Abstract
Background:
Normalized truncated navicular height (NTNH) is a non-invasive, easy to perform, and simple clinical measure of static foot posture. However, its sensitivity and specificity in evaluation of the static foot posture in children have not been investigated yet.
Objective:
To investigate the intra-rater reliability, sensitivity, and specificity of NTNH in evaluation of the static foot posture in children using radiographic measure as a gold standard measure.
Methods:
A cross-sectional study of a random sample of 300 school children aged 6–12 years old. Intra-rater reliability, minimal detectable change, sensitivity, and specificity of NTNH were investigated. NTNH as a clinical measure of static foot posture was calculated and compared to the radiographic measure and displayed on the receiver operating characteristic (ROC) curve.
Results:
NTNH demonstrated an intra-rater reliability of . The sensitivity and specificity of NTNH were 88.1% and 99.5%, respectively. The optimal cutoff point for the diagnosis of flat foot using NTNH in children aged 6–12 years is NTNH .
Conclusion:
NTNH is a sensitive and specific measure of static foot posture in the children aged 6–12 years. It is recommended to be used as a screening measure of static foot posture in children as it is easy, simple to perform, and a non-invasive clinical measure.
Keywords: Reliability, sensitivity, specificity, normalized truncated navicular height, foot posture, children
Introduction
Foot is a very complex structure that has to function as a rigid lever during the push-off phase of locomotion, while the foot needs to be pliable for shock absorption. The interaction that creates functional adaptability is accomplished by means of alignment of the bones, muscles, and tendons. The foot bones move in a triplanar direction to accomplish the locking and unlocking of the foot structure. The complexity of the foot makes the investigation thereof challenging.1
Medial longitudinal arch (MLA) is one of the most important foot structures related to these actions because it participates in the absorption of ground forces and as a result MLA height could be used for the evaluation of foot posture.2 Without this arched configuration, the transmitted forces at the foot would exceed the physiological weight bearing capabilities of the tarsal bones.3 The height of MLA has been considered to be a relevant factor in injuries in the lower extremity.4,5
Foot posture refers to a combination of static and dynamic measurements of the foot in order to describe the foot in an overarching fashion, relating the static foot measurements with the dynamic foot function.6 Foot posture is therefore related to the anatomy of the foot as well as to its functional role. The MLA is a critical variable in determining the foot posture.7
There is no single definitive method used in the literature to evaluate foot posture.8 There are two types of measurements used in the evaluation of static foot posture; either direct or indirect measurements. Direct measurements include radiographic or ultrasound evaluation.9 Indirect measurements include visual observation,10 rear foot angle measurements,11 navicular tuberosity measurements,12 and footprint parameters.13 Many parameters can be obtained from the footprints, including arch angle (AA), arch index (AI), Chippaux–Smirak Index (CSI),14 and Staheli Index (SI).15
Radiographic techniques are regarded as the gold standard measure for assessing the skeletal alignment of the foot in a static weight bearing position. So, it can be used for the validation of the clinical measures of static foot posture.16-18
Validity of clinical assessment measures can be defined as an evidence that a clinical measurement technique actually measures what it is supposed to measure. Thus, it is clear that validity is a fundamental prerequisite for the usefulness of a clinical measurement technique.19
Sensitivity and specificity are important measures of validity of a test. Sensitivity of a test is defined as its ability to obtain a positive result when the individual is truly diseased. Specificity of a test is defined as its ability to obtain a negative result when the individual is a truly non-diseased.20
In fact, the radiographic measures have specific limitations such as the harmful risk of radiation exposure especially for the pediatric population, the cost, and the need for specialized practitioners. So, the development of an inexpensive, simple, non-invasive, reliable, and valid clinical method for the evaluation of static foot posture that could be used instead of the more invasive and sophisticated radiographic measures is essential not only for clinical practice, but also for the research work.21
The major drawback for the researchers is that the available literature about validating the clinical measures of static foot posture is limited. Furthermore, some studies had investigated young to middle-aged adults or older populations,13,16,18,22,23 while others had studied children of certain age using only one clinical assessment measure.24 So, these results cannot assumed to be equally valid nor standardized for the pediatric population as the pediatric foot undergoes several age-related changes till it reaches full skeletal maturation.
