Abstract
Background and Objectives
Acute Ischemic stroke (AIS) is a time-sensitive emergency and patients frequently present to, and are transferred from emergency departments (EDs). We sought to evaluate potential factors, particularly organizational, that may influence the timeliness of inter-facility transfer for ED patients with AIS.
Methods
We conducted semi-structured interviews at three EDs that routinely transfer AIS patients. A structured interview guide was developed and piloted prior to use. Staff were asked about perceived facilitators and barriers to timely and high quality emergency care for patients with AIS who require transfer. Each interview was audio recorded, transcribed, coded, and analyzed using an iterative inductive-deductive approach to build a list of themes and subthemes, and identify supporting quotes.
Results
We interviewed 45 ED staff (administrative staff, nurses, and physicians) involved in acute stroke care. We identified four major themes influencing the execution of inter-facility transfers of AIS patients: 1) Processes, 2) Historical experiences; 3) Communication; and 4) Resources. Pre-existing protocols that standardized processes (e.g., auto-acceptance protocols) and reduced unnecessary communication, combined with direct communication with the neurology team at the comprehensive stroke center, and the flexibility and availability of human and physical resources (e.g., staff and equipment) were commonly cited as facilitators. Lack of communication of clinical and operational outcomes back to transferring ED staff was viewed as a lost opportunity for process improvement, inter-organization relationship building, and professional satisfaction.
Conclusions
ED staff view the inter-facility transfer of AIS patients as highly complex with multiple opportunities for delay. Coordination through the use of protocols and communication pre- and post-transfer represented opportunities to facilitate transfers. Staff and clinicians at transferring facilities identified multiple opportunities to enhance existing processes and ongoing communication quality among facilities involved in the acute management of patients with AIS.
Keywords: ischemic stroke, health care delivery systems, emergency care, transfers, qualitative methods
INTRODUCTION
Stroke is a time-sensitive neurologic emergency affecting nearly 800,000 Americans annually. Strokes are typically ischemic in nature and individuals experiencing them frequently present to the emergency department (ED).1 Acute ischemic stroke (AIS) patients treated rapidly with intravenous tissue plasminogen activator (tPA) are significantly more likely to have an improved neurological outcome at 3–6 months.1 Large vessel occlusion (LVO) strokes (e.g., internal carotid, basilar, or middle cerebral arteries), are responsible for approximately 100,000 strokes annually,2 can be neurologically devastating, and are time-sensitive.3 Both the American Heart Association (AHA) and American Stroke Association (ASA) recommend treating LVOs by mechanical thrombectomy (Class I, Level of Evidence: A).2 Yet nearly half of the U.S. population is more than 60 minutes by ground transport from the closest endovascular-capable hospital and often requires inter-facility transfer to the preferred treatment.3
In a study of patients with AIS who received mechanical thrombectomy, most patients were transferred, yet transfer itself was associated with delayed treatment and worse neurological outcomes.4 Delays at transferring facilities, mostly occurring in EDs,5 further complicate access to specialized stroke care. The source of delays at transferring EDs, however, is poorly understood and represents a potential opportunity for reducing transfer delays and otherwise improving the quality of the transfer process.
We build on prior quantitative research that has identified delays and their clinical consequences by using qualitative methods to explore the mechanisms underlying observed delays. Qualitative research richly captures the process dynamics surrounding more and less successful transfers. Specifically, we examine the perceptions of ED staff and providers’ who regularly participate in transfers to capture the facilitators and barriers to the provision of timely care at the transferring ED. In doing so, we gain a deeper understanding of the transfer process as well as provide a foundation for more refined quantitative empirical research in the future.
METHODS
We conducted and analyzed semi-structured interviews of staff (administrative, nursing, emergency physicians, and neurologists) at three EDs in the metropolitan Nashville, TN area. This study was approved by the Vanderbilt University Medical Center IRB.
Participants
We identified three EDs in the Nashville, TN metropolitan area that are not comprehensive stroke centers. Characteristics of these EDs can be seen in Table 1. All three facilities are relatively low-volume EDs with varying degrees of Neurology availability. At Facility A, a neurologist was not consistently available in-person and rarely admitted AIS patients. Neurologists were regularly consulted at the comprehensive stroke center when an AIS was suspected. At Facility B, a neurohospitalist was available for consults in the ED during weekday business hours. After hours, teleneurology was used with the comprehensive stroke center for suspected AIS consults. All patients treated with thrombolysis or suspected of an LVO were transferred. A Facility C, Neurology was available 24/7 for in-person consultation but patients treated with thrombolysis or suspected of an LVO were transferred. Subsequently, all three EDs routinely transfer AIS patients to a single comprehensive stroke center in metro Nashville, TN. However, two additional comprehensive stroke centers are available as alternatives.
