Abstract
Background:
Gender confirming primary breast augmentation is becoming more common. The purpose of this study was to compare the demographic and anatomical differences in cis-female and trans-female populations.
Methods:
This was a retrospective analysis of trans-female patients and cis-female patients undergoing primary breast augmentation at a single institution. Analysis included patient demographics and preoperative chest measurements including sternal notch to nipple distance (SSN), breast width (BW), nipple to inframammary fold distance (N-IMF), and nipple to midline distance (N-M). Continuous variables were compared using independent t tests, and discrete variables were compared using Pearson’s χ2 tests.
Results:
Eighty-two trans-female and 188 cis-female patients undergoing primary breast augmentation were included. Trans-female patients were older (40.37 versus 34.07), more likely to have psychological comorbidities (50% versus 12.23%), and had a higher body mass index, 27.46 kg/m2 versus 22.88 kg/m2 (P = 1.91E-07), than cis-female patients. Cis-female patients most commonly had an ectomorph body habitus (52% versus 26%), whereas trans-female patients most commonly had an endomorph body habitus (40% versus 7%). Pseudoptosis or ptosis was more commonly seen in cis-female patients (P = 0.0056). There were significant differences in preoperative breast measurements including sternal notch to nipple distance, BW, and N-M between groups, but not in N-IMF. The ratio of BW/N-IMF was statistically significant (P = 2.65E-07 on right), indicating that the similarity in N-IMF distance did not adjust for the difference in BW.
Conclusions:
The trans-female and cis-female populations seeking primary breast augmentation have significant demographic and anatomical differences. This has implications for surgical decision-making and planning to optimize outcomes for trans-female patients.
INTRODUCTION
Treatment of gender dysphoria through transition from the male to trans-feminine phenotype relies on an adequate acquisition of female secondary sex characteristics.1 However, despite estrogen therapy, as many as 60% of patients fail to achieve adequate breast growth and require implant-based augmentation to realize a more feminine chest shape.2 Although augmentation in trans-female patients shares obvious similarities with cis-gender augmentation procedures, there are also significant differences. The trans-female chest differs morphologically to both cis-female and cis-male chests due to the exposure of testosterone during adolescence and exogenous estrogen during gender transition. As trans breast augmentation procedures become more commonplace, it is important to understand these differences and associated implications for surgical planning.
In this study, we hypothesized that there are significant differences in the preoperative breast measurements between the cis- and trans-female populations, most notably the ratio between breast width (BW) and nipple to inframammary fold distance (N-IMF) distance. Furthermore, we postulate that the trans-female patients’ demographics and comorbidities differ from the cosmetic patient population, particularly in regard to age, comorbidities, and body mass index (BMI). We have noticed that transgender augmentation patients in our clinic tend to fall into the “endomorph” body type, which is in sharp contrast to our cis gender patients, who tend to have a more “mesomorph” build (Fig. 1). In this study, we attempted to validate these subjective observations and use this information to demonstrate how these differences influence preoperative counseling, implant selection, and surgical planning, all of which are unique to the trans-female population.
Fig. 1.
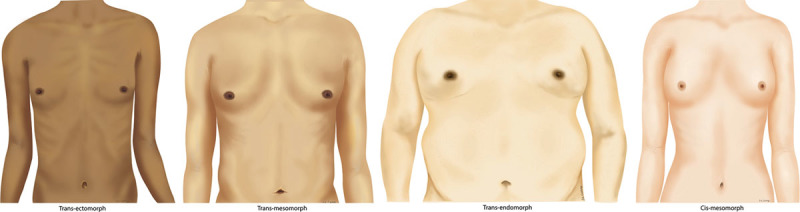
Illustration of all 3 body type classifications in transgender patients, compared with the most common cis-mesomorph body type.
Fig. 2.
