Abstract
Faced with a critical shortage of physicians in Africa, which hampered the efforts of the U.S. President’s Emergency Plan for AIDS Relief (PEPFAR), the Medical Education Partnership Initiative (MEPI) was established in 2010 to increase the number of medical graduates, the quality of their education, and their retention in Africa. To summarize the accomplishments of the initiative, lessons learned, and remaining challenges, the authors conducted a narrative review of MEPI—from the perspectives of the U.S. government funding agencies and implementing agencies—by reviewing reports from grantee institutions and conducting a search of scientific publications about MEPI. African institutions received 11 programmatic grants, totaling $100 million in PEPFAR funds, to implement MEPI from 2010 to 2015. The National Institutes of Health (NIH) provided an additional 8 linked and pilot grants, totaling $30 million, to strengthen medical research capacity. The 13 grant recipients (in 12 countries) partnered with dozens of additional government and academic institutions, including many in the United States, forming a robust community of practice in medical education and research. Interventions included increasing the number of medical school enrollees, revising curricula, recruiting new faculty, enhancing faculty development, expanding the use of clinical skills laboratories and community and rural training sites, strengthening computer and telecommunications capacity, and increasing e-learning. Research capacity and productivity increased through training and support. Additional support from NIH for faculty development, and from PEPFAR for health professions education and research, is sustaining and extending MEPI’s transformative effect on medical education in select African sites.
The shortage of health care workers, especially physicians, in sub-Saharan Africa is critical. According to the World Health Organization, that region had only 0.3 physicians per 1,000 population in 2013.1 In contrast, there were 3.2 physicians per 1,000 population in Europe and 1.4 per 1,000 worldwide.1 The 225,120 physicians in sub-Saharan Africa in 2013 represent just a fraction of the estimated current need for 867,876.2 Significant shortcomings in medical education compound the overall shortage. The sub-Saharan African Medical Schools Study, published in 2011, documented pervasive faculty shortages in basic and clinical sciences, poor physical and communications infrastructure, inadequate linkages with other medical research and education centers in Africa and abroad, and little use of external accreditation.2
The U.S. President’s Emergency Plan for AIDS Relief (PEPFAR) began in 2003 to alleviate the global epidemic of HIV infection and AIDS. By 2011, 3.9 million people had begun lifesaving antiretroviral treatment with PEPFAR support3; nonetheless, limitations in the number of health workers and the quality of their education were among the greatest constraints in achieving and extending these accomplishments, especially in sub-Saharan Africa where the burden of HIV infection and AIDS was the highest. To address this challenge, the first PEPFAR reauthorization in 2008 included a congressional mandate to train 140,000 new health care workers, including doctors, nurses, and other allied health professionals.4
In 2010, PEPFAR partnered with the U.S. National Institutes of Health (NIH) and the U.S. Health Resources and Services Administration (HRSA) to establish the Medical Education Partnership Initiative (MEPI) to substantially support medical education at select medical schools in sub-Saharan Africa to boost the quantity of medical graduates, the quality of their education, and their retention where they are most needed—all while providing or enhancing research capabilities and ensuring sustainability.5,6 HRSA and NIH announced the first MEPI grants in October 2010 and invested a total of $130 million over five years (2010–2015) to directly support medical schools in 12 sub-Saharan African countries.
Here, we describe the implementation, accomplishments, and effect of this first phase of MEPI and its related activities. We also explain some of the challenges, limitations, and lessons for future initiatives to support health professions education in sub-Saharan Africa, including considerations of the scale and time frame needed to effect significant, positive, population-wide changes in health outcomes.
Information Sources
This article represents a qualitative, narrative review of the first phase of MEPI implementation (2010–2015) and related activities. As mentioned, we have focused on the main objectives, accomplishments, critical success factors, and lessons learned. Our primary data sources for this article included the reports from the MEPI implementation sites, periodic programmatic summary documents, and the five-year summary report prepared by the MEPI grant recipient principal investigators (PIs).7
These sources provided information derived from a detailed monitoring framework established at the inception of MEPI. The framework included 161 quantitative indicators, such as the number of medical school graduates per year, and 42 qualitative indicators, such as descriptions of how MEPI helped increase the number of medical school graduates. Monitors conducted annual surveys and site visits, and PIs prepared annual school summary reports. The final survey was conducted in August 2015, so additional accomplishments accrued after the last survey and may not be reflected in this article.
Our article reflects our experiences—conducting site visits and holding discussions with MEPI PIs and implementation partners—as program officers, technical staff, and leaders for MEPI funding organizations. Our article also includes select findings from 58 articles (2010–2017) related to MEPI (which we discovered through an April 2017 PubMed search using the key words “MEPI” and “Medical Education Partnership Initiative”).