Table 1.
Characteristics of the facilities included in the study.
| Site | Type of Facility | Rural/Urban | ApproximateAnnual ED Volume | Staff Interviewed |
|---|---|---|---|---|
| Facility A | Community | Urban | 33,000 | • ED Nurses (7) • Emergency Physicians (4) |
| Facility B | Community | Rural | 30,000 | • ED Nurses (7) • Emergency Physicians (3) • Staff (3) • Neurologist (1) |
| Facility C | Federal | Urban | 25,000 | • ED Nurses (12) • Emergency Physicians (4) • Staff (3) • Neurologist (1) |
Staff and clinicians were recruited through clinical leadership (e.g., nurse managers and medical directors) at each facility. Among the 45 interviewees, there were 26 ED nurses, 11 emergency physicians, two neurologists, and six medical technologists or administrative support staff. Participants were interviewed over a three-month period. Participants were offered the opportunity to participate in a drawing for a $100 gift card. In addition, letters were written to administrators recognizing staff efforts to participate in research.
Procedure
We used individual interviews rather than focus groups to retain confidential responses and the attendant psychological safety needed when discussing sensitive organizational processes.6 A written semi-structured interview guide was developed de novo using the following three categories based on the Donabedian model of quality7: organizational processes (including formal and informal protocols), infrastructure (e.g., physical and human resources), and organizational behavior which includes work relationships, communication, and the coordination that occur both internal and external to the organization. Although organizational behavior was not part of the original Donabedian model, we included this category because it furthers our understanding of performance by elucidating the mechanisms by which individuals and groups translate their actions into performance. Within these three categories, interview topics included staff roles, recognition and diagnosis of emergent conditions, admission and transfer processes, interpersonal and inter-facility communication, and perceived facilitators and barriers to timely care. The written guide included open-ended questions and the interviewers asked unscripted follow-up questions when appropriate (Table 2). Prior to use, interviewers piloted the interview guides with 3 non-study ED staff and found that interviews lasted between 20 and 30 minutes. Each interview was conducted in English, audio recorded, and transcribed for analysis.
Table 2.
Semi-structure interview guide questions
| Sample interview questions |
|---|
| 1. Describe your responsibilities in the emergency department |
| 2. When a patient with an acute ischemic stroke is identified, walk me through the process of transferring that patient to another institution? |
| 3. Please tell me about 1–2 situations in which the transfer of patients with an acute ischemic stroke went particularly well. Poorly? |
| 4. Describe any barriers that make it difficult to transfer patients to a different facility. |
| 5. If you have been at another facility that transfers patients with acute ischemic stroke, how do the processes at this current facility differ? |
| 6. Please describe any challenges to sharing information with stroke center staff members |
| 7. Do you receive any feedback (positive or negative) from the receiving facility after the patient is transferred? |
| 8. What would you most like to see improved in the stroke transfer process? |
A codebook was developed and refined by three investigators (MH, KB, MJW) using the interview guide and a preliminary review of the transcripts. Coding transcripts were managed using Excel (Microsoft, Inc. Redmond, WA). Each statement was treated as a separate quote and could be assigned up to five different codes. Two investigators independently coded each transcript and then reviewed and reconciled their codes to produce a final coding of each transcript. Disagreements between the two coders were first resolved through discussion. If a mutual agreement was not met, a third coder served as an arbiter.
Analysis was approached using an iterative inductive-deductive approach. Coded data were aggregated and processed using SPSS v25 (IBM, Inc. Armonk, NY). A frequency distribution of coding categories was created and the quotes were sorted by category. The sorted quotes were organized into themes and subthemes and used to create a conceptual framework for understanding the inter-facility transfer process. All investigators agreed upon the final organization of themes and subthemes.
