Abstract
AIM
To assess and compare the impact of a daily disposable contact lens (CL) with high water content on the ocular surface and comfort of the presbyopic and non-presbyopic population after one day of use.
METHODS
Totally 20 presbyopes and 30 non-presbyopes non-contact wearers were fitted with nesofilcon A CLs. CL thickness was measured to assess material stability during daily wear, and ocular surface parameters were also assessed. Optical quality was analyzed for all cases. In addition, CL comfort was rated.
RESULTS
No significant differences were found in CL thickness, tear film osmolarity, average tear break-up time, bulbar redness, central corneal thickness, corneal volume, root-mean-square of higher-order aberrations (RMS of HOAs) and vertical and horizontal coma, either as a function of the group or time of use. A significant decrease in tear meniscus height and first break-up of the tear film was found in the presbyopic group (P=0.038; P=0.007 respectively). A decrease in spherical aberration coefficient was found after CL insertion (P=0.031 monofocal CL; P=0.023 low addition multifocal CL; P=0.016 high addition multifocal CL). Multifocal CL were thicker than monofocal CL (P=0.045). Comparison between groups showed more discomfort in presbyopes than non-presbyopes (P=0.003).
CONCLUSION
This study evidence that the behavior of the daily disposable CL with high water content seems to be stable during the day of use. Ocular parameters measured during wear show that CL behavior is the same for presbyopes and non-presbyopes, being more uncomfortable for presbyopes.
Keywords: nesofilcon A hydrogel material, ocular surface parameters, presbyopia, multifocal daily contact lenses
INTRODUCTION
Presbyopia affects people from the fifth decade of life on. With increasing longevity, most people can expect to spend almost half their lives as presbyopes. It has been reported that presbyopes prefer contact lens (CL) correction when good vision and comfort can be achieved[1]. However, although the number of presbyopes using CL has experienced significant growth in recent years, for various reasons, attempts to take advantage of this opportunity have so far enjoyed only limited success[2]–[5]. International surveys of CL prescribing for presbyopes reveal that CL fittings are much less frequent in older age groups. These data show that many CL wearers stop using their CLs at the onset of presbyopia.
Discomfort is one of the major issues related to CL wear dropout[6]. Numerous factors have been identified as having an impact on CL comfort, which can be classified into the CL itself (material, design, lens interaction) and environmental (inherent patients' factors, ocular environmental, external environmental)[6]. It is interesting to note that ocular changes reported as age-dependent such as a decreased number of meibomian glands, a decreased lacrimal production and tear stability may all influence the success of CL wear[7]. Despite these physiological differences between the older and younger population, CL materials, surface treatment, lens edge design etc. are the same for presbyopes and the younger population. Considering that: 1) the modality of CL interaction (material and design) with patients' inherent ocular surface characteristics is a key factor for comfort; 2) CL discomfort is one of the major issues related to CL wear dropout[6], it would be interesting to explore and compare CL and ocular surface interaction in the presbyopic and non-presbyopic populations.
A recent study[8] showed that a daily disposable soft hydrogel CL did not impact significantly on the tear film and minimized ocular complications in first-time young wearers.
The aim of this work was to assess and compare the interaction between a daily disposable CL and the ocular surface in a presbyopic and non-presbyopic population, and evaluate CL comfort after one day of use. Optical quality for two different additions for multifocal CLs was also compared while these lenses were being used.
SUBJECTS AND METHODS
Ethical Approval
The study protocol adhered to the tenets of the Declaration of Helsinki. Informed consent was obtained from all patients after the purpose and the possible consequences of the study had been explained to them.
This prospective study was carried out with a total sample of 50 eyes of 20 presbyopic subjects (12 females and 8 males with a mean age of 53.94±7.57y) and 30 non-presbyopic subjects (18 females and 12 males with a mean age of 27.00±5.97y). All of them were first-time wearers. Participants were free of any ocular pathology. Exclusion criteria included astigmatism over 0.75 D, ocular surface disease, systemic disease, history of ocular surgery or inflammation, and presenting systemic or ocular conditions.
