Abstract
Background:
The effects of perioperative nonsteroidal anti-inflammatory drugs (NSAIDs) on soft tissue healing in humans have yet to be established.
Purpose:
To systematically review the literature addressing the effects of perioperative NSAID administration on soft tissue healing and clinical patient outcomes.
Study Design:
Systematic review; Level of evidence, 3.
Methods:
This review study was conducted in accordance with the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) statement. A review of the literature regarding the existing evidence for clinical effects of NSAID use on soft tissue healing was performed through use of the Cochrane Database of Systematic Reviews, the Cochrane Central Register of Controlled Trials, PubMed (1980 to present), and MEDLINE. Inclusion criteria for articles were as follows: outcome studies after soft tissue (ligament, meniscus, tendon, muscle) healing after surgical procedure with perioperative NSAID administration, at least 1 year of follow-up, English language, and human participants.
Results:
A total of 466 studies were initially retrieved, with 4 studies satisfying all inclusion criteria. Among the surgical procedures reported, 93% of the patients (4144/4451) underwent anterior cruciate ligament (ACL) reconstruction, 3% (120/4451) underwent rotator cuff repair, 3% (155/4451) underwent Bankart shoulder repair, and 1% (32/4451) underwent meniscal repair. The reported surgical failure rate among patients administered NSAIDs was 3.6% (157/4360). The reported surgical failure rate among control participants not given NSAIDs was 3.7% (147/3996). NSAID use showed no statistically significant effect on need for reoperation in meniscal repair (P = .99), ACL reconstruction (P = .8), and Bankart repair (P = .8) compared with no NSAID administration. Celecoxib administration had a significantly higher rate of retear (37%) after rotator cuff repair compared with ibuprofen (7%) (P = .009).
Conclusion:
Insufficient data are available to definitively state the effects of perioperative NSAIDs on soft tissue healing. Use of NSAIDs should be considered on a case-by-case basis and may not affect healing rates following either meniscal, ACL, rotator cuff, or Bankart repair. However, celecoxib (a selective COX-2 inhibitor) may inhibit tendon-to-bone healing in rotator cuff repair. Further research through clinical trials is required to fully determine whether NSAIDs have an adverse effect on soft tissue healing.
Keywords: sports medicine, soft tissue, NSAIDs, healing, ACL, meniscus, rotator cuff, Bankart
Nonsteroidal anti-inflammatory drugs (NSAIDs) are used to aid recovery by decreasing inflammation and pain after injury.1 This is attributed to the ability of NSAIDs to reduce prostaglandin production through the inhibition of cyclooxygenase (COX), an important enzyme for the formation of prostaglandin, an inflammatory mediator, from arachidonic acid.2 The subsequent reduction of prostaglandin concentration alters the cell signaling cascade after musculoskeletal injury and diminishes the inflammatory response.
The inflammatory cascade is a natural response to injury that entails the recruitment of macrophages and neutrophils that remove the resultant necrotic cell debris after an injury to provide an initial connective tissue framework.15 Interfering with the inflammatory process by using NSAIDs has been theorized to affect bone and soft tissue healing. The use of NSAIDs after orthopaedic surgery is a controversial topic with ongoing research. Conflicting results have been found regarding whether NSAIDs interfere with bone healing after surgery.4,6,9,12,19 However, the effects of NSAIDs on soft tissue healing in humans have yet to be established. Numerous studies on animal models have examined the effects of NSAIDs on soft tissue healing but have reported conflicting results.7,8,10,11,13
NSAIDs are an effective means of controlling postoperative pain after orthopaedic surgical procedures. Given the opioid crisis in the United States, it is relevant to look for safe alternatives for pain control.29 Thus, the aim of our study was to examine all available clinical studies regarding the effect of perioperative NSAID administration on soft tissue (ligament, meniscal, tendon, muscle) healing and clinical patient outcomes after sports medicine orthopaedic surgery procedures. We then analyzed differences in healing among varying sports medicine procedures to determine whether administering NSAIDs caused a detrimental effect. Our hypothesis was that perioperative NSAID administration does not affect soft tissue healing after sports medicine surgical procedures.