RESULTS
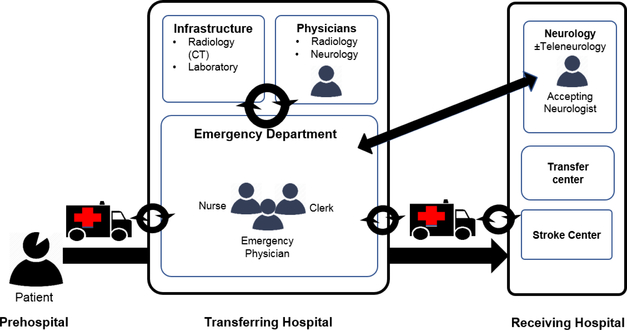
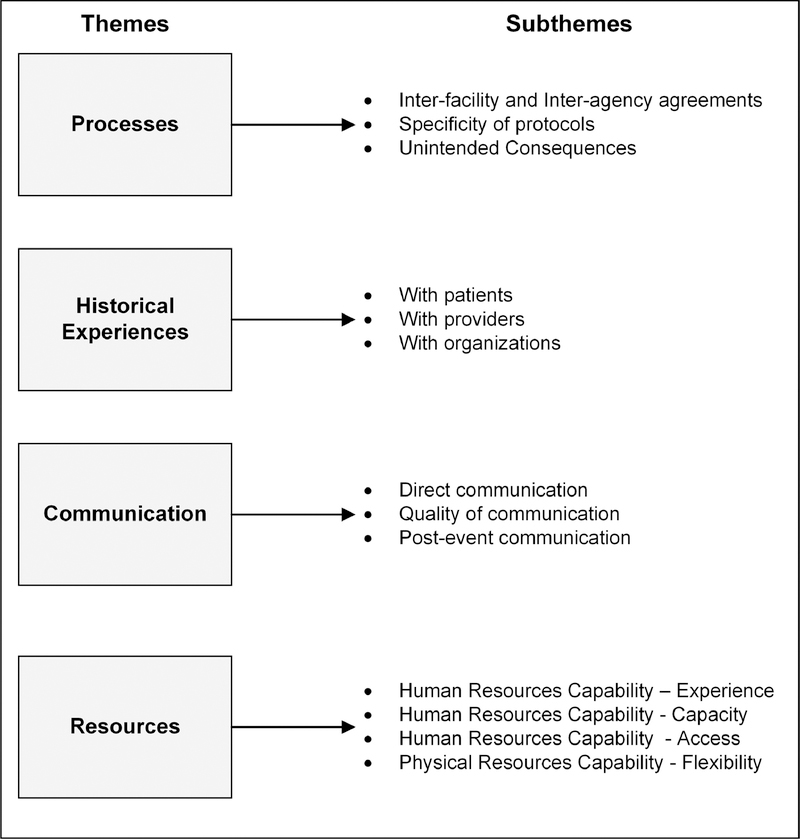
Four trained interviewers conducted 45 interviews that discussed the inter-facility transfer of patients with AIS. Breakdown of staff roles by site can be seen in Table 1. From analysis of these interviews, we developed a process flow map to summarize the specific stages and processes that affect AIS patients as they are diagnosed, receive acute medical treatment, and factors described by interviewees as influencing inter-facility transfer timeliness (Figure 1). Comprehensive results are presented by theme and accompanying subtheme as organized in Figure 2 with quotes in Supplemental Tables 1–3. Major themes, and representative quotes are presented below.
Figure 1.
Process flow map for inter-facility transfer of stroke patients. Black arrows indicate possible communication between individuals involved in the transfer process.
Figure 2.
Organization of themes and subthemes identified through interviews.
Processes
The first theme (Supplemental Table 1) involved the processes EDs use to diagnose, treat, and transfer patients with AIS. Specifically, this theme includes the formal agreements (e.g., protocols) between prehospital agencies and transferring EDs, transferring EDs and comprehensive stroke centers, the comprehensiveness of these agreements, and the unintended consequences resulting from these processes.
Inter-facility and Inter-Agency Agreements
Facility B developed protocols with local EMS agencies to formalize prehospital notification for patients that EMS suspected of AIS. This protocol was recognized by staff and clinicians as a successful strategy allowing the ED to rapidly align resources in order to prepare for the incoming patient. Once the prehospital stroke protocol was activated, resources were quickly made available:
“Neurology is notified, lab is notified, we make an announcement so if we have tertiary people that need to come down and respond like respiratory therapy, nursing supervisor, all of that is handled within the first few minutes of when the patient arrives.”
-ED Nurse; Facility B.
“Anything that’s not protocol seems to add delay....I never realized how much time you save.”
-Neurologist; Facility B.
Pre-existing arrangements (e.g., auto-acceptance of stroke patients) between facilities were viewed as particularly useful to facilitate the transfer of acute stroke patients to a comprehensive stroke center:
“The tPA patients to [stroke center] are pretty easy, because it’s the auto-accept.”