MEPI Funding and Grants
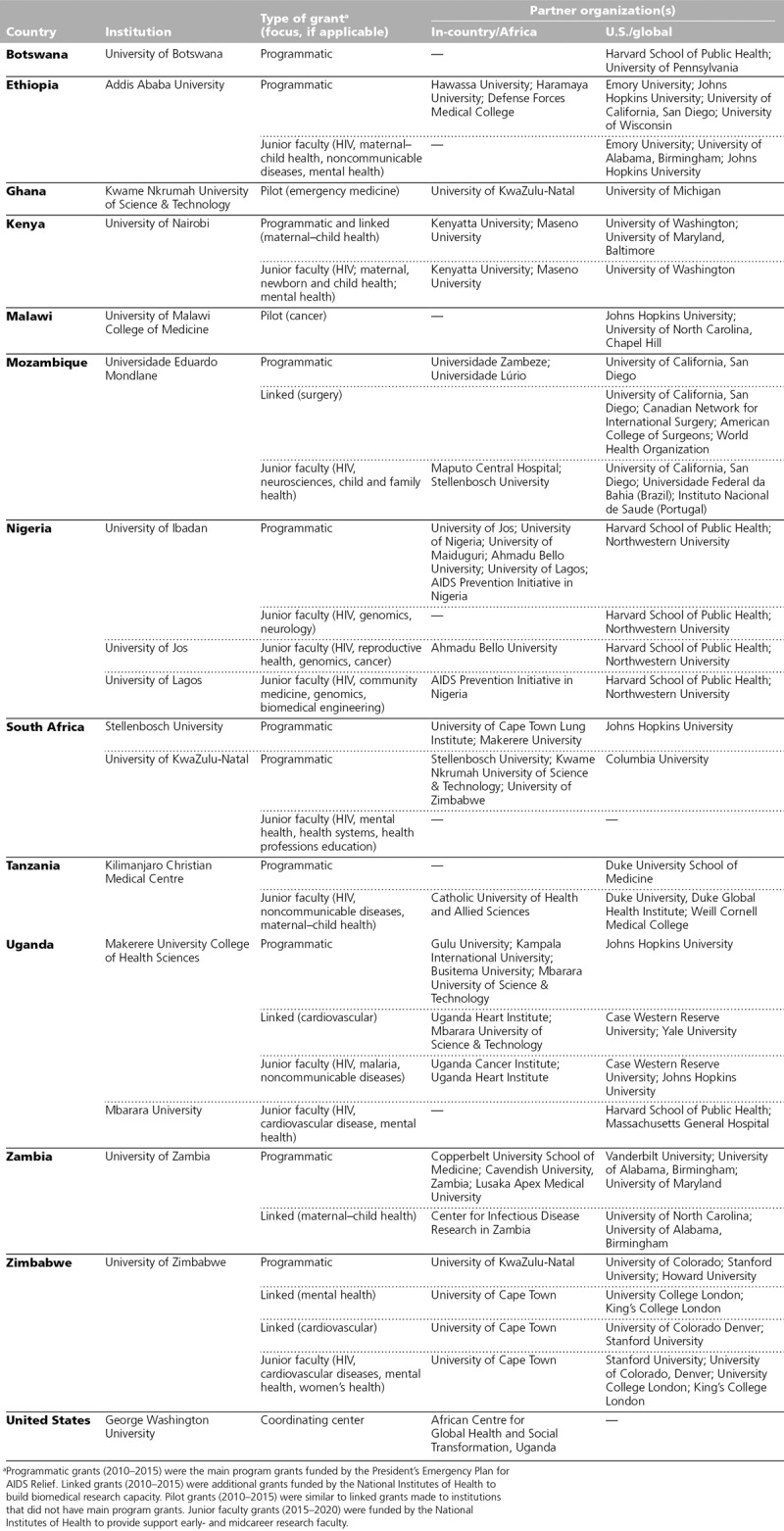
PEPFAR, which is administered by the Office of the Global AIDS Coordinator in the U.S. Department of State, funded the MEPI programmatic grants in 2010, providing $100 million over a five-year period through 11 grants to 11 institutions in 10 countries (Appendix 1). Two HHS agencies were designated to administer MEPI based on their respective competencies. The Fogarty International Center (FIC) at NIH supported 7 of the grants, while HRSA’s HIV/AIDS Bureau managed the other 4. FIC, which facilitates global health research conducted by NIH, had been increasingly engaged with African medical research and educational institutions since the inception of the AIDS International Training and Research Program in the late 1980s.8 HRSA, which largely focuses on improving access to and quality of care in the United States, had been increasingly engaged in Africa overseeing HIV/AIDS program implementation since the inception of PEPFAR. Concurrent with MEPI, HRSA had the lead role in implementing the companion PEPFAR-funded Nursing Education Partnership Initiative.6 In addition to the 11 programmatic grants awarded to African institutions, HRSA also provided funding to a U.S.-based coordinating center (George Washington University [GWU]) to facilitate and monitor MEPI; this funding was administered by HRSA through a cooperative agreement.
In addition, the NIH Common Fund and seven other NIH institutes, centers, and offices (ICOs; see List 1) provided $30 million over a five-year period beginning in 2010 to build biomedical research capacity. With these funds, FIC administered an additional 6 linked grants in five of the countries with MEPI programmatic grants, plus 2 pilot grants in two countries that did not have MEPI programmatic grants, increasing the total number of MEPI grantee institutions to 13.
In sum, in the first phase of MEPI described herein, NIH awarded 19 foreign grants (totaling $130 million) to 13 institutions in 12 countries (Appendix 1). The funding amounts for the programmatic grants ranged from a total of $8.6 to $9.3 million per institution over the five-year implementation period, while the funding amounts for the linked and pilot grants ranged from a total of $1.9 to $2.5 million per institution over five years.
