Abstract
Introduction
The autonomic nervous system (ANS) plays a vital role in regulation of the physiological processes during normal and pathological conditions. Heart rate variability (HRV) is regarded as a major indicator of the self-regulatory strength and balance of parasympathetic nervous system (PNS) and sympathetic nerve system (SNS) impulses, as interpreted by the intrinsic nervous system of the heart. The present study focuses on the evaluation of the effects of audible and mindful practice of chanting meditation on HRV and on the cognitive disposition.
Methodology
The subjects were randomly assigned to 2 different sounds based on monotone repetition. One was the Hare Krishna Mantram (HKM-Sanskrit experimental sound) and the other was a concocted sound (Sanskrit placebo). Changes in vagal tone were measured with respect to both time domain and frequency domains. Five-min baseline and postmeditation measurements were obtained on different days over the next 6 wk. The subjects who chanted the placebo/sham sound switched to the experimental sound at the 4-wk mark for the next 2 wk. All subjects completed an experience survey.
Results
Paired t test results for all HRV parameters achieved statistical significance in the test group. Statistical significance in all the aforementioned measures of HRV was also observed on switching the control group placebo sound chanting to the experimental sound. HRV wave forms showed relaxation, a pattern and experience survey suggests an increase in attributes associated with higher self-regulation.
Conclusion
This study suggests statistically significant efficacy data and that a larger randomized study is feasible to test the potential of the audible repetition of the HKM in clinical settings. It may therefore enable beneficial lifestyle for health creation and thus play a role in the prevention of chronic diseases. Further, large scale studies are required for a better perspective on the effect of mantram repetition on the HRV
Introduction
The popular treatise on Ayurveda, the Charaka Samhita (200 BCE) and other Vedic texts on personal empowerment, cite the process of audible self-repetition of the specific sounds (Mantram-Japa) as the optimal method for self-regulation.1,2 Audible mantram repetition (AuMR) is a common daily practice in India, even today. A mantram is a Sanskrit-derived word for manas, or “mind,” and tra, or “that which delivers”— phrases that when repeated attentively can deliver one from day-to-day stress. Little is known about the operating mechanisms of mantram chanting that affect human physiology. Previous randomized clinical trials by Bormann showed that the silent meditation technique at VA Medical Centers (Mantram Repetition Program [MRP]) fostered reduced self-reported and clinician-reported posttraumatic stress disorder (PTSD) symptoms at the 8-week follow-up mark.3,4 Improved outcomes were also found in HIV-infected adults who participated in MRP, along with reductions of salivary cortisol at post intervention.5 Wolf and Abell published their findings on audible repetition of the Sanskrit sound, the Hare Krishna Mantram (HKM), where subjects experienced a decrease in stress and subclinical depression.6 We therefore selected the same, as an experimental sound in this study to verify their findings.
This study focuses on the effects of a self-induced state of undivided attention to audible monotone repetition of specific sounds (AuMR technique) in novice subjects. The change seen in heart rate variability (HRV), during 5-minute recordings before and after practice of HKM, was compared with HRV of subjects who vibrated a concocted Sanskrit sound. In other words, we attempted to measure effects of attentively vibrating 2 qualitatively different Sanskrit sounds on a fundamental predictor of well-being.
HRV is the beat-to-beat fluctuation in heart rate (HR) that reflects the balance between the sympathetic nervous system (SNS) and parasympathetic nervous system (PNS).7 Previously, HRV was indirectly measured on an electrocardiogram, which shows the beat-to-beat variation in the heart beat—the R-R interval (ie, the interval between successive ventricular contractions).8 Power spectral frequency domain analysis of HRV is the preferred method of measurement of HRV in recent times, considering its higher consistency and reliability. It is constituted by 3 different components viz: very low frequency (VLF) component (0.003 Hz to 0.04 Hz), low frequency (LF) component (0.04 Hz to 0.15 Hz), and high frequency (HF) component (0.15 Hz to 0.4 Hz).8 The VLF band is associated with the SNS and renin-angiotensin system. The LF band indicates the baroreceptor activity and the HF band is associated with vagal activity and respiratory regulation.9-12
Periodic changes in HRV are an indicator of well-being. On the contrary, decreased variability in the R-R interval corresponds to a wide range of clinical ailments.13 HRV has been associated as a positive marker for aerobic fitness, stress resilience, and physiological and psychological flexibility14-16; and a negative marker for rheumatoid arthritis, stress, depression, neurological disorders (Parkinson’s disease, Alzheimer dementia), stroke, diabetes mellitus, and coronary artery disease.17-21
Mindfulness meditation in many cases is mental training that enhances an individual’s core psychological capabilities, such as attention and emotional self-regulation.22 Chanting meditation, like other meditation practices, focuses on the interaction among brain, body, mind, and behavior.23 It has been an integral part of lifestyle in India since antiquity.24 Scientific investigations have reported that mantram chanting had a positive effect on both physiological and psychological functions of the body.24 The objective of the present study was to investigate the effects of audible mantram repetition on flexibility of HRV in healthy subjects. This can imply its potential for utilization in the prevention of chronic illnesses.
Methodology
Study Design
This was an observational, randomized, double-arm, controlled, repeated measures study conducted in Colorado. The study fulfilled the criteria for an institutional review board exempt category because it is nonpharmacological, noninvasive, and reports the causality of a health-promoting behavior. Informed consent was obtained from each subject prior to the study.
Study Characterization
Caucasian and Hispanic subjects of either gender (21 to 63 y old) were included in the study. The subjects were in stable health, without any prior exposure to the AuMR meditation.