Normalized truncated navicular height (NTNH) is a non-invasive, easy to perform, and simple clinical measure of static foot posture.18 However, its sensitivity and specificity in evaluation of the static foot posture in children have not been investigated yet. Therefore, this study aimed to investigate the intra-rater reliability, sensitivity, and specificity of NTNH in the children aged 6–12 years.
Methods
Sample size calculation
The sample size was calculated with a confidence level of 95% [at 5% type-1 error ()], power level of 80%, a precision of % and a standard deviation (SD) of navicular height (NH) () obtained from a previous study26 using the below formula27:
where is the standard normal variate with a value of 1.96 [at 5% type-1 error ()], SD is the standard deviation of variable obtained from a previous literature or pilot study, and is the absolute error or precision decided by the researcher. So the sample size calculation is as follows:
A sample of 300 participants was included in the study assuming any information loss.
Participants
A random sample of 300 healthy asymptomatic (without foot or ankle pain) children aged 6–12 years was recruited from ten schools in Cairo, Egypt, using stratified random sampling method. The parents were contacted by telephone in order to confirm the agreement about participation of their children in the study and to arrange for an appointment. Before participation in the study, the children and their parents were informed about the aims, methods, and time period of the study. The parents or caregivers gave a signed informed consent for the participation of their children in the study.
The participants were excluded if they have a history of neuromuscular disorders, structural lower limb deformities, joint rheumatic pathology, history of foot or ankle injury (such as fractures, etc.), genetic conditions or syndromes affecting the gait or posture (e.g., Down syndrome ), history of major surgeries in the lower limbs, peripheral vascular disorders, history of foot or ankle surgical intervention, abnormal gait pattern, foot and ankle pain during walking, or abnormal body mass index (BMI).
The participants were stratified according to their age into two subgroups of equal size () from both sexes (male and female) in each group as follows: Group A contains participants aged 6–9 years old and group B contains participants aged between 9 years, 1 day and 12 years old. This study was conducted in accordance with the Declaration of Helsinki and was approved by Cairo University Human Research and Ethical Committee, Cairo, Egypt.
Measurement
Demographic data
Each participant was given an identity (ID) number. Participant’s age (in years), sex, height (cm), weight (kg), and body mass index (kg/m2) were obtained. Both weight and height were measured with the children’s shoes and socks removed. Body mass index was calculated using the standard Quetelet Index (body weight divided by height squared; in kg/m2).28 Only participants with normal BMI were included in this study, we had followed the BMI-based classification system of childhood obesity as proposed by the International Obesity Task Force (IOTF). IOTF developed specific percentile cutoff levels for BMI by age and sex in children. This approach is based on the fact that the BMI cutoffs define overweight and obesity in children as a function of age and sex.29 Characteristics of the study participants were displayed in Table 1.
Table 1.
Demographic characteristics of the study participants.
| Group A (6–9 years) | Group B (9 years, 1 day–12 years) | Total | |
|---|---|---|---|
| Characteristic | |||
| Age (years) | 7.95 0.92 | 10.93 0.94 | 9.44 1.76 |
| Weight (kg) | 27.53 2.40 | 37.83 4.33 | 32.68 6.23 |
| Height (m) | 1.30 0.03 | 1.45 0.07 | 1.38 0.09 |
| BMI (kg/m2) | 16.23 0.76 | 17.70 0.64 | 16.96 1.01 |
| Male | 73 (48.7%) | 75 (50%) | 148 (49.3%) |
| Female | 77 (51.3%) | 75 (50%) | 152 (50.7%) |
| Normal foot | 49 (32.7%) | 48 (32%) | 97 (32.3%) |
| Flat arched foot | 101 (67.3%) | 102 (68%) | 203 (67.7%) |
Data are presented as mean standard deviation for continuous variables and as number (percentage %) for categorical variables. BMI: body mass index.
Clinical measurements of static foot posture
Measurement of static foot posture was performed for each participant using NTNH. All clinical measurements were performed by the same examiner who was blinded to the participants’ identity.