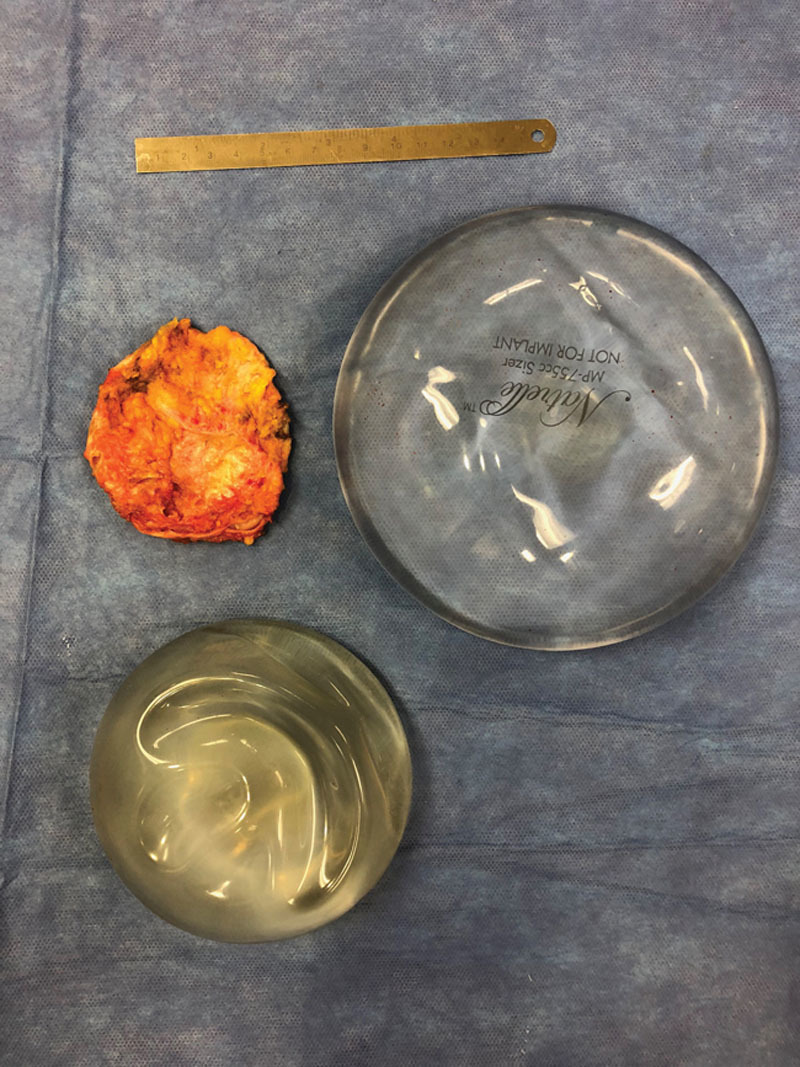
Implant removed due to inadequate base width compared to replacement implant with 16.5 cm base width.
METHODS
This is a retrospective analysis of prospectively collected data by a single surgeon who evaluated trans-female patients for augmentation mammaplasty between April 2016 and February 2018. For the control group, we included all cis-female patients seen by 2 senior surgeons at the same institution between September 1998 and July 2017. Inclusion criteria were the following: age between 18 and 80 years old, documentation of preoperative chest measurements, and access to preoperative photos. Transgender patients were required to have a diagnosis of gender dysphoria and meet all World Professional Association for Transgender Health criteria for gender confirmation surgery (GCS). All transgender patients are required to have been on exogenous estrogen for at least 1 year before consultation.
Demographic data, such as age at the time of consult, BMI, smoking status, and other relevant social history were analyzed between the 2 groups. Specific preoperative measurements were recorded in metrics (centimeter/millimeter), including N-IMF, nipple to midline distance (N-M), sternal notch to nipple distance (SNN), base BW, and areolar diameter.