The grants resulted in a large number of substantive national, regional, and global partnerships, including many with U.S. universities. In addition, many of the PIs formed collaborative networks in their countries with other universities and with ministries of health and education that did not receive MEPI funds (see Appendix 1).
Coordination of MEPI
The U.S.-based MEPI coordinating center at GWU and its Uganda-based counterpart, the African Centre for Global Health and Social Transformation (ACHEST), supported the MEPI institutions by providing technical assistance, developing capacity in medical education research, supporting and coordinating the monitoring and evaluation of MEPI-funded programs and activities, organizing annual meetings, and fostering collaboration. According to site visit reports and survey results, GWU and ACHEST facilitated the formation of technical working groups in, initially, six areas: e-learning, physician tracking, medical education research, community-based medical education, competency-based medical education, and research support centers. Later working groups focused on monitoring and evaluation and on library information science. Within these eight areas, MEPI institutions established their own priorities and implemented their own plans to meet the MEPI goals in alignment with national policies and needs (Table 1).9
Table 1.
Key Interventions and Examples Thereof Funded by the Medical Education Partnership Initiative (MEPI)a

The PIs of the programmatic grants (n = 11), the PIs of the linked and pilot grants (n = 8), and the coordinating center came together in 2011 to form the MEPI PI Council. This council served as a leadership group for MEPI, provided a coordinated channel of communication among grantees and funding organizations, and established common policies for publication and partnership agreements. The MEPI PI Council selected from among its membership a chair and a vice chair. Each chair and vice chair served for a one-year term, and the vice chair assumed the role of chair the following year. The MEPI PI Council met biannually at varying MEPI host institutions, including in an annual symposium organized to foster collaboration and share best practices and lessons learned in medical education and research. The MEPI PI Council further supported collaboration and communication by encouraging PIs to visit other schools as members of site visit teams. The annual symposium evolved into a major meeting on medical education and research in Africa with more than 250 participants from MEPI-funded programs, academia, governments, and national and international partner agencies.
In the third year of MEPI, much of the coordination role was transitioned to ACHEST and the MEPI PI Council as a result of their demonstrated capacity; GWU continued to support networking by hosting webinars, maintaining the MEPI website, and publishing and distributing newsletters.
Increasing the Quantity and Quality of Doctors and Other Health Professionals
To increase the number of medical graduates, MEPI institutions employed a variety of strategies, such as increasing the number of enrollees, using new pedagogical methods, expanding teaching facilities, collaborating with other medical schools, and supporting the launch of new medical schools in their respective countries. For example, enrollment in internal medicine more than doubled in Zimbabwe and in Mozambique from an average of 10 students per year prior to MEPI to 75 in 2012.10 The number of new students at the MEPI schools peaked at over 2,500 per year from 2010 to 2015.7 Training and recruiting additional faculty was required in some countries, such as in Zambia where 70 postgraduate students helped fill basic science faculty positions including at two new schools, the addition of which increased the number of students in Zambia from 54 to 250.11 In Tanzania, faculty incentives and recruitment efforts increased the number of faculty members from 96 to 167 in under five years.7 Some countries focused on specialists according to national priority. For example, in Ghana, 15 emergency physicians and 59 emergency nurses were graduated, 500 medical students were trained in emergency medicine, and 300 district health care workers were trained in HIV/AIDS care in the emergency department.7 Ethiopia had already greatly increased the number of medical school enrollees,12 so there the support from MEPI was largely focused on improving the quality of education, faculty training, retention, and research capacity.13
Curricula were reviewed and revised as needed at all MEPI institutions to adapt to new health care needs and new educational methods and technologies. Seven schools revised their curricula to follow the tenets of competency-based medical education, which prepares graduates to be able to apply specific competencies in care situations. Competencies may cover critical thinking, information management, communication skills, clinical skills, knowledge of population health, foundational scientific knowledge, and professional values and attitudes. The template that the University of Ibadan developed to tailor its curriculum to address core competencies became the national standard for Nigeria.7 HIV/AIDS was also integrated into training curricula. For example, the University of KwaZulu-Natal (UKZN) in South Africa incorporated HIV/AIDS training into degree programs in internal medicine, pharmacy, nursing, and family medicine.7 Makerere University in Uganda enhanced HIV/AIDS content and training in the community-based clerkship, while Kwame Nkrumah University of Science and Technology (KNUST) in Ghana incorporated training in recognizing and treating HIV in emergency settings into the curriculum.7
Faculty development, a critical component of improving faculty effectiveness and retention, was achieved mainly through short courses in subjects including teaching methods, leadership, mentoring, epidemiology, and research. Nine of 13 schools established or strengthened medical education departments.14 Master’s degree programs in health professions education were introduced at three schools.7 Twelve schools funded faculty conference registration and travel.7 Most schools also supported research mentoring, research seed grants, and the acquisition of computer hardware and other office equipment. Many faculty were supported to pursue additional advanced degrees. MEPI funds were used to hire 51 staff at six schools, of whom all but 4 were expected to be retained with other funds after the MEPI grant period.7
One of the MEPI technical working groups focused on e-learning, which was adopted at 12 of the 13 MEPI institutions.7,15 In Ghana, for example, KNUST made many of their didactic lectures and training modules available online—and then documented thousands of page views. Clinical skills laboratories and simulation learning, which allow students to learn without interfering with patient care, were established or strengthened at 7 MEPI schools, some of which served medical and nursing students in interprofessional teams.7 Library resources were strengthened at all schools. Improvements included providing librarian training; discarding outdated materials; purchasing new books; and procuring e-books, electronic journal subscriptions, and computer hardware, thereby establishing e-library information centers. In Kenya, for example, the library services at the University of Nairobi College of Health Sciences were improved in partnership with the University of Maryland Health Sciences and Human Services Library.16
Retention and Rural Placement
Retention of medical graduates in-country is a long-term goal that was not feasible to ascertain over the five-year MEPI implementation period; however, graduate tracking systems were established, and several key activities addressed this goal.17 In Tanzania, for example, nearly 100% of medical graduates were being tracked through alumni associations, social media, and other approaches.7 Further, the Year Five Report7 noted a shift in student attitude in Zimbabwe, where, at the beginning of MEPI, most students (80%) indicated that they planned to leave the country, but by the end, most (82%) said that they planned to remain.
