At the start of this century, despite tremendous efforts to promote healthcare personnel (HCP) influenza vaccination by government agencies, professional societies, and visible vaccine champions, the HCP influenza vaccination rate remained unacceptably low (~45%). Subsequently, the perception of HCP influenza immunization evolved from an employee health benefit to an important measure of a healthcare facility’s quality and patient safety program, moving an increasing number of facilities to mandate influenza vaccination. The rationale for these policies centers upon several core concepts: (1) the role HCP play in healthcare-associated pathogen transmission, (2) the lack of clear symptoms of influenza in many HCP, and (3) the vulnerability of patients to complications from influenza. Since 2005, when Virginia Mason Medical Center required influenza immunization as a condition of employment [1], leading to vaccination rates of 98.9%, more institutions have implemented similar programs [2–7], including all Veteran’s Administration hospitals in 2017 [8]. Based on an annual survey of HCP conducted by the Centers for Disease Prevention and Control, the percentage of HCP working under an employer vaccination requirement increased from 20.9% during the 2011–2012 influenza season to 44.1% during the 2017–2018 season [9]. Mandatory programs do have some implementation differences, including mask use for unvaccinated HCP during the influenza season, allowed exemptions (eg, only medical vs allowance for personal belief exemption), and consequences for noncompliance. It is important to note that although a few HCP have had their employment terminated due to vaccine refusal, the actual reported number of HCP dismissed is very small compared with the thousands of HCP encompassed by these policies.
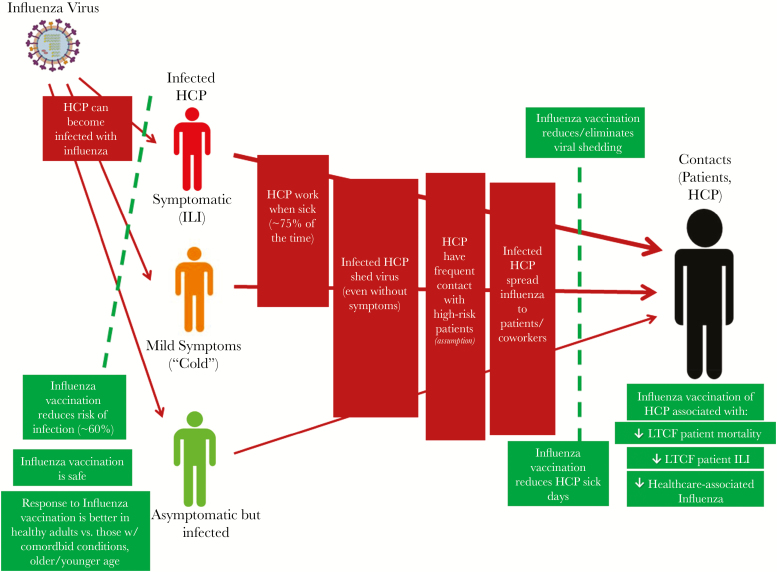
Despite a growing number hospitals with a mandatory HCP influenza vaccination policy, opposition to this patient safety strategy still occasionally emerges [10]. In this commentary, we present the rationale for HCP influenza vaccination and the supporting evidence along the “causal transmission pathway” (Figure 1) that this intervention reduces patient harm. As a part of our argument, we have made several reasonable assumptions: (1) influenza vaccine is moderately effective and safe, (2) HCP have frequent contact with persons at high risk for complications from influenza infection (ie, their patients), and (3) most HCP are (and therefore behave like) healthy adults. We will use data that examines laboratory-confirmed influenza infection but also include supporting data from HCP with influenza-like illness (ILI). We recognize the challenges of using ILI as an outcome, because many cases of ILI are not due to influenza and many cases of influenza do not result in ILI. However, data examining the behaviors of HCP surrounding ILI and associated risks have clear applicability to influenza. We also acknowledge continued challenges with mandatory policies and the continued need for advancements in the effectiveness of the vaccine and in the prevention of all healthcare-associated respiratory infections (eg, reducing presenteeism). Finally, the role of requiring influenza vaccination in healthcare settings should be considered one aspect of a global infection prevention policy that includes and does not supplant the need for hand hygiene, isolation, surveillance, etc.
Figure 1.
Causal transmission pathway for the development of healthcare-associated influenza. HCP, healthcare personnel; ILI, influenza-like illness; LTCF, long-term care facility.
HOW IS INFLUENZA TRANSMITTED, PARTICULARLY IN THE HOSPITAL SETTING?
Influenza is transmitted person-to-person, primarily via droplets, and HCP infection is the first step in the causal pathway (Figure 1). In a systematic review and meta-analysis of 29 studies encompassing 97 influenza seasons, the incidence rate (IR) of influenza among HCP was 18.7 of 100 HCP (95% confidence interval [CI], 15.8–22.1) with an IR ratio of 3.4 (95% CI, 1.2–5.7) among unvaccinated HCP [11]. Data also indicate that exposure to ill HCP and ill patients increases a hospitalized patient’s risk of developing healthcare-associated influenza (HAI). Using the clinical endpoint of ILI, Vanhems et al [12] noted that the relative risk (RR) of developing healthcare-associated ILI (HA-ILI) was significantly increased based on exposure to HCP and patients with identified ILI. Specifically, for patients exposed to at least 1 contagious HCP compared with those with no documented hospital exposure, the RR of HA-ILI was 5.48 (95% CI, 2.09–14.37); for patients exposed to at least 1 contagious patient, the RR was 17.96 (95% CI, 10.07–32.03); and for patients exposed to at least 1 contagious patient and 1 contagious HCP, the RR was 34.75 (95% CI, 17.70–68.25).