Direct measurement of the highest point of MLA in the sagittal plane is one of the simplest methods of providing the clinician with quantifiable information regarding foot structure. The prominent navicular bone generally represents the highest point of MLA.18 With the participant standing in a relaxed position, the most medial prominence of the navicular tuberosity was palpated and marked with an ink marker pen. A steel ruler was used to measure the navicular height from the ground which is defined as the perpendicular distance from the marked navicular tuberosity to the ground.
NTNH is obtained by dividing NH by the truncated foot length (the distance from the first metatarsophalangeal joint line to the most posterior aspect of the heel)18,21 as shown in Fig. 1. The navicular height and the truncated foot length in the current study were measured in centimeters. A lower normalized navicular height ratio indicates a flatter foot. In order to address the intra-rater reliability of NTNH, clinical measurement of static foot posture for all participants was repeated one week apart.
Fig. 1.
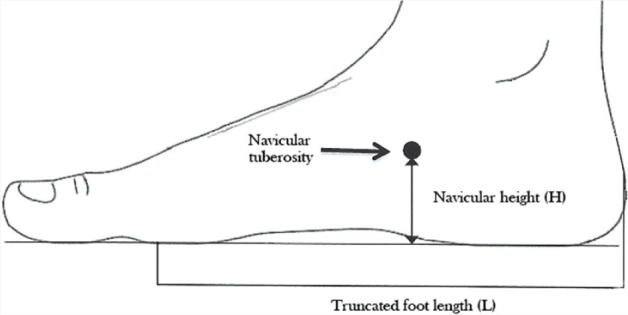
Normalized truncated navicular height calculation. : Height of the navicular tuberosity from the ground; : truncated foot length; .
Radiographic measurements
Radiographic techniques are considered as the gold standard measure for the assessment of skeletal alignment of the foot in a static weight bearing position21 for the reason that the skeletal components of MLA can be clearly imaged. Furthermore, the radiographic measurements have high reliability.22,30 Lateral radiographic view of the foot from the static weight bearing position was obtained, the calcaneal inclination angle (CIA) and talus first metatarsal angle (T1MA) were measured. These angles are chosen to represent the foot posture based on ease of measurement, good reliability, and the degree by which they reflect foot posture in the sagittal view.30
Lateral radiographic view was obtained using the standard procedures as described by Benedetti et al.31 Each participant was asked to stand with the knee extended and feet positioned in front of the cassette. The film cassette was held vertically in a groove and in contact with the medial border of the evaluated foot. A radiography tube was directed at 90∘ to the film, centered on talus and at a distance of 102 cm.
Meary’s angle or lateral view T1MA has been used to identify the apex of deformity in patients with pes cavus (high arched foot) and pes planus (flat foot) on the lateral weight bearing radiograph. It is the angle between the longitudinal axes and talus and the first metatarsal bone. In the normal weight bearing foot, the midline axis of the talus lies in line with the midline axis of the first metatarsal bone (Fig. 2), while, in the pronated foot the talar axis does not come in line with the midline axis of the first metatarsal bone. The normal reference range of Meary’s angle is between and +4∘; Meary’s angle (convex upward) indicates pes cavus; Meary’s angle (convex downward) indicates pes planus.32 The participants were classified as normal and flat arched feet according to the Meary’s angle (Table 1).
Fig. 2.
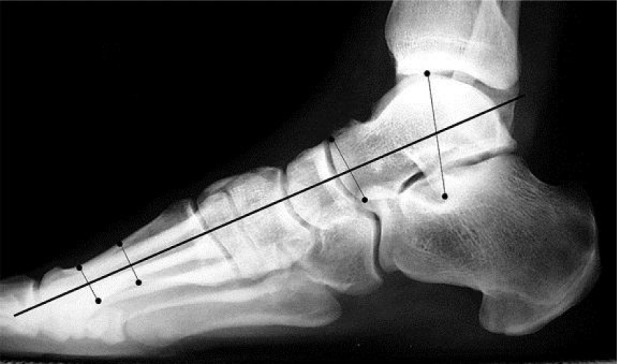
Normal weight bearing lateral view talus first metatarsal angle the talar axis comes in line with the first metatarsal axis.