Most MEPI schools expanded community-based education to make training more relevant to the local context by adding new community sites and sending more students to the sites.18,19 The Uganda consortium, for example, increased the number of sites by 43% to 162 sites in 72 districts.7 Further, the MEPI consortium in Uganda included Mbarara University of Science and Technology, a new medical school, which, located in a rural area, strengthened Uganda’s decentralized medical education model. In Ethiopia, MEPI provided resources, including a minibus for student transport and Internet access to decongest overcrowded classrooms and to support the training of students in rural areas.7 The University of Nairobi adapted a U.S. model for regional training to provide clinical training at 14 decentralized training sites throughout Kenya without requiring costly new construction.20 Additionally, preceptorships or honorary teaching appointments were given to some rural practitioners in Nigeria, which boosted their morale and motivated them to remain in rural practice.7 Five schools targeted recruitment of students from rural or underserved populations as a strategy to increase retention of graduates in these communities. UKZN focused its research capacity building on rural sites to facilitate trainees returning there as mentors.21
HIV Service Delivery
Increasing capacity for high-quality services to prevent HIV infection and to provide care and treatment for people living with HIV was the principal reason for the establishment of MEPI and was a particular focus throughout both planning and implementation. According to the MEPI Year Five Report, activities included revising both undergraduate and postgraduate curricula to incorporate new HIV guidelines; providing preservice and in-service HIV/AIDS training for physicians, nurses, midwives, and others; and supporting myriad HIV-focused research activities.7 At UKZN, for example, MEPI supported 22 PhD candidates who conducted research projects on HIV clinical and laboratory services and health systems. At Stellenbosch University in South Africa, faculty participated in a clinician mentoring program focused on HIV and tuberculosis coinfection. The University of Malawi trained colposcopy screeners, oncology nurses, palliative care nurses, clinical officers, and counselors who returned to their clinics to train their colleagues in HIV-associated cervical cancer screening and treatment through visual techniques (e.g., visual inspection with acetic acid) and cryotherapy. The program provided integrated services including cancer screening, family planning, and HIV care at three clinics delivering care to 15,000 HIV-infected women per year. In addition to the HIV/AIDS-focused research and training, another success is the number of people who received care. According to the Year Five Report,7 an estimated 12,000 people living with HIV/AIDS received treatment and care services from MEPI trainees in Mozambique, and in Zimbabwe, more than one million HIV prevention, care, and treatment services were provided from 2011 to 2014 by MEPI trainees.
Research Support
All MEPI institutions conducted courses on research-related topics such as research methods, the design of research studies (including in implementation science22), data collection, data management and analysis, scientific manuscript and grant writing, and research ethics. According to one internal NIH report (November 2015), students from MEPI institutions in nine countries conducted 511 original mentored research projects. By 2015, a total of 376 publications were attributed to support from MEPI; of these, 307 had a MEPI school faculty member as the first author, 109 concerned medical education, and 51 focused on HIV/AIDS.7 By 2015, MEPI faculty had given over 400 presentations at scientific meetings worldwide, including at the African Conference on Emergency Medicine, the Third Global Forum on Human Resources for Health, and the World Health Summit.7 In MEPI year five (2015), nearly 3,000 undergraduates, 552 postgraduates, and 129 PhD candidates were reported to be participating in MEPI-funded research.7
At each MEPI institution, 5% of the programmatic grant funding was dedicated to strengthening research administration. Many institutions established research support centers to assist faculty and students with designing research investigations, identifying and applying for funds, administrating grants post award, and analyzing data.23 Most MEPI institutions successfully applied for grants from the NIH and other international funders, such as the Wellcome Trust; overall, 10 schools reported 26 successful grant awards by 2015.7
Further, in 2014–2015, the NIH Common Fund and nine other NIH ICOs (List 1) committed an additional $36.5 million (over and above the original $130 million) from 2015 to 2020 to support early- and midcareer faculty in HIV/AIDS and other scientific areas at MEPI institutions under the MEPI Junior Faculty Program (Appendix 1). These 11 grants (awarded to 11 institutions in 8 countries) illustrate the strengthening research enterprise at MEPI institutions.
