Abstract
IN BRIEF In this feasibility study, we evaluated the impact of a contact-based education patient panel in an Endocrine and Metabolism course on second-year medical students’ diabetes attitudes and diabetes stigma. Prior to the patient panel, some medical students harbored stigma toward people with diabetes, thus confirming patients’ reports in the literature of diabetes stigma on the part of health care professionals. Importantly, the one-time contact-based educational approach improved students’ diabetes attitudes and reduced diabetes stigma.
Individuals with diabetes must follow specific self-care recommendations, including following a healthy diet (1), engaging in regular physical activity (2,3), monitoring blood glucose levels (4), taking medications, and attending regular clinical appointments (5–7). These self-care behaviors are critically linked to improved optimal glycemia; however, integrating them into one’s daily life can be challenging (8–10). Recent National Health and Nutrition Examination Survey (NHANES) data show that half of adults with diabetes are not meeting recommended glycemic targets for diabetes care (11). Prior research shows that this may be because patients are not able to carry out self-care recommendations (12). As a result, some patients blame themselves for difficulty achieving treatment goals and direct their frustration and disappointment inward (12,13).
Considering the role that lifestyle plays in the management of diabetes, stigma may be influencing how people view the disease and, in turn, how the disease is treated. Diabetes stigma refers to negative feelings, such as exclusion, rejection, or blame, associated with having diabetes (14). The most common diabetes stigma, regardless of type of diabetes, was the perception that people with diabetes were responsible for developing their diabetes (14). Negative perceived attributions by health care professionals, friends, and family, such as people with diabetes are “weak,” “lazy,” and “gluttons” (15) or “poor,” “bad,” and “not terribly intelligent” (13), may contribute to greater social stigma and discrimination. Additional studies have shown that patients with diabetes who internalize stigma feel a lower sense of self-worth (16) and report higher psychological distress and lower quality of life (17). These findings emphasize the need to educate people about the causes of diabetes as well as the day-to-day management of the disease. For these reasons, innovative educational interventions are needed to dispel diabetes-related stigma as the number of people with diabetes continues to rise. Health care professionals, in particular, are well positioned to provide support to individuals with diabetes and engage in advocacy to fight against stigma and discrimination (17).
Contact-based education may be an effective approach to improve compassionate care and decrease diabetes-related stigma. For example, contact-based anti-stigma interventions have been shown to reduce stigma toward mental health problems among health care professional students (18,19) and community members (20). Contact-based education uses social contact between groups experiencing stigma and audiences who may be stigmatizing them (18,20–22). A key component of contact-based education is incorporating patient stories along with the social interaction (23). Importantly, the success of the contact depends on the patient being in recovery or good health (20). Thus, contact-based education may be a helpful approach to destigmatize diabetes among health care professionals. The purpose of our study was to evaluate the impact of a contact-based educational approach on second-year medical students’ attitudes toward diabetes. We hypothesized that a contact-based patient panel of people with diabetes would increase positive attitudes toward diabetes.
Methods
This feasibility study evaluated the impact on medical students of a contact-based educational approach in an Endocrine and Metabolism course. Specifically, we measured second-year medical students’ attitudes toward diabetes before and after a contact-based patient panel to 1) assess changes (positive or negative) in attitudes pre- and post-panel and 2) explore students’ stigma toward diabetes. The Ohio University Office of Research Compliance approved the protocol and all recruitment procedures and materials.
Participants
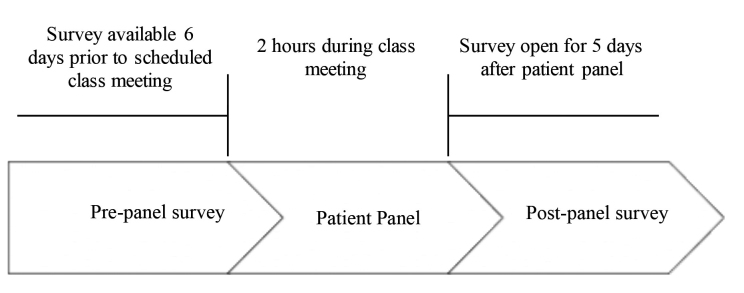
Second-year medical students enrolled at a large osteopathic medical school in the Midwest were invited to participate in an online, anonymous assessment before and after a diabetes patient panel. Students completed the pre-panel and post-panel assessments prior to receiving any lecture material on diabetes so that they would provide a baseline viewpoint of their own attitudes toward diabetes (Figure 1). The research team distributed the assessment via email on 4 January 2018; a reminder email with the assessment was distributed 4 days later. The post-panel assessment was distributed on 10 January 2018 with a reminder email sent 5 days later. Participation in the study was voluntary.
