Abstract
Background:
Gender affirmation surgery (GAS) has a positive impact on the health of transgender patients; however, some centers employ body mass index (BMI) as a strict selection criterion for surgical candidacy. Several single-center studies have found no clear correlation between BMI and complication rates. We conducted a retrospective multicenter study at 2 university-based centers to test the null hypothesis: obesity is not a significant determinant of the risk of acute surgical complications in patients undergoing penile inversion vaginoplasty (PIV).
Methods:
This is a retrospective chart review of all adult patients at the University of Michigan and the University of Miami undergoing gender-affirming PIV with minimum follow-up time of 3 months between 1999 and 2017. A logistic regression model of analysis is used to examine the predictive factors for surgical complications and delayed revision urethroplasty in our patient sample.
Results:
One hundred and one patients met inclusion criteria for this study. The mean BMI at the time of procedure was 26.9kg/m2 (range 17.8–48.2). Seventeen patients (16.8%) had major complications and 36 patients (35.6%) had minor complications. On logistic regression analysis, none of the recorded covariates were significant predictors of delayed revision urethroplasty or major, minor, or any complications.
Conclusions:
We found that obese patients can safely undergo GAS and that BMI alone should not preclude appropriately selected patients from undergoing GAS. We acknowledge that selection based on overall health and other medical comorbidities is certainly warranted for gender-affirming PIV and all other surgical procedures.
INTRODUCTION
Gender dysphoria is clinically significant distress caused by the incongruence between an individual’s anatomic sex and intrinsic gender identity.1 Significant evidence suggests that interventions such as gender-affirming surgery (GAS) have a positive impact on the psychological health, well-being, and quality of life of transgender patients.2–4 Accordingly, the scientific medical community, including most medical professional organizations and many insurance carriers, considers GAS as medically necessary for properly selected surgical candidates.5,6 Despite these proven benefits of GAS, multiple barriers exist for individuals seeking these surgical interventions. These obstacles include persistent cultural biases and outdated conceptions of transgender identity, a relative paucity of qualified surgeons and the resulting access-to-care delays, and, even for patients with insurance coverage, financial barriers.7 Individuals seeking GAS should also fulfill time-consuming requirements detailed in the Standards of Care of the World Professional Association of Transgender Health before undergoing GAS.8
Even if a patient has negotiated all these obstacles, transgender persons are often also faced with stringent medical criteria for surgery. Current estimates indicate that >600 million people throughout the world are classified as obese, defined as a body mass index (BMI) >30.9 Across a wide spectrum of surgical procedures, obesity has been shown to be a risk factor for surgical complications, including delayed wound healing and wound failure, surgical site infection, and postoperative venous thromboembolic events (VTEs).10–12 Although there have been few studies specifically examining obesity as a risk factor for surgical complications following gender-affirming vaginoplasty, some centers and surgeons employ BMI as a selection criteria for surgical candidacy,13 denying vaginoplasty to patients with BMIs over an arbitrary cutoff (usually 30 or 35).13
The most commonly employed procedure for GAS in transgender women is penile inversion vaginoplasty (PIV): a complex procedure where the male genital anatomy is disassembled and the components are used to create an anatomically accurate vulva, a sensate neoclitoris, and a neovagina suitable for penetrative intercourse (see Figs. 1, 2). Data from multiple single-center series demonstrate that this procedure is safe and effective, but also that the reported overall surgical complication rate ranges from <30 to >70%.14–21 Because each of these studies reflects a single-center, unique patient population, and varying criteria for surgical candidacy, we questioned whether the 2-fold variance in reported complication rates after PIV could be related to differing degrees of obesity in each center’s patient population. Single-center and single-surgeon studies have questioned the use of arbitrary cutoffs and the effects of BMI on postoperative complication rates following GAS via retrospective analysis and have found no clear correlation.14,21 We were unable to find any multicenter studies confirming these findings in the scientific literature.
Fig. 1.
