Abstract
Cancer stem cells (CSCs) are one of the reasons for the relapse of cancer cells and metastasis. They have drug resistance against most chemotherapeutic agents. CSCs are also responsible for tumor cell heterogeneity and cause minimal residual disease. In order to achieve complete regression of tumors, CSCs have to be targeted. Recent advances in immunotherapies have shown promising outcomes in curing cancer, which are also applicable to target CSCs. CSCs express immune markers and exhibit specific immune characteristics in various cancers, which can be used in immunotherapies to target CSCs in the tumor microenvironment. Recently, various strategies have been used to target CSCs. Adaptive T-cells, dendritic cell (DC)-based vaccines, oncolytic viruses, immune checkpoint inhibitors, and combination therapies are now being used to target CSCs. Here, we discuss the feasibility of these immunological approaches and the recent trends in immunotherapies to target CSCs.
Keywords: cancer stem cells, immunotherapy, combination therapy
1. Introduction
According to cancer stem cells (CSCs) theory, CSCs are small numbers of cells that are hidden in tumors and fuel cancer growth [1]. CSCs have the capacity for self-renewal, differentiation, and tumorigenicity if relocated into an animal model [2]. The existence of CSCs or cancer-initiating cells has been reported in various cancers [3,4,5,6]. One of the greatest therapeutic struggles with cancer is to eradicate CSCs [7]. The relapse of cancer cells, heterogeneity of tumor cells, metastasis, and minimal residual disease are the major consequences of CSCs [8]. CSCs are resistant to conventional therapies, and escaped CSCs keep inducing tumor formation even after complete eradication of adult cancer cells [9]. Epithelial mesenchymal transition (EMT), interleukin-4 (IL-4) signaling, drug efflux proteins, and upregulation of aldehyde dehydrogenase (ALDH) activity are perhaps the reasons for the resistance of CSCs to conventional therapies [10]. The aberrant expression of Janus-activated kinase/signal transducer and activator of transcription, Hedgehog, Wnt, Notch, phosphatidylinositol 3-kinase/phosphatase and tensin homolog, and nuclear factor-κB signaling pathways in various CSCs have been reported [5]. In order to distinguish them from just cancer cells, different markers have been used. Most of the studies reported that the main CSC markers are CD133, CD44, IL-6R, and ALDH [11]. The CSC niche of the tumor microenvironment (TME) plays important roles in the metastasis of cancer cells, which has been reported in various cancer models [12]. Endothelial cells, myofibroblasts, and pericytes in niche participate angiocrine signals, malignant conversion, and the protection of metastasis, respectively. Co-inhibitory molecules and immune checkpoint ligands, such as programmed death-ligand 1 (PD-L1) and programmed death-ligand 2 (PD-L2), are highly expressed on CSCs of various cancers. PD-1 is receptor for these ligands, which express on immune cells. The interaction between PD-L1/PD-L2 and PD-1 aids CSCs in escaping from the killing [13,14]. In order to target these molecules of CSCs, the immune checkpoint blockade of anti-PD-L1 has been used. Previously published review articles elaborate strategies of targeting CSCs using these markers, but the major limitation is paucity of immune molecules targeting [11,15,16].
In this review, in order to understand immunotherapy-based targeting of CSCs, we covered topics related to CSCs and stem cells, surface receptors, immune escaping mechanisms, and recent trends in CSC-targeted immunotherapy.
2. CSCs and Normal Stem Cells
Normal stem cells and CSCs have similar functional capabilities. Both cells can proliferate extensively with a self-renewal ability [17]. In order to identify CSC populations in solid tumors, specific surface markers are used. Despite the fact that normal stem cells and CSCs share most markers (CD29, CD44, CD133, etc.) [18], the coexpressions of CD176 (Thomsen-Friedenreich antigen) and other surface markers can be used to characterize CSCs in tumors. Populations of CD44+, CD133+, CD176+ CSCs were reported in lung, breast, and liver cancers [19]. In prostate cancer, coexpressions of CD44, α2β1 integrin, CD133, CD49f, and CD176 were characterized as stem cell-like cells [20].
Mutations in stem cells can raise cancer stem-like cells, and some studies reported this transformation. Genomic instability and abrogated tumor suppression mechanisms are associated with this transformation [21]. Environmental aberrancy during differentiation of embryonic stem cells leads to CSCs, which are characterized by spontaneously accumulated DNA lesions with senescence and apoptosis resistance [22]. Malignant liposarcomas were aroused from induced pluripotent stem cells under the influence of tumor-derived extracellular vesicles, which were isolated from the conditioned medium of a mouse lewis lung carcinoma cell line [23]. The oncogenic manipulation of mouse embryonic stem cells can generate cancer-like stem cells, which was reported in an ovarian teratoma in vivo model. The insertion of oncogenic elements—SV40 LTg and HrasV12—by using a mouse stem virus long terminal repeat-based retroviral system induced cancer-like stem cells [24].
The formation of CSCs from nonstem cancer cells (NSCCs) has also been reported. Interleukin-6 mediates the maintenance of tumor heterogeneity through a dynamic equilibrium between CSCs and NSCCs. The conversion of NSCCs to CSCs was reported in genetically different breast cell lines, human breast tumors, and a prostate cell line. This transformation is mediated by IL-6 secretion. Differential expressions of various microRNAs were also reported in this transformation [25]. The role of hypoxia in CSCs formation from NSCCs was demonstrated in colorectal cell lines. Hypoxia prevents differentiation of enterocytes and goblet cells by downregulating CDX1 and Notch1 [26].
3. Surface Receptors on CSCs
CSCs express various immune receptors on their surfaces. These receptors play key roles in the therapeutic resistance and metastasis of cancers. The roles of CSC surface receptors in tumorigenesis and immune resistance have been reported. The leucine-rich repeat-containing G-protein-coupled receptor 5 (Lgr5) is identified as colorectal cancer (CRC). CSCs and its cell ablation restricts primary tumors, but they do not completely suppress tumor formation. Proliferative Lgr5− cells attempt to replenish the Lgr5+ CSC pool in the TME and promote rapid re-initiation of tumor growth upon treatment cessation [27]. CD95 expression and CD95 signaling are associated with EMT differentiation programs in gastrointestinal cancer [28]. It is also demonstrated that stimulation of CD95 maintains the CSC pool of an increased number of cancer cells with stem cell traits [29]. The constitutive expression of HLA-E on glioblastoma stem-like cells inhibits NK cell-mediated lysis [30]. CD133+ CSCs in colon cancer are resistant to apoptosis due to production of IL-4. Treatment with an IL-4Rα antagonist or anti-IL-4 neutralizing antibody enhanced the antitumor efficacy of standard drugs and confirmed the autocrine mechanism of IL-4 in CSCs in colon cancer [31]. In CRC patients, the higher CD133+ CSCs proportion was associated with lower numbers of activated dendritic cells (DCs) [32]. The expression pattern of three surface receptors—CD133, Trop-2, and α2β1 integrin—have been identified as putative markers in human prostate cancer [33]. Platelet-derived growth factor receptors α and β (PDGFR-α/β) were upregulated and promoted migration, invasion, and chemotherapy resistance in sarcoma CSCs. The PDGFR-α/β can be targeted as potential therapeutic candidates for sarcoma treatment [34]. In ovarian CSCs, receptor tyrosine kinase-like orphan receptor 1 (ROR1) expression revealed its functional role in promoting migration/invasion. Humanized mAb (specific for ROR1 (UC-961)) inhibited the capacity of ovarian cancer cells to migrate and form spheroides [35]. Toll-like receptor 4 expression on CSCs of hepatocellular carcinoma (HCC) was reported. It was associated with tumor invasion, migration, and a poor prognosis of HCC [36]. The high expression of MHC I in melanoma, colon cancer, and pancreatic cancer is associated with CDK1 upregulation. Further, the interaction between CDK1 and Sox2 promotes tumor initiation in human melanoma [37]. Inhibition of the MDM2-p53 interaction reduces ALDHhigh and CD44high CSCs in mucoepidermoid carcinoma. A marked decrease in expression of Bmi-1 and in a fraction of ALDHhigh CD44high was demonstrated in this model [38]. Rapid tumorigenesis was associated with the surface expression of PD-L1, E-cadherin, CD24, and VEGFR2 in epithelial CSCs, which was established from the ascites of a bladder cancer patient. These surface expressions were also closely linked with signatures of immune evasion, increased stemness, increased calcium signaling, transformation, and novel E-cadherin–RalBP1 interaction [39]. PD-L1 expression on CSCs of breast cancer promotes the expression of OCT-4A and Nanog transcription factors. These expressions sustain the stemness of breast cancer through the activation of the PI3K/AKT pathway [40]. Apart from these roles, some of the surface receptors have been commonly used to characterize CSCs and projected as biomarkers in various cancers (Table 1).