Two independent reviewers classified each participant based on preoperative photographs (see Table 2 and Fig. 1). Patients were classified as to their body habitus (ectomorph, mesomorph, endomorph), their ptosis grade, and if their breast showed signs of constricted lower pole or herniating areola. Patients who were thin and lean with low muscle content were classified as having an ectomorph body habitus. On contrary, those patients with underdeveloped muscles, elevated BMI, and likelihood of storing fat were classified as having an endomorph body habitus. Finally, those patients with an average or muscular build were classified as having a mesomorph body habitus. Breast ptosis was classified based on the modified Regnault ptosis scale.3
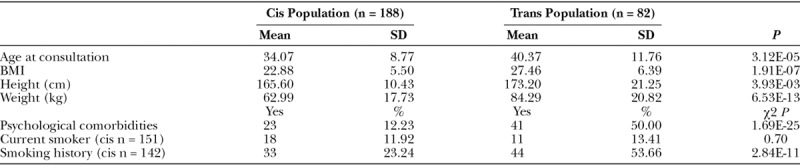
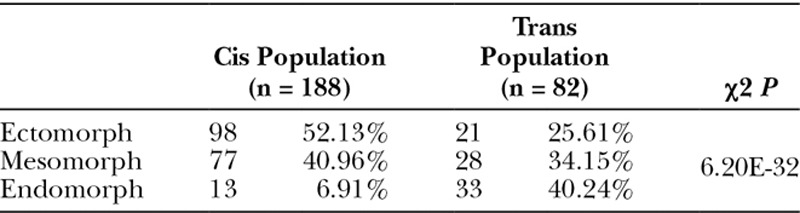
Table 2.
Patient Demographics and Characteristics
Statistical comparisons were conducted using independent t tests for continuous variables and Pearson’s χ2 test for discrete variables. Demographics were analyzed using descriptive statistics, reporting means and frequencies. All analysis was conducted using Microsoft Excel (Microsoft Corporation, Redmond, Wash.). This study was approved by the Institutional Review Board of Oregon Health & Science University.
RESULTS
Patient Demographics and Characteristics
The study population included 82 trans-female patients and 188 cis-female patients seeking primary breast augmentation. The mean time trans-female patients were on estrogen was 54.3 months. Patient demographics and characteristics including age at consultation, BMI (kilogram per square meter), height (centimeter), and weight (kilogram), as well as current and past smoking status and diagnosed psychological comorbidities of depression or anxiety were compared and can be seen in Table 1. Trans-female patients were more likely to seek primary breast augmentation consultation at an older age compared with cis-female patients, 40.37 versus 34.07 years of age, respectively (P = 3.12E-05). Trans-female patients were also more likely to be taller (P = 3.93E-03), weigh more (P = 6.53E-13), and had a statistically significantly higher BMI than cis-female patients, 27.46 kg/m2 versus 22.88 kg/m2 (P = 1.91E-07) at the time of consultation.
Table 1.
Body Habitus in Trans- and Cis-female Populations
There were no significant difference in current smoking status between trans-female and cis-female patients, 11.92% versus 13.41% (P = 0.70). However, trans-female patients were much more likely to have a history of smoking compared with cis-female patients, 51.95% versus 22.82% (P = 2.124E-08). Trans-female patients were statistically more likely to have a diagnosis of depression or anxiety than cis-female patients, 50.0% versus 12.23% (P = 1.69E-25).
Cis-female patients seeking primary breast augmentation were more likely to be classified as having an ectomorph (52% versus 26%) or a mesomorph body habitus (41% versus 34%). On the contrary, trans-female patients were more likely to be classified as having an endomorph body habitus compared with cis-females (40% versus 7%).
Trans-female characteristics regarding duration of social transition and exogenous estrogen are shown in Table 3. The trans-female population in this study on average socially transitioned 84.9 months before consultation with a range of 12–348 months. These patients had been on hormone therapy for on average of 54.20 months before consultation with a range of 12–360 months.
Table 3.