Contact Lenses
The CL material evaluated in this study was nesofilcon A (Biotrue® ONEday, Bausch & Lomb, USA). This soft hydrogel lens is a conventional hydrogel called HyperGel. This material is a copolymer of HEMA and N-vinyl pyrrolidone with a water content of 78% and a modulus of 0.49 MPa. At the same time, the lens incorporates a UV filter. This lens presents a DK/t (@-3.00 D) of 42 with a total lens diameter of 14.2 mm and a back optic zone radius of 8.6 mm. Non-presbyopic participants were fitted with monofocal CL and presbyopes with multifocal CL (low add in one eye and high add in the other, randomly) without any refraction in order to avoid the impact of the different CL thickness due to different power refraction on the measurements. Multifocal CL has a center-near aspheric optics (3-Zone Progressive Design).
Measurements
Tear film osmolarity
Tear film osmolarity was measured using the TearLab Nanoliter osmometer (TearLab Corp, San Diego, CA, USA) in both eyes of each participant according to the manufacturer's instructions. It was done in first place in order to avoid reflex tearing.
Automated keratography
All participants underwent imaging with the Keratograph 5M® (K5M; Oculus GmbH, Wetzlar, Germany) equipped with a modified tear film scanning function. Three measurements of tear meniscus height, first break-up of the tear film, the average time of all tear film break-up incidents and bulbar redness were obtained automatically by Oculus K5M software according to the manufacturer's instructions.
Optical coherence tomography
All participants underwent imaging with an Optical Coherence Tomography Optovue® (OptovueInc, Fremont, USA) equipped with a scan speed of 26 000 A-scan/second and a depth resolution of 5 microns (µm). The device was used for measuring CL thickness variations.
Corneal measurements
Three measurements of corneal central thickness and corneal volume at 10 mm were obtained by a rotating Scheimpflug camera system for anterior segment analysis (Pentacam, Oculus GmbH, Wetzlar, Germany). Also, measurements of wavefront aberrations including the root-mean-square of higher-order aberrations (RMS of HOAs) and single high order coefficients Z(3, -1) (vertical coma), Z(3, 1) (horizontal coma) and Z(4, 0) (spherical aberration) were assessed in subjects when wearing the CLs. These aberration patterns were assessed for a pupil size of 4.5 mm.
Subjective comfort assessment
The visual analogue scale is a psychometric response scale, which can be used in questionnaires. It is a measurement instrument for subjective characteristics or attitudes that cannot be directly measured. When responding on a visual analogue scale item, respondents specify their level of agreement to a statement by indicating a position along a continuous line between two end-points. Patients were required to respond to the following points: A, comfort after 20min of CL wear (0, very uncomfortable to 10, very comfortable); B, comfort after 8h of CL wear (0, very uncomfortable to 10, very comfortable); C, dryness after 20min of CL wearing (0, no dryness to 10, extreme dryness) and D, dryness after 8h of CL wearing (0, little dryness to 10 high dryness).
Study Protocol
The clinical examinations were performed in the following order to minimize the effect of the previous measurement: tear film osmolarity (TearLab Corp, USA); tear meniscus height, bulbar redness, first break-up of the tear film and the average time of all tear film break-up incidents (Keratograph 5M, Oculus, Germany); CL thickness [Ocular coherence tomography; Optovue® (OptovueInc, USA)]; corneal central thickness, corneal volume at 10 mm and wavefront aberration values [RMS of HOAs, Z(3, -1), Z(3, 1) and Z(4, 0)] (Pentacam, Oculus, Germany). Finally, information about the level of satisfaction with the CL was obtained by the visual analogue scale questionnaire. A 5-minute interval between each test was established, and all tests were performed in the same order. All the measurements were performed by the same examiner.
Tear film osmolarity was measured before CL insertion (baseline) and after 20min and 8h of wear. CL thickness was measured after 20min and 8h of wear. Corneal central thickness and corneal volume were assessed before and after the lens was removed. The remaining measurements were taken before CL insertion, after 20min and 8h of wear and after the lens was removed. With the exception of osmolarity, each parameter was measured three times per eye and per device.
Changes in the cornea or in the CL after one day of use could induce changes in the optical quality of the eye-lens system. For this reason, variations in wavefront aberrations of the patients were assessed and compared when wearing the CL under analysis (monofocal CL, multifocal CL low addition and multifocal CL high addition).
For the comparison between presbyopes and non-presbyopes, only one eye of each patient was considered in random order.