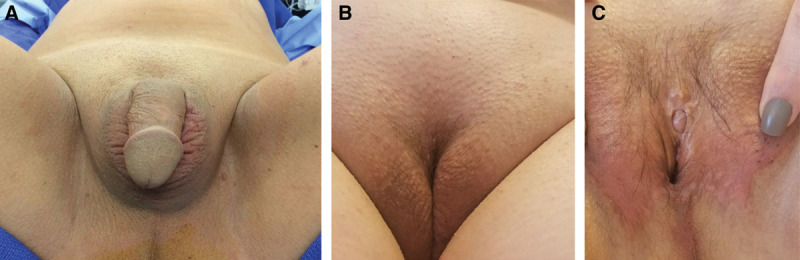
PIV result in transgender patient with BMI ≤30: (A) preoperative and (B and C) 6-month postoperative images following gender-affirming PIV. Patient had successful vaginal penetrative intercourse by 3 months with orgasm via clitoral stimulation. Postoperative course was uncomplicated. Patient classified as “nonobese.”
Fig. 2.
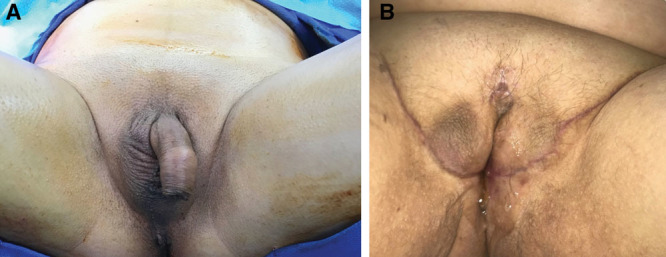
PIV result in transgender patient with BMI ≥30: (A) preoperative and (B) 3-month postoperative images following gender-affirming PIV. Patient BMI of 37; a vaginal depth of 4 inches was achieved. Patient experience debridement of neoclitoris eschar postoperatively with no significant tissue loss. Clitoral orgasm has been achieved, though patient has not engaged in penetrative vaginal intercourse. Patient classified as “obese.”
Larger gender-affirming PIV outcome studies currently available in the literature are not representative of patients with BMIs in the obese range, as the selection criteria of the author’s patients exclude all surgical candidates with a BMI >30.16,21 To contribute to the conclusions that can be drawn from current literature as it relates to surgical outcomes and patient BMI in gender-affirming PIV, we retrospectively reviewed the records of transgender patients who underwent PIV at 2 university-based centers to test the following null hypothesis: obesity is not a significant determinant of the risk of acute surgical complications in patients undergoing PIV.
METHODS
We conducted a retrospective chart review of all adult (≥18 years of age) patients who had a minimum follow-up time of 3 months after undergoing gender-affirming PIV between 1999 and 2017 at both the University of Michigan and the University of Miami. All transgender PIV candidates are required to have met World Professional Association of Transgender Health Standards of Care criteria before surgery.8 In addition, patients are required to meet the general fitness guidelines that apply to all surgical procedures at both institutions, including no current tobacco use, A1c hemoglobin level <8%, and well-managed respiratory or cardiac disease if present. Among these selection criteria, BMI alone was not used as an exclusionary factor for gender-affirming PIV candidacy at either institution.
This study was approved independently by the Institutional Review Boards (IRBs) at both participating institutions (Michigan IRB No. HUM00055218; Miami IRB No. 20160775). Patients were identified using a running database of transgender surgical patients (Miami) or by database query of the entire medical records system based on diagnostic and procedure codes (Michigan). Patients who underwent vaginoplasty by other techniques were excluded.
Patient charts were reviewed and dependent variables were recorded, including demographic data (age, race) and comorbidities, including BMI at the time of procedure, cross-sex hormone therapy, smoking history (current or former), diabetes mellitus, coronary artery disease, and hypertension.
Operative notes and procedural records were used to obtain the operative time of each procedure and any recorded intraoperative complications. Operative times of patients who underwent simultaneous procedures (other than orchiectomy) were not included, as the operative times for these combined procedures would not be representative of the operative time required for PIV alone. We chose to include operative times for PIV procedures performed with a concurrent orchiectomy, as orchiectomy is very commonly performed during a PIV procedure in patients who have not previously undergone an orchiectomy, and orchiectomy may be considered part of the standard gender-affirming PIV.