FIGURE 1.
Illustration of study flow.
Contact-Based Education Patient Panel
Individuals with diabetes from a local community group, Diabetes Community Partners, were invited to participate on a 2-hour patient panel about their experiences of living with diabetes. Patients were given a list of six questions prior to the panel to guide the discussion with the medical students. Questions included the following: 1) When were you diagnosed with diabetes? 2) What worries or fears do you have about diabetes? 3) What do you do to take care of diabetes? 4) What is the hardest thing about living with diabetes? 5) What misconceptions do people have about diabetes? and 6) What do you want medical students to know about diabetes? Four patients with type 2 diabetes, one patient with type 1 diabetes, and one spouse of a patient with type 1 diabetes participated on the panel.
Measures
Participating students completed the Diabetes Attitude Scale-3 (24), a 33-item scale that measures diabetes-related attitudes with five discrete subscales: 1) need for special training, 2) seriousness of type 2 diabetes, 3) value of tight glucose control, 4) psychosocial impact of diabetes, and 5) attitude toward patient autonomy. Health care professionals and patients are asked to rate their level of agreement on a 5-point Likert scale, ranging from strongly agree = 5 to strongly disagree = 1. The scale demonstrates superior subscale reliability scores and high content validity (24). We inadvertently left question 28, which measures the seriousness of type 2 diabetes, off the survey. However, we believe this mistake did not affect the reliability of the survey because question 25 also measured the seriousness of type 2 diabetes.
Participants also completed a series of short-answer questions in the pre-panel survey, including “Have you had any personal experiences with diabetes or exposure to diabetes among your family and friends?” and “Do you have any stigma against people with diabetes?” Short-answer questions in the post-panel survey included “Did your attitude toward diabetes change after listening to the speakers on the patient panel?”
Finally, we collected participants’ sociodemographic information (age, sex, race/ethnicity, rural/urban character of the locale where they grew up) and their planned specialty choice.
Data Collection
Participants completed the anonymous survey online via the electronic survey service Qualtrics (Provo, UT). Qualtrics permitted the research team to download students’ survey responses into a spreadsheet without including identifying information (i.e., email address and name). To link participants’ pre-panel and post-panel survey responses, we included three questions at the beginning of the survey that served as a unique identifier (i.e., favorite ice cream flavor, favorite animal, the number of the day in the month the participant was born); this unique identifier has been successfully used by the research team in previous studies to protect participant anonymity. All participants provided informed consent via the online survey prior to participation. No researchers were present when potential participants decided to participate or decline in order to ameliorate any perceived pressure to participate. Students with questions about the study were directed to email or phone the principal investigator (E.A.B.). Participation in the survey took ∼15 minutes.
Data Analysis
We assessed demographic factors using descriptive statistics and presented them as means and SDs or sample size and percentages. We performed independent samples t tests to compare Diabetes Attitude Scale subscale scores by respondents with diabetes experience, χ2 tests to compare respondents with diabetes experience by respondents with diabetes stigma, and paired t tests to examine changes in the Diabetes Attitude Scale subscale scores before and after the patient panel to assess changes in attitudes toward diabetes. In addition, we determined effect sizes using Cohen d by calculating the mean difference between the pre-panel and post-panel survey responses divided by the pooled SD. We defined statistical significance as a P value <0.05 and conducted analyses in SPSS statistical software version 23.0 (IBM Corp., Armonk, NY).
We analyzed the open-ended short-answer questions via content and thematic analyses (25). First, two researchers (E.A.B. and L.L.J.) independently marked and categorized key words, phrases, and texts to identify codes that described students’ experiences, stigmas, and attitudes toward diabetes. The researchers revised, discussed, and resolved coding discrepancies through consensus to establish intercoder reliability (26). The Cohen κ coefficient for the interrater agreement between the two coders was 0.969, indicating almost perfect agreement (27,28). Next, one member of the research team (L.L.J.) entered the agreed-upon codes in NVivo 11 software (QSR International, Victoria, Australia) to organize, sort, and structure the data to facilitate thematic analysis. Second, we conducted thematic analysis to identify patterns across the data (29,30). The selected themes described students’ experiences with diabetes, misconceptions about diabetes, and changes in attitudes after the patient panel. We derived themes from data that occurred multiple times, both within and across short-answer responses. Each theme includes words expressed by the participants to demonstrate that the concepts were grounded in the data.