Data Analysis
Statistical analyses were performed using SAS software, version 9.4 (SAS Institute, Inc., Cary, NC, USA). Normality of the data distribution was tested using the Kolmogorov-Smirnov test. The ANOVA test and Kruskal-Wallis test were used for comparisons between groups. When statistically significant differences were found, post hoc tests were performed for multiple comparisons (Tukey's HSD). Values are expressed as mean±standard deviation (SD) and the significance level was set at P<0.05.
RESULTS
Tables 1 and 2 provide descriptive statistics for tear film osmolarity (measured at baseline, 20min and 8h after CL wear), tear meniscus height, bulbar redness, first break-up of the tear film and the average time of all tear film break-up incidents (measured at baseline, 20min, 8h after CL wear and after CL removal) for non-presbyopes and presbyopes, respectively. In non-presbyopes, no differences were found for any of the ocular parameters analyzed as a factor of time (Table 1). In presbyopes, tear film osmolarity, bulbar redness and the average time of all tear film break-up incidents were not found to be significantly different as a factor of time. First break-up of the tear film and tear meniscus height measurements were found to be significantly different (P=0.038; P=0.007 respectively). Post hoc comparisons between each of the time points revealed significant decrease for first break-up of the tear film between baseline and 8h after CL wear and 20min and 8h after CL wear (P=0.034; P=0.029, respectively). The same analysis revealed a significant decrease for tear meniscus height between baseline and 20min and baseline and 8h of CL wear (P=0.02; P=0.014, respectively).
Table 1. Descriptive statistics for clinical parameters obtained for non-presbyopes.
| Parameters | Baseline | 20min after CL wear | 8h after CL wear | After removal |
| Tear film osmolarity (mOsms/L) | 298.67±5.48 | 294.08±9.38 | 297.92±9.57 | |
| Tear meniscus height (mm) | 0.186±0.045 | 0.179±0.023 | 0.156±0.156 | 0.182±0.052 |
| Bulbar redness (score) | 0.85±0.30 | 0.76±0.21 | 0.92±0.37 | 1.06±0.43 |
| First break-up tear film (s) | 7.56±5.52 | 4.62±2.02 | 5.70±2.13 | 8.33±5.31 |
| Average break-up tear film (s) | 9.39±6.08 | 9.27±3.90 | 9.78±3.22 | 9.88±5.36 |
mean±SD
Table 2. Descriptive statistics for clinical parameters obtained for presbyopes.
| Parameters | Baseline | 20min after CL wear | 8h after CL wear | After removal |
| Tear film osmolarity (mOsms/L) | 312.41±12.52 | 309.00±7.75 | 312.59±12.28 | |
| Tear meniscus height (mm) | 0.371±0.171 | 0.254±0.083a | 0.249±0.089b | 0.369±0.180 |
| Bulbar redness (score) | 0.92±0.26 | 0.98±0.27 | 1.03±0.33 | 1.16±0.35 |
| First break-up tear film (s) | 8.50±5.13 | 9.29±3.67c | 6.54±2.83b | 10.31±5.13 |
| Average break-up tear film (s) | 13.80±5.04 | 14.95±3.65 | 12.92±3.85 | 11.15±4.50 |
aStatistically significant differences between baseline and 20min; bStatistically significant differences between baseline and 8h of use; cStatistically significant differences between 20min and 8h of use.
mean±SD
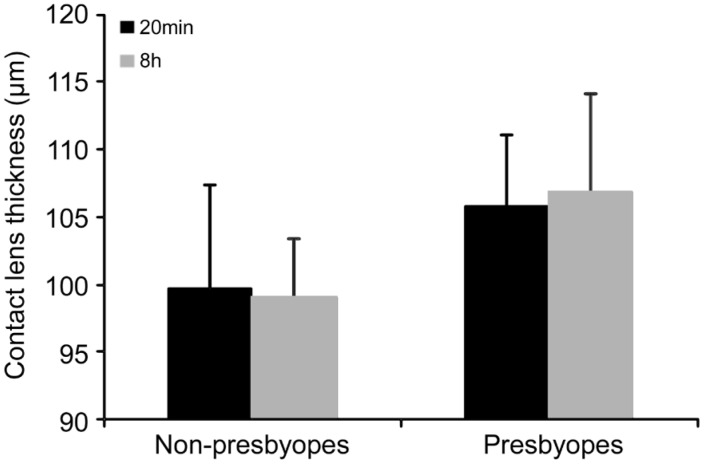
Figure 1 shows central CL thickness values measured 20min and 8h after lens insertion. The thickness of the lens did not change as a factor of time in any group (P=0.321 non-presbyopes; P=0.356 presbyopes). Multifocal lens was thicker than monofocal lens (P=0.045 at 20min; P=0.006 at 8h).
