Abstract
Objective
We investigated the effects of prolonged‐release melatonin (PRM) on idiopathic rapid eye movement (REM) sleep behavior disorder (iRBD).
Methods
In this 4‐week, randomized, double–blind, placebo–controlled pilot study, 30 participants with polysomnography–confirmed iRBD were assigned to receive PRM 2 mg per day, PRM 6 mg per day, or placebo. Medication was administered orally 30 min before bedtime. Primary outcomes included scores from the Clinical Global Impression‐Improvement (CGI‐I) and the Korean version of the RBD questionnaire‐Hong Kong (RBDQ‐KR). The secondary outcomes included RBDQ‐KR factor 1 and factor 2 subscores, the Pittsburgh Sleep Quality Index score, the Epworth Sleepiness Scale score, the Short Form Health Survey version 2 score, and the frequency of dream–enacting behaviors assessed using a sleep diary.
Results
After 4 weeks, there were no differences in the proportions of patients with a CGI‐I score of much improved or very much improved among the study groups. In addition, RBDQ‐KR scores and secondary outcomes were not improved in all groups at 4 weeks, and there were no differences between the groups.
Conclusion
Our findings suggest that PRM may not be effective in treating RBD–related symptoms within the dose range used in this study. Further studies using doses higher than 6 mg per day are warranted.
Introduction
Rapid eye movement (REM) sleep behavior disorder (RBD) is a complex parasomnia characterized by loss of muscular atonia and dream–enacting behaviors (DEB) during REM sleep.1 In the absence of associated provoking factors or comorbidities, RBD has been generally classified as idiopathic or primary. When RBD is precipitated by medications or is related to other neurological or neurodegenerative disorders, autoimmune diseases, or brainstem lesions, it is classified as secondary.2 Previous longitudinal studies showed that more than 80% of the patients with idiopathic RBD developed α‐synucleinopathies such Parkinson's disease, dementia with Lewy bodies, or multiple system atrophy.3, 4
Since DEB in patients with RBD can contribute to sleep disruption and severe injuries for both the patients and their bed partners, it should be controlled with appropriate management.5, 6 Clonazepam is preferentially considered for the treatment of RBD symptoms but should be used with caution in patients with dementia, gait disorders, or concomitant obstructive sleep apnea.7 For this reason, alternative therapeutics to control RBD symptoms that also ensure effectiveness and safety are critically needed. Growing evidence suggests that melatonin is an effective treatment option for RBD.8
A prolonged‐release melatonin (PRM) formulation mimics the endogenous profile by releasing melatonin throughout the night, and this drug has been approved for the treatment of primary insomnia in many countries.9 Given that RBD usually occurs during the few hours prior to wake onset,10 PRM may be a better choice to improve RBD symptoms than immediate–release melatonin formulations with a short half‐life. Therefore, this 4‐week, randomized, placebo–controlled pilot study aimed to evaluate the efficacy and safety of low–dose (2 mg/day) and higher–dose (6 mg/day) PRM in patients with idiopathic RBD (iRBD).
Methods
Participants
Patients with RBD aged 18 or older were recruited from the Department of Neurology at Seoul National University Hospital (SNUH). The presence of RBD was defined based on the third edition of the International Classification of Sleep Disorders11 as an increase in tonic or phasic chin electromyography activity during REM sleep on polysomnography (PSG), and repeated episodes of behavior or vocalization that either are documented by PSG during REM sleep or occur in association with dream content during sleep. We excluded patients who (1) had any sign of dementia and parkinsonism confirmed on the Mini–Mental State Examination (below 26 points) and neurologic examination performed by a neurologist; (2) were treated for RBD; (3) received any medication that can affect RBD symptoms, such as selective serotonin reuptake inhibitors, tricyclic antidepressants, or monoamine oxidase inhibitors; or (4) had moderate to severe sleep apnea (apnea‐hypopnea index of 15 or greater) confirmed by PSG.
This study was approved by the Institutional Review Board of SNUH (1505‐084‐673) and was registered at ClinicalTrials.gov (NCT02836743). Written informed consent to participate was obtained from all enrolled patients.