Methods
This study was conducted in accordance with the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) statement. A systematic review of the existing evidence for clinical effects of NSAID use on soft tissue healing was performed through use of the Cochrane Database of Systematic Reviews, the Cochrane Central Register of Controlled Trials, PubMed (1980 to present), and MEDLINE. Searches were performed using the following terms: nonsteroidal anti-inflammatory drug OR NSAID AND meniscus OR ligament OR tendon OR muscle OR soft tissue AND healing. The searches were performed in June 2018.
Inclusion criteria for articles were as follows: outcome studies of soft tissue (ligament, meniscal, tendon, muscle) healing after surgical procedure with perioperative NSAID administration, at least 1 year of follow-up, English language, and human patients. We excluded case reports, case series, and animal model studies. We reviewed titles, abstracts, and, when necessary, the full text of all identified articles to assess inclusion and exclusion criteria. All references from the included studies were reviewed to identify any other relevant articles, and no additional articles were discovered.
The primary outcome measure of our study was to compile all existing studies examining clinical effects of NSAIDs on soft tissue healing after sports medicine orthopaedic surgery procedures in human patients. The secondary outcomes of our study included identifying the procedures performed and their objective outcome scores to assess soft tissue healing rates. The level of evidence for each article was reported according to Wright et al.28 Of the 4 studies included, 3 studies3,22,24 were retrospective reviews with matched cohorts, providing level 3 evidence. The remaining study21 was described as a level 1 randomized controlled trial. However, the 24-month follow-up was 46% (82/180); therefore, we consider the level of evidence to be level 2 as a poor-quality randomized controlled trial.
Risk of bias was analyzed for each of the studies included. The study by Oh et al21 was a randomized controlled trial and was therefore assessed by use of the Cochrane “risk of bias” tool.14 Risk-of-bias judgment was deemed “low” across domains 1 through 5, and the study was therefore considered to have a low risk of bias. The remaining 3 studies were retrospective cohort studies providing level 3 evidence and as such were analyzed by use of the ROBINS-I (Risk Of Bias In Non-randomized Studies–of Interventions) assessment tool.25 All 3 retrospective cohort studies were analyzed across domains 1 through 7 via the ROBINS-I assessment tool and were assigned an overall risk-of-bias judgment of “moderate.”
Results
Study Selection
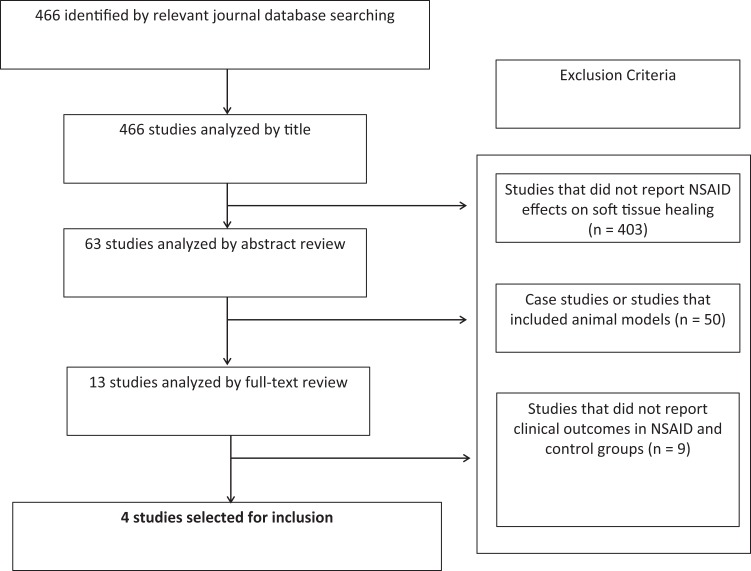
A total of 466 articles were initially retrieved. A PRISMA flowchart demonstrates the selection of articles based on inclusion and exclusion criteria (Figure 1). Studies that did not report the effects of NSAIDs on soft tissue healing were excluded based on title (n = 403). Studies or case studies that were performed on animal models were excluded based on abstract review (n = 50). Studies that did not report clinical outcomes following NSAID administration with no comparison with control groups were excluded upon full-text analysis (n = 9). Ultimately, we identified 4 studies on the effects of perioperative NSAIDs on healing after sports medicine procedures in humans.3,21,22,24
Figure 1.
