Abstract
Background:
Certain approaches to managing a strict gluten-free diet (GFD) for celiac disease (CD) may lead to impaired psychosocial well-being, diminished quality of life (QOL) and disordered eating. This study aimed to understand adolescents’ approaches to managing a GFD and the association with QOL.
Methods:
Thirty adolescents with CD (13–17 years old) following the GFD for at least one year completed the Celiac Dietary Adherence Test (CDAT) and QOL survey. Their approaches to GFD management were explored using a semi-structured interview, where key themes were developed using an iterative process, and further analyzed using a psychosocial rubric to classify management strategies and QOL. CDAT ratings were compared across groups.
Results:
GFD management strategies were classified onto a 4-point scale. Adaptive eating behaviors were characterized by greater flexibility (vs rigidity), trust (vs avoidance), confidence (vs controlling behavior) and awareness (vs preoccupation with) maintaining a GFD. Approximately half the sample (53.3%) expressed more maladaptive approaches to maintaining a GFD and those who did so were older with lower CD-specific pediatric quality of life (CDPQOL) scores, mean subscale differences ranging from 15.0 points for Isolation (t = 2.4, p = 0.03, df = 28) to 23.4 points for Limitations (t = 3.0, p = 0.01, df = 28).
Conclusions:
Adolescents with CD who manage a GFD with maladaptive eating behaviors similar to known risk factors for feeding and eating disorders experience diminished QOL. Per CD management recommendations, we recommend ongoing follow-up with gastroenterologists and dietitians, and psychosocial support referrals, as needed.
Keywords: childhood eating behaviors, eating disorders, coeliac disease, quality of life
Introduction
Celiac Disease (CD) is a multisystem autoimmune disorder that damages the small intestine and is triggered by dietary gluten, the main protein found in wheat, barley, and rye.1 CD affects approximately 1% of the US population.2 Current treatment for CD requires strict avoidance of all foods that contain gluten.3 For those with CD, exposure to even a small amount of gluten may cause a range of symptoms3–5 and complications including anemia, osteoporosis, and cancer.6, 7 Observational studies using duodenal mucosal healing as a marker of adherence, suggest that adherence to a strict gluten-free diet (GFD) can help to decrease symptoms and risk of long-term complications.8, 9
Maintaining the GFD requires increased control around food including monitoring of food labels, avoiding unsafe grains, and detailed questioning to avoid cross-contact with gluten containing foods. These constraints can be hard to accept and follow, especially for adolescents, an age group typically burdened by acute concern regarding fitting in with peers, wanting to feel normal, and gluten-free food displeasure.10–14 Adherence and self-advocacy are particularly problematic for adolescents as they venture outside of the home and become more independent.13–14 The focus on food and eating behaviors, and possibly even adherence to a gluten-free diet, may be associated with an increased risk of psychosocial problems and disordered eating patterns and behaviors in adolescents with CD.15–21
A spectrum of behavioral health difficulties exists of feeding and eating disorders.21 Disordered eating behaviors include dieting, purging, binge eating, fasting and the use of excessive physical activity to control weight and/or body shape.21–24 While healthy eating patterns fluctuate based on factors such as food availability and proximity, fluctuation to the point of nutrient deficiency or excess weight change, indicate disordered eating.21–25 Planning and preparing food should not dominate thoughts and dictate behaviors above and beyond that of other daily activities.24 Recent research on disordered eating in CD indicates that both extreme GFD adherence and dietary transgressions are associated with disordered eating patterns.26–32 For those who fail to adhere to their GFD, the challenges of managing the GFD may lead to restrictive or bulimic eating behaviors.31–33 For those who are extremely adherent to the GFD, anxiety around gluten cross-contamination may lead to limited food choices or eating only in situations with complete control over food preparation, which may mimic disordered eating.21,27,34,35 Patterns of cognition and behavior that cause individuals to become socially isolated, to refuse attendance at social events involving food or to avoid eating in settings outside the house, a marked interference with psychosocial functioning, can be considered disordered.22 Currently there is limited description of how individuals adhere to the GFD.
In a prior study, we found that hypervigilance to a strict GFD among adults with CD correlated with diminished quality of life (QOL); the relationship was present, but less robust among adolescents.36 In the present study our objective was to analyze data from a semi-structured interview describing adolescent approaches to managing a strict GFD, and to identify associations between these approaches and CD-specific pediatric quality of life (CDPQOL). The interview explored barriers and facilitators to adhering to a strict GFD. An inductive content analytic approach was used to identify management approaches which might affect QOL. These data will help to inform future nutrition education strategies which can promote a strict GFD while maximizing QOL for adolescents with CD.
Materials and methods
Recruitment36
Data were collected in the course of a cross-sectional prospective study of both adults (n = 50) and adolescents (n = 30) with CD. The present analysis is restricted to the adolescent subgroup (13–17 years old). The study was conducted at the Celiac Disease Center in New York City at the Columbia University Medical Center. Adolescents, who were no older than 17 years at enrollment, with a self-reported duodenal biopsy-confirmed diagnosis of CD, in accordance with US guidelines37 at least one year prior to enrollment and willing to participate in three visits (the first one in-person and two subsequent ones by telephone) over a one-month period were included. Exclusions included: 1) CD diagnosis < 1 year prior to enrollment; 2) serum or self-diagnosed CD (without biopsy); and 3) age < 13 years old. Completers received a $25 Amazon gift card.