DOES INFLUENZA CAUSE ASYMPTOMATIC INFECTION AND IS THIS ASSOCIATED WITH VIRAL SHEDDING?
Once the HCP is infected with influenza, the risk of transmission to contacts increases and is based on the degree of clinical symptoms (Figure 1); however, the influenza virus can be transmitted while someone is asymptomatic or paucisymptomatic. Viral shedding is more pronounced among persons with symptoms but clearly occurs in asymptomatic individuals [13], and influenza virus is detectable in the upper airway and nasopharynx of influenza-infected persons up to several days before symptom onset. Household studies in which contacts of an influenza-infected index case are followed prospectively using symptom capture and laboratory testing can help examine secondary transmission patterns. Among a cohort of 824 households, 224 cases of secondary influenza infection were detected [14]. Viral shedding without symptoms varied by influenza strain type and was detected before onset of respiratory symptoms in influenza A-infected persons peaking within the first 2 days of clinical illness. Influenza B shedding peaked up to 2 days before symptom onset. The authors noted that “[t]he start of viral shedding before symptom onset, albeit at low levels...indicates the potential for influenza virus transmission in the pre-symptomatic phase of the illness before it becomes clinically apparent.” Another study used prospective surveillance and found viral shedding using polymerase chain reaction testing whether any signs or symptoms were reported in 14% of 59 subjects who were a household contacts of an index influenza-infected case [13]. Although influenza is clearly detectable in the nasopharynx of asymptomatic persons, there is some debate regarding the role this plays in transmission: that is, is there shedding and spread outside of the nasopharynx if no symptoms are present? However, one pragmatic nuance with this debate is that even if an asymptomatic person does not result in transmission of virus to others, the development of symptoms, even mild ones, can facilitate spread.
HEALTHCARE PERSONNEL WHO ARE INFECTED WITH INFLUENZA WILL STAY HOME FROM WORK, WON’T THEY? WHAT EVIDENCE IS THERE THAT MANDATING VACCINATION WILL AFFECT THIS?
Unfortunately, HCP presenteeism, or working while ill, occurs frequently and plays a key role in the transmission of pathogens in healthcare settings [15]. In several published surveys, approximately 75% of HCP who develop an infectious illness (ie, ILI or gastrointestinal infection) have reported working while ill [15, 16]. Data consistently show that HCP, even with classic ILI with fever, still come to work and work for an average of several days while ill [15, 17–19]. Add in the asymptomatically infected HCP, who may shed virus before symptom onset, and the practically of “just staying home once symptoms develop” falls apart. Data on the impact of mandatory influenza vaccination and HCP sick days are emerging. After the institution of a province-wide vaccination with masking policy in British Columbia, HCP absenteeism due to all-cause illness in vaccinated versus unvaccinated HCP significantly declined during the policy’s first season [20]. In a cluster randomized clinical trial, Frederick et al [21] found that among those HCP who reported at least 1 sick day, vaccinated HCP were absent significantly less when compared with unvaccinated HCP (odds ratio [OR] for 2012–2013 and 2013–2014, 0.82; 95% CI, 0.72–0.93; OR for 2014–2015, 0.81; 95% CI, 0.69–0.95).
BUT HEALTHCARE-ASSOCIATED INFLUENZA IS A VERY RARE EVENT, RIGHT?
The ultimate goal of influenza vaccination of HCP is to prevent influenza infection in their contacts, namely, patients and other HCP. Disregarding the scientific rationale that supports vaccination as a measure to prevent influenza infection and, therefore, reduce the burden of potential vectors of HAI, some opponents of mandatory HCP vaccination call for clear evidence on the impact of this outcome before advocating a mandatory stance. Comprehensive estimates of the burden of HAI have been hampered by lack of a standardized definitions, varying methods of surveillance, and lack of recognition of influenza as a cause of nosocomial respiratory disease (resulting in lack of testing for this pathogen) [22].
Fortunately, a growing evidence base notes that this outcome is more frequent than previously suspected and that HCP vaccination can prevent it. Nosocomial outbreaks are well documented in many different patient populations and clinical settings [22], and attack rates among patients and staff may be as high as 54% [23]. In many of these outbreaks, infections occurred in unvaccinated HCP, and HCP were linked epidemiologically to influenza transmission. Outbreaks have also been described when an individual or index case is minimally symptomatic [24]. Robust population-based data reinforce the impression from outbreak studies. A Canadian prospective laboratory-based surveillance program found that 17.3% of laboratory-confirmed influenza among hospitalized adults were healthcare-associated [25]. In Toronto, between 2005 and 2012, 318 nosocomial cases of influenza and 57 deaths were reported. Almost 7% were associated with outbreaks, and in these cases the case fatality rate was 18% (written personal communication, Allison McGeer [26]). In a survey of academic centers in the United States, the identified rate of HAI reported by most facilities (using only clinically collected testing as opposed to systematic surveillance and testing of all patients with new respiratory illness during their hospitalization) was comparable to previously reported rates as well as rates of other healthcare-associated infections [27]. Still, this likely underestimated the true burden of these infections.
