Abstract
Background:
Two-staged implant-based reconstruction (IBR) is the most common breast reconstructive modality. Recently, technological and surgical advances have encouraged surgeons to revisit prepectoral IBR. Data comparing prepectoral against subpectoral IBR in women under the age of 40 are lacking.
Methods:
Retrospective chart review of patients under the age of 40 years old, who underwent immediate 2-staged IBR at our institution, was performed. Patient’s demographics, clinical characteristics, operative details, and early surgical outcomes of prepectoral and subpectoral reconstruction were compared. Data with values of P < 0.05 were considered statistically significant.
Results:
Between 2012 and 2016, 100 patients (187 breasts) who underwent prepectoral and 69 patients (124 breasts) who underwent subpectoral IBR were included. Median follow-up was 17.9 and 17.5 months in the prepectoral and subpectoral groups, respectively. Total number of complications including both stages of reconstruction was 20 (10.7%) and 19 (15.3%) in the prepectoral and subpectoral groups, respectively (P = 0.227). Specific complications, including hematoma, seroma, skin flap necrosis, wound dehiscence, and breast infections, were not significantly different among groups. Ten (5.4%) devices, including implants and tissue expander, required explantation in the prepectoral group and 8 (6.5%) in the subpectoral group (P = 0.683). Explantation was most commonly due to infection (n = 14), and all of them occurred during the first stage (P < 0.001).
Conclusions:
Early complications and implant explantation rates are comparable among prepectoral and subpectoral breast reconstruction in women under 40 years old. Based on these results, we believe that prepectoral IBR is a safe, reliable, and promising reconstructive option.
BACKGROUND
According to the American Cancer Society, 1 in 8 women will develop breast cancer over the course of their lifetime.1 Although the risk of developing breast cancer increases with age, 7% of all breast cancers are diagnosed under the age of 40.2 Management of this group of patients is challenging as they tend to have more aggressive cancers and recurrence rates, and more frequently require adjuvant radiation and chemotherapy.3–7 These patients also have high incidence of deleterious genetic mutations and fertility concerns.3,4 As a result, coordination with a multidisciplinary team is necessary in most patients and a coordinated plan of sequencing of interventions. Additionally, advances in screening protocols, genetic testing, and increased awareness have led to an increase in the number of patients undergoing risk-reducing mastectomies with subsequent reconstruction.8
Breast reconstruction has been shown to improve quality of life and social and psychological satisfaction of female patients undergoing mastectomy.9–12 Current data suggest that self-image and sexuality after mastectomy are more negatively affected in this young population.13 Furthermore, younger patients are also more likely to choose implant-based reconstruction (IBR) than flap reconstruction due to concerns over abdominal wall morbidity, potential effect on future pregnancies, and the increased likelihood of undergoing a contralateral mastectomy.14–16
IBR remains the most common reconstructive approach among women undergoing mastectomy and has significantly evolved over the last 2 decades.17–20 Muscle coverage, whether total or partial, has been historically advocated as the preferred approach because it adds an additional layer of vascularized coverage to the implant.21–25 However, current practices have evolved toward prepectoral implant reconstruction as it reduces animation deformity, pain, and muscle spasms, compared with the subpectoral approach, while maintaining optimal esthetic results.26–31 The prepectoral approach has evolved with introduction of newer generations of tissue expanders (TEs), implants, acellular dermal matrices (ADMs), and intraoperative flap perfusion technology.32–36
There is paucity of breast reconstruction outcome studies specific to this group of young patients. Furthermore, comparative studies assessing outcomes of the prepectoral and subpectoral approaches are lacking.16,37,38 The aim of this study is to compare outcomes and complications between prepectoral and subpectoral IBR in women younger than 40 years old. To our knowledge, this is the first study to address this comparison in this young age group.
METHODS
A retrospective electronic chart review was performed to identify all consecutive patients who underwent Implant-Based Breast Reconstruction, from January 2012 to December 2016 at our institution. Patients between 18 and 40 years old, who underwent mastectomy and immediate 2-staged breast reconstruction at our institution, were included. Patients were excluded if they had planned autologous breast reconstruction, were lost to follow-up before completing definitive reconstruction, or did not consent to use of their medical records for research purposes. This study was approved by our institutional review board.