Enrollment was between March and August 2016. Our target enrollment was 30 adolescents. Those affiliated with the Celiac Disease Center of Columbia University (~5000 members: those interested in CD, including a mix of patients and family members) were emailed to ascertain interest in the study. There were two additional follow-up emails. Among the 45 adolescents who responded to the email invitation, 15 were ineligible (11 lacked duodenal biopsy to confirm CD; 3 never scheduled an appointment) and 30 were eligible and enrolled.
Demographic and medical history variables36
Gender (male, female), age, self-described race (White, African-American, Asian, Other), self-described ethnicity (Hispanic, non-Hispanic), zip code of home residence, and education (highest level/grade achieved) were assessed. Medical history included self-reported height, weight, and years since CD diagnosis.
Celiac disease pediatric specific quality of life38
CDPQOL was evaluated with a 17-item validated survey instrument.38 Participants responded to Likert scales questions ranging from 0 = Never to 4 = Almost Always. Answers were transformed and combined, obtaining four subscales and a Total score. Social items (n = 7) measured how much respondents feel misunderstood, are a burden, and self-esteem. Uncertainty items (n = 3) measured how much they worry about their future, college, and getting older with CD. Isolation items (n = 4) measured how much participants feel different from their friends and family because of their CD diagnosis. Limitation items (n = 3) measured how much they feel nervous about eating at friends’ homes or avoid parties. Higher CDPQOL scores indicated better QOL, where the possible overall score range was 0 to 100.
Gluten-free diet (GFD) adherence and symptoms39
Dietary adherence was measured using the Celiac Dietary Adherence Test (CDAT). The CDAT is a 7-item validated, self-administered, survey instrument that includes two items about persistent symptoms (i.e.; headaches and low energy) and 5 items about attitudes and behaviors related to gluten exposure (including one item that specifically asks about frequency of eating gluten on purpose). Total scores range from 7 to 35, higher scores implying worse adherence to the GFD. Total scores > 13 indicate poor adherence.39 The symptoms subscale ranges from 2 to 10, with a higher score implying worse symptoms. Eating gluten on purpose scores ranged from 1 to 5, higher scores implying worse adherence to the GFD. Three 24-h dietary recalls were also collected over a 1-month period and reviewed for quantity and frequency of intentional or unintentional gluten exposure by determining level of vigilance36 (e.g., asks thorough questions when dining out, has eliminated cross-contamination potential in kitchen, review of diet reveals no obvious gluten sources, etc.) each recorded on a 6 point Likert scale ranging from 1 (excellent adherence) to 6 (not following a gluten-free diet, GFD). Those that received an excellent adherence score for all three days of 24h dietary recalls were considered to be ‘extremely vigilant’ (i.e., only scores of 1 for all categories). All others were considered to be ‘less vigilant’ (scores of 2 – 6 for any of the categories on any of the three days of 24-h dietary recalls).
Adaptive and maladaptive eating patterns
As no tools are available to assess eating patterns in CD, a semi-structured interview was used to explore key themes concerning the management of the GFD. Adolescents were asked: 1) What do you see as the major challenges to following a strict GFD? 2) What do you see as the things that help make it easy to follow a strict GFD? Prompts to elicit clarity were offered, including to understand motivations, as appropriate. At the end of each interview, adolescents were given the opportunity to discuss other issues, apart from their parents, including intentional gluten consumption. Interviewers hand transcribed detailed notes during the interview. Interview responses formed the basis of our classification of eating behaviors as described below.
Data analysis
Analysis of quantitative data
Frequencies and percentages are presented for categorical variables, means and standard deviations for continuous data. Differences by gender and percentage Extremely Vigilant between eating behavior groups were assessed with chi-squares tests. Differences by continuous variables (i.e.; age, BMI, CDPQOL and CDAT) were assessed with one-way analyses of variance and t-tests. As appropriate, comparisons of continuous variables were repeated using ANCOVA to control for age at enrollment. The program SPSS 19.0 (IBM Corp., Armonk, NY, USA) for Windows was used for analysis.
Qualitative analysis of adaptive and maladaptive eating classification scheme
Consistent with Fade and Swift (2011),40 responses to the semi-structured interviews were read repeatedly by the first author and inductively coded on paper copies first literally, then into interpretative themes. Key themes were developed into a framework for coding the entire dataset. To enhance reliability, the coding process and emerging themes were discussed among the authors until consensus was achieved. A decision trail was used to ensure transparency.
The analysis of the semi-structured interview data was guided by a psychosocial rubric previously used to identify management strategies and disordered eating in patients with diabetes41 (See Supplementary Material for Coding Matrix). Individuals were classified as having adaptive or maladaptive eating thoughts and behaviors. Adaptive eating behaviors were characterized by greater flexibility, trust, confidence and a less active focus on maintaining a GFD (i.e.; acceptance vs preoccupation). Maladaptive eating behaviors were characterized by greater rigidity, avoidance, controlling behavior and preoccupation with maintaining a GFD.
Participants were classified into four groups by two researchers who were blinded to the CDPQOL scores. Group 1) described only adaptive eating behaviors; Group 2) those who expressed mostly adaptive behaviors, with a few maladaptive behaviors; Group 3) expressed several maladaptive behaviors, with few adaptive behaviors; and Group 4) had mostly maladaptive behaviors. One of the interviewers had participated in the original interviews. Discrepancies between the two coders were resolved by discussion and review of 24-h dietary recall, if needed.
Ethical approval
The Institutional Review Boards at both Teachers College, Columbia University and the Columbia University Medical Center approved this study. Written consent was obtained from all participants.