-Emergency physician; Facility B.
“If teleneurology is involved and they make the recommendation to transfer up there, then it’s pretty easy because I’m on the phone with a neurologist who’s making the recommendation.”
-Emergency physician; Facility B.
However, pre-existing agreements could also have unintended consequences and introduce transfer delays if the intended responsibilities were not met by the designated party. Prearranged transfer agreements were not always effective:
“We’re at the mercy of very poor contract with an EMS crew. If they’ve only got one [ambulance]...and ‘I won’t dispatch it to you right now.’ “
-ED nurse; Facility C.
“Sometimes [the comprehensive stroke center will] require a fee sheet, sometimes they don’t, so maybe having a very set ... a set list that’s not operator-dependent would be helpful that we could print and put at the clerk desk so that they know.
-Emergency physician; Facility B.
Specificity of Protocols
Another recognized limitation was that the initiation criteria were unclear and left to the discretion of the ED provider:
“Criteria are so broad. Basically anybody coming in saying they feel weak or they feel dizzy or woozy... That can be a third of my patient population during a day.”
-Emergency physician; Facility B.
With studies supporting the rapid identification and treatment of LVOs and subsequent change in the stroke guidelines,2 the consideration of a potential LVO in the acute evaluation of stroke patients was raised by transferring ED staff, particularly whether the initial radiologic imaging should change. Each of the EDs reported that angiographic imaging to evaluate cerebral vasculature for a potential LVO was infrequently done and even more rarely initiated by an emergency physician. When asked why angiographic imaging (e.g., CT angiography [CTA]) was seldom performed, uncertainty when a patient required a CTA and potential delays in performing the scan were cited:
“There’s not a standard on when I might [order a CTA] initially... we have worked on [guidelines], but to me, they’re still hard to pick out.”
-Emergency physician; Facility B.
However, ordering a CTA as part of the initial work-up was viewed as potentially enhancing the timeliness of care:
“It saves time [to order CTA as the initial study] if it’s the protocol, ‘cause if it’s not the usual standard action, then there’s more of a delay usually.”
-Neurologist; Facility C.
Unintended Consequences
Despite the perception that the use of protocols and early CTA imaging may save time, none of the transferring sites included CTA imaging in their stroke protocols. An unintended consequence emerged that decisions were made ad hoc and on a case-by-case basis. For example, the decision to order a CTA was made by consulting neurologists and could introduce delays:
“We have situations where patients are sent back that we have a circumstance where the non-cont head CT is unremarkable and the teleneurologist makes a recommendation for a CTA now, and so then they go back to the scanner for a contrasted study, have to wait on another scan, upload those images, a second or third conversation with the neurologist in [stroke center] and then they make a decision after that on whether or not we’re going to send them or not or they’re an interventional candidate.”
-Emergency physician; Facility B.
Even the transfer destination may not be decided until a stroke occurred:
“The decision to where the patient goes, where they’re transferred, who they go to, is all made by the [ED] physician.”
-Neurologist; Facility C.
Historical Experiences
The historical involvement of the transferring ED with patients, providers, and between organizations during acute stroke care comprised the next theme (Supplemental Table 2). Interviewees described prior events and relationships that have shaped current practices. These experiences were seen as having a mixed influence on the timeliness of care for AIS patients. As an example of historical experiences serving as a facilitator, interviewees at all three sites described the importance of reliable and timely transfer as shaping their distinct modes of transportation for AIS patients. Facility A uses the 911 system, Facility B uses local EMS, and Facility C is close enough to a comprehensive stroke center that they can usually use a wheelchair to transport the patient. As an emergency physician at Facility B described:
“EMS is based out of the hospital so there is a truck here 24/7 so whenever we determine we have a transfer we simply call them, the [Emergency Operations Center], and if that truck is gone they’ll call one of the other trucks in that’s covering and get them here almost within minutes usually.”
-Emergency physician; Facility B.
Prior experiences with neurology may also build relationships between specialties and influence changes in provider behavior. For example, ordering angiographic imaging to detect LVOs has increased as a result of cross-specialty relationships:
“We consult...a fair amount through the teleneurology... and I would say probably two-thirds of the time that CTA recommendation comes from [teleneurology].”
-Emergency physician; Facility B.