Study design and procedures
This was a randomized, double–blind, placebo–controlled pilot study. At baseline, we obtained medical histories, performed physical examinations, and administered self–report questionnaires. Patients with suspected RBD were admitted to SNUH for overnight PSG, which was recorded using Embla RemLogic software (Natus, Pleasanton, CA). Participants who met the inclusion criteria were then randomly assigned to receive PRM 2 mg/day (one Circadin® 2 mg tablet plus two placebo tablets), PRM 6 mg/day (three Circadin® 2 mg tablets), or placebo (three placebo tablets) for 4 weeks. The tablets were identical in appearance. Randomization was performed at the SNUH Clinical Research Unit with a list of computer–generated random numbers (block of size 3). Medication was administered orally 30 min before bedtime. The participants were followed up at 4 weeks after treatment when self‐questionnaires were repeated and the participant's sleep diary, drug compliance, possible side effects, and concomitant medications were assessed. The use of medications affecting RBD symptoms was not allowed during the trial.
Measurements
Self‐questionnaires included the Clinical Global Impression–Improvement (CGI‐I) scale for evaluating general improvement,12 the Korean version of the RBD questionnaire‐Hong Kong (RBDQ‐KR), which consists of factor 1 (dream‐related) and factor 2 (behavior manifestation) questions to evaluate the clinical severity of RBD,13, 14 the Pittsburgh Sleep Quality Index (PSQI) to evaluate subjective sleep complaints,15 the Epworth Sleepiness Scale (ESS) to evaluate daytime sleepiness,16 and the Short Form Health Survey version 2 (SF‐36v2), which consists of physical component summary (PCS) and mental component summary (MCS) scales to evaluate health–related quality of life.17 The frequency of each scale item in the RBDQ‐KR at the 4‐week follow‐up was mainly based on the patients’ average symptoms during the treatment period. The frequency of DEB was assessed using a sleep diary. Adverse events were defined as any unintended responses thought to be related to treatment.
End points
The trial had two primary end points. The first primary end point was the proportion of patients with a CGI‐I evaluation of very much improved or much improved at 4 weeks. The second primary end point was the change from baseline to 4 weeks in the RBDQ‐KR total score. The secondary end points were the changes in the RBDQ‐KR factor 1 and factor 2 subscores, PSQI score, ESS score, SF‐36v2 PCS and MCS scores, and DEB frequency per week.
Statistical analysis
All analyses were carried out on the per‐protocol principle. Baseline characteristics were compared using the Fisher's exact test for categorical variables and the Kruskal–Wallis test for continuous variables. Changes from baseline to 4 weeks after treatment in questionnaire scores and DEB frequency were evaluated with the Wilcoxon signed–ranked test to assess the effect within a group and with the Kruskal–Wallis test to compare the group effects. All statistical tests were two‐tailed and differences were considered significant at a level of P < 0.05. Calculations were performed with SPSS 23.0 (SPSS Inc., Chicago, IL).
Results
Demographics and clinical characteristics
Between July 2016 and November 2017, a total of 30 patients were randomized. Of those, 20 patients received treatment (PRM 2 mg/day, n = 11; PRM 6 mg/day, n = 9) and 25 completed 4 weeks of the trial (last visit in December 2017) (Fig. 1). Two of 11 patients receiving PRM 2 mg/day reported adverse events including headache (n = 1) and nausea/vomiting (n = 1), which led to removal from the study. None of the patients receiving PRM 6 mg/day or placebo reported adverse events. Two other patients receiving PRM 2 mg/day and one patient receiving placebo dropped out of the study due to poor compliance to medication regimens. Finally, 25 patients were analyzed in this study. Demographic and baseline characteristics were similar across the study groups (Table 1).
Figure 1.
