Abstract
Life expectancy has increased as a result of advancements in health care services; thus, maintaining healthy dentition is an important factor in overall health. Furthermore, the growing desire of elderly patients to maintain their teeth has led to an increased need for the performance of complex dental treatment in elderly patients. Root canal therapy is an essential phase of such treatments. Elderly patients may exhibit one or more systemic conditions that require special care, in addition to other changes that occur within the dentition and oral mucosa as a result of aging. These make root canal treatment in elderly patients a great challenge. The aim of this review was to characterize pathologic and physiologic changes in elderly patients that can interfere with root canal treatment procedures, as well as attitudes of elderly patients toward such treatment, guidelines and clinical considerations for management of root canal treatment in elderly patients.
Aging involves successive and increasing changes with time, many of which lead to impaired structural soundness; in addition, such changes increase susceptibility to diseases and functional disabilities.1 Life expectancy has increased as a result of advancements in health care services.2 Industrialized countries will have a potential increase in life expectancy for 65% of women and 85% of men, which will lead to an increasing need for health and social services.3 This increasing life expectancy will be reflected in dental healthcare services, as well as other healthcare fields, such that the need to retain and preserve teeth will also increase.4 The maintenance of healthy dentition is an important factor in overall health. Furthermore, the growing desire of elderly patients to maintain their teeth will lead to an increased need for the performance of complex dental treatment; root canal therapy is considered an essential phase of these procedures to maintain teeth. Elderly patients may exhibit systemic diseases or special needs that increase the importance of maintaining healthy teeth.4 Elderly patients may have more untreated apical disease than other adults, so they may exhibit a greater need to undergo root canal therapy.5 Indeed, according to a survey of diplomates of the American Board of Endodontics, patients over 65 years of age comprise 26% of all endodontically treated patients.6 Increased age is associated with an increasing number of teeth that require root canal treatment, as well as an increasing number of teeth with periapical disease.5 One of the consequences of tooth loss among elderly patients may be loss of self-confidence and a sensation of aging.7 Therefore, quality of life and emotional well-being in elderly patients may be improved by maintenance of healthy dentition. There is a misconception among some dental practitioners in that they expect the prognosis of root canal therapy in elderly patients to be poor, as a result of several factors: technical difficulties, physical and cognitive limitations, and a disinterest in preservation of their natural teeth.8
The aim of this review is to characterize pathologic and physiologic changes in elderly patients that can interfere with root canal treatment procedures, as well as attitudes of elderly patients toward such treatment, guidelines and clinical considerations for management of root canal treatment in elderly patients, and the prognosis of such treatment in elderly patients.
Pathologic and physiologic changes in elderly patients
Elderly patients may suffer from one or more systemic conditions.9 Age itself is considered a risk factor for a large number of diseases, injuries, hospitalization, length of hospitalization, and adverse drug reactions.10 Moreover, aging may influence nearly all parts of the body.11 The effects of aging on major organ systems can be summarized as follows: 1) Changes in structure, function, metabolism, and blood flow in the aging brain, which may cause cognitive impairments, most frequently episodic memory changes, as well as an increased risk of hallucination in acute cases; 2) Increased blood pressure with reduced cardiac output and reduced chronotropic and inotropic responses to beta-receptor stimulation; 3) Changes in the mechanical properties of the respiratory system, which can lead to reduced arterial oxyhemoglobin saturation and reduced response to hypoxia; 4) Alterations in esophageal motility, delayed gastric emptying, and reduction in hepatic metabolism; 5) Reduced renal function; 6) Reduced hormone secretion from peripheral glands and reduced tissue responsiveness to hormones.11
