Abstract
Objectives:
To determine the association between emergency department (ED) visits, glycemic control and the quality of preventive diabetes care among diabetic patients in a Saudi community.
Methods:
This study was an observational, cross-sectional study that collected data through interview-based surveys between February and April 2017. Data were collected from 530 diabetic patients in the diabetes clinics at King Saud Medical City, the tertiary center of Riyadh, Kingdom of Saudi Arabia.
Results:
This study found statistically significant relationships (p<0.05) between ED visits and patient age, the glycated hemoglobin (HbA1c) and education level. Emergency department visits increased by 43% for each unit of increase in HbA1c (odds ratio [OR]=1.43, 95% confidence interval (CI)=1.26-1.62). Graduating from high school decreased the odds of visiting the ED by 43% (OR=0.57, 95% CI=0.34-0.94). Most of the participants were not followed for possible microvascular complications; the majority did not visit nephrology (96.2%), ophthalmology (78.3%) and neurology (97.9%) clinics within the 12 months prior to the interviews.
Conclusion:
Emergency department visits can indicate poor glycemic control in diabetic patients. Additionally, the current practices of preventive diabetes care in Saudi Arabia are not sufficient, according to the diabetic standards of care recommended by the American Diabetes Association.
Diabetes mellitus (DM) is a cluster of metabolic diseases defined by hyperglycemia, which result from imperfections in insulin secretion, action or both.1 The sequela of chronic, untreated diabetes may be long-term impairment of different organs, especially the kidneys, eyes, nerves, blood vessels and heart.1 Worldwide, the prevalence of diabetes has approximately doubled (from 4.7% to 8.5%) in the adult population since 1980, with an estimated 415 million diabetic patients and 5 million diabetes-related deaths in 2015.2,3 In Saudi Arabia, the overall adults’ prevalence of DM is 23.7%, and as declared by the International Federation of Diabetes, Saudi Arabia is one of the 10 most affected countries in the world.4,5 Furthermore, diabetes is considered the leading cause of vision loss in the industrialized world, as well as the chief cause of renal failure, which requires dialysis or renal transplantation in the United States (US), Japan and Europe.6 The US alone spends more than $218 billion each year on medical expenses related to diabetes.7 As diabetes is a chronic disease, people who are diagnosed with diabetes require regular clinical follow ups to mitigate and manage the potential complications.8 The American Diabetes Association (ADA) guidelines recommend that all diabetic patients obtain education and ongoing support for the self-management of diabetes.8 Each patient should be engaged in improving their own self-care regimen, including the self-monitoring of blood glucose, compliance with multiple medications, adherence to the prescribed diet and exercise, proper foot care and risk elimination such as smoking cessation and annual immunizations.9,10 Although these recommendations are accepted globally, they are not implemented in many populations of diabetic patients.11,12 Therefore, it is still difficult to estimate successful self-care accurately.13 Moreover, when diabetic patients select the emergency department (ED) for their care, it costs many resources and does not translate into the preventive care that clearly is necessary for this chronic condition.14-17 Prior studies worldwide found a positive relation between diabetic patients’ visits to the ED and poor diabetes management.18,19 There is limited current literature about the relation between ED visits, glycemic control and the quality of diabetes care in the Saudi community. This study aimed to illustrate the relationship of ED visits and glycemic control together with determination of the preventive diabetes care among diabetic patients in a Saudi community.
Methods
This study was an observational, cross-sectional study that collected data through interview-based surveys between February and April 2017. Data were collected in the diabetes clinics at King Saud Medical City, the tertiary center in Riyadh, Kingdom of Saudi Arabia. Ethical approval was obtained from the Institutional Review Board of Al-Imam Muhammad Ibn Saud Islamic University and a written informed consent was taken from all participated patients.