Partnerships
Grantees used MEPI funding to strengthen in-country partnerships with medical institutions to improve medical education and research training.24 For example, Makerere collaborated with four other universities in Uganda; the five universities shared technical and faculty resources, and faculty from all five institutions worked together to revise curricula.24 In Nigeria, more than 1,600 faculty, graduate students, and resident doctors (from a consortium of nine institutions) were trained in career development as part of a comprehensive alliance, heralding a new era of collaboration among research universities.25
All MEPI institutions also worked closely with the ministries of health and ministries of education in their countries. Senior government officials regularly participated in in-country MEPI meetings and the international MEPI PI Council annual symposium. In Zambia, for example, MEPI worked with the Ministry of Health to adapt the obstetrical and neonatal guidelines developed for the university teaching hospital for use at the provincial and district levels.7 Additionally, MEPI institutions in Zimbabwe and Kenya worked with the ministries of health in those countries to strengthen disease outbreak investigations, responses, and surveillance systems.7 In Tanzania, the Kilimanjaro Christian Medical University improved information and communications infrastructure through the successful establishment of e-learning with tablet computers for all medical students; as a result, the Ministry of Education planned to develop e-learning as a primary tool for all higher learning institutions and invested in providing Internet accessibility to all universities.26
MEPI also supported interprofessional collaboration. Training across the MEPI network included thousands of nurses, midwives, laboratory technicians, pharmacists, and other allied health professionals. Additionally, MEPI institutions provided cross-discipline training, such as laboratory training for clinicians,27 and use of skills laboratories for simulated learning for physician, nursing, and other health professions trainees.
Several international South–South partnerships occurred (Appendix 1). For example, KNUST in Ghana collaborated with UKZN in South Africa; KNUST faculty, residents, and nursing trainees shared their emergency medicine expertise while UKZN faculty, residents, and nursing trainees contributed their HIV expertise. In another international, South–South collaboration, Universidade Eduardo Mondlane in Mozambique established resident exchanges and collaborative research with the Universidade Federal da Bahia and Fiocruz in Brazil.
Finally, MEPI supported many North–South collaborations. Every MEPI programmatic, linked, and pilot grant included one or more collaborations with institutions in the United States, Canada, or Europe (Appendix 1).
Taken together, these MEPI-established partnerships and networks constituted a community of practice. This extended group of faculty and trainees interacted regularly through telecommunications and meetings to share common interests and innovative solutions to improve health professions education and research capacity. This community helped leverage resources, disseminate and implement more effective practices, and ensure relevancy and support over the long term.28
Sustainability
Sustainability was a priority of MEPI from the outset. It was an important element in the MEPI grant review criteria and became increasingly important over the five-year implementation period. Sustainability and capacity building were particularly emphasized in the evolution of North–South collaborations. MEPI-supported activities, such as developing enrollment and retention policies, revising curricula, and reforming pedagogical methods, were integrated into the work of partner sub-Saharan African institutions. In Zimbabwe, for example, lectures on cardiovascular physiology were developed with visiting professors from a U.S. university, and teaching responsibility was gradually turned over to Zimbabwean junior faculty and postdoctoral fellows.7
Some MEPI institutions attracted monetary support from their governments and/or nonmonetary support from other donors to sustain select MEPI activities after the grant funding ended, but most anticipated having to scale down their programs. In response to a year five (2015) survey,7 most schools reported that they would have to cut back MEPI-supported programs, especially the research activities, by 25% to 50% when MEPI funding ended; however, no school said the number of faculty and students enrolled would be reduced. Six schools said that the most durable MEPI-funded resource was information and communication technology, making this the most common response.7
The 11 MEPI Junior Faculty Program grants (Appendix 1) were also important to consolidate and sustain the research capacity developed through the original programmatic, linked, and pilot MEPI grants.
Summary and Success Factors
MEPI was successful in achieving its primary goal: increasing the numbers of medical school enrollees and graduates in the institutions it supported. Additionally, numerous activities to increase the quality of education and retention and rural placement of medical graduates were successfully implemented. Capacity to conduct biomedical research was strengthened and scientific productivity was increased through MEPI support. Lastly, several elements (e.g., partnerships, additional funding and support, enduring technology) to help ensure sustainability were successfully incorporated. Importantly, early indicators, such as additional grant funding, multiple publications, and ongoing international and intranational partnerships, have demonstrated MEPI’s lasting impact on medical education in Africa.
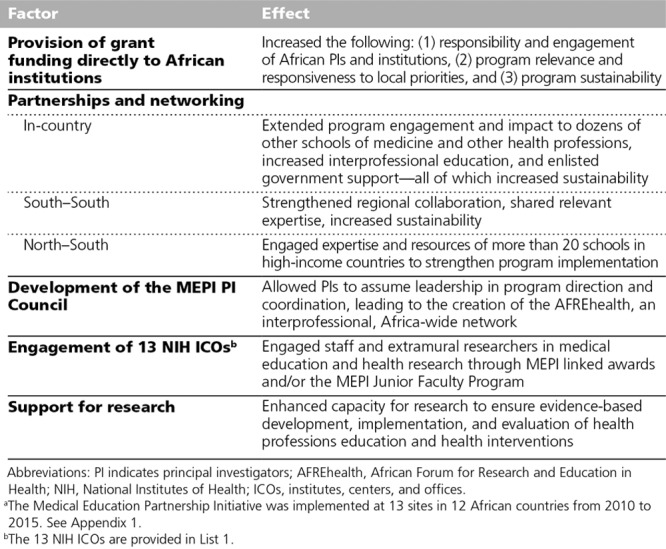
One of the critical success factors (Table 2) for MEPI was ensuring the leadership of the African grantees and institutions by awarding the competitive grants directly to the leaders of the institutions themselves, rather than routing the funding through U.S.-based institutions. This direct funding allowed the African grantees control, thereby increasing their engagement and responsiveness and also enhancing the relevance of MEPI projects to local priorities. Partnerships and networking were also critical to the initiative’s success. To illustrate, one PI commented, “MEPI demonstrates that North–South as well as South–South partnerships, with an explicit focus on improving local health systems through better education, can be designed to empower partners in the South with support from collaborators in the North.”29 In-country partnerships and resource sharing with other schools of medicine and other health professions effectively multiplied the reach and effectiveness of the initiative.