Results
Of the 243 students invited to participate in the study, 208 completed the survey for a response rate of 85.6%. The mean age of the respondents was 25.6 ± 3.2 years, 45.2% (n = 94) identified as female, 72.0% (n = 149) identified as white, 32.2% (n = 67) grew up in a town (i.e., 2,500–50,000 people), and 38.9% (n = 81) planned to pursue primary care (Table 1). Of the 208 students, 132 (63.5%) reported direct experiences with individuals diagnosed with type 1 or type 2 diabetes. Two respondents (1.0%) reported having diabetes; 12.5% (n = 26) had a first-degree relative (i.e., parent, sibling, child), 38.9% (n = 81) had a second-degree relative (i.e., aunt, uncle, cousin, or grandparent), and 22.6% (n = 47) had a friend diagnosed with diabetes from whom they learned about the disease.
TABLE 1.
Participants’ Demographic Characteristics (n = 208)
| Variable | All participants |
|---|---|
| Age, years (mean ± SD) | 25.6 ± 3.3 |
| Sex | |
| Female | 94 (45.2) |
| Male | 111 (53.4) |
| Prefer not to answer | 3 (1.4) |
| Hispanic/Latino | 11 (5.3) |
| Race | |
| American Indian | 1 (0.5) |
| Asian | 17 (8.2) |
| Black/African American | 14 (6.8) |
| Mixed | 14 (6.8) |
| Other | 12 (5.8) |
| White/Caucasian | 149 (72.0) |
| Community grew up in | |
| Major metropolitan area (>1,000,000 people) | 5 (2.4) |
| Metropolitan area (500,001–1,000,000 people) | 17 (8.2) |
| City (100,001–500,000 people) | 48 (23.1) |
| Small city (50,001–100,000 people) | 44 (21.2) |
| Town (2,500–50,000 people) | 67 (32.2) |
| Rural area (<2,500 people) | 27 (13.0) |
| Plan to pursue primary care | |
| Yes | 81 (38.9) |
| No | 127 (61.1) |
Data are n (%) unless otherwise indicated.
Responses to the five Diabetes Attitude Scale subscales are presented in Table 2. Pre-panel mean scores showed respondents generally agreed with the “Need for special training” (4.46), “Seriousness of type 2 diabetes” (4.06), “Value of tight glucose control” (3.96), “Psychosocial impact of diabetes” (4.23), and “Attitude toward patient autonomy” (4.01) (Table 2). Respondents with prior experiences with family and friends with diabetes reported more positive attitudes regarding “Need for special training” (mean difference = 0.14, t = 2.054, P = 0.017) and “Psychosocial impact of diabetes” (mean difference = 0.15, t = 2.149, P = 0.017) compared with respondents without prior experience. When asked about stigma pre-panel, 29.4% (n = 55 out of a total of 187) of the respondents reported harboring stigma toward people with diabetes, particularly those with type 2 diabetes. Respondents expressing personal stigma toward diabetes did not differ by prior experience with diabetes (χ2 = 1.572, P = 0.210). However, respondents harboring diabetes stigma reported less agreement regarding the “seriousness of type 2 diabetes” (t = 2.080, P = 0.039); no other subscale score differed by diabetes stigma.
TABLE 2.