Patient demographics and characteristics were collected including age, body mass index, smoking status (current, prior, never), comorbidities, type of mastectomy (skin sparing, nipple sparing), intent of surgery (therapeutic or prophylactic), location of the TE/implant (subpectoral or prepectoral), use of ADM, and additional oncologic treatment (radiation and/or chemotherapy). Postoperative complications, including primary wound dehiscence, skin flap necrosis, seroma, hematoma, breast infection, and implant or TE explantation, were recorded. Primary wound dehiscence was defined as full-thickness wound separation ≥0.5 cm unrelated to proceeding complications. Skin flap necrosis was defined as full-thickness skin necrosis. Seroma and hematomas were defined as those who were symptomatic and required aspiration or evacuation in the operating room. Breast infection was defined using the Centers for Disease Control and Prevention criteria for surgical site infections.39 Implant and TE explantation were defined as device removal secondary to a complication.
Statistical Analysis
Categorical variables were reported as counts and percentages. Continuous data were evaluated by the Shapiro–Wilk test for normal distributions. Data with normal distribution were reported as means with SD, and comparisons were performed with the t test. Data with no normal distribution were presented as medians with interquartile ranges for the 25th–75th percentile, and comparisons were performed with the Mann–Whitney–Wilcoxon test. Categorical data were presented as a percentage and analyzed using the chi-square test, and for samples smaller than 5 data points, the Fisher exact test was used. A value of P < 0.05 was considered significant. Conditional logistic regression models were performed using JMP Pro 13 soft ware (JMP, Pro 13, SAS Institute Inc, Cary, NC, 1989-2019).
RESULTS
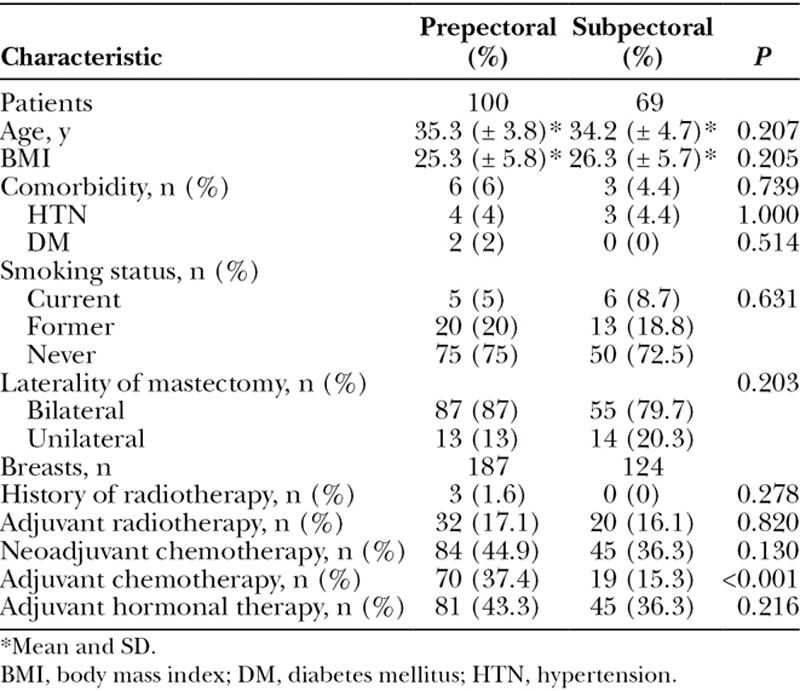
A total of 169 patients were identified, who met the inclusion criteria and make up the study population, which included 311 breasts. Patient’s demographics are summarized in Table 1. Of these, 100 patients (187 breasts) underwent prepectoral and 69 (124 breasts) underwent subpectoral reconstruction; all were 2-stage breast reconstructions. Patients who underwent prepectoral and subpectoral reconstruction were similar on almost all characteristics. The mean age was 35.3 (±3.8) in the prepectoral group and 34.2 (±4.7) in the subpectoral group (P = 0.207). Mean body mass index was 25.3 (±5.8) in the prepectoral group and 26.3 (±5.7) in the subpectoral group (P = 0.205). At the time of the surgery, 6 (6%) patients had comorbidities in the prepectoral group and 3 (4.4%) patients in the subpectoral group (P = 0.739). The majority of patients were nonsmokers, and prior breast radiation was rare in both groups. Five (5%) patients were active smokers in the prepectoral group, and 6 (8.7%) in the subpectoral group (P = 0.631). The majority of all procedures were bilateral, 87 (87%) in the prepectoral group and 55 (79.7%) in the subpectoral group (P = 0.203). Neoadjuvant chemotherapy was administered to 84 (44.9%) and 45 (36.3%) breasts in the prepectoral and subpectoral groups, respectively (P = 0.130). The only significant difference observed between the 2 groups was a higher use of adjuvant chemotherapy in the prepectoral group (37.4%) compared with the subpectoral group (15.3%; P < 0.001).