Mild cognitive impairment (MCI) has been observed in approximately 15-20% of people aged 65 or older.12 People with MCI, especially MCI involving memory problems, are more susceptible to the development of Alzheimer’s or other dementias than people without MCI.13,14 Senile dementia is a common phenomenon among the elderly that can result in memory loss, confusion, inability to perform decision-making tasks, comprehension difficulties, and inability to learn new tasks required for appropriate treatment.15,16 Importantly, aging is considered a risk factor for cardiovascular disease (CVD).17-19 People over 65 years of age have a higher prevalence rate of CVD, compared with younger people.18 Osteoporosis is another risk factor in elderly patients. In the European Union countries, approximately 5% of people aged 50 years or older have osteoporosis and receive frequent treatment with bisphosphonates.20 In patients undergoing bisphosphonates treatment, it may be better to save compromised teeth by root canal therapy, as the extraction of these teeth may cause bisphosphonate-related osteonecrosis of the jaw.21 Additionally, people over 65 years of age have a greater prevalence of hearing problems, such that approximately 1 in 3 people 65-74 years of age has some degree of hearing loss, and approximately half of people over 75 years of age have difficulties in hearing which create difficulties in communication during dental treatment.22 Similarly, visual problems increase with age, such that the prevalence of wearing eyeglasses is greater than 90% among elderly patients.9 Finally, psychological health is considered an important factor in elderly patients, as some experience depression due to loneliness or a feeling of neglect.15,16
Effects of aging in oral soft tissues
Aging affects the oral mucosa, such that it becomes thinner, smoother, and exhibits an edematous appearance. Moreover, it shows a loss of elasticity and stippling.23 The tongue becomes smoother and loses filiform papillae.23 With age, the oral mucosa becomes susceptible to several pathoses, such as Candida infections; it also demonstrates reduced wound healing.23 Periodontal support is affected by age: in general, less than 3 mm gingival recession has been observed on the buccal surfaces of elderly patients.24 According to National Health and Nutrition Examination Survey in the USA, periodontitis steadily increases from 30 to 80 years of age.24 The flow rates of submandibular and sublingual salivary glands are reduced with aging, whereas the flow rates of the parotid and minor glands do not appear to significantly change with aging.25 Xerostomia is not considered a normal aspect of aging. It is estimated that between 25% and 50% of older adults exhibit xerostomia.26 This may occur as a result of various biological reasons, such as: a history of radiotherapy to the head and neck area, salivary gland diseases, diabetes, alcoholic cirrhosis, cystic fibrosis, hormonal imbalance, autoimmune diseases (such as Sjögren syndrome, rheumatoid arthritis, or systemic lupus erythematosus), AIDS, or Parkinson’s disease.27-29 Xerostomia may also constitute a side effect of some medications, especially in patients who use multiple medications.30 Importantly, medications used for CVD treatment are known to reduce salivary flow.31 Additionally, the following types of drugs can reduce salivary flow: anticholinergic, antidepressant, antipsychotic, diuretic, antihypertensive, sedative and anxiolytic, antihistamine, opioid analgesic agents, and nonsteroidal anti-inflammatory drugs.28 Social and psychological conditions such as depression, anxiety, and stress may constitute causative factors of hyposalivation.27,28 Hyposalivation can lead to inadequate bicarbonate and urea buffering, remineralization, and sugar and acid clearance, which may cause an increase rate of caries.28,32
Aging-related changes to the dentition
Several changes occur in the dentition with age, which are considered normal aspects of the aging process and not disease. These changes include: enamel wearing, enamel chipping, appearance of fracture lines, staining of the chipped areas and fracture lines, exposure of the dentin, which will wear more quickly than enamel, deposition of secondary dentin, and recession in the size of the pulp chamber and canals (this is often observed radiographically).33 Dark coloring of the teeth is an aspect of aging that results from stain accumulation and secondary dentin deposition.33 Tooth microstructure changes with age, such that the mineral content increases and organic content decreases.34,35 These changes influence the mechanical, physical, and chemical properties of enamel and dentin, such that they become more brittle and susceptible to fracture.35 Increasing root canal calcification with age increases the technical difficulty of root canal treatment.36 Increasing calcification of the pulp chamber and root canals may complicate pulp vitality tests during endodontic diagnosis and may lead to false responses. Furthermore, cleaning and shaping of calcified canals is technically difficult and requires the practitioner to be patient and calm.36 In elderly patients, most cases of pulp necrosis occur without the classic symptoms of reversible and irreversible pulpitis.6 In general, aging pulps can be considered “sclerosed” or “calcified,” due to the continued deposition of regular secondary dentin.37 With increasing age, the number of odontoblasts decreases and the reparative ability of the pulp is reduced.37 The most common oral conditions among elderly patients are: dental caries, tooth loss, periodontal disease, dry mouth, and oral precancer/cancer.38
Attitudes of elderly patients towards nonsurgical root canal treatment