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flow diagram. Search and selection criteria for systematic review of the literature addressing effects of perioperative nonsteroidal anti-inflammatory drug (NSAID) administration on soft tissue healing and clinical patient outcomes.
Patient Demographics
The review included a total of 4451 patients (2523 male, 1928 female), mean age 29.5 years (range, 15.9-61 years), who underwent soft tissue surgical repair and were administered NSAIDs perioperatively (Table 1). Weighted mean follow-up was 2.8 years (range, 21-66 months). Oh et al21 reported that 108 of 120 patients were evaluated for 2 weeks, but only 57 of 120 patients had a follow-up of 2 years in order to assess retear rates.
TABLE 1.
Study Design, Patient Demographics. and Clinical Outcome Scales of Included Perioperative NSAID Effect Studiesa
| Study | Level of Evidence | No. of Patients Administered NSAID (Male/Female) | Mean Patient Age, y | Mean Follow-up | Outcome Scales |
|---|---|---|---|---|---|
| Proffen et al22 | 3 | 32 (14/18) | 15.9 | 5.5 y | Need for reoperation |
| Soreide et al24 | 3 | 4144 (2404/1740) | 28.9 | 2.8 y | Graft survival; need for reoperation |
| Oh et al21 | 1 | 120 (39/81) | 61 | 108/120 patients assessed for 2 wk 57/120 patients had 2-y follow-up |
Retear of rotator cuff |
| Blomquist et al3 | 3 | 155 (66/89) | 24 | 21 mo | Recurrence of shoulder dislocation; need for reoperation |
aNSAID, nonsteroidal anti-inflammatory drug.
Procedures Performed
Among the studies included, 4 procedures were identified: 93% (4144/4451) of patients underwent anterior cruciate ligament (ACL) reconstruction,24 3% (120/4451) underwent rotator cuff repair,21 3% (155/4451) underwent Bankart shoulder repair,3 and 1% (32/4451) underwent meniscal repair.22 The type of NSAID administered was reported in 3 of 4 studies (Table 2). Proffen et al22 solely used ketorolac with a dosage adjusted to body weight and did not specific the length of treatment. Soreide et al24 used diclofenac, ketorolac, celecoxib, or another NSAID for a mean of 6.7 days but did not report the dosage. Oh et al21 compared celecoxib (200 mg twice a day) versus ibuprofen (385 mg 3 times a day) administered for 14 days after treatment. Blomquist et al3 did not report the specific NSAID used or the dosage but noted that the NSAID was administered for an interval ranging from 1 to 7 days postoperatively.
TABLE 2.