Results
Characteristics of study sample by eating behavior groups
All (30) participants [80% female; mean (SD) age 15.6 (1.5) yrs] completed the study. Roughly half of adolescents (53.3%, n=16) were classified as having maladaptive eating behaviors (i.e.; Groups 3 & 4, see Table 1). Maladaptive eating behavior was associated with increased age at study enrollment (16.4 (1.0) yrs vs 14.7 (1.5) yrs, t = −3.6, df = 1, p = 0.001). Neither age at diagnosis nor BMI was associated with maladaptive eating behavior. There was no significant relationship between gender and eating behavior group.
Table 1:
Age and BMI by Eating Behavior
| Most Adaptive n = 7 | Adaptive n = 7 | Maladaptive n = 11 | Most Maladaptive n = 5 | TOTAL n = 30 | Linear trend* | Adaptive vs Maladaptive** n = 14 vs 16 | |||
|---|---|---|---|---|---|---|---|---|---|
| n (%) | n (%) | n (%) | n (%) | χ2 | p | χ2 | p | ||
| Female | 5 (71.4) | 6 (85.7) | 8 (72.7) | 5 (100.0) | 24 (80.0) | 0.6 | .43 | 0.0 | .86 |
| Male | 2 (28.6) | 1 (14.3) | 3 (27.3) | 0 (0.0) | 6 (20.0) | ||||
| Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | F | p | t | p | |
| Age at CD diagnosis (yrs) | 9.4 (4.6) | 9.8 (4.3) | 8.7 (4.6) | 12.6 (6.4) | 9.8 (4.8) | 0.9 | .35 | −.2 | .88 |
| Age at enrollment (yrs) | 14.7 (1.7) | 14.7 (1.3) | 16.1 (1.1) | 17.0 (0.6) | 15.6 (1.5) | 13.0 | .001 | −3.6 | .001 |
| BMI kg/m2 | 18.6 (2.8) | 19.8 (2.4) | 21.0 (1.6) | 19.7 (2.8) | 20.0 (2.4) | 1.1 | .30 | −1.6 | .11 |
Linear trend χ2 and F, both df = 1
Most adaptive + Adaptive vs Maladaptive + Most maladaptive, χ2 with continuity correction df = 1; t-test df = 28
CDPQOL, symptoms and adherence by eating behavior groups
Table 2 presents the relationships between CDPQOL, CDAT scores, eating behavior status and level of strict adherence.
Table 2:
| Most Adaptive n = 7 | Adaptive n = 7 | Maladaptive n =11 | Most Maladaptive n =5 | TOTAL n = 30 | Linear trend* | Adaptive vs Maladaptive n = 14 vs 16 t-test** ANCOVA*** | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | F | p | t | p | F | p | |
| CDPQOL | |||||||||||
| TOTAL | 76.9 (12.5) | 81.9 (11.5) | 61.4 (12.2) | 63.5 (14.8) | 70.1 (14.9) | 7.0 | .01 | 3.9 | .001 | 6.4 | .02 |
| Social | 77.0 (15.3) | 79.1 (16.4) | 63.0 (12.2) | 62.9 (19.3) | 70.0 (16.3) | 4.5 | .04 | 2.8 | .01 | 1.9 | .18 |
| Uncertainty | 79.8 (15.1) | 79.8 (22.0) | 56.8 (16.2) | 66.7 (11.8) | 69.2 (19.2) | 4.1 | .05 | 3.3 | .003 | 4.6 | .04 |
| Isolation | 76.8 (12.9) | 87.5 (13.0) | 66.5 (16.1) | 68.8 (29.0) | 74.2 (18.6) | 2.0 | .17 | 2.4 | .03 | 3.4 | .08 |
| Limitations | 73.8 (27.4) | 83.3 (12.7) | 55.3 (23.7) | 55.0 (19.2) | 66.1 (24.2) | 4.5 | .04 | 3.0 | .01 | 5.2 | .03 |
| CDAT | |||||||||||
| Overall | 9.3 (1.7) | 10.0 (1.5) | 10.9 (2.2) | 10.2 (2.9) | 10.2 (2.1) | 0.9 | .34 | −1.4 | .17 | 1.2 | .28 |
| Headaches & Low Energy | 3.4 (1.0) | 3.1 (1.1) | 4.1 (0.9) | 4.6 (2.7) | 3.8 (1.4) | 3.1 | .09 | −1.9 | .06 | 0.4 | .54 |
| Eaten Gluten on Purpose | 1.1 (0.4) | 1.3 (0.5) | 1.0 (0.0) | 1.0 (0.0) | 1.1 (0.3) | 1.7 | .20 | 2.0 | .05 | 2.9 | .10 |
| n (%) | n (%) | n (%) | n (%) | n (%) | χ2 | p | χ2 p**** | ||||
| Extremely vigilant | 1 (14.3) | 1 (14.3) | 4 (36.4) | 1 (20.0) | 7 (23.3) | 0.5 | .47 | 0.4 .51 | |||
Higher CDPQOL sub-scores and overall scores suggest higher degree of QOL; Scales 0 – 100.
Higher CDAT scores suggest lower adherence
Linear trend χ2 and F, both df = 1, χ2 with continuity correction
Most adaptive + Adaptive vs Maladaptive + Most maladaptive, t-test df = 28
Most adaptive + Adaptive vs Maladaptive + Most maladaptive, controlling for age at enrollment, Main Effects F, df = 1
Most adaptive + Adaptive vs Maladaptive + Most maladaptive, χ2 with continuity correction, df = 1.