Postoperative records and visit notes were examined to identify major and minor complications following surgery, as well as delayed revision urethroplasty reoperation for divergent urine stream. Major complications included VTE and any complication requiring reoperation and/or hospital readmission during the initial recovery process. Minor complications included delayed wound healing or dehiscence and incomplete graft take without reoperation, infection not requiring surgical intervention or intravenous antibiotics, transfusion requirement without return to the operating room (intraoperative or postoperative), and intraoperative rectal or urethral injury managed during the first operation and that resolved without sequelae. Delayed revision urethroplasty for divergent urine stream was not considered as a major or minor complication for this procedure; instances were analyzed and reported separately as an additional outcome. Other delayed revisions for cosmetic purposes were not included as complications of this procedure. Major and minor complications were not mutually exclusive.
Descriptive statistics were performed to characterize the demographics of the sample population. Demographics were compared between sites using t tests. Primary outcomes included major complications, minor complications, and any complication. Delayed revision urethroplasty was included as a secondary outcome. Univariate logistic regression was performed first using all covariates as potential predictors of major complications, minor complications, any complications, and delayed revision urethroplasty. Next, multivariate logistic regression models were used to evaluate for any independent effect of age, BMI, diabetes mellitus, and smoking history on each of the 3 outcome variables. Additionally, predictors of operative time were analyzed using multivariate linear regression, including BMI, simultaneous orchiectomy, and study site. Alpha was set at 0.05, and beta error (the statistical power to conclude “no difference”) was calculated post hoc for each outcome variable. Primary statistical analyses were performed using SPSS (IBM). Post hoc power calculations were performed with z-test for logistic regression using G*Power (Universität Düsseldorf).
RESULTS
One hundred and one patients met inclusion criteria for this study (23: Miami, 78: Michigan). The mean age of the study patients at the time of procedure was 42 years, and the mean BMI was 26.9 (ranging from 17.8 to 48.2). Twenty-seven patients had a BMI in the obese range (≥30, 26.5%). The majority (n = 84, 83.2%) of the study population were identified as White. Twelve patients (11.9%) had diabetes mellitus and 31 patients (30.7%) had a history of smoking; 3 of whom may have been current smokers at the time of the procedure. All patients were presumed to have been on cross-sex hormone therapy before surgery, although data were unavailable to confirm this in 2 patients. With the exception of operative time (discussed below), there were no other statistically significant differences between the demographics of the study population at each study site. No patients were lost-to-follow-up at the 3-month timepoint. Full demographic information may be found in Table 1.
Table 1.
Demographics of the Sample Population Overall and by Site Using Descriptive Statistics
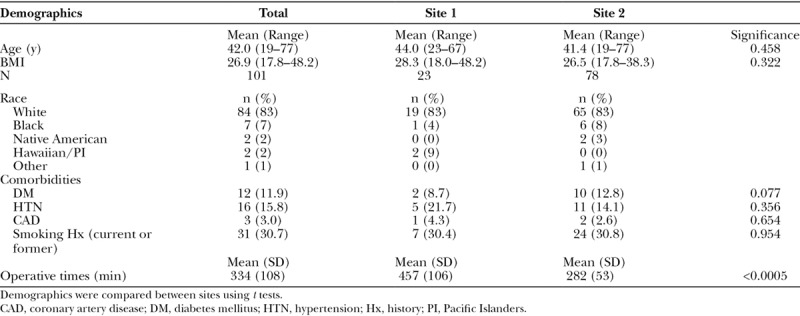
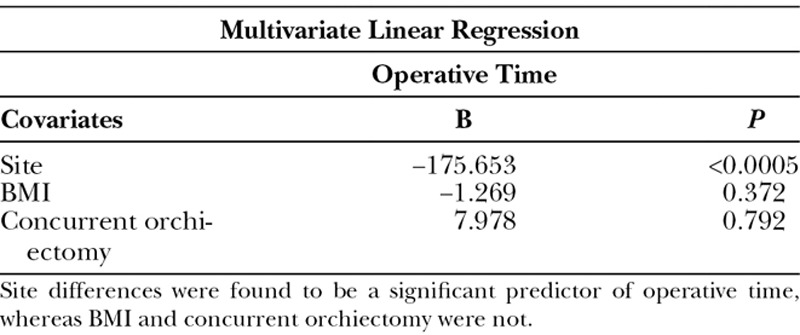
Differences in mean operative times between 2 sites were compared using an independent sample t test and were found to be statistically significant (P < 0.0005), with significantly longer operative times at site 1 versus site 2 (457 and 282 minutes, respectively). Predictors of increased operative time were analyzed using multivariate linear regression analysis (Table 2). The study site at which each procedure was performed was found to be the only significant predictor of the difference in operative time, after controlling for BMI and concurrent orchiectomy. Neither BMI nor orchiectomy was found to be significant predictors of operative time.