Table 1.
Cancer stem cells (CSCs) biomarkers in various cancers.
| Cancer | Biomarkers | Reference |
|---|---|---|
| Colorectal Cancer | CD133, CD24, CD29, CD44, CD166, EpCAM, Lgr5 | [41,42] |
| Gastric Carcinoma | CD44, CD133, CD166, EpCAM | [43] |
| Head and Neck Carcinomas | CD44, CD133, CD166 | [44] |
| HCC | CD133, CD44, CD90, CD13, OVC, EpCAM | [45,46] |
| Prostate cancer | Integrins, CD44, CD133, CD166, Trop2, CD117, ABCG2 | [47] |
| Ovarian cancer | CD24, CD44, CD117, CD133, ABCG2, EpCAM | [48] |
Abbreviations: ABCG2, ATP-binding cassette super-family G member 2; EpCAM, Epithelial cell adhesion molecule; HCC, hepatocellular carcinoma.
4. Immune Escaping of CSCs and TME
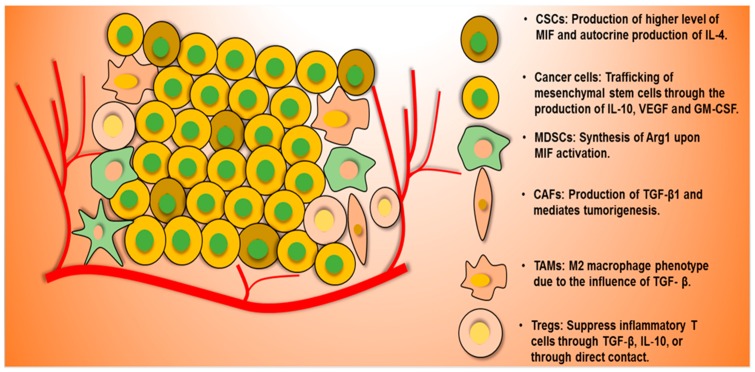
CSCs, having a low expression of MHC I molecules, natural killer cells (NK cells) receptors, and other innate immune receptors, can escape from killing by cancer killer cells such as NK cells and T-cells. Most of the signaling pathways, which participate in normal stem cell physiological roles, such as EGF/EGFR, FGF/FGFR, Hedgehog, HER2, JAK/STAT, MAPK, Myc, NF-κB, PTEN/PI3K, and Wnt, are dysregulated in CSCs as receptors, ligands, oncogenes, or transcription factors, according to the context and types of cancers. It has also been observed that normal stem cells markers (Nanog, Sox2, Oct4, and Klf) are over-expressed in CSCs. These aberrant expressions make CSCs immunoresistant against antitumor immunity [49,50]. In addition, a TME consists of both immune cells and stromal cells, with cancer cells as well as CSCs; tumor-associated macrophages (TAMs), tumor-infiltrating lymphocytes (TILs), regulatory T-cells, myeloid derived suppressor cells (MDSCs), DCs, NK cells, and natural killer T-cells are filtrated from bone marrow. Stromal cells include blood and lymphatic endothelial cells and cancer-associated fibroblasts [51]. They secrete various cytokines and chemokines (which are also responsible for their antitumor immunity), metastasis, and suppression in the anticancer therapeutic efficacy [52,53]. The interactions between CSCs and cellular components through these cytokines and chemokines severely suppress antitumor immunity [54]. The general roles of each type of cells in a TME are shown in Figure 1. For instance, the markers expressed in CSCs and immune cells affect the prognosis of stage III colon cancer patients. Patients categorized as SOX2low/FoxP3high expression showed good prognosis, whereas patients categorized as SOX2high/PD-L1low indicated poor prognosis [55]. Furthermore, other mechanisms have been reported in various cancers and are summarized in Table 2.
Figure 1.
General roles of CSCs and other cells in tumor microenvironment (TME) and the mechanisms of immune escaping, and tumorigenesis. CSCs produces of higher level of migration inhibitory factor (MIF) and autocrine production of IL-4 in order to escape macrophage killing. Cancer cells produce IL-10, VEGF, and GM-CSF, which are involved in trafficking of mesenchymal stem cells. Myeloid derived suppressor cells (MDSCs) secrete Arg1 through MIF1 activation. CAFs mediate tumorigenesis through TGF-β. M2 macrophage promotes tumorigenesis for TGF-β response. TGF-β and IL-10 of T-regulatory cells suppress T-effector cells. (Abbreviations: CAFs, cancer-associated fibroblasts; CSC, cancer stem cells; FAS, fas cell surface death receptor; GM-CSF, granulocyte-macrophage colony-stimulating factor; IL-10, interleukin-10; MDSCs, myeloid-derived suppressor cells, TGF-β, tumor growth factor-beta; VEGF, vascular endothelial growth factor).
Table 2.
Immune resistance of CSCs and their mechanism in various cancers.
| CSCs in Cancer | Immune Molecules | Immunological Characterization | Mechanism of Action | Reference |
|---|---|---|---|---|
| Glioblastoma multiforme | MHC-I, MHC-II and NKG2D | Weakly positive for MHC-I, MHC-II, and negative for NKG2D ligand molecules | Lower immunogenicity and higher suppressive activity of GBM CSCs | [56] |
| MIC-1 | MΦ inhibitory cytokine-1 (MIC-1) | Inhibition of MΦ/microglia phagocytosis and T-cell proliferation | [57] | |
| B7-H1 and soluble galectin-3 | B7-H1 and soluble galectin-3 | Inhibition of T-cell proliferation and induction of T regulatory cell activation | [58] | |
| MIF and Arg1 | CSCs produce higher level of macrophage migration inhibitory factor (MIF) | CSCs released MIF induces Arg1 from MDSCs through CXCR mediated mechanism. Arg1 suppresses T-cell antitumor activity | [59] | |
| TLR4 | Reduced TLR4 Expression | TBK1 expression through TLR4 signals to suppress RBBP5 | [60] | |
| Colon cancer | IL-4 | Autocrine production of IL-4 | Tumor growth and treatment resistant | [31] |
| IL-4 | High expression of IL-4 and expression of CRC-associated Ag COA-1 | IL-4 and CIC-mediated suppression of anti-tumor T-cell responses | [61] | |
| Melanoma | IL-2 | Inhibition of IL-2 dependent T-cell action and induction of CD4+ CD25+ FoxP3+ regulatory T-cells | Evasion of antitumor immunity and immunotherapeutic resistance | [62] |
| Breast cancer | MICA, MICB and NKG2D | Downregulation of ligands, MICA and MICB for stimulatory NK cell receptor NKG2D | Autologous/allogeneic NK cells toxicity resistant | [63] |
| CD47 | Over expression of CD47 on CSCs by HIF-1 | HIF-1-induced CD47 expression on CSCs and cancer cells escapes from phagocytosis by bone marrow-derived macrophages | [64] | |
| PD-L1 | Enriched PD-L1 expression through EMT/βcatenin/STT3/PD-L1 signaling axis | EMT and MET upregulate PD-L1 through STT3-dependent PD-L1 N-glycosylation | [65] | |
| Pancreatic adenocarcinoma | CXCR4 | CD133+ and CD133+ CXCR4+ CSCs | CD133+ CSCs responsible for tumorigenic and highly resistant to standard chemotherapy. CD133+ CXCR4+ CSCs dictate metastatic phenotype of the individual tumor | [66] |
| TGF-β1 | Interaction between hCAP-18/LL-37 expression of stroma of PDAC and TGF- β1 | hCAP-18/LL-37 expression of stroma of PDAC and TGF- β1 mediated tumorigenesis | [67] | |
| Ovarian cancer | CXCR4 and CXCL12 | CXCR4+CD133+ OVCAR-5 cells were resistant to cisplatin | Overexpression of ABCG2 drug transport and migrates towards CXCR4 ligand and CXCL12 | [68] |
Abbreviations: ABCG2, ATP-binding cassette super-family G member 2; AgCOA-1, antigen COA1; Arg1, arginase 1; B7-H1, B7 homolog 1; CICs, cancer-initiating cells; CSCs, cancer stem cells; CRC, colorectal cancer; CXCR, C-X-C chemokine receptor; CXCR4, C-X-C chemokine receptor 4; CXCL12, C-X-C motif chemokine 12; EMT, epithelial mesenchymal transition; GBM, glioblastoma multiforme; hCAP-18/LL-37, human cationic antimicrobial protein18 leucine leucine-37; HIF-1, hypoxia-inducible factor; IL-4, interleukin 4; MET, mesenchymal–epithelial transition; MHC I; major histocompatibility complex I; MHC II, major histocompatibility complex II; MICA, MHC class I polypeptide-related sequence A; MICB, MHC class I polypeptide-related sequence B; NK cells, natural killer cells; NKG2D, natural killer group 2D; PDAC, pancreatic ductal adenocarcinoma; PD-L1, programmed death-ligand 1; RBBP5, retinoblastoma binding protein; STT3,dolichyl-diphosphooligosaccharide-protein glycosyltransferase subunit STT3; TBK1, tank-binding kinase 1; TGF- β1, transforming growth factor-beta 1; TLR4, toll-like receptor 4.
