 cases, radiolucencies seen by the investigator were associated with recurrent sacroiliac joint pain, and, in 1 case, a revision surgical procedure was performed to address apparent loosening of the implants. Implant engagement length into the sacrum was largest for the cranial-most implants and progressively decreased for the more caudal implants. Typically, the superior-most implant can be placed deeply into the sacral ala above the S1 neuroforamen. The sacral ala progressively narrows caudally and the presence of neuroforamina precludes deep implant placement for implants placed more caudally. Although increased total implant engagement length into the sacrum may improve sacroiliac joint stabilization, we were unable to demonstrate a significant relationship with clinical responses.
Binding of bone to implants within the sacrum and ilium was commonly seen; bridging bone, reflecting intra-articular fusion, which was not evaluated in our study, may take longer9,26. However, in contrast to other joints that are surgically fused, the sacroiliac joint has very little inherent motion; our data substantiate that permanent stabilization with implants showing avid bone binding at 12 months results in excellent patient outcomes; whether maneuvers to accelerate fusion with obliteration of the sacroiliac joint improve patient outcomes is unclear.
No unanticipated adverse events occurred. The rate of revision surgical procedures in subjects undergoing sacroiliac joint arthrodesis (2 cases) was low and consistent with prior trials and analyses9,11,15,27,28, which showed that the perforation of sacral nerve foramina rarely occurs after sacroiliac joint arthrodesis27. In the literature, the revision rates after sacroiliac joint arthrodesis (3.4% at 4 years27) are lower than after a lumbar spine surgical procedure (14% at 4 years29).
Our findings are consistent with findings from a U.S. randomized trial9, a prospective U.S. single-arm study11, and several retrospective cohorts12-18. The improvements that we observed in low back pain were also similar to those observed in patients in the Swedish Spine Register of various spine surgical procedures30.
Our study has multiple strengths, including its multicenter design according to a uniform clinical protocol with a control group receiving maximal conservative management, a standardized diagnostic algorithm, similar implant placement configurations across participating study centers, and 2-year follow-up. The primary limitation of our study was a lack of subject and outcome assessor blinding, which would have been challenging because implants are radiopaque and preventing subjects from seeing their radiographic studies would have been impossible. The large effect sizes seen strongly argue against a marked contribution from placebo effects. Although our trial followed nonsurgical European guidelines for the treatment of sacroiliac joint pain with intensive physical therapy provided, it is possible that more intensive conservative management might have provided somewhat better results. An additional limitation was the high crossover rate after 6 months. Finally, we note that our study utilized sacroiliac joint arthrodesis with a single system (triangular titanium implants); whether our results apply to other sacroiliac joint arthrodesis surgical approaches, systems, and devices is not known. Except for smoking status, baseline parameters were distributed evenly across treatment groups. Subjects assigned to sacroiliac joint arthrodesis were more likely to be smokers; if smoking reduces the rate of bone-healing, as is commonly accepted, the increased proportion of smokers in the sacroiliac joint arthrodesis group would have biased study results against sacroiliac joint arthrodesis. Post-randomization interventions or subject behaviors that could have impacted the study’s results were not readily apparent; some subjects in the conservative management group received prolonged physical therapy, which theoretically could have increased its effect. The collection of information to support the calculation of health indices (e.g., Charlson Comorbidity Index31) and further opioid history during a 6-month period prior to the study start could also have been helpful. An analysis of predictors of response in the conservative management group is also of interest; however, our sample size was too small to accomplish this goal.
In conclusion, minimally invasive sacroiliac joint arthrodesis with triangular titanium implants was safe and effective at 2 years for the treatment of chronic sacroiliac joint pain and provided lasting improvements compared with conservative management. Our findings suggest that minimally invasive sacroiliac joint arthrodesis may be a reasonable option for patients with sacroiliac joint pain not responsive to 6 months of conservative management.
Appendix
The details on the study design are available with the online version of this article as a data supplement at jbjs.org (http://links.lww.com/JBJS/F144).