Additional Characteristics of the Trans-female Population (n = 82)
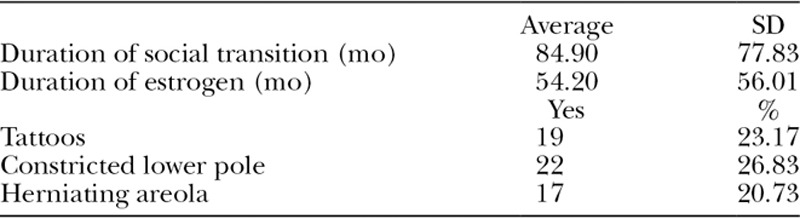
As previously noted, trans-female patients seeking primary breast augmentation do so due to failure to develop natural feminine breast shape despite estrogen therapy. Trans-female patients tend to have interrupted breast development with a constricted lower pole and without return of contour between the areola and the surrounding breast. In this study, 26.83% of trans-female patients demonstrated a constricted lower pole and 20.73% demonstrated herniating areola on physical examination.
Patient population differences in breast ptosis can be seen in Table 4.
Table 4.
Breast Ptosis on Physical Examination
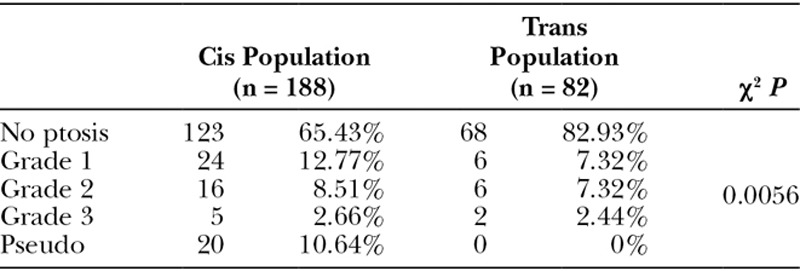
Trans-female patients were more likely to have no breast ptosis on physical examination than cis-female patients, 82.93% versus 65.43%, respectively. Likely due to breast changes after breastfeeding, cis-female patients were much more likely to present with pseudoptosis (20.2% versus 0.0%) or grade I–III breast ptosis compared with trans-female patients (P = 0.0056).
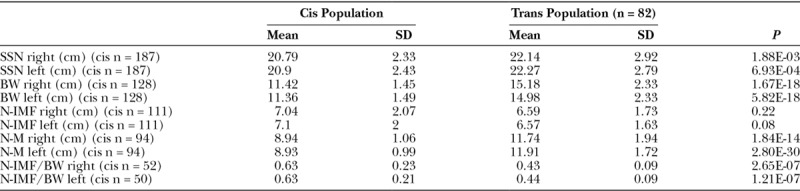
Preoperative Breast Measurements
Breast measurements on physical examination include SNN, BW, N-IMF, and N-M. Table 5 demonstrates the significant differences between cis-female and trans-female breast measurements. All measurements were significantly larger in trans-female patients, with the exception of N-IMF distance bilaterally. Looking at the BW/N-IMF ratio, however, the N-IMF comes out as relatively shorter when compared to the overall breast dimension.
Table 5.
Preoperative Breast Measurements of Cis- and Trans-female Patients
DISCUSSION
The masculine and feminine chest have distinct features that are commonly recognized: male chests are wider, have minimal breast tissue with little to no expansion of the skin envelope, smaller areolas, lateralized nipple–areola complex with less projection, a wider sternum, and greater pectoral muscle bulk.4–6 The cis-female chest undergoes changes as a result of puberty, including breast tissue growth and other morphometric changes that do not resemble the cis-male chest. Although it is anecdotally understood that the trans-female chest resembles neither the cis female or cis male, the existing literature does not address the morphometric changes that result from the limited effects of exogenous estrogen. Furthermore, with the expansion of GCS in the United States, providers who may not routinely treat this patient population will be involved in their care, and it is important to understand how demographic differences and population factors unique to the trans community can impact the preoperative counseling. This paper tried to scientifically address both of those aspects.