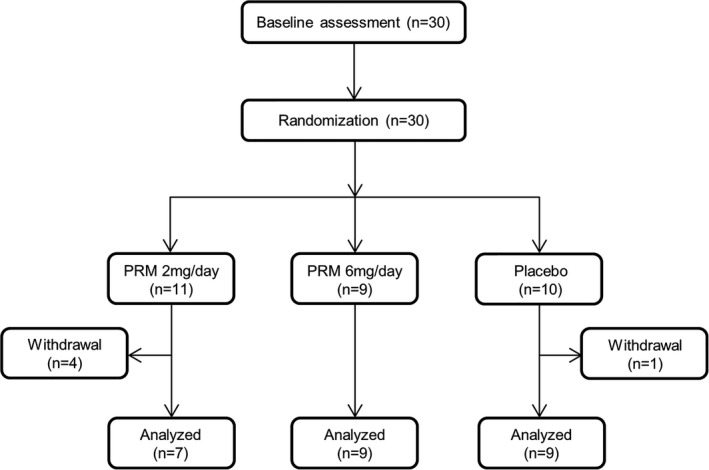
A flow chart illustrating the study process. PRM, prolonged‐release melatonin.
Table 1.
Baseline characteristics
| PRM 2 mg/day (n = 7) | PRM 6 mg/day (n = 9) | Placebo (n = 9) | P value | |
|---|---|---|---|---|
| Clinical variables | ||||
| Male sex | 4 (57%) | 5 (56%) | 7 (78%) | 0.662 |
| Age, years | 68.1 (9.1) | 64.7 (8.3) | 66.4 (8.5) | 0.599 |
| Age at onset, years | 64.4 (11.5) | 61.0 (8.1) | 63.0 (9.9) | 0.852 |
| Disease duration, years | 3.7 (3.5) | 3.7 (2.9) | 3.4 (2.7) | 0.938 |
| Body mass index, kg/m2 | 24.1 (4.9) | 23.3 (2.7) | 23.2 (2.8) | 0.998 |
| MMSE score | 28.5 (1.4) | 28.6 (1.1) | 27.7 (1.2) | 0.676 |
| Polysomnographic variables | ||||
| Time in bed, min | 500.6 (27.0) | 491.1 (43.9) | 501.8 (45.7) | 0.960 |
| Total sleep time, min | 399.4 (58.5) | 398.3 (73.9) | 374.5 (50.4) | 0.650 |
| Wake after sleep onset, min | 80.4 (43.1) | 74.8 (43.9) | 104.2 (44.1) | 0.084 |
| Sleep efficiency, % | 79.7 (10.0) | 79.6 (12.9) | 72.8 (7.1) | 0.250 |
| Sleep latency, min | 20.7 (9.5) | 25.9 (40.2) | 13.1 (7.3) | 0.279 |
| REM sleep latency, min | 111.7 (36.1) | 86.4 (34.7) | 129.2 (48.5) | 0.102 |
| N1 sleep, % | 28.0 (13.8) | 23.9 (6.2) | 30.6 (9.4) | 0.244 |
| N2 sleep, % | 47.5 (13.6) | 50.0 (6.4) | 42.5 (8.6) | 0.157 |
| N3 sleep, % | 3.9 (4.9) | 4.5 (5.6) | 7.1 (7.6) | 0.669 |
| REM sleep, % | 20.5 (6.3) | 21.6 (6.7) | 20.7 (6.8) | 0.892 |
| AHI, events/h | 5.9 (3.7) | 5.5 (4.5) | 7.7 (6.4) | 0.813 |
Data are n (%) and the mean (standard deviation).
AHI, apnea–hypopnea index; MMSE, Mini–Mental State Examination; PRM, prolonged‐released melatonin.
Primary outcomes
After 4 weeks, there were no differences in the proportions of patients with a CGI‐I score of very much improved or much improved across the study groups (P = 1.000; Fig. 2). All groups showed no significant improvement in the RBDQ‐KR total score at 4 weeks after treatment compared with the total score at baseline (Fig. 3). Changes in the RBDQ‐KR total score also did not differ among the groups (P = 0.744) (Table 2).
Figure 2.
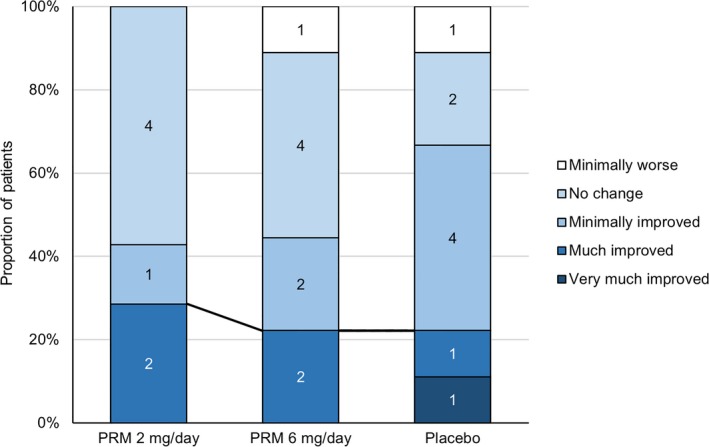
Proportion of patients for each Clinical Global Impression‐Improvement score at the 4‐week follow‐up. PRM, prolonged‐release melatonin.