Teeth retained through nonsurgical root canal treatment are highly valued by elderly patients.39 The priorities of elderly patients differ from those of younger patients. This difference may influence the treatment plan, as the objective of treatment in elderly patients is more closely guided by short-term goals and asymptomatic function than by esthetics and longtime stability.4 Elderly patients have positive attitudes towards nonsurgical root canal treatment, but may refuse dental implants due to fear or cost.36,40 Nonsurgical root canal treatment is appreciated by elderly patients because of several factors: relief of pain and swelling, improved chewing and digestion, improved esthetic appearance and self-esteem, and enhanced preservation of natural teeth; dignity, speech, and support of existing prostheses.36 However, some elderly patients have negative opinions regarding nonsurgical root canal treatment, including: the extended length of the dental visit, the extended length of time that the mouth must remain open, dryness of the mouth due to the length of the visit, and inconvenience from rubber dam isolation.36 The main causes for avoidance of dental treatment by elderly persons are: high cost, fear of pain, lack of knowledge or understanding the requirement of dental care, reduced cognitive ability, reduced ability to tolerate treatment steps, and limited mobility.41
Clinical considerations for elderly patients undergoing root canal treatment
Preservation of the teeth in elderly patients provides several benefits: maintenance of an intact dental arch, increased retention of removable dentures, provision of abutments for fixed prostheses, preservation of occlusion, and preservation of alveolar bone in cases treated by overdentures. Dental care for elderly patients requires accurate knowledge, good technical skill, and experience in empathetic patient management.42 Root canal treatment in elderly patients is considered a great challenge due to technical difficulties from a calcified and limited pulp chamber.39 The strategic importance of the tooth is crucial in determining whether to save the tooth by root canal treatment or perform extraction; however, root canal treatment is contraindicated in some medical conditions. Some of these conditions include: patients requiring radiotherapy to the head and neck region, and poor compliance (for example, in patients with Parkinson’s disease, tremors, or dementia).39
The following recommendations should be considered for management of root canal treatment in elderly patients
1) Informed consent and communication with patients’ treating physicians are essential steps before any procedure. It is important that all older patients should know the risks and other choices.43 2) Strict evaluation of medical history and medications of elderly patients, in consultation with their physicians.44 Treatment appointments should be scheduled according to the physical and mental condition of elderly patients.43 3) The emotional needs of elderly patients should be considered. Dental practitioners should make every effort to satisfy their patients.16 4) Prescribe prophylactic antibiotics when indicated.43 5) The results of pulp vitality tests (heat, cold, and electrical pulp test) in elderly patients may not be accurate because of calcification or root canals.45 6) The reduction of periodontal ligament width in elderly patients, makes intraligamentary anesthesia a difficult step. Intraosseous anesthesia can be considered as a practical alternative, but a transient increase in heart rate could occur due to epinephrine.46,47 7) Mepivacaine 3% can be used as a safe choice for elderly patients with medical conditions.48 8) Patients’ eyes should be shielded from the intensity of clinicians’ lights.43 9) Preoperative radiographs should be evaluated carefully; access cavity preparation and exploring of canal orifices should be performed delicately.49 In some cases, the tooth structure may be scarified to obtain appropriate access to the cavity. Ultrasonic endodontic tips have particular significance in negotiation of calcified canal orifices.43 Preparation of an adequate access cavity in case of severe calcification of the pulp chamber is very challenging and may lead to a tremendous loss of tooth structure. an innovative approach to treat teeth with pulp canal calcifications by using an intra-oral scan with CBCT data to produce a template for a guided access cavity preparation and root canal localizatio.50 10) Magnification and transillumination to identify calcified canals comprise another useful aid during root canal treatment in elderly patients.4 11) Pillows should be used for back/neck comfort as needed.4 12) Blankets should be available if the office temperature is too cool for elderly patients.43 13) The use of bite blocks is recommended to ensure comfortable jaw opening during long procedures.43 However, practitioners should avoid jaw fatigue-the session should be terminated as rapidly as possible.43 14) Single-tooth isolation is the best choice for root canal treatment. However, severely deteriorated teeth may require multitooth rubber dam isolation.43 15) Single-visit root canal treatment, if possible, has several advantages for elderly patients, especially for those patients who depend on others for transportation or who require physical assistance to visit the dental office.43 16) Cementum deposition continues for a lifetime, this will lead to cementum thickness increasing. This morphological change will increase the distance between apical foramen and radiographic apex.4 All these changes will reduce the reliability of working length determination by X-Ray.