Alternatively, negative experiences with providers and organizations can have a lingering influence:
“A lot of times [receiving providers are] really difficult because ‘well you need neurosurgery, now you need a neurologist, you need this.’ There’s kind of a battle sometimes about whether or not they feel like the transfer is appropriate.”
- ED nurse; Facility A.
Communication
Another theme (Supplemental Table 2) that emerged from the interviews was the vital role that communication plays in acute stroke care. Specifically, interviewees discussed three subthemes involving the need for direct communication with specialist decision-makers, the quality of communication, and post-event communication.
Direct Communication
When a situation was urgent, interviewees emphasized the importance of immediately speaking directly with the specialist (e.g., the neurointerventionalist), who will make the decision about care rather than going through the transfer center. One emergency physician reported that calling the transfer center at the comprehensive stroke center was tedious and potentially introduced delays for patients who may need endovascular management. As a result:
“The stroke [coordinator]... just gave the direct line to interventionalist, so I go ahead and call up one directly. [The interventionalists] call the transfer center and if you do that, it goes really quickly.”
-Emergency physician; Facility B.
Quality of Communication
Transferring ED staff cited the number of conversations required with the receiving transfer center staff as potentially impeding rapid transfer. Additional conversations could result in communication with staff who were unaware of the urgency of the situation or even basic information about the patient:
“If I feel like that message is being missed, then [ ] I’ll tell the transfer center that from the beginning, that I consider this an emergency.”
-Neurologist; Facility B.
“Oftentimes we end up giving report twice...Sometimes I give report to the transfer center and it stops there. Other times I give a brief report to the transfer center and then we have to call either the ER or the unit to give report essentially a second time.”
-ED Nurse; Facility A.
Post-Event Communication
The lack of knowledge of outcomes for their patients was consistently identified by staff at all three transferring EDs as problematic. To the extent that transferring staff received feedback it was typically negative. However, when provided, even negative feedback was a source of clinical education and ongoing process improvement. :
“Sometimes we do [hear feedback] and we always recognize that, don’t expect any feedback unless you screwed up. We’re resolved to that.”
-Emergency physician; Facility C.
Not all feedback to referring EDs was negative. Transferring ED staff identified benefits of receiving feedback:
“It’s random I feel like. We don’t get notified by every patient, but here and there we’ll receive notification about it, which is very rewarding.”
-ED Nurse; Facility A.
“That’s the only way something’s going to change, because otherwise we don’t know if what we did affected the care or not.”
-Emergency physician; Facility B.
Resources
The final theme (Supplemental Table 3) we identified from interviews involves the human and physical resources used in the acute care of stroke patients. Human resources refers to staff such as unit clerks, nurses, and physicians, who are involved in a patient’s acute stroke care. Interviews identified that the experience level of the human resources, the number and availability of team members, and skill level were important characteristics in acute stroke care. In particular, the flexibility of staff, especially nurses, and their ability to stop what they were doing to help out was also seen as an essential characteristic necessary to delivering timely care to patients with AIS:
“My experience here has been, you get something like...possible stroke, everybody stops what they’re doing if it’s not emergent and runs and helps to move everybody along. To get the patient taken care of.”
- ED nurse; Facility C.
The presence and subsequent use of physical resources was also identified as important to the timeliness of transferring ED care. In particular, equipment used to transmit patient records between facilities could potentially be a facilitator or a barrier of timely care:
“If we’re transferring a patient and we’ve already uploaded it, the doctors have an opportunity to review all the imaging and some of the records before they even get there.”
- ED nurse; Facility B.
“There always seems to be issues with the fax machine. It seems like we could use some other sort of technology at this point.”
-Emergency physician; Facility C.
DISCUSSION
As care for AIS rapidly advances, inter-facility transfer will play an integral role in patients accessing high quality and timely stroke care. To our knowledge, this is the first qualitative evaluation to identify themes of barriers and facilitators that exist in the provision of acute care to stroke patients at EDs frequently requiring inter-facility transfer. A qualitative analysis is essential because although prior research has identified inter-facility transfer delays and their clinical consequences, there is a less developed understanding of how and why the delays occur. Qualitative research captures the dynamics that underlie observed differences and, as such, provides a set of mechanisms to test in future quantitative work. Specifically, this study has four important findings for enhancing the timeliness of inter-facility stroke transfers. First, inter-facility transfer for patients with AIS is a complex process that requires substantial coordination and preparation between agencies and facilities. Second, staff reported that prior experiences with other organizations can build ongoing relationships that are particularly important in the efficiency at the moment of transfer. Third, communication, particularly post-event patient outcome reporting may be important for ongoing process improvement and staff satisfaction. Finally, the availability and flexibility of human and physical resources to diagnose and transfer AIS patients are important considerations.