Procedure
The enrolled individuals were assigned to 2 interventions, both based on audible monotone repetition. The experimental group subjects chanted the experimental sound: “Hare Krishna Hare Krishna Krishna Krishna Hare Hare Hare Rama Hare Rama Rama Rama Hare Hare.” And the control group subjects chanted a concocted Sanskrit sound, “Thilla Kaasta Mahisha Bandhanam” (placebo sound). Emphasis was laid on the attentiveness to the individual syllables during chanting at a sustained speed and tone. The subjects were trained to audibly chant their assigned mantram. They chanted for 30 minutes daily in any posture (except lying down), to obtain at least 3 data points in the course of 4 to 6 weeks. Baseline HRV data were recorded sitting through the emWave Pro sensor (HeartMath, Boulder Creek, CA, USA) clipped to the ear lobe (for 5 min). The subjects in the control group were switched to the experimental sound after 4 weeks; their HRV parameters were measured for the next 2 weeks.
HRV Analysis
The HRV tracings were analyzed by both time and power spectral frequency domain methods. The change in HRV from baseline to postmeditation was measured with respect to inter beat index (IBI), VLF, LF, and HF waves.
Statistical Analysis
The continuous data were presented as mean ± standard deviation (SD) and categorical in terms of percentage. Analysis was performed using the paired t test method using the statistical software available in the Data Analysis menu of Microsoft Excel (Redmond, WA, USA). A P value less than .05 (P < .05) was considered statistically significant.
Results
Study Population
We initially intended to have 8 subjects in both groups and 16 subjects were enrolled for the study. Overall there were 4 dropouts. This left us with 12 subjects who were randomly assigned to the 2 groups, 7 in the experimental group and 5 in the control group. The reasons behind dropping out varied from a personal commitment, in the case of the experimental group subject, and lack of focus and commitment in the placebo group subjects. The mean age of the subjects in the experimental group and the control group was 32.14 ± 12.44 years and 49.8 ± 14.58 years, respectively.
Study Outcomes
HRV Curve Patterns
After the participant applied the AuMR technique, heart rhythm wave patterns were measured using emWave Pro. Figure 1 is a panel of representative HRV curves from the experimental group (3 males and 1 female) and the control group (2 male) participants. Wave forms shifted from that of an erratic HR premeditation, to smoother, more regular, lower amplitude seen in states of relaxation postmeditation. Such a pattern was absent when the AuMR technique was applied to the placebo sound.
Figure 1.

Effects of Experimental Sound (HKM) on HRV Wave Forms Before and After Meditation
Overall Statistical Data
A significant P value (<.05) was observed in postmeditation HRV variables (time and power spectral frequency domains) in the experimental group. However, this change was in the control group, was not significant (P = .53) (Table 2, Table 3, and Figure 2). A significant P value ranging from .00 to .04 was observed overall, for all the variables on switching the control group chant, from placebo sound to experimental sound (Table 4).