Figure 3.
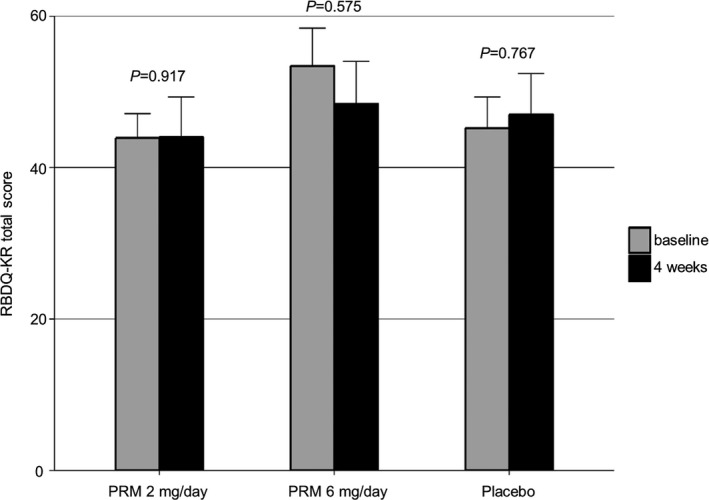
Changes in the Korean version of the REM sleep behavior disorder questionnaire‐Hong Kong (RBDQ‐KR) score at baseline and the 4‐week follow‐up. PRM, prolonged‐release melatonin.
Table 2.
Primary and secondary outcomes at baseline and 4 weeks according to study group
| PRM 2 mg/day (n = 7) | PRM 6 mg/day (n = 9) | Placebo (n = 9) | Group difference | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | 4 weeks | Difference | P | Baseline | 4 weeks | Difference | P | Baseline | 4 weeks | Difference | P | P | |
| RBDQ‐KR | 43.9 (8.4) | 44.0 (14.0) | 0.1 (9.6) | 0.917 | 53.4 (15.0) | 48.4 (16.9) | −5.0 (23.8) | 0.575 | 45.2 (12.2) | 47.0 (16.1) | 1.8 (8.7) | 0.767 | 0.744 |
| Factor 1 | 14.4 (3.4) | 15.7 (4.0) | 1.3 (5.7) | 0.500 | 17.0 (5.3) | 16.7 (7.2) | −0.3 (6.4) | 0.833 | 14.4 (4.6) | 14.1 (7.9) | −0.3 (5.0) | 0.726 | 0.782 |
| Factor 2 | 29.4 (7.1) | 28.3 (11.6) | −1.1 (5.3) | 0.581 | 36.4 (11.3) | 31.8 (11.4) | −4.7 (17.8) | 0.477 | 31.1 (9.1) | 32.9 (11.9) | 1.8 (8.5) | 0.438 | 0.585 |
| PSQI | 5.1 (0.8) | 6.1 (3.0) | 1.0 (3.5) | 0.528 | 6.3 (2.7) | 5.6 (2.6) | −0.8 (2.7) | 0.498 | 4.9 (2.2) | 6.0 (3.0) | 1.1 (4.1) | 0.497 | 0.500 |
| ESS | 4.6 (2.7) | 4.6 (3.5) | 0.0 (3.5) | 0.609 | 9.6 (3.5) | 8.2 (5.0) | −1.3 (2.4) | 0.103 | 6.8 (1.3) | 5.4 (1.9) | −1.4 (1.6) | 0.089 | 0.090 |
| SF‐36v2, physical | 47.6 (3.2) | 50.2 (5.6) | 2.6 (4.6) | 0.176 | 48.0 (7.1) | 48.5 (6.3) | 0.5 (6.6) | 0.594 | 54.1 (3.1) | 50.9 (5.9) | −3.2 (4.6) | 0.102 | 0.091 |
| SF‐36v2, mental | 54.7 (5.9) | 52.3 (9.7) | −2.4 (13.0) | 0.735 | 48.1 (7.9) | 48.9 (12.0) | 0.8 (7.6) | 0.953 | 53.2 (5.1) | 52.4 (3.9) | −0.8 (7.7) | 0.779 | 0.879 |
| DEB frequency | 3.9 (1.7) | 2.6 (2.5) | −1.3 (1.4) | 0.352 | 3.3 (1.4) | 2.9 (2.4) | −0.4 (1.6) | 0.307 | 4.1 (2.8) | 3.5 (2.9) | −0.6 (1.9) | 0.397 | 0.850 |
Data are n (%) and the mean (standard deviation).