Participants, data collection and processing
All participants had diagnosed diabetes. Exclusion of patients was based on their diagnosis of gestational diabetes, psychiatric illness, or if they were medically unstable and hence incapable of answering questions or were unwilling to participate. This study was completed by 530 participants, aged between 18-70 years. Participants answered questions about demographics (age, gender, marital status, nationality, education level, employment and body mass index), diagnosis (type of DM, age at time of DM diagnosis and presence of other comorbid diseases), treatments (oral hypoglycemic agent, insulin and others), diabetic microvascular complications (retinopathy, nephropathy and neuropathy), follow-ups for these particular complications (ophthalmic, nephrology and neurology clinics) and the frequency and quantity of ED admissions in the 12 months prior to the interviews. In addition, each patient’s medical file supplied data on glycemic control (glycated hemoglobin [HbA1c] and fasting blood sugar), lipid profile (total cholesterol level, triglycerides, low-density lipoprotein and high-density lipoprotein) in mmol/L unit and kidney function tests (creatinine and urea). These lab tests, regular measurements, and follow-ups for surveillance and management were used to predict which diabetic patients were at risk for inadequate care based on the 2016 ADA recommendations.20
Data analysis
The Chi-square test was utilized to examine the bivariate relationships between all-out categorical variables and ED visits. The t-test was used to compare continuous variables across the 2 groups of interest (visited the ED in the past 12 months, or not). Collinearity was assessed with the Pearson correlation.
The independent predictors of ED visitation were determined by binary logistic regression test. Only 3 variables (age, level of education and HbA1c) showed significant association with the visitation of ED in the initial univariate test, and were then included in a step-wise manner to the binary logistic regression analysis model. Models were compared using the likelihood ratio test with the least parsimonious model. Odds ratios (OR) and 95% confidence intervals (CI) were calculated. Significance of regression coefficients was assessed using the Wald test. Lastly, 2-tailed hypothesis testing was performed, and p<0.05 was considered statistically significant. Statistical analysis was completed using the Statistical Package for Social Science (SPSS) Version 25, (IBM Corp., Armonk, NY, USA).
Results
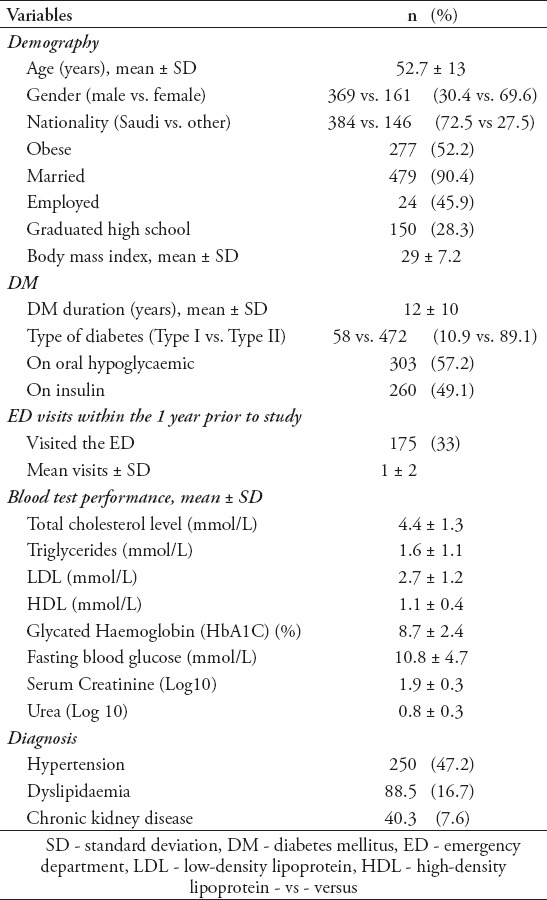
Table 1 contains the descriptive characteristics of participants besides the t-test analyses and the chi-square analyses. In this study, the number of included DM patients is 530. The mean age for patients was 52.62±13 years. Males constituted 69.6% (n=369) of the study population while females constituted 30.4% (n=161). Type I diabetic patients comprised 10.9% of the study population (n=58) while type II diabetic patients constituted the remaining 89.1% (n=472). The average body mass index (BMI) was 28.95±7.24. Most of the patients were Saudi (n=384, 72.5%). More than half of these patients had not visited the ED during the 12 months prior to the study (n=355, 67%), and the average number of the visits during that time was 1±2. The mean HbA1c was higher than the target (8.69±2.41). Almost half of the patients had hypertension (n=250, 47.2%) and less than 20% of the patients had another comorbidity (most commonly dyslipidemia and chronic kidney disease).
Table 1.
Characteristics of the study population (N=530).
Tables 2 and 3 provide the t-test analyses along with the chi-square analyses of the variables of interest versus visiting the ED. Statistically significant relations emerged between ED visits and patient age, HbA1c and education level (p<0.05 for all). Those 3 variables were then included in a binary logistic regression, the results showed 2 of them were statistically significant. Hemoglobin A1c was significantly associated with visiting the ED, with a 43% increase in the odds of visiting the ED with each one-unit increase in HbA1c (OR=1.43, 95% CI=1.26-1.62). Graduation from high school decreased the odds of visiting the ED by 43% (OR=0.57, 95% CI=0.34-0.94).