Table 2.
Effects of AuMR on Time Domain and Frequency Domain Variables in the Experimental Group
| Pre | HR | IBI | lnTotal | lnVLF | lnLF | lnHF | lnLF/lnHF | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Post | Pre | Post | Pre | Post | Pre | Post | Pre | Post | Pre | Post | Pre | Post | Pre | ||
| Female 1 | Average | 75.3 | 71.3 | 813.4 | 847.8 | 6.9 | 7.2 | 5.4 | 5.5 | 5.6 | 5.9 | 6.1 | 6.7 | -0.6 | -0.4 |
| SD | 11.1 | 2.1 | 121.3 | 25.2 | 0.4 | 0.2 | 0.8 | 0.4 | 0.6 | 0.1 | 0.5 | 0.3 | 0.9 | 0.7 | |
| P Value | .556 | .642 | .355 | .904 | .483 | .265 | .184 | ||||||||
| Female 2 | Average | 77.4 | 71.0 | 790.9 | 861.5 | 8.0 | 8.1 | 6.2 | 6.9 | 7.7 | 7.3 | 5.3 | 6.3 | 2.4 | 1.0 |
| SD | 7.4 | 7.5 | 72.0 | 86.2 | 8.0 | 8.1 | 0.4 | 0.3 | 0.4 | 0.8 | 0.2 | 0.3 | 0.4 | 0.5 | |
| P Value | .106 | .129 | .678 | .020 | .397 | .047 | .016 | ||||||||
| Female 3 | Average | 74.1 | 71.3 | 826.6 | 875.5 | 7.4 | 8.0 | 5.3 | 6.8 | 6.5 | 6.5 | 4.4 | 7.0 | 2.2 | 0.6 |
| SD | 9.0 | 12.2 | 111.7 | 164.0 | 0.8 | 1.1 | 0.4 | 0.6 | 1.9 | 1.3 | 0.8 | 1.1 | 0.2 | 1.0 | |
| P Value | .307 | .250 | .286 | .074 | .517 | .106 | .084 | ||||||||
| Female 4 | Average | 59.5 | 52.9 | 1013.3 | 1155.4 | 7.4 | 8.3 | 6.2 | 6.7 | 6.7 | 7.5 | 4.8 | 6.9 | 1.9 | 0.5 |
| SD | 5.0 | 0.4 | 80.6 | 11.2 | 0.4 | 0.8 | 0.7 | 1.4 | 0.3 | 0.4 | 0.6 | 1.2 | 0.5 | 0.9 | |
| P Value | .108 | .090 | .254 | .716 | .173 | .044 | .034 | ||||||||
| Male 1 | Average | 76.3 | 68.4 | 796.7 | 894.2 | 7.5 | 8.1 | 5.1 | 5.7 | 7.1 | 7.6 | 6.6 | 6.8 | 1.2 | 0.7 |
| SD | 5.8 | 6.1 | 63.6 | 89.5 | 0.3 | 0.6 | 0.3 | 1.1 | 0.4 | 0.6 | 0.6 | 0.9 | 0.6 | 0.8 | |
| P Value | .002 | .025 | .151 | .315 | .377 | .100 | .532 | ||||||||
| Male 2 | Average | 67.3 | 61.5 | 896.0 | 980.8 | 4.9 | 6.0 | 4.3 | 5.4 | 3.5 | 4.5 | 3.1 | 4.1 | 0.4 | 0.4 |
| SD | 5.4 | 4.3 | 75.3 | 71.2 | 0.5 | 0.4 | 0.5 | 0.6 | 0.5 | 0.5 | 0.3 | 0.2 | 0.5 | 0.2 | |
| P Value | .014 | .003 | .156 | .229 | .158 | .063 | .822 | ||||||||
| Male 3 | Average | 60.5 | 54.7 | 1007.9 | 1102.4 | 5.8 | 6.5 | 4.7 | 5.6 | 4.9 | 5.4 | 4.0 | 4.7 | 0.9 | 0.7 |
| SD | 9.3 | 3.6 | 145.9 | 70.6 | 0.4 | 0.3 | 0.4 | 0.1 | 0.5 | 0.8 | 0.8 | 0.3 | 0.4 | 0.7 | |
| P Value | .220 | .167 | .086 | .035 | .438 | .118 | .803 | ||||||||
| All Female | Average | 70.1 | 65.6 | 884.3 | 951.6 | 7.4 | 7.9 | 5.5 | 6.5 | 6.7 | 7.0 | 5.3 | 6.5 | 1.6 | 0.7 |
| SD | 11.2 | 10.8 | 146.6 | 162.7 | 0.6 | 0.8 | 0.9 | 0.9 | 1.1 | 1.0 | 0.7 | 1.0 | 1.3 | 1.0 | |
| P Value | .009 | .006 | .032 | .010 | .252 | .000 | .003 | ||||||||
| All Male | Average | 66.8 | 60.4 | 913.9 | 1007.9 | 6.2 | 7.0 | 4.7 | 5.8 | 5.2 | 5.9 | 4.5 | 5.2 | 0.8 | 0.6 |
| SD | 7.8 | 5.9 | 113.9 | 95.7 | 1.3 | 1.1 | 0.5 | 0.8 | 1.7 | 1.6 | 1.6 | 1.3 | 0.5 | 0.5 | |
| P Value | .000 | .000 | .003 | .002 | .039 | .001 | .517 | ||||||||
| All Participants | Average | 69.2 | 63.0 | 886.7 | 979.4 | 6.8 | 7.5 | 5.3 | 6.1 | 6.0 | 6.5 | 4.9 | 5.9 | 1.2 | 0.5 |
| SD | 9.2 | 8.8 | 120.3 | 134.0 | 1.1 | 1.0 | 0.7 | 0.9 | 1.5 | 1.3 | 1.1 | 1.2 | 1.1 | 0.9 | |