Electronic apex locators (EALs) are considered accurate devices for determination working length.51 Electronic apex locators can be used safely in patients with cardiovascular implantable electronic devices, when general precautions are followed.52 17) Rotary NiTi instrumentation reduces treatment time and procedural accidents during cleaning and shaping.53 However, because the canals are much narrower, this approach requires additional time, effort, and care to prepare the root canal and reduce the risk of binding and separation.4 A single-file NiTi system is considered appropriate for elderly patients who require short times for canal preparation; the use of the single-file reciprocating motion system is not influenced by the operator’s experience.54
If the canals are identified calcified radiographically, the clinician should locate the canals with proper magnification; prepare the canals with stiff, pre-curved stainless-steel hand K- files size 6, 8 and 10, followed by nickel titanium rotary glide path files with lubricant and copious irrigation. After preparing adequate glide path the canal instrumentation completed with a single-file NiTi system. 18) The use of a single-cone with bioceramic sealers is a viable option for obturation, which has achieved a high success rate.55 19) Full coverage restorations on molars in elderly patients exhibit a high success rate.56 If a post is used in restoration of endodontically treated teeth, the taper of the post should be particularly careful, as excessive taper can cause vertical root fracture. A post is not necessary when performing root canal treatment through the full crown; the decision can be made to continue using this crown.43 20) Non-surgical root canal retreatment is an efficient way for management of unhealed endodontic lesions, regardless of a patient’s age.8,36 Generally, considerations and indications for endodontic surgery are not affected by age, medical considerations may require consultation but do not contraindicate surgical treatment when extraction is the alternative.43 The elderly frail patients experience significantly more postoperative complications after surgical procedures.57
When to consider endodontic referral
The performance of root canal treatment in elderly patients as an alternative to extraction may exceed the ability of the general dental practitioner; in such cases, referral to an endodontist may be necessary.43 The general practitioner must be able to determine the degree of difficulty and associated risks, and determine his or her own skill for performing the necessary treatment. The practitioner must also determine when the patient should be referred to the appropriate specialist.58
There are no definitive criteria for referral. However, when an elderly patient cannot tolerate treatment procedures performed by a general practitioner, the patient should be referred to an endodontist.4 Elderly patients with medical conditions such as diabetes may be better served by endodontists.43,59 Cases with factors that can complicate root canal treatment, such as periodontal problems and severe breakdown that require special procedures for isolation, should be referred to an endodontist.43
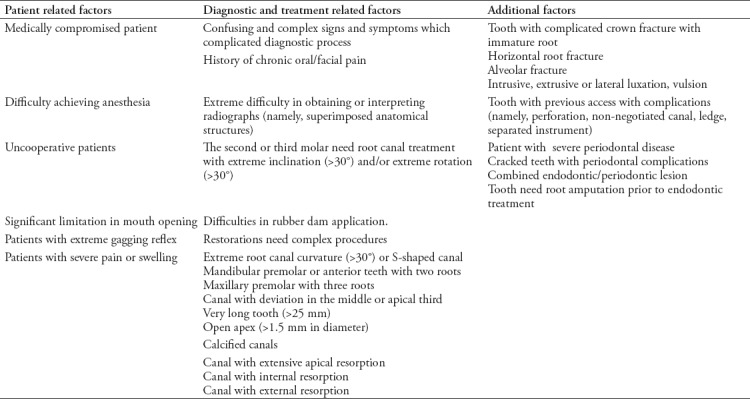
Table 1 shows the factors that identify difficult situations that must be referred to the appropriate specialist for treatment. These factors have been determined on the basis of the American Association of Endodontists AAE Case Difficulty Assessment Form.58 This form is an important and valuable tool to predict potential complications of root canal therapy and the number of visits needed for treatment.60
Table 1.
The factors that identify difficult situations that must be referred to the appropriate specialist for root canal treatment.
Clinical outcome
The objectives of root canal treatment are to remove intracanal infection and prevent the canal from reinfection by creating a suitable environment for healing of apical periodontitis.4 An in vitro study revealed that disinfection of older dentin is more difficult than disinfection of younger dentin.61 However, a systematic review found no influence of age on the success rate of initial root canal treatment.62 Patient age alone should not be considered as a prognostic factor.36 In cases with vital pulps, the prognosis of root canal treatment was very good, but medical conditions and systematic disease should include adequate controls and accurate assessment.63 Importantly, the prognosis of cases with preoperative periapical lesions is poorer than that of other cases; systemic diseases may have a more substantial role.63 Although periradicular tissues heal readily in both elderly and young patients, a 6-month recall period to evaluate repair by means of radiographs may be inadequate.64,65 Studies that suggest differences in success among age groups must note the smaller numbers (typically in this older treatment group) and the local factors that make treatment difficult.
In conclusion, root canal treatment in elderly patients has a significant role in comprehensive dental care due to the increased presence of an “aging society.” Root canal treatment in elderly patients with complex conditions and problems with functional dependence requires special care and advanced training. There is a need to improve education programs and curriculum to include training regarding suitable dental care procedures for this branch of dentistry.