After obtaining the lateral radiographic view, the X-ray film was placed on the radiographic view box. A marker pen, ruler, and a protractor marked at one degree interval were used for the angular measurements. The radiographic angular measurements were done by an experienced radiologist.
Statistical analysis
To satisfy the independence assumption of statistical analysis, only a measurement from one foot was analyzed. This was confirmed by other studies33-35 that had found no statistically relevant difference between right foot and left foot for children and adolescents as well as for adults. The right foot was chosen randomly and the measurements obtained from the right foot were analyzed for all participants.
Mean and SD were calculated for the quantitative variables, while the qualitative variables were expressed as an absolute value () and percentage (%). To determine the intra-rater reliability of NTNH, intra-class correlation coefficient (ICC) had been calculated (model 3,1) with 95% confidence interval (95%CI). Reliability was defined as excellent (0.75–1.00), good (0.60–0.74), fair (0.40–0.59), and poor ().36
The minimum detectable changes (MDCs) at 95% confidence interval (MDC) of NTNH were calculated based on the reliability analysis. The MDC is the minimal amount of change that can be considered above the threshold of error expected in measurement. The below formulas37 were used for calculation:
where SEM is the standard error of measurement, ICC is the intra-class correlation coefficient value, SD is the standard deviation, and 1.96 is the value of -score associated with 95%CI.
Using the radiographic measure of the lateral view T1MA as a gold standard measure of static foot posture, the sensitivity and specificity of NTNH were calculated for the whole group of 300 participants.
The clinical measurement results of NTNH were displayed on the receiver operating characteristic (ROC) curve and the area under the curve (AUC) was computed. The AUC varies between 0.5 and 1 and it is commonly used as an index of the test’s performance: high accuracy (), moderate accuracy (0.7–0.9), low accuracy (0.5–0.7), or a result of chance (0.5).23
Another benefit of the ROC curve is helping in identifying the optimal cutoff point by balancing the sensitivity and specificity using the Youden Index. The Youden Index () is defined as the maximum vertical distance between the ROC curve and the chance line and is calculated from the following formula28:
All statistical tests were conducted using IBM SPSS Statistics for Windows, Version 20.0 (IBM Corp., Armonk, NY). The statistical significance level was set at .
Results
Descriptive statistics for the studied clinical and radiographic measures are displayed in Table 2. Intra-rater reliability for NTNH was examined using ICC. NTNH demonstrated high intra-rater reliability with an ICC of 0.98 and 95%CI of 0.97–0.99. The SEM for NTNH was 0.005 and the MDC was 0.014 (Table 3).
Table 2.
Descriptive statistics for the clinical and radiographic measures of static foot posture.
| Group A (6–9 years) | Group B (9 years, 1 day–12 years) | ||||
|---|---|---|---|---|---|
| () | () | ||||
| Measure | Normal arched () | Flat arched () | Normal arched () | Flat arched () | Total () |
| NH (cm) | 2.4 0.52 | 1.6 0.41 | 3.5 0.61 | 2.1 0.11 | 2.4 0.41 |
| Truncated foot length (cm) | 14.2 2.22 | 14.1 1.9 | 16.8 2.13 | 17.1 2.11 | 15.5 2.09 |
| NTNH | 0.17 0.03 | 0.12 0.05 | 0.20 0.04 | 0.12 0.03 | 0.15 0.03 |
| T1MA (deg) | 2.5 1.1 | 6.5 2.3 | 3 0.90 | 7 2.2 | 2 1.62 |
Data are presented as mean standard deviation. NH: navicular height; NTNH: normalized truncated navicular height; T1MA: talus first metatarsal angle (obtained from the lateral view).
Table 3.
Intra-rater reliability, sensitivity, and specificity of normalized truncated navicular height.
| Statistical parameter | NTNH () |
|---|---|
| ICC (95%CI) | 0.98 (0.97–0.99) |
| SEM | 0.005 |
| MDC | 0.014 |
| Sensitivity (%) | 88.1 |
| Specificity (%) | 99.5 |
| AUC (95%CI) | 0.98 (0.97–0.99) |
| Cutoff point |
ICC: intra-class correlation coefficient; 95%CI: 95% confidence interval; NTNH: normalized truncated navicular height; SEM: standard error of measurements; MDC: minimal detectable change at 95%CI; AUC: area under the ROC curve.