| P Value | .000 | .000 | .000 | .001 | .012 | .000 | .006 | ||||||||
Note: P < .05 is considered statistically significant.
Abbreviations: AuMR, Audible mantram repetition; HR, heart rate; IBI, inter beat index; VLF, very low frequency; LF, low frequency; HF, high frequency; SD, standard deviation.
Table 3.
Effects of AuMR on Time Domain and Frequency Domain Variables in Control Group
| Pre | HR | IBI | lnTotal | lnVLF | lnLF | lnHF | lnLF/lnHF | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Post | Pre | Post | Pre | Post | Pre | Post | Pre | Post | Pre | Post | Pre | Post | Pre | ||
| Female 1 | Average | 57.8 | 53.7 | 1043.3 | 1121.2 | 5.8 | 6.3 | 5.6 | 5.0 | 5.0 | 5.3 | 5.7 | 4.6 | 0.0 | 0.6 |
| SD | 3.1 | 2.7 | 54.9 | 56.2 | 1.3 | 0.6 | 0.9 | 0.7 | 0.6 | 0.6 | 0.5 | 0.8 | 0.6 | 0.7 | |
| P Value | .140 | .128 | .686 | .287 | .651 | .156 | .448 | ||||||||
| Female 2 | Average | 66.3 | 59.8 | 864.7 | 1018.1 | 6.3 | 6.8 | 4.8 | 5.6 | 5.2 | 4.9 | 5.2 | 5.9 | -0.1 | -1.1 |
| SD | 0.2 | 7.2 | 76.8 | 130.3 | 0.5 | 0.6 | 0.7 | 0.3 | 0.8 | 0.9 | 0.6 | 0.8 | 0.6 | 0.3 | |
| P Value | .291 | .104 | .339 | .295 | .628 | .026 | .211 | ||||||||
| Female 3 | Average | 77.0 | 67.8 | 783.1 | 888.6 | 5.3 | 5.2 | 3.8 | 3.3 | 3.7 | 4.2 | 4.3 | 4.3 | -0.6 | -0.1 |
| SD | 6.0 | 4.2 | 59.6 | 53.3 | 0.4 | 0.4 | 1.0 | 0.4 | 0.8 | 0.4 | 0.8 | 0.7 | 0.2 | 0.6 | |
| P Value | .013 | .001 | .057 | .387 | .535 | 1.000 | .260 | ||||||||
| Male 1 | Average | 67.0 | 62.1 | 905.5 | 981.1 | 6.6 | 7.0 | 5.6 | 5.9 | 5.7 | 5.7 | 4.9 | 5.6 | 1.8 | 0.1 |
| SD | 6.7 | 7.9 | 86.3 | 117.0 | 0.5 | 0.4 | 0.3 | 0.5 | 1.0 | 0.7 | 0.3 | 0.6 | 1.8 | 1.0 | |
| P Value | .022 | .054 | .053 | .192 | 1.000 | .111 | .344 | ||||||||
| Male 2 | Average | 61.5 | 55.0 | 986.5 | 1098.1 | 6.7 | 6.4 | 5.8 | 5.7 | 5.5 | 4.9 | 5.3 | 4.3 | 0.2 | 0.7 |
| SD | 5.1 | 3.9 | 84.0 | 75.1 | 0.6 | 0.0 | 0.6 | 0.6 | 0.7 | 0.6 | 0.8 | 0.6 | 0.5 | 0.3 | |
| P Value | .132 | .137 | .405 | .891 | .456 | .151 | .204 | ||||||||
| All Female | Average | 67.1 | 60.4 | 897.1 | 1009.3 | 5.8 | 6.1 | 4.7 | 4.7 | 4.6 | 4.8 | 5.1 | 5.0 | -0.2 | -0.2 |
| SD | 9.6 | 7.5 | 128.1 | 126.2 | 0.8 | 0.8 | 1.1 | 1.1 | 0.9 | 0.8 | 0.8 | 1.0 | 0.5 | 0.9 | |
| P Value | .002 | .001 | .455 | .868 | .633 | .678 | .909 | ||||||||
| All Male | Average | 64.3 | 58.5 | 946.0 | 1039.6 | 6.7 | 6.7 | 5.7 | 5.8 | 5.6 | 5.3 | 5.1 | 5.0 | 1.0 | 0.4 |
| SD | 6.1 | 6.8 | 88.1 | 108.8 | 0.5 | 0.4 | 0.4 | 0.5 | 0.7 | 0.7 | 0.6 | 0.9 | 1.4 | 0.7 | |
| P Value | .007 | .011 | .941 | .834 | .422 | .802 | .455 | ||||||||
| All | Average | 65.9 | 59.7 | 916.6 | 1021.4 | 6.2 | 6.3 | 5.1 | 5.1 | 5.0 | 5.0 | 5.1 | 5.0 | 0.3 | 0.0 |
| SD | 8.2 | 7.1 | 113.0 | 116.5 | 0.8 | 0.7 | 1.0 | 1.0 | 1.0 | 0.8 | 0.7 | 0.9 | 1.1 | 0.8 | |
| Participants | P Value | .000 | .000 | .456 | .976 | .931 | .615 | .554 | |||||||
Note: P < .05 is considered statistically significant.
Abbreviations: AuMR, audible mantram repetition; HR, heart rate; IBI, inter beat index; VLF, very low frequency; LF, low frequency; HF, high frequency; SD, standard deviation.
Figure 2.
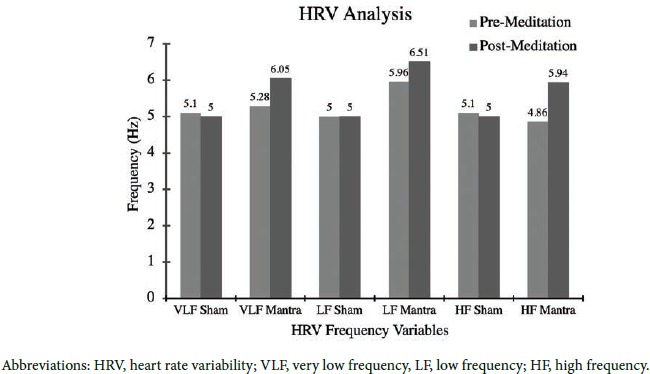
Effect of Meditation Sound on HRV Frequency Variables
Table 4.
