Abstract
Objective
To outline an approach to assessing the risk of emergencies in one’s medical practice and determining the equipment and medications required for emergencies and the necessary staff training to meet this important facet of patient care.
Sources of information
The emergency preparedness recommendations presented in this article are based on data collected from family physicians’ current preparedness plans, formal physician evaluation and informal feedback provided after 2 large group presentations, and the authors’ expertise in areas including family medicine, emergency medicine, prehospital care, and pharmacology.
Main message
Delineating risk based on practice profile, location, and demographic characteristics will inform the development of an appropriate plan to meet both public expectations and professional obligations. Reviewing the plan or having a practice drill of the plan once developed will improve the process in the event of an emergency. It is also essential to have medication and equipment checked periodically for expiry dates and proper functioning.
Conclusion
Physicians will encounter office emergencies at some time in their practice. Appropriate risk assessment, planning, and preparedness will allow the provision of high-quality care, safety for staff members, the best patient outcomes, and the reward of having managed a time-sensitive problem in an efficient and effective manner.
The definition of emergency set forth by Geddes in 1970 was “anyone, anything, anytime.”1 By this definition, all physicians’ offices, private clinics, and walk-in clinics are at risk. In addition, there is an expectation that physicians will assist patients who present to their practices with emergencies, and a public expectation that emergencies that develop as complications of care, therapies, and procedures will be addressed. This public expectation is aligned with an obligation delineated by the Canadian Medical Protective Association that physicians must provide basic emergency care in addition to effectively managing foreseeable complications and emergencies from therapies and procedures provided to the practice population.2 The Canadian Medical Association’s code of ethics states that physicians must “provide whatever appropriate assistance [they] can to any person with an urgent need for medical care.”3
Reflection on how effectively and efficiently emergencies could be managed in any practice setting will identify gaps in preparedness and begin the process of needs assessment for the office. This article provides case-based guidance on lifesaving maneuvers and therapies for 3 examples of emergencies that could be encountered in family medicine.4,5
Case descriptions
Case 1. A 72-year-old man develops acute chest discomfort and associated intense diaphoresis in your office waiting room while waiting for a scheduled routine appointment. He is known to have hypertension and type 2 diabetes without a history of coronary artery disease.
Case 2. An 18-year-old man comes to your walk-in office for asthma that has been worse than normal for a few weeks. He smokes 15 cigarettes daily and has been trying to quit. He has been very short of breath for an hour and you are unable to hear breath sounds with auscultation of the left side of his chest. His trachea is shifted to the right side on clinical examination.
Case 3. You are excising a nevus from a 52-year-old woman’s arm. She begins to feel weak soon after you administer the local anesthetic. She then develops an urticarial rash, wheezing, and a feeling of impending doom.
Sources of information
The information presented in this article is largely based on peer-reviewed scientific literature and organizational resources.2,4–7 The emergency preparedness recommendations presented in this article are based on data collected from family physicians’ current office preparedness plans, physician formal evaluation and informal feedback provided after 2 large group presentations, and the authors’ expertise in areas including family medicine, emergency medicine, prehospital care, and pharmacology.
Main message
When assessing your practice for risk of emergencies, ask yourself the following reflective questions:
Are you and your staff prepared for emergencies?
Have you considered approaches to training staff members and ensuring you provide a good standard of care in such situations?
What are the risks specific to your practice?
Preparation, planning, and training will make the difference between a panicked response and a still-stressful but successful outcome. The following steps are required to effectively plan for such events:
review emergency situations encountered in the practice during the past year or longer;
develop a plan for these and for other common emergencies;
ensure the required equipment and medications are on site and up-to-date; and
carry out an exercise to establish roles and responsibilities.
The expectation is not that physicians will provide full-scope emergency care, but that basic first aid and reasonable processes for predictable emergency care will be in place to minimize patient risk.
Common office emergencies.
Emergencies might be caused by patients misinterpreting the urgency or severity of their medical condition and presenting to the office, or by side effects of treatment provided in the office. Emergencies sometimes encountered in office settings include cardiovascular incidents and, at the extreme, cardiac arrest.4,6 Another important group of emergencies includes common illnesses and conditions such as infectious diseases, environmental illnesses, respiratory ailments (predominantly asthma), and traumatic injuries.4 Other office emergencies include neurologic events, allergic reactions and anaphylaxis, diabetic distress, abdominal illnesses, back pain, enteric hemorrhages, vaginal bleeding and obstetric issues, and poisonings or toxic ingestions or exposures.4
Risk assessment.