Footnotes
References
- 1.López-Otín C, Blasco MA, Partridge L, Serrano M, Kroemer G. The hallmarks of aging. Cell. 2013;153:1194–1217. doi: 10.1016/j.cell.2013.05.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mathers CD, Stevens GA, Boerma T, White RA, Tobias MI. Causes of international increases in older age life expectancy. The Lancet. 2015;385:540–548. doi: 10.1016/S0140-6736(14)60569-9. [DOI] [PubMed] [Google Scholar]
- 3.Kontis V, Bennett JE, Mathers CD, Li G, Foreman K, Ezzati M. Future life expectancy in 35 industrialised countries:projections with a Bayesian model ensemble. The Lancet. 2017;389:1323–1335. doi: 10.1016/S0140-6736(16)32381-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Johnstone M, Parashos P. Endodontics and the ageing patient. Aust Dent J. 2015;60:20–27. doi: 10.1111/adj.12281. [DOI] [PubMed] [Google Scholar]
- 5.Hamedy R, Shakiba B, Pak JG, Barbizam JV, Ogawa RS, White SN. Prevalence of root canal treatment and periapical radiolucency in elders:a systematic review. Gerodontology. 2016;33:116–127. doi: 10.1111/ger.12137. [DOI] [PubMed] [Google Scholar]
- 6.Goodis HE, Rossall JC, Kahn AJ. Endodontic status in older US adults:report of a survey. J Am Dent Assoc. 2001;132:1525–1530. doi: 10.14219/jada.archive.2001.0085. [DOI] [PubMed] [Google Scholar]
- 7.Bidinotto AB, Santos CM, Tôrres LH, de Sousa Md, Hugo FN, Hilgert JB. Change in quality of life and its association with oral health and other factors in community-dwelling elderly adults-a prospective cohort study. J Am Geriatr Soc. 2016;64:2533–2538. doi: 10.1111/jgs.14482. [DOI] [PubMed] [Google Scholar]
- 8.Hamedy R, Shakiba B, White SN. Essential elder endodontics. Gerodontology. 2016;33:433. doi: 10.1111/ger.12248. [DOI] [PubMed] [Google Scholar]
- 9.Yellowitz JA, Schneiderman MT. Elder's oral health crisis. J Evid Based Dent Pract. 2014;14:191–200. doi: 10.1016/j.jebdp.2014.04.011. [DOI] [PubMed] [Google Scholar]
- 10.Chen YC, Fan JS, Chen MH, Hsu TF, Huang HH, Cheng KW, et al. Risk factors associated with adverse drug events among older adults in emergency department. Eur J Intern Med. 2014;25:49–55. doi: 10.1016/j.ejim.2013.10.006. [DOI] [PubMed] [Google Scholar]
- 11.Alvis BD, Hughes CG. Physiology considerations in geriatric patients. Anesthesiol Clin. 2015;33:447–456. doi: 10.1016/j.anclin.2015.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Roberts R, Knopman DS. Classification and epidemiology of MCI. Clin Geriatr Med. 2013;29:753–772. doi: 10.1016/j.cger.2013.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kantarci K, Weigand S, Przybelski S, Shiung M, Whitwell J, Negash S, et al. Risk of dementia in MCI combined effect of cerebrovascular disease, volumetric MRI, and 1H MRS. Neurology. 2009;72:1519–1525. doi: 10.1212/WNL.0b013e3181a2e864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mitchell AJ, Shiri-Feshki M. Rate of progression of mild cognitive impairment to dementia–meta-analysis of 41 robust inception cohort studies. Acta Psychiatr Scand. 2009;119:252–265. doi: 10.1111/j.1600-0447.2008.01326.x. [DOI] [PubMed] [Google Scholar]
- 15.Yellowitz JA. Cognitive function, aging, and ethical decisions:recognizing change. Dent Clin North Am. 2005;49:389–410. doi: 10.1016/j.cden.2004.10.010. [DOI] [PubMed] [Google Scholar]
- 16.Patil MS, Patil SB. Geriatric patient-psychological and emotional considerations during dental treatment. Gerodontology. 2009;26:72–77. doi: 10.1111/j.1741-2358.2008.00245.x. [DOI] [PubMed] [Google Scholar]
- 17.North BJ, Sinclair DA. The intersection between aging and cardiovascular disease. Circ Res. 2012;110:1097–1108. doi: 10.1161/CIRCRESAHA.111.246876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Heidenreich PA, Trogdon JG, Khavjou OA, Butler J, Dracup K, Ezekowitz MD, et al. Forecasting the future of cardiovascular disease in the United States:a policy statement from the American Heart Association. Circulation. 2011;123:933–944. doi: 10.1161/CIR.0b013e31820a55f5. [DOI] [PubMed] [Google Scholar]