Table 2.
Multivariate Linear Regression Results Analyzing Site, BMI, and Concurrent Orchiectomy as Possible Predictors of Increased Operative Time
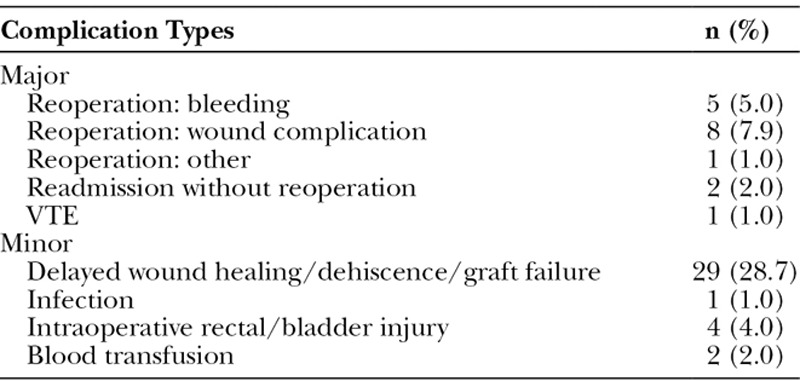
With regard to the outcome variables, 17 patients (16.8%) had major complications and 36 patients (35.6%) had minor complications. As these complications were not mutually exclusive, 53 patients (52.5%) experienced ≥1 major or minor complication following the procedure. Eleven patients (10.9%) required delayed revision urethroplasty for divergent urine stream (Table 3). The frequency of each particular type of complication is shown in Table 4.
Table 3.
Frequency of the Study Outcome Variables (Major Complications, Minor Complications, Any Complication, and Delayed Revision Urethroplasty) Overall and between Sites
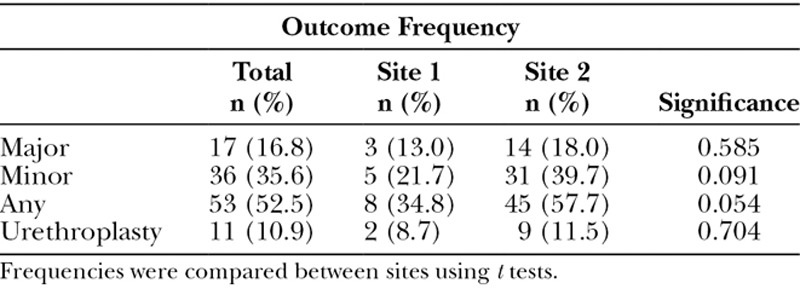
Table 4.
Overall Frequencies of Individual Types of Complications Categorized as Either Major or Minor Complications
On univariate logistic regression analysis, none of the recorded covariates were significant predictors of major, minor, or any complications in univariate analysis, or delayed revision urethroplasty for divergent urine stream (Table 5). Multivariate analysis was performed next using age, BMI, diabetes mellitus, and smoking history, as these covariates were most likely to have an impact on surgical complication rate. None of these covariates were found to have significant predictive value for on any of the 4 primary or secondary outcome variables (Table 6). In fact, mean BMI of patients who did experience a major, minor, or any complication was found to be lower than the mean BMI of patients who did not experience a major complication. This trend was not seen in 11 cases of delayed revision urethroplasty; the mean BMI of patients requiring urethroplasty was slightly larger (27.15) than the BMI of patients who did not (26.91), though this difference was not found to be statistically significant. Histograms of the relationship between BMI and major, minor, and any complication, as well as delayed revision urethroplasty, may be found in Figures 3–6, respectively.
Table 5.