DEB, Dream–enacting behaviors; ESS, Epworth Sleepiness Scale; PRM, prolonged‐released melatonin; PSQI, Pittsburgh Sleep Quality Index; RBDQ‐KR, Korean version of the REM sleep behavior disorder questionnaire‐Hong Kong; SF‐36v2, Short Form Health Survey version 2.
Secondary outcomes
The RBDQ‐KR factor 1 and factor 2 subscores, PSQI score, ESS score, SF‐36v2 PCS and MCS scores, and DEB frequency did not show improvement in all groups at 4 weeks with no differences among the groups (Table 2).
Discussion
To our knowledge, this is the first randomized controlled study to investigate the effect of PRM in patients with iRBD. The results found that neither low–dose nor higher–dose PRM improved the frequency or severity of RBD symptoms over the 4‐week trial period, and there were no significant differences from the placebo in the primary or secondary outcomes. Although the difference in the RBDQ‐KR Factor 2 score decreased from 36.4 to 31.8 at 4 weeks after treatment with PRM 6 mg/day, the standard deviation was relatively high and its p ‐> P value did not show a trend toward statistical significance (P = 0.477).
Previous studies have shown beneficial effects of melatonin on RBD–related symptoms,18, 19, 20, 21, 22, 23 and thus, this drug has been recognized as the second–line treatment option for RBD.8, 24 However, we did not find any beneficial effect of PRM in the current study. This conflicting result may be explained by the difference in pharmacokinetics between the drugs used. PRM has stable plasma melatonin concentration with a long elimination half‐life, whereas immediate–release melatonin formulations show a short–term increase in melatonin concentration with a short elimination half‐life.25 In opposition to our hypothesis, the pharmacokinetics of PRM may be unsuitable to produce a therapeutic effect in patients with iRBD. Alternatively, the dosage of melatonin may be insufficient to treat RBD symptoms. Some cases of melatonin treatment for RBD reported using up to 12 mg of melatonin,8 which is much higher than our dose. Therefore, before a definite conclusion can be reached about the efficacy of PRM in the treatment of RBD, further studies using doses higher than 6 mg/day should be conducted.
In contrast to previous studies,18, 20, 21, 22 the current study included only patients with iRBD. The effect of melatonin may differ between idiopathic and secondary RBD. Previous evidence suggests that melatonin protects exogenous levodopa from autoxidation in the striatum, which increases striatal levodopa bioavailability.26, 27 Considering that the striatal dopamine circuit regulates sleep quality,28 the combined use of melatonin and levodopa may yield synergistic effects on RBD, and therefore, melatonin may be more effective in some patients with secondary RBD. This theory may also explain the lack of effect of melatonin on iRBD in the current study, which is supported by previous studies of a melatonin receptor agonist showing that its efficacy was clearer in secondary RBD than in iRBD.27, 29
On the other hand, the possibility that melatonin itself is ineffective for the treatment of RBD cannot be excluded. Most of the previous observations are limited by retrospective design, open nature or the lack of a placebo–control arm. Only one randomized, double–blind, placebo–controlled crossover trial investigated the effect of melatonin in eight patients with idiopathic or secondary RBD.21 In this study, compared to baseline, treatment with melatonin over a 4‐week period decreased the number of 30‐s REM sleep epochs without muscle atonia, from 39% to 27% and led to a significant improvement in the CGI–Severity score from 6.1 to 4.6. However, the changes were not statistically significant compared to those in the placebo group. Only the CGI–Change score was lower in the melatonin treatment group than in the placebo group, but its median value was 3.3 (3 = minimally improved; 4 = no change). These findings do not clearly show that melatonin is superior to placebo in improving RBD symptoms.