Surgical Procedure, NSAID Treatment Modality, and Clinical Failure Rates of Included Perioperative NSAID Effect Studiesa
| Study | Tissue/Procedure | Drug | Dosage | Length of Treatment | Failure Rate | P Value |
|---|---|---|---|---|---|---|
| Proffen et al22 | Meniscal repair | Ketorolac | 7.5-60 mg (adjusted to body weight) | Perioperative | NSAID: 34% (11/32) Control: 35% (26/75) |
.99 |
| Soreide et al24 | ACL reconstruction | Diclofenac (91.5%) Ketorolac (3.1%) Celecoxib (2.4%) Other NSAIDs (1%) |
NR | Mean, 6.7 days | NSAID: 3% (127/4144) Control: 3% (109/3678) |
.794 |
| Oh et al21 | Rotator cuff repair | Celecoxib (50%) Ibuprofen (50%) |
Celecoxib (200 mg, 2 times per day) Ibuprofen (385 mg, 3 times per day) |
14 days after surgery | Celecoxib: 37% (11/30) Ibuprofen: 7% (2/27) |
.009 |
| Blomquist et al3 | Bankart repair | NSAID | NR | 1-3 days (50%) 4-7 days (41%) ≥7 days (9%) |
NSAID: 5% (6/127) Control: 5% (12/243) |
.8 |
aACL, anterior cruciate ligament; NR, not reported; NSAID, nonsteroidal anti-inflammatory drug.
Outcome Data
In all 4 studies, healing rates were objectively measured by the need for reoperation or revision after initial surgery.3,21,22,24 The reported surgical failure rate among all patients administered NSAIDs was 3.6% (157/4360). The reported surgical failure rate among control participants who were not given NSAIDs was 3.7% (147/3996). Surgical failure rates among patients administered NSAIDs for each procedure were as follows: meniscal repair, 34% (11/32)22; ACL reconstruction, 3% (127/4144)24; rotator cuff repair, 23% (celecoxib 11/30 and ibuprofen 2/27)21; and Bankart repair, 5% (6/127).3 NSAID use showed no statistically significant effect on need for reoperation after meniscal repair (P = .99), ACL reconstruction (P = .8), and Bankart repair (P = .8) compared with no NSAID administration. Celecoxib had a significantly higher rate of retear after rotator cuff repair compared with ibuprofen (P = .009). Blomquist et al3 reported a recurrence rate of anterior shoulder dislocation after Bankart repair in 12% (15/127) of patients administered NSAIDs versus 14% (34/243), with a P value of .56, indicating no significant difference.
Complications
Proffen et al22 and Soreide et al24 reported that patients had no complications, whereas Blomquist et al3 did not report whether any patients had complications. Oh et al21 reported side effects of nausea, somnolence, gastrointestinal disorders, and pruritis 3 days after surgery as well as nausea, somnolence, and gastrointestinal disorders 2 weeks after surgery, with no significant difference between celecoxib and ibuprofen.
Discussion
The most important finding of this study was that perioperative NSAID administration does not affect soft tissue (meniscus, ligament, tendon) healing after sports medicine surgical procedures. Of the 3 studies examining ACL, shoulder labrum/capsule, or meniscus tissue, no difference in healing was found regardless of whether NSAIDs were administered.3,22,24 For rotator cuff repairs, celecoxib had a significant adverse effect on healing versus indomethacin.21
A recent systematic review indicated that NSAIDs had no effect on nonunion rates of bone healing after fracture or spinal fusion healing in clinical studies.4 Furthermore, another systematic review indicated that NSAID administration affected bone healing but not soft tissue healing; that review, conducted by Chen and Dragoo,6 was based solely on 9 animal studies. Chen and Dragoo6 concluded that NSAIDs did not demonstrate a difference in soft tissue healing according to markers such as tendon biomechanical strength and cross-sectional area measurements. Our finding of no difference in the rate of reoperation after NSAID administration indicates that the observed findings in animal studies may correlate clinically.
The observed difference in effects of NSAIDs on bone versus soft tissue healing may be due to the differences in pathways involved in healing. NSAIDs inhibit the COX-2 enzyme, further inhibiting prostaglandins, which are required for osteoblast and osteoclast activation during bone healing. However, soft tissue healing relies on many pathways and growth factors, including platelet-derived growth factor, among others, that are not affected by NSAIDs blocking the inflammatory pathway. Furthermore, tendon-to-bone healing involves a third category, which relies on a combined healing model including both bone and soft tissue.5 NSAIDs were not shown to affect soft tissue healing but did have a detrimental effect on tendon-to-bone healing in animal models.6 NSAIDs have a direct effect on the mediators involved in tendon healing.26,27 However, successful surgical reattachment of a failed tendon relies on the quality of soft tissue as well as fixation on bone. Formation of the subsequent enthesis relies on fibrous scar tissue and bone healing, in which NSAIDs may interfere with the inflammatory process.