Practice characteristics will determine the risk and types of emergencies likely to be encountered. Facets of a practice to consider include patient demographic characteristics, location, and procedures and therapies offered.
A review of incidents from the past few years, as well as the frequency of each type of incident, might provide useful information, if available. Box 1 presents factors in determining the risk of various events in your office.
Box 1. Suggestions for risk stratification in the office.
Patient demographic characteristics
Age range
Sex
Social status
Poverty
Rates of crime and addiction
Disease prevalence
Patient mobility
Office location and makeup
Office size and no. of staff members
Local supports
Inner-city location
Rural vs urban location
Time to emergency department
Transportation available
Nearby industry
Treatments and therapies provided
Vaccinations
Injectable medications
Obstetric services or intrauterine device insertion
Minor surgery
Allergy testing
Psychiatric treatment
Cosmetic procedures
Patient demographic characteristics: Demographic characteristics of both the population and the practice must be considered to effectively prepare for office emergencies. Consider age, employment status, and socioeconomic status; the prevalence of addiction, illness, and crime; and mobility perspectives, to list a few.
Location: Access to an emergency department might not be practically feasible for some members of the community, making the primary care practice their initial point of care in an emergency situation. Offices in rural locations must prepare for a longer emergency response time and longer prehospital treatment phase than those in urban settings, where prehospital response time is shorter. Other considerations regarding practice location include nearby industries, halfway houses, prisons, theme parks, and homes for troubled youth; other local resources that might help to inform the emergency plan can be consulted. In some areas, crime and addiction are prevalent and this should be considered in an emergency safety plan for patients and for staff members. If there is an elevator or another barrier to accessing the office, an evacuation plan for those with mobility issues should be outlined.
Procedures and therapies offered: The administration of parenteral medications as part of a practice increases the risk of allergy and anaphylaxis, bleeding, and other conditions such as syncope.
If minor procedures are part of the practice profile, preparation for emergencies must include consideration of potential complications. Procedures such as allergy testing or immunizations, therapeutic injections, phlebotomy, and minor therapeutic or surgical procedures should be included in the risk assessment. In this realm, appropriate planning is essential to effectively manage all emergencies resulting from these procedures until help has arrived.
Emergencies: the basics.
All staff members should have current first aid certification, current basic life support or cardiopulmonary resuscitation certification, and automatic external defibrillator training. Other aspects of the emergency response plan, such as preparedness and familiarity, will vary based on the practice population and nature and incidence of events and situations.
Overall approach.
In a clinical emergency situation, the first step is always assessment of the patient’s airway, breathing, and circulatory status followed by recording a complete set of vital signs including heart rate, blood pressure, respiratory rate, and glucose level. In the case of an unconscious patient, an automatic external defibrillator should be immediately applied, if available, to assess the cardiac rhythm and deliver a shock if appropriate. Medical assistance should be ongoing while a call is placed to 911, which provides access to emergency services anywhere in Canada and the United States. Emergency services cannot be accessed via text message. In Ontario, calling 911 also provides access to CritiCall, a provincial system that coordinates patient transfers to the appropriate level of care. In cases where these steps are to be carried out by the same person, the initial assessment and resuscitation might have to take place at the same time as the telephone call to emergency services, which should not be delayed.
After this, attention to patient privacy (crowd control) and assistance will be the main role for anyone in a position to help. If there is any question about the safety of others in the office, this is the time to guide patients and staff to a safe area.
A list of medications and equipment to be considered for the office setting is provided in Table 1. All items included in the plan must be kept current, and personnel will require periodic refresher training on administering medications and using equipment, as well as on emergency situation protocols, to avoid skill decline. It is also important to note that some medications, such as benzodiazepines and opioids, are controlled substances and will have to be properly stored in accordance with government guidelines.8 In general, these guidelines require that the substances are contained in a locked storage device that is secured to the building.8 This device must also be located within a secure room.
Table 1.
Equipment and medications to consider for the office emergency kit
| SETTING | EQUIPMENT OR CONSIDERATION | MEDICATION |
|---|---|---|
| Recommended for all settings |
|
|
| Suggested for some settings |
|
|
IO—intraosseous, IV—intravenous.