WHAT IS THE EVIDENCE THAT MANDATORY HEALTHCARE PERSONNEL INFLUENZA VACCINATION POLICIES IMPACT HEALTHCARE-ASSOCIATED INFLUENZA AND OTHER PATIENT OUTCOMES?
We have walked through the steps of transmission of influenza in healthcare settings, from infection (even if asymptomatic) of HCP, to factors such as presenteeism that facilitate exposure to infected HCP, and to data illustrating the burden of HAI. The impact of HCP vaccination on this patient outcome has support from several key sources. Herd immunity is defined as vaccine efficacy among unvaccinated contacts [28], or, stated differently, the impact of immunization of a part of a population on the transmission and subsequent development of disease in the rest of that population. Because the immunogenicity and direct effectiveness from influenza vaccination is reduced in certain persons (eg, older adults, young children, immunocompromised individuals), vaccination of healthy adults in the population will help break the chain of transmission to all in the population. This effect from influenza vaccination has been shown in several large populations, including the vaccination of children in Japan [29] and among Hutterite colonies in Canada [30] and the subsequent impact on winter pneumonia and influenza mortality and laboratory-confirmed influenza in adults. The studies demonstrating the importance of herd immunity are often cited as rationale for HCP vaccination in hospitals, in part due to the extreme challenge of assessing this impact in an acute care setting. Many of the patients in healthcare settings may not be able to mount as robust or protective an immune response to influenza vaccine, making it important that those who can (ie, healthy adult HCP) become vaccinated to prevent spread in the population get immunized. This difference in vaccine effectiveness (VE) between HCP and their patients was nicely illustrated by Vanhems et al [31] in which VE among HCP was 89% compared with 42% in their patients.
The data also illustrate an effect on patient outcomes due to vaccination of acute care HCP. One early study demonstrated a significant correlation between increased HCP influenza vaccination rates and reduced HAI among patients [32]. The study is limited by its ecologic study design but does provide some initial suggestion of a potential impact. More recently, investigators at the MD Anderson Cancer Center examined the impact of increasing HCP influenza immunization over the course of 8 years. The proportion of influenza infections that were healthcare-associated among patients significantly decreased and was significantly associated with increased HCP vaccination rates [33]. A cluster randomized trial in the Netherlands of HCP at 6 medical centers, where the intervention arms offered vaccination to HCP versus no vaccination at control facilities, noted a significantly lower rate of HAI among internal medicine patients at the facilities with the higher (albeit still very low) rates of HCP influenza vaccination (3.9% vs 9.7% of patients) [34]. In another study encompassing 7 influenza seasons and over 62 000 hospitalized patients, a significant association was noted between increasing influenza vaccine coverage among HCP and decreasing healthcare-associated ILI among patients at an Italian acute care hospital. Specifically, as vaccination coverage dropped from 13.2% to 3.1%, the frequency of healthcare-associated ILI in patients increased from 1.1% to 5.7% (P < .001) [35]. Stevenson et al [36] examined the impact of vaccination rates on the percentage of long-term care facilities reporting an outbreak and found that if less than 25% of staff were vaccinated, close to 50% of facilities reported an outbreak. The rate of outbreaks decreased incrementally as the percentage of HCP were vaccinated, and if over 75% of HCP were vaccinated, the rate of influenza outbreaks decreased to 25%—a 50% reduction. Modeling studies have estimated that in both acute and long-term care settings, there is no HCP vaccination rate above which additional HCP vaccination coverage will not lead to further protection of patients [37, 38]. In these studies, vaccination of 100% of HCP in the acute care model resulted in a 43% reduction in the risk of influenza among hospitalized patients and a 60% risk reduction among nursing home patients. Finally, a nested case-control study in France noted a significant association between lower rates of laboratory-confirmed HAI among patients and higher (≥35%) vaccination rates among HCP [39].
It is important to acknowledge the impact of influenza vaccination among HCP practicing in long-term care settings. Higher vaccination rates of HCP have been significantly associated with reductions in patient mortality in multiple, large-scale clinical trials. Three cluster-randomized trials demonstrated that HCP vaccination was associated with a statistically significant decrease in mortality among nursing home patients [40–42]. A fourth study, conducted in France among 40 facilities that included nearly 3500 residents and 2000 HCP, revealed a significant reduction in the risk of all-cause patient mortality between the 2 study arms even after adjustment for resident age, resident vaccination status, resident disability score, and Charlson comorbidity index (OR = 0.80 in intervention arm vs control arm) [43]. Increased HCP vaccination rates also significantly correlated with reduced patient mortality rates. These investigations do have some limitations, including concerns about outcome assessment in both study arms, vaccination ascertainment in both study arms, infrequent laboratory-confirmation of influenza, and lack of a significant impact on laboratory-confirmed influenza. Nonetheless, this striking patient mortality benefit in long-term care facilities from HCP vaccination is remarkably consistent across all 4 studies. In addition, after formalized assessment and consideration of this evidence base using the Grading of Recommendations Assessment, Development and Evaluation (GRADE) approach, Ahmed et al [44] found that the pooled risk ratio for both all-cause mortality and ILI were lower and 0.71 (95% CI, 0.59–0.85) and 0.58 (95% CI, 0.46–0.73) with the use of HCP influenza vaccination. Some have argued that these studies do not provide evidence that vaccinating HCP against influenza protects patients in the acute care setting, calling for similar studies in each unique patient population. However, this stance ignores that the biological rationale for vaccination of HCP to reduce influenza spread does not vary by practice setting. Although in a long-term care setting, the interactions between HCP and patient may be more prolonged and frequent in nature, in an acute care setting, the patient has interactions with many more unique HCP, each of whom could be shedding influenza at the time of contact. Although very provocative, it should also be noted that the false claims that these studies comprise the majority of scientific rationale supporting HCP influenza vaccination policies [10] is simply untrue, as reflected by the evidence provided in this commentary and in position papers advocating such programs [45, 46].