Further differentiation between NSAID classes may be made, specifically with selective COX-2 inhibitors. Oh et al21 found that selective COX-2 inhibitors (celecoxib) significantly lowered tendon-to-bone healing after surgical repair of rotator cuff compared with nonselective indomethacin. A similar finding was observed by Lu et al17 in a rabbit model of rotator cuff healing. However, Cohen et al7 demonstrated that both indomethacin and celecoxib impaired rotator cuff healing in an animal model, with no difference observed between indomethacin and celecoxib. Rotator cuff healing is modulated by multiple enzymes including COX-1 and COX-2.20 Although an interplay of growth mediators is involved in rotator cuff healing, selectivity toward COX-2 inhibition may be a factor leading to delayed healing.
Dose and duration of NSAID use varied among studies. Blomquist et al3 and Soreide et al24 did not specify the dosing regimen used. All studies noted the length of NSAID treatment.3,21,22,24 Proffen et al22 delivered a dosage of ketorolac that was adjusted to patients’ body weight, ranging from 7.5 to 60 mg, either intraoperatively or in the postanesthesia care unit for patients undergoing meniscal repair. Soreide et al24 delivered diclofenac, ketorolac, celecoxib, or another NSAID for a mean length of treatment of 6.7 days in patients undergoing ACL reconstruction. Oh et al21 delivered celecoxib 200 mg 2 times a day and ibuprofen 385 mg 3 times a day for a 14-day period following rotator cuff repair. Blomquist et al3 did not specify which NSAID was used or the dosage but did report that 50% of patients received NSAIDs for 1 to 3 days, 41% received NSAIDs for 4 to 7 days, and 9% received NSAIDs for 7 days or more after Bankart repair. Although Blomquist et al3 were the only investigators who recorded multiple treatment durations, they did not report whether this had an impact on healing rate. NSAIDs have been shown to demonstrate a dose-dependent effect on bone healing, however further research is needed to clinically investigate this relationship following soft tissue procedures.16
Although our search criteria included muscle healing, we found no studies investigating healing postoperatively. We did find that NSAIDs had an adverse effect on muscle injury and acute hamstring tears in the long term.18,23
Limitations
This study has some limitations. Despite a complete review of the available literature, only a small number of studies met the inclusion criteria. These studies were heterogeneous with regard to their findings and the strength of their conclusions. In addition, variability in the type of procedures performed, along with a wide range of type of NSAIDs, duration of treatment, and dosage, affected the strength of pooling these studies. Consequently, it was difficult to achieve statistically significant conclusions and perform a meta-analysis. Therefore, our review is a descriptive systematic review, and no definitive conclusions can be made. The finding of only 4 clinical studies analyzing the effects of NSAIDs on soft tissue healing highlights the need for more research in human patients.
As with any systematic review, there is the possibility of noninclusion of relevant articles. However, our search strategy combined with searching the reference lists of all relevant articles should have minimized this type of bias.