- 19.Paneni F, Cañestro CD, Libby P, Lüscher TF, Camici GG. The aging cardiovascular system:understanding it at the cellular and clinical levels. J Am Coll Cardiol. 2017;69:1952–1967. doi: 10.1016/j.jacc.2017.01.064. [DOI] [PubMed] [Google Scholar]
- 20.Hernlund E, Svedbom A, Ivergård M, Compston J, Cooper C, Stenmark J, et al. Osteoporosis in the European Union:medical management, epidemiology and economic burden. A report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA) Arch Osteoporos. 2013;8:136. doi: 10.1007/s11657-013-0136-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.AlRahabi MK, Ghabbani HM. Clinical impact of bisphosphonates in root canal therapy. Saudi Med J. 2018;39:232–238. doi: 10.15537/smj.2018.3.20923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Walling AD, Dickson GM. Hearing loss in older adults. Am Fam Physician. 2012;85:1150–1156. [PubMed] [Google Scholar]
- 23.Razak PA, Richard KJ, Thankachan RP, Hafiz KA, Kumar KN, Sameer K. Geriatric oral health:a review article. J Int Oral Health. 2014;6:110–116. [PMC free article] [PubMed] [Google Scholar]
- 24.Eke PI, Dye BA, Wei L, Slade GD, Thornton-Evans GO, Borgnakke WS, et al. Update on prevalence of periodontitis in adults in the United States:NHANES 2009 to 2012. J Periodontol. 2015;86:611–22. doi: 10.1902/jop.2015.140520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Smith CH, Boland B, Daureeawoo Y, Donaldson E, Small K, Tuomainen J. Effect of aging on stimulated salivary flow in adults. J Am Geriatr Soc. 2013;61:805–808. doi: 10.1111/jgs.12219. [DOI] [PubMed] [Google Scholar]
- 26.Nagler R. Salivary glands and the aging process:mechanistic aspects, health-status and medicinal-efficacy monitoring. Biogerontology. 2004;5:223–233. doi: 10.1023/B:BGEN.0000038023.36727.50. [DOI] [PubMed] [Google Scholar]
- 27.Navazesh M, Kumar SK. Measuring salivary flow:challenges and opportunities. J Am Dent Assoc. 2008;139:35S–40S. doi: 10.14219/jada.archive.2008.0353. [DOI] [PubMed] [Google Scholar]
- 28.Wiener RC, Wu B, Crout R, Wiener M, Plassman B, Kao E, et al. Hyposalivation and xerostomia in dentate older adults. J Am Dent Assoc. 2010;141:279–284. doi: 10.14219/jada.archive.2010.0161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hjertstedt J, Barnes SL, Sjostedt JM. Investigating the impact of a community-based geriatric dentistry rotation on oral health literacy and oral hygiene of older adults. Gerodontology. 2014;31:296–307. doi: 10.1111/ger.12038. [DOI] [PubMed] [Google Scholar]
- 30.Johanson CN, Österberg T, Lernfelt B, Ekström J, Birkhed D. Salivary secretion and drug treatment in four 70-year-old Swedish cohorts during a period of 30 years. Gerodontology. 2015;32:202–210. doi: 10.1111/ger.12089. [DOI] [PubMed] [Google Scholar]
- 31.Scelza MFZ, Silva DdF, Ahiadzro NK, Da Silva LE, Scelza P. The influence of medication on salivary flow of the elderly:preliminary study. Gerodontology. 2010;27:278–282. doi: 10.1111/j.1741-2358.2009.00326.x. [DOI] [PubMed] [Google Scholar]
- 32.Dawes C. Salivary flow patterns and the health of hard and soft oral tissues. J Am Dent Assoc. 2008;139:18S–24S. doi: 10.14219/jada.archive.2008.0351. [DOI] [PubMed] [Google Scholar]
- 33.Lamster IB, Asadourian L, Del Carmen T, Friedman PK. The aging mouth:differentiating normal aging from disease. Periodontol 2000. 2016;72:96–107. doi: 10.1111/prd.12131. [DOI] [PubMed] [Google Scholar]
- 34.He B, Huang S, Zhang C, Jing J, Hao Y, Xiao L, et al. Mineral densities and elemental content in different layers of healthy human enamel with varying teeth age. Arch Oral Biol. 2011;56:997–1004. doi: 10.1016/j.archoralbio.2011.02.015. [DOI] [PubMed] [Google Scholar]