Effect on Time Domain and Frequency Domain Variables after Switching Placebo Sound to Experimental Sound
| Pre | HR | IBI | lnTotal | lnVLF | lnLF | lnHF | lnLF/lnHF | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Post | Pre | Post | Pre | Post | Pre | Post | Pre | Post | Pre | Post | Pre | Post | Pre | ||
| Female 1 | Average | 60.5 | 62.4 | 946.9 | 1013.3 | 5.8 | 6.2 | 4.1 | 4.9 | 4.4 | 4.6 | 4.0 | 4.9 | -0.4 | -1.0 |
| SD | 3.0 | 2.8 | 19.6 | 21.9 | 1.1 | 0.8 | 0.4 | 0.1 | 1.4 | 1.4 | 1.2 | 1.3 | 0.0 | 0.6 | |
| P Value | .724 | .265 | .205 | .156 | .900 | .033 | .437 | ||||||||
| Female 2 | Average | 62.3 | 61.7 | 966.8 | 974.9 | 6.5 | 6.5 | 5.3 | 4.8 | 4.7 | 5.3 | 5.8 | 5.9 | -1.1 | -0.6 |
| SD | N/A | ||||||||||||||
| P Value | |||||||||||||||
| Female 3 | Average | 66.9 | 61.4 | 897.3 | 977.9 | 4.6 | 4.9 | 2.6 | 3.8 | 3.7 | 4.0 | 3.3 | 3.4 | 0.4 | 0.6 |
| SD | 1.6 | 0.9 | 23.3 | 15.1 | 0.3 | 0.1 | 0.8 | 0.1 | 0.1 | 0.0 | 0.2 | 0.1 | 0.1 | 0.1 | |
| P Value | .063 | .049 | .500 | .344 | .126 | .656 | .295 | ||||||||
| Male 1 | Average | 76.2 | 70.3 | 789.5 | 857.4 | 6.0 | 6.8 | 5.1 | 6.2 | 4.4 | 5.3 | 4.8 | 5.1 | -0.4 | 0.2 |
| SD | 2.8 | 3.0 | 29.6 | 33.9 | 0.6 | 0.4 | 0.8 | 0.6 | 0.1 | 0.4 | 0.1 | 0.6 | 0.1 | 0.8 | |
| P Value | .011 | .029 | .458 | .440 | .111 | .728 | .500 | ||||||||
| Male 2 | Average | 61.6 | 52.8 | 985.9 | 1141.4 | 5.6 | 6.4 | 4.6 | 5.7 | 4.7 | 4.7 | 3.4 | 4.5 | 1.4 | 0.2 |
| SD | 7.9 | 2.9 | 131.1 | 63.7 | 0.5 | 0.4 | 1.1 | 0.3 | 0.4 | 0.9 | 0.4 | 0.7 | 0.6 | 0.5 | |
| P Value | .158 | .124 | .158 | .324 | 1.000 | .040 | .185 | ||||||||
| All Female | Average | 62.6 | 62.1 | 930.3 | 1001.5 | 5.4 | 5.8 | 3.6 | 4.5 | 4.2 | 4.4 | 3.7 | 4.4 | -0.1 | -0.4 |
| SD | 4.3 | 2.1 | 31.8 | 25.7 | 1.0 | 1.0 | 0.9 | 0.6 | 1.1 | 1.1 | 0.9 | 1.2 | 0.5 | 1.0 | |
| P Value | .540 | .021 | .099 | .157 | .018 | .270 | .896 | ||||||||
| All Male | Average | 67.5 | 59.8 | 907.3 | 1027.8 | 5.8 | 6.5 | 4.8 | 5.9 | 4.6 | 4.9 | 3.9 | 4.7 | 0.7 | 0.2 |
| SD | 9.9 | 9.9 | 142.8 | 162.8 | 0.5 | 0.4 | 0.9 | 0.5 | 0.3 | 0.7 | 0.8 | 0.7 | 1.0 | 0.5 | |
| P Value | .029 | .038 | .056 | .111 | .423 | .063 | .429 | ||||||||
| All Participants | Average | 65.5 | 60.6 | 918.6 | 1023.6 | 5.8 | 6.4 | 4.6 | 5.6 | 4.5 | 4.8 | 3.9 | 4.8 | 0.4 | -0.1 |
| SD | 8.8 | 8.3 | 118.4 | 133.4 | 0.6 | 0.5 | 0.8 | 0.6 | 0.6 | 0.8 | 0.8 | 0.8 | 1.0 | 0.8 | |
| P Value | .033 | .003 | .016 | .026 | .115 | .023 | .482 | ||||||||
Note: P < .05 is considered statistically significant.
Abbreviations: AuMR, audible mantram repetition, HR, heart rate, IBI, inter beat index, VLF, very low frequency, LF, low frequency, HF, high frequency, SD, standard deviation.
Individual participant HRV data are also illustrated in Tables 2, 3, and 4. Six of the 7 subjects in the experimental group (Table 1) exhibited significant improvement in at least 1 parameter. Power spectral frequency measures improved (P < .05) in females 2, 3, and 4 (lnVLF, lnHF and lnLF/lnHF ratio) and male 3 (lnTotal and lnVLF). In terms of time domain measures of HRV, males 1 and 2 in the experimental group exhibited statistically significant reduction of mean HR and mean interbeat index, whereas individuals in the control group (Table 2) exhibited no significant improvement in power spectral frequency measures at all. Time domain measures (mean heart rate and interbeat index) decreased significantly in female 3 and male 1 (Table 2). The data of placebo group subjects reassigned to the HKM, at the 4-week mark, is depicted in Table 4. They exhibited an improvement of the power spectral frequency domains in 3 separate instances (lnLF of female 1 and lnHF of female 1 and male 2), at the 6-week mark. This finding was absent during the preceding 4 weeks when the same individuals practiced chanting of the placebo Sanskrit sound (Table 3). The number of significant P values in time domains remained unchanged in Tables 3 and 4.
Table 1.
Participant Demographics
| Subject Number | Experimental Group | Control Group | ||
|---|---|---|---|---|
| Participant | Age (y) | Participant | Age (y) | |
| 1 | Female 1 | 26 | Female 1 | 50 |
| 2 | Female 2 | 27 | Female 2 | 27 |
| 3 | Female 3 | 25 | Female 3 | 63 |
| 4 | Female 4 | 29 | Male 1 | 47 |
| 5 | Male 1 | 21 | Male 2 | 62 |
| 6 | Male 2 | 40 | ||
| 7 | Male 3 | 57 | ||
| Average Age | 32.14 | 49.80 | ||
| Standard Deviation | 12.44 | 14.58 | ||
Subjective Evaluation of Meditation Effects
A supplemental survey composed of 13 questions was conducted after 4 weeks for both the groups. Overall there was an 83% to 100% increase in love, deep inner peace, and connection toward a “higher power.” However, only 20% to 80% increase was reported by the control group (Figure 3 and Figure 4).
Figure 3.