IS THERE A CASE FOR UNIVERSAL VACCINATION OF HEALTHCARE PERSONNEL? ARE SUCH POLICIES JUSTIFIED FROM AN EPIDEMIOLOGICAL AND/OR PUBLIC POLICY PERSPECTIVE?
The impact of mandatory influenza vaccination programs clearly leads to high vaccination rates [1–3, 5–7, 47–49], and implementation of a mandatory policy (in the setting of a multifaceted influenza infection control program) is arguably the most effective strategy to increase rates above desired targets. These programs have also been associated with reductions in HCP sick days and with reductions in HAI infection among patients. The concept of requiring influenza immunization as a condition of HCP employment has now been endorsed by a growing list of professional societies and quality organizations, including every major North American infectious diseases and infection prevention organization (Table 1) [4]. In 2015, the American Nurses Association (ANA), a group that initially had not supported influenza immunization as a condition of employment, reversed their position and endorsed such a policy for the safety of HCP and their patients [50–52].
Table 1.
Selected National Organizations Recommending Healthcare Personnel Influenza Immunization as a Condition of Employment
| •American Academy of Family Physicians (AAFP) |
| •American Academy of Pediatrics (AAP) |
| •American College of Physicians (ACP) |
| •American Hospital Association (AHA) |
| •American Medical Directors Association (AMDA) |
| •American Nurses Association (ANA) |
| •American Pharmacists Association |
| •American Public Health Association (APHA) |
| •Association for Professionals in Infection Control and Epidemiology (APIC) |
| •Infectious Diseases Society of America (IDSA) |
| •National Association of County and City Health Officials (NACCHO) |
| •National Business Group on Health |
| •National Foundation for Infectious Diseases (NFID) |
| •National Patient Safety Foundation (NPSF) |
| •Society for Healthcare Epidemiology of America (SHEA) |
| •United States Department of Defense |
| •Veteran’s Health Administration (VA) |
The hallmark of determining whether a policy is impactful is to measure several different realms that may be important to the audience in question. In healthcare, this impact is commonly examined by looking at the effect on the various parties that may be affected: on patients, the HCPs, and the institution and its mission. This would be true in the setting of a policy that mandates influenza vaccination in healthcare settings. Such a policy would impact infection prevention, occupational safety, and the institution. Loeb et al [30] have argued that both interventions and assessment must be evidence based and hence reflect the best practices in medicine and science including those derived from research evaluations of the appropriate outcomes, and sometimes from a preponderance of evidence. He says that “Evidence-based infection control is...the explicit, judicious and conscientious use of current best evidence from infection control research in making decisions about the prevention and control of infection on” individuals and populations. Most institutions approach policy evaluation by examining the short, medium, and finally long-term impact. Hence, to look at a policy’s impact, an assessment would include an examination of the impact from several perspectives including the impact on the morbidity and mortality of patients, their satisfaction with their care, and the associated “costs.” An institution will also evaluate the effect on their employees and ask questions about whether a policy keeps employees safer (in this case, infection free) and healthier and whether such policies do or do not improve employee engagement and satisfaction. Finally, institutions do consider their reputation within a community and may look at the impact of a policy on perceptions of the institution.
From a societal point of view, the question is as follows: “does a policy improve public health?” Important public health measures of a policy impact include decreased morbidity, mortality, and costs. In some instances, the components of a measure may assess generalizability across multiple acute and or long-term hospitals. In addition, a societal or public health perspective may include a global assessment of the impact on the work force and determine whether influenza vaccination improved the health of a large population of workers. One framework to assess policy impact and benefits evaluates 5 key areas to assess: relevance, efficiency, efficacy, impact, and sustainability (Table 2) [53]. Such policies that mandate influenza vaccination in healthcare settings meet these criteria given the risk.
Table 2.