Table 2.
The relationship between continuous demographics characteristics and visiting the emergency department (N=530)
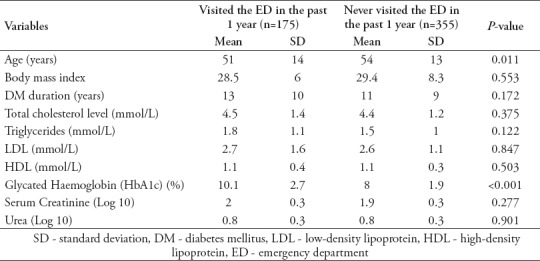
Table 3.
The relationship between categorical demographics characteristics and visiting the emergency department (N= 530).
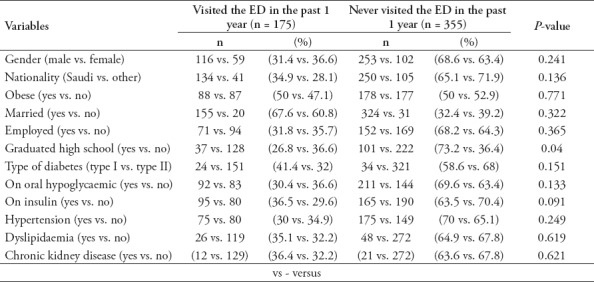
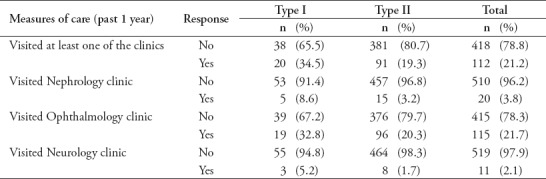
Table 4 provides information about participant follow-ups for possible microvascular complications in the 12 months prior to the study. The large majority of both type 1 and type 2 DM patients did not follow up with nephrology (96.2%), ophthalmology (78.3%), or neurology (97.9%) clinics, combining both types of diabetes during the 12 months in question.
Table 4.
Preventative care behaviours for the past year among diabetic patients in Saudi Arabia.
Discussion
This study determined that there is an independent positive relationship between HbA1C and ED visits, which continue its significance in accordance to the adjustment achieved by analysis of logistic regression. Every unit of increase in HbA1c had an adjusted OR of 1.43. This finding agrees with the results of other studies. Chiou et al (2009) analyzed 7 years of data (1999-2006) from type 2 diabetic patients who received care under a diabetes disease management program provided by the Louisiana State University Health Care Services Division (LSU HCSD) in New Orleans, Louisiana, US.18 The authors stated that the better (lower) levels of HbA1c of DM patients were associated with lower visits into the ED (OR=0.8173, 95% CI=0.7444 -0.8974).18 Moreover, Moss et al (1999) studied a sample of 2990 diabetic patients in an 11-county area of southwest Wisconsin, US, to evaluate the risks of admission. They discovered that elevated HbA1c was significantly associated with the increment of hospitalization risk (OR= 1.27, 95% CI=1.16-1.39) for a one-unit increment.19 The medical records from the ED visits demonstrated that these patients had higher risks of cardiovascular, neurological, renal and ophthalmic problems, precipitating more frequent and longer admissions compared with a non-diabetic population.21 Jiang et al19 (2003) highlighted the importance of greater age as a risk for multiple admissions and hospitalizations, though our study did not find this effect to be significant after adjusting for confounders as in Moss et al22(1999).