Univariate Logistic Regression Results Evaluating BMI, Age, History of DM, and History of Smoking Independently as Possible Predictors of Major Complications, Minor Complications, Any Complication, and Delayed Revision Urethroplasty
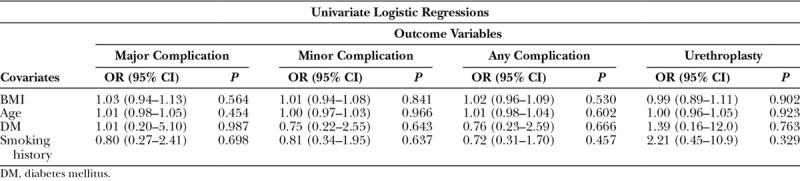
Table 6.
Multivariate Logistic Regression Results Evaluating BMI, Age, History of DM, and History of Smoking Together as Possible Predictors of Major Complications, Minor Complications, Any Complication, and Delayed Revision Urethroplasty
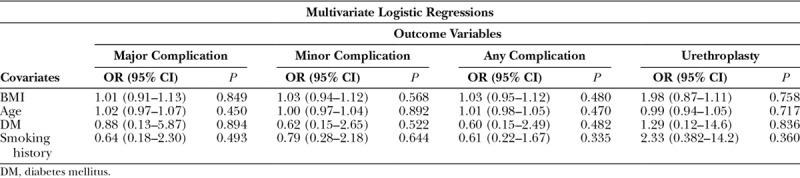
Fig. 3.
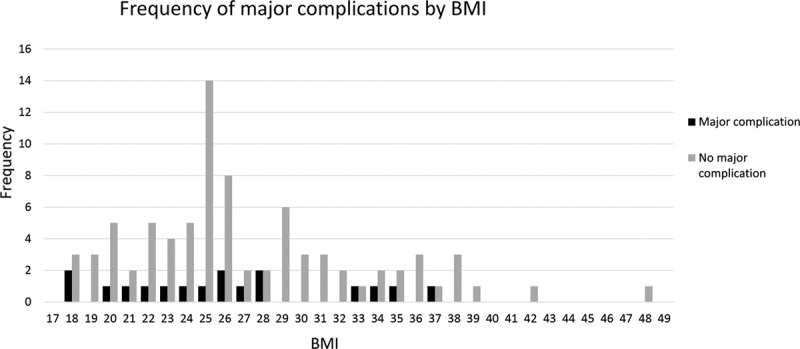
Histogram of the frequency of patients with major complications vs no major complications by BMI. Black columns indicate the number of patients within each BMI range who experienced a major complication, whereas gray columns indicate the number of patients who did not.
Fig. 6.
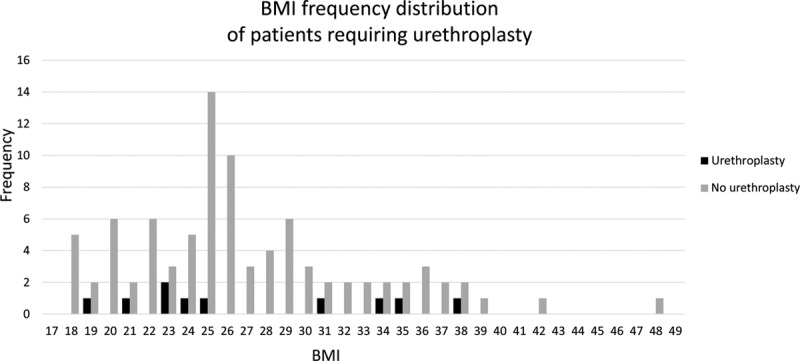
Histogram of the frequency of patients who required delayed revision urethroplasty by BMI. Black columns indicate the number of patients within each BMI range who required delayed revision urethroplasty following their PIV, whereas gray columns indicate the number of patients who did not.
Using these data, we performed a post hoc power analysis to determine the effect size at which the beta error of our conclusions would be <0.05. For total complications, this study was only powered to detect a very large increase in complication risk: 15% absolute increase in complication rate per 1 SD increase in mean BMI (mean 26.9 ± 6.0) with a beta of 0.031 (power = 0.969). For example, we can conclude that a patient with a BMI of 32.9 does not have >15% absolute increased risk of complications compared with a patient with a BMI of 26.9 (67.5% versus 52.5%). Most surgeons would consider a smaller increase in complication risk to be meaningful when considering risk stratifying patients for surgery; however, these data support our conclusion that GAS can safely be performed on otherwise carefully selected obese patients without a uniquely large effect of BMI on risk of complications in GAS when compared with other surgical procedures.