As our interviewees detailed, coordination prior to, during, and after a time-sensitive emergency like AIS among these potentially disparate organizations was an essential element to ensure timely transfer and high quality care. In fact, the study of coordination among different departments, organizations, and roles, is well-recognized as affecting organizational quality and timeliness. Specifically, “relational coordination,”8 is a well-established theory in the field of organizational behavior and highly relevant to inter-facility transfers of patients with AIS. Specifically, relational coordination entails the frequency, timeliness, accuracy, and problem solving nature of communication as well as the quality of relationships between clinical staff and providers which entails a focus on shared goals, shared knowledge, and mutual respect between. AHRQ recognizes relational coordination as a conceptual model to guide development, implementation, and evaluation of care coordination interventions.9 Gittell and colleagues have found that higher levels of relational coordination interactions are associated with improved patient outcomes, higher quality of care, lower nurse turnover, and reduced hospital and intensive care unit length of stay.10–14 Moreover, enhanced relational coordination may also explain why some health care systems have outperforming systems of care for other time-sensitive emergencies (e.g., ST-elevation myocardial infarction).15 For example, emergency physicians acknowledged that teleneurology enhanced the quality of interaction with their consulting neurologists by recognizing individuals and associating this familiarity with diagnostic preferences.
Among all three EDs in this study, there was a lack of clarity about when to initiate a protocol (e.g., vague symptoms) or when a patient with AIS may be eligible for endovascular treatment. Emergency physicians cited this uncertainty as creating confusion about the acute diagnostic evaluation of these patients and reflecting an absence of well-developed protocols. While standards exist for the management of AIS patients and protocols are commonly in place to streamline care of these patients, the challenge identified is the specificity and flexibility of these protocols. For example, providing guidance on key steps such as the use of angiographic imaging in AIS work-up. Rather than the ED attempting to anticipate the consultant’s recommendations as occurs frequently in other time-sensitive emergencies (e.g., consideration of an aortic dissection in the setting of an ST-elevation myocardial infarction), emergency physicians frequently cited the need and desire for the stroke neurologist to be actively involved in the selection of diagnostic and therapeutic options. As some clinicians noted, this approach resulted in piecemeal evaluations of patients with suspected AIS and substantial delays as patients return from radiology receiving a non-contrasted head CT only to return for subsequent angiographic imaging.
Our findings related to the directness and quality of communication mirror the attributes of communication encapsulated by the communication elements (e.g., communication accuracy) of relational coordination. Our findings related to prior experience suggest how these experiences can both create clear expectations and build relationships between individuals from distinct organizations that smooth coordination and are consistent with the relational components (e.g., shared knowledge and mutual respect) of relational coordination. Future research can more directly assess relational coordination using established measures and link it to the effectiveness and timeliness of inter-facility AIS transfers.
Interviewees identified the value of post-event communication about the patient’s clinical and operational (e.g., arrival-to-tPA) outcomes, but that feedback rarely reached the transferring ED providers. Consistent with other studies on patient feedback, ED providers rarely hear about patient outcomes despite the perceived value to staff and clinicians.16,17 In fact, feedback is recognized as highly important to the improvement of stroke systems of care. Feedback by itself may be effective at reducing door-to-needle times,18 and is recognized as one of the 10 key strategies to reduce door-to-needle times for the administration of thrombolysis in the American Heart Association/American Stroke Association’s Target: Stroke initiative.19
This work identifies six potential opportunities to enhance the timeliness of inter-facility transfer of patients with AIS (see Table 3). First, effective protocol development requires interdisciplinary coordination to develop a workflow that is resilient to process breakdown. Iterative development is necessary to refine and develop a finalized protocol that is successfully implemented. Second, processes developed or refined should emphasize simplicity by reducing the number of steps transferring facilities face and accommodate atypical presentations. For example, a single phone call to the comprehensive stroke center including all of the responsible physicians and staff (e.g., vascular neurologist, intensivist, and access nurse with the transferring ED physician). Third, leaders with sufficient decision-making authority (e.g., medical director or hospital administrator) should be engaged in process development and oversight of ongoing