The sensitivity and specificity of NTNH were 88.1% and 99.5%, respectively, as shown in Table 3 and are illustrated in Table 4.
Table 4.
Cross-tabulation of T1MA * NTNH for the study participants ().
| NTNH | |||||
|---|---|---|---|---|---|
| N | P | Total | |||
| T1MA | N | Count | 190 | 13 | 203 |
| % within NTNH | 99.5% | 11.9% | 67.7% | ||
| P | Count | 1 | 96 | 97 | |
| % within NTNH | 0.5% | 88.1% | 32.3% | ||
| Total | Count | 191 | 109 | 300 | |
| % within NTNH | 100.0% | 100.0% | 100.0% | ||
TIMA: talus first metatarsal angle; NTNH: normalized truncated navicular height; P: positive result (abnormal); N: negative result (normal).
From the ROC curve of NTNH (Fig. 3), the AUC was 0.98 with 95%CI of 0.97–0.99. The optimal cutoff point for the diagnosis of flat arched foot in children aged 6–12 years is NTNH (Table 3).
Fig. 3.
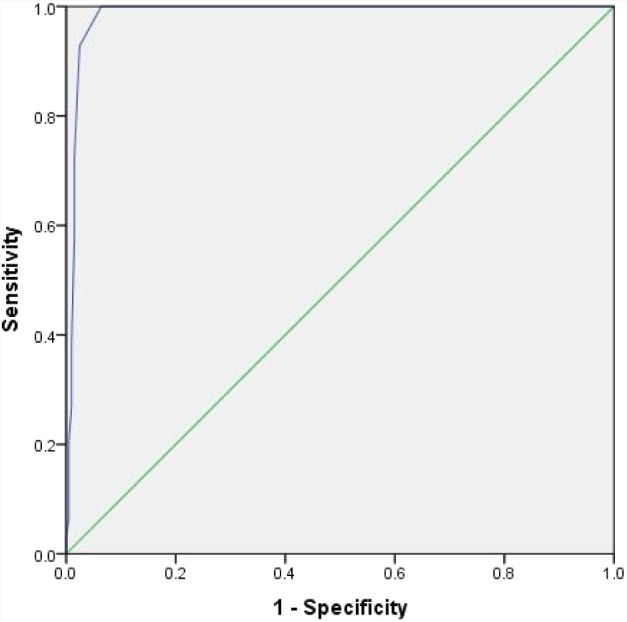
ROC curve for NTNH.
Discussion
The main purpose of this study was to investigate sensitivity and specificity of NTNH as the clinical measures of static foot posture in children aged 6–12 years using the radiographic measure as a gold standard.
The first consideration before interpreting the results of sensitivity and specificity is to discuss the intra-rater (test–retest) reliability for NTNH.
NTNH had demonstrated excellent intra-rater reliability with an ICC of 0.98 and 95%CI of 0.97–0.99. The SEM for NTNH is 0.005 that indicates high reliability because SEM is an index to measure the expected variations in the observed scores due to measurement errors when repeated over time, so, the higher the reliability, the lower the SEM.37 Moreover, the MDC for NTNH was 0.014. Thus, a change in NTNH measurement of at least 0.014 needs to occur when the test is repeated at a confidence level of 95% such that it reflects the real NTNH measurement change and not a difference expected from measurement errors.
The current study results of intra-rater reliability were inconsistent with the previous study done by Menz et al.38 in 2003; this is because they reported a moderate intra-rater reliability of normalized navicular height (NNH) with an ICC value of 0.76 in a sample of 31 participants aged 76–87 years. This could be attributed to different characteristics of the sample as they used a different age group and it is known that aging is usually associated with arthritic changes which could lead to development of foot deformities. Consequently, that should affect the foot posture.