Total CDPQOL score was positively associated with eating behavior status (linear trend F = 7.0, df = 1, p = 0.01), as was the Social subscale (linear trend F = 4.5, df = 1, p = 0.04), Uncertainty subscale (linear trend F = 4.1, df = 1, p = 0.05) and Limitations subscale (linear trend F = 4.5, df = 1 p = 0.04). In each case, maladaptive eating was associated with diminished CDPQOL. Though the linear trend for the Isolation subscale did not attain significance (F = 2.0, df = 1, p=0.17), the pattern of means was consistent with that of the other subscales. The two maladaptive eating behavior groups had a lower Total and CDPQOL subscale scores than the two adaptive eating behavior groups and the differences in mean scores, ranging from 15.0 for Isolation to 23.4 for Limitations.
Since CDPQOL of scores tended to be negatively correlated with age at enrollment (CDPQOL subscale scores Social: r = −.51, p =0.004, Uncertainty: r = −.42, p = 0.020, Isolation: r = −.25 p = 0.19, Limitations: r = −.31, p = 0.10, TOTAL: r = −.49, p = 0.006), the two group comparisons were repeated using ANCOVA. Significant differences remained after controlling for age at enrollment for CDPQOL subscale scores Uncertainty (Main Effects F = 4.6, df = 1, p = 0.04), Limitations (Main Effects F = 5.2, df = 1, p = 0.03) and TOTAL (Main Effects F = 6.4, df = 1, p = 0.02).
The CDAT total score did not differ by eating behavior group. However, the 2-item Headache and Low Energy subscale score trended toward being worse (i.e., higher) in the Maladaptive groups (t = −1.9, p = 0.06) while the single item about eating gluten on purpose was significantly better (i.e. lower) (t = 2.0 p = 0.05). The maladaptive groups had a higher percentage of the extremely vigilant (31.3% vs 14.3%), but as there were only seven extremely vigilant participants, the difference was not significant (χ2 = 0.5, p = 0.47).
Qualitative assessment of adaptive and maladaptive eating characteristics
Flexibility vs rigidity
Adolescents with adaptive eating behaviors expressed flexibility in their approach to maintaining a GFD, were able to find acceptable gluten free options when eating outside the home and felt confident to try new restaurants or food products that could accommodate their needs (“Gotten a lot easier over the years”). They used problem-focused coping strategies to reduce the risk of gluten contamination in a variety of settings. By contrast, adolescents with maladaptive eating behaviors were rigid in their GFD management, rarely willing to experiment with new restaurants or new food products (“I will only eat at trusted places”). While these strategies ensured the avoidance of gluten, they did not remove the source of distress.
Trust vs avoidance
For adolescents with adaptive eating behaviors, the ability to trust others ensured inclusion in social events and maintenance of the GFD. These adolescents, while aware of gluten cross-contamination, managed this risk by asking questions and trusting the responses. They used external resources to help maintain their GFD (“I order GF and say it’s for CD,” “Great Aunt makes sure I have something to eat – GF brownies, desserts – will call and ask if there is something that I want in particular”). In contrast, adolescents with maladaptive eating behaviors were heavily burdened by cross-contamination concerns when dining outside the home (“I worry about being out and being contaminated”), and anxiety and fear were prevalent in new situations. To manage, one adolescent said, “I won’t tell people I have celiac disease … will offer to cook” preferring the safety of her own preparations; some would refuse to eat outside the home (“Don’t go out to eat because of GF”). These adolescents controlled the risk of gluten contamination by using emotion-focused and internalizing approaches, such as not attending school team/sporting functions involving food (“Ended up having to skip a summer program – there would be no GF assistance”) and thoughts of family gatherings were angst filled (“I dread Thanksgiving”).
Confidence vs controlling behavior
Adolescents with adaptive eating behaviors had confidence in their ability to advocate for themselves and to maintain the GFD (“I use an index card with all the information”). If necessary, they would consume naturally gluten-free foods (“I bring my own fruit”, “chips, soda are fine”). They maintained a large social network of friends, classmates, family and others, who they made aware of their CD status, and who often advocated on their behalf (“My parents cook from scratch”, “Friends keep GF food for me”). In contrast, adolescents with maladaptive eating behaviors reported not informing their social network of their CD diagnosis or gluten-free requirements (“Hard going out with friends when dining out”). They internalized their coping and did not use sources of support around them to maintain the GFD (“Don’t eat others cooking”, “Stick to prepackaged food”). Instead, they felt a need to be in control of food situations and expected to inspect the kitchens where food would be prepared (“Have to go to restaurants on my downtime to take time to talk with the manager/chef”). They monitored food preparation and would visit or call restaurants in advance, thoroughly interview the staff on gluten cross-contamination measures (“A hawk – I notice everything in preparation”). For some, the perceived lack of control when eating outside the home often meant refusing events involving food and using avoidance strategies to manage their GFD (Strictly GF home – no one allowed to bring anything gluten into home”).
Awareness vs preoccupation
For adolescents with adaptive eating behaviors, maintaining a GFD was important but did not dominate daily thoughts outside of meal times (“Restaurant – not trustworthy – they’ll be wrong about stuff and don’t understand – but I’m still nice about it”). They reported becoming more aware of the GFD and how to manage it and reflected on the “increasing amount of gluten-free products.” These adolescents were still aware of the risks of cross-contamination when eating outside the home (“Restaurants can make stupid mistakes”), but accepted cross-contamination incidents and learned from them. By contrast, adolescents with maladaptive eating behaviors were preoccupied with future eating options (“I do a lot of research”, “You’re always planning your meal”), spending hours researching locations or using internet forums or mobile applications to determine whether a restaurant might be acceptable (“Look up restaurants ahead of time”). Some would make sure to eat before they went outside the home, and when cross-contamination did occur outside the home, were upset and dwelled on the incident (“I was upset that the [restaurant] staff not knowledgeable”). See Supplementary Materials, Table 4, for a summary of the various eating behavior patterns and representative quotes.