Table 1.
Patient’s Characteristics
Surgical Characteristics
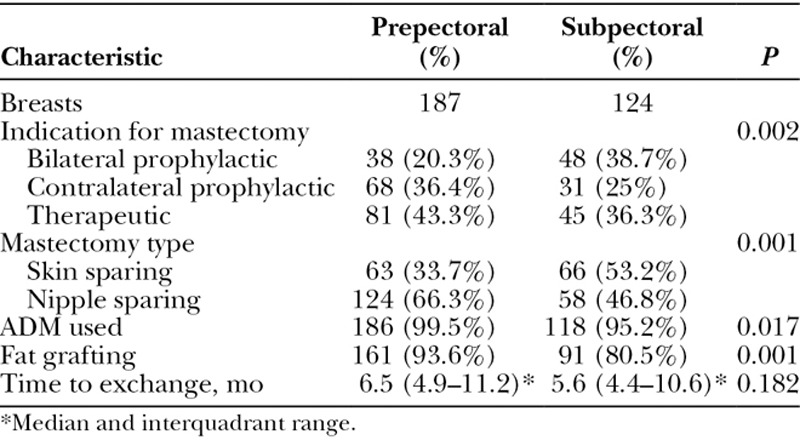
Surgical characteristics of the 2 groups showed several differences, as shown in Table 2. The following are reported per breast. Of all the mastectomies in the prepectoral group, 106 (56.7%) were done prophylactically; of these 68 (36.4%) were contralateral prophylactic mastectomies and 38 (20.3%) for high-risk patients. In the subpectoral group, 79 (63.7%) mastectomies were prophylactic; of these 31 (25%) were contralateral prophylactic mastectomies and 48 (38.7%) for high-risk patients. Therapeutic mastectomies were performed in 81 (43.3%) prepectoral and 45 (36.3%) subpectoral breasts (P = 0.002). Nipple-sparing mastectomies were performed in 124 (66.3%) breasts in the prepectoral group and 58 (46.8%) breasts in the subpectoral group (P = 0.001). ADM use was higher in the prepectoral group [186 (99.5%) prepectoral cases compared with 118 (95.2%) subpectoral breast reconstructions, respectively (P = 0.017)]. Autologous fat grafting during the second stage of reconstruction was performed more frequently in the prepectoral group [161 (93.6%) breasts in the prepectoral group and 91 (80.5%; P = 0.001) in the subpectoral group]. The median time between TE and implant exchange in the prepectoral group was 6.5 (4.9–11.2) months, and 5.6 (4.4–10.6) months in the subpectoral group (P = 0.182).
Table 2.
Surgical Characteristics
Surgical Outcomes and Complications
Median follow-up was similar; 17.9 (12.1–24.2) months in the prepectoral group, and 17.5 (9–28.9) months in the subpectoral group (P = 0.844). Table 3 summarizes the surgical outcomes and complications of both groups. Overall, complications occurred more frequently at the first stage (11.3%) compared with the second stage (1.3%; P < 0.001). The total number of complications including both stages of reconstruction did not vary between groups with 20 (10.7%) and 19 (15.3%) complications in the prepectoral and subpectoral groups, respectively (P = 0.227).