Furthermore, Evans et al.39 had reported moderate intra-rater reliability of navicular height with an ICC of 0.69 in a sample of 10 children aged four years. This may be due to the small sample size which could have an impact on the measurement results. In addition, the variable and formative nature of the navicular bone will seem to make it a difficult structure to be used in the assessment of foot posture in four-year-old children especially if the examiner was unfamiliar with the child’s developing foot as the navicular bone is the last foot bone to ossify between the ages of 2 years and 5 years and navicular ossification is reported to occur later in boys than girls.40 So, the certainty of correctly locating the navicular tuberosity in the pre-school children sometimes is adversely affected by the local soft tissue.
Xiong et al.2 in 2010 had studied the medial longitudinal arch characteristics in a sample of adult participants from Hong Kong. They reported a good inter-rater reliability of NTNH with an ICC value of 0.9 which is consistent with the present study results.
To the best of our knowledge, there is a shortage of previous literature about the validity of clinical measures of static foot posture in children. The current study results revealed that NTNH is a sensitive and specific measure of static foot posture in children with a sensitivity of 88.1% and a specificity of 99.5%. Menze and Munteanu,18 had stated that NTNH is a valid clinical measure as it demonstrated strong correlation (-values ranges from 0.72 to 0.76) with the corresponding navicular height obtained from the radiographs in older population with a sample size of 95 participants. They based their decision upon the correlation, but they did not investigate the sensitivity, specificity, or predictive values of this clinical measure.
The ROC curve results indicates that NTNH has high accuracy level () in the assessment of static foot posture. Moreover, the current study results demonstrated that the optimal cutoff point for the diagnosis of flat arched foot in children aged 6–12 years is NTNH .
The most important findings of this study are the ability to prove that NTNH can be introduced as a sensitive, specific clinical measure of static foot posture in children as well as the ability to detect the optimal cutoff point for the diagnosis of flat arched foot in children (6–12 years) using NTNH. Given our experience to date, we believe that it is much easier, more precise, and with fewer mistakes to calculate NTNH than to measure the axis of the talus, navicular, or calcaneus bone in a radiographic X-ray film.
Study limitations
The primary limitations of the current study are that a certain age group (6–12 years) in the pediatric population was studied; only participants with normal BMI were studied; also we did not investigate the inter-rater reliability, predictive values, and likelihood ratio of NTNH as clinical measures. So, these items should be addressed in the future research.
Conclusion
NTNH is a sensitive and specific measure of static foot posture in children. Therefore, NTNH can be used clinically as a screening tool for the evaluation of static foot posture or as a part of a comprehensive foot evaluation in children.
Conflict of Interest
The authors declare that there is no conflict of interest.
Funding/Support
The authors declare that no funding was provided for this study.
Author Contributions
Hoda A. El-Talawy, Faten H. Abdelazim and Fatma A. Hegazy conceptualized the study and substantially contributed to the design of the study, revised the manuscript, and provided the final approval of the version to be published. Emad A. Aboelnasr contributed to the design of the study, collected, analyzed, and interpreted the data, drafted the manuscript and revised it critically, and provided the final approval of the version to be published.
References
- 1. Caravaggi P, Pataky T, Goulermas JY, Savage R, Crompton R. A dynamic model of the windlass mechanism of the foot: Evidence for early stance phase preloading of the plantar aponeurosis. J Exp Biol 2009;212:2491–9. [DOI] [PubMed] [Google Scholar]
- 2. Xiong S, Goonetilleke RS, Witana CP, Weerasinghe TW, Au EY. Foot arch characterization: A review, a new metric, and a comparison. J Am Podiatr Med Assoc 2010;100:14–24. [DOI] [PubMed] [Google Scholar]
- 3. Zuil-Escobar JC, Martínez-Cepa CB, Martín-Urrialde JA, Gómez-Conesa A. Reliability and accuracy of static parameters obtained from ink and pressure platform footprints. J Manipulative Physiol Ther 2016;39:510–17. [DOI] [PubMed] [Google Scholar]
- 4. Williams DS, McClay IS. Measurements used to characterize the foot and the medial longitudinal arch: Reliability and validity. Phys Ther 2000;80:864–71. [PubMed] [Google Scholar]
- 5. Queen RM, Mall NA, Hardaker WM, Nunley JA. Describing the medial longitudinal arch using footprint indices and a clinical grading system. Foot Ankle Int 2007;28:456–62. [DOI] [PubMed] [Google Scholar]
- 6. Redmond AC, Crosbie J, Ouvrier R. Development and validation of a novel rating system for scoring standing foot posture: The foot posture index. Clin Biomech 2006;21:89–98. [DOI] [PubMed] [Google Scholar]
- 7. Mathewson, E. Foot Posture in school children from the western cape: Differences between footwear use, gender and race. Doctoral dissertation. Stellenbosch: Stellenbosch University, 2016.