- 35.Yahyazadehfar M, Ivancik J, Majd H, An B, Zhang D, Arola D. On the mechanics of fatigue and fracture in teeth. Appl Mech Rev. 2014;66:0308031–3080319. doi: 10.1115/1.4027431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Shakiba B, Hamedy R, Pak JG, Barbizam JV, Ogawa R, White SN. Influence of increased patient age on longitudinal outcomes of root canal treatment:a systematic review. Gerodontology. 2017;34:101–109. doi: 10.1111/ger.12231. [DOI] [PubMed] [Google Scholar]
- 37.Murray PE, Stanley HR, Matthews JB, Sloan AJ, Smith AJ. Age-related odontometric changes of human teeth. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002;93:474–482. doi: 10.1067/moe.2002.120974. [DOI] [PubMed] [Google Scholar]
- 38.Petersen PE, Yamamoto T. Improving the oral health of older people:the approach of the WHO Global Oral Health Programme. Community Dent Oral Epidemiol. 2005;33:81–92. doi: 10.1111/j.1600-0528.2004.00219.x. [DOI] [PubMed] [Google Scholar]
- 39.Allen PF, Whitworth JM. Endodontic considerations in the elderly. Gerodontology. 2004;21:185–194. doi: 10.1111/j.1741-2358.2004.00039.x. [DOI] [PubMed] [Google Scholar]
- 40.Müller F, Salem K, Barbezat C, Herrmann FR, Schimmel M. Knowledge and attitude of elderly persons towards dental implants. Gerodontology. 2012;29:e914–23. doi: 10.1111/j.1741-2358.2011.00586.x. [DOI] [PubMed] [Google Scholar]
- 41.Liu Y-e, While AE, Norman IJ, Ye W. Health professionals'attitudes toward older people and older patients:A systematic review. J Interprof Care. 2012;26:397–409. doi: 10.3109/13561820.2012.702146. [DOI] [PubMed] [Google Scholar]
- 42.MacEntee MI. The educational challenge of dental geriatrics. J Dent Educ. 2010;74:13–9. [PubMed] [Google Scholar]
- 43.Newton CW, Coil JM. Effects of age and systemic health on endodontics. In: Hargreaves K, Berman L, editors. Cohen's pathways of the pulp. USA: Elsevier Inc; 2016. [Google Scholar]
- 44.Williams BR, Kim J. Medication use and prescribing considerations for elderly patients. Dent Clin North Am. 2005;49:411–427. doi: 10.1016/j.cden.2004.10.001. [DOI] [PubMed] [Google Scholar]
- 45.Newton CW, Hoen MM, Goodis HE, Johnson BR, McClanahan SB. Identify and determine the metrics, hierarchy, and predictive value of all the parameters and/or methods used during endodontic diagnosis. J Endod. 2009;35:1635–1644. doi: 10.1016/j.joen.2009.09.033. [DOI] [PubMed] [Google Scholar]
- 46.Mortazavi H, Baharvand M. Review of common conditions associated with periodontal ligament widening. Imaging Sci Dent. 2016;46:229–237. doi: 10.5624/isd.2016.46.4.229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Zarei M, Ghoddusi J, Sharifi E, Forghani M, Afkhami F, Marouzi P. Comparison of the anaesthetic efficacy of and heart rate changes after periodontal ligament or intraosseous X-Tip injection in mandibular molars:a randomized controlled clinical trial. Int Endod J. 2012;45:921–926. doi: 10.1111/j.1365-2591.2012.02050.x. [DOI] [PubMed] [Google Scholar]
- 48.Drum M, Reader A, Nusstein J, Fowler S. Successful pulpal anesthesia for symptomatic irreversible pulpitis. J Am Dent Assoc. 2017;148:267–271. doi: 10.1016/j.adaj.2017.01.002. [DOI] [PubMed] [Google Scholar]
- 49.Nadig RR, Usha G, Kumar V, Rao R, Bugalia A. Geriatric restorative care-the need, the demand and the challenges. J Conserv Dent. 2011;14:208–214. doi: 10.4103/0972-0707.85788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kiefner P, Connert T, ElAyouti A, Weiger R. Treatment of calcified root canals in elderly people:a clinical study about the accessibility, the time needed and the outcome with a three-year follow-up. Gerodontology. 2017;34:164–170. doi: 10.1111/ger.12238. [DOI] [PubMed] [Google Scholar]