Table 3.
Surgical Complications and Outcomes
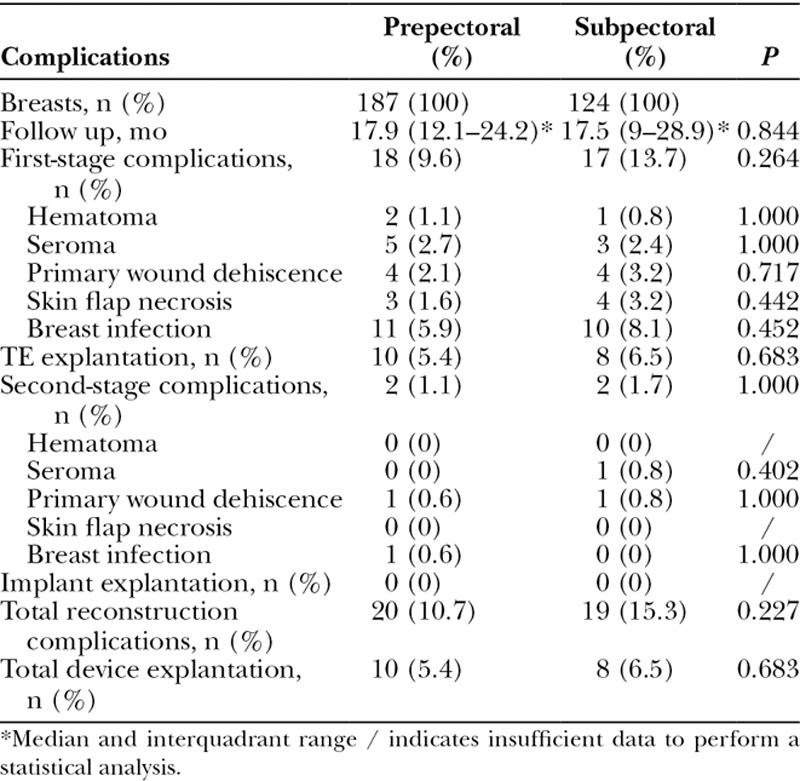
During first stage of breast reconstruction, the number of surgical complications was 18 (9.6%) in the prepectoral group and 17 (13.7%) in the subpectoral group (P = 0.264). Complications in the prepectoral and subpectoral groups included hematomas 2 (1.1%) and 1 (0.8%), respectively (P = 1.000); seromas 5 (2.7%) and 3 (2.4%), respectively (P = 1.000); primary wound dehiscence 4 (2.1%) and 4 (3.2%), respectively (P = 0.717); skin flap necrosis 3 (1.6%) and 4 (3.2%), respectively (P = 0.442); and infections 11 (5.9%) and 10 (8.1%), respectively (P = 0.452). There were 10 (5.4%) TEs explanted in the prepectoral group and 8 (6.5%) in the subpectoral group (P = 0.683). Of the 10 TEs explanted in the prepectoral group, 9 were secondary to infections and 1 was secondary to primary wound dehiscence. In the subpectoral group, 5 TEs were lost secondary to infections, 2 secondary to wound dehiscence, and 1 due to mastectomy flap necrosis.
After permanent implant placement, there were 2 (1.1%) surgical complications in the prepectoral group and 2 (1.7%) in the subpectoral group (P = 1.000). These complications, in the prepectoral and subpectoral groups, included seroma 0 (0%) and 1 (0.8%), respectively (P = 0.402); primary wound dehiscence 1 (0.6%) and 1 (0.8%), respectively (P = 1.000); and infections 1 (0.6%) and 0 (0%), respectively (P = 1.000). There were no cases of hematomas or skin flap necrosis, and no implants required explantation in either group.
DISCUSSION
This study evaluates the outcomes and complications of prepectoral and subpectoral IBRs in women younger than 40 years old. No significant difference was found in the total complication rate between the 2 groups (10.7% versus 15.3%, respectively; P = 0.227). In addition, total device explantation rate was comparable between the 2 groups. Our study also found no significant differences between the 2 groups in terms of specific complication rates, including hematoma, seroma, skin flap necrosis, primary wound dehiscence, and breast infections.