Trans-female patients had a significantly higher rate of smoking history and psychiatric comorbidities, which is well in line with the higher rates of mental health comorbidities and low socioeconomic status described in the overall transgender population.7,8 The trans cohort primarily came through the state Medicaid program (Oregon Health Plan), whereas the cosmetic population was predominately private pay. This exemplifies an essential difference between those 2 populations. The transgender population is disproportionately burdened with mental comorbidities and traumatic experiences, as well as prior discrimination within the medical setting.
Patients presenting for cosmetic cis-gender augmentation represent certain subgroups of the cis-gender population, which is reflected in a lower mean age and SD when compared with the trans-female group (40.48 versus 34.07). The same findings were true for BMI, height, and body habitus. This is an interesting finding in that surgeons will be presented with a more heterogenous patient population of a wide age group and body habitus range and should be prepared to alter their approach accordingly. For example, contrary to what one would expect, the increase in age did not correlate with increased ptosis. Trans females were significantly less likely to have relevant ptosis that would necessitate a discussion of mastopexy. This makes sense in light of the absence of breastfeeding and the late onset of breast growth in these patients.
If the clinician considers that a typical trans patient is likely to be a tall endomorph patient with elevated BMI and larger BW on clinical examination, it may be prudent to select a larger implant that accommodates the transverse chest dimensions. Selection of the appropriate implant under these circumstances will allow the surgeon to achieve feminine proportions with medial fullness and perhaps more cleavage.9 Consider a patient with a base width of 16.5 cm and an implant choice with a width of 16 cm. The available sizes for Allergan Natrelle Inspira would be: extra-full N/A; full N/A; moderate 685; low-plus 590; low 510. Those are large-sized implants and differ from the average cis-female augmentation.10 In practice, the senior author uses implants with a wide BW for a vast majority of patients. Figure 3 shows a patient who underwent augmentation with an implant that was too narrow for her base width of 18.5 cm. We exchanged the approximately 400 mL implant with a 755 mL moderate profile implant with a base width of 16.5 cm. The patient desired projection. Otherwise a low-profile implant with an even wider base width would have been advisable. This case nicely illustrates the more proportional appearance of the lateral breast border in this wider chested individual.
Fig. 3.
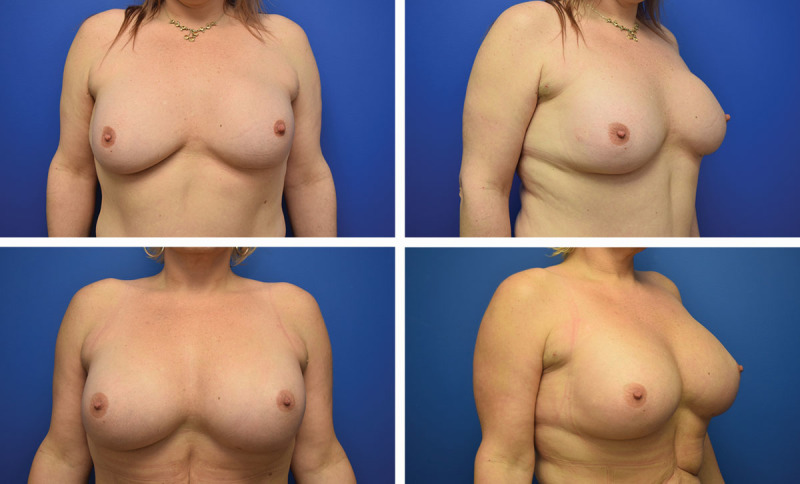
Before and after photos of trans-female patient who presented for revision augmentation. The wider base width implant shown below provides superior cleavage and lateral fullness.