5. Targeting CSCs by Immunotherapy
Immunotherapy targets CSCs through immune cells such as cytokine-induced killer (CIK) cells, NK cells, γδ T-cells, and CD8+ T-cells. DC-based vaccines also target CSCs [69]. Besides, oncolytic virotherapy (OVT) induces antitumor immunity through immunogenic cell death and the activation of the T-cell [70]. It also targets CSCs in combination with other immunotherapies. Recently, most of the targeting strategies use combination therapy, which is commonly consisted of DC-based vaccines, oncolytic viruses, and immune checkpoint blockades. The eradication of CSCs and its therapeutic efficacy are usually associated with the infiltration of lymphocytes, M1 macrophage polarization, and the induction of antitumor cytokines in the TME. The targeting strategies against CSCs in various cancers are listed in Table 3.
Table 3.
Recent advances in targeting CSCs by immunotherapy.
| Immuno-Therapy | Targeting Approach | Cancer Model | Reference |
|---|---|---|---|
| Adoptive T-cell therapy | CAR T-cells against EpCAM antigen. Peripheral blood lymphocytes expressing EpCAM-specific chimeric antigen receptors targeted EpCAM+ CSCs | Prostate cancer | [72] |
| CAR T-cells, targeting membrane bound IL-15 | Leukemia | [73] | |
| CD8+ cytotoxic T-cells, specific for the CSCs antigen ASB4 | Colon cancer | [74] | |
| CIK cells transduced with CAR T- cells against CD123 | Acute myeloid leukemia | [75] | |
| Autologous CIK cells | Melanoma | [76] | |
| CIK cells-NKG2D ligands | HCC | [77] | |
| CIK cells- NKG2D ligands | Nasopharyngeal carcinoma | [78] | |
| NK cells from healthy donors | High-grade non-muscle invasive bladder cancer | [79] | |
| NK cells | Pancreatic cancer | [80] | |
| NK cells | Oral squamous carcinoma | [81] | |
| γδ and CD8+ T-cells | Breast cancer | [82] | |
| DC-based vaccine | CSCs lysate-pulsed DCs | Malignant melanoma | [83] |
| CSCs lysate-pulsed DCs | Squamous cell carcinoma | [84] | |
| DCs charged with total lysates of Panc-1 CSCs | Pancreatic cancer | [85] | |
| DCs loaded with NANOG peptide | Ovarian cancer | [86] | |
| ALDHhigh SCC7 specific CSCs-DCs | Squamous cell cancer | [87] | |
| ALDHhigh D5 CSCs-DCs | Metastatic melanoma | ||
| ALDHhigh CSC-pulsed DCs | Metastatic melanoma | [88] | |
| ALDHhigh CSC-pulsed DCs | Squamous cell cancer | ||
| Oncolytic virotherapy | Oncolytic herpes simplex virus armed with IL-12 | Glioblastoma | [89] |
| Oncolytic adenovirus targeting CD133+ CSCs | Glioblastoma | [90] | |
| Oncolytic vaccinia virus (GLV-1h68) targeting ALDHhigh stem cell-like cancer cells | Breast cancer | [91] | |
| Oncolytic vaccinia virus targeting ID8-T tumor model that harbors CD44+ CD117+ cancer-initiating cells | Ovarian cancer | [92] | |
| Cancer-favoring oncolytic vaccinia virus: stem-cell-like colon (CD133+ and CD44+) cancer cells | Colon cancer | [42] | |
| Oncolytic measles viruses: targeting CD133+ tumor-initiating cells | HCC | [93] | |
| Cancer-favoring oncolytic vaccinia virus: metastatic hepatocellular carcinoma (CD44+) | HCC | [46] | |
| Others | Monoclonal antibody against Lgr5 | Colon cancer | [94] |
| IFN-β therapy: targeting type I IFN signaling | Triple negative breast cancer | [49] | |
| Blockade of the IL-8 receptor | Breast cancer | [95] | |
| Combination therapy | DC-based vaccine in combination with anti-PD-L1 and anti-CTLA-4 | Melanoma | [96] |
| Oncolytic herpes simplex virus in combination with anti-PD-1 and anti-CTLA-4 | Glioblastoma | [97] | |
| STDENVANT (a vaccine comprising of GSC lysate, DCs, and TLR9 agonist CpG motif-containing oligo-deoxynucleotides) in combination with anti-PD-L1 | Glioblastoma | [98] | |
| CSCs vaccine (streptavidin-granulocyte-macrophage-colony stimulating factor surface-modified bladder CSCs) in combination with anti-PD-1 | Bladder cancer | [99] |
Abbreviations: ALDH, aldehyde dehydrogenase; CAR, chimeric antigen receptor; CCR7, CC-chemokine receptor 7; CIK cells, Cytokine-induced killer cells; CRC, colorectal cancer; CSCs, cancer stem cells; CTLA-4, cytotoxic T-lymphocyte–associated antigen 4; CXCR1, C-X-C chemokine receptor 1; DC, dendritic cells; HCC, hepatocellular carcinoma; IFN-β, interferon-beta; IFN-γ, interferon-gamma; IL-8, interleukin 8; IL-12, interleukin 12; NK, natural killer; NKG2D, natural killer group 2D; PD-1, Programmed cell death-1; PD-L1, programmed death-ligand 1; TLR9, toll-like receptor 9.
5.1. Adoptive T-Cell Therapy
Adoptive T-cell therapy (ACT) is a type of personalized therapy that uses cancer-bearing host immune cells with direct anticancer activity to treat cancer. TILs from naturally occurring tumors have intrinsic antitumor activity. ACT involves the isolation of TILs from a patient, cultured in the presence of IL-2 and evaluation of specific tumor recognition. These processes are followed by the reinfusion of selected TILs to the same patient [71]. Recently, engineered T-cells with chimeric antigen T-cell receptors (CAR T-cells) against the antigens of CSCs have also been developed and evaluated in various cancer models. In prostate cancer, CAR T-cells targeted against EpCAM antigens eradicated CSCs in PC3M and PC3 tumor models [72]. CAR T-cells engineered with membrane-bound chimeric IL-15 induce CSC memory T-cells in tumor-specific T-cells in CD19+ leukemia [73]. The selective killing of CSCs by adoptively transferred CD8+ cytotoxic T-cells, specific for the CSCs antigen ASB4, was reported colon cancer [74].
Adoptive immunotherapy also includes the adoptive transfer of cytokine-induced killer (CIK) cells. CIK cells with CAR T-cells that are transduced against CD123 strongly killed CD123+ cell lines and primary acute myeloid leukemia cells [75]. MHC-independent antitumor activity in chemotherapy and BRAF inhibitor-surviving CSCs was reported in melanoma [76]. A partial NKG2D-ligands recognition with CSCs and its therapeutic efficacy by CIK cells was shown in HCC and nasopharyngeal carcinoma [77,78].
The adoptive transfer of NK cells from healthy donors showed the killing of stem-like and differentiated tumor cells upon activation with IL-2 and IL-15. CSCs that shifted towards being susceptible to cisplatin therapy were also noted in high-grade non-muscle invasive bladder cancer [79]. In various cancer models, the adoptive transfer of NK cells led to upregulation of NK cells activation ligands, such as MICA/B, Fas and DR5 on CSCs. NKG2D-dependent mechanisms of killing of CSCs were also revealed in these models [80]. The adoptive transfer of NK cells in oral squamous carcinoma showed the expansion and functional activation of super-charged NK cells by osteoclast in both an IL-12- and an IL-15-dependent manner against CSCs [81].