DISCUSSION
It has been demonstrated that obesity is associated with an increased risk of surgical complications across various surgical procedures, leading many surgeons and surgical centers to use absolute BMI cutoffs as exclusionary factors in gender-affirming PIV candidacy.13 In Medicare claims data, it has also been shown that transgender persons have increased medical comorbidities, including obesity, than cisgender persons.22 In the authors’ clinical experience, it is not uncommon for surgeons to implement a BMI cutoff of <30 or 35, which effectively precludes many patients from undergoing medically necessary surgical treatment of gender dysphoria. This common practice has recently been questioned by Gaither et al. and Buncamper et al. in single-center studies; neither of which identified elevated BMI as a predictor of postoperative complications. In this multicenter retrospective cohort, we contribute support to their findings that elevated BMI alone should not completely preclude transgender PIV patients from undergoing what is otherwise highly beneficial and life-changing surgery. GAS should be offered to obese transgender patients with the same selection criteria that are applied to patients for any other medically necessary surgical procedure, without a strict cutoff based on BMI alone. We acknowledge that operating on obese patients many pose additional challenges during a PIV procedure, such as higher blood loss in developing the prerectal space and lipectomy in the mons pubis area to remove fat deep to Scarpa’s fascia. Though these are issues that may surface during the procedure, the challenges can be easily met with skill and experience of any well-trained plastic surgeon. In our analysis, BMI was not a predictor of increased operating time.
Conditions associated with obesity, such as diabetes, were not shown to be significantly associated with increased complication rates (major, minor, or any) in our study. This mildly conflicts with findings of Buncamper et al., which suggest that diabetes is a predictor of delayed wound healing in gender-affirming PIV (a complication classified as a minor complication in our study).21 However, due to the relatively small sample size of our dataset, we did not perform logistic regression for any specific complications (such as delayed wound healing).
The University of Michigan and University of Miami do not use BMI cutoffs as an exclusionary factor for transgender PIV surgery, as evidenced by the range of BMI included in our sample (maximum BMI recorded = 48.2). We do, however, often recommend reasonable and healthy lifestyle modifications such as weight loss, exercise, and appropriate diabetes management, which may include specific hemoglobin A1c goals (reflective of general fitness guidelines for all surgeries23). Ideal preoperative conditions may be unobtainable for some patients, even despite their best efforts. Following a thorough discussion of the risks associated with deconditioned or poorly controlled diabetes, we work with each patient to set reasonable, safe, and personalized preoperative goals. Our results support the growing body of literature that suggests obese patients can safely undergo gender-affirming PIV procedures when experienced surgeons, proper medical clearance, and preoperative counseling criteria are met. Therefore, we offer that a more individualized model of surgical selection criteria can be employed to help facilitate increased access to gender-affirming PIV procedures.24
With regard to site differences, though we did not determine significant site differences in patient demographics or medical comorbidities, there was a significant difference found between operative times even after accounting for patient BMI and concurrent orchiectomy during the PIV procedure. We hypothesize that this variation between sites can be largely attributed to surgeon differences and minor deviations in operative technique. It does not seem that BMI itself plays a significant role in increasing operative time for this procedure.
Limitations of our study include the relatively small sample size; predominance of White patients in our sample population; the retrospective study design; and because patients sometimes travel significant distances to obtain gender-affirming PIV, the possibility that some complications may not have been treated and recorded in the study site’s medical record system. In addition, the very high complication rate reported in all series of gender-affirming PIV cases dictates that only factors with a large impact on complications will be significant in regression analysis. The relatively small sample size and therefore relatively low power of this study limits our abilities to definitively demonstrate the absence of any effect of BMI on complications following gender-affirming PIV. Rather, we accept that BMI may have some limited effect of the surgical outcomes of this procedure in the same way that it has been demonstrated to have a limited effect on the complication rates of all surgical procedures. We can, however, conclude that the effect of BMI on the complication rate of gender-affirming PIV is not uniquely large, and that it is safe to perform this procedure in otherwise surgically qualified patients with a high BMI. Furthermore, we acknowledge that patient satisfaction of cosmetic results was not specifically addressed in our study. Inclusion of patient-reported outcome measures, such as satisfaction with vaginal depth, was beyond the scope of this study. Inclusion of this qualitative data could help identify a surgeon’s intent to satisfy esthetic result in an addition to avoiding surgical complications. Overall, in our experience, we find that transgender patients undergoing GAS report the procedure to be highly beneficial with a strongly positive impact on their self-image and quality of life, regardless of their BMI.