Framework to Assess the Effectiveness of a Public Health Policy Using Mandatory Healthcare Personnel (HCP) Influenza Vaccination as an Example
| Characteristics | Definition | Example of Impact of Mandatory Influenza HCP Vaccination Policies |
|---|---|---|
| Relevance | To determine the relevance of a mandatory influenza vaccination, assess whether the policy aligns with the priorities, strategic goals, and needs of the institution and region. Test whether the policy led to an outcome of interest. | 1. Decreases transmission of nosocomial influenza in the hospital among both patients and HCPs. 2. Decreases mortality and absenteeism could also be reasonable outcomes to consider. 3. Increases presence of HCP at work during influenza season. |
| Efficiency | Measured in several ways, including a determination of whether the policy led to the desired outcome, in a cost-effective way. | • Improves patient and HCP safety • Decreases patient readmissions • Enhances timeliness that patients are seen by maintaining a work force? • Improves patient flow through an institution by keeping workers safer and healthier? |
| Efficacy | Efficacy requires determining whether the policy lead to stated goals. | • Decreases nosocomial influenza • Decreases work absenteeism/provision of a healthier work force • Enhances environmental safety for patients by decreased transmission and acquisition of influenza? |
| Impact | Examine the positive and negative impacts of the policy. | • Decreases nosocomial influenza and patient mortality and improved HCP health? • Potentially affects employee satisfaction and may improve HCP engagement? • May or may not affect employee retention? • Provides HCPs, patients, and families with reassurance knowing the institution puts safety first. |
| Sustainability | Includes the long-term outcomes of such a policy including the impact on influenza transmission, HCP absenteeism, and HCP engagement over time. | • Includes many examples above and may be the most important of the criteria noted. |
Furthermore, Reichert et al [29] demonstrated the impact of vaccination of children on the general health and mortality of the public, especially those over the age of 65. These authors note the long-term and sustainable impact of vaccinating a cohort of individuals who will respond well to the influenza vaccine on those who may respond less well. The authors found that this policy of vaccinating children against influenza decreased deaths by 37 000–49 000. Policy reversal led to an increase in mortality in the elderly. Likewise, the impact of the policies that have increased influenza vaccination in HCPs in conjunction with a robust infection prevention program have fulfilled these criteria, leading to improved patient safety by decreasing nosocomial transmission of influenza, potentially decreasing mortality, and improving the health of HCP.
ARE THE ARGUMENTS FOR POLICIES MANDATING INFLUENZA VACCINE ETHICAL, AND HOW CAN THESE BE BALANCED AGAINST HEALTHCARE PERSONNEL AUTONOMY?
Many individuals have published discussions on the ethical arguments for mandating influenza vaccination for HCP [54–56] that are excellent summaries of the issues. Others have argued that mandatory influenza vaccination is coercive, invasive, and places patient protection above HCP autonomy [45, 57]. Although it is important to recognize these arguments, it is also important to place these arguments within the context of a HCP’s ethical duty to protect patient safety [45, 58]. This duty consists of acting in the patient’s interest, working to protect vulnerable patients, and not placing patients at undue risk of harm [45]. Furthermore, it is key to understand that up to 50% of influenza infections in HCPs are asymptomatic, paucisymptomatic, or simply unrecognized.
Along with the notion of HCP immunization as a measure of quality and safety, the view that HCP immunization aligns with and is an expected professional responsibility of HCP has also gained traction in recent years. In 2011, the American Medical Association, although not endorsing mandatory influenza immunization specifically, noted in their Code of Medical Ethics that physicians should “accept immunization absent a recognized medical, religious, or philosophic reason not to be immunized” and, if they are not immunized, to accept the decision of a “health care institution, or other appropriate authority to adjust their practice activities...(e.g., wear masks or refrain from direct patient care).” [59] The ANA notes that their members have a “professional and ethical obligation” to protect themselves and their patients and should be vaccinated against influenza in the absence of medical or religious exemptions [60]. Finally, in 2015, the National Patient Safety Foundation Board advocated for 2 “must do’s” for HCP to ensure patient safety: hand washing and HCP influenza vaccination [61].
The concern regarding HCP autotomy and the infringement on their right to choose regarding their personal health has been at the crux of the mandatory immunization debate. As noted above, in instances where the health of others may be impacted by the personal choices of the individuals, there is precedent for putting the public health above that of the individual autonomy. This has been reflected in laws prohibiting smoking in public areas to reduce the risk of second-hand exposure of others and with other immunization requirements (eg, for school entry). Healthcare personnel have other requirements as part of their occupation that may interfere with personal autonomy and freedom of choice. Surgical personnel are not allowed to perform sterile surgery wearing their street clothes due to clear safety concerns. Refusal to perform hand hygiene before patient contact is contrary to a culture of safety and would be addressed as unacceptable behaviors at many healthcare facilities. In addition, HCP are already faced with mandatory vaccination (eg, varicella) and annual invasive procedures (eg, tuberculin skin testing), and the legal precedent of mandatory vaccination is established [45, 62]. Thus, there is clear precedent in healthcare where protection of patients and other HCP overrides personal autonomy, especially when the risk of the proposed intervention to the individual is negligible. Regarding antagonism between employee and employer, evidence is mixed. Several employee unions have sued healthcare systems to end mandatory HCP influenza vaccination programs, yet surveys in several healthcare systems have shown that a majority of HCP support mandatory HCP influenza vaccination [3, 63–65].
CONCLUSIONS
In sum, the data show that influenza is common among HCP and influenza infection is frequently paucisymptomatic in this group of motivated professions whose commitment to being present is a known reality. In general, this is a healthy group who develops a robust immune response to the vaccine. Vaccination against influenza in this “herd” has been shown to protect the vulnerable, reduce nosocomial transmission of influenza, and decrease patient mortality. The ethical responsibilities of HCP require them to protect the patients under their care. These tenets have been reviewed and upheld by the most thoughtful and prestigious ethicists in healthcare. The strength of the data has led professional organizations to support the policies mandating influenza vaccine. We feel passionately that mandating influenza vaccination is part of the HCP’s personal responsibility and that these policies should be part of a comprehensive program to reduce healthcare-acquired respiratory infections. It is time to bury the hatchet on this argument, to follow the teachings from the bulk of the clinical evidence, and to embrace the importance of this policy.