Discussion
Adolescents with CD develop different approaches to managing a GFD and different eating behaviors. Maladaptive eating behaviors associated with GFD management (i.e.; those characterized by rigidity, avoidance, controlling behavior and preoccupation) were reported by about half (53.3%) of our study sample. These maladaptive eating behaviors were described more often by older adolescents and were associated with diminished QOL. While maladaptive eating behavior rates remain unknown, research suggests that adolescents with autoimmune disorders with a digestive component, such as CD, are at significantly increased risk of developing an eating disorder.31 Estimates of adolescents with CD having or being affected by eating disorders are as high as 30%.19
At present, it is unclear how GFD management approaches develop. Factors to consider in the development of maladaptive eating patterns include personality attributes, self-efficacy and ease of adapting to challenging situations, internality, coping strategies, CD and GFD knowledge of both self and others, and environmental and social support.11,35,42–44 In addition, level of adherence to the GFD may also be a trigger.20 Regardless of their specific antecedents, CD-related maladaptive eating behaviors deserve consideration. The relationships we have described between specific eating behavior patterns and CDPQOL can help inform the development of interventions to promote GFD adherence while preserving QOL.
All adolescents in this study recognized the health benefits of maintaining a GFD. Several described symptoms (both gastrointestinal and non-gastrointestinal) when exposed to gluten, but for most, these symptoms had not occurred recently. While those in the maladaptive groups reported a significantly lower frequency of intentional gluten exposure, all groups had means closer to 1 (no exposure) than to 2 (1 – 2 times in the past month) indicating good GFD management. Percentage of hypervigilance to gluten adherence, though more than double in the maladaptive group, was not significantly different. Again, we were constrained by a small sample size. The issue is worth further research, as the trend is consistent with recent findings in another highly adherent adolescent population.48 While the total CDAT score did not differ across eating behavior groups, the symptom-related items trended worse among the maladaptive groups. A measure of symptoms and perceived severity when gluten exposure occurs may have been more differentiating.
Adolescents with maladaptive eating behaviors described a more emotion-focused and internalizing approach, expressed being nervous or anxious, spending a lot of time considering options, and relying on their own best judgment rather than involving others. These characteristics have striking similarities to personality and temperamental traits of those deemed to be at risk of diagnosable eating disorders; i.e. neuroticism, perfectionism, and obsessiveness.21 In comparison, adolescents with more adaptive eating behaviors expressed a more problem-focused approach to maintaining the GFD. They relied on eating choices that tended to be naturally gluten-free or used techniques, like carrying instruction cards for restaurants to describe dietary restrictions. Their approach was more externalizing, allowing others to assist and advocate for them.
Adolescents with maladaptive eating behaviors tended to be older [16.4 (1.0) yrs vs 14.7 (1.5) yrs] and older subjects tended to have lower CDPQOL scores. Older adolescents most likely have more occasion to navigate social situations involving eating outside of the home. With the onset of adulthood comes increased responsibility for self-management.47
We believe our findings that maladaptive eating behaviors were associated with lower quality of life scores were not only statistically significant, but clinically meaningful, as well. For the adult version of the Celiac-Disease Quality of Life (CD-QOL) instrument,49 a difference of approximately 10 points on the CD-QOL scale was suggestive of clinical significance. A decline in 10 points on the CD-QOL scale was shown to be enough to move individuals into a worse category of self-rated health, psychological distress, functional status, or pain.49 For the adolescent version, there is no published data on the clinical significance of differences in the life CDPQOL scores. However, adolescents from the same population as the current study who participated in a later pilot study were asked (in addition to the CDPQOL items) to self-rate their quality of life (QOL) related to their CD on a scale of 1 = Poor, 2 = Fair, 3 = Good, 4 = Very Good or 5 = Excellent. Total CDPQOL and subscale scores were all linearly related across these self-rating categories. Most adolescents fell into the Excellent to Very Good range and average mean differences in CDPQOL scores between the Excellent and Very Good groups were generally about 15–20 points. In the current study, the differences in means between the two maladaptive eating behavior groups were also on the order of 15–20 points. Thus, we feel confident that our findings suggest not just statistical significance, but clinical meaning as well.