Figure 1. CL thickness values expressed in microns (µm) for presbyopes and non-presbyopes.
This parameter was measured 20min and 8h after CL insertion.
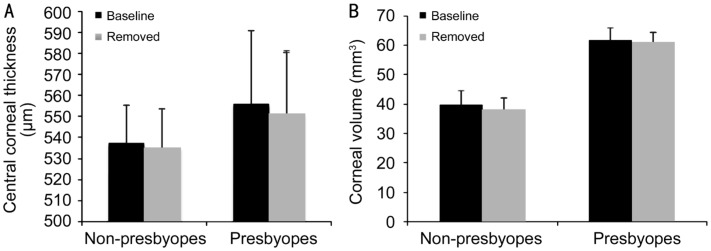
Figure 2 shows data from central corneal thickness (Figure 2A) and corneal volume (Figure 2B) for non-presbyopes and presbyopes at baseline and after CL was removed. No changes were found as a factor of the time in any of the groups analyzed.
Figure 2. Central corneal thickness (A) and corneal volume (B) for non-presbyopes and presbyopes measured before CL insertion and after the lens was removed.
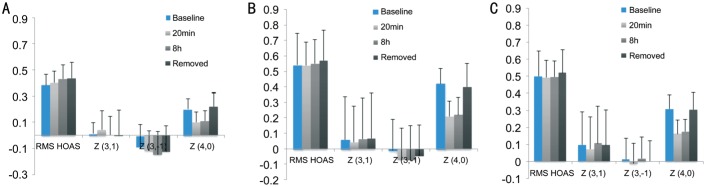
Wavefront aberrations were analyzed in order to assess the optical quality of the ocular surface. Figure 3 shows the results obtained for RMS of HOAs, horizontal and vertical coma, and spherical aberrations for each of the CL analyzed. Analysis of the results revealed no significant variations in the RMS of HOAs, horizontal and vertical coma for any of the lenses as a factor of time. Spherical aberration decreased significantly after CL insertion (P=0.031 monofocal CL; P=0.023 low addition multifocal CL; P=0.016 high addition multifocal CL) and kept stable during wear for all lenses. After removal, previous spherical aberration values were achieved for the three CLs.
Figure 3. Wavefront aberration values: RMS of HOAs, vertical coma [Z(3, -1)], horizontal coma [Z(3, 1)] and spherical aberration [Z(4, 0)] for the eye-lens system.
Optical quality parameters were measured at four different times: before insertion of the lens, 20min, and 8h after wearing and, finally, when the lens was removed for the CLs studied: monofocal CL (A), multifocal CL high addition (B) and multifocal CL low addition (C). Data from wavefront aberration values is measured in micron.
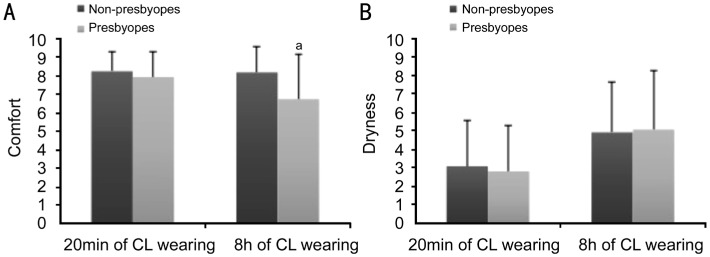
Figure 4 shows the results obtained for the visual analogue scale questionnaire for comfort (Figure 4A) and dryness (Figure 4B) for non-presbyopes and presbyopes. Statistically significant differences were found in dryness during CL wear for both groups (P=0.020; P=0.015 respectively). Comparison between both questionnaire results were statistically different (P=0.002). Post hoc comparisons revealed a significant decrease in comfort after 8h of CL wear for presbyopes (P=0.003).
