Abstract
IN BRIEF In the management of diabetes, adequate health literacy is necessary to help patients monitor their caloric and carbohydrate intake and monitor their blood glucose to achieve adequate glycemic control. This cross-sectional study was conducted to assess the health literacy of patients with diabetes from East Harlem in New York City using the validated Newest Vital Sign screening tool and to investigate its association with microvascular complications of diabetes. Lower health literacy was found to be associated with higher microvascular complications in these patients with diabetes.
The disease burden related to diabetes is high and continues rising worldwide. The latest estimates disclose a global prevalence of 382 million in 2013 alone, and that is expected to rise to 592 million by 2035 (1). According to the Centers for Disease Control and Prevention, the total estimated cost for diagnosis and treatment of diabetes in the United States in 2017 was $327 billion.
The aim of this study was to evaluate the role of health literacy in attaining adequate glycemic control of type 2 diabetes and whether this has any impact on long-term complications of diabetes. Health literacy was assessed with a validated screening tool, the Newest Vital Sign (NVS) (2), in both primary care and nonprimary care settings.
Methods
We conducted a cross-sectional observational study at New York City Health and Hospitals/Metropolitan Hospital Center (Health+Hospital Metropolitan), a university-affiliated community hospital that provides inpatient and comprehensive outpatient services to the population of East Harlem in New York City. A sample size of 170 was calculated for a 95% CI and a 5% margin of error. This was based on a “below basic” health literacy rate in the United States, as described in the 2003 National Assessment of Adult Literacy survey (3). All known outpatients with diabetes as well as those inpatients with diabetes who were also seen as outpatients in the affiliated clinics from August 2017 to February 2018 were eligible for inclusion. Patients with type 1 diabetes and any patients who did not wish to enroll were excluded. A verbal consent was sought, and the study was approved by the Biomedical Research Alliance of New York.
The main outcome measures for the study were microvascular and macrovascular complications. The cut-off for adequate literacy was a score ≥3 on the NVS questionnaire tool. Therefore, cases were considered to be those patients whose NVS scores were 0–2 (indicating inadequate literacy), and control subjects were those with NVS scores of 3–6 (indicating adequate literacy). English proficiency, ability to read and write, A1C level, and microvascular complications of diabetes (i.e., nephropathy, retinopathy, and neuropathy) were logged. Evidence of nephropathy was considered to be positive microalbuminuria test values and/or treatment with low-dose ACE inhibitors. Evidence of neuropathy was considered to be treatment with gabapentin or pregabalin for neuropathy for the past year. Evidence of retinopathy was based on findings of direct funduscopic examination in the eye clinic within the past year. The patients were considered to have macrovascular complications if they had cerebrovascular disease (as evidenced in brain imaging), coronary artery disease (as evidenced by positive findings on coronary angiography), or peripheral vascular disease (as evidenced by arterial duplex scan of the extremities). Multivariate analysis was performed to evaluate the effect of age, sex, and duration of diabetes as confounding variables with regard to diabetes control.
A total of 170 patients with type 2 diabetes, including 122 cases (mean age 59.2 ± 12.28 years, 54% females, mean duration of diabetes 11.77 ± 8.9 years) and 48 control subjects (mean age 57.9 ± 10.3 years, 52% females, mean duration of diabetes 11.25 ± 10.68 years) were enrolled. Data were analyzed by univariate and multivariate logistic regression using Stata Statistical Software, release 12 (Stata Corp., College Station, Tex.).
Results
At Health+Hospitals Metropolitan, it was found that 71% of the patients with diabetes were unable to appropriately answer a questionnaire based on a Nutrition Facts label. Of these patients, 20% reported not being able to read or write, and 30% had not reached the fifth grade of primary education, suggesting inadequate health literacy. Microvascular complications were present in 61% of cases and 42% of control subjects. The odds of having microvascular complications were 2.15 times higher for patients with an NVS score of 0–2 compared with patients with an NVS score of 3–6 in the univariate analysis (odds ratio [OR] 2.15, 95% CI 1.09–4.25, P = 0.026). The association persisted in multivariate regression, after adjusting for age, sex, and duration of diabetes (OR 2.18, 95% CI 1.07–4.46, P = 0.032). The odds of developing neuropathy were 2.3 higher in cases compared to control subjects (OR 2.3, 95% CI 1.05–5.2, P = 0.037) in the multivariate regression model. The odds of developing retinopathy were 2.21 in cases as compared to control subjects, with borderline significance (P = 0.054) in the multivariate regression model (Table 1). However, results were not significant for nephropathy or macrovascular complications.