Table 2.
Factors Contributing to the Success of the Medical Education Partnership Initiative (MEPI)a
The emergence of the robust network of MEPI PIs in the MEPI PI Council was another key factor in the initiative’s overall success and sustainability. The group continues to communicate regularly, meet, share best practices, and coordinate activities in the newly formed African Forum for Research and Education in Health,30 a direct successor to the MEPI PI Council.
The inclusion of research as a main component of MEPI was helpful to establish an academic foundation for activities and to engage and retain not only faculty at MEPI institutions but also international scholars. The research focus also helped to mobilize substantial additional resources from NIH institutes through the MEPI pilot and linked awards and through the ongoing MEPI Junior Faculty Program. The benefits of strengthening research capacity in MEPI institutions are expected to have a lasting effect in the training of physicians through new, evidence-based approaches; in the provision of outstanding, cutting-edge care to patients; and in turn, in the creation of medical centers of excellence.31
Lessons Learned and Limitations
The coordinating center at GWU played an important role in not only supporting and providing technical assistance to the MEPI institutions but also incubating the community of practice. One drawback, however, was the perceived conflict of interest that arose from both evaluating and facilitating the MEPI institutions. In retrospect, designating separate institutions for facilitating and evaluating MEPI may have been advantageous. In addition, while each site reported substantial information, a limitation in the evaluation was the lack of systematic summary data across all sites across all five years. This idiosyncrasy in reporting is typical for separate NIH grants awarded under a single funding opportunity announcement, but it does limit our ability to report reliable quantitative summary data. Moreover, assessing the longer-term national effect of MEPI was beyond the scope of the required grant reporting. Future work could include national surveys to assess the number, retention, and rural placement of doctors, as well as the numbers of grants awarded to and publications emanating from MEPI institutions. Finally, as staff members of the funding and implementing agencies, we acknowledge the potential for bias in assessing and reporting the accomplishments and outcomes of MEPI.
Future Directions
The achievements in the first phase of MEPI have been considerable, and taken together, they provide a foundation for additional gains.32 These accomplishments align well with the vision articulated in 2010 by the Lancet Commission on the Education of Health Professionals for the 21st Century:
all health professionals in all countries should be educated to mobilize knowledge and to engage in critical reasoning and ethical conduct so that they are competent to participate in patient and population-centered health systems as members of locally responsive and globally connected teams.33
Major gaps remain in the quantity and retention of health care workers, in the quality of health professions education, and in the resources available for research to decrease the incidence of HIV/AIDS and meet other global health goals.1 Future support for health professions education and research capacity building in Africa should seek to consolidate, broaden, and further improve the progress made to date. Additional investments (including domestic resources); international health workforce policy interventions (e.g., task shifting); and emphases (with goals measured by quantitative data) on performance, productivity, efficiency, quality, and innovation are all needed.1 The long-term social and economic value of investments—including the creation of quality jobs in the health sector, leveraged domestic and foreign investment in health care and research, and improved health care and health outcomes—could be substantial.
With support from the NIH, the National Academy of Medicine convened a workshop in Uganda in 2016 with African health professions leaders to discuss extending the work of the MEPI PI Council and establishing an African association for health professions education and research. Interprofessional membership—including doctors, nurses, and other allied health professionals—would be a core feature of such an association. The 2016 workshop participants also recommended disseminating educational resources and sharing best practices in health professions education; encouraging research on educational methodologies and approaches; and integrating biomedical, behavioral, clinical, and operational research into health professions education and practice.34
In addition to support for an African health professions education association,35 additional programmatic support for high-HIV-burden, low-resource PEPFAR countries is anticipated. Such monetary support will further strengthen the quality of medical and nursing education, increase the retention of health professionals post training, fund research on best educational practices, and enhance the capacity of students to conduct health research.36 As with the first phase of MEPI, these activities are intended to be relevant and responsive to national and international needs and policies.1,37
Conclusions
MEPI succeeded in increasing the number of graduates from African medical schools, in improving the quality of their education, and in enhancing the retention of physicians where they were most needed. Biomedical research capacity and productivity were also increased—and are being sustained with additional NIH support for junior faculty at 11 institutions in 8 countries. The transformative impact of MEPI on medical education in Africa will be extended with planned additional PEPFAR support for an African association for health professions education and research35 and new programmatic grants36 for interprofessional education and research in high-HIV-burden, low-resource PEPFAR countries.