The adoptive transfers of γδ and CD8+ T-cells upregulated MHC class I and CD54/ICAM-1 on CSC-like cells and induced antigen specific-killing by CD8+ T-cells in breast cancer. Synergism between MHC-restricted and non-MHC-restricted T-cells was shown in this model [82].
5.2. DC-Based Vaccines
The therapeutic efficacy of DC-based vaccines against CSCs have been reported in various cancers. DCs pulsed with cancer cell lines or CSC lysates were used as vaccines to evaluate the therapeutic efficacy. In the malignant melanoma model, CSCs lysate-pulsed DCs induced IFN-γ and IL-4 secretion in vaccinated mice. These effects mediated the suppression of tumor growth and prolonged survival in immunized mice [83]. The downregulation of chemokine (C-C motif) receptors CCR7, CCR10, and their ligands CCL21, CCL27, and CCL28 were associated with therapeutic efficacy in melanoma and squamous cell carcinoma [84]. DCs charged with total lysates of Panc-1 CSCs induced INF-γ and IL-2 secretion, and mediated lymphocytes were reported in pancreatic cancer in an in vitro model [85]. DCs loaded with NANOG peptides induced highly specific anti-tumor T-cell responses against CSCs in ovarian cancer [86]. An ALDHhigh SCC7-specific CSC-DC vaccine showed the reduction of local tumor relapse and prolonged host survival in squamous cell cancer. As a metastatic model, in D5 melanoma, the inhibition of primary tumor growth, reduced spontaneous lung metastases, and increased host survival were reported. These therapeutic efficacies were associated with the downregulation of CCR10 on ALDHhigh D5 CSCs and its ligands on lung tissues [87]. Furthermore, the therapeutic efficacy of DC-based vaccines was successfully shown in immunocompetent murine models. Using ALDHhigh CSC-pulsed DCs in D5 melanoma and SCC7 squamous cell cancer models, high levels of IgG bound CSCs and CSCs lysis in presence of complement were reported Cytotoxic T Lymphocytes (CTLs) harvested from peripheral blood mononuclear cells or splenocytes of vaccinated mice were also capable of killing CSCs in vitro [88].
5.3. Oncolytic Virotherapy (OVT)
OVT induces antitumor immunity through immunogenic cell death and the activation of T-cells. Various studies indicated the therapeutic efficacy of OVT against CSCs. Oncolytic herpes simplex virus armed with IL-12 (G47∆-mIL12) infection and the induction of tumor regression were reported in syngeneic mice bearing intracerebral 005 tumors. An IFN-γ release, the inhibition of angiogenesis, and a reduction of the number of regulatory T-cells in the tumor were also noted in glioblastoma [89]. The selective infection of CD133-targeted oncolytic adenovirus in CD133+ CSCs was also reported in glioblastoma [90]. The oncolytic vaccinia virus, GLV-1h68 strain selectively replication, and killing of stem cell-like cancer cells (higher ALDH1 activity) were reported in breast cancer model [91]. In ovarian cancer, the killing of CD44+ CD117+ cancer-initiating cells by CXCR4 antagonist expressed-oncolytic vaccinia virus infection was reported [92]. The cancer-favoring oncolytic vaccinia virus’ selective infection and therapeutic efficacy against stem-cell-like colon (CD133+ and CD44+) cancer cells in combine with fluorouracil were reported in colon cancer [42]. Oncolytic measles viruses targeted and lysed CD133+ tumor-initiating cells in HCC [93].
5.4. Other Immunotherapeutic Approaches
Other immunotherapeutic approaches, like blockades against immune receptors and ligands, were also used target CSCs in bulk tumors. A monoclonal antibody against Lgr5 in colon cancer showed the suppression of Lgr5, Wnt pathway in CSCs and tumor volume reduction [94]. In triple negative breast cancer, the IFN-β mediated suppression of E-M/CSC plasticity by re-engaging type I IFN signaling in CSCs was reported [49]. A blockade of the IL-8 receptor CXCR1 caused the induction of aggressive apoptosis through FASL/FAS signaling and it was mediated by the FAK/AKT/FOXO3A pathway in CSCs of breast cancer [95].
5.5. Combination Immunotherapy
To target and complete eradicate of CSCs, combined immunotherapy approaches have been developed recently. A DC-based vaccine in combination with anti-PD-L1 and anti-CTLA-4 showed the elimination of ALDHhigh CSCs, enhanced T-cell expansion, suppressed TGF-β secretion, enhanced IFN-γ secretion, and significantly enhanced host specific CD8+ T-cells against CSCs in mouse melanoma [96]. An oncolytic herpes simplex virus expressing IL-12 eradicated glioblastoma stem-like cells in combination with anti-PD-1 and anti-CTLA-4. CD4+, CD8+ T-cells, intratumoral M1-like macrophages, and an increased ratio of ‘T effector: T regulatory cells’ was responsible for the therapeutic efficacy of triple combination efficacy in glioblastoma [97]. In another glioblastoma study, STDENVANT, a vaccine comprising GSC lysate, DCs, and TLR9 agonist CpG motif-containing oligodeoxynucleotides with anti-PD-L1, showed greater survival advantage and decreased the Treg cell population in the brain [98]. Combination therapy consisted of a streptavidin-granulocyte-macrophage-colony stimulating factor surface-modified bladder CSCs vaccine with anti-PD-1 showed an increase in the population of CD4+, CD8+, and CD8+ IFN-γ+ cells and a strong induction of a specific antitumor immune response against bladder cancer [99].
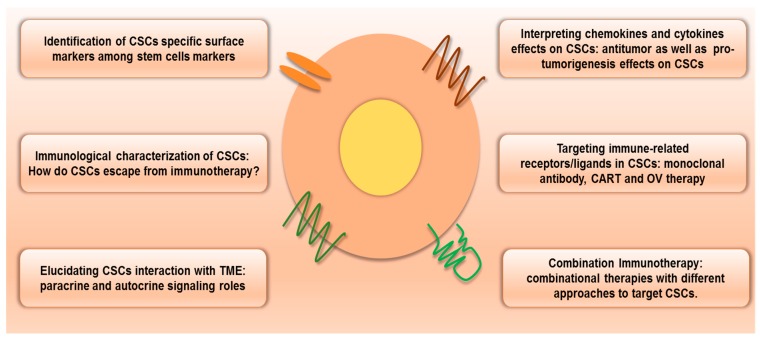
6. Conclusions
As a sub population of bulk tumors, CSCs resist conventional cancer therapies, escaping from antitumor immunity through lower expression of immune recognizing receptors. The TME and niche also play vital roles in immune escaping. Various cytokines and chemokines of stromal cells and immune cells in the TME severely suppress antitumor immune activity against CSCs. Combination immunotherapies would be an ideal approach to restore antitumor immunity against CSCs. These approaches may help the complete eradication of CSCs. However, a more immunological characterization of CSCs and interactions between cellular components in the TME must be revealed. Prospective immunotherapeutic approaches to target CSCS may need to understand CSCs, their niche, and the TME together with related mechanisms (Figure 2). The TME includes various immune cells, nonimmune cells, cancer cells, and CSCs. Interaction between cellular components in the TME can affect other cells’ fates through cytokines and chemokines. These can be considered for CSC-targeted therapy. Recently, a relapse pathway of glioblastoma has been elucidated through single cell molecular analysis. Within single cells, it found three mutated genes involved in the RAS/GEF GTP-dependent signaling pathway in glioblastoma [100]. Single cell molecular analysis can be applied to reveal the interfaces of immune cells, stromal cells, cancer cells, and CSCs in the TME. This approach could elucidate the heterogeneity of tumor progression. These approaches may contribute to develop more smart CSC-targeted therapeutic approaches [101].
Figure 2.
Prospective immunotherapeutic approaches to target CSCs. In order to target CSCs by immunotherapy, the identification CSCs specific surface markers and the immunological characterization of immune escaping with a complete elucidation of interaction with the TME are required. Chemokines’ and cytokines’ roles on CSCs are also related to immunotherapy. Immune receptors/ligands-based targeting by monoclonal antibody, CART and OV therapy. Owing to increase therapeutic efficacy, combination immunotherapy that consists of different approaches to target CSCs would be an ideal one (Abbreviations: CART, chimeric antigen receptor T-cells; CSCs, cancer stem cells; TME, tumor microenvironment, OV, oncolytic viruses).