TABLE 1.
Comparison of Odds of Having Complications Between Cases and Control Subjects
| Univariate OR (95% CI) | Multivariate OR (95% CI) | |
|---|---|---|
| Microvascular complications | 2.15 (1.09–4.25) | 2.18 (1.07–4.46) |
| Neuropathy | 2.3 (1.04–5.05) | 2.3 (1.05–5.2) |
| Retinopathy | 2.01 (0.95–4.24) | 2.21 (0.98–4.97) |
| Nephropathy | 1.57 (0.76–3.23) | 1.61 (0.74–3.78) |
| Macrovascular complications | 0.82 (0.31–2.15) | NA |
Bold type denotes statistical significance (P <0.05).
NA, not applicable.
Discussion
Health literacy is the degree to which individuals have the capacity to obtain, process, and understand basic health information and services needed to make appropriate health decisions (4). It has been suggested that limited health literacy and numeracy skills lead to poor self-management behavior and lower glycemic control in patients with diabetes (4–6). The hypothesis for this cross-sectional study was that higher health literacy leads to improved diabetes control. Our aim was to adequately describe the health literacy of the population served by Health+Hospitals Metropolitan, using the validated NVS health literacy screening tool and to use this information to determine whether limited health literacy is associated with worse outcomes in patients with diabetes.
The study was conducted in primary care and nonprimary care settings. Patients with type 2 diabetes were asked to complete the NVS questionnaire and were also evaluated to ascertain whether they were at their glycemic goal. The main outcomes for the study were microvascular and macrovascular complications.
The NVS tool was used to assess health literacy because it is more feasible and less time-consuming (3 minutes) that other widely used tools such as the Test of Functional Heath Literacy in Adults (22 minutes), the Short-Form Test of Functional Health Literacy in Adults (7 minutes), and the Diabetes Numeracy Test (33 minutes) (7,8). Additionally, the NVS is available in both English and Spanish (2). The NVS provides an ice cream nutrition label (Figure 1), which patients used to answer a six-item questionnaire (Figure 2). For our study, the patients with a score of <3 were considered to have inadequate health literacy (cases), and their diabetes control outcomes were compared to control subjects who had a score of 3–6 (Figure 3).
FIGURE 1.
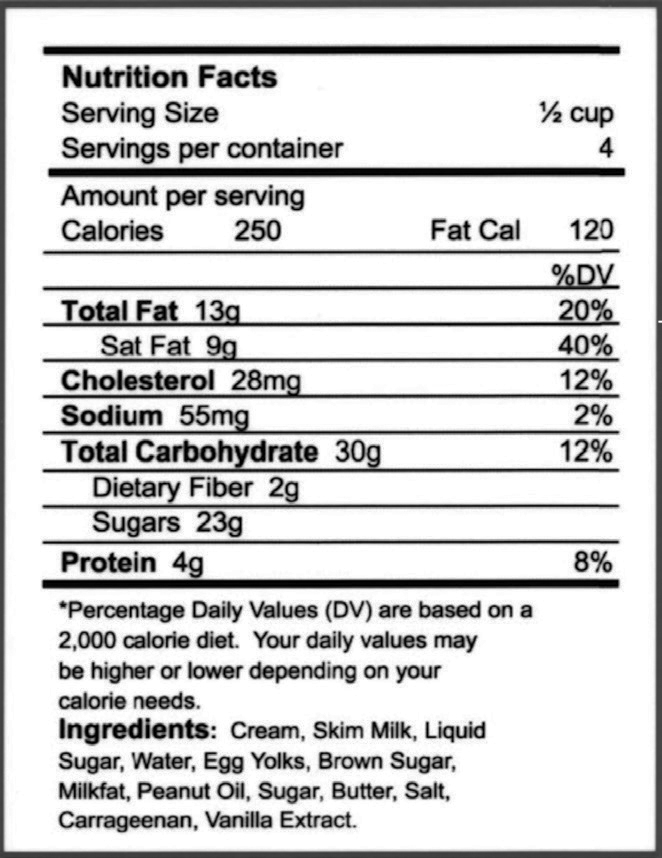
Nutrition Facts label for a pint container of ice cream, provided as part of the NVS.