Experience Survey of Meditation Effect on Experimental Group
Figure 4.

Experience Survey of Meditation Effect on Control Group
Discussion
Since antiquity, Sanskrit texts in Ayurveda have depicted the mantram meditation as a health code to adopt a lifestyle of conscious health creation. Audible chanting or use of mantrams has always been an integral part of Ayurveda and has been recognized as a valid method by which to enhance one’s health.1 This pilot study was conducted to validate those claims that mantram meditation has health benefits. We designed our research to reveal unambiguous results or effects on HRV parameters. Our design included one such authorized mantram sequence, the HKM, practiced by the Vedic traditions as prescribed in their texts, as well as a pseudo chanting sequence, which was not mentioned in the texts. This study finds preliminary efficacy data of the AuMR technique. In addition, this was a feasibility study to assess its capacity to enroll participants into a study of a larger sample size and participant adherence to the interventions. This technique is easy to learn and is convenient due to being audible and adaptable. Khalsa et al25 demonstrated an increase in cerebral blood flow to temporal lobe and posterior cingulate gyrus in audible chanting meditators, using single-photon emission computed tomography. HRV is a reliable measure ofvagal tone (PNS). Increase in HRV was observed postmeditation in this investigation. HRV is the physiological phenomena of variation of the R-R intervals, which provides the assessment of ANS activity.26 According to Tiller and McCraty, as HRV increases, more sine-wave pattern impulses generated in heart rhythm are transmitted through the vagus to the executive function centers in the brain.27,28 Sine-wave patterns are associated with positive emotional states without changes in breathing.29,30 The neural networks receiving these sensory stimuli enter into a state of neural synchrony. The central autonomic network plays a pivotal role in the modulation of neuronal activity.31 The end result of positive emotional states is cerebral cortical facilitation, resulting in increased inner tranquility, working memory, and psychological resilience.
In summary, the intrinsic nervous system of the heart positively affects vagal tone, which, in turn, is transmitted to the executive function centers of the brain.32 HRV was also shown to be strongly predictive of a person’s willpower to creating health promoting lifestyles.33 The present investigation shows a physiological improvement in HRV, as well as subjective psychological well-being, thus confirming this effect. When the data from each individual in both groups are considered, we found female subjects demonstrated higher baseline HRV than men, which confirms previous reports.34 This finding provides insights into the workings of a plausible pathway regarding how the AuMR technique affects the brain function. Reduction in HRV is medically significant because low HRV is associated with several chronic illnesses such as PTSD, myocardial infarction, anxiety, and degenerative neurological disorders.17-21 Chronic diseases can be prevented by elevating HRV through meditation, which promotes cardiac relaxation by increasing the ANS regulation.35 Vickhoff et al36 reported that mantram chanting elicited a high and regular amplitude variation that led to an elevated frequency domain of HRV Similarly, Bernardi et al37 showed that mantram chanting harmonizes and strengthens intrinsic cardiovascular rhythms and affects the baroreflex sensitivity. The baroreflex modification leads to a reduction in HR and, hence, increases HRV.37
The present study evaluates the effects of audible mantram-repetition on HRV through ANS regulation. Postmeditation, an increase in HRV with decreased HR was observed for all subjects in the experimental group, overall. Further, significant changes occurred in some HRV variables, on switching the control group chanting from placebo sound to experimental sound. This indicates that the AuMR technique elicits beneficial time and frequency domain changes marking an increase in HRV. The findings of our study are consistent with the previous studies, which demonstrated a significant increase in HRV through controlled regulation of ANS. This may also explain the findings of Wolf and Abell5 that the AuMR technique of HKM improves psychosocial function. Desh et al conducted a clinical trial to evaluate the effect of meditation on human physiology and observed that meditation significantly affects ANS. They concluded that meditation decreased the basal cardiac parameters, including HR and blood pressure, due to an increased function of PNS, and with augmentation of control over the SNS.38
Similarly, Delgado et al39 reported the postmeditation increase in HRV (indexed by increased lnLF/lnHF ratio) and autonomic regulation. In our study also, the lnLF/lnHF ratio showed a significant increase within the experimental group. According to Ferreira et al,40 the basic downstream mechanism behind increased HRV depends on the balance between SNS and PNS. SNS releases norepinephrine and produces positive inotropic and chronotropic responses through β-adrenoceptors stimulation. These responses lead to an increase in HR hence decreasing HRV. Conversely, the PNS releases acetylcholine through muscarinic receptor stimulation, which produces negative inotropic and chronotropic responses. Therefore, SNS and PNS operate antagonistically, and an increased HRV is observed under dominance of PNS activity.40 Similarly, Friedman demonstrated that predominance of vagal tone influences are associated with high HR control and elevated HRV. Low vagal HR control and decreased HRV has been associated with varied pathological states such as anxiety.41 Based on our study, we can conclude that mantram chanting leads to predominance of PNS in the sympatho-vagal balance. Consequently, elevated PNS activity induces smoother beat-to-beat variations of the heart, an indicator of increased HRV. The HRV curve patterns, changed from that of an erratic HR to a more regular and lower amplitude seen in states of relaxation associated with positive emotional states (Figure 1), validate the findings of Wolf and Abell.5
Some limitations of this preliminary study include a small sample size and short-term measurements of HRV. Second, there were more women than men in each group, which had an effect on the group average (females have higher vagal tone than males). Finally, HRV measurement among the control subjects had lesser data points available when they chanted the HKM for only 2 weeks. In addition, we were able to obtain only 1 HRV data point from 1 of the control group participants (female 2; see Table 3), as she could not return for the second HRV measurement, after switching to HKM.