Young patients are typically more active and more likely to engage in physical activities which tend to exacerbate the risk for animation deformity, pain, and muscle spasms, which are associated with subpectoral implant placement.13,40,41 Although a few studies have discussed IBR in young patients, ours is the first to stratify results according to implant placement location.16,42 Prepectoral reconstruction has the advantage of sparing patients’ muscle-related complications, which can be especially beneficial in this younger higher risk population.26–29 Although concerns such as rippling and capsular contracture are potential feared complications of prepectoral reconstruction, in recent practice, this has been avoided with the introduction of ADM and fat grafting.34,35,43,44 In our study, 99.5% of patients who underwent prepectoral breast reconstruction had ADM placement, and 93.6% underwent subsequent fat grafting during the second stage of reconstruction.
Prepectoral breast reconstruction is an emerging technique whereby the implant is placed above the pectoralis major muscle.45 In a literature review of prepectoral implant-based breast reconstruction, including 14 articles and 654 breasts with mean age of 51, Chatterjee et al.46 reported complication rates of skin flap necrosis (7.8%), seroma (6.7%), and explantation of prosthesis (4.6%). This is comparable to our prepectoral implants results: 1.6% necrosis, 2.7% seroma, and 5.4% explantation. When a meta-analysis was performed on 4 of these studies comparing 219 prepectoral and 408 dual-plane implants, the authors found no significant difference in the complication rates.46 Nahabedian and Cocilovo38 compared the outcomes of 39 prepectoral implants and 50 partial subpectoral implants with a mean follow-up of 8.7 months and reported total complication rates of 20.5% and 22%, respectively. The prepectoral versus subpectoral infection rates were 8.1% and 4.8%, seroma rates 4.8% and 2.4%, and device explantation rates were 6.5% and 7.2%, respectively. Walia et al.47 and Bettinger et al.48 reported complication rates similar to ours in patients of all ages undergoing prepectoral IBR.
Few studies in the literature directly compared prepectoral and subpectoral breast reconstruction. In one study done in Manchester, Baker et al.49 compared short-term outcomes in 40 patients, and showed equivalent pain, early complications, and patient-reported outcomes. Furthermore, a study from Italy published in 2014 compared 34 subpectoral and 39 prepectoral immediate breasts reconstructions, in patients with no history of radiotherapy, smoking, or comorbidities, and reported very low complication rates.50 Last, a study from the University of California, San Francisco, published in 2017 showed similar results when comparing 84 prepectoral and 186 subpectoral breast reconstructions.51
Limitations and Recommendations
Although this is a large study and the first to report a comparison of subpectoral versus prepectoral IBR in a population under 40, it carries some limitations. This is a single institution retrospective review, and the decision of TE placement was up to the discretion of the treating plastic surgeon. Although we could not identify any significant difference in the demographics of the 2 populations, there is likely inherent selection bias in the placement choice. Our study was limited to reporting complications, and thus, important issues of costs and cosmetic outcomes were not addressed. We report similar short-term complications with a prepectoral approach; unfortunately, we do not have long-term follow-up and thus cannot report on capsular contracture, ptosis, and long-term cosmetic outcomes. The first stage of IBR inherently carries a higher risk for complications and patients should be followed with caution for early identification and management of complications, to improve the final outcome. Further high-quality multicenter prospective studies with longer follow-up are necessary to provide convincing evidence of superiority of one approach over the other.
CONCLUSIONS
Early surgical complications are comparable among prepectoral and subpectoral breast reconstruction in women under 40 years old. Based on these results, we believe that the prepectoral approach is reproducible and safe in this population. However, longer follow-up studies are necessary to analyze long-term results. Our study provides additional support to the available literature and further suggests the viability and safety of prepectoral IBR for younger patients with breast cancer.
Footnotes
Published online 13 March 2019.
Disclosure: Dr. Jacobson is a consultant for Allergan, Inc. None of the other authors has any financial disclosures.