Author Contributions
Conceptualization, S.Y.Y.; writing the manuscript, N.B. and S.Y.Y.; supervision, S.Y.Y.; project administration, S.Y.Y.
Funding
This research was supported by the Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education (Grant no. NRF-2016R1D1A1B03935221, NRF-2017R1C1B5015034, and NRF-2018R1D1A1B07050358).
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Batlle E., Clevers H. Cancer stem cells revisited. Nat. Med. 2017;23:1124–1134. doi: 10.1038/nm.4409. [DOI] [PubMed] [Google Scholar]
- 2.Yu Z., Pestell T.G., Lisanti M.P., Pestell R.G. Cancer stem cells. Int. J. Biochem. Cell Biol. 2012;44:2144–2151. doi: 10.1016/j.biocel.2012.08.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zhang S., Balch C., Chan M.W., Lai H.C., Matei D., Schilder J.M., Yan P.S., Huang T.H., Nephew K.P. Identification and characterization of ovarian cancer-initiating cells from primary human tumors. Cancer Res. 2008;68:4311–4320. doi: 10.1158/0008-5472.CAN-08-0364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Singh S.K., Hawkins C., Clarke I.D., Squire J.A., Bayani J., Hide T., Henkelman R.M., Cusimano M.D., Dirks P.B. Identification of human brain tumour initiating cells. Nature. 2004;432:396–401. doi: 10.1038/nature03128. [DOI] [PubMed] [Google Scholar]
- 5.Ricci-Vitiani L., Lombardi D.G., Pilozzi E., Biffoni M., Todaro M., Peschle C., De Maria R. Identification and expansion of human colon-cancer-initiating cells. Nature. 2007;445:111–115. doi: 10.1038/nature05384. [DOI] [PubMed] [Google Scholar]
- 6.Lapidot T., Sirard C., Vormoor J., Murdoch B., Hoang T., Caceres-Cortes J., Minden M., Paterson B., Caligiuri M.A., Dick J.E. A cell initiating human acute myeloid leukaemia after transplantation into scid mice. Nature. 1994;367:645–648. doi: 10.1038/367645a0. [DOI] [PubMed] [Google Scholar]
- 7.Kaur G., Sharma P., Dogra N., Singh S. Eradicating cancer stem cells: Concepts, issues, and challenges. Curr. Treat. Options Oncol. 2018;19:20. doi: 10.1007/s11864-018-0533-1. [DOI] [PubMed] [Google Scholar]
- 8.Pattabiraman D.R., Weinberg R.A. Tackling the cancer stem cells—What challenges do they pose? Nat. Rev. Drug Discov. 2014;13:497–512. doi: 10.1038/nrd4253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kaiser J. The cancer stem cell gamble. Science. 2015;347:226–229. doi: 10.1126/science.347.6219.226. [DOI] [PubMed] [Google Scholar]
- 10.Doherty M.R., Smigiel J.M., Junk D.J., Jackson M.W. Cancer stem cell plasticity drives therapeutic resistance. Cancers. 2016;8:8. doi: 10.3390/cancers8010008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Codd A.S., Kanaseki T., Torigo T., Tabi Z. Cancer stem cells as targets for immunotherapy. Immunology. 2018;153:304–314. doi: 10.1111/imm.12866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kise K., Kinugasa-Katayama Y., Takakura N. Tumor microenvironment for cancer stem cells. Adv. Drug Deliv. Rev. 2016;99:197–205. doi: 10.1016/j.addr.2015.08.005. [DOI] [PubMed] [Google Scholar]
- 13.Wu Y., Chen M., Wu P., Chen C., Xu Z.P., Gu W. Increased pd-l1 expression in breast and colon cancer stem cells. Clin. Exp. Pharmacol. Physiol. 2017;44:602–604. doi: 10.1111/1440-1681.12732. [DOI] [PubMed] [Google Scholar]
- 14.Dong P., Xiong Y., Yue J., Hanley S.J.B., Watari H. Tumor-intrinsic pd-l1 signaling in cancer initiation, development and treatment: Beyond immune evasion. Front. Oncol. 2018;8:386. doi: 10.3389/fonc.2018.00386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kim Y.J., Siegler E.L., Siriwon N., Wang P. Therapeutic strategies for targeting cancer stem cells. J. Cancer Metastasis Treat. 2016;2:233. doi: 10.20517/2394-4722.2016.26. [DOI] [Google Scholar]
- 16.Yoshida G.J., Saya H. Therapeutic strategies targeting cancer stem cells. Cancer Sci. 2016;107:5–11. doi: 10.1111/cas.12817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Shackleton M. Normal stem cells and cancer stem cells: Similar and different. Semin. Cancer Biol. 2010;20:85–92. doi: 10.1016/j.semcancer.2010.04.002. [DOI] [PubMed] [Google Scholar]
- 18.Kim W.-T., Ryu C.J. Cancer stem cell surface markers on normal stem cells. BMB Rep. 2017;50:285–298. doi: 10.5483/BMBRep.2017.50.6.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lin W.M., Karsten U., Goletz S., Cheng R.C., Cao Y. Expression of cd176 (thomsen-friedenreich antigen) on lung, breast and liver cancer-initiating cells. Int. J. Exp. Pathol. 2011;92:97–105. doi: 10.1111/j.1365-2613.2010.00747.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Li F., Glinskii O.V., Mooney B.P., Rittenhouse-Olson K., Pienta K.J., Glinsky V.V. Cell surface thomsen-friedenreich proteome profiling of metastatic prostate cancer cells reveals potential link with cancer stem cell-like phenotype. Oncotarget. 2017;8:98598–98608. doi: 10.18632/oncotarget.21985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yoshioka K., Atsumi Y., Nakagama H., Teraoka H. Development of cancer-initiating cells and immortalized cells with genomic instability. World J. Stem Cells. 2015;7:483–489. doi: 10.4252/wjsc.v7.i2.483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fujimori H., Shikanai M., Teraoka H., Masutani M., Yoshioka K. Induction of cancerous stem cells during embryonic stem cell differentiation. J. Biol. Chem. 2012;287:36777–36791. doi: 10.1074/jbc.M112.372557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yan T., Mizutani A., Chen L., Takaki M., Hiramoto Y., Matsuda S., Shigehiro T., Kasai T., Kudoh T., Murakami H., et al. Characterization of cancer stem-like cells derived from mouse induced pluripotent stem cells transformed by tumor-derived extracellular vesicles. J. Cancer. 2014;5:572–584. doi: 10.7150/jca.8865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cho S., Park H., Jarboe E.A., Peterson C.M., Bae Y.H., Janat-Amsbury M.M. Design and characterization of bioengineered cancer-like stem cells. PLoS ONE. 2015;10:e0141172. doi: 10.1371/journal.pone.0141172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Iliopoulos D., Hirsch H.A., Wang G., Struhl K. Inducible formation of breast cancer stem cells and their dynamic equilibrium with non-stem cancer cells via il6 secretion. Proc. Natl. Acad. Sci. USA. 2011;108:1397–1402. doi: 10.1073/pnas.1018898108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yeung T.M., Gandhi S.C., Bodmer W.F. Hypoxia and lineage specification of cell line-derived colorectal cancer stem cells. Proc. Natl. Acad. Sci. USA. 2011;108:4382–4387. doi: 10.1073/pnas.1014519107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.De Sousa e Melo F., Kurtova A.V., Harnoss J.M., Kljavin N., Hoeck J.D., Hung J., Anderson J.E., Storm E.E., Modrusan Z., Koeppen H., et al. A distinct role for lgr5(+) stem cells in primary and metastatic colon cancer. Nature. 2017;543:676–680. doi: 10.1038/nature21713. [DOI] [PubMed] [Google Scholar]
- 28.Zheng H., Li W., Wang Y., Xie T., Cai Y., Wang Z., Jiang B. Mir-23a inhibits e-cadherin expression and is regulated by ap-1 and nfat4 complex during fas-induced emt in gastrointestinal cancer. Carcinogenesis. 2014;35:173–183. doi: 10.1093/carcin/bgt274. [DOI] [PubMed] [Google Scholar]