CONCLUSIONS
Since the development of gender-affirming surgeries, transgender persons have faced stringent criteria for patient selection. Given the profound impact of this procedure both physically and psychologically, strict adherence to guidelines for surgical candidacy is most certainly warranted. Medical comorbidities must also be taken into consideration for any surgical procedure, including GAS. However, both our results and data from existing literature support the conclusion that BMI is not associated with a uniquely large increase in the rate of complications of gender-affirming PIV, and that GAS may be safely performed on carefully selected obese patients.
Fig. 4.
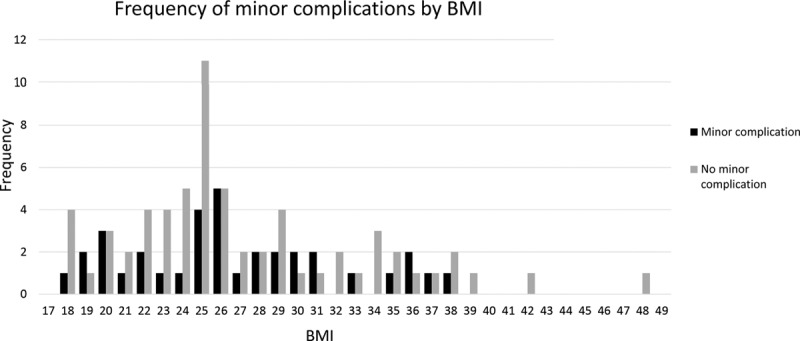
Histogram of the frequency of patients with minor complications vs no minor complications by BMI. Black columns indicate the number of patients within each BMI range who experienced a minor complication, whereas gray columns indicate the number of patients who did not.
Fig. 5.
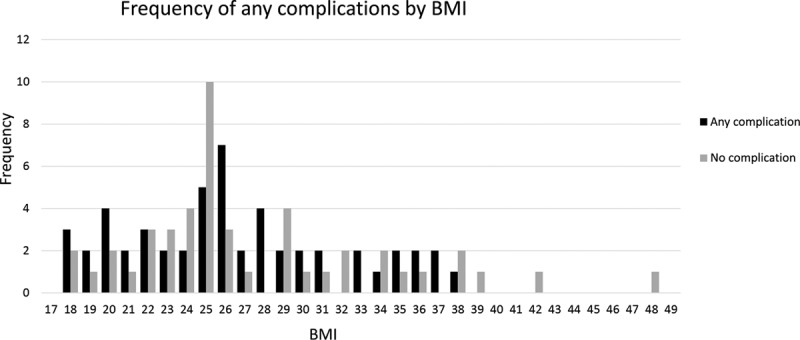
Histogram of the frequency of patients who experienced any complication vs no complications by BMI. Black columns indicate the number of patients within each BMI range who experienced any complication, whereas gray columns indicate the number of patients who experienced neither a major nor minor complication.
Footnotes
Published online 13 March 2019.
Disclosure: None of the authors has any financial conflict of interest related to the conclusions or subject matter of this work. None of the authors has a financial interest in any of the products, devices, or drugs mentioned in this manuscript.