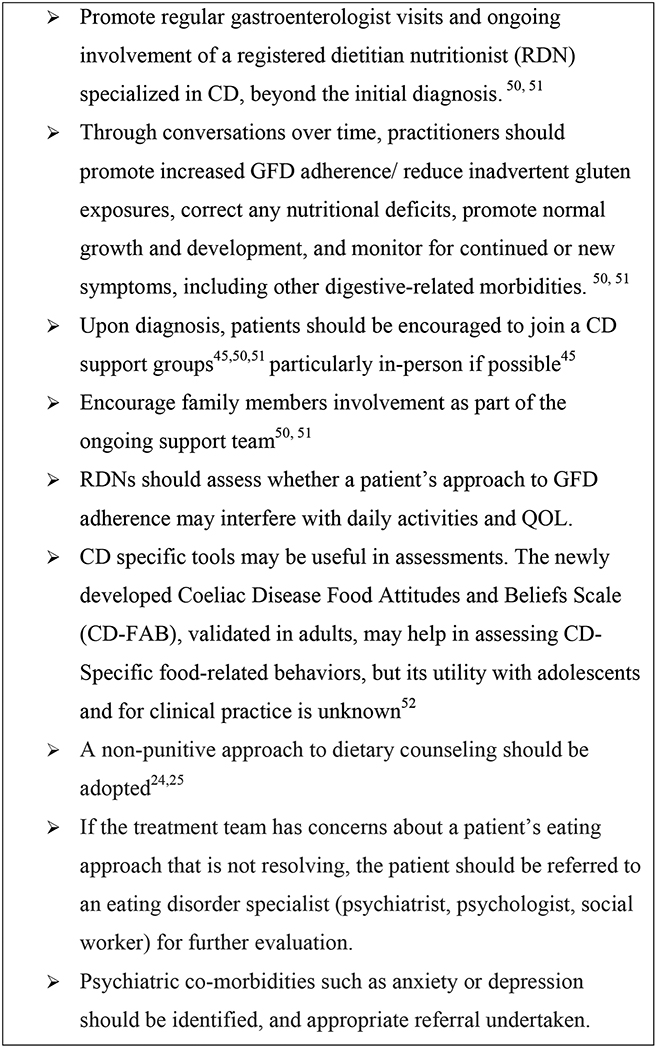
Until research determines the exact “strictness” of the GFD that will ensure healing of the mucosal lesion, CD patients will continue to be advised to maintain a strict GFD. The current guidance for periodic visits should be in accordance with current CD management recommendations.50,51 Trained CD-specialist dietitians can assist with this counseling,50,51 with possible referrals to psychotherapist to rule out eating concerns, including Avoidant/Restrictive Food Intake Disorder.21 Encouraging family participation in care, including joining in person CD support groups, may help.45, 50,51 Consideration may be given to CD specific tools.52 Parents, physicians and dietitians can all play a role in supporting positive eating behaviors and attitudes.12,18,19,45–47,50,51 (See Figure 1)
Figure 1.
Considerations for prevention of eating difficulties in adolescents with celiac disease
Limitations
This cross-sectional cohort study, investigating data from a larger study at an urban referral center,36 presents results on a fairly homogenous sample. Findings may not be generalizable. Recall bias is inherent in the items that the participants choose to self-report. Participants did not necessarily offer responses that addressed all dimensions of our eating behavior classification rubric; a structured interview may have allowed finer distinctions. Observational studies are another option for future research. Small sample size may have limited our ability to determine significance in certain results. Our symptom measure was based on just two items from the self-administered CDAT. A more extensive questionnaire on symptoms would have been preferable. Personality traits, parental psychosocial difficulties, including anxiety and depression, perceptions of costs and knowledge, as well as a diagnosable feeding or eating disorder, may also play a role in the relationship between eating behaviors and QOL, but were not measured in this study.21,46 Despite these limitations, to the authors knowledge, this is the first mixed methods analysis that describes the approach towards maintaining a GFD, highlighting the need for additional eating behavior research among adolescents with CD.
Conclusion
Roughly half (53.3%) of the adolescents with CD in this study, expressed maladaptive eating behaviors in managing a GFD. Maladaptive eating behaviors were characterized by rigidity, avoidance, controlling behavior and preoccupation, all known risk factors for the development of diagnosable eating disorders. Maladaptive behaviors in this study sample were associated with diminished CDPQOL. Practitioners should encourage patients and their families to pursue on-going follow-up with themselves as well as a trained CD-specialized dietitian to promote GFD adherence to a GFD in a way that promotes higher QOL with positive behavioral approach to GFD management, providing psychosocial support, as warranted. Early intervention may prevent further complications. Our results highlight the vulnerability of adolescent CD patients as they transition into adulthood47 when they may seek less medical care for their CD. It is in this transition period, while being susceptible to the aggravation of maladaptive eating patterns, that support may be most needed.
Supplementary Material
Acknowledgements
The authors are grateful to Shari Keats for her help in classification of the adolescents.
Conflict of interests and funding
The authors JC, RW, AL, PZ, NR, JS, and RS declare that they have no conflicts of interest to disclose. PG serves on the Advisory board of ImmusanT, Cellimmune and ImmunogenX. BL serves as a consultant for Takeda and serves on the Advisory Board of Innovate Biopharmaceuticals
Funding support provided by the Provost Investment Fund at Teachers College Columbia University. This publication was also supported by the National Center for Advancing Translational Sciences, National Institutes of Health, through Grant Number UL1TR000040. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Footnotes
Transparency Declaration
The lead author affirms that this manuscript is an honest, accurate, and transparent account of the study being reported. The reporting of this work is compliant with STROBE53 guidelines. The lead author affirms that no important aspects of the study have been omitted and that any discrepancies from the study as planned have been explained.