Compromising on the BW will hinder the ability to create medial cleavage but—maybe more importantly—will provide adequate lateral fullness. On the other end of the spectrum is the ectomorph body type where ideally a textured implant would assist in providing the most natural chest shape. In the setting of uncertainty around breast implant–associated anaplastic large cell lymphoma, it is the senior author’s practice to reserve textured implants for patients who independently ask for this implant, are of the ectomorph type and have enough health literacy to understand the severe risks associated with these implants. These implants are not routinely offered unless there is a specific request. Figure 4 shows a patient of ectomorph type with textured implants. Figure 5 shows a mesomorph body type and Figure 6 shows an endomorph body type.
Fig. 4.

Trans-female patient with ectomorph body type—395 mL Allergan Natrelle 410FM textured silicone shaped implants in a submuscular pocket. (Patient counseled on risk of breast implant–associated large cell lymphoma.)
Fig. 5.

Mesomorph body type—445 mL SSM Allergan Natrelle silicone round implants in a subglandular pocket (written permission given by patient to publish despite identifiers).
Fig. 6.

Endomorph body type—685 mL SSM Allergan Natrelle silicone round implants in a subglandular pocket.
The N-IMF distance was not statistically significant between 2 groups. However, if we look at the ratio of BW/N-IMF, then we do find a ratio that is statistically significant and confirming that the N-IMF distance is shorter in the trans-female population (P = 2.65E-07 on right). This translated into a clinical need to substantially lower the inframammary fold in most trans-female patients if an implant of appropriate base width is chosen. This has also been the practical experience of the senior author on this manuscript. Although comparative data were not available for the cis-female control group, we did find a constricted lower pole in over a fourth of the trans-female population and in over a fifth of a herniating areola. These observations suggest that the trans breast is phenotypically similar to a mildly tuberous breast, which is perhaps consistent with arrested development between Tanner stages 2 and 4.11 Surgically, the constricted lower pole must be addressed with radial scoring. Areolar herniation in most cases was mild, and an inframammary incision is still a viable option.
Another interesting finding was that that in our trans data, the average NAC width was 3.43 cm with an SD of 0.89. While we did not directly compare this measurement to the cis-female NAC, the number can be compared with the Beer et al.5 paper citing an ideal male NAC width of 2.69. The relevance of this finding is that some trans-female patients are candidates for a periareolar approach due to significant areolar enlargement after treatment with exogenous estrogen.
In the senior author’s practice, the above data assist in deciding on an implant. Knowing the differences between populations allows for better communication with the patient and guidance in decision-making on 4 aspects of the breast augmentation consult: choice of implant, placement plane, incision site, and size. Estrogen starts to encourage breast growth and body fat redistribution within 3–6 months, with full effects in 2–3 years and 2–5 years, respectively.12 It is, therefore, warranted to at least wait a year after beginning estrogen before performing augmentation. Further increase in volume may occur after augmentation. Although there are no commonly agreed on breast cancer screening guidelines for trans females, University of California, San Francisco has recommended that screening should not start before the age of 50 years and after the patient at least have been on exogenous hormones for 5–10 years.12
Limitations of this study include that the measurements in the cis-female population were performed by different surgeons, and there may be variability in the measurement method. There was also significant variation in which preoperative measurements were taken for cis-patients, preventing the full cohort to be compared with the trans cohort for each preoperative measurement. The trans-female population in this study has a statistically higher variability in SD that is greater than the relative increase of the respective measurement’s magnitude. This is not surprising as the trans-female population experience is not homogeneous. In addition to genetic variability inherent to any population (cis-female patients included), the trans-female population has unique hormonal factors at play. There are a vast number of medical and surgical options for females in transition, and each patient presents at a different stage in the process. All are on estrogen therapy, but from variable ages of initiation, formulations, doses, and lengths of time. As noted previously, estrogen begins to promote breast growth and body fat redistribution within 3–6 months, but its full effects are not seen for several years.12 These circumstances produce a complexity in the patient population that is unparalleled by the cis-gender group.