REFERENCES
- 1.Davy Z. The DSM-5 and the politics of diagnosing transpeople. Arch Sex Behav. 2015;44:1165–1176. [DOI] [PubMed] [Google Scholar]
- 2.Schmidt L, Levine R. Psychological outcomes and reproductive issues among gender dysphoric individuals. Endocrinol Metab Clin North Am. 2015;44:773–785. [DOI] [PubMed] [Google Scholar]
- 3.Ainsworth TA, Spiegel JH. Quality of life of individuals with and without facial feminization surgery or gender reassignment surgery. Qual Life Res. 2010;19:1019–1024. [DOI] [PubMed] [Google Scholar]
- 4.Djordjevic ML, Salgado CJ, Bizic M, et al. Gender dysphoria: the role of sex reassignment surgery. Sci World J. 2014;2014:645109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Transcend Legal. Medical organization statements. Available at https://transcendlegal.org/medical organization-statements. Accessed March 19, 2018. [Google Scholar]
- 6.Human Rights Campaign. Finding insurance for transgender-related healthcare. Available at https://www.hrc.org/resources/finding-insurance-for-transgender-related-healthcare. Accessed March 19, 2018. [Google Scholar]
- 7.Roberts TK, Fantz CR. Barriers to quality health care for the transgender population. Clin Biochem. 2014;47:983–987. [DOI] [PubMed] [Google Scholar]
- 8.The World Professional Association for Transgender Health. Standards of care for the health of transsexual, transgender and gender nonconforming people. Available at https://s3.amazonaws.com/amo_hub_content/Association140/files/Standards%20of%20Care%20V7%20-%202011%20WPATH%20(2)(1).pdf. Accessed September 3, 2017. [Google Scholar]
- 9.World Health Organization. Obesity and overweight fact sheet. Available at http://www.who.int/mediacentre/factsheets/fs311/en/. Accessed September 3, 2017.
- 10.Pierpont YN, Dinh TP, Salas RE, et al. Obesity and surgical wound healing: a current review. ISRN Obes. 2014;2014:638936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Waisbren E, Rosen H, Bader AM, et al. Percent body fat and prediction of surgical site infection. J Am Coll Surg. 2010;210:381–389. [DOI] [PubMed] [Google Scholar]
- 12.Epstein NE. More risks and complications for elective spine surgery in morbidly obese patients. Surg Neurol Int. 2017;8:66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Goddard JC, Vickery RM, Qureshi A, et al. Feminizing genitoplasty in adult transsexuals: early and long-term surgical results. BJU Int. 2007;100:607–613. [DOI] [PubMed] [Google Scholar]
- 14.Hadj-Moussa M, Ohl DA, Kuzon WM. Feminizing genital gender-confirmation surgery. Sex Med Rev. 2018; in press [DOI] [PubMed] [Google Scholar]
- 15.Horbach SE, Bouman MB, Smit JM, et al. Outcome of vaginoplasty in male-to-female transgenders: a systematic review of surgical techniques. J Sex Med. 2015;12:1499–1512. [DOI] [PubMed] [Google Scholar]
- 16.Gaither TW, Awad MA, Osterberg EC, et al. Postoperative complications following primary penile inversion vaginoplasty among 330 male-to-female transgender patients. J Urol. 2017;17:717–18. [DOI] [PubMed] [Google Scholar]
- 17.Krege S, Bex A, Lümmen G, et al. Male-to-female transsexualism: a technique, results and long-term follow-up in 66 patients. BJU Int. 2001;88:396–402. [DOI] [PubMed] [Google Scholar]
- 18.Raigosa M, Avvedimento S, Yoon TS, et al. Male-to-female genital reassignment surgery: a retrospective review of surgical technique and complications in 60 patients. J Sex Med. 2015;12:1837–1845. [DOI] [PubMed] [Google Scholar]
- 19.Reed H. Aesthetic and functional genital and perineal surgery: male. Sem Plast Surg. 2011;25:177–178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sigurjonsson H, Rinder J, Möllermark C, et al. Male to female gender reassignment surgery: surgical outcomes of consecutive patients during 14 years. JPRAS Open. 2015;6:69–73. [Google Scholar]
- 21.Buncamper ME, van der Sluis WB, van der Pas RS, et al. Surgical outcome after penile inversion vaginoplasty: a retrospective study of 475 transgender women. Plast Reconstr Surg. 2016;138:999–1007. [DOI] [PubMed] [Google Scholar]
- 22.Dragon CN, Guerino P, Ewald E, et al. Transgender medicare beneficiaries and chronic conditions: exploring fee-for-service claims data. LGBT Health. 2017;4:404–411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Harrison B, Khansa I, Janis JE. Evidence-based strategies to reduce postoperative complications in plastic surgery. Plast Reconstr Surg. 2016;137:351–360. [DOI] [PubMed] [Google Scholar]
- 24.Fredriksen-Goldsen KI, Cook-Daniels L, Kim HJ, et al. Physical and mental health of transgender older adults: an at-risk and underserved population. Gerontologist 2014;54:488–500. [DOI] [PMC free article] [PubMed] [Google Scholar]