Raman et al23 (2012) studied a group of 1414 diabetic patients in Sankara Nethralaya, India, and found that the prevalence of any type of microvascular complication was 30.2% (OR= 30.2, 95% CI=24.5-35.9). The current ADA preventive care guidelines recommend follow ups for possible microvascular complications, including nephropathy, retinopathy and neuropathy. In the Raman et al23 (2012) study, more than 75% of the interviewed diabetic patients had not attended any of these specialty clinics in the 12 months prior to the interview. These results agree with the findings of other studies, conducted in different settings as well as in different countries, all of which support the implementation of the preventive measures recommended by the ADA. For instance, in a prospective study of diabetic patients in Alabama, US, between January 2012 and May 2015, Keenum et al24 (2006) found that only one-third of their patients clung to the recommendations for eye care follow ups. In Tanzania, Mtuya et al25 (2016) found that 75.4% of the participants did not attend the recommended referral eye care appointment during 2012. The reasons for these poor rate of follow ups was attributed to low financial status, unclearness of referral process, unawareness of the potential of treatments of these complications by DM patients.25,26
Study limitations
The limitations of this study include its use of interviews, which created a reliance on self-reported data that is at risk for misclassification. In addition, this study included data collected from only one tertiary center; however, as this center is the largest of the kingdom, it is likely that the patient group was representative of the larger population of interest, and the chance of bias of selection is low. This study further limited by the questionnaire was not formally validated. Also, as with all cross-sectional studies, this study suggests relations but cannot demonstrate causation. Consequently, further prospective cohorts and interventional trials should be conducted to verify the outcomes we report. This study was advantageous from the perspective of sample size, which reflected a representative cross-section of diabetic patients in the capital city of Saudi Arabia. The data is recent and thus applicable to the current population. Lastly, this research fills a gap in the contemporary literature about the relation between ED visits, glycemic control and the quality of diabetes care among DM patients in the Saudi community.
In conclusion, this study demonstrated that ED visits by diabetic patients can indicate poor glycemic control, quantified by HbA1c. Additionally, the current practice of preventive diabetes care (namely, the frequency of follow-ups to monitor for possible microvascular complications) does not satisfy the current ADA recommendations. There is a need for further prospective studies on a large cohort of patients to substantiate these results and to elucidate the factors that drive the current poor practices of diabetes care.
Acknowledgment
The authors would like to thank The Med Writers through a freelance platform, Upwork for English language editing.
Footnotes
References
- 1.American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2010;33:S62–S69. doi: 10.2337/dc10-S062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization. Global report on diabetes [Internet] Available from http://www.who.int/diabetes/global-report/en/
- 3.Ogurtsova K, da Rocha Fernandes J, Huang Y, Linnenkamp U, Guariguata L, Cho N, et al. IDF Diabetes Atlas:Global estimates for the prevalence of diabetes for 2015 and 2040. Diabetes Res Clin Pract. 2017;128:40–50. doi: 10.1016/j.diabres.2017.03.024. [DOI] [PubMed] [Google Scholar]
- 4.Al-Nozha MM, Al-Maatouq MA, Al-Mazrou YY, Al-Harthi SS, Arafah MR, Khalil MZ, et al. Diabetes mellitus in Saudi Arabia. Saudi Med J. 2004;25:1603–1610. [PubMed] [Google Scholar]
- 5.Guariguata L, Whiting D, Hambleton I, Beagley J, Linnenkamp U, Shaw J. Global estimates of diabetes prevalence for 2013 and projections for 2035. Diabetes Res Clin Pract. 2014;103:137–149. doi: 10.1016/j.diabres.2013.11.002. [DOI] [PubMed] [Google Scholar]
- 6.Litzelman DK, Slemenda CW, Langefeld CD, Hays LM, Welch MA, Bild DE, et al. Reduction of lower extremity clinical abnormalities in patients with non-insulin-dependent diabetes mellitus;a randomized, controlled trial. Ann Intern Med. 1993;119:36–41. doi: 10.7326/0003-4819-119-1-199307010-00006. [DOI] [PubMed] [Google Scholar]
- 7.Dall TM, Zhang Y, Chen YJ, Quick WW, Yang WG, Fogli J. The economic burden of diabetes. Health Aff (Millwood) 2010;29:297–303. doi: 10.1377/hlthaff.2009.0155. [DOI] [PubMed] [Google Scholar]