- 29.Ceppi P., Hadji A., Kohlhapp F.J., Pattanayak A., Hau A., Liu X., Liu H., Murmann A.E., Peter M.E. Cd95 and cd95l promote and protect cancer stem cells. Nat. Commun. 2014;5:5238. doi: 10.1038/ncomms6238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wolpert F., Roth P., Lamszus K., Tabatabai G., Weller M., Eisele G. Hla-e contributes to an immune-inhibitory phenotype of glioblastoma stem-like cells. J. Neuroimmunol. 2012;250:27–34. doi: 10.1016/j.jneuroim.2012.05.010. [DOI] [PubMed] [Google Scholar]
- 31.Todaro M., Alea M.P., Di Stefano A.B., Cammareri P., Vermeulen L., Iovino F., Tripodo C., Russo A., Gulotta G., Medema J.P., et al. Colon cancer stem cells dictate tumor growth and resist cell death by production of interleukin-4. Cell Stem Cell. 2007;1:389–402. doi: 10.1016/j.stem.2007.08.001. [DOI] [PubMed] [Google Scholar]
- 32.Szarynska M., Olejniczak A., Kobiela J., Laski D., Sledzinski Z., Kmiec Z. Cancer stem cells as targets for dc-based immunotherapy of colorectal cancer. Sci. Rep. 2018;8:12042. doi: 10.1038/s41598-018-30525-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Trerotola M., Rathore S., Goel H.L., Li J., Alberti S., Piantelli M., Adams D., Jiang Z., Languino L.R. Cd133, trop-2 and α2β1 integrin surface receptors as markers of putative human prostate cancer stem cells. Am. J. Transl. Res. 2010;2:135. [PMC free article] [PubMed] [Google Scholar]
- 34.Chang K.K., Yoon C., Yi B.C., Tap W.D., Simon M.C., Yoon S.S. Platelet-derived growth factor receptor-alpha and -beta promote cancer stem cell phenotypes in sarcomas. Oncogenesis. 2018;7:47. doi: 10.1038/s41389-018-0059-1. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 35.Zhang S., Cui B., Lai H., Liu G., Ghia E.M., Widhopf G.F., 2nd, Zhang Z., Wu C.C., Chen L., Wu R., et al. Ovarian cancer stem cells express ror1, which can be targeted for anti-cancer-stem-cell therapy. Proc. Natl. Acad. Sci. USA. 2014;111:17266–17271. doi: 10.1073/pnas.1419599111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Liu W.T., Jing Y.Y., Yu G.F., Han Z.P., Yu D.D., Fan Q.M., Ye F., Li R., Gao L., Zhao Q.D., et al. Toll like receptor 4 facilitates invasion and migration as a cancer stem cell marker in hepatocellular carcinoma. Cancer Lett. 2015;358:136–143. doi: 10.1016/j.canlet.2014.12.019. [DOI] [PubMed] [Google Scholar]
- 37.Ravindran Menon D., Luo Y., Arcaroli J.J., Liu S., KrishnanKutty L.N., Osborne D.G., Li Y., Samson J.M., Bagby S., Tan A.C., et al. Cdk1 interacts with sox2 and promotes tumor initiation in human melanoma. Cancer Res. 2018;78:6561–6574. doi: 10.1158/0008-5472.CAN-18-0330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Andrews A., Warner K., Rodriguez-Ramirez C., Pearson A.T., Nor F., Zhang Z., Kerk S., Kulkarni A.S., Helman J.I., Brenner J.C., et al. Ablation of cancer stem cells by therapeutic inhibition of the mdm2-p53 interaction in mucoepidermoid carcinoma. Clin. Cancer Res. 2018 doi: 10.1158/1078-0432.CCR-17-2730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Jinesh G.G., Manyam G.C., Mmeje C.O., Baggerly K.A., Kamat A.M. Surface pd-l1, e-cadherin, cd24, and vegfr2 as markers of epithelial cancer stem cells associated with rapid tumorigenesis. Sci. Rep. 2017;7:9602. doi: 10.1038/s41598-017-08796-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Almozyan S., Colak D., Mansour F., Alaiya A., Al-Harazi O., Qattan A., Al-Mohanna F., Al-Alwan M., Ghebeh H. Pd-l1 promotes oct4 and nanog expression in breast cancer stem cells by sustaining pi3k/akt pathway activation. Int. J. Cancer. 2017;141:1402–1412. doi: 10.1002/ijc.30834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Langan R.C., Mullinax J.E., Raiji M.T., Upham T., Summers T., Stojadinovic A., Avital I. Colorectal cancer biomarkers and the potential role of cancer stem cells. J. Cancer. 2013;4:241–250. doi: 10.7150/jca.5832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Yoo S.Y., Bang S.Y., Jeong S.N., Kang D.H., Heo J. A cancer-favoring oncolytic vaccinia virus shows enhanced suppression of stem-cell like colon cancer. Oncotarget. 2016;7:16479–16489. doi: 10.18632/oncotarget.7660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Nguyen P.H., Giraud J., Chambonnier L., Dubus P., Wittkop L., Belleannee G., Collet D., Soubeyran I., Evrard S., Rousseau B., et al. Characterization of biomarkers of tumorigenic and chemoresistant cancer stem cells in human gastric carcinoma. Clin. Cancer Res. 2017;23:1586–1597. doi: 10.1158/1078-0432.CCR-15-2157. [DOI] [PubMed] [Google Scholar]
- 44.Curtarelli R.B., Goncalves J.M., Dos Santos L.G.P., Savi M.G., Nor J.E., Mezzomo L.A.M., Rodriguez Cordeiro M.M. Expression of cancer stem cell biomarkers in human head and neck carcinomas: A systematic review. Stem Cell Rev. 2018;14:769–784. doi: 10.1007/s12015-018-9839-4. [DOI] [PubMed] [Google Scholar]
- 45.Xiao Y., Lin M., Jiang X., Ye J., Guo T., Shi Y., Bian X. The recent advances on liver cancer stem cells: Biomarkers, separation, and therapy. Anal. Cell. Pathol. 2017;2017:5108653. doi: 10.1155/2017/5108653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Yoo S.Y., Jeong S.N., Kang D.H., Heo J. Evolutionary cancer-favoring engineered vaccinia virus for metastatic hepatocellular carcinoma. Oncotarget. 2017;8:71489–71499. doi: 10.18632/oncotarget.17288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Zhang K., Zhou S., Wang L., Wang J., Zou Q., Zhao W., Fu Q., Fang X. Current stem cell biomarkers and their functional mechanisms in prostate cancer. Int. J. Mol. Sci. 2016;17:1163. doi: 10.3390/ijms17071163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Muinao T., Deka Boruah H.P., Pal M. Diagnostic and prognostic biomarkers in ovarian cancer and the potential roles of cancer stem cells—An updated review. Exp. Cell Res. 2018;362:1–10. doi: 10.1016/j.yexcr.2017.10.018. [DOI] [PubMed] [Google Scholar]
- 49.Doherty M.R., Cheon H., Junk D.J., Vinayak S., Varadan V., Telli M.L., Ford J.M., Stark G.R., Jackson M.W. Interferon-beta represses cancer stem cell properties in triple-negative breast cancer. Proc. Natl. Acad. Sci. USA. 2017;114:13792–13797. doi: 10.1073/pnas.1713728114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Zhang D., Tang D.G., Rycaj K. Cancer stem cells: Regulation programs, immunological properties and immunotherapy. Semin. Cancer Biol. 2018;52:94–106. doi: 10.1016/j.semcancer.2018.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Turley S.J., Cremasco V., Astarita J.L. Immunological hallmarks of stromal cells in the tumour microenvironment. Nat. Rev. Immunol. 2015;15:669–682. doi: 10.1038/nri3902. [DOI] [PubMed] [Google Scholar]
- 52.Klemm F., Joyce J.A. Microenvironmental regulation of therapeutic response in cancer. Trends Cell Biol. 2015;25:198–213. doi: 10.1016/j.tcb.2014.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Nagarsheth N., Wicha M.S., Zou W. Chemokines in the cancer microenvironment and their relevance in cancer immunotherapy. Nat. Rev. Immunol. 2017;17:559–572. doi: 10.1038/nri.2017.49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Relation T., Dominici M., Horwitz E.M. Concise review: An (im)penetrable shield: How the tumor microenvironment protects cancer stem cells. Stem Cells. 2017;35:1123–1130. doi: 10.1002/stem.2596. [DOI] [PubMed] [Google Scholar]
- 55.Miller T.J., McCoy M.J., Hemmings C., Bulsara M.K., Iacopetta B., Platell C.F. The prognostic value of cancer stem-like cell markers sox2 and cd133 in stage iii colon cancer is modified by expression of the immune-related markers foxp3, pd-l1 and cd3. Pathology. 2017;49:721–730. doi: 10.1016/j.pathol.2017.08.007. [DOI] [PubMed] [Google Scholar]