REFERENCES
- 1.American Cancer Society. Breast Cancer Facts & Figures 2017–2018. 2017–2018American Cancer Society. [Google Scholar]
- 2.Anders CK, Johnson R, Litton J, et al. Breast cancer before age 40 years. Semin Oncol. 2009;36:237–249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Samphao S, Wheeler AJ, Rafferty E, et al. Diagnosis of breast cancer in women age 40 and younger: delays in diagnosis result from underuse of genetic testing and breast imaging. Am J Surg. 2009;198:538–543. [DOI] [PubMed] [Google Scholar]
- 4.Peppercorn J. Breast cancer in women under 40. Oncology (Williston Park). 2009;23:465–474. [PubMed] [Google Scholar]
- 5.Anders CK, Hsu DS, Broadwater G, et al. Young age at diagnosis correlates with worse prognosis and defines a subset of breast cancers with shared patterns of gene expression. J Clin Oncol. 2008;26:3324–3330. [DOI] [PubMed] [Google Scholar]
- 6.Carey LA, Perou CM, Livasy CA, et al. Race, breast cancer subtypes, and survival in the Carolina Breast Cancer Study. JAMA. 2006;295:2492–2502. [DOI] [PubMed] [Google Scholar]
- 7.Gajdos C, Tartter PI, Bleiweiss IJ, et al. Stage 0 to stage III breast cancer in young women. J Am Coll Surg. 2000;190:523–529. [DOI] [PubMed] [Google Scholar]
- 8.Kummerow KL, Du L, Penson DF, et al. Nationwide trends in mastectomy for early-stage breast cancer. JAMA Surg. 2015;150:9–16. [DOI] [PubMed] [Google Scholar]
- 9.McKenna RJ, Sr, Greene T, Hang-Fu LC, et al. Implications for clinical management in patients with breast cancer. Long-term effects of reconstruction surgery. Cancer. 1991;68(5 suppl):1182–1183. [DOI] [PubMed] [Google Scholar]
- 10.Santosa KB, Qi J, Kim HM, et al. Long-term patient-reported outcomes in postmastectomy breast reconstruction. JAMA Surg. 2018;153:891–899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mundy LR, Homa K, Klassen AF, et al. Breast cancer and reconstruction: normative data for interpreting the BREAST-Q. Plast Reconstr Surg. 2017;139:1046e–1055e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dean C, Chetty U, Forrest AP. Effects of immediate breast reconstruction on psychosocial morbidity after mastectomy. Lancet. 1983;1:459–462. [DOI] [PubMed] [Google Scholar]
- 13.Fobair P, Stewart SL, Chang S, et al. Body image and sexual problems in young women with breast cancer. Psychooncology. 2006;15:579–594. [DOI] [PubMed] [Google Scholar]
- 14.Fayanju OM, Stoll CR, Fowler S, et al. Contralateral prophylactic mastectomy after unilateral breast cancer: a systematic review and meta-analysis. Ann Surg. 2014;260:1000–1010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jones NB, Wilson J, Kotur L, et al. Contralateral prophylactic mastectomy for unilateral breast cancer: an increasing trend at a single institution. Ann Surg Oncol. 2009;16:2691–2696. [DOI] [PubMed] [Google Scholar]
- 16.Vogel JE, Chu C, McCullough M, et al. Breast cancer in women under age 40 years: treatment by total mastectomy and reconstruction. Ann Plast Surg. 2011;66:557–560. [DOI] [PubMed] [Google Scholar]
- 17.El-Sabawi B, Carey JN, Hagopian TM, et al. Radiation and breast reconstruction: algorithmic approach and evidence-based outcomes. J Surg Oncol. 2016;113:906–912. [DOI] [PubMed] [Google Scholar]
- 18.Ricci JA, Treiser MD, Tao R, et al. Predictors of complications and comparison of outcomes using SurgiMend fetal bovine and AlloDerm human cadaveric acellular dermal matrices in implant-based breast reconstruction. Plast Reconstr Surg. 2016;138:583e–591e. [DOI] [PubMed] [Google Scholar]