Acknowledgments
Potential conflicts of interest. All authors: No reported conflicts of interest. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest.
References
- 1. Rakita RM, Hagar BA, Crome P, Lammert JK. Mandatory influenza vaccination of healthcare workers: a 5-year study. Infect Control Hosp Epidemiol 2010; 31:881–8. [DOI] [PubMed] [Google Scholar]
- 2. Babcock HM, Gemeinhart N, Jones M, et al. Mandatory influenza vaccination of health care workers: translating policy to practice. Clin Infect Dis 2010; 50:459–64. [DOI] [PubMed] [Google Scholar]
- 3. Feemster KA, Prasad P, Smith MJ, et al. Employee designation and health care worker support of an influenza vaccine mandate at a large pediatric tertiary care hospital. Vaccine 2011; 29:1762–9. [DOI] [PubMed] [Google Scholar]
- 4. Immunization Action Coalition. Honor Roll for Patient Safety Mandatory Influenza Vaccination for Healthcare Workers. Available at: http://www.immunize.org/honor-roll/. Accessed 3 January 2019.
- 5. Karanfil LV, Bahner J, Hovatter J, Thomas WL. Championing patient safety through mandatory influenza vaccination for all healthcare personnel and affiliated physicians. Infect Control Hosp Epidemiol 2011; 32:375–9. [DOI] [PubMed] [Google Scholar]
- 6. Quan K, Tehrani DM, Dickey L, et al. Voluntary to mandatory: evolution of strategies and attitudes toward influenza vaccination of healthcare personnel. Infect Control Hosp Epidemiol 2012; 33:63–70. [DOI] [PubMed] [Google Scholar]
- 7. Septimus EJ, Perlin JB, Cormier SB, et al. A multifaceted mandatory patient safety program and seasonal influenza vaccination of health care workers in community hospitals. JAMA 2011; 305:999–1000. [DOI] [PubMed] [Google Scholar]
- 8. U.S. Department of Veterans Affairs. Flu Resources for Health Professionals - Seasonal Influenza Prevention Program for VHA Health Care Personnel - Directive 1192. Available at: https://www.publichealth.va.gov/flu/professionals/index.asp. Accessed 3 January 2019.
- 9. Black CL, Yue X, Ball SW, et al. Influenza vaccination coverage among health care personnel - United States, 2017-18 influenza season. MMWR Morb Mortal Wkly Rep 2018; 67:1050–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. De Serres G, Skowronski DM, Ward BJ, et al. Influenza vaccination of healthcare workers: critical analysis of the evidence for patient benefit underpinning policies of enforcement. PLoS One 2017; 12:e0163586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Kuster SP, Shah PS, Coleman BL, et al. Incidence of influenza in healthy adults and healthcare workers: a systematic review and meta-analysis. PLoS One 2011; 6:e26239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Vanhems P, Voirin N, Roche S, et al. Risk of influenza-like illness in an acute health care setting during community influenza epidemics in 2004–2005, 2005–2006, and 2006–2007: a prospective study. Arch Intern Med. 2011; 171:151–7. [DOI] [PubMed] [Google Scholar]
- 13. Lau LL, Cowling BJ, Fang VJ, et al. Viral shedding and clinical illness in naturally acquired influenza virus infections. J Infect Dis 2010; 201:1509–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Ip DK, Lau LL, Chan KH, et al. The dynamic relationship between clinical symptomatology and viral shedding in naturally acquired seasonal and pandemic influenza virus infections. Clin Infect Dis 2016; 62:431–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Widera E, Chang A, Chen HL. Presenteeism: a public health hazard. J Gen Intern Med 2010; 25:1244–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Weingarten S, Riedinger M, Bolton LB, et al. Barriers to influenza vaccine acceptance. A survey of physicians and nurses. Am J Infect Control 1989; 17:202–7. [DOI] [PubMed] [Google Scholar]
- 17. Jena AB, Meltzer DO, Press VG, Arora VM. Why physicians work when sick. Arch Intern Med 2012; 172:1107–8. [DOI] [PubMed] [Google Scholar]
- 18. Jena AB, Baldwin DC Jr, Daugherty SR, et al. Presenteeism among resident physicians. JAMA 2010; 304:1166–8. [DOI] [PubMed] [Google Scholar]
- 19. Ng TC, Lee N, Hui SC, et al. Preventing healthcare workers from acquiring influenza. Infect Control Hosp Epidemiol 2009; 30:292–5. [DOI] [PubMed] [Google Scholar]
- 20. Van Buynder PG, Konrad S, Kersteins F, et al. Healthcare worker influenza immunization vaccinate or mask policy: strategies for cost effective implementation and subsequent reductions in staff absenteeism due to illness. Vaccine 2015; 33:1625–8. [DOI] [PubMed] [Google Scholar]
- 21. Frederick J, Brown AC, Cummings DA, et al. Protecting healthcare personnel in outpatient settings: the influence of mandatory versus nonmandatory influenza vaccination policies on workplace absenteeism during multiple respiratory virus seasons. Infect Control Hosp Epidemiol 2018; 39:452–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Voirin N, Barret B, Metzger MH, Vanhems P. Hospital-acquired influenza: a synthesis using the outbreak reports and intervention studies of nosocomial infection (ORION) statement. J Hosp Infect 2009; 71:1–14. [DOI] [PubMed] [Google Scholar]
