Abstract
Background
The epidural dexmedetomidine combined with ropivacaine has been successfully used for labor analgesia. We compared the effects of dexmedetomidine and sufentanil as adjuvants to local anesthetic for epidural labor analgesia.
Methods
Eighty nulliparous women were enrolled in the double-blind study and randomly divided into two groups. Group D received 0.5 µg/mL dexmedetomidine with 0.1% ropivacaine for epidural labor analgesia, and group S (control group) received 0.5 µg/mL sufentanil with 0.1% ropivacaine for labor analgesia. Hemodynamic parameters were monitored. Pain was assessed using a visual analog scale. The onset of epidural analgesia, duration of stages of labor, Ramsay Sedation Scale, blood loss, neonatal Apgar scores, umbilical artery blood pH and adverse effects, such as respiratory depression, nausea, vomiting, pruritus, and bradycardia, were recorded.
Results
Compared with the control group, visual analog scale values after cervical dilation >3 cm were lower in group D (P<0.05) and first-stage labor duration was shorter in group D (378.5±52.6 vs 406.5±58.2, P<0.05). Ramsay Sedation Scale values were higher in group D compared to the control group (2.8±0.6 vs 2.4±0.5, P<0.05). No significant differences in side effects were observed between the groups.
Conclusion
Dexmedetomidine is superior to sufentanil in analgesic effect and duration in first-stage labor during epidural analgesia when combined with 0.1% ropivacaine (www.chictr.org.cn, registration ChiCTR-OPC-16008548).
Keywords: dexmedetomidine, sufentanil, epidural, analgesia, labor
Introduction
As an α2-adrenoceptor agonist, dexmedetomidine possesses anxiolytic, sedative, and analgesic properties without causing respiratory depression.1–3 Dexmedetomidine combined with ropivacaine has been successfully used for epidural labor analgesia, with fewer side effects.4,5 However, epidural local anesthetics combined with opioids are often accompanied by adverse effects, such as pruritus, nausea, and vomiting. The present study was designed to compare the effects of dexmedetomidine and sufentanil as adjuvants to local anesthetic for epidural labor analgesia.
Methods
This study was conducted in accordance with the Declaration of Helsinki and approved by the ethical committee of Jiaxing Women and Children’s Hospital (Chairman Professor L Xia) on April 16, 2016. Written informed consent was signed by the parturients. From August 2016 to December 2016, 80 nulliparous women with American Society of Anesthesiologists grade I–II, aged 20–35 years, weight 55–85 kg, and gestation ≥37 weeks were enrolled in this prospective, double-blind study. Patients with a history of severe cardiopulmonary disease, bradycardia, cervical dilatation >3 cm, contraindications to epidural analgesia, and undergoing cesarean section or labor induction were excluded from this study. Parturients were randomly divided into the control group (group S, n=40) and the dexmedeto-midine group (group D, n=40) using a computer-generated random-number table.
After entering the delivery room, parturients’ vital signs, such as blood pressure, heart rate, and SpO2, were monitored every 5 minutes, and fetal heart rate was also monitored using a Doppler fetal heart monitor. Venous access was established. Epidural analgesia was carried out when cervical dilatation was about 2 cm. Parturients were positioned in the left lateral decubitus position, and epidural puncture was performed at the estimated level of L2–3 interspace by an 18-gauge epidural needle using loss of resistance to air. An epidural catheter was inserted 3–4 cm cephaladly into the epidural space. After a negative aspiration test for blood and cerebrospinal fluid, a test dose of 3 mL 1% lidocaine was administered. Subsequently, parturients received 10 mL 0.5 µg/mL dexmedetomidine or 0.5 µg/mL sufentanil combined with 0.1% ropivacaine as loading dose, and this mixed solution was infused continuously by a patient-controlled-analgesia pump (Jiangsu Aipeng Medical Devices, China) at a rate of 6 mL/h. The women were instructed to use the pump for a bolus dose. A rescue bolus of 6 mL (lockout 20 minutes) was administered by the pump when visual analog scale (VAS) score was ≥5 (0= no pain, 10= maximum pain). Local-anesthetic solutions for epidural labor analgesia were prepared by another anesthetist, and investigators were blind to these solutions. Cervical dilatation progress was assessed by skilled midwives at intervals of 2 hours during the latent phase and every hour during the active phase.