Differences Between Mean Diabetes Attitude Scale Subscale Scores Pre– and Post–Patient Panel (n = 177)
| Subscale | Pre-panel | Post-panel | P | Cohen d |
|---|---|---|---|---|
| Need for special training | 4.46 ± 0.46 | 4.57 ± 0.46 | 0.028 | 0.24 |
| Seriousness of type 2 diabetes | 4.06 ± 0.44 | 4.27 ± 0.45 | 0.000 | 0.47 |
| Value of tight glucose control | 3.96 ± 0.38 | 4.06 ± 0.47 | 0.042 | 0.23 |
| Psychosocial impact of diabetes | 4.23 ± 0.47 | 4.50 ± 0.43 | 0.000 | 0.60 |
| Attitude toward patient autonomy | 4.01 ± 0.44 | 4.16 ± 0.47 | 0.003 | 0.33 |
Following the panel, we observed positive improvements in diabetes attitudes for all five subscales (Table 2): “need for special training” (mean improvement = 0.11, t = −2.215, P = 0.028, n = 177); “seriousness of type 2 diabetes” (mean improvement = 0.21, t = −4.461, P <0.001); “value of tight glucose control” (mean improvement = 0.10, t = −2.054, P = 0.042); “psychosocial impact of diabetes” (mean improvement = 0.26, t = –5.577, P <0.001); and “attitude toward patient autonomy” (mean improvement = 0.15, t = −3.061, P = 0.003). Post-panel mean scores ranged from 4.06 (“value of tight glucose control”) to 4.57 (“need for special training”). We observed the largest magnitude of change in the “psychosocial impact of diabetes” subscale, with a Cohen d of 0.60 indicating a medium effect (Table 2). For the 55 respondents reporting diabetes stigma, we observed positive changes in diabetes attitudes post-panel in “seriousness of type 2 diabetes” (mean difference = 0.20, t = −2.043, P = 0.048) and “value of tight glucose control” (mean difference = 0.22, t = −2.069, P = 0.045). For the short-answer questions post-panel, only 34 of the 55 respondents answered the question, and of these, 26 indicated a positive change in attitudes. This finding did not differ from respondents who did not report pre-panel diabetes stigma (χ2 = 0.103; P = 0.749).
Themes
Diabetes Stigma: People With Type 2 Diabetes Bring It on Themselves
The 55 respondents (29.4%; total n = 187) indicating personal stigma toward people with diabetes felt that type 2 diabetes was self-inflicted, as demonstrated by the following quotations (see Table 3 for additional quotations):
“Those with type 2 ‘brought it on themselves’ in a way because of poor lifestyle and diet choices.” [ID 518]
“I have a small stigma against people with type 2 diabetes because I usually think it is self-inflicted.” [ID 776]
TABLE 3.
Additional Respondents’ Representative Quotations
| Theme | |
|---|---|
| Diabetes stigma: people with type 2 diabetes bring it on themselves | “There is an association (whether warranted or not) with personal responsibility (or lack-thereof).” [ID 420] |
| “For individuals with type 2 diabetes, who, for variety of reasons fail to manage or prevent their condition: yes, I see them as weak willed and lazy. I know that there are socioeconomic and educational barriers that propagate this condition in these people, but even so, I can’t ‘drink the Koolaid’ and look at these patients solely as victims of circumstances entirely out of their control.” [ID 866] | |
| “I find I have a stigma against some people with type 2 diabetes because they could have prevented the disease on their own with lifestyle changes. It’s harder for me to feel as empathetic towards them, but I have to remember their life circumstances such as education, access to food, how they were raised, etc.” [ID 827] | |
| “I understand a bit more about the disease and realize there are a lot of factors that go into it, and sometimes socioeconomic status is truly what is causing the non-ideal blood sugar levels.” [ID 177] | |
| Diabetes attitude changes: increased empathy and understanding | “I think I have a greater appreciation for those who have diabetes and the daily struggles they endure as their disease affects almost every aspect of their lives.” [ID 472] |
| “It made me see the panel as people and not just diabetes patients.” [ID 818] | |
| “I think that I will take it much more seriously. I was under the impression that ‘Hypertension and Diabetes’ are run-of-the-mill primary care doctor issues; but after a year and a half of school and seeing how these diseases can affect other organ systems, I understand the necessity of good blood glucose control. Moreover, hearing what the speakers fear most in regard to their diabetes gave the disease a human face to tie to it and take its treatment more seriously.” [ID 509] | |
| “I am going to try to be more compassionate and try to think of the patient’s experience and bias before I form my own opinions. As a doctor, I am there as an educator and a healer, not a judge and a jury.” [ID 484] | |
| “I have a lot more respect for people with the disease. I honestly did not realize how taxing diabetes can be and the drastic changes it can have on your body.” [ID 308] |
These respondents overtly directed stigma toward people with type 2 diabetes and not type 1 diabetes. Further, they made assumptions about patients’ health beliefs by stating that patients with type 2 diabetes do not take care of their bodies or do not care about their health. Several respondents wrote comments voicing their judgement about patients with type 2 diabetes:
“I do judge the people that develop diabetes later in life because of poor lifestyle and eating habits. I see this as a lack of concern for their own well-being. In general, I find obesity and those who let themselves gain ridiculous amounts of weight to be disgusting.” [ID 730]
Respondents with bias toward type 2 diabetes described feeling less empathy toward these patients because they could have prevented the disease or managed it better:
“I do not have as much sympathy for those who struggle with type 2 if they refuse to put together a good health plan for themselves.” [ID 939]