Figure 4. Comparison between results of the questionnaire for non-presbyopes and presbyopes.
The results found for comfort (A) and dryness (B). aStatistically significant differences between both groups, P<0.05.
DISCUSSION
It is very well known that CL prescribing is much less frequent for the presbyopic population. Considering that discomfort is one of the major issues related to CL wear dropout[6], in the present study, the interaction between CL and ocular surface of a daily disposable CL on a group of presbyopes was analyzed, as well as the comfort during a day of use.
Nesofilcon A was the material selected for this study. It is a new material developed with the aim of reducing discontinuation rates as it is made with high water content and an internal surfactant that prevents dehydration. It has been proven[8] not to significantly impact the tear film layer and ocular surface when this CL was fitted in a younger population. Since the same material is used to manufacture center-near aspheric multifocal CLs for presbyopes, this study was performed to analyze the integrity of the ocular surface when this multifocal CL was fitted in a presbyopic population for one day of use.
An increased tear film osmolarity has been related to the pathophysiology of dry eye disease[9] and several studies maintain the usefulness of tear film osmolarity for diagnosis and severity grading[9]. It is widely reported that CL use could induce dryness symptoms, while various studies have related CL use to low or moderate variations in tear osmolarity[10]–[11]. This is why tear film osmolarity changes were analyzed at baseline, 20min and 8h after insertion fitting. It should be noted that the achieved results showed no differences in tear osmolarity for any of the two lenses as a function of time, suggesting that these daily disposable CLs may not induce changes in the ocular surface during one day of wearing, and do not impact homeostasis significantly. This result agrees with the study performed by Ruíz-Alcocer et al[8] with a younger population. On the other hand, it is interesting to note that the tear film osmolarity in the presbyopic group was higher than in non-presbyopes. Although this parameter was stable during CL use, this finding highlights the fact that the ocular surface integrity in presbyopes is different from that in younger people. It could explain why the interaction between the CL material and comfort could be different in young and presbyopic people.
For both groups, a reduction in the tear meniscus height was found after CL insertion (not significantly for non-presbyopes). This result agrees with previous studies, which found a tear meniscus height decrease after CL insertion, especially with high water content CL[12]. This fact can be explained because in the normal tear system, the tear drainage system maintains a dynamic balance so that the tear volume sustains a relatively steady state and keeps the ocular surface wet[13]. Palakuru et al[14]–[15] have reported that the lower tear meniscus may regulate the tear drainage system. It may be possible that an increase in tear secretion by the lacrimal gland, contributing to the increase of tear meniscus height, could compensate for dehydration or increased evaporation with CL wear. However, the decrease in corneal sensitivity with CL wear[16] may lead to a reduction in tear secretion through the reflex sensory loop[17]. Therefore, even when greater evaporation occurs with high water content CL wear in the setting of a dehydrated surface, a decrease in corneal sensitivity can result in a decrease of tear meniscus height. Furthermore, a reduction in the amount of tear meniscus that could be related to discomfort has been suggested by some authors[18]. In the present study, reductions in tear meniscus height after 20min and 8h of use were found in multifocal CL while tear meniscus height in monofocal CL group seemed to be stable. These findings agree with Del Águila-Carrasco et al[18] results so the reduction in tear meniscus height can be associated with discomfort in patients fitted with multifocal CLs as discussed later. Other types of material with different water content, thickness or composition such as silicone hydrogel could affect the cornea differently, improving the comfort in the presbyopic population.
In the present study, corneal volume remained stable during the period of study. Only a slight increase (not significant) was observed for monofocal and multifocal CL during wear. These results agree with other studies[18] performed with monofocal CL and different materials.
Despite the findings showing no significant increase in bulbar redness related to time or group after one day of use, nesofilcon A might affect the ocular surface as some studies have found an increase in bulbar redness after two months of CL wear[19].
A previous study[20] showed that break-up of the tear film measurements can be used as an interesting tool in the assessment of pre-corneal and pre-lens tear film quality for prescribing CLs. For this reason, measurements of the first and mean break-up of the tear film for presbyopes and non-presbyopes were taken. In the present study, no differences before CL insertion were found in these values between both groups. Also, average time of all tear film breakup remained stable during the day of use for both groups. Post hoc comparisons for first break-up of the tear film revealed a significant decrease between baseline and 8h after CL wear and 20min and 8h after CL wear (P=0.034; P=0.029, respectively) for the presbyopic population. After CL removal, previous values in first break-up of the tear film were recovered.