Supplementary Material
Footnotes
A commentary by Mark C. Lee, MD, is linked to the online version of this article at jbjs.org.
Disclosure: The study was funded by SI-BONE (Santa Clara, California), the manufacturer of the iFuse Implant System used in the study. One author of this study (D.C.) is an employee at SI-BONE. Four authors (D.K., R.P., E.V.E., and B.S.) are consultants to SI-BONE. The study sponsors participated in study design, data collection, data analysis, data interpretation, and writing of the report. One author of this study (J.D.) had full access to all study data and had final responsibility for the decision to submit for publication. Study data are available through the Yale University Open Data Access (YODA) data-sharing program. The Disclosure of Potential Conflicts of Interest forms are provided with the online version of the article. (http://links.lww.com/JBJS/F143).
References
- 1.Vos T, Flaxman AD, Naghavi M, Lozano R, Michaud C, Ezzati M, Shibuya K, Salomon JA, Abdalla S, Aboyans V, Abraham J, Ackerman I, Aggarwal R, Ahn SY, Ali MK, Alvarado M, Anderson HR, Anderson LM, Andrews KG, Atkinson C, Baddour LM, Bahalim AN, Barker-Collo S, Barrero LH, Bartels DH, Basáñez MG, Baxter A, Bell ML, Benjamin EJ, Bennett D, Bernabé E, Bhalla K, Bhandari B, Bikbov B, Bin Abdulhak A, Birbeck G, Black JA, Blencowe H, Blore JD, Blyth F, Bolliger I, Bonaventure A, Boufous S, Bourne R, Boussinesq M, Braithwaite T, Brayne C, Bridgett L, Brooker S, Brooks P, Brugha TS, Bryan-Hancock C, Bucello C, Buchbinder R, Buckle G, Budke CM, Burch M, Burney P, Burstein R, Calabria B, Campbell B, Canter CE, Carabin H, Carapetis J, Carmona L, Cella C, Charlson F, Chen H, Cheng AT, Chou D, Chugh SS, Coffeng LE, Colan SD, Colquhoun S, Colson KE, Condon J, Connor MD, Cooper LT, Corriere M, Cortinovis M, de Vaccaro KC, Couser W, Cowie BC, Criqui MH, Cross M, Dabhadkar KC, Dahiya M, Dahodwala N, Damsere-Derry J, Danaei G, Davis A, De Leo D, Degenhardt L, Dellavalle R, Delossantos A, Denenberg J, Derrett S, Des Jarlais DC, Dharmaratne SD, Dherani M, Diaz-Torne C, Dolk H, Dorsey ER, Driscoll T, Duber H, Ebel B, Edmond K, Elbaz A, Ali SE, Erskine H, Erwin PJ, Espindola P, Ewoigbokhan SE, Farzadfar F, Feigin V, Felson DT, Ferrari A, Ferri CP, Fèvre EM, Finucane MM, Flaxman S, Flood L, Foreman K, Forouzanfar MH, Fowkes FG, Franklin R, Fransen M, Freeman MK, Gabbe BJ, Gabriel SE, Gakidou E, Ganatra HA, Garcia B, Gaspari F, Gillum RF, Gmel G, Gosselin R, Grainger R, Groeger J, Guillemin F, Gunnell D, Gupta R, Haagsma J, Hagan H, Halasa YA, Hall W, Haring D, Haro JM, Harrison JE, Havmoeller R, Hay RJ, Higashi H, Hill C, Hoen B, Hoffman H, Hotez PJ, Hoy D, Huang JJ, Ibeanusi SE, Jacobsen KH, James SL, Jarvis D, Jasrasaria R, Jayaraman S, Johns N, Jonas JB, Karthikeyan G, Kassebaum