- 23. Horcajada JP, Pumarola T, Martínez JA, et al. A nosocomial outbreak of influenza during a period without influenza epidemic activity. Eur Respir J 2003; 21:303–7. [DOI] [PubMed] [Google Scholar]
- 24. Patrozou E, Mermel LA. Does influenza transmission occur from asymptomatic infection or prior to symptom onset? Public Health Rep 2009; 124:193–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Taylor G, Mitchell R, McGeer A, et al. Healthcare-associated influenza in Canadian hospitals from 2006 to 2012. Infect Control Hosp Epidemiol 2014; 35:169–75. [DOI] [PubMed] [Google Scholar]
- 26. Characteristics of Hospital-Acquired Influenza in Adults in Southern Ontario, 2005–2012. Poster Abstract Session: Viral Infections: Epidemiology, October 10, 2014. The Pennsylvania Convention Center: IDExpo Hall BC. Available at: https://idsa.confex.com/idsa/2014/webprogram/Paper46156.html
- 27. Talbot TR, Dellit TH, Hebden J, et al. Factors associated with increased healthcare worker influenza vaccination rates: results from a national survey of university hospitals and medical centers. Infect Control Hosp Epidemiol 2010; 31:456–62. [DOI] [PubMed] [Google Scholar]
- 28. Kim TH. Seasonal influenza and vaccine herd effect. Clin Exp Vaccine Res 2014; 3:128–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Reichert TA, Sugaya N, Fedson DS, et al. The Japanese experience with vaccinating schoolchildren against influenza. N Engl J Med 2001; 344:889–96. [DOI] [PubMed] [Google Scholar]
- 30. Loeb M, Russell ML, Moss L, et al. Effect of influenza vaccination of children on infection rates in Hutterite communities: a randomized trial. JAMA 2010; 303:943–50. [DOI] [PubMed] [Google Scholar]
- 31. Vanhems P, Baghdadi Y, Roche S, et al. Influenza vaccine effectiveness among healthcare workers in comparison to hospitalized patients: A 2004-2009 case-test, negative-control, prospective study. Hum Vaccin Immunother. 2016; 12:485–90. doi:10.1080/21645515.2015.1079677 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Salgado CD, Giannetta ET, Hayden FG, Farr BM. Preventing nosocomial influenza by improving the vaccine acceptance rate of clinicians. Infect Control Hosp Epidemiol 2004; 25:923–8. [DOI] [PubMed] [Google Scholar]
- 33. Frenzel E, Chemaly RF, Ariza-Heredia E, et al. Association of increased influenza vaccination in health care workers with a reduction in nosocomial influenza infections in cancer patients. Am J Infect Control 2016; 44:1016–21. [DOI] [PubMed] [Google Scholar]
- 34. Riphagen-Dalhuisen J, Burgerhof JG, Frijstein G, et al. Hospital-based cluster randomised controlled trial to assess effects of a multi-faceted programme on influenza vaccine coverage among hospital healthcare workers and nosocomial influenza in the Netherlands, 2009 to 2011. Euro Surveill 2013; 18:20512. [DOI] [PubMed] [Google Scholar]
- 35. Amodio E, Restivo V, Firenze A, et al. Can influenza vaccination coverage among healthcare workers influence the risk of nosocomial influenza-like illness in hospitalized patients? J Hosp Infect 2014; 86:182–7. [DOI] [PubMed] [Google Scholar]
- 36. Stevenson CG, McArthur MA, Naus M, et al. Prevention of influenza and pneumococcal pneumonia in Canadian long-term care facilities: how are we doing? CMAJ 2001; 164:1413–9. [PMC free article] [PubMed] [Google Scholar]
- 37. van den Dool C, Bonten MJ, Hak E, Wallinga J. Modeling the effects of influenza vaccination of health care workers in hospital departments. Vaccine 2009; 27:6261–7. [DOI] [PubMed] [Google Scholar]
- 38. van den Dool C, Bonten MJ, Hak E, et al. The effects of influenza vaccination of health care workers in nursing homes: insights from a mathematical model. PLoS Med 2008; 5:e200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Bénet T, Régis C, Voirin N, et al. Influenza vaccination of healthcare workers in acute-care hospitals: a case-control study of its effect on hospital-acquired influenza among patients. BMC Infect Dis 2012; 12:30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Potter J, Stott DJ, Roberts MA, et al. Influenza vaccination of health care workers in long-term-care hospitals reduces the mortality of elderly patients. J Infect Dis 1997; 175:1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Carman WF, Elder AG, Wallace LA, et al. Effects of influenza vaccination of health-care workers on mortality of elderly people in long-term care: a randomised controlled trial. Lancet 2000; 355:93–7. [DOI] [PubMed] [Google Scholar]
- 42. Hayward AC, Harling R, Wetten S, et al. Effectiveness of an influenza vaccine programme for care home staff to prevent death, morbidity, and health service use among residents: cluster randomised controlled trial. BMJ 2006; 333:1241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Lemaitre M, Meret T, Rothan-Tondeur M, et al. Effect of influenza vaccination of nursing home staff on mortality of residents: a cluster-randomized trial. J Am Geriatr Soc 2009; 57:1580–6. [DOI] [PubMed] [Google Scholar]