Regarding CL behavior during wear, the thickness of soft CL can vary during one day of use due to dehydration or interaction with the tear film. In the present study, no changes in CL thickness were found for any CL or time of use. A recent study[21] evaluated the surface water characteristics of nesofilcon A and other CL materials. In relation to nesofilcon A, the authors concluded that nesofilcon A maintained its water content both at the time of insertion and after 15min of wear. This could explain why the lens made with nesofilcon A maintained its thickness after 20min and 8h of use. Future studies could analyze dehydration to see if lens thickness remains stable over a longer period with monofocal and multifocal CL.
In this regard, the results show that multifocal CLs are thicker than monofocal CL (Figure 2). This change in the CL thickness could affect the central corneal thickness during wear[22]. However, no changes in central corneal thickness were found during the period of study for any of the CLs studied. These results agree with the study by Ruíz-Alcocer et al[8] in monofocal CLs. So, the central lens thickness difference between lenses was not enough to affect the central corneal thickness during the wear of any of the CL considered. Therefore, it could suggest that the material allows sufficient oxygen to the cornea to avoid complications such as corneal swelling during the period of study regardless of the design of CLs.
In this study, no statistically significant variations were noted for coma-like and RMS of HOAs at any time for each of CLs considered. Spherical aberration decreased significantly after CL insertion for the three CLs (P=0.031 monofocal CL; P=0.023 low addition multifocal CL; P=0.016 high addition multifocal CL) and remained stable during wear for all lenses. These results are expected due to the design of each CL[23]–[26]. After removal, previous spherical aberration values were achieved for the three CLs. If an increase in optical aberrations had been found, blurred vision associated with tear film instability would have manifested[27]–[29]. Thus, these lenses seem to maintain tear film optical quality after 8h of wear regardless of the design of CLs fitted and the addition chosen for the multifocal CL.
It has been proved[1] that one of the most important facts that affect multifocal CL wear is comfort. In the present study, the level of comfort of the CL was measured with the visual analogue scale. Presbyopes reported lower comfort than non-presbyopes (Figure 4). This loss of comfort can affect the CL dropout[6],[30] in presbyopic patients. Ocular surface differences between non-presbyopic and presbyopic patients as a recent study by Rico-del-Viejo et al[7] suggests and the difference in CL thickness between monofocal and multifocal CLs manufactured with the same material seem to be the most important factors explaining this situation.
In conclusion, the behaviour of daily disposable CL made with nesofilcon A hydrogel seemed to be stable during the day of use. The ocular parameters measured during the wearing showed that CL behavior was the same for presbyopes and non-presbyopes, being more uncomfortable for presbyopes. Future studies should be directed on the use of new materials that take into account the differences in the ocular surface between presbyopes and non-presbyopes.
Acknowledgments
Conflicts of Interest: Lorente-Velázquez A, None; García-Montero M, None; Gómez-Sanz FJ, None; Rico del Viejo L, None; Hernández-Verdejo JL, None; Madrid-Costa D, None.