Supporting Information
Coding Matrix. Table 4. Lived experience patterns and quotes by eating behavior
References:
- 1.Lebwohl B, Sanders DS, Green PHR (2018) Coeliac disease. Lancet 391, 70–81. [DOI] [PubMed] [Google Scholar]
- 2.Rubio-Tapia A, Ludvigsson JF, Brantner TL et al. (2012) The prevalence of celiac disease in the United States. Am J Gastroenterol 107, 1538–1544. [DOI] [PubMed] [Google Scholar]
- 3.Green PH, Cellier C (2007) Celiac disease. N Engl J Med 357, 1731–1743. [DOI] [PubMed] [Google Scholar]
- 4.Green PH (2005) The many faces of celiac disease: clinical presentation of celiac disease in the adult population. Gastroenterology 128, S74–78. [DOI] [PubMed] [Google Scholar]
- 5.Barratt SM, Leeds JS, Sanders DS (2013) Factors influencing the type, timing and severity of symptomatic responses to dietary gluten in patients with biopsy-proven coeliac disease. J Gastrointestin Liver Dis 22, 391–396. [PubMed] [Google Scholar]
- 6.Green PH, Fleischauer AT, Bhagat G et al. (2003) Risk of malignancy in patients with celiac disease. Am J Med 115, 191–195. [DOI] [PubMed] [Google Scholar]
- 7.Meyer D, Stavropolous S, Diamond B et al. (2001) Osteoporosis in a north american adult population with celiac disease. Am J Gastroenterol 96, 112–119. [DOI] [PubMed] [Google Scholar]
- 8.Lebwohl B, Granath F, Ekbom A et al. (2013) Mucosal healing and risk for lymphoproliferative malignancy in celiac disease: a population-based cohort study. Ann Intern Med 159, 169–175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mearin ML (2007) Celiac disease among children and adolescents. Curr Probl Pediatr Adolesc Health Care 37, 20. [DOI] [PubMed] [Google Scholar]
- 10.Ludvigsson JF, Agreus L, Ciacci C et al. (2016) Transition from childhood to adulthood in coeliac disease: the Prague consensus report. Gut 65, 1242–1251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wagner G, Berger G, Sinnreich U et al. (2008) Quality of life in adolescents with treated coeliac disease: influence of compliance and age at diagnosis. J Pediatr Gastroenterol Nutr 47, 555–561. [DOI] [PubMed] [Google Scholar]
- 12.Biagetti C, Gesuita R, Gatti S et al. (2015) Quality of life in children with celiac disease: A paediatric cross-sectional study. Dig Liver Dis 47, 927–932. [DOI] [PubMed] [Google Scholar]
- 13.Olsson C, Lyon P, Hörnell A et al. (2009) Food that makes you different: the stigma experienced by adolescents with celiac disease. Qual Health Res 19, 9. [DOI] [PubMed] [Google Scholar]
- 14.Rosen A, Ivarsson A, Nordyke K et al. (2011) Balancing health benefits and social sacrifices: a qualitative study of how screening-detected celiac disease impacts adolescents’ quality of life. BMC Pediatr 11, 32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chauhan JC, Kumar P, Dutta AK et al. (2010) Assessment of dietary compliance to gluten free diet and psychosocial problems in Indian children with celiac disease. Indian J Pediatr 77, 649–654. [DOI] [PubMed] [Google Scholar]
- 16.Mazzone L, Reale L, Spina M et al. (2011) Compliant gluten-free children with celiac disease: an evaluation of psychological distress. BMC Pediatr 11, 46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bellini A, Zanchi C, Martelossi S et al. (2011) Compliance with the gluten-free diet: the role of locus of control in celiac disease. J Pediatr 158, 463–466 e465. [DOI] [PubMed] [Google Scholar]
- 18.Wagner G, Zeiler M, Berger G et al. (2015) Eating Disorders in Adolescents with Celiac Disease: Influence of Personality Characteristics and Coping. Eur Eat Disord Rev 23, 361–370. [DOI] [PubMed] [Google Scholar]
- 19.Karwautz A, Wagner G, Berger G et al. (2008) Eating pathology in adolescents with celiac disease. Psychosomatics 49, 399–406. [DOI] [PubMed] [Google Scholar]
- 20.Ludvigsson JF, Lebwohl B, Chen Q et al. (2018) Anxiety after coeliac disease diagnosis predicts mucosal healing: a population-based study. Aliment Pharmacol Ther 48, 1091–1098. [DOI] [PubMed] [Google Scholar]
- 21.American Psychiatric Association (2013) Diagnostic and statistical manual of mental disorders, 5 ed Arlington, VA: American Psychiatric Association, 335–345. [Google Scholar]
- 22.Grilo C (2012) Eating and weight disorders. New York, NY: Psychology Press: [Google Scholar]
- 23.Arigo D, Anskis AM, Smyth JM (2012) Psychiatric comorbidities in women with celiac disease. Chronic Illn 8, 45–55. [DOI] [PubMed] [Google Scholar]
- 24.Rosen DS (2003) Eating disorders in children and young adolescents: etiology, classification, clinical features, and treatment. Adolesc Med Clin 14, 49–59. [PubMed] [Google Scholar]
- 25.Freeland-Graves JH, Nitzke S, Academy of N et al. (2013) Position of the academy of nutrition and dietetics: total diet approach to healthy eating. J Acad Nutr Diet 113, 307–317. [DOI] [PubMed] [Google Scholar]
- 26.Leffler DA, Dennis M, George JBE et al. (2007) The interaction between eating disorders and celiac disease: an exploration of 10 cases. Eur J Gastroenterol Hepatol 19, 251–255. [DOI] [PubMed] [Google Scholar]
- 27.Satherley R, Howard R, Higgs S (2015) Disordered eating practices in gastrointestinal disorders. Appetite 84, 240–250. [DOI] [PubMed] [Google Scholar]