Importantly, 132 respondents (70.6%) stated that they did not have any personal stigma toward people with diabetes. These respondents recognized that the etiology of diabetes extends beyond diet and exercise and includes genetic factors and social determinants of health:
“I think stigma is harsh. There is the thought of most cases of type 2 diabetes being preventable with lifestyle changes, but we don’t know/can’t judge lifestyles due to the multifaceted issues that are difficult to compute (e.g., socioeconomic status, access to primary care, access to food, genetics). These factors and more make it extremely difficult to judge or have stigmas about people with diabetes.” [ID 949]
Respondents also felt strongly that patients with diabetes should not be judged for their dietary or exercise choices, as articulated by the following quotation:
“People are people, and there is a lot of misinformation on the Internet about what diabetes is. You never know what has happened in a person’s life, and I think judging people for dietary or exercise choices helps no one.” [ID 974]
Further, many believed that the role of the physician was to educate patients rather than place blame or judgment:
“Regardless of the etiology of a patient’s diabetes, the job of the physician is to treat and educate patients to the best of our ability, not to judge the lifestyle or decisions of a patient. Often, there is more to a person’s disease and story then we can assume.” [ID 415]
“Most people are not to blame for their disease and deserve help and education rather than ridicule or judgment.” [ID 215]
Diabetes Attitude Changes: Increased Empathy and Understanding
After the panel, 106 respondents (77.4%; total n = 137) showed a positive change in their attitudes toward diabetes. Respondents overwhelmingly reported an increased understanding of the seriousness of diabetes and empathy for the day-to-day struggles of managing diabetes. Listening to panel members’ struggles with hypoglycemia and hyperglycemia, as well as diabetes complications, appeared to affect respondents’ attitudes, as evidenced in the following statements:
“I feel more empathy for those with diabetes because the panel allowed me to hear more people’s stories about the struggles that come with living with diabetes.” [ID 938]
“I do believe that my attitude changed. I have more empathy for the daily struggle associated with managing one’s blood sugar. I still believe that people need to have the self-motivation to manage their condition but I have a greater understanding as to why that can be difficult.” [ID 382]
Respondents also learned about self-care behaviors, psychosocial issues, and financial costs from panel members:
“I am more aware of the psychosocial aspect of the disease and must be able to address that aspect of patient care in the future.” [ID 903]
To many of the respondents, hearing directly from the people with diabetes humanized the disease. As this respondent expressed:
“I didn’t know much about diabetes before listening to the panel. I thought it was a disease ‘those people’ get. The panel really personalized it for me. I am very interested in learning more about it and helping my patients manage it in the future.” [ID 635]
Further, respondents emphasized the importance of being compassionate with patients and remaining nonjudgmental. This respondent recognized that the role of the physician was to educate and help the patient:
“I think listening to the panel reminded me how important it is to be compassionate, patient, and nonjudgmental when I’m talking with patients about their health and lifestyle. It can be easy to get into a routine with patients, especially if they have the ‘same’ disease, but it’s so important to go into every appointment fresh and ready to work as part of their team.” [ID 409]
Listening to panel members increased respondents’ understanding of diabetes along with their respect for the people managing it. Respondents commented on the amount of effort people with diabetes put into managing their diabetes:
“I gained a better understanding of diabetes in general but also gained a higher sense of respect for people with diabetes that work to control their disease. I never realized how much work had to be put in to keep their glucose levels stable, and listening to how people started exercising and taking better care of themselves was encouraging.” [ID 434]
Discussion
In this feasibility study, we assessed second-year medical students’ diabetes attitudes and diabetes stigma before and after a contact-based educational panel. Nearly one-third of respondents reported harboring stigma toward patients with type 2 diabetes. These respondents believed that type 2 diabetes was a result of unhealthy eating and sedentary lifestyles, which resulted in people being overweight or obese. They felt less empathy for patients with type 2 diabetes because they thought patients could have prevented the disease or controlled it better. Importantly, more than two-thirds of respondents did not hold stigma toward any patients with diabetes. These respondents acknowledged that the cause of diabetes extended beyond lifestyle factors and included genetics and social determinants of health. Further, these respondents thought that the role of the physician was to educate and treat patients rather than judge and blame them for their disease. After the contact-based education patient panel, all five Diabetes Attitude Scale subscales improved, with the largest effect on the “psychosocial impact of diabetes” subscale. Qualitatively, more than three-quarters of respondents indicated a positive change in their attitude toward diabetes, with most noting an increase in empathy and understanding of the disease. After listening to panel members, respondents were more aware of the severity of diabetes and the daily struggles patients faced managing it. Both the quantitative and qualitative data support the use of a one-time contact-based education approach to improve diabetes attitudes and reduce diabetes stigma among medical students.