Outcome measures and data collection
Blood pressure, heart rate, and SpO2 were monitored and recorded. Pain was evaluated with VAS. Onset of epidural analgesia, total analgesic consumption, duration of stages of labor, Ramsay Sedation Scale (RSS), blood loss, neonatal Apgar scores, and umbilical-artery blood gas were also noted. Onset of analgesia was defined as time from epidural administration to VAS <3, and duration of the first stage of labor was defined as time from epidural administration to 10 cm cervical dilatation. Blood loss was estimated by measuring the weight of medical gauze (1 kg approximately 1,000 mL).
Side effects, ie, hypotension, pruritus, sedation, nausea/vomiting, shivering, respiratory depression (hypoxemia), and maternal bradycardia, were also recorded and managed. The adverse effects were defined as: respiratory depression – SpO2 <90% when inhaling air; hypotension – systolic blood-pressure reduction >20% from baseline (before analgesia); maternal bradycardia – heart-rate reduction >20% from baseline (before analgesia); and fetal bradycardia – fetal heart rate <120 beats per minute.
Level of sedation was evaluated using the RSS (1, patient anxious, agitated, or restless; 2, patient cooperative, oriented, tranquil, and alert; 3, patient responds to commands; 4, asleep, but with brisk response to light glabellar tap or loud auditory stimulus; 5, asleep, sluggish response to light glabellar tap or loud auditory stimulus; 6, asleep, no response).6 RSS values were recorded every 60 minutes during labor. Excessive sedation was defined as RSS value >4.
Statistical analysis
As the primary outcome was the duration of the first stage and the secondary outcome the effects of analgesia, 36 samples were needed in each group at an α-error of 0.05 and power of 0.80 according to our pilot data. Analysis was performed with SPSS 17.0. Numerical variables are presented as mean ± SD. Categorical data are presented as numbers and percentages. Means were analyzed by Mann–Whitney U test and categorical data analyzed by χ2. P<0.05 was considered significant.
Results
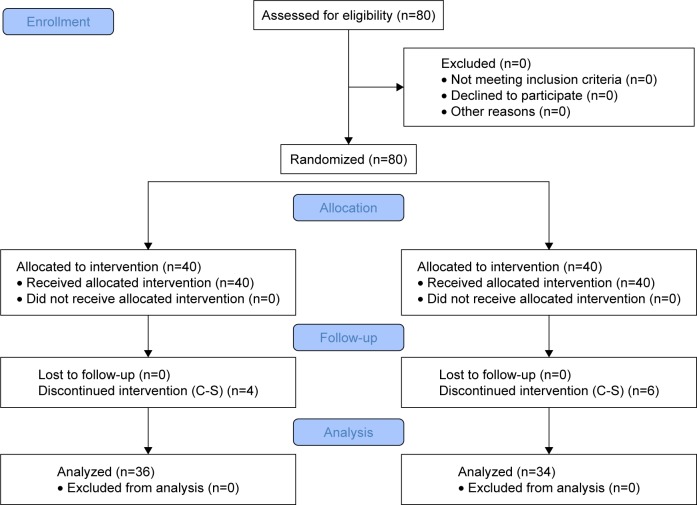
Eighty parturients were enrolled in this study (Figure 1). Ten women (four in group D and six in group S) were withdrawn from the study, as they had prolonged duration of first-stage labor (>12–16 hrs) and required cesarean section. There were no significant differences in age, weight, height, or gestational weeks between the groups (P>0.05, Table 1).
Figure 1.
Flow diagram of study.
Abbreviation: C-S, Cesarean section.
Table 1.