- 19.Cemal Y, Albornoz CR, Disa JJ, et al. A paradigm shift in U.S. breast reconstruction: part 2. The influence of changing mastectomy patterns on reconstructive rate and method. Plast Reconstr Surg. 2013;131:320e–326e. [DOI] [PubMed] [Google Scholar]
- 20.Albornoz CR, Bach PB, Mehrara BJ, et al. A paradigm shift in U.S. breast reconstruction: increasing implant rates. Plast Reconstr Surg. 2013;131:15–23. [DOI] [PubMed] [Google Scholar]
- 21.Nahabedian MY. Innovations and advancements with prosthetic breast reconstruction. Breast J. 2018;24:586–591. [DOI] [PubMed] [Google Scholar]
- 22.Barnea Y, Friedman O, Arad E, et al. An oncoplastic breast augmentation technique for immediate partial breast reconstruction following breast conservation. Plast Reconstr Surg. 2017;139:348e–357e. [DOI] [PubMed] [Google Scholar]
- 23.Salgarello M, Visconti G, Barone-Adesi L. Use of the subpectoral fascia flap for expander coverage in postmastectomy breast reconstruction. Plast Reconstr Surg. 2011;127:1010–1011; author reply 10111012. [DOI] [PubMed] [Google Scholar]
- 24.Banbury J, Yetman R, Lucas A, et al. Prospective analysis of the outcome of subpectoral breast augmentation: sensory changes, muscle function, and body image. Plast Reconstr Surg. 2004;113:701–707; discussion 708. [DOI] [PubMed] [Google Scholar]
- 25.Gruber RP, Kahn RA, Lash H, et al. Breast reconstruction following mastectomy: a comparison of submuscular and subcutaneous techniques. Plast Reconstr Surg. 1981;67:312–317. [DOI] [PubMed] [Google Scholar]
- 26.Sigalove S, Maxwell GP, Sigalove NM, et al. Prepectoral implant-based breast reconstruction: rationale, indications, and preliminary results. Plast Reconstr Surg. 2017;139:287–294. [DOI] [PubMed] [Google Scholar]
- 27.Salibian AA, Frey JD, Choi M, et al. Subcutaneous implant-based breast reconstruction with acellular dermal matrix/mesh: a systematic review. Plast Reconstr Surg Glob Open. 2016;4:e1139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gabriel A, Sigalove S, Sigalove NM, et al. Prepectoral revision breast reconstruction for treatment of implant-associated animation deformity: a review of 102 reconstructions. Aesthet Surg J. 2018;38:519–526. [DOI] [PubMed] [Google Scholar]
- 29.Hammond DC, Schmitt WP, O’Connor EA. Treatment of breast animation deformity in implant-based reconstruction with pocket change to the subcutaneous position. Plast Reconstr Surg. 2015;135:1540–1544. [DOI] [PubMed] [Google Scholar]
- 30.Harless C, Jacobson SR. Current strategies with 2-staged prosthetic breast reconstruction. Gland Surg. 2015;4:204–211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Woo A, Harless C, Jacobson SR. Revisiting an old place: single-surgeon experience on post-mastectomy subcutaneous implant-based breast reconstruction. Breast J. 2017;23:545–553. [DOI] [PubMed] [Google Scholar]
- 32.Brown MH, Shenker R, Silver SA. Cohesive silicone gel breast implants in aesthetic and reconstructive breast surgery. Plast Reconstr Surg. 2005;116:768–779; discussion 780. [DOI] [PubMed] [Google Scholar]
- 33.Kim SE, Jung DW, Chung KJ, et al. Immediate direct-to-implant breast reconstruction using anatomical implants. Arch Plast Surg. 2014;41:529–534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Spear SL, Parikh PM, Reisin E, et al. Acellular dermis-assisted breast reconstruction. Aesthetic Plast Surg. 2008;32:418–425. [DOI] [PubMed] [Google Scholar]
- 35.Clemens MW, Kronowitz SJ. Acellular dermal matrix in irradiated tissue expander/implant-based breast reconstruction: evidence-based review. Plast Reconstr Surg. 2012;130(5 suppl 2):27S–34S. [DOI] [PubMed] [Google Scholar]