Managing the scene: The first steps to managing the scene are to acknowledge the emergency and assess for immediate safety risks. Then identify the team leader, usually the physician, and call 911. The next steps are protecting patient privacy, ensuring the safety of the staff members and other patients, and supporting the team leader. This support might include obtaining equipment or medications, organizing people, and documenting individuals and treatments or procedures. In larger offices with a greater number of staff members these tasks can be shared by several people.
Posters and reminder cards in easily visible locations for staff are helpful, as emergency situations are infrequent and stressful. The reminder cards should be easily accessible and reviewed periodically. Planning ahead to make this kind of support available will be appreciated when it is needed. For example, a poster on anaphylactic reactions7 can be downloaded through the Dalhousie Academic Detailing Service, an evidence-based physician education program.
Assessing the patient: Care required for emergencies will vary based on clinical presentation; however, all patients will require an assessment of their airway, breathing, and circulation. After this, all vital signs, including bedside glucose level, should be recorded. A focused history and examination to identify the details of the condition and initiation of appropriate therapy or management is sometimes all that is required to stabilize a patient for transport.
Patient privacy should be optimized. Sentinel events such as pain ratings, syncope or seizures, timing of medications given, and responses to therapies should be documented. Reassuring the patient and his or her family members is important, as is verbal communication of the immediate care plan. Family members or accompanying persons will also need to know if they can accompany the patient and, if not, to which facility the patient will be transported.
Treatment will be determined by the urgency of therapy required, the severity and lethality of the condition, and the time it will take for the patient to reach an emergency care centre or emergency department. In some situations, intravenous antimicrobials or fluids are indicated, while in others these can delay definitive care. Each case will be unique and clinicians must be comfortable making these decisions at the time of the event.
Transitioning care: Once the patient’s condition has stabilized, or after transfer of care to paramedics, the team leader should inform the emergency department staff of the patient’s condition for continuity of care. Ideally, a list of medications and the team’s documentation of the event should be copied to send with the patient or the paramedics.
Some patients will refuse to accept an ambulance transfer. If they are too sick to drive and pose a substantial and immediate risk to others, or you believe they lack capacity to make an informed decision, you have a duty to inform the police. Otherwise they must be fully informed of the risk of being driven to the emergency department in a private vehicle by a friend or family member, and this discussion must be clearly documented in the patient’s medical record along with the chronology of the incident. It is a good practice to inform patients who have been waiting that there has been an emergency and to apologize for the delay.
Transfer of care to emergency medical services: Many office emergencies require activating 911 services. In these cases, transfer of care will often occur between the office staff and the paramedics. As transfer of care is a high-risk situation for medical errors, it is important to communicate to the paramedics the nature of the emergency, the interventions provided, and your impression and plan. Any documentation available, including medical history, allergies, medications, and details regarding the emergency, should be provided at this time.
In Canada, the scope of practice of paramedics varies from basic to advanced life support (ALS) based on paramedic designation and training. Ensure the appropriate level of care is dispatched by communicating an approximate level of care that the patient has received and will require. This might avoid the transfer delays that ensue when a patient has received or requires a higher level of care than the responding paramedics are qualified to provide.
Interventions provided during transport to hospital might be limited if you work in a system that does not provide ALS prehospital care, or if an ALS-capable paramedic is not available. As these situations are more likely in rural areas with a long transport time to hospital, one option is to contact the on-call physician supporting the paramedics and work out a treatment plan the paramedics can then be authorized to provide. The paramedics on scene should be able to facilitate establishing this communication.
In rural areas involving management of critically ill patients or unexpected cases of substantial trauma, the use of prehospital air transport is often overlooked as an option. Early activation is important in these cases, as flight crews often need time for preflight procedures. Communication of this potential need to the dispatch centre at the onset of the emergency will allow flight crews this time, and a decision to launch will be made based on local protocol.
Considerations for violent or agitated patients.
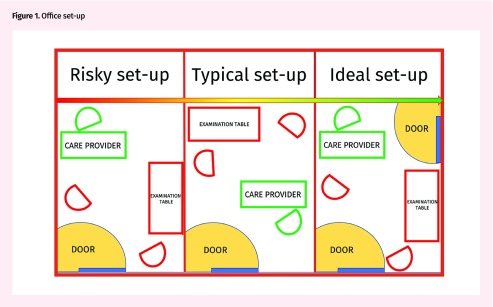
Occasionally, a patient will become upset or agitated. A plan must be in place to provide both help for the patient and an exit strategy for the physician. An examination room with an easy egress (doctor nearest to the door) should be available in all office settings (Figure 1). Staff members should be instructed to place patients in this room if they are agitated, have problematic substance use, or are angry.