Data of parturients
| Group D (n=36) | Group S (n=34) | P-value | |
|---|---|---|---|
|
| |||
| Age (years) | 27.3±3.6 | 26.7±3.1 | 0.460 |
| Weight (kg) | 70.8±4.7 | 69.5±5.4 | 0.289 |
| Height (cm) | 159.3±2.9 | 160.4±3.2 | 0.225 |
| Gestational age (weeks) | 39.8±1.2 | 40.1±1.3 | 0.323 |
| Onset of analgesia (minutes) | 14.4±3.4 | 13.9±2.6 | 0.542 |
| Duration of first stage (minutes) | 378.5±52.6 | 406.5±58.2 | 0.042* |
| Duration of second stage (minutes) | 38.6±5.4 | 40.3±6.7 | 0.251 |
| Blood loss (mL) | 192.7±13.8 | 198.3±14.5 | 0.108 |
| Mode of delivery (vaginal/cesarean) | 36/4 | 34/6 | 0.653 |
| 1-minute Apgar score | 8.7±0.7 | 8.9±0.6 | 0.181 |
| 5-minute Apgar score | 9.6±0.5 | 9.7±0.7 | 0.496 |
| Umbilical artery pH | 7.22±0.06 | 7.23±0.07 | 0.504 |
| Umbilical artery PaO2 (mmHg) | 28.8±2.5 | 29.7±3.3 | 0.488 |
| Ramsay Sedation Scale | 2.8±0.6 | 2.4±0.5 | 0.002* |
| Total analgesics (mL) | 71.5±12.2 | 78.1±10.5 | 0.021* |
Notes:
P<0.05 compared with group S. Data presented as mean ± SD or numbers. Group D received 0.5 µg/mL dexmedetomidine with 0.1% ropivacaine for epidural labor analgesia, and group S (control group) received 0.5 µg/mL sufentanil with 0.1% ropivacaine for labor analgesia.
VAS values were lower in group D than group S when cervical dilation was >3 cm (Figure 2). There were significant differences in VAS values after cervical dilation >3 cm between the group D and group S, but no significant differences within 3 cm of cervical dilation. Moreover, total analgesic consumption was reduced in group D over group S, (71.5±12.2 vs 78.1±10.5, P<0.05). Duration of the first stage of labor was shorter in group D than group S (378.5±52.6 vs 406.5±58.2, P<0.05). RSS values in both groups were 1–3, with significant differences between the groups (2.8±0.6 vs 2.4±0.5, P<0.05), but no excessive sedation was observed. The incidence of hypotension, shivering, nausea, vomiting, hypoxemia, and bradycardia was similar in both groups. No pruritus or motor block was observed in group D, and there were no significant differences in side effects between the groups (Table 2).
Figure 2.
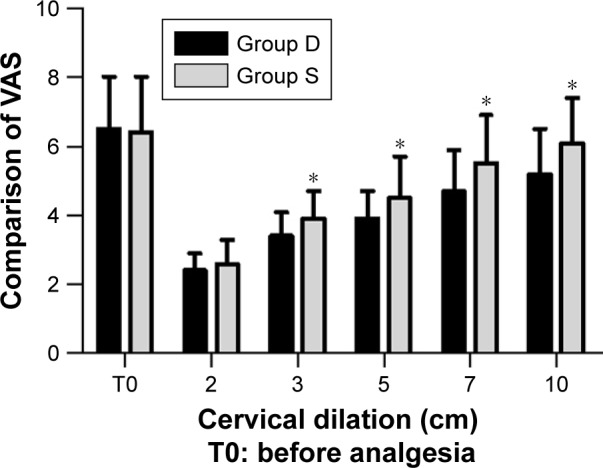
Comparison of visual analog scale (VAS) values at different cervical dilatations.
Notes: Group D received 0.5 µg/mL dexmedetomidine with 0.1% ropivacaine for epidural labor analgesia, and group S (control group) received 0.5 µg/mL sufentanil with 0.1% ropivacaine for labor analgesia. P<0.05.
Table 2.
Side effects of epidural analgesia
| Group D (n=36) | Group S (n=34) | P-value | |
|---|---|---|---|
|
| |||
| Hypotension | 0 | 0 | 1 |
| Pruritus | 0 | 1 (2.9%) | 0.131 |
| Nausea and vomiting | 1 (2.7%) | 3 (8.8%) | 0.122 |
| Maternal bradycardia | 0 | 0 | 1 |
| Fetal bradycardia | 3 (8.3%) | 2 (5.8%) | 0.506 |
| Respiratory depression | 0 | 0 | 1 |
| Shivering | 2 (5.5%) | 3 (8.8%) | 0.371 |
| Excessive sedation | 0 | 0 | 1 |
Notes: Data were presented as n (%). Group D received 0.5 µg/mL dexmedetomidine with 0.1% ropivacaine for epidural labor analgesia, and group S (control group) received 0.5 µg/mL sufentanil with 0.1% ropivacaine for labor analgesia.