- 56.Di Tomaso T., Mazzoleni S., Wang E., Sovena G., Clavenna D., Franzin A., Mortini P., Ferrone S., Doglioni C., Marincola F.M., et al. Immunobiological characterization of cancer stem cells isolated from glioblastoma patients. Clin. Cancer Res. 2010;16:800–813. doi: 10.1158/1078-0432.CCR-09-2730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Wu A., Wei J., Kong L.Y., Wang Y., Priebe W., Qiao W., Sawaya R., Heimberger A.B. Glioma cancer stem cells induce immunosuppressive macrophages/microglia. Neuro-Oncol. 2010;12:1113–1125. doi: 10.1093/neuonc/noq082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Wei J., Barr J., Kong L.Y., Wang Y., Wu A., Sharma A.K., Gumin J., Henry V., Colman H., Sawaya R., et al. Glioma-associated cancer-initiating cells induce immunosuppression. Clin. Cancer Res. 2010;16:461–473. doi: 10.1158/1078-0432.CCR-09-1983. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 59.Otvos B., Silver D.J., Mulkearns-Hubert E.E., Alvarado A.G., Turaga S.M., Sorensen M.D., Rayman P., Flavahan W.A., Hale J.S., Stoltz K., et al. Cancer stem cell-secreted macrophage migration inhibitory factor stimulates myeloid derived suppressor cell function and facilitates glioblastoma immune evasion. Stem Cells. 2016;34:2026–2039. doi: 10.1002/stem.2393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Alvarado A.G., Thiagarajan P.S., Mulkearns-Hubert E.E., Silver D.J., Hale J.S., Alban T.J., Turaga S.M., Jarrar A., Reizes O., Longworth M.S., et al. Glioblastoma cancer stem cells evade innate immune suppression of self-renewal through reduced tlr4 expression. Cell Stem Cell. 2017;20:450–461. doi: 10.1016/j.stem.2016.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Volonte A., Di Tomaso T., Spinelli M., Todaro M., Sanvito F., Albarello L., Bissolati M., Ghirardelli L., Orsenigo E., Ferrone S., et al. Cancer-initiating cells from colorectal cancer patients escape from t cell-mediated immunosurveillance in vitro through membrane-bound il-4. J. Immunol. 2014;192:523–532. doi: 10.4049/jimmunol.1301342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Schatton T., Schutte U., Frank N.Y., Zhan Q., Hoerning A., Robles S.C., Zhou J., Hodi F.S., Spagnoli G.C., Murphy G.F., et al. Modulation of t-cell activation by malignant melanoma initiating cells. Cancer Res. 2010;70:697–708. doi: 10.1158/0008-5472.CAN-09-1592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Wang B., Wang Q., Wang Z., Jiang J., Yu S.C., Ping Y.F., Yang J., Xu S.L., Ye X.Z., Xu C., et al. Metastatic consequences of immune escape from nk cell cytotoxicity by human breast cancer stem cells. Cancer Res. 2014;74:5746–5757. doi: 10.1158/0008-5472.CAN-13-2563. [DOI] [PubMed] [Google Scholar]
- 64.Zhang H., Lu H., Xiang L., Bullen J.W., Zhang C., Samanta D., Gilkes D.M., He J., Semenza G.L. Hif-1 regulates cd47 expression in breast cancer cells to promote evasion of phagocytosis and maintenance of cancer stem cells. Proc. Natl. Acad. Sci. USA. 2015;112:E6215–E6223. doi: 10.1073/pnas.1520032112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Hsu J.M., Xia W., Hsu Y.H., Chan L.C., Yu W.H., Cha J.H., Chen C.T., Liao H.W., Kuo C.W., Khoo K.H., et al. Stt3-dependent pd-l1 accumulation on cancer stem cells promotes immune evasion. Nat. Commun. 2018;9:1908. doi: 10.1038/s41467-018-04313-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Hermann P.C., Huber S.L., Herrler T., Aicher A., Ellwart J.W., Guba M., Bruns C.J., Heeschen C. Distinct populations of cancer stem cells determine tumor growth and metastatic activity in human pancreatic cancer. Cell Stem Cell. 2007;1:313–323. doi: 10.1016/j.stem.2007.06.002. [DOI] [PubMed] [Google Scholar]
- 67.Sainz B., Jr., Alcala S., Garcia E., Sanchez-Ripoll Y., Azevedo M.M., Cioffi M., Tatari M., Miranda-Lorenzo I., Hidalgo M., Gomez-Lopez G., et al. Microenvironmental hcap-18/ll-37 promotes pancreatic ductal adenocarcinoma by activating its cancer stem cell compartment. Gut. 2015;64:1921–1935. doi: 10.1136/gutjnl-2014-308935. [DOI] [PubMed] [Google Scholar]
- 68.Cioffi M., D’Alterio C., Camerlingo R., Tirino V., Consales C., Riccio A., Ierano C., Cecere S.C., Losito N.S., Greggi S., et al. Identification of a distinct population of cd133(+)cxcr4(+) cancer stem cells in ovarian cancer. Sci. Rep. 2015;5:10357. doi: 10.1038/srep10357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Teitz-Tennenbaum S., Wicha M.S., Chang A.E., Li Q. Targeting cancer stem cells via dendritic-cell vaccination. Oncoimmunology. 2012;1:1401–1403. doi: 10.4161/onci.21026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Badrinath N., Heo J., Yoo S.Y. Viruses as nanomedicine for cancer. Int. J. Nanomed. 2016;11:4835–4847. doi: 10.2147/IJN.S116447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Rosenberg S.A., Restifo N.P. Adoptive cell transfer as personalized immunotherapy for human cancer. Science. 2015;348:62–68. doi: 10.1126/science.aaa4967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Deng Z., Wu Y., Ma W., Zhang S., Zhang Y.Q. Adoptive t-cell therapy of prostate cancer targeting the cancer stem cell antigen epcam. BMC Immunol. 2015;16:1. doi: 10.1186/s12865-014-0064-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Hurton L.V., Singh H., Najjar A.M., Switzer K.C., Mi T., Maiti S., Olivares S., Rabinovich B., Huls H., Forget M.A., et al. Tethered il-15 augments antitumor activity and promotes a stem-cell memory subset in tumor-specific t cells. Proc. Natl. Acad. Sci. USA. 2016;113:E7788–E7797. doi: 10.1073/pnas.1610544113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Miyamoto S., Kochin V., Kanaseki T., Hongo A., Tokita S., Kikuchi Y., Takaya A., Hirohashi Y., Tsukahara T., Terui T., et al. The antigen asb4 on cancer stem cells serves as a target for ctl immunotherapy of colorectal cancer. Cancer Immunol. Res. 2018;6:358–369. doi: 10.1158/2326-6066.CIR-17-0518. [DOI] [PubMed] [Google Scholar]
- 75.Tettamanti S., Marin V., Pizzitola I., Magnani C.F., Giordano Attianese G.M., Cribioli E., Maltese F., Galimberti S., Lopez A.F., Biondi A., et al. Targeting of acute myeloid leukaemia by cytokine-induced killer cells redirected with a novel cd123-specific chimeric antigen receptor. Br. J. Haematol. 2013;161:389–401. doi: 10.1111/bjh.12282. [DOI] [PubMed] [Google Scholar]
- 76.Gammaitoni L., Giraudo L., Macagno M., Leuci V., Mesiano G., Rotolo R., Sassi F., Sanlorenzo M., Zaccagna A., Pisacane A., et al. Cytokine-induced killer cells kill chemo-surviving melanoma cancer stem cells. Clin. Cancer Res. 2017;23:2277–2288. doi: 10.1158/1078-0432.CCR-16-1524. [DOI] [PubMed] [Google Scholar]