Conclusion
We believe that our review of the available literature provides guidance regarding the use of NSAIDs following sports medicine orthopaedic surgery procedures in terms of healing rates and the need for reoperation. Insufficient data are available to definitively state the effects of perioperative NSAIDs on soft tissue healing. Use of NSAIDs should be considered on a case-by-case basis and may not affect healing rates after meniscal, ACL, rotator cuff, or Bankart repair. However, celecoxib (a selective COX-2 inhibitor) may inhibit tendon-to-bone healing in rotator cuff repair. Further research in clinical trials is required to fully determine whether NSAIDs have a negligible effect on soft tissue healing.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: A.R.V. has received educational support from DJO, Smith & Nephew, and Supreme Orthopedic Systems; research support from DJO; and hospitality payments from RTI Surgical. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
References
- 1. Abdul-Hadi O, Parvizi J, Austin MS, Viscusi E, Einhorn T. Nonsteroidal anti-inflammatory drugs in orthopaedics. J Bone Joint Surg Am. 2009;91(8):2020–2027. [PubMed] [Google Scholar]
- 2. Almekinders LC. The efficacy of nonsteroidal anti-inflammatory drugs in the treatment of ligament injuries. Sports Med. 1990;9(3):137–142. [DOI] [PubMed] [Google Scholar]
- 3. Blomquist J, Solheim E, Liavaag S, Baste V, Havelin LI. Do nonsteroidal anti-inflammatory drugs affect the outcome of arthroscopic Bankart repair? Scand J Med Sci Sports. 2014;24(6):e510–e514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Borgeat A, Ofner C, Saporito A, Farshad M, Aguirre J. The effect of nonsteroidal anti-inflammatory drugs on bone healing in humans: a qualitative, systematic review. J Clin Anesth. 2018;49:92–100. [DOI] [PubMed] [Google Scholar]
- 5. Bunker DLJ, Ilie V, Ilie V, Nicklin S. Tendon to bone healing and its implications for surgery. Muscles Ligaments Tendons J. 2014;4(3):343–350. [PMC free article] [PubMed] [Google Scholar]
- 6. Chen MR, Dragoo JL. The effect of nonsteroidal anti-inflammatory drugs on tissue healing. Knee Surg Sports Traumatol Arthrosc. 2013;21(3):540–549. [DOI] [PubMed] [Google Scholar]
- 7. Cohen DB, Kawamura S, Ehteshami JR, Rodeo SA. Indomethacin and celecoxib impair rotator cuff tendon-to-bone healing. Am J Sports Med. 2006;34(3):362–369. [DOI] [PubMed] [Google Scholar]
- 8. Dahners LE, Gilbert JA, Lester GE, Taft TN, Payne LZ. The effect of a nonsteroidal antiinflammatory drug on the healing of ligaments. Am J Sports Med. 1988;16(6):641–646. [DOI] [PubMed] [Google Scholar]
- 9. DePeter KC, Blumberg SM, Dienstag Becker S, Meltzer JA. Does the use of ibuprofen in children with extremity fractures increase their risk for bone healing complications? J Emerg Med. 2017;52(4):426–432. [DOI] [PubMed] [Google Scholar]
- 10. Ferry ST, Dahners LE, Afshari HM, Weinhold PS. The effects of common anti-inflammatory drugs on the healing rat patellar tendon. Am J Sports Med. 2007;35(8):1326–1333. [DOI] [PubMed] [Google Scholar]
- 11. Forslund C, Bylander B, Aspenberg P. Indomethacin and celecoxib improve tendon healing in rats. Acta Orthop Scand. 2003;74(4):465–469. [DOI] [PubMed] [Google Scholar]
- 12. Geusens P, Emans PJ, de Jong JJA, van den Bergh J. NSAIDs and fracture healing. Curr Opin Rheumatol. 2013;25(4):524–531. [DOI] [PubMed] [Google Scholar]
- 13. Hanson CA, Weinhold PS, Afshari HM, Dahners LE. The effect of analgesic agents on the healing rat medial collateral ligament. Am J Sports Med. 2005;33(5):674–679. [DOI] [PubMed] [Google Scholar]