- 8. Stavlas P, Grivas TB, Michas C, Vasiliadis E, Polyzois V. The evolution of foot morphology in children between 6 and 17 years of age: A cross-sectional study based on footprints in a Mediterranean population. J Foot Ankle Surg 2005;44:424–8. [DOI] [PubMed] [Google Scholar]
- 9. Razeghi M, Batt ME. Foot type classification: A critical review of current methods. Gait Posture 2002;15:282–91. [DOI] [PubMed] [Google Scholar]
- 10. Dahle LK, Mueller MJ, Delitto A, Diamond JE. Visual assessment of foot type and relationship of foot type to lower extremity injury. J Orthop Sports Phys Ther 1991;14:70–74. [DOI] [PubMed] [Google Scholar]
- 11. Tsai LC, Yu B, Mercer VS, Groos MT. Comparison of different structural foot types for measures of standing postural control. J Orthop Sports Phys Ther 2006;36:952–3. [DOI] [PubMed] [Google Scholar]
- 12. Brody DM. Techniques in the evaluation and treatment of the injured runner. Orthop Clin North Am 1982;13:541–58. [PubMed] [Google Scholar]
- 13. Cavanagh PR, Rodgers MM. The arch index: A useful measure from footprints. J Biomech 1987;20:547–51. [DOI] [PubMed] [Google Scholar]
- 14. Forriol F, Pascual J. Footprint analysis between three and seventeen years of age. Foot Ankle 1990;11:101–4. [DOI] [PubMed] [Google Scholar]
- 15. Chen CH, Huang MH, Chen TW, Weng MC, Lee CL, Wang GJ. The correlation between selected measurements from footprint and radiograph of flatfoot. Arch Phys Med Rehabi 2006;87:235–40. [DOI] [PubMed] [Google Scholar]
- 16. Menz HB. Alternative techniques for the clinical assessment of foot pronation. J Am Podiatr Med Assoc 1998;88:119–29. [DOI] [PubMed] [Google Scholar]
- 17. McPoil TG, Cornwall MW, Vicenzino B, Teyhen DS, Molloy JM, Christie DS, Collins N. Effect of using truncated versus total foot length to calculate the arch height ratio. Foot 2008;18:220–27. [DOI] [PubMed] [Google Scholar]
- 18. Menz HB, Munteanu SE. Validity of 3 clinical techniques for the measurement of static foot posture in older people. J Orthop Sports Phys Ther 2005;35:479–86. [DOI] [PubMed] [Google Scholar]
- 19. Hall SJ, Getchell N. Measurement of variables in research. In Hall SJ, Getchell N (eds.). Research Methods in Kinesiology and the Health Sciences. Baltimore: Lippincott Williams & Wilkins, pp. 233–45.