This study has potential limitations. The participants were enrolled from one institute, and their number was small. Furthermore, because follow‐up PSG was not performed, the impact of melatonin on PSG parameters could not be investigated. Nevertheless, although this pilot study has inadequate power to detect a statistical significance, the results suggest that PRM may be ineffective for treating RBD symptoms within the dose range used in this study.
Author Contributions
Drs. JS Jun, R Kim, and JI Byun designed the research, acquired and analyzed the data, and drafted the manuscript. Drs. TJ Kim, JA Lim, JS Sunwoo, ST Lee, KI Park, K Chu, MH Kim, and SK Lee made critical revisions to the manuscript. Dr. KY Jung designed the research, analyzed the data, and made critical revisions to the manuscript.
Conflict of Interest
No conflicting relationship exists for the authors.
Acknowledgments
We thank Pf. Carlos H. Schenck for his insightful review and comments.
Funding Information
This work was supported by the National Research Foundation of Korea (NRF) grants funded by the Minister of Science, ICT and Future Planning, Republic of Korea (No. NRF‐2014R1A2A2A04003858; 2017M3C7A1029485).
[Correction added on 17 April 2019 after first online publication on 07 March 2019: The funding information has been corrected.]
Funding Statement
This work was funded by National Research Foundation of Korea (NRF) grant ; Minister of Science, ICT and Future Planning, Republic of Korea grants NRF‐2014R1A2A2A04003858 and 2017M3C7A1029485.
References
- 1. Schenck CH, Bundlie SR, Mahowald MW. Chronic behavioral disorders of human REM sleep: a new category of parasomnia. Sleep 1986;9:293–308. [DOI] [PubMed] [Google Scholar]
- 2. Högl B, Stefani A, Videnovic A. Idiopathic REM sleep behaviour disorder and neurodegeneration ‐ an update. Nat Rev Neurol 2018;14:40–55. [DOI] [PubMed] [Google Scholar]
- 3. Schenck CH, Boeve BF, Mahowald MW. Delayed emergence of a parkinsonian disorder or dementia in 81% of older men initially diagnosed with idiopathic rapid eye movement sleep behavior disorder: a 16‐year update on a previously reported series. Sleep Med 2013;14:744–748. [DOI] [PubMed] [Google Scholar]
- 4. Iranzo A, Tolosa E, Gelpi E, et al. Neurodegenerative disease status and post‐mortem pathology in idiopathic rapid‐eye‐movement sleep behaviour disorder: an observational cohort study. Lancet Neurol 2013;12:443–453. [DOI] [PubMed] [Google Scholar]
- 5. Schenck CH, Hurwitz TD, Mahowald MW. Symposium: normal and abnormal REM sleep regulation: REM sleep behaviour disorder: an update on a series of 96 patients and a review of the world literature. J Sleep Res 1993;2:224–231. [DOI] [PubMed] [Google Scholar]
- 6. Wallace DM, Shafazand S, Carvalho DZ, et al. Sleep‐related falling out of bed in Parkinson's disease. J Clin Neurol 2012;8:51–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Howell MJ, Schenck CH. Rapid eye movement sleep behavior disorder and neurodegenerative disease. JAMA Neurol 2015;72:707–712. [DOI] [PubMed] [Google Scholar]
- 8. McGrane IR, Leung JG, St Louis EK, Boeve BF. Melatonin therapy for REM sleep behavior disorder: a critical review of evidence. Sleep Med 2015;16:19–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Lyseng‐Williamson KA. Melatonin prolonged release: in the treatment of insomnia in patients aged ≥ 55 years. Drugs Aging 2012;29:911–923. [DOI] [PubMed] [Google Scholar]
- 10. Boeve BF. REM sleep behavior disorder: updated review of the core features, the RBD‐neurodegenerative disease association, evolving concepts, controversies, and future directions. Ann N Y Acad Sci 2010;1184:15–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. American Academy of Sleep Medicine . International Classification of Sleep Disorders. 3rd ed. Darien, IL: American Academy of Sleep Medicine, 2014. [Google Scholar]