The P value for HF data became significant in male 2 (aged 62 y) (Table 4), in whom we obtained 3 HRV data measurements during the 2-week period of practicing the HKM. This suggests that more data point collection beyond 4 weeks could have resulted in a significant change in the parameters in other subjects as well. Moreover, this was an unexpected finding, because it is harder to augment HRV in older men, in general.34
Our observations under controlled conditions seem to show a definite corroboration of health benefits. This indicates that claims regarding the efficacy of AuMR in particular may not be summarily dismissed, but rather merit attention and further research. Future studies are warranted to measure the long-term effects of AuMR on HRV and the inflammatory pathway. It can be a part of a suite of solutions for a wide range of diseases or disorders, particularly those caused by or related to lack of age adjusted healthy vagal tone. This could be an affordable and convenient preventative measure for checking the world’s chronic disease epidemic
Conclusion
This preliminary study suggests statistically significant efficacy data, and that a larger randomized study is worthwhile to test the potential of audible repetition of the HKM in clinical settings; Further, large-scale studies are required for a better perspective on the effects of mantram repetition on HRV.
Acknowledgements
The corresponding author acknowledges Knowledge Isotopes Pvt Ltd (http://www.knowledgeisotopes.com) for the medical writing assistance and Mr K. M. Rajaram and Dr Ryan Bissett for their suggestions.
Biographies
Venugopal R. Damerla, MD, ABoLM, is a staff physician at the Department of Internal Medicine/Primary Care, Denver Veterans Affairs Medical Center and lead scientist at the Prabhupada Research Institute for Integrative Medicine based in Longmont, Colorado.
Babette Goldstein, MED, is a certified yoga teacher and instructor of Mantram Science, at Prabhupada Research Institute for Integrative Medicine.
David Wolf, MSW, PhD, is a life coach and director, Satvatove Institute based in Gainesville, Florida.
Krishna Madhavan, PhD, is a professional research assistant at the Department of Pediatric Oncology, University of Colorado Denver, Anschutz Medical Campus, Aurora, Colorado.
Nancy Patterson BA, is an Instructor of Mantram Science, Prabhupada Research Institute for Integrative Medicine
Footnotes
Author Disclosure Statement
Funding Sources: Prabhupada Research Institute for Integrative Medicine. The authors declare no conflicts of interest.
References
- 1.Charaka S, Sutra S. The 3 Basic Desires of Life. Delhi, India: Chaukhambha Orientalia. [Google Scholar]
- 2.Bhaktivedanta Swami AC, Bhagavad G. As It Is. New York, NY: Macmillan; 1972. [Google Scholar]
- 3.Buttner MM, Bormann JE, Weingart K, Andrews T, Ferguson M, Afari N. Multi-site evaluation of a complementary, spiritually-based intervention for Veterans: The Mantram Repetition Program. Complement Ther Clin Pract. 2016;22:74-79. [DOI] [PubMed] [Google Scholar]
- 4.Bormann JE, Oman D, Walter KH, Johnson BD. Mindful attention increases and mediates psychological outcomes following mantram repetition practice in veterans with posttraumatic stress disorder. Med Care. 2014;52:S13-S18. [DOI] [PubMed] [Google Scholar]
- 5.Bormann JE, Gifford AL, Shively M, et al. Effects of spiritual mantram repetition on HIV outcomes: a randomized controlled trial. J Behav Med. 2006;29(4):359-376. [DOI] [PubMed] [Google Scholar]
- 6.Wolf DB, Abell N. Examining the effects of meditation techniques on psychosocial functioning. Res Soc Work Pract. 2003;13(1):27-42. [Google Scholar]
- 7.Evans S, Seidman LC, Tsao JC, Lung KC, Zeltzer LK, Naliboff BD. Heart rate variability as a biomarker for autonomic nervous system response differences between children with chronic pain and healthy control children. J Pain Res. 2013;6:449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tyagi A, Cohen M. Yoga and heart rate variability: A comprehensive review of the literature. Internat J Yoga. 2016;9(2):97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bansal D, Khan M, Salhan A, eds. A review of measurement and analysis of heart rate variability. Computer and Automation Engineering, 2009 ICCAE’09 International Conference on; 2009: IEEE. [Google Scholar]
- 10.Medicore. Heart rate variability analysis system clinical information. Medicore Web site. http://medi-core.com/download/HRV_clinical_manual_ver3.0.pdf. Accessed September 25, 2018.