- 77.Rong X.X., Wei F., Lin X.L., Qin Y.J., Chen L., Wang H.Y., Shen H.F., Jia L.T., Xie R.Y., Lin T.Y., et al. Recognition and killing of cancer stem-like cell population in hepatocellular carcinoma cells by cytokine-induced killer cells via nkg2d-ligands recognition. Oncoimmunology. 2016;5:e1086060. doi: 10.1080/2162402X.2015.1086060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Wei F., Rong X.X., Xie R.Y., Jia L.T., Wang H.Y., Qin Y.J., Chen L., Shen H.F., Lin X.L., Yang J., et al. Cytokine-induced killer cells efficiently kill stem-like cancer cells of nasopharyngeal carcinoma via the nkg2d-ligands recognition. Oncotarget. 2015;6:35023–35039. doi: 10.18632/oncotarget.5280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Ferreira-Teixeira M., Paiva-Oliveira D., Parada B., Alves V., Sousa V., Chijioke O., Munz C., Reis F., Rodrigues-Santos P., Gomes C. Natural killer cell-based adoptive immunotherapy eradicates and drives differentiation of chemoresistant bladder cancer stem-like cells. BMC Med. 2016;14:163. doi: 10.1186/s12916-016-0715-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Ames E., Canter R.J., Grossenbacher S.K., Mac S., Chen M., Smith R.C., Hagino T., Perez-Cunningham J., Sckisel G.D., Urayama S., et al. Nk cells preferentially target tumor cells with a cancer stem cell phenotype. J. Immunol. 2015;195:4010–4019. doi: 10.4049/jimmunol.1500447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Kaur K., Cook J., Park S.H., Topchyan P., Kozlowska A., Ohanian N., Fang C., Nishimura I., Jewett A. Novel strategy to expand super-charged nk cells with significant potential to lyse and differentiate cancer stem cells: Differences in nk expansion and function between healthy and cancer patients. Front. Immunol. 2017;8:297. doi: 10.3389/fimmu.2017.00297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Chen H.C., Joalland N., Bridgeman J.S., Alchami F.S., Jarry U., Khan M.W.A., Piggott L., Shanneik Y., Li J., Herold M.J., et al. Synergistic targeting of breast cancer stem-like cells by human gammadelta t cells and cd8(+) t cells. Immunol. Cell Biol. 2017;95:620–629. doi: 10.1038/icb.2017.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Dashti A., Ebrahimi M., Hadjati J., Memarnejadian A., Moazzeni S.M. Dendritic cell based immunotherapy using tumor stem cells mediates potent antitumor immune responses. Cancer Lett. 2016;374:175–185. doi: 10.1016/j.canlet.2016.01.021. [DOI] [PubMed] [Google Scholar]
- 84.Lu L., Tao H., Chang A.E., Hu Y., Shu G., Chen Q., Egenti M., Owen J., Moyer J.S., Prince M.E., et al. Cancer stem cell vaccine inhibits metastases of primary tumors and induces humoral immune responses against cancer stem cells. Oncoimmunology. 2015;4:e990767. doi: 10.4161/2162402X.2014.990767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Yin T., Shi P., Gou S., Shen Q., Wang C. Dendritic cells loaded with pancreatic cancer stem cells (cscs) lysates induce antitumor immune killing effect in vitro. PLoS ONE. 2014;9:e114581. doi: 10.1371/journal.pone.0114581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Wefers C., Schreibelt G., Massuger L., de Vries I.J.M., Torensma R. Immune curbing of cancer stem cells by ctls directed to nanog. Front. Immunol. 2018;9:1412. doi: 10.3389/fimmu.2018.01412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Hu Y., Lu L., Xia Y., Chen X., Chang A.E., Hollingsworth R.E., Hurt E., Owen J., Moyer J.S., Prince M.E., et al. Therapeutic efficacy of cancer stem cell vaccines in the adjuvant setting. Cancer Res. 2016;76:4661–4672. doi: 10.1158/0008-5472.CAN-15-2664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Ning N., Pan Q., Zheng F., Teitz-Tennenbaum S., Egenti M., Yet J., Li M., Ginestier C., Wicha M.S., Moyer J.S., et al. Cancer stem cell vaccination confers significant antitumor immunity. Cancer Res. 2012;72:1853–1864. doi: 10.1158/0008-5472.CAN-11-1400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Cheema T.A., Wakimoto H., Fecci P.E., Ning J., Kuroda T., Jeyaretna D.S., Martuza R.L., Rabkin S.D. Multifaceted oncolytic virus therapy for glioblastoma in an immunocompetent cancer stem cell model. Proc. Natl. Acad. Sci. USA. 2013;110:12006–12011. doi: 10.1073/pnas.1307935110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Sato-Dahlman M., Miura Y., Huang J.L., Hajeri P., Jacobsen K., Davydova J., Yamamoto M. Cd133-targeted oncolytic adenovirus demonstrates anti-tumor effect in colorectal cancer. Oncotarget. 2017;8:76044–76056. doi: 10.18632/oncotarget.18340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Wang H., Chen N.G., Minev B.R., Szalay A.A. Oncolytic vaccinia virus glv-1h68 strain shows enhanced replication in human breast cancer stem-like cells in comparison to breast cancer cells. J. Transl. Med. 2012;10:167. doi: 10.1186/1479-5876-10-167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Gil M., Komorowski M.P., Seshadri M., Rokita H., McGray A.J., Opyrchal M., Odunsi K.O., Kozbor D. Cxcl12/cxcr4 blockade by oncolytic virotherapy inhibits ovarian cancer growth by decreasing immunosuppression and targeting cancer-initiating cells. J. Immunol. 2014;193:5327–5337. doi: 10.4049/jimmunol.1400201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Bach P., Abel T., Hoffmann C., Gal Z., Braun G., Voelker I., Ball C.R., Johnston I.C., Lauer U.M., Herold-Mende C., et al. Specific elimination of cd133+ tumor cells with targeted oncolytic measles virus. Cancer Res. 2013;73:865–874. doi: 10.1158/0008-5472.CAN-12-2221. [DOI] [PubMed] [Google Scholar]
- 94.Kemper K., Prasetyanti P.R., De Lau W., Rodermond H., Clevers H., Medema J.P. Monoclonal antibodies against lgr5 identify human colorectal cancer stem cells. Stem Cells. 2012;30:2378–2386. doi: 10.1002/stem.1233. [DOI] [PubMed] [Google Scholar]
- 95.Ginestier C., Liu S., Diebel M.E., Korkaya H., Luo M., Brown M., Wicinski J., Cabaud O., Charafe-Jauffret E., Birnbaum D., et al. Cxcr1 blockade selectively targets human breast cancer stem cells in vitro and in xenografts. J. Clin. Investig. 2010;120:485–497. doi: 10.1172/JCI39397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Zheng F., Dang J., Zhang H., Xu F., Ba D., Zhang B., Cheng F., Chang A.E., Wicha M.S., Li Q. Cancer stem cell vaccination with pd-l1 and ctla-4 blockades enhances the eradication of melanoma stem cells in a mouse tumor model. J. Immunother. 2018;41:361–368. doi: 10.1097/CJI.0000000000000242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Saha D., Martuza R.L., Rabkin S.D. Macrophage polarization contributes to glioblastoma eradication by combination immunovirotherapy and immune checkpoint blockade. Cancer Cell. 2017;32:253–267. doi: 10.1016/j.ccell.2017.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Zhu S., Lv X., Zhang X., Li T., Zang G., Yang N., Wang X., Wu J., Chen W., Liu Y.J., et al. An effective dendritic cell-based vaccine containing glioma stem-like cell lysate and cpg adjuvant for an orthotopic mouse model of glioma. Int. J. Cancer. 2018 doi: 10.1002/ijc.32008. [DOI] [PubMed] [Google Scholar]
- 99.Shi X., Zhang X., Li J., Mo L., Zhao H., Zhu Y., Hu Z., Gao J., Tan W. Pd-1 blockade enhances the antitumor efficacy of gm-csf surface-modified bladder cancer stem cells vaccine. Int. J. Cancer. 2018;142:2106–2117. doi: 10.1002/ijc.31219. [DOI] [PubMed] [Google Scholar]
- 100.Chen X., Wen Q., Stucky A., Zeng Y., Gao S., Loudon W.G., Ho H.W., Kabeer M.H., Li S.C., Zhang X., et al. Relapse pathway of glioblastoma revealed by single-cell molecular analysis. Carcinogenesis. 2018;39:931–936. doi: 10.1093/carcin/bgy052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Li S.C., Tachiki L.M., Kabeer M.H., Dethlefs B.A., Anthony M.J., Loudon W.G. Cancer genomic research at the crossroads: Realizing the changing genetic landscape as intratumoral spatial and temporal heterogeneity becomes a confounding factor. Cancer Cell Int. 2014;14:115. doi: 10.1186/s12935-014-0115-7. [DOI] [PMC free article] [PubMed] [Google Scholar]