The degree to which patients experience diabetes stigma has numerous implications for individual and public health. Patients who perceive more diabetes stigma report higher levels of psychological distress, more pronounced depressive symptoms, less social support, and lower quality of life (17). Patients with psychological distress and depression are less likely to adhere to dietary, exercise, and medication regimens (31,32) and more likely to have suboptimal glycemia (32) and to experience complications (e.g., retinopathy, neuropathy, nephropathy, macrovascular complications of cardiovascular disease, hypertension, and sexual dysfunction [33,34]), poor physical functioning (35), increased hospitalization, and mortality (36). Stigma and negative experiences with type 2 diabetes can alter feelings of self-worth and lead to internalized stigma (16). Internalized stigma then can lead to fewer self-care behaviors, treatment nonadherence, difficulties with meaningful social interactions, and social isolation (14,16). When patients develop a negative relationship with their diabetes, they may change how they behave in public, try to hide the disease, have a lower sense of self-worth, and internalize stigma (16). They may struggle with meaningful social interactions and feel disconnected from friends and loved ones (16).
People with diabetes consistently report feelings of “blame and shame” (13,14), including self-blame (12,16). Many patients report feeling that most of the blame is directed at obesity as opposed to type 2 diabetes. This is consistent with our findings, but it is notable that patients with diabetes who do not struggle with weight also experience self-blame (13). Negative stereotypes, including the idea that patients with diabetes are lazy and gluttonous, are prevalent in the literature (13,14,17), and our findings reflect the common perception that patients are to blame for their condition.
Patients report stigma originating from many sources, including the media, family and social contacts, and health care providers. Stigmatizing interactions with health care providers can feel hurtful and judgmental. In the obesity literature, this is shown to be demotivating (37) and may cause patients to avoid medical appointments, search for information from other sources, or seek a new health care provider (13,37). Patients may also perceive that others think they create a burden on the health care system (14). Stigma may also increase with increasing therapy intensity, and patients requiring insulin therapy (with type 1 or type 2 diabetes) may be experiencing greater stigma than those who do not require insulin (14).
Experiencing diabetes stigma predicts higher A1C, higher BMI, and poorer self-reported glucose control; further, poor glucose control predicts feeling more stigma (14). This makes sense in the context of our findings, where students often cited weight and a lack of concern for personal health habits as “causes” of diabetes. Patients with type 2 diabetes may also feel judged more harshly when compared to patients with type 1 diabetes (13), which is consistent with our finding that reported stigma was directly entirely at patients with type 2 diabetes. This is not consistent with the findings of Liu et al. (14) that patients with type 1 diabetes perceive more stigma, which may be explained by the intensity of therapy and inherent increased “visibility” of type 1 diabetes (13,14).
This study was strengthened by our very high response rate, which increases the reliability and validity of the study findings. However, the study is not without limitations. Data from one medical school limits the generalizability of our findings to other programs, although this medical school has three campuses with very different geographical regions (rural, suburban, and urban). The Endocrine and Metabolism course is offered only to second-year students, limiting our ability to enroll students in the first, third, or fourth years. Our findings may be susceptible to selection bias, as students who volunteered to participate may have been more willing or motivated to answer questions about diabetes stigma and diabetes attitudes. Finally, stigma may be underreported due to social desirability bias. Future follow-up studies should use a randomized control design to assess the impact of two different educational interventions on medical student attitudes toward diabetes: a one-time contact-based educational panel versus a standard lecture-based course in diabetes.
In conclusion, this is the first study to explore diabetes attitudes and diabetes stigma in medical students. Our findings show that some medical students carry stigma toward patients with type 2 diabetes, which is supported by prior research in which patients described negative interactions with health care providers (13). Although medical students are not yet practicing providers, they do have patient contact and will soon be licensed practitioners. This finding is noteworthy because it documents that students harbor stigma toward people with type 2 diabetes. Importantly, this stigma can be changed with a simple and time-efficient educational intervention.
Acknowledgments
Acknowledgments
We thank the students who participated in the study and shared their attitudes about diabetes. We also thank the members of Diabetes Community Partners who participated in the patient panel and donated their time to share their experiences of living with diabetes to help educate medical students.