- 36.Komorowska-Timek E, Gurtner GC. Intraoperative perfusion mapping with laser-assisted indocyanine green imaging can predict and prevent complications in immediate breast reconstruction. Plast Reconstr Surg. 2010;125:1065–1073. [DOI] [PubMed] [Google Scholar]
- 37.Zhu L, Mohan AT, Abdelsattar JM, et al. Comparison of subcutaneous versus submuscular expander placement in the first stage of immediate breast reconstruction. J Plast Reconstr Aesthet Surg. 2016;69:e77–e86. [DOI] [PubMed] [Google Scholar]
- 38.Nahabedian MY, Cocilovo C. Two-stage prosthetic breast reconstruction: a comparison between prepectoral and partial subpectoral techniques. Plast Reconstr Surg. 2017;140(6S Prepectoral Breast Reconstruction):22S–30S. [DOI] [PubMed] [Google Scholar]
- 39.Russo V, Watkins J. NHSN Surgical Site Infection Surveillance in 2018. 2018Center for Disease Control, CDC. [Google Scholar]
- 40.Ducic I, Seiboth LA, Iorio ML. Chronic postoperative breast pain: danger zones for nerve injuries. Plast Reconstr Surg. 2011;127:41–46. [DOI] [PubMed] [Google Scholar]
- 41.Spear SL, Schwartz J, Dayan JH, et al. Outcome assessment of breast distortion following submuscular breast augmentation. Aesthetic Plast Surg. 2009;33:44–48. [DOI] [PubMed] [Google Scholar]
- 42.Matsumoto WK, Munhoz AM, Okada A, et al. Influence of advanced age on postoperative outcomes and total loss following breast reconstruction: a critical assessment of 560 cases. Rev Col Bras Cir. 2018;45:e1616. [DOI] [PubMed] [Google Scholar]
- 43.Qureshi AA, Odom EB, Parikh RP, et al. Patient-reported outcomes of aesthetics and satisfaction in immediate breast reconstruction after nipple-sparing mastectomy with implants and fat grafting. Aesthet Surg J. 2017;37:999–1008. [DOI] [PubMed] [Google Scholar]
- 44.Spear SL, Coles CN, Leung BK, et al. The safety, effectiveness, and efficiency of autologous fat grafting in breast surgery. Plast Reconstr Surg Glob Open. 2016;4:e827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Highton L, Johnson R, Kirwan C, et al. Prepectoral implant-based breast reconstruction. Plast Reconstr Surg Glob Open. 2017;5:e1488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Chatterjee A, Nahabedian MY, Gabriel A, et al. Early assessment of post-surgical outcomes with pre-pectoral breast reconstruction: a literature review and meta-analysis. J Surg Oncol. 2018;117:1119–1130. [DOI] [PubMed] [Google Scholar]
- 47.Walia GS, Aston J, Bello R, et al. Prepectoral versus subpectoral tissue expander placement: a clinical and quality of life outcomes study. Plast Reconstr Surg Glob Open. 2018;6:e1731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Bettinger LN, Waters LM, Reese SW, et al. Comparative study of prepectoral and subpectoral expander-based breast reconstruction and Clavien IIIb score outcomes. Plast Reconstr Surg Glob Open. 2017;5:e1433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Baker BG, Irri R, MacCallum V, et al. A prospective comparison of short-term outcomes of subpectoral and prepectoral strattice-based immediate breast reconstruction. Plast Reconstr Surg. 2018;141:1077–1084. [DOI] [PubMed] [Google Scholar]
- 50.Casella D, Bernini M, Bencini L, et al. TiLoop® Bra mesh used for immediate breast reconstruction: comparison of retropectoral and subcutaneous implant placement in a prospective single-institution series. Eur J Plast Surg. 2014;37:599–604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Sbitany H, Piper M, Lentz R. Prepectoral breast reconstruction: a safe alternative to submuscular prosthetic reconstruction following nipple-sparing mastectomy. Plast Reconstr Surg. 2017;140:432–443. [DOI] [PubMed] [Google Scholar]


