A 74-year-old man was admitted to the intensive care unit for progressive muscle weakness leading to hypercarbic respiratory failure requiring intubation, elevated creatine kinase, diplopia, and bilateral ptosis. Due to concern for severe, progressive inflammatory myositis, he was started on pulse dose methylprednisolone 1 g daily for 3 days followed by 1 mg/kg daily and intravenous immunoglobulin (IVIG) infusions. After 1 week of glucocorticoid treatment, he developed dark, bloody stools with clots and abdominal discomfort. On further history, he had been having rare, intermittent bloody diarrhea over the past year. He was born in Mexico and no known family history of colon cancer.
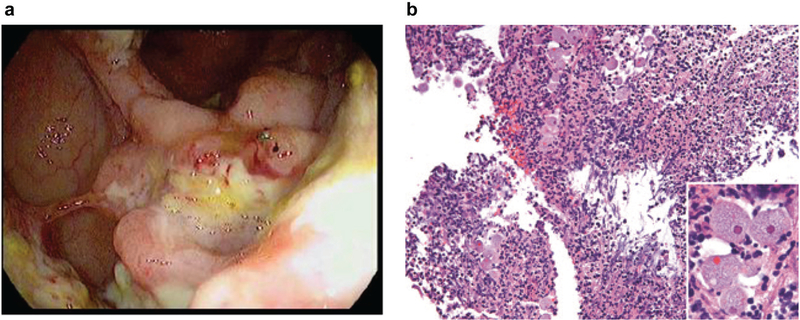
With concern for a possible paraneoplastic syndrome underlying his myopathy, a CT scan of the chest, abdomen, and pelvis obtained the day of his bloody stools identified eccentric cecal wall thickening concerning for malignancy. He subsequently underwent a colonoscopy, and a circumferential area of an ulcerated, friable fungating mass in the ascending colon extending into the cecum was seen (Fig. 1a). Additionally, other multiple foci of ulcerated masses were identified in the cecum and transverse colon. Biopsies were taken. Although atypical, the overall clinical picture was felt to be most concerning for colon cancer.
Fig. 1.
a Sample colonoscopy image of a circumferential, ulcerated, friable fungating mass in the cecum. b Necrotic exudates from the cecal mass. Abundant necrotic parenchyma and acute exudates with collections of amebic trophozoites (H&E ×100). Insert: trophozoites with prominent central, eosinophilic karyosome (H&E ×600)
Surprisingly, histologic sections showed a dense acute inflammatory infiltrate with ulceration and necrosis, as well as numerous amebic organisms with foamy cytoplasm and occasionally containing erythrocytes, consistent with Entamoeba histolytica amebic colitis and ameboma (Fig. 1b). E. histolytica immunoglobin levels later resulted as positive. Separately, a muscle biopsy was consistent with polymyositis, and his presenting symptoms responded to treatment with corticosteroids and IVIG. Although rare cases have described muscle abscesses, myositis is not a known complication associated with E. histolytica infection. It was thus felt that immunosuppression with high dose steroids for treatment of polymyositis led to the progression of a chronic infection in light of his 1-year history of intermittent bloody stools. His amebic colitis was treated with 3 weeks of metronidazole followed by a 1 week of oral paromomycin given his immunosuppression and an episode of recurrent bleeding.
E. histolytica is an important enteric pathogen in developing countries, causing amebic colitis and extra-intestinal manifestations including hepatic abscesses. Patients typically have a history of diarrhea with or without blood. Considered a rare complication, amebomas are a mass of granulation tissue surrounding a dense inflammatory core secondary to chronic amebic infection. They occur most commonly in the cecum and ascending colon in the and can mimic colon cancer, both radiographically and endoscopically (1). They are usually associated with concurrent hepatic abscesses (2) which were interestingly not seen in this patient. Serological testing is a helpful adjunct in the diagnosis of intestinal amebiasis (3). Corticosteroids are associated with an increased risk of fulminant amebic colitis (4). Finally, treatment with metronidazole followed by paromomycin is highly effective.
This case report of a patient who immigrated from an endemic region on immunosuppressive therapy with the surprising finding of ameboma illustrates the need to consider it in the differential diagnosis of colonic masses in the appropriate clinical context.
Acknowledgments
Financial support: None.
Footnotes
Guarantor of the article: Nielsen Fernandez-Becker, MD, PhD.
Potential competing interests: None.
Patient consent: Informed consent from the patient or their designated decision maker was obtained for publication of their information.
REFERENCES
- 1.Lin C-C, Kao K-Y. Ameboma: a colon carcinoma-like lesion in a colonoscopy finding. Case Rep Gastroenterol. 2013;7: 438–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Misra SP, Misra V, Dwivedi M. Ileocecal masses in patients with amebic liver abscess: etiology and management. World J Gastroenterol. 2006; 12:1933–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Haque R, Huston CD, Hughes M, et al. Amebiasis. N Engl J Med. 2003;348:1565–73. [DOI] [PubMed] [Google Scholar]
- 4.Shirley D-A, Moonah S. Fulminant amebic colitis after corticosteroid therapy: a systematic review. PLoS Negl Trop Dis. 2016;10:e0004879. [DOI] [PMC free article] [PubMed] [Google Scholar]