N, Kawakami N, Keren A, Khoo JP, King CH, Knowlton LM, Kobusingye O, Koranteng A, Krishnamurthi R, Lalloo R, Laslett LL, Lathlean T, Leasher JL, Lee YY, Leigh J, Lim SS, Limb E, Lin JK, Lipnick M, Lipshultz SE, Liu W, Loane M, Ohno SL, Lyons R, Ma J, Mabweijano J, MacIntyre MF, Malekzadeh R, Mallinger L, Manivannan S, Marcenes W, March L, Margolis DJ, Marks GB, Marks R, Matsumori A, Matzopoulos R, Mayosi BM, McAnulty JH, McDermott MM, McGill N, McGrath J, Medina-Mora ME, Meltzer M, Mensah GA, Merriman TR, Meyer AC, Miglioli V, Miller M, Miller TR, Mitchell PB, Mocumbi AO, Moffitt TE, Mokdad AA, Monasta L, Montico M, Moradi-Lakeh M, Moran A, Morawska L, Mori R, Murdoch ME, Mwaniki MK, Naidoo K, Nair MN, Naldi L, Narayan KM, Nelson PK, Nelson RG, Nevitt MC, Newton CR, Nolte S, Norman P, Norman R, O’Donnell M, O’Hanlon S, Olives C, Omer SB, Ortblad K, Osborne R, Ozgediz D, Page A, Pahari B, Pandian JD, Rivero AP, Patten SB, Pearce N, Padilla RP, Perez-Ruiz F, Perico N, Pesudovs K, Phillips D, Phillips MR, Pierce K, Pion S, Polanczyk GV, Polinder S, Pope CA, 3rd, Popova S, Porrini E, Pourmalek F, Prince M, Pullan RL, Ramaiah KD, Ranganathan D, Razavi H, Regan M, Rehm JT, Rein DB, Remuzzi G, Richardson K, Rivara FP, Roberts T, Robinson C, De Leòn FR, Ronfani L, Room R, Rosenfeld LC, Rushton L, Sacco RL, Saha S, Sampson U, Sanchez-Riera L, Sanman E, Schwebel DC, Scott JG, Segui-Gomez M, Shahraz S, Shepard DS, Shin H, Shivakoti R, Singh D, Singh GM, Singh JA, Singleton J, Sleet DA, Sliwa K, Smith E, Smith JL, Stapelberg NJ, Steer A, Steiner T, Stolk WA, Stovner LJ, Sudfeld C, Syed S, Tamburlini G, Tavakkoli M, Taylor HR, Taylor JA, Taylor WJ, Thomas B, Thomson WM, Thurston GD, Tleyjeh IM, Tonelli M, Towbin JA, Truelsen T, Tsilimbaris MK, Ubeda C, Undurraga EA, van der Werf MJ, van Os J, Vavilala MS, Venketasubramanian N, Wang M, Wang W, Watt K, Weatherall DJ, Weinstock MA, Weintraub R, Weisskopf MG, Weissman MM, White RA, Whiteford H, Wiersma ST, Wilkinson JD, Williams HC, Williams SR, Witt E, Wolfe F, Woolf AD, Wulf S, Yeh PH, Zaidi AK, Zheng ZJ, Zonies D, Lopez AD, Murray CJ, AlMazroa MA, Memish ZA. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012. December 15;380(9859):2163-96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hudson TJ, Edlund MJ, Steffick DE, Tripathi SP, Sullivan MD. Epidemiology of regular prescribed opioid use: results from a national, population-based survey. J Pain Symptom Manage. 2008. September;36(3):280-8. Epub 2008 Jul 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Volkow ND. America’s addiction to opioids: heroin and prescription drug abuse. 2014. May 14 https://www.drugabuse.gov/about-nida/legislative-activities/testimony-to-congress/2014/americas-addiction-to-opioids-heroin-prescription-drug-abuse. Accessed 2018 Oct 15.