Funding
This research was supported by Health Resources & Services Administration grant no. D04RH28409.
Duality of Interest
No potential conflicts of interest relevant to this article were reported.
Author Contributions
E.A.B. provided substantial contributions to conception and design, acquisition of data, and data analysis. E.A.B., E.H.G., and L.L.J. provided substantial contributions to the interpretation of data and drafted the article. E.A.B., E.H.G., L.L.J., and T.R.F. revised the article critically for important intellectual content and gave final approval of the version of the article to be published. E.A.B. is the guarantor of this work and, as such, had full access to all the data in the study and takes full responsibility for the integrity of the data and the accuracy of the data analysis.
References
- 1.Pi-Sunyer FX, Maggio CA, McCarron DA, et al. Multicenter randomized trial of a comprehensive prepared meal program in type 2 diabetes. Diabetes Care 1999;22:191–197 [DOI] [PubMed] [Google Scholar]
- 2.Conn VS, Hafdahl AR, Mehr DR, Lemaster JW, Brown SA, Nielsen PJ. Metabolic effects of interventions to increase exercise in adults with type 2 diabetes. Diabetologia 2007;50:913–921 [DOI] [PubMed] [Google Scholar]
- 3.Maiorana A, O’Driscoll G, Goodman C, Taylor R, Green D. Combined aerobic and resistance exercise improves glycemic control and fitness in type 2 diabetes. Diabetes Res Clin Pract 2002;56:115–123 [DOI] [PubMed] [Google Scholar]
- 4.Karter AJ, Ackerson LM, Darbinian JA, et al. Self-monitoring of blood glucose levels and glycemic control: the Northern California Kaiser Permanente Diabetes registry. Am J Med 2001;111:1–9 [DOI] [PubMed] [Google Scholar]
- 5.Jacobson AM, Adler AG, Derby L, Anderson BJ, Wolfsdorf JI. Clinic attendance and glycemic control: study of contrasting groups of patients with IDDM. Diabetes Care 1991;14:599–601 [DOI] [PubMed] [Google Scholar]
- 6.Dyer PH, Lloyd CE, Lancashire RJ, Bain SC, Barnett AH. Factors associated with clinic non-attendance in adults with type 1 diabetes mellitus. Diab Med 1998;15:339–343 [DOI] [PubMed] [Google Scholar]
- 7.Khan H, Lasker SS, Chowdhury TA. Exploring reasons for very poor glycaemic control in patients with type 2 diabetes. Prim Care Diabetes 2011;5:251–255 [DOI] [PubMed] [Google Scholar]
- 8.Gafarian CT, Heiby EM, Blair P, Singer F. The Diabetes Time Management Questionnaire. Diabetes Educ 1999;25:585–592 [DOI] [PubMed] [Google Scholar]
- 9.Wdowik MJ, Kendall PA, Harris MA. College students with diabetes: using focus groups and interviews to determine psychosocial issues and barriers to control. Diabetes Educ 1997;23:558–562 [DOI] [PubMed] [Google Scholar]
- 10.Rubin RR, Peyrot M. Psychological issues and treatment for people with diabetes. J Clin Psychol 2001;57:457–478 [DOI] [PubMed] [Google Scholar]
- 11.Carls G, Huynh J, Tuttle E, Yee J, Edelman SV. Achievement of glycated hemoglobin goals in the US remains unchanged through 2014. Diabetes Ther 2017;8:863–873 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Beverly EA, Ritholz MD, Brooks KM, et al. A qualitative study of perceived responsibility and self-blame in type 2 diabetes: reflections of physicians and patients. J Gen Intern Med 2012;27:1180–1187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Browne JL, Ventura A, Mosely K, Speight J. ‘I call it the blame and shame disease’: a qualitative study about perceptions of social stigma surrounding type 2 diabetes. BMJ Open 2013;3:e003384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Liu NF, Brown AS, Younge MF, Guzman SJ, Close KL, Wood R. Stigma in people with type 1 or type 2 diabetes. Clin Diabetes 2017;35:27–34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tak-Ying Shiu A, Kwan JJ, Wong RY. Social stigma as barrier to diabetes self-management: implications for multi-level interventions. J Clin Nursing 2003;12:149–150 [DOI] [PubMed] [Google Scholar]