REFERENCES
- 1.Rueff EM, Bailey MD. Presbyopic and non-presbyopic contact lens opinions and vision correction preferences. Cont Lens Anterior Eye. 2017;40(5):323–328. doi: 10.1016/j.clae.2017.03.010. [DOI] [PubMed] [Google Scholar]
- 2.Morgan PB, Efron N. Contact lens correction of presbyopia. Cont Lens Anterior Eye. 2009;32(4):191–192. doi: 10.1016/j.clae.2009.05.003. [DOI] [PubMed] [Google Scholar]
- 3.Morgan PB, Efron N, Woods CA, International Contact Lens Prescribing Survey Consortium An international survey of contact lens prescribing for presbyopia. Clin Exp Optom. 2011;94(1):87–92. doi: 10.1111/j.1444-0938.2010.00524.x. [DOI] [PubMed] [Google Scholar]
- 4.Morgan PB, Woods CA, Tranoudis, et al. International contact lens prescribing in 2016. Contact Lens Spectrum. 2017;32:30–35. [Google Scholar]
- 5.Pérez-Prados R, Piñero DP, Pérez-Cambrodí RJ, Madrid-Costa D. Soft multifocal simultaneous image contact lenses: a review. Clin Exp Optom. 2017;100(2):107–127. doi: 10.1111/cxo.12488. [DOI] [PubMed] [Google Scholar]
- 6.Nichols KK, Redfern RL, Jacob JT, Nelson JD, Fonn D, Forstot SL, Huang JF, Holden BA, Nichols JJ. The TFOS international workshop on contact lens discomfort: report of the definition and classification subcommittee. Invest Ophthalmol Vis Sci. 2013;54(11):TFOS14. doi: 10.1167/iovs.13-13074. [DOI] [PubMed] [Google Scholar]
- 7.Rico-Del-Viejo L, Lorente-Velázquez A, Hernández-Verdejo JL, García-Mata R, Benítez-Del-Castillo JM, Madrid-Costa D. The effect of ageing on the ocular surface parameters. Cont Lens Anterior Eye. 2018;41(1):5–12. doi: 10.1016/j.clae.2017.09.015. [DOI] [PubMed] [Google Scholar]
- 8.Ruiz-Alcocer J, Monsálvez-Romín D, García-Lázaro S, Albarrán-Diego C, Hernández-Verdejo JL, Madrid-Costa D. Impact of contact lens material and design on the ocular surface. Clin Exp Optom. 2018;101(2):188–192. doi: 10.1111/cxo.12622. [DOI] [PubMed] [Google Scholar]
- 9.Potvin R, Makari S, Rapuano CJ. Tear film osmolarity and dry eye disease: a review of the literature. Clin Ophthalmol. 2015;9:2039–2047. doi: 10.2147/OPTH.S95242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nichols JJ, Sinnott LT. Tear film, contact lens, and patient-related factors associated with contact lens-related dry eye. Invest Ophthalmol Vis Sci. 2006;47(4):1319–1328. doi: 10.1167/iovs.05-1392. [DOI] [PubMed] [Google Scholar]
- 11.Miller WL, Doughty MJ, Narayanan S, Leach NE, Tran A, Gaume AL, Bergmanson JP. A comparison of tear volume (by tear meniscus height and phenol red thread test) and tear fluid osmolality measures in non-lens wearers and in contact lens wearers. Eye Contact Lens. 2004;30(3):132–137. doi: 10.1097/01.icl.0000138714.96401.2b. [DOI] [PubMed] [Google Scholar]
- 12.Nagahara Y, Koh S, Maeda N, Nishida K, Watanabe H. Prominent decrease of tear meniscus height with contact lens wear and efficacy of eye drop instillation. Eye Contact Lens. 2015;41(5):318–322. doi: 10.1097/ICL.0000000000000134. [DOI] [PubMed] [Google Scholar]
- 13.Craig JP, Willcox MD, Argüeso P, Maissa C, Stahl U, Tomlinson A, Wang JH, Yokoi N, Stapleton F, members of TFOS International Workshop on Contact Lens Discomfort The TFOS International Workshop on Contact Lens Discomfort: report of the contact lens interactions with the tear film subcommittee. Invest Ophthalmol Vis Sci. 2013;54(11):TFOS123–TFOS156. doi: 10.1167/iovs.13-13235. [DOI] [PubMed] [Google Scholar]
- 14.Palakuru JR, Wang JH, Aquavella JV. Effect of blinking on tear dynamics. Invest Ophthalmol Vis Sci. 2007;48(7):3032–3037. doi: 10.1167/iovs.06-1507. [DOI] [PubMed] [Google Scholar]
- 15.Palakuru JR, Wang JH, Aquavella JV. Effect of blinking on tear volume after instillation of midviscosity artificial tears. Am J Ophthalmol. 2008;146(6):920–924. doi: 10.1016/j.ajo.2008.06.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lowther GE, Hill RM. Sensitivity threshold of the lower lid margin in the course of adaptation to contact lenses. Am J Optom Arch Am Acad Optom. 1968;45(9):587–594. doi: 10.1097/00006324-196809000-00003. [DOI] [PubMed] [Google Scholar]