Discussion
The ideal epidural analgesia should provide parturients with satisfactory analgesia without side effects for the mother or newborn, such as motor block, nausea, vomiting, pruritus, and fetal distress. In our study, we found that the analgesic effect of epidural dexmedetomidine was superior to sufentanil and duration of first-stage labor shortened during epidural labor analgesia when administered with 0.1% ropivacaine, with fewer side effects.
Ropivacaine combined with sufentanil has been used widely for epidural labor analgesia.7–9 In our study, we found that VAS values after cervical dilation >3 cm were significantly lower in group D than group S, and total analgesic consumption was reduced in group D. This indicated that adding dexmedetomidine to ropivacaine for labor analgesia provided better analgesic effect than sufentanil combined with ropivacaine. Dexmedetomidine possesses sedative and analgesic properties by activating α2 receptors in the spinal cord.10 Previous studies have reported that dexmedetomidine is a better adjuvant compared to fentanyl when added to ropivacaine in terms of providing prolonged analgesic effect and reducing total consumption of analgesia.11,12 These findings are in concordance with our results in this study. We also found that duration of first-stage labor was shortened when dexmedetomidine combined with 0.1% ropivacaine was used for labor analgesia. An in vitro study proved that dexmedetomidine has the potential to enhance the frequency of uterine contractions.13 As an α2-adrenoceptor agonist, dexmedetomidine can bring about contractions of uterus smooth muscles and fasten the duration of the first stage of labor. There was no significant difference with regard to SpO2 and motor block during labor. SpO2 values were >90% in group D, suggesting that epidural dexmedetomidine did not result in respiratory depression. RSS values were 1–3 in both groups during labor. There was a significant difference in RSS between the groups, but no excessive sedation was observed in this study. We found RSS values increased obviously in the dexmedetomidine group because dexmedetomidine produced sedative and analgesic effects by acting on α2-adrenergic receptors. Many studies have shown that RSS values with addition of dexmedetomidine to local anesthetic are greater compared to addition of fentanyl,11,12,14 and these findings are in good agreement with our results. Opioids are well known to cause side effects such as, pruritus, nausea, vomiting, and respiratory depression. Compared with opioids, dexmedetomidine did not cause pruritus and had fewer complications of nausea and vomiting during analgesia.15 Dexmedetomidine can be used safely for epidural labor analgesia.
Limitations
Dexmedetomidine is not licensed for epidural use by the US Food and Drug Administration. The effects of dexmedetomidine on mother and fetus need further study with larger-sample trials.16 In summary, dexmedetomidine is superior to sufentanil in terms of improved analgesic effect and short duration of the first stage of labor during epidural labor analgesia when administered with 0.1% ropivacaine.
Data sharing
The authors will share participant data, such as blood pressure, heart rate, and pain scores. No other study-related documents will be available. The data will be accessible 6 months after publication from http://www.sohu.com.
Acknowledgments
This work was supported by the Jiaxing Science and Technology Bureau Fund (2017AY3305071). We thank our colleagues for their help in this study.