- 44. Ahmed F, Lindley MC, Allred N, et al. Effect of influenza vaccination of healthcare personnel on morbidity and mortality among patients: systematic review and grading of evidence. Clin Infect Dis 2014; 58:50–7. [DOI] [PubMed] [Google Scholar]
- 45. Talbot TR, Babcock H, Caplan AL, et al. Revised SHEA position paper: influenza vaccination of healthcare personnel. Infect Control Hosp Epidemiol 2010; 31:987–95. [DOI] [PubMed] [Google Scholar]
- 46. Talbot TR, Bradley SE, Cosgrove SE, et al. Influenza vaccination of healthcare workers and vaccine allocation for healthcare workers during vaccine shortages. Infect Control Hosp Epidemiol 2005; 26:882–90. [DOI] [PubMed] [Google Scholar]
- 47. Doby E, Stockmann C, Petersen S, et al. Mandatory employee vaccination policy with termination for non-compliance increases vaccine coverage in a large, not-for-profit health system [poster, abstract 432]. IDWeek (San Diego, CA) October 18, 2012. [Google Scholar]
- 48. Parada J, Chauhan D, Gaughan B, Koller M, Schleffendorf C, Hindle P. Duh, why didn’t we do this sooner?! Three year experience with mandatory seasonal influenza immunization for all personnel in a university medical center [poster, abstract 436]. IDWeek (San Diego, CA) October 18, 2012. [Google Scholar]
- 49. Kidd F, Wones R, Momper A, et al. From 51% to 100%: mandatory seasonal influenza vaccination. Am J Infect Control 2012; 40:188–90. [DOI] [PubMed] [Google Scholar]
- 50. Poland GA, Tucker S. The nursing profession and patient safety and healthcare provider influenza immunization: the puzzling stance of the American Nursing Association. Vaccine 2012; 30:1753–5. [DOI] [PubMed] [Google Scholar]
- 51. Bennett JA, Block D. Nursing leadership to ensure patient and health worker protection from influenza. Vaccine 2012; 30:1756–8. [DOI] [PubMed] [Google Scholar]
- 52. American Nurses Association. American Nurses Association Makes New Recommendation That All Nurses Should Be Immunized Against Vaccine-Preventable Diseases (8/20/15). Avaiable at: http://www.nursingworld.org/MainMenuCategories/Policy-Advocacy/Positions-and-Resolutions/ANAPositionStatements/Position-Statements-Alphabetically/Immunizations.html. Accessed 3 January 2019.
- 53. Weyrauch V. How to monitor and evaluate policy influence? Toolkit No. 2.2012. Available at: http://r4d.dfid.gov.uk/pdf/outputs/GDNet/guia04_ingles_cippec_me1.pdf. Accessed 3 January 2019.
- 54. Caplan A, Shah NR. Managing the human toll caused by seasonal influenza: New York State’s mandate to vaccinate or mask. JAMA 2013; 310:1797–8. [DOI] [PubMed] [Google Scholar]
- 55. Ottenberg AL, Wu JT, Poland GA, et al. Vaccinating health care workers against influenza: the ethical and legal rationale for a mandate. Am J Public Health 2011; 101:212–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Zimmerman RK. Ethical analyses of institutional measures to increase health care worker influenza vaccination rates. Vaccine 2013; 31:6172–6. [DOI] [PubMed] [Google Scholar]
- 57. Isaacs D, Leask J. Should influenza immunisation be mandatory for healthcare workers? No. BMJ 2008; 337:a2140. [DOI] [PubMed] [Google Scholar]
- 58. Poland GA. Mandating influenza vaccination for health care workers: putting patients and professional ethics over personal preference. Vaccine 2010; 28:5757–9. [DOI] [PubMed] [Google Scholar]
- 59. American Medical Association. AMA Code of Medical Ethics Opinion 8.7, “Routine Universal Immunization of Physicians.” Available at: https://www.ama-assn.org/delivering-care/ethics/routine-universal-immunization-physicians. Accessed 3 January 2019.
- 60. American Nurses Association. Immunize. Available at: https://www.nursingworld.org/practice-policy/work-environment/health-safety/immunize/. Accessed 3 January 2019.
- 61. Health Affairs Blog. The ‘Must Do’ List: Certain Patient Safety Rules Should Not Be Elective (August 20, 2015). Available at: http://healthaffairs.org/blog/2015/08/20/the-must-do-list-certain-patient-safety-rules-should-not-be-elective/. Accessed 3 January 2019.
- 62. Stewart AM. Mandatory vaccination of health care workers. N Engl J Med 2009; 361:2015–7. [DOI] [PubMed] [Google Scholar]
- 63. Douville LE, Myers A, Jackson MA, Lantos JD. Health care worker knowledge, attitudes, and beliefs regarding mandatory influenza vaccination. Arch Pediatr Adolesc Med 2010; 164:33–7. [DOI] [PubMed] [Google Scholar]
- 64. deSante JE, Caplan A, Shofer F, Behrman AJ. Physician attitudes towards influenza immunization and vaccine mandates. Vaccine 2010; 28:2517–21. [DOI] [PubMed] [Google Scholar]
- 65. Poland GA, Ofstead CL, Tucker SJ, Beebe TJ. Receptivity to mandatory influenza vaccination policies for healthcare workers among registered nurses working on inpatient units. Infect Control Hosp Epidemiol 2008; 29:170–3. [DOI] [PubMed] [Google Scholar]