- 4.Bernard TN, Jr, Kirkaldy-Willis WH. Recognizing specific characteristics of nonspecific low back pain. Clin Orthop Relat Res. 1987. April;217:266-80. [PubMed] [Google Scholar]
- 5.Sembrano JN, Polly DW., Jr How often is low back pain not coming from the back? Spine (Phila Pa 1976). 2009. January 1;34(1):E27-32. [DOI] [PubMed] [Google Scholar]
- 6.Schwarzer AC, Aprill CN, Bogduk N. The sacroiliac joint in chronic low back pain. Spine (Phila Pa 1976). 1995. January 1;20(1):31-7. [DOI] [PubMed] [Google Scholar]
- 7.DePalma MJ, Ketchum JM, Saullo TR. Etiology of chronic low back pain in patients having undergone lumbar fusion. Pain Med. 2011. May;12(5):732-9. Epub 2011 Apr 11. [DOI] [PubMed] [Google Scholar]
- 8.Stark JG, Fuentes JA, Fuentes TI, Idemmili C. The history of sacroiliac joint arthrodesis: a critical review and introduction of a new technique. Curr Orthop Pract. 2011. November;22(6):545-57. [Google Scholar]
- 9.Polly DW, Swofford J, Whang PG, Frank CJ, Glaser JA, Limoni RP, Cher DJ, Wine KD, Sembrano JN; INSITE Study Group. Two-year outcomes from a randomized controlled trial of minimally invasive sacroiliac joint fusion vs. non-surgical management for sacroiliac joint dysfunction. Int J Spine Surg. 2016. August 23;10:28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sturesson B, Kools D, Pflugmacher R, Gasbarrini A, Prestamburgo D, Dengler J. Six-month outcomes from a randomized controlled trial of minimally invasive SI joint fusion with triangular titanium implants vs conservative management. Eur Spine J. 2017. March;26(3):708-19. Epub 2016 May 14. [DOI] [PubMed] [Google Scholar]
- 11.Duhon BS, Bitan F, Lockstadt H, Kovalsky D, Cher D, Hillen T; SIFI Study Group. Triangular titanium implants for minimally invasive sacroiliac joint fusion: 2-year follow-up from a prospective multicenter trial. Int J Spine Surg. 2016. April 20;10:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rudolf L. Sacroiliac joint arthrodesis-MIS technique with titanium implants: report of the first 50 patients and outcomes. Open Orthop J. 2012;6:495-502. Epub 2012 Nov 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cummings J, Jr, Capobianco RA. Minimally invasive sacroiliac joint fusion: one-year outcomes in 18 patients. Ann Surg Innov Res. 2013. September 16;7(1):12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gaetani P, Miotti D, Risso A, Bettaglio R, Bongetta D, Custodi V, Silvani V. Percutaneous arthrodesis of sacro-iliac joint: a pilot study. J Neurosurg Sci. 2013. December;57(4):297-301. [PubMed] [Google Scholar]
- 15.Sachs D, Capobianco R, Cher D, Holt T, Gundanna M, Graven T, Shamie AN, Cummings J., Jr One-year outcomes after minimally invasive sacroiliac joint fusion with a series of triangular implants: a multicenter, patient-level analysis. Med Devices (Auckl). 2014. August 28;7:299-304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ledonio CGT, Polly DW, Jr, Swiontkowski MF. Minimally invasive versus open sacroiliac joint fusion: are they similarly safe and effective? Clin Orthop Relat Res. 2014. June;472(6):1831-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Smith AG, Capobianco R, Cher D, Rudolf L, Sachs D, Gundanna M, Kleiner J, Mody MG, Shamie AN. Open versus minimally invasive sacroiliac joint fusion: a multi-center comparison of perioperative measures and clinical outcomes. Ann Surg Innov Res. 2013. October 30;7(1):14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Vanaclocha V, Herrera JM, Sáiz-Sapena N, Rivera-Paz M, Verdú-López F. Minimally invasive sacroiliac joint fusion, radiofrequency denervation, and conservative management for sacroiliac joint pain: 6-year comparative case series. Neurosurgery. 2018. January 1;82(1):48-55. [DOI] [PubMed] [Google Scholar]