Estrogen therapy is an imperfect solution for chest feminization for some, and these are the patients who present to the plastic surgeon. However, there are patients in which estrogen either produces a fully developed chest or an underdeveloped chest that is cosmetically pleasing or adequate from the patient’s perspective. The patient satisfied with hormone therapy does not present to the plastic surgeon, and therefore these numbers are difficult to quantify. It is also important to note that breast implants are currently not Food and Drug Administration approved for male gender reassignment surgery and are currently used off-label. This is because the core studies involved in approval did not include “male assigned at birth” patients.
CONCLUSIONS:
Although surgical similarities exist between the operative choices and technique for cis-female and trans-female breast augmentation, marked differences also exist. Surgeons see a wider age, BMI, and body habitus range in this population. Chest measurements reveal a statistically lower N-IMF/BW ratio when compared with the cis-female cohort, necessitating not only larger implant selection but also frequent need to lower the inframammary fold. Plastic surgeons treating these patients should be familiar with these differences and understand the needs specific to this patient population.
Footnotes
Published online 13 March 2019.
Disclosures: The authors have no financial interest to declare in relation to the content of this article. This study was funded by a grant from Allergan pharmaceutical plc.
REFERENCES
- 1.Berli JU, Knudson G, Fraser L, et al. What surgeons need to know about gender confirmation surgery when providing care for transgender individuals: a review. JAMA Surg. 2017;152:394–400. [DOI] [PubMed] [Google Scholar]
- 2.Kanhai RC, Hage JJ, Karim RB, et al. Exceptional presenting conditions and outcome of augmentation mammaplasty in male-to-female transsexuals. Ann Plast Surg. 1999;43:476–483. [DOI] [PubMed] [Google Scholar]
- 3.Regnault P. Breast ptosis. Definition and treatment. Clin Plast Surg. 1976;3:193–203. [PubMed] [Google Scholar]
- 4.Agarwal CA, Wall VT, Mehta ST, et al. Creation of an aesthetic male nipple areolar complex in female-to-male transgender chest reconstruction. Aesthetic Plast Surg. 2017;41:1305–1310. [DOI] [PubMed] [Google Scholar]
- 5.Beer GM, Budi S, Seifert B, et al. Configuration and localization of the nipple-areola complex in men. Plast Reconstr Surg. 2001;108:1947–1952; discussion 1953. [DOI] [PubMed] [Google Scholar]
- 6.Hage JJ, van Kesteren PJ. Chest-wall contouring in female-to-male transsexuals: basic considerations and review of the literature. Plast Reconstr Surg. 1995;96:386–391. [DOI] [PubMed] [Google Scholar]
- 7.James SE, Herman JL, Rankin S, et al. The Report of the 2015 U.S. Transgender Survey. 2016National Center for Transgender Equality. [Google Scholar]
- 8.Winter S, Diamond M, Green J, et al. Transgender people: health at the margins of society. Lancet. 2016;388:390–400. [DOI] [PubMed] [Google Scholar]
- 9.Liu YJ, Thomson JG. Ideal anthropomorphic values of the female breast: correlation of pluralistic aesthetic evaluations with objective measurements. Ann Plast Surg. 2011;67:7–11. [DOI] [PubMed] [Google Scholar]
- 10.Young VL, Nemecek JR, Nemecek DA. The efficacy of breast augmentation: breast size increase, patient satisfaction, and psychological effects. Plast Reconstr Surg. 1994;94:958–969. [DOI] [PubMed] [Google Scholar]
- 11.Templeman C, Hertweck SP. Breast disorders in the pediatric and adolescent patient. Obstet Gynecol Clin North Am. 2000;27:19–34. [DOI] [PubMed] [Google Scholar]
- 12.Deutsch MB, Radix A, Wesp L. Breast cancer screening, management, and a review of case study literature in transgender populations. Semin Reprod Med. 2017;35:434–441. [DOI] [PubMed] [Google Scholar]