maintenance. Once protocols are developed, they should be reviewed, particularly incorporating ongoing feedback from transferring facilities to identify opportunities for further simplification. Fourth, a formal mechanism for both positive and negative feedback between facilities should be developed to encourage communication. Including the transferring ED physicians and staff along with receiving clinical staff encourages interdisciplinary and interorganizational communication. Our findings suggested at best inefficient and often nonexistent mechanisms for positive or negative feedback. Fear of potential repercussions further limited the communication of negative feedback. Fifth, measurement and reporting of operational performance and clinical outcomes should be encouraged. Improving performance is challenging without feedback grounded in actionable and specific data. Transparent communication of results should be reported to individual staff and clinicians involved in cases. Finally, ongoing education in both clinical and operational processes is needed regardless of experience level, particularly with respect to infrequently used processes. Communication was an important theme with several identified recommendations. First, post-event communication of patient outcomes represents an opportunity for inter-organizational learning and professional development that can also enhance relationships between organizations. This feedback was vital for staff in earlier stages of the AIS care to understand what happened to their patients, ongoing process improvement, and potentially bolster overall staff morale. Fostering and building such relationships also allows for the development and refinement of standards or protocols between facilities that ultimately benefit the patient by reducing the time to definitive stroke care. Our data suggest that receiving stroke centers should consider creating non-judgmental forums with transferring EDs that foster open discussion of and learning from process breakdowns or potential breakdowns. Finally, receiving hospitals should minimize the number of potential communications as these represent opportunities for redundant communication or misdirected communication that goes to individuals not sufficiently familiar with the urgency of stroke transfers, both of which unnecessarily slow transfer. Finally, consistent with prior work,20,21 flexible human and physical resources are essential to the delivering timely emergency care.
Table 3.
Opportunities identified for improvement of inter-facility transfer delays for AIS
| Strategy (Theme) | Recommendation |
|---|---|
| Collaborative Protocol Development (Historical Experiences, Processes) | Successful protocol development requires patience to iteratively develop a protocol amongst interdisciplinary clinical specialties. |
| Develop Simple Processes (Processes) | Identifying simple processes that reduce unnecessary steps (e.g., single phone call) |
| Leadership Engagement (Resources) | Leaders with authority should be involved in process redesign and ongoing maintenance. |
| Feedback Mechanism (Historical Experiences, Communication) | Formal mechanisms to deliver both positive and negative feedback between clinical disciplines and organizations should be developed. |
| Measure and Report (Communication) | When possible, quantify and trend performance and clinical outcomes. |
| Education (Processes and Communication) | Identify opportunities for staff and provider education for operational workflow and clinical learning. Recognize that these are ongoing learning challenges that may need to be refreshed. |
LIMITATIONS
Our findings should be considered in light of the study’s limitations. First, while we used three distinct EDs, these interviews were conducted in the southeastern region of the U.S., also known as the “stroke belt.” This area has an unusually high incidence of stroke,22 making this region particularly important to ongoing efforts to improve the quality of stroke care. Second, our findings reflect the perceived influence of each theme on timeliness and subsequent patient outcomes. Future research will need to directly link these themes to observed outcomes. Third, interviews are potentially subject to recall bias potentially limiting the accuracy of recalled events. Nevertheless, this work provides several key insights to further guide examination, development, and improvement of stroke systems of care.
CONCLUSIONS
Inter-facility transfer of patients with AIS is a complex process requiring timely, highly coordinated efforts among multiple healthcare organizations including hospitals and EMS agencies. Efforts to enhance intra- and inter-organizational coordination through high quality and learning-oriented communication, recurring relationships, and consistent feedback represent potentially modifiable source of intervention for improving the quality and timeliness of care.
Supplementary Material
Acknowledgments
Financial Support: Dr. Ward is supported by NIH K23 HL127130. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. All authors had full access to all the data in the study and had final responsibility for the decision to submit for publication. Dr. Froehler is supported by funding from NIH/NINDS, Medtronic, Stryker, and Microvention. He is also a consultant for Medtronic, Stryker, Balt USA, Viz AI, Control Medical, and Neurvana.