FIGURE 2.
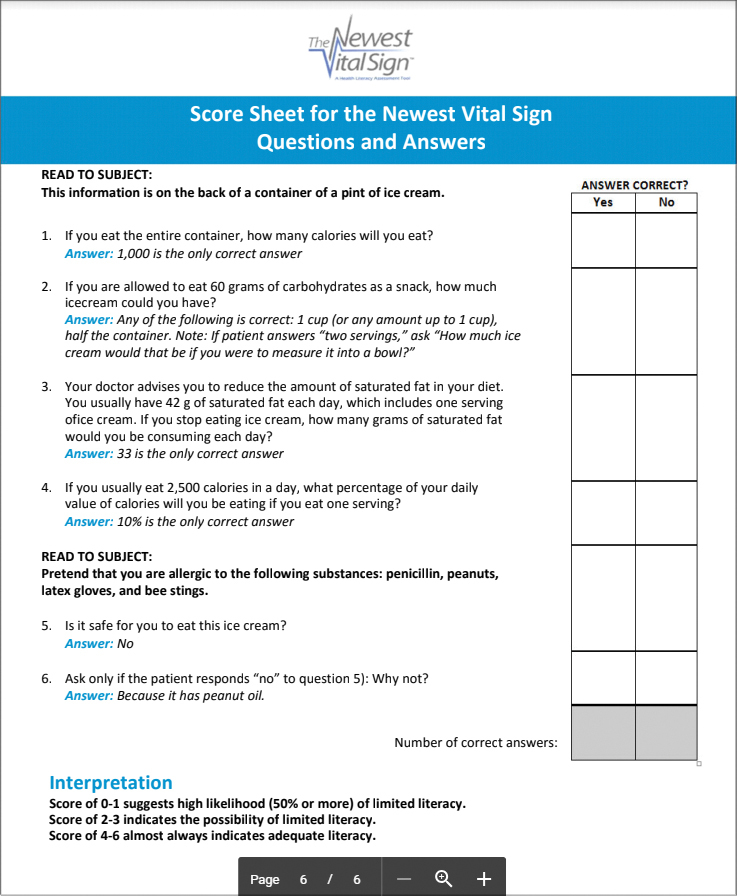
Score sheet for the NVS questionnaire. Patients with an NVS score of 0–2 were taken as cases, whereas those with a score of 3–6 were considered control subjects.
FIGURE 3.
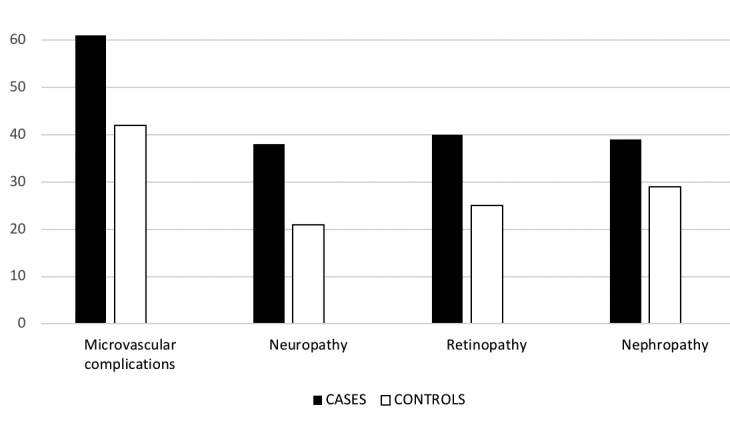
Bar diagram representing the percentages of cases and control subjects having various diabetes complications.
The odds of having microvascular complications were found to be higher in patients with low NVS scores in univariate and multivariate analyses. Neuropathy was associated with low NVS scores on multivariate analysis after adjusting for age, sex, and duration of diabetes. This study is unique in using the NVS tool in both primary care and nonprimary care settings. Our findings confirm the findings of a few current investigators (9,10), but unfortunately, the literature is also replete with competing results that find no association between health literacy and glycemic control (11,12).