- 17.Stern ME, Beuerman RW, Fox RI, Gao J, Mircheff AK, Pflugfelder SC. The pathology of dry eye: the interaction between the ocular surface and lacrimal glands. Cornea. 1998;17(6):584–589. doi: 10.1097/00003226-199811000-00002. [DOI] [PubMed] [Google Scholar]
- 18.Del Águila-Carrasco AJ, Ferrer-Blasco T, García-Lázaro S, Esteve-Taboada JJ, Montés-Micó R. Assessment of corneal thickness and tear meniscus during contact-lens wear. Cont Lens Anterior Eye. 2015;38(3):185–193. doi: 10.1016/j.clae.2015.01.010. [DOI] [PubMed] [Google Scholar]
- 19.Sapkota K, Franco S, Lira M. Daily versus monthly disposable contact lens: Which is better for ocular surface physiology and comfort? Cont Lens Anterior Eye. 2018;41(3):252–257. doi: 10.1016/j.clae.2017.12.005. [DOI] [PubMed] [Google Scholar]
- 20.Mousavi M, Jesus DA, Garaszczuk IK, Szczesna-Iskander DH, Iskander DR. The utility of measuring tear film break-up time for prescribing contact lenses. Cont Lens Anterior Eye. 2018;41(1):105–109. doi: 10.1016/j.clae.2017.08.003. [DOI] [PubMed] [Google Scholar]
- 21.Schafer J, Steffen R, Reindel W, Chinn J. Evaluation of surface water characteristics of novel daily disposable contact lens materials, using refractive index shifts after wear. Clin Ophthalmol. 2015;9:1973–1979. doi: 10.2147/OPTH.S90376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chao C, Richdale K, Jalbert I, Doung K, Gokhale M. Non-invasive objective and contemporary methods for measuring ocular surface inflammation in soft contact lens wearers-a review. Cont Lens Anterior Eye. 2017;40(5):273–282. doi: 10.1016/j.clae.2017.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Madrid-Costa D, Ruiz-Alcocer J, García-Lázaro S, Ferrer-Blasco T, Montés-Micó R. Optical power distribution of refractive and aspheric multifocal contact lenses: effect of pupil size. Cont Lens Anterior Eye. 2015;38(5):317–321. doi: 10.1016/j.clae.2015.03.008. [DOI] [PubMed] [Google Scholar]
- 24.Wagner S, Conrad F, Bakaraju RC, Fedtke C, Ehrmann K, Holden BA. Power profiles of single vision and multifocal soft contact lenses. Cont Lens Anterior Eye. 2015;38(1):2–14. doi: 10.1016/j.clae.2014.07.008. [DOI] [PubMed] [Google Scholar]
- 25.Papadatou E, Del Águila-Carrasco AJ, Esteve-Taboada JJ, Madrid-Costa D, Cerviño-Expósito A. Objective assessment of the effect of pupil size upon the power distribution of multifocal contact lenses. Int J Ophthalmol. 2017;10(1):103–108. doi: 10.18240/ijo.2017.01.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Plainis S, Atchison DA, Charman WN. Power profiles of multifocal contact lenses and their interpretation. Optom Vis Sci. 2013;90(10):1066–1077. doi: 10.1097/OPX.0000000000000030. [DOI] [PubMed] [Google Scholar]
- 27.Liu HX, Thibos L, Begley CG, Bradley A. Measurement of the time course of optical quality and visual deterioration during tear break-up. Invest Ophthalmol Vis Sci. 2010;51(6):3318–3326. doi: 10.1167/iovs.09-4831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Montés-Micó R, Cerviño A, Ferrer-Blasco T, García-Lázaro S, Madrid-Costa D. The tear film and the optical quality of the eye. Ocul Surf. 2010;8(4):185–192. doi: 10.1016/s1542-0124(12)70233-1. [DOI] [PubMed] [Google Scholar]
- 29.Denoyer A, Rabut G, Baudouin C. Tear film aberration dynamics and vision-related quality of life in patients with dry eye disease. Ophthalmology. 2012;119(9):1811–1818. doi: 10.1016/j.ophtha.2012.03.004. [DOI] [PubMed] [Google Scholar]
- 30.Richdale K, Sinnott LT, Skadahl E, Nichols JJ. Frequency of and factors associated with contact lens dissatisfaction and discontinuation. Cornea. 2007;26(2):168–174. doi: 10.1097/01.ico.0000248382.32143.86. [DOI] [PubMed] [Google Scholar]