Figure 1.
Office set-up
A concealed panic button can silently alert others that a health care provider requires aid and might be of use once a risk assessment has been completed or if a provider feels unsafe at any time. A brief interruption by others should be encouraged when there are loud voices or disruptive sounds from any area in the office.
Staff should agree on a code word that can be used in different phrases to indicate that all is fine, that help is required, or that the authorities must be called immediately. Code words should be clear (eg, the list) and should be used in a context that articulates the health care provider’s need: “please call for the list right now” means “call the police straight away”; “please bring the list” means “your assistance is required now”; or “please don’t worry about the list” means “everything is fine and the situation is a flare of temper and poses no danger to anyone.” These statements might be accompanied by others, such as “everything is fine,” aimed at keeping the patient as calm as possible. The code word must be rehearsed and repeated often and actively listened for by office staff in potentially dangerous situations. Examples of phrases using a code word are provided in Table 2.
Table 2.
Suggested phrasing for code words: Examples using code word the list.
| SITUATION | EXAMPLE OF PHRASING |
|---|---|
| Urgent: call police now |
|
| Urgent assistance required: help |
|
| Everything is fine: do not worry |
|
| Please check back in 5 min |
|
Removing other patients and staff from the area might be indicated in some situations for privacy or safety reasons. When a call is placed to the authorities for assistance, other patients, families, and staff members should be moved from the immediate area.
Although clinicians and staff might be frightened, remaining calm is crucial to getting control of the situation. Approach these situations delicately and empathize with the patient about his or her feelings or anger, offer the patient medication to help him or her calm down, and remind the patient that there is support and help available and that the staff want to do what is best for him or her. Often there will be no opportunity to collect a detailed history, and performing a physical examination might place providers at increased risk and should be deferred. Documentation and alerting the emergency department should also be deferred until help has arrived.
Case resolutions
With the risk checklist reviewed, the medication and equipment lists considered, and plans for emergency presentation in the office in mind, we revisit our cases in Table 3 and explore what care we will be able to provide for these patients.9–13
Table 3.
Revisiting the cases
| CASE | SUGGESTED PLAN OF ACTION | |
|---|---|---|
|
| ||
| MINIMUM ACTION | MAXIMUM ACTION | |
| Case 1: 72-year-old man with acute chest discomfort and associated intense diaphoresis; known hypertension and type 2 diabetes; no coronary artery disease |
|
|
| Case 2: 18-year-old man with asthma that has been worse than normal for a few weeks; smokes 15 cigarettes per day and has been trying to quit; and has been very short of breath for 1 h. You are unable to hear breath sounds with auscultation of the left side of his chest. His trachea is shifted to the right side |
|
|
| Case 3: 52-year-old woman feels weak when you administer a local anesthetic; develops an urticarial rash, wheezing, and a feeling of impending doom |
|
|
IO—intraosseous, IV—intravenous.
Conclusion
Physicians will all encounter emergencies at their place of work at some time. Appropriate risk assessment, planning, and preparedness will allow the provision of high-quality care, safety for staff members, the best patient outcomes, and the reward of having managed a time-sensitive problem in an efficient and effective manner.
Editor’s key points
▸ Physicians have a legal, moral, and ethical obligation to provide basic emergency care to patients who present to their practices, in addition to managing foreseeable complications and emergencies from therapies and procedures they provide. These events are rare; however, all medical practices require some emergency preparedness.
▸ To prepare for emergencies, review an inventory of past incidents, your practice pattern, and the social and demographic factors that will delineate the risk of certain types of emergencies in your practice. Consider the types of emergencies you are most likely to see in your office in particular and include these in your plan.
▸ To prepare for commonly encountered situations, set up an emergency kit including medications and equipment, and place posters or reminder cards in the office where they can be easily found; assign a person to check that the kit is up-to-date every month. To help manage patients who become agitated or violent, set up the office to allow easy egress. Allow staff to enter the office, overriding patient privacy, should there be raised voices or loud noises from within. Designate code words to alert staff of the severity of a situation.
Footnotes
Contributors
All authors contributed to the literature review and interpretation, and to preparing the manuscript for submission.
Competing interests
None declared
This article is eligible for Mainpro+ certified Self-Learning credits. To earn credits, go to www.cfp.ca and click on the Mainpro+ link.
This article has been peer reviewed.