A limitation of this study was that the majority of the population served by the hospital has limited health literacy; therefore, we were unable to gather data for an adequate number of control subjects with adequate health literacy and higher NVS scores. Also, there are many potentially intervening variables in the link between health literacy and its outcomes (e.g., empowerment [13], self-efficacy [14], and depression [15]) that should be considered while adjusting variables during multivariate analysis.
Moving forward, we hope to encourage practitioners to increase awareness of healthy meal plans for diabetes and diabetes self-management among patients by using cost-effective measures such as nutritional classes and videos that are designed for patients of all literacy levels. This will reduce expenditures necessary to treat the complications of diabetes and thus decrease the overall financial burden of diabetes on both patients and society.
Conclusion
Lower health literacy as suggested by lower NVS scores was significantly associated with a higher risk of overall microvascular complications and specifically neuropathy in patients with type 2 diabetes.
Acknowledgments
Duality of Interest
No potential conflicts of interest relevant to this article were reported.
Author Contributions
B.K.M. researched data and wrote the manuscript; S.A.D.Y.S. researched data and reviewed and edited the manuscript; R.D. researched data; S.D. performed statistical analysis; and J.O. reviewed the manuscript. B.K.M. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
References
- 1.Forouhi NG, Wareham NJ. Epidemiology of diabetes. Medicine (Abingdon) 2014;42:698–702 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Weiss BD, Mays MZ, Martz W, et al. Quick assessment of literacy in primary care: the Newest Vital Sign. Ann Fam Med 2005;3:514–522 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cutilli CC, Bennett IM. Understanding the health literacy of America: results of the National Assessment of Adult Literacy. Orthop Nurs 2009;28:27–34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schillinger D, Grumbach K, Piette J, et al. Association of health literacy with diabetes outcomes. JAMA 2002;288:475–482 [DOI] [PubMed] [Google Scholar]
- 5.Aring AM, Jones DE, Falko JM. Evaluation and prevention of diabetic neuropathy. Am Fam Phys 2005;71:2123–2128 [PubMed] [Google Scholar]
- 6.Kim S, Love F, Quistberg DA, Shea JA. Association of health literacy with self-management behavior in patients with diabetes. Diabetes Care 2004;27:2980–2982 [DOI] [PubMed] [Google Scholar]
- 7.Parker RM, Baker DW, Williams MV, Nurss JR. The Test of Functional Health Literacy in Adults: a new instrument for measuring patients’ literacy skills. J Gen Intern Med 1995;10:537–541 [DOI] [PubMed] [Google Scholar]
- 8.Huizinga MM, Elasy TA, Wallston KA, et al. Development and validation of the Diabetes Numeracy Test (DNT). BMC Health Serv Res 2008;8:96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Olesen K, Reynheim ALF, Joensen L, et al. Higher health literacy is associated with better glycemic control in adults with type 1 diabetes: a cohort study among 1399 Danes. BMJ Open Diabetes Res Care 2017;5:e000437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cavanaugh KL. Health literacy in diabetes care: explanation, evidence and equipment. Diabetes Manag (Lond) 2011;1:191–199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Al Sayah F, Majumdar SR, Williams B, Robertson S, Johnson JA. Health literacy and health outcomes in diabetes: a systematic review. J Gen Intern Med 2013;28:444–452 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bailey SC, Breg AG, Crutchfield TM, et al. Update on health literacy and diabetes. Diabetes Educ 2014;40:581–604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shin KS, Lee EH. Relationships of health literacy to self-care behaviors in people with diabetes aged 60 and above: empowerment as a mediator. J Adv Nurs 2018;74:2362–2372 [DOI] [PubMed] [Google Scholar]
- 14.Osborn CY, Cavanaugh K, Wallston KA, Rothman RL. Self-efficacy links health literacy and numeracy to glycemic control. J Health Commun 2010;15:146–158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Maneze D, Everett B, Astorga C, Yogendran D, Salamonson Y. The influence of health literacy and depression on diabetes self-management: a cross-sectional study. J Diabetes Res 2016;2016:3458969. [DOI] [PMC free article] [PubMed] [Google Scholar]