- 28.Passananti V, Siniscalchi M, Zingone F et al. (2013) Prevalence of eating disorders in adults with celiac disease. Gastroenterol Res Pract 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mårild K, Størdal K, Bulik CM et al. (2017) Celiac Disease and Anorexia Nervosa: A Nationwide Study. Pediatrics 139. [DOI] [PubMed] [Google Scholar]
- 30.Hommer RE, Swedo SE (2017) Anorexia and Autoimmunity: Challenging the Etiologic Constructs of Disordered Eating. Pediatrics 140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zerwas S, Larsen JT, Petersen L et al. (2017) Eating Disorders, Autoimmune, and Autoinflammatory Disease. Pediatrics 140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Golden NH, Park KT (2017) Celiac Disease and Anorexia Nervosa-An Association Well Worth Considering. Pediatrics 139. [DOI] [PubMed] [Google Scholar]
- 33.Satherley RM, Howard R, Higgs S (2016) The prevalence and predictors of disordered eating in women with coeliac disease. Appetite 107, 260–267. [DOI] [PubMed] [Google Scholar]
- 34.Sverker A, Hensing G, Hallert C (2005) ‘Controlled by food’- lived experiences of coeliac disease. J Hum Nutr Diet 18, 171–180. [DOI] [PubMed] [Google Scholar]
- 35.Schebendach JE, Mayer LE, Devlin MJ et al. (2008) Dietary energy density and diet variety as predictors of outcome in anorexia nervosa. Am J Clin Nutr 87, 810–816. [DOI] [PubMed] [Google Scholar]
- 36.Wolf RL, Lebwohl B, Lee AR et al. (2018) Hypervigilance to a Gluten-Free Diet and Decreased Quality of Life in Teenagers and Adults with Celiac Disease. Dig Dis Sci 63, 1438–1448. [DOI] [PubMed] [Google Scholar]
- 37.Hill ID, Dirks MH, Liptak GS et al. (2005) NASPGHAN Guideline for the diagnosis and treatment of celiac disease in children: recommendations of the North American Society for Pediatric Gastroenterology, Hepatology and Nutrition. J Pediatr Gastroenterol Nutr 63, 156–165. [DOI] [PubMed] [Google Scholar]
- 38.Jordan NE, Li Y, Magrini D et al. (2013) Development and validation of a celiac disease quality of life instrument for North American children. J Pediatr Gastroenterol Nutr 57, 477–486. [DOI] [PubMed] [Google Scholar]
- 39.Leffler DA, Dennis M, Edwards George JB et al. (2009) A simple validated gluten-free diet adherence survey for adults with celiac disease. Clin Gastroenterol Hepatol 7, 530–536, 536 e531–532. [DOI] [PubMed] [Google Scholar]
- 40.Fade SA, Swift JA (2011) Qualitative research in nutrition and dietetics: data analysis issues. J Hum Nutr Diet 24, 106–114. [DOI] [PubMed] [Google Scholar]
- 41.May M, Fletcher M (2012) Eat what you love, love what you eat, with diabetes: a mindful eating program for thriving with prediabetes or diabetes. Oakland, CA: New Harbinger Publications, Inc. [Google Scholar]
- 42.Bulik CM (2002) Eating disorders in adolescents and young adults. Child Adolesc Psychiatr Clin N Am 11, 201–218. [DOI] [PubMed] [Google Scholar]
- 43.Smith MM, Goodfellow L (2011) The relationship between quality of life and coping strategies of adults with celiac disease adhering to a gluten-free diet. Gastroenterol Nurs 34, 460–468. [DOI] [PubMed] [Google Scholar]
- 44.Roma E, Roubani A, Kolia E et al. (2010) Dietary compliance and life style of children with coeliac disease. J Hum Nutr Diet 23, 176–182. [DOI] [PubMed] [Google Scholar]
- 45.Lee AR, Wolf R, Contento I et al. (2016) Coeliac disease: the association between quality of life and social support network participation. J Hum Nutr Diet 29, 383–390. [DOI] [PubMed] [Google Scholar]
- 46.Esenyel S, Unal F, Vural P (2014) Depression and anxiety in child and adolescents with follow-up celiac disease and in their families. Turk J Gastroenterol 25, 381–385. [DOI] [PubMed] [Google Scholar]
- 47.Reilly NR, Hammer ML, Ludvigsson JF et al. (2016) 35 Transition of Care in Celiac Disease: Adolescent to Adult Care. Gluten Intake is Common, and Follow Up is Poor. Gastroenterology 150. [Google Scholar]
- 48.Tokatly Latzer IT, Lerner-Geva L, Stein D et al. (2018) Disordered eating behaviors in adolescents with celiac disease. Eat Weight Disord. 10.1007/s40519-018-0605-z [epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 49.Dorn SD, Hernandez L, Minaya MT et al. The development and validation of a new coeliac disease quality of life survey (CD-QOL). Aliment Pharmacol Ther 31, 666–675. [DOI] [PubMed] [Google Scholar]
- 50.Ludvigsson JF, Bai JC, Biagi F et al. (2014) Diagnosis and management of adult coeliac disease: guidelines from the British Society of Gastroenterology. Gut 63, 1210–1228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Rubio-Tapia A, Hill ID, Kelly CP et al. (2013) ACG clinical guidelines: diagnosis and management of celiac disease. Am J Gastroenterol 108, 656–676; quiz 677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Satherley RM, Howard R, Higgs S (2018) Development and Validation of the Coeliac Disease Food Attitudes and Behaviours Scale. Gastroenterol Res Pract 2018, 6930269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.von Elm E, Altman DG, Egger M et al. (2007) The strenthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. PLos Med 4, e296. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.