La traduction en français de cet article se trouve à www.cfp.ca dans la table des matières du numéro d’avril 2019 à la page e132.
References
- 1.The direct and indirect measurement of blood pressure: by L. A. Geddes, M.E., Ph.D., Chicago, 1970, Year Book Medical Publishers, Inc., 196 pages. Price $11.00 [book review] Am Heart J. 1970;80(3):435–6. [Google Scholar]
- 2.Canadian Medical Protective Association . Preparing for a medical emergency—anticipating the unexpected in an office or clinic. Ottawa, ON: Canadian Medical Protective Association; 2013. Available from: www.cmpa-acpm.ca/en/advice-publications/browse-articles/2013/preparing-for-a-medical-emergency-anticipating-the-unexpected-in-an-office-or-clinic. Accessed 2019 Feb 14. [Google Scholar]
- 3.Canadian Medical Association . CMA code of ethics. Ottawa, ON: Canadian Medical Association; 2004. Available from: www.cma.ca/Assets/assets-library/document/en/advocacy/policy-research/CMA_Policy_Code_of_ethics_of_the_Canadian_Medical_Association_Update_2004_PD04-06-e.pdf. Accessed 2019 Feb 14. [Google Scholar]
- 4.Liddy C, Dreise H, Gaboury I. Frequency of in-office emergencies in primary care. Can Fam Physician. 2009;55:1004–5.e1-4. Available from: www.cfp.ca/content/cfp/55/10/1004.full.pdf. Accessed 2019 Feb 13. [PMC free article] [PubMed] [Google Scholar]
- 5.Johnston CL, Coulthard MG, Schluter PJ, Dick ML. Medical emergencies in general practice in south-east Queensland: prevalence and practice preparedness. Med J Aust. 2001;175(2):99–103. doi: 10.5694/j.1326-5377.2001.tb143540.x. [DOI] [PubMed] [Google Scholar]
- 6.Toback SL. Medical emergency preparedness in office practice. Am Fam Physician. 2007;75(11):1679–84. [PubMed] [Google Scholar]
- 7.Dalhousie Academic Detailing Service . Anaphylactic reaction? Highly likely if any of the following criteria are met. Halifax, NS: Dalhousie University; 2017. Available from: https://cdn.dal.ca/content/dam/dalhousie/pdf/faculty/medicine/departments/core-units/cpd/GP%20Anaphylaxis%20handout.pdf. Accessed 2019 Feb 14. [Google Scholar]
- 8.Office of Controlled Substances Therapeutic Products Programme . Directive on physical security requirements for controlled substances (security requirements for licensed dealers for the storage of controlled substances) Ottawa, ON: Health Canada; 1999. Available from: www.canada.ca/en/health-canada/services/health-concerns/reports-publications/controlled-substances-precursor-chemicals/directive-physical-security-requirements-controlled-substances-licensed-dealers-security-requirements-storage.html. Accessed 2018 Jun 1. [Google Scholar]
- 9.CredibleMeds . Resources for healthcare professionals. Oro Valley, AZ: CredibleMeds; 2013. Available from: https://crediblemeds.org/healthcare-providers. Accessed 2018 Jun 1. [Google Scholar]
- 10.Van de Werf F, Bax J, Betriu A, Blomstrom-Lundqvist C, Crea F, Falk V, et al. Management of acute myocardial infarction in patients presenting with persistent ST-segment elevation: the Task Force on the Management of ST-Segment Elevation Acute Myocardial Infarction of the European Society of Cardiology. Eur Heart J. 2008;29(23):2909–45. doi: 10.1093/eurheartj/ehn416. Epub 2008 Nov 12. [DOI] [PubMed] [Google Scholar]
- 11.Trauma Pro How to: needle decompression of the chest [video] 2010. YouTube; Available from: www.youtube.com/watch?v=UvHJ4pjNh2Q&t=74s. Accessed 2018 Aug 21.
- 12.Pumphrey RS. Lessons for management of anaphylaxis from a study of fatal reactions. Clin Exp Allergy. 2000;30(8):1144–50. doi: 10.1046/j.1365-2222.2000.00864.x. [DOI] [PubMed] [Google Scholar]
- 13.Simons KJ, Simons FE. Epinephrine and its use in anaphylaxis: current issues. Curr Opin Allergy Clin Immunol. 2010;10(4):354–61. doi: 10.1097/ACI.0b013e32833bc670. [DOI] [PubMed] [Google Scholar]