- 14. Higgins JPT, Sterne JAC, Savović J, et al. A revised tool for assessing risk of bias in randomized trials. Cochrane Database Syst Rev. 2016;10(suppl 1):29–31. [Google Scholar]
- 15. Jones E, Churchman SM, English A, et al. Mesenchymal stem cells in rheumatoid synovium: enumeration and functional assessment in relation to synovial inflammation level. Ann Rheum Dis. 2010;69(2):450–457. [DOI] [PubMed] [Google Scholar]
- 16. Li Q, Zhang Z, Cai Z. High-dose ketorolac affects adult spinal fusion: a meta-analysis of the effect of perioperative nonsteroidal anti-inflammatory drugs on spinal fusion. Spine. 2011;36(7):e461–e468. [DOI] [PubMed] [Google Scholar]
- 17. Lu Y, Li Y, Li F-L, Li X, Zhuo H-W, Jiang C-Y. Do different cyclooxygenase inhibitors impair rotator cuff healing in a rabbit model? Chin Med J. 2015;128(17):2354–2359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Mackey AL, Mikkelsen UR, Magnusson SP, Kjaer M. Rehabilitation of muscle after injury—the role of anti-inflammatory drugs. Scand J Med Sci Sports. 2012;22(4):e8–e14. [DOI] [PubMed] [Google Scholar]
- 19. McDonald E, Winters B, Nicholson K, et al. Effect of postoperative ketorolac administration on bone healing in ankle fracture surgery. Foot Ankle Int. 2018;39(10):1135–1140. [DOI] [PubMed] [Google Scholar]
- 20. Oak NR, Gumucio JP, Flood MD, et al. Inhibition of 5-LOX, COX-1, and COX-2 increases tendon healing and reduces muscle fibrosis and lipid accumulation after rotator cuff repair. Am J Sports Med. 2014;42(12):2860–2868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Oh JH, Seo HJ, Lee Y-H, Choi H-Y, Joung HY, Kim SH. Do selective COX-2 inhibitors affect pain control and healing after arthroscopic rotator cuff repair? A preliminary study. Am J Sports Med. 2018;46(3):679–686. [DOI] [PubMed] [Google Scholar]
- 22. Proffen BL, Nielson JH, Zurakowski D, Micheli LJ, Curtis C, Murray MM. The effect of perioperative ketorolac on the clinical failure rate of meniscal repair. Orthop J Sports Med. 2014;2(5):2325967114529537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Reynolds JF, Noakes TD, Schwellnus MP, Windt A, Bowerbank P. Non-steroidal anti-inflammatory drugs fail to enhance healing of acute hamstring injuries treated with physiotherapy. S Afr Med J. 1995;85(6):517–522. [PubMed] [Google Scholar]
- 24. Soreide E, Granan L-P, Hjorthaug GA, Espehaug B, Dimmen S, Nordsletten L. The effect of limited perioperative nonsteroidal anti-inflammatory drugs on patients undergoing anterior cruciate ligament reconstruction. Am J Sports Med. 2016;44(12):3111–3118. [DOI] [PubMed] [Google Scholar]
- 25. Sterne JA, Hernán MA, Reeves BC, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016;355:i4919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Tsai W-C, Hsu C-C, Chen CPC, Chen MJL, Lin M-S, Pang J-HS. Ibuprofen inhibition of tendon cell migration and down-regulation of paxillin expression. J Orthop Res. 2006;24(3):551–558. [DOI] [PubMed] [Google Scholar]
- 27. Tsai W-C, Tang F-T, Hsu C-C, Hsu Y-H, Pang J-HS, Shiue C-C. Ibuprofen inhibition of tendon cell proliferation and upregulation of the cyclin kinase inhibitor p21CIP1. J Orthop Res. 2004;22(3):586–591. [DOI] [PubMed] [Google Scholar]
- 28. Wright JG, Swiontkowski MF, Heckman JD. Introducing levels of evidence to the journal. J Bone Joint Surg Am. 2003;85(1):1–3. [PubMed] [Google Scholar]
- 29. Zhao-Fleming H, Hand A, Zhang K, et al. Effect of non-steroidal anti-inflammatory drugs on post-surgical complications against the backdrop of the opioid crisis. Burns Trauma. 2018;6(1):25. [DOI] [PMC free article] [PubMed] [Google Scholar]