- 51.Piasecki L, dos Reis PJ, Jussiani EI, Andrello AC. A micro-computed tomographic evaluation of the accuracy of 3 electronic apex locators in curved canals of mandibular molars. J Endod. 2018;44:1872–1877. doi: 10.1016/j.joen.2018.09.001. [DOI] [PubMed] [Google Scholar]
- 52.AlRahabi MK, Ghabbani HM. Influence and safety of electronic apex locators in patients with cardiovascular implantable electronic devices:a systematic review. Libyan J Med. 2019;14:1547071. doi: 10.1080/19932820.2018.1547071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Alrahabi M. Comparative study of root-canal shaping with stainless steel and rotary NiTi files performed by preclinical dental students. Technol Health Care. 2015;23:257–265. doi: 10.3233/THC-150895. [DOI] [PubMed] [Google Scholar]
- 54.Muñoz E, Forner L, Llena C. Influence of operator's experience on root canal shaping ability with a rotary nickel-titanium single-file reciprocating motion system. J Endod. 2014;40:547–550. doi: 10.1016/j.joen.2013.08.027. [DOI] [PubMed] [Google Scholar]
- 55.Chybowski EA, Glickman GN, Patel Y, Fleury A, Solomon E, He J. Clinical outcome of non-surgical root canal treatment using a single-cone technique with endosequence bioceramic sealer:a retrospective analysis. J Endod. 2018;44:941–945. doi: 10.1016/j.joen.2018.02.019. [DOI] [PubMed] [Google Scholar]
- 56.Spielman H, Schaffer SB, Cohen MG, Wu H, Vena DA, Collie D, et al. Restorative outcomes for endodontically treated teeth in the practitioners engaged in applied research and learning network. J Am Dent Assoc. 2012;143:746–755. doi: 10.14219/jada.archive.2012.0262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Makary MA, Segev DL, Pronovost PJ, Syin D, Bandeen-Roche K, Patel P, et al. Frailty as a predictor of surgical outcomes in older patients. J Am Coll Surg. 2010;210:901–908. doi: 10.1016/j.jamcollsurg.2010.01.028. [DOI] [PubMed] [Google Scholar]
- 58.American Association of Endodontists. [[cited 2018]];Treatment Standards. Available from: https://www.aae.org/specialty/wp-content/uploads/sites/2/2018/04/TreatmentStandards_Whitepaper.pdf . [Google Scholar]
- 59.Chávez EM, Wong LM, Subar P, Young DA, Wong A. Dental care for geriatric and special needs populations. Dent Clin North Am. 2018;62:245–267. doi: 10.1016/j.cden.2017.11.005. [DOI] [PubMed] [Google Scholar]
- 60.Haug SR, Solfjeld AF, Ranheim LE, Bårdsen A. Impact of case difficulty on endodontic mishaps in an undergraduate student clinic. J Endod. 2018;44:1088–1095. doi: 10.1016/j.joen.2018.03.012. [DOI] [PubMed] [Google Scholar]
- 61.Ozdemir HO, Buzoglu HD, Calt S, Stabholz A, Steinberg D. Effect of ethylenediaminetetraacetic acid and sodium hypochlorite irrigation on Enterococcus faecalis biofilm colonization in young and old human root canal dentin:in vitro study. J Endod. 2010;36:842–846. doi: 10.1016/j.joen.2010.01.008. [DOI] [PubMed] [Google Scholar]
- 62.Ng YL, Mann V, Rahbaran S, Lewsey J, Gulabivala K. Outcome of primary root canal treatment:systematic review of the literature-Part 2. Influence of clinical factors. Int Endod J. 2008;41:6–31. doi: 10.1111/j.1365-2591.2007.01323.x. [DOI] [PubMed] [Google Scholar]
- 63.Aminoshariae A, Kulild JC, Mickel A, Fouad AF. Association between systemic diseases and endodontic outcome:a systematic review. J Endod. 2017;43:514–519. doi: 10.1016/j.joen.2016.11.008. [DOI] [PubMed] [Google Scholar]
- 64.Walton RE. Torabinejad MM, Fouad A, Walton R. Endodontics:Principles and practice. Philadelphia (PA): Elsevier Inc; 2015. Geriatric endodontics. [Google Scholar]
- 65.Frisk F, Hakeberg M. A 24-year follow-up of root filled teeth and periapical health amongst middle aged and elderly women in Göteborg, Sweden. Int Endod J. 2005;38:246–254. doi: 10.1111/j.1365-2591.2005.00944.x. [DOI] [PubMed] [Google Scholar]