List 1
The NIH Institutes, Centers, and Offices Providing Funding for MEPI Institutionsa
The 7 NIH ICOs providing funding ($30 million) for linked and pilot grants (2010–2015)
National Heart, Lung and Blood Institute
National Human Genome Research Institute
National Institute of Mental Health
National Institute of Neurological Disorders and Stroke
National Institute of Nursing Research
Office of AIDS Research
Office of Research on Women’s Health
The 9 NIH ICOs providing funding ($36.5 million) through the MEPI Junior Faculty Program (2015–2020)
Eunice Kennedy Shriver National Institute of Child Health and Human Development
National Heart, Lung, and Blood Institute
National Institute of Dental and Craniofacial Research
National Institute of Mental Health
National Institute of Neurological Disorders and Stroke
National Institute of Nursing Research
National Institute on Minority Health and Health Disparities
Office of AIDS Research
Office of Research on Women’s Health
Abbreviations: NIH indicates National Institutes of Health; ICOs, institutes, centers, and offices; MEPI, Medical Education Partnership Initiative.
aMEPI was implemented at 13 sites in 12 African countries from 2010 to 2015. See Appendix 1.
Acknowledgments:
The authors thank Dr. Joel Breman for his critical review of this article.
Appendix 1. The Countries, Institutions, Principal Investigators, Grant Types, and Partner Organizations Involved in the Medical Education Partnership Initiative (MEPI)
Footnotes
Funding/Support: None reported.
Other disclosures: None reported.
Ethical approval: Reported as not applicable.
Disclaimer: The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the U.S. government.
Previous presentations: A previous article described the midterm accomplishments of the Medical Education Partnership Initiative (MEPI) from the National Institutes of Health perspective: Glass RI, Razak MH, Said M. The importance of research in the MEPI program: Perspectives from the National Institutes of Health. Acad Med. 2014;89:S9-S10.
References
- 1.World Health Organization. Health Workforce Requirements for Universal Health Coverage and the Sustainable Development Goals. October 2016. Geneva, Switzerland: World Health Organization; http://www.who.int/hrh/resources/health-observer17/en. Accessed September 28, 2018. [Google Scholar]
- 2.Mullan F, Frehywot S, Omaswa F, et al. Medical schools in sub-Saharan Africa. Lancet. 2011;377:1113–1121. [DOI] [PubMed] [Google Scholar]
- 3.El-Sadr WM, Holmes CB, Mugyenyi P, et al. Scale-up of HIV treatment through PEPFAR: A historic public health achievement. J Acquir Immune Defic Syndr. 2012;60(suppl 3):S96–S104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.110th Congress. H.R.5501—Tom Lantos and Henry J. Hyde United States Global Leadership Against HIV/AIDS, Tuberculosis, and Malaria Reauthorization Act of 2008. https://www.congress.gov/bill/110th-congress/house-bill/5501. Accessed October 3, 2018.
- 5.Collins FS, Glass RI, Whitescarver J, Wakefield M, Goosby EP. Public health. Developing health workforce capacity in Africa. Science. 2010;330:1324–1325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Goosby EP, von Zinkernagel D. The Medical and Nursing Education Partnership Initiatives. Acad Med. 2014;89(8 suppl):S5–S7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Derbew M, Donkor P, Hakim J, et al. Medical Education Partnership Initiative year 5 report. http://www.mepinetwork.org/images/stories/MEPI%20Year%205%20Report_No%20Appendixes.pdf. Published 2016. Accessed September 28, 2018.
- 8.Breman JG, Bridbord K, Kupfer LE, Glass RI. Global health: The Fogarty International Center, National Institutes of Health: Vision and mission, programs, and accomplishments. Infect Dis Clin North Am. 2011;25:511–536, vii. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Virgínia Noormahomed E, Carrilho C, Ismail M, et al. The Medical Education Partnership Initiative (MEPI), a collaborative paradigm for institutional and human resources capacity building between high- and low- and middle-income countries: The Mozambique experience. Glob Health Action. 2017;10:1272879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mocumbi AO, Carrilho C, Aronoff-Spencer E, et al. Innovative strategies for transforming internal medicine residency training in resource-limited settings: The Mozambique experience. Acad Med. 2014;89(8 suppl):S78–S82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Simuyemba M, Talib Z, Michelo C, et al. Strengthening faculty recruitment for health professions training in basic sciences in Zambia. Acad Med. 2014;89(8 suppl):S98–S101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mengistu BS, Vins H, Kelly CM, et al. Student and faculty perceptions on the rapid scale-up of medical students in Ethiopia. BMC Med Educ. 2017;17:11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Derbew M, Animut N, Talib ZM, Mehtsun S, Hamburger EK. Ethiopian medical schools’ rapid scale-up to support the government’s goal of universal coverage. Acad Med. 2014;89(8 suppl):S40–S44. [DOI] [PubMed] [Google Scholar]
- 14.Kiguli-Malwadde E, Talib ZM, Wohltjen H, et al. Medical education departments: A study of four medical schools in Sub-Saharan Africa. BMC Med Educ. 2015;15:109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Vovides Y, Chale SB, Gadhula R, et al. A systems approach to implementation of eLearning in medical education: Five MEPI schools’ journeys. Acad Med. 2014;89(8 suppl):S102–S106. [DOI] [PubMed] [Google Scholar]