- 19.Dengler JD, Kools D, Pflugmacher R, Gasbarrini A, Prestamburgo D, Gaetani P, van Eeckhoven E, Cher D, Sturesson B. 1-year results of a randomized controlled trial of conservative management vs. minimally invasive surgical treatment for sacroiliac joint pain. Pain Physician. 2017. September;20(6):537-50. [PubMed] [Google Scholar]
- 20.Mens JM, Vleeming A, Snijders CJ, Koes BW, Stam HJ. Reliability and validity of the active straight leg raise test in posterior pelvic pain since pregnancy. Spine (Phila Pa 1976). 2001. May 15;26(10):1167-71. [DOI] [PubMed] [Google Scholar]
- 21.Fairbank JC, Pynsent PB. The Oswestry Disability Index. Spine (Phila Pa 1976). 2000. November 15;25(22):2940-52; discussion 2952. [DOI] [PubMed] [Google Scholar]
- 22.EuroQol Group. EuroQol—a new facility for the measurement of health-related quality of life. Health Policy. 1990. December;16(3):199-208. [DOI] [PubMed] [Google Scholar]
- 23.Zung WW, Richards CB, Short MJ. Self-rating depression scale in an outpatient clinic. Further validation of the SDS. Arch Gen Psychiatry. 1965. December;13(6):508-15. [DOI] [PubMed] [Google Scholar]
- 24.R: A language and environment for statistical computing. Vienna: R Core Team; 2013. [Google Scholar]
- 25.Dengler J, Duhon B, Whang P, Frank C, Glaser J, Sturesson B, Garfin S, Cher D, Rendahl A, Polly D; INSITE, iMIA, SIFI Study Groups. Predictors of outcome in conservative and minimally invasive surgical management of pain originating from the sacroiliac joint: a pooled analysis. Spine (Phila Pa 1976). 2017. November 1;42(21):1664-73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rudolf L, Capobianco R. Five-year clinical and radiographic outcomes after minimally invasive sacroiliac joint fusion using triangular implants. Open Orthop J. 2014. October 17;8:375-83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cher DJ, Reckling WC, Capobianco RA. Implant survivorship analysis after minimally invasive sacroiliac joint fusion using the iFuse Implant System(®). Med Devices (Auckl). 2015. November 23;8:485-92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cher D, Wroe K, Reckling WC, Yerby S. Postmarket surveillance of 3D-printed implants for sacroiliac joint fusion. Med Devices (Auckl). 2018. September 28;11:337-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Martin BI, Mirza SK, Flum DR, Wickizer TM, Heagerty PJ, Lenkoski AF, Deyo RA. Repeat surgery after lumbar decompression for herniated disc: the quality implications of hospital and surgeon variation. Spine J. 2012. February;12(2):89-97. Epub 2011 Dec 21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Strömqvist B, Fritzell P, Hägg O, Jönsson B, Sandén B; Swedish Society of Spinal Surgeons. Swespine: the Swedish spine register : the 2012 report. Eur Spine J. 2013. April;22(4):953-74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373-83. [DOI] [PubMed] [Google Scholar]
- 32.Vleeming A, Albert HB, Östgaard HC, Sturesson B, Stuge B. European guidelines for the diagnosis and treatment of pelvic girdle pain. Eur Spine J. 2008. June;17(6):794-819. Epub 2008 Feb 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Childs JD, Piva SR, Fritz JM. Responsiveness of the numeric pain rating scale in patients with low back pain. Spine (Phila Pa 1976). 2005. June 1;30(11):1331-4. [DOI] [PubMed] [Google Scholar]
- 34.Copay AG, Cher DJ. Is the Oswestry Disability Index a valid measure of response to sacroiliac joint treatment? Qual Life Res. 2016. February;25(2):283-92. Epub 2015 Aug 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.