Footnotes
Author contributions
All authors contributed to data analysis, drafting or revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Nie Y, Liu Y, Luo Q, Huang S. Effect of dexmedetomidine combined with sufentanil for post-caesarean section intravenous analgesia: a randomised, placebo-controlled study. Eur J Anaesthesiol. 2014;31(4):197–203. doi: 10.1097/EJA.0000000000000011. [DOI] [PubMed] [Google Scholar]
- 2.Hall JE, Uhrich TD, Barney JA, Arain SR, Ebert TJ. Sedative, anesthetic, and analgesic properties of small-dose dexmedetomidine infusions. Anesth Analog. 2000;90(3):699–705. doi: 10.1097/00000539-200003000-00035. [DOI] [PubMed] [Google Scholar]
- 3.Yousef AA, Salem HA, Moustafa MZ. Effect of mini-dose epidural dexmedetomidine in elective cesarean section using combined spinal-epidural anesthesia: a randomized double-blinded controlled study. J Anesth. 2015;29(5):708–714. doi: 10.1007/s00540-015-2027-7. [DOI] [PubMed] [Google Scholar]
- 4.Wangping Z, Ming R. Optimal dose of epidural dexmedetomidine added to ropivacaine for epidural labor analgesia: a pilot study. Evid Based Complement Alternat Med. 2017;2017:4. doi: 10.1155/2017/7924148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhao Y, Xin Y, Liu Y, Yi X, Liu Y. Effect of epidural dexmedetomidine combined with ropivacaine in labor analgesia: a randomized double-blinded controlled study. Clin J Pain. 2017;33(4):319–324. doi: 10.1097/AJP.0000000000000411. [DOI] [PubMed] [Google Scholar]
- 6.Ramsay MA, Savege TM, Simpson BR, Goodwin R. Controlled sedation with alphaxalone-alphadolone. Br Med J. 1974;2(5920):656–659. doi: 10.1136/bmj.2.5920.656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Beilin Y, Halpern S. Ropivacaine versus bupivacaine for epidural labor analgesia. Anesth Analog. 2010;111:482–487. doi: 10.1213/ANE.0b013e3181dd869b. [DOI] [PubMed] [Google Scholar]
- 8.Boulier V, Gomis P, Lautner C, Visseaux H, Palot M, Malinovsky JM. Minimum local analgesic concentrations of ropivacaine and levobupi-vacaine with sufentanil for epidural analgesia in labor. Int J Obstetric Anesth. 2009;18(3):226–230. doi: 10.1016/j.ijoa.2009.02.002. [DOI] [PubMed] [Google Scholar]
- 9.Benhamou D, Ghosh C, Mercier FJ. A randomized sequential allocation study to determine the minimum effective analgesic concentration of levobupivacaine and ropivacaine in patients receiving epidural analgesia for labor. Anesthesiology. 2003;99(6):1383–1386. doi: 10.1097/00000542-200312000-00022. [DOI] [PubMed] [Google Scholar]
- 10.Al-Mustafa MM, Badran IZ, Abu Ali HM, Al-Barazangi BA, Massad IM, Al-Ghanem SM. Intravenous dexmedetomidine prolongs bupivacaine spinal analgesia. Middle East J Anesthesiol. 2009;20(2):225–231. [PubMed] [Google Scholar]
- 11.Bajwa SJ, Arora V, Kaur J, Singh A, Parmar SS. Comparative evaluation of dexmedetomidine and fentanyl for epidural analgesia in lower limb orthopedic surgeries. Saudi J Anaesth. 2011;5(4):365–370. doi: 10.4103/1658-354X.87264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kiran S, Jinjil K, Tandon U, Kar S. Evaluation of dexmedetomidine and fentanyl as additives to ropivacaine for epidural anesthesia and postoperative analgesia. J Anaesthesiol Clin Pharmacol. 2018;34(1):41–45. doi: 10.4103/joacp.JOACP_205_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sia AT, Kwek K, Yeo GS. The in vitro effects of clonidine and dexmedetomidine on human myometrium. Int J Obstetric Anesth. 2005;14(2):104–107. doi: 10.1016/j.ijoa.2004.11.004. [DOI] [PubMed] [Google Scholar]
- 14.Zhang X, Wang D, Shi M, Luo Y. Efficacy and safety of dexmedetomidine as an adjuvant in epidural analgesia and anesthesia: a systematic review and meta-analysis of randomized controlled trials. Clin Drug Investig. 2017;37(4):343–354. doi: 10.1007/s40261-016-0477-9. [DOI] [PubMed] [Google Scholar]
- 15.Grewal A. Dexmedetomidine: GA. New avenues. J Anaesthesiol Clin Pharmacol. 2011;27:297–302. doi: 10.4103/0970-9185.83670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Konakci S, Adanir T, Yilmaz G, Rezanko T. The efficacy and neurotoxicity of dexmedetomidine administered via the epidural route. Eur J Anesthesiol. 2008;25(5):403–409. doi: 10.1017/S0265021507003079. [DOI] [PubMed] [Google Scholar]