- 16.Mayo A. Improving medical education in Kenya: An international collaboration. J Med Libr Assoc. 2014;102:96–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chen C, Baird S, Ssentongo K, et al. Physician tracking in sub-Saharan Africa: Current initiatives and opportunities. Hum Resour Health. 2014;12:21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Talib ZM, Baingana RK, Sagay AS, Van Schalkwyk SC, Mehtsun S, Kiguli-Malwadde E. Investing in community-based education to improve the quality, quantity, and retention of physicians in three African countries. Educ Health (Abingdon). 2013;26:109–114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mariam DH, Sagay AS, Arubaku W, et al. Community-based education programs in Africa: Faculty experience within the Medical Education Partnership Initiative (MEPI) network. Acad Med. 2014;89(8 suppl):S50–S54. [DOI] [PubMed] [Google Scholar]
- 20.Child MJ, Kiarie JN, Allen SM, et al. Expanding clinical medical training opportunities at the University of Nairobi: Adapting a regional medical education model from the WWAMI program at the University of Washington. Acad Med. 2014;89(8 suppl):S35–S39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lalloo UG, Bobat RA, Pillay S, Wassenaar D. A strategy for developing future academic leaders for South Africa in a resource-constrained environment. Acad Med. 2014;89(8 suppl):S55–S59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Osanjo GO, Oyugi JO, Kibwage IO, et al. Building capacity in implementation science research training at the University of Nairobi. Implement Sci. 2016;11:30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mashaah T, Hakim J, Chidzonga M, et al. Strengthening research governance for sustainable research: Experiences from three Zimbabwean universities. Acad Med. 2014;89(8 suppl):S69–S72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Talib ZM, Kiguli-Malwadde E, Wohltjen H, et al. Transforming health professions’ education through in-country collaboration: Examining the consortia among African medical schools catalyzed by the Medical Education Partnership Initiative. Hum Resour Health. 2015;13:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Olaleye DO, Odaibo GN, Carney P, et al. Enhancement of health research capacity in Nigeria through North–South and in-country partnerships. Acad Med. 2014;89(8 suppl):S93–S97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lisasi E, Kulanga A, Muiruri C, et al. Modernizing and transforming medical education at the Kilimanjaro Christian Medical University College. Acad Med. 2014;89(8 suppl):S60–S64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Guarner J, Amukele T, Mehari M, et al. Building capacity in laboratory medicine in Africa by increasing physician involvement: A laboratory medicine course for clinicians. Am J Clin Pathol. 2015;143:405–411. [DOI] [PubMed] [Google Scholar]
- 28.Frehywot S, Mullan F, Vovides Y, et al. Building communities of practice: MEPI creates a commons. Acad Med. 2014;89(8 suppl):S45–S49. [DOI] [PubMed] [Google Scholar]
- 29.Olapade-Olaopa EO, Baird S, Kiguli-Malwadde E, Kolars JC. Growing partnerships: Leveraging the power of collaboration through the Medical Education Partnership Initiative. Acad Med. 2014;89(8 suppl):S19–S23. [DOI] [PubMed] [Google Scholar]
- 30.Omaswa F, Kiguli-Malwadde E, Donkor P, et al. Medical Education Partnership Initiative gives birth to AFREhealth. Lancet Glob Health. 2017;5:e965–e966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Glass RI, Razak MH, Said M. The importance of research in the MEPI program: Perspectives from the National Institutes of Health. Acad Med. 2014;89(8 suppl):S9–S10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Omaswa FG. The contribution of the Medical Education Partnership Initiative to Africa’s renewal. Acad Med. 2014;89(8 suppl):S16–S18. [DOI] [PubMed] [Google Scholar]
- 33.Frenk J, Chen L, Bhutta ZA, et al. Health professionals for a new century: Transforming education to strengthen health systems in an interdependent world. Lancet. 2010;376:1923–1958. [DOI] [PubMed] [Google Scholar]
- 34.National Academies of Sciences, Engineering, and Medicine. Establishing an African Association for Health Professions Education and Research—Workshop in Brief. April 19, 2016. Washington, DC: National Academies of Sciences, Engineering, and Medicine; http://nationalacademies.org/hmd/Reports/2016/Establishing-an-African-Association-for-Health-Professions-Education-and-Research.aspx. Accessed September 28, 2018. [PubMed] [Google Scholar]
- 35.Department of Health and Human Services, Fogarty International Center, National Institutes of Health. African Association for Health Professions Education and Research (R25 Clinical Trials Not Allowed). January 12, 2018. Bethesda, MD: Department of Health and Human Services, Fogarty International Center, National Institutes of Health; https://grants.nih.gov/grants/guide/rfa-files/RFA-TW-18-001.html. Accessed September 28, 2018. [Google Scholar]
- 36.Department of Health and Human Services, Fogarty International Center, National Institutes of Health. Health-Professional Education Partnership Initiative (HEPI) (R25 Clinical Trial Not Allowed). December 18, 2017. Bethesda, MD: Department of Health and Human Services, Fogarty International Center, National Institutes of Health; https://grants.nih.gov/grants/guide/rfa-files/RFA-TW-17-001.html. Accessed September 28, 2018. [Google Scholar]
- 37.Kim JY, Evans TG. Redefining the measure of medical education: Harnessing the transformative potential of MEPI. Acad Med. 2014;89(8 suppl):S29–S31. [DOI] [PubMed] [Google Scholar]