- 8.American Diabetes Association. Standards of medical care in diabetes--2012. Diabetes Care. 2012;35:S11–S63. doi: 10.2337/dc12-s011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Childs BP, Grothe J. Optimizing self-care with diabetes complications and comorbidities. In: Weinger K, Carver CA, editors. Contemporary Diabetes:Educating Your Patient with Diabetes. New York (NY): Humana Press; 2009. [Google Scholar]
- 10.American Diabetes Association. Standards of medical care for patients with diabetes mellitus. Diabetes Care. 2003;26:S33–S50. doi: 10.2337/diacare.26.2007.s33. [DOI] [PubMed] [Google Scholar]
- 11.McGlynn EA, Asch SM, Adams J, Keesey J, Hicks J, DeCristofaro A, et al. The quality of health delivered to adults in the United States. N Engl J Med. 2003;348:2635–2645. doi: 10.1056/NEJMsa022615. [DOI] [PubMed] [Google Scholar]
- 12.Blevins T. Value and utility of self-monitoring of blood glucose in non-insulin-treated patients with type 2 diabetes mellitus. Postgrad Med. 2013;125:191–204. doi: 10.3810/pgm.2013.05.2668. [DOI] [PubMed] [Google Scholar]
- 13.McNabb WL. Adherence in diabetes:can we define it and can we measure it? Diabetes Care. 1997;20:215–218. doi: 10.2337/diacare.20.2.215. [DOI] [PubMed] [Google Scholar]
- 14.Hwang U, Concato J. Care in the emergency department:how crowded is overcrowded? Acad Emerg Med. 2004;11:1097–1101. doi: 10.1197/j.aem.2004.07.004. [DOI] [PubMed] [Google Scholar]
- 15.Miro O, Sanchez M, Espinosa G, Coll-Vinent B, Bragulat E, Milla J, et al. Analysis of patient flow in the emergency department and the effect of an extensive reorganisation. Emerg Med J. 2003;20:143–148. doi: 10.1136/emj.20.2.143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rivers EP, Nguyen HB, Huang DT, Donnino MW. Critical care and emergency medicine. Curr Opin Crit Care. 2002;8:600–606. doi: 10.1097/00075198-200212000-00020. [DOI] [PubMed] [Google Scholar]
- 17.Siegel B. The emergency department:rethinking the safety net for the safety net. Health Aff (Millwood) 2004;23:W146–W148. doi: 10.1377/hlthaff.w4.146. [DOI] [PubMed] [Google Scholar]
- 18.Chiou S, Campbell C, Horswell R, Myers L, Culbertson R. Use of the emergency department for less-urgent care among type 2 diabetics under a disease management program. BMC Health Serv Res. 2009;9:233. doi: 10.1186/1472-6963-9-223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Moss SE, Klein R, Klein BEK. Risk factors for hospitalization in people with diabetes. Arch Intern Med. 1999;159:2053–2057. doi: 10.1001/archinte.159.17.2053. [DOI] [PubMed] [Google Scholar]
- 20.Standards of Medical Care in Diabetes-2016:summary of revisions. Diabetes Care. 2016;39:S4–S5. doi: 10.2337/dc16-S003. [DOI] [PubMed] [Google Scholar]
- 21.Donnan PT, Leese GP, Morris AD. Hospitalizations for people with type 1 and type 2 diabetes compared with the nondiabetic population of Tayside, Scotland:a retrospective cohort study of resource use. Diabetes Care. 2000;23:1774–1779. doi: 10.2337/diacare.23.12.1774. [DOI] [PubMed] [Google Scholar]
- 22.Jiang H, Stryer D, Friedman B, Andrews R. Multiple hospitalizations for patients with diabetes. Diabetes Care. 2003;26:1421–1426. doi: 10.2337/diacare.26.5.1421. [DOI] [PubMed] [Google Scholar]
- 23.Raman R, Ganesan S, Pal S, Kulothungan V, Sharma T. Prevalence and risk factors for diabetic retinopathy in rural India. Sankara Nethralaya Diabetic Retinopathy Epidemiology and Molecular Genetic Study III (SN-DREAMS III), report no 2. BMJ Open Diabetes Res Care. 2014;2:e000005. doi: 10.1136/bmjdrc-2013-000005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Keenum Z, McGwin G, Witherspoon CD, Haller JA, Clark ME, Owsley C. Patients'adherence to recommended follow-up eye care after diabetic retinopathy screening in a publicly funded county clinic and factors associated with follow-up eye care use. JAMA Ophthalmol. 2016;134:1221–1228. doi: 10.1001/jamaophthalmol.2016.3081. [DOI] [PubMed] [Google Scholar]
- 25.Mtuya C, Cleland C, Philippin H, Paulo K, Njau B, Makupa W, et al. Reasons for poor follow-up of diabetic retinopathy patients after screening in Tanzania:a cross-sectional study. BMC Ophthalmol. 2016;16:115. doi: 10.1186/s12886-016-0288-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Vengadesan N, Ahmad M, Sindal MD, Sengupta S. Delayed follow-up in patients with diabetic retinopathy in South India:social factors and impact on disease progression. Indian J Ophthalmol. 2017;65:376–384. doi: 10.4103/ijo.IJO_620_16. [DOI] [PMC free article] [PubMed] [Google Scholar]