- 16.Kato A, Fujimaki Y, Fujimori S, et al. A qualitative study on the impact of internalized stigma on type 2 diabetes self-management. Patient Educ Couns 2016;99:1233–1239 [DOI] [PubMed] [Google Scholar]
- 17.Gredig D, Bartelsen-Raemy A. Diabetes-related stigma affects the quality of life of people living with diabetes mellitus in Switzerland: implications for healthcare providers. Health Soc Care Community 2017;25:1620–1633 [DOI] [PubMed] [Google Scholar]
- 18.Patten SB, Remillard A, Phillips L, et al. Effectiveness of contact-based education for reducing mental illness-related stigma in pharmacy students. BMC Med Educ 2012;12:120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Papish A, Kassam A, Modgill G, Vaz G, Zanussi L, Patten S. Reducing the stigma of mental illness in undergraduate medical education: a randomized controlled trial. BMC Med Educ 2013;13:141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Corrigan PW, Larson J, Sells M, Niessen N, Watson AC. Will filmed presentations of education and contact diminish mental illness stigma? Community Ment Health J 2007;43:171–181 [DOI] [PubMed] [Google Scholar]
- 21.Perry J, Watkins M, Gilbert A, Rawlinson J. A systematic review of the evidence on service user involvement in interpersonal skills training of mental health students. J Psychiatr Ment Health Nurs 2013;20:525–540 [DOI] [PubMed] [Google Scholar]
- 22.Schneebeli C, O’Brien A, Lampshire D, Hamer HP. Service user involvement in undergraduate mental health nursing in New Zealand. Int J Ment Health Nurs 2010;19:30–35 [DOI] [PubMed] [Google Scholar]
- 23.Pinfold V, Thornicroft G, Huxley P, Farmer P. Active ingredients in anti-stigma programmes in mental health. Int Rev Psychiatry 2005;17:123–131 [DOI] [PubMed] [Google Scholar]
- 24.Anderson RM, Fitzgerald JT, Funnell MM, Gruppen LD. The third version of the Diabetes Attitude Scale. Diabetes Care 1998;21:1403–1407 [DOI] [PubMed] [Google Scholar]
- 25.Krippendorff KH. Content Analysis: An Introduction to Its Methodology. 2nd ed. Thousand Oaks, CA, Sage Publications, Inc., 2004 [Google Scholar]
- 26.Neuendorf KA. The Content Analysis Guidebook. Thousands Oaks, CA, Sage Publications, 2002 [Google Scholar]
- 27.Cohen J. Weighted kappa: nominal scale agreement with provision for scaled disagreement or partial credit. Psychol Bull 1968;70:213–220 [DOI] [PubMed] [Google Scholar]
- 28.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics 1977;33:159–174 [PubMed] [Google Scholar]
- 29.Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77–101 [Google Scholar]
- 30.Aronson J. A pragmatic view of thematic analysis. Qual Rep 1995;2:1–3 [Google Scholar]
- 31.Lin EH, Katon W, Von Korff M, et al. Relationship of depression and diabetes self-care, medication adherence, and preventive care. Diabetes Care 2004;27:2154–2160 [DOI] [PubMed] [Google Scholar]
- 32.Lustman PJ, Anderson RJ, Freedland KE, de Groot M, Carney RM, Clouse RE. Depression and poor glycemic control: a meta-analytic review of the literature. Diabetes Care 2000;23:934–942 [DOI] [PubMed] [Google Scholar]
- 33.Jacobson AM. The psychological care of patients with insulin-dependent diabetes mellitus. N Engl J Med 1996;334:1249–1253 [DOI] [PubMed] [Google Scholar]
- 34.de Groot M, Anderson R, Freedland KE, Clouse RE, Lustman PJ. Association of depression and diabetes complications: a meta-analysis. Psychosom Med 2001;63:619–630 [DOI] [PubMed] [Google Scholar]
- 35.Bell RA, Smith SL, Arcury TA, Snively BM, Stafford JM, Quandt SA. Prevalence and correlates of depressive symptoms among rural older African Americans, Native Americans, and whites with diabetes. Diabetes Care 2005;28:823–829 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rosenthal MJ, Fajardo M, Gilmore S, Morley JE, Naliboff BD. Hospitalization and mortality of diabetes in older adults: a 3-year prospective study. Diabetes Care 1998;21:231–235 [DOI] [PubMed] [Google Scholar]
- 37.Puhl RM, Heuer CA. The stigma of obesity: a review and update. Obesity (Silver Spring) 2009;17:941–964 [DOI] [PubMed] [Google Scholar]