- 20. Akobeng AK. Understanding diagnostic tests 1: sensitivity, specificity and predictive values. Acta Paediatr 2007;96:338–41. [DOI] [PubMed] [Google Scholar]
- 21. Murley GS, Menz HB, Landorf KB. A protocol for classifying normal- and flat-arched foot posture for research studies using clinical and radiographic measurements. J Foot and Ankle Res 2009;2:22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Saltzman CL, Nawoczenski DA, Talbot KD. Measurement of the medial longitudinal arch. Arch Phys Med Rehabil 1995;76:45–9. [DOI] [PubMed] [Google Scholar]
- 23. Pita-Fernández S, González-Martín C, Seoane-Pillado T, López-Calviño B, Pértega-Díaz S, Gil-Guillén V. Validity of footprint analysis to determine flatfoot using clinical diagnosis as the gold standard in a random sample aged 40 years and older. J Epidemiol 2015;25:148–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Targett R, Mathieson I. Evaluation of foot posture development in children between 3–11 years of age using foot posture index. J Foot Ankle Res 2010;3:17.20799935 [Google Scholar]
- 25. Waseda A, Sudaa Y, Inokuchi S, Nishiwaki Y, Toyama Y. Standard growth of foot arch in childhood and adolescent derived from measurement results of 10,155 children. Foot Ankle Surg 2014;20:208–14. [DOI] [PubMed] [Google Scholar]
- 26. Morrison SC, Durward BR, Watt GF, Donaldson MD. Prediction of anthropometric foot characteristics in children. J Am Podiatr Med Assoc 2009;99:497–502. [DOI] [PubMed] [Google Scholar]
- 27. Charan J, Biswas T. How to calculate sample size for different study designs in medical research? Indian J Psychol Med 2013;35:121–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Chang JH, Wang SH, Kuo CL, Shen HC, Hong YW, Lin LC. Prevalence of flexible flatfoot in Taiwanese school-aged children in relation to obesity, gender, and age. Eur J Pediatr 2010;169:447–52. [DOI] [PubMed] [Google Scholar]
- 29. Kêkê LM, Samouda H, Jacobs J, di Pompeo C, Lemdani M, Hubert H, Zitouni D, Guinhouya BC. Body mass index and childhood obesity classification systems: A comparison of the French, International Obesity Task Force (IOTF) and World Health Organization (WHO) references. Revue d’Epidemiologie et de Sante Publique 2015;63:173–82. [DOI] [PubMed] [Google Scholar]
- 30. Kataz MA, Davidson RS, Chan PS, Sullivan RJ. Plain radiographic evaluation of pediatric foot and its deformities. U.P.O.J 1997;10:30–39. [Google Scholar]
- 31. Benedetti MG, Berti L, Straudi S, Ceccarelli F, Giannini S. Clinicoradiographic assessment of flexible flatfoot in children. J Am Podiatr Med Assoc 2010;100:463–71. [DOI] [PubMed] [Google Scholar]
- 32. Wald S, Woerter K. Measurements and classifications in musculoskeletal radiology. Stuttgart, Germany: George Thieme Verlag, 2014, pp. 59–76. [Google Scholar]
- 33. Menz HB. Two feet or one person: Problems associated with statistical analysis of paired data in foot and ankle medicine. Foot 2004;14:2–5. [Google Scholar]
- 34. Cheng JC, Leung SS, Leung AK, Guo X, Sher A, Mak AF. Change of foot size with weightbearing: A study of 2829 children 3 to 18 years of age. Clin Orthop Relat Res 1997;342:123–31. [PubMed] [Google Scholar]
- 35. Xiong S, Goonetilleke RS, Zhao J, Li W, Witana CP. Foot deformations under different load-bearing conditions and their relationships to stature and body weight. Anthropol Sci 2009;117:77–88. [Google Scholar]
- 36. Cicchetti Domenic V. Guidelines, criteria, and rules of thumb for evaluating normed and standardized assessment instruments in psychology. Psychol Assess 1994;6:284–90. [Google Scholar]
- 37. Weir JP. Quantifying test–retest reliability using the intraclass correlation coefficient. J Strength Cond Res 2005;19:231–40. [DOI] [PubMed] [Google Scholar]
- 38. Menz HB, Tiedemann A, Kwan MM, Latt MD, Sherrington C, Lord SR. Reliability of clinical tests of foot and ankle characteristics in older people. J Am Podiatr Med Assoc 2003;93:380–87. [DOI] [PubMed] [Google Scholar]
- 39. Evans AM, Scutter SD, Iasiello H. Measuring the paediatric foot: A criterion validity and reliability study of navicular height in 4-year-old children. Foot 2003;13:76–82. [Google Scholar]
- 40. Kelikian AS, Sarrafian SK. Sarrafian’s anatomy of the foot and ankle: descriptive, topographic, functional. Lippincott Williams & Wilkins, 2011, pp 40–120.