- 11.Usui H, Nishida Y. The very low-frequency band of heart rate variability represents the slow recovery component after a mental stress task. PloS one. 2017;12(8):e0182611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shaffer F, Ginsberg J. An overview of heart rate variability metrics and norms. Front Pub Health. 2017;5:258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Vanderlei LCM, Pastre CM, Hoshi RA, Carvalho TDd, Godoy MFd. Basic notions of heart rate variability and its clinical applicability. Braz J Cardiovasc Surg. 2009;24(2):205. [DOI] [PubMed] [Google Scholar]
- 14.Billman GE. Heart rate variability: A historical perspective. Front Physiology. 2011;2:86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ferreira LF, Rodrigues GD, Soares PPdS. Quantity of aerobic exercise training for the improvement of heart rate variability in older adults. Int J Cardiovasc Sci. 2017;30(2):157-162. [Google Scholar]
- 16.An E, Nolty A, Rensberger J, Hennig N, Amano S, Buckwalter J. B-65 heart Rate variability as an index of stress resilience. Arch Clin Neuropsychol. 2016;31(6):637. [Google Scholar]
- 17.Wood SK. Cardiac autonomic imbalance by social stress in rodents: Understanding putative biomarkers. Front Psychology. 2014;5:950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Anichkov D, Platonova A. Clinical significance of heart rate variability indexes derived from 5-minute and 24-hour ECG recordings in patients with rheumatoid arthritis. Ration Pharmacother Cardiol. 2016;5(1):77-82. [Google Scholar]
- 19.Thayer JF, Ahs F, Fredrikson M, Sollers JJ, III, Wager TD. A meta-analysis of heart rate variability and neuroimaging studies: implications for heart rate variability as a marker of stress and health. Neurosci Biobehav Reviews. 2012;36(2):747-756. [DOI] [PubMed] [Google Scholar]
- 20.Oka H. Heart Rate Variability and Neurological Disorders: Clinical Assessment of the Autonomic Nervous System. New York, NY: Springer; 2017. [Google Scholar]
- 21.Cygankiewicz I, Zareba W. Heart Rate Variability: Handbook of Clinical Neurology. New York, NY: Elsevier; 2013. [DOI] [PubMed] [Google Scholar]
- 22.Tang Y-Y, Holzel BK, Posner MI. The neuroscience of mindfulness meditation. Nat Rev Neurosci. 2015;16(4):213. [DOI] [PubMed] [Google Scholar]
- 23.National Center for Complementary and Integrative Health (NCCIH). Meditation: In depth. NCCIH Web site. https://nccih.nih.gov/health/ meditation/overview.htm. Updated April 2016. June 2, 2018.
- 24.Kumar S, Nagendra H, Manjunath N, Naveen K, Telles S. Meditation on OM: Relevance from ancient texts and contemporary science. Int J Yoga. 2010;3(1):2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Khalsa DS, Amen D, Hanks C, Money N, Newberg A. Cerebral blood flow changes during chanting meditation. Nuclear Med Communicat. 2009;30(12):956-961. [DOI] [PubMed] [Google Scholar]
- 26.No authors listed Heart Rate Variability and Sudden Cardiac Death. Clinical Trials Web site. https://clinicaltrials.gov/ct2/show/NCT00005235. Updated December 24, 2015. Accessed August 19, 2018.
- 27.Tiller WA, McCraty R, Atkinson M. Cardiac coherence: A new, noninvasive measure of autonomic nervous system order. Altern Ther Health Med. 1996;2(1):52-65. [PubMed] [Google Scholar]
- 28.McCraty R, Atkinson M, Tiller WA, Rein G, Watkins AD. The effects of emotions on short-term power spectrum analysis of heart rate variability. Am J Cardiolog. 1995;76(14):1089-1093. [DOI] [PubMed] [Google Scholar]
- 29.Porges SW. The polyvagal perspective. Biol Psychol. 2007;74(2):116-143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Thayer JF, Hansen AL, Saus-Rose E, Johnsen BH. Heart rate variability, prefrontal neural function, and cognitive performance: The neurovisceral integration perspective on self-regulation, adaptation, and health. Annals Behav Med. 2009;37(2):141-153. [DOI] [PubMed] [Google Scholar]
- 31.Oppenheimer S, Hopkins D. Suprabulbar neuronal regulation of the heart. Neurocardiology. 1994:309-341. [Google Scholar]
- 32.McCraty R, Atkinson M, Tomasino D, Bradley RT. The coherent heart heartbrain interactions, psychophysiological coherence, and the emergence of system-wide order. Integral Rev. 2009;5(2):1 [Google Scholar]
- 33.Suzanne C, Segerstrom SC, Nes LC: Heart rate variability reflects self-regulatory strength,effort,and fatigue. Physiol Sci. 2007;18(3):275-281. [DOI] [PubMed] [Google Scholar]
- 34.Moodithaya S, Avadhany ST. Gender differences in age-related changes in cardiac autonomic nervous function. J Aging Research. 2012;2012:679345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Azam MA. The psychophysiology of maladaptive perfectionism and mindfulness meditation: An investigation using heart rate variability. Research Gate Web site. https://www.researchgate.net/publication/305083121_The_Psychophysiology_of_Maladaptive_Perfectionism_and_Mindfulness_Meditation. Published July 2015. Accessed September 25, 2018.
- 36.Vickhoff B, Malmgren H, Åström R, et al. Music structure determines heart rate variability of singers. Front Psychol. 2013;4:334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bernardi L, Sleight P, Bandinelli G, et al. Effect of rosary prayer and yoga mantras on autonomic cardiovascular rhythms: comparative study. BMJ. 2001;323(7327):1446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Deepak D, Sinha AN, Gusain VS, Goel A. A study on effects of meditation on sympathetic nervous system functional status in meditators. J Clin Diagnost Res. 2012;6(6):1. [Google Scholar]
- 39.Delgado-Pastor LC, Perakakis P, Subramanya P, Telles S, Vila J. Mindfulness (Vipassana) meditation: Effects on P3b event-related potential and heart rate variability. Int J Psychophysiol. 2013;90(2):207-214. [DOI] [PubMed] [Google Scholar]
- 40.Ferreira M, Jr, Zanesco A. Heart rate variability as important approach for assessment autonomic modulation. Motriz. 2016;22(2):3-8. [Google Scholar]
- 41.Friedman BH. An autonomic flexibility: Neurovisceral integration model of anxiety and cardiac vagal tone. Biologic Psychol. 2007;74(2):185-199. [DOI] [PubMed] [Google Scholar]