- 12. Busner J, Targum SD. The clinical global impressions scale: applying a research tool in clinical practice. Psychiatry (Edgmont) 2007;4:28–37. [PMC free article] [PubMed] [Google Scholar]
- 13. Li SX, Wing YK, Lam SP, et al. Validation of a new REM sleep behavior disorder questionnaire (RBDQ‐HK). Sleep Med 2010;11:43–48. [DOI] [PubMed] [Google Scholar]
- 14. Yoo S, Moon HJ, Do SY, et al. The REM sleep behavior disorder screening quesionnaire: validation study of the Korean version (RBDQ‐KR). J Clin Sleep Med 2017;13:1429–1433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Buysse DJ, Reynolds CF, Monk TH, et al. The Pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res 1989;28:193–213. [DOI] [PubMed] [Google Scholar]
- 16. Johns MW. A new method for measuring daytime sleepiness: the epworth sleepiness scale. Sleep 1991;14:540–545. [DOI] [PubMed] [Google Scholar]
- 17. Jenkinson C, Coulter A, Wright L. Short form 36 (SF36) health survey questionnaire: normative data for adults of working age. BMJ 1993;306:1437–1440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Kunz D, Bes F. Melatonin as a therapy in REM sleep behavior disorder patients: an open‐labeled pilot study on the possible influence of melatonin on REM‐sleep regulation. Mov Disord 1999;14:507–511. [DOI] [PubMed] [Google Scholar]
- 19. Takeuchi N, Uchimura N, Hashizume Y, et al. Melatonin therapy for REM sleep behavior disorder. Psychiatry Clin Neurosci 2001;55:267–269. [DOI] [PubMed] [Google Scholar]
- 20. Boeve BF, Silber MH, Ferman TJ. Melatonin for treatment of REM sleep behavior disorder in neurologic disorders: results in 14 patients. Sleep Med 2003;4:281–284. [DOI] [PubMed] [Google Scholar]
- 21. Kunz D, Mahlberg R. A two‐part, double‐blind, placebo‐controlled trial of exogenous melatonin in REM sleep behaviour disorder. J Sleep Res 2010;19:591–596. [DOI] [PubMed] [Google Scholar]
- 22. McCarter SJ, Boswell CL, St Louis EK, et al. Treatment outcomes in REM sleep behavior disorder. Sleep Med 2013;14:237–242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Lin CM, Chiu RNMSHY, Guilleminault C. Melatonin and REM behavior disorder. J Sleep Disord Ther 2013;2:118. [Google Scholar]
- 24. Aurora RN, Zak RS, Auerbach SH, et al. Best practice guide for the treatment of REM sleep behavior disorder (RBD). J Clin Sleep Med 2010;6:85–95. [PMC free article] [PubMed] [Google Scholar]
- 25. Roth T, Nir T, Zisapel N. Prolonged release melatonin for improving sleep in totally blind subjects: a pilot placebo‐controlled multicenter trial. Nat Sci Sleep 2015;7:13–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Rocchitta G, Migheli R, Esposito G, et al. Endogenous melatonin protects L‐DOPA from autoxidation in the striatal extracellular compartment of the freely moving rat: potential implication for long‐term L‐DOPA therapy in Parkinson's disease. J Pineal Res 2006;40:204–213. [DOI] [PubMed] [Google Scholar]
- 27. Kashihara K, Nomura T, Maeda T, et al. Beneficial effects of ramelteon on rapid eye movement sleep behavior disorder associated with Parkinson's disease ‐ results of a multicenter open trial. Intern Med 2016;55:231–236. [DOI] [PubMed] [Google Scholar]
- 28. Qiu MH, Yao QL, Vetrivelan R, et al. Nigrostriatal dopamine acting on globus pallidus regulates sleep. Cereb Cortex 2016;26:1430–1439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Esaki Y, Kitajima T, Koike S, et al. An open‐labeled trial of ramelteon in idiopathic rapid eye movement sleep behavior disorder. J Clin Sleep Med 2016;12:689–693. [DOI] [PMC free article] [PubMed] [Google Scholar]