Footnotes
Conflicts of Interest: None
Conference Presentation: This work was presented at the International Stroke Conference on January 25, 2018
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Wardlaw JM, Murray V, Berge E, del Zoppo GJ. Thrombolysis for acute ischaemic stroke. Cochrane Database Syst Rev. 2014;7:CD000213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Powers WJ, Rabinstein AA, Ackerson T, et al. 2018 Guidelines for the Early Management of Patients With Acute Ischemic Stroke: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke. 2018;49(3):e46–e110. [DOI] [PubMed] [Google Scholar]
- 3.Adeoye O, Albright KC, Carr BG, et al. Geographic access to acute stroke care in the United States. Stroke. 2014;45(10):3019–3024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Froehler MT, Saver JL, Zaidat OO, et al. Interhospital Transfer Prior to Thrombectomy is Associated with Delayed Treatment and Worse Outcome in the STRATIS Registry. Circulation. 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ng FC, Low E, Andrew E, et al. Deconstruction of Interhospital Transfer Workflow in Large Vessel Occlusion: Real-World Data in the Thrombectomy Era. Stroke. 2017;48(7):1976–1979. [DOI] [PubMed] [Google Scholar]
- 6.Edmondson AC. Learning from mistakes is easier said than done: Group and organizational influences on the detection and correction of human error. The Journal of Applied Behavioral Science. 2004;40(1):66–90. [Google Scholar]
- 7.Donabedian A The quality of care. How can it be assessed? JAMA. 1988;260(12):1743–1748. [DOI] [PubMed] [Google Scholar]
- 8.Gittell JH. Supervisory span, relational coordination and flight departure performance: A reassessment of postbureaucracy theory. Organ Sci. 2001;12(4):468–483. [Google Scholar]
- 9.McDonald KM, Sundaram V, Bravata DM, et al. Closing the quality gap: a critical analysis of quality improvement strategies (Vol. 7: Care Coordination; ). 2007. [PubMed] [Google Scholar]
- 10.Baggs JG. Development of an Instrument to Measure Collaboration and Satisfaction About Care Decisions. J Adv Nurs. 1994;20(1):176–182. [DOI] [PubMed] [Google Scholar]
- 11.Baggs JG, Ryan SA, Phelps CE, Richeson JF, Johnson JE. The Association between Interdisciplinary Collaboration and Patient Outcomes in a Medical Intensive-Care Unit. Heart Lung. 1992;21(1):18–24. [PubMed] [Google Scholar]
- 12.Gittell JH. Coordinating mechanisms in care provider groups: Relational coordination as a mediator and input uncertainty as a moderator of performance effects. Management Science. 2002;48(11):1408–1426. [Google Scholar]
- 13.Shortell SM, Zimmerman JE, Rousseau DM, et al. The performance of intensive care units: does good management make a difference? Med Care. 1994;32(5):508–525. [DOI] [PubMed] [Google Scholar]
- 14.Gittell JH, Fairfield KM, Bierbaum B, et al. Impact of relational coordination on quality of care, postoperative pain and functioning, and length of stay: a nine-hospital study of surgical patients. Med Care. 2000;38(8):807–819. [DOI] [PubMed] [Google Scholar]
- 15.Shah R, Goldstein SM, Unger BT, Henry TD. Explaining Anomalous High Performance in a Health Care Supply Chain*. Decision Sciences. 2008;39(4):759–789. [Google Scholar]
- 16.Lavoie CF, Plint AC, Clifford TJ, Gaboury I. “I never hear what happens, even if they die”: a survey of emergency physicians about outcome feedback. CJEM. 2009;11(6):523–528. [DOI] [PubMed] [Google Scholar]
- 17.Le Grand Rogers R, Narvaez Y, Venkatesh AK, et al. Improving emergency physician performance using audit and feedback: a systematic review. Am J Emerg Med. 2015;33(10):1505–1514. [DOI] [PubMed] [Google Scholar]
- 18.Ghrooda E, Alcock S, Jackson AC. Improvement in thrombolytic therapy administration in acute stroke with feedback. Can J Neurol Sci. 2012;39(6):789–792. [DOI] [PubMed] [Google Scholar]
- 19.Fonarow GC, Smith EE, Saver JL, et al. Improving door-to-needle times in acute ischemic stroke: the design and rationale for the American Heart Association/American Stroke Association’s Target: Stroke initiative. Stroke. 2011;42(10):2983–2989. [DOI] [PubMed] [Google Scholar]
- 20.Laker LF, Froehle CM, Lindsell CJ, Ward MJ. The flex track: flexible partitioning between low- and high-acuity areas of an emergency department. Ann Emerg Med. 2014;64(6):591–603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ward MJ, Ferrand YB, Laker LF, et al. The nature and necessity of operational flexibility in the emergency department. Ann Emerg Med. 2015;65(2):156–161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lanska DJ, Kuller LH. The geography of stroke mortality in the United States and the concept of a stroke belt. Stroke. 1995;26(7):1145–1149. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.