Abstract
Antimicrobial resistance happens when microorganisms mutates in manners that render the drugs like antibacterial, antiviral, antiparasitic and antifungal, ineffective. The normal mutation process is encouraged by the improper use of antibiotics. Mutations leading to quinolone resistance occur in a highly conserved region of the quinolone resistance-determining region (QRDR) of DNA gyrAse and topoisomerase IV gene. We analyzed antibiotic resistant genes and single nucleotide polymorphism (SNP) in gyrA and parC genes in QRDR in 120 E. coli isolates (both diarrheagenic and non-pathogenic) recovered from fresh stool samples collected from children aged less than 5 years from Delhi, India. Antibiotic susceptibility testing was performed according to standard clinical and laboratory standards institute (CLSI) guidelines. Phylogenetic analysis showed the clonal diversity and phylogenetic relationships among the E. coli isolates. The SNP analysis depicted mutations in gyrA and parC genes in QRDR. The sul1 gene, responsible for sulfonamide resistance, was present in almost half (47.5%) of the isolates across the diseased and healthy samples. The presence of antibiotic resistance genes in E. coli isolates from healthy children indicate the development, dissemination and carriage of antibiotic resistance in their gut. Our observations suggest the implementation of active surveillance and stewardship programs to promote appropriate antibiotic use and minimizing further danger.
Introduction
Childhood diarrhoea, a major cause of child mortality globally, affects an estimated 2.2 million children in developing countries alone [1]. Antimicrobial drugs have played an important role in reducing death toll caused by infectious diseases. However, infections caused by multidrug-resistant (MDR) organisms have emerged as a huge threat to the community and hospitalized patients. In this regard the emergence of MDR E. coli isolates from human, animal and environmental sources have posed a major concern worldwide [2, 3].
Study of antimicrobial resistance and regional variation is vital for the development and implementation of interventional strategies. E. coli, though a commensal, has acquired resistance to various groups of antimicrobials at a rapid rate in diverse geographical areas, emphasizing the need of antimicrobial resistance (AMR) surveillance, especially in low resource settings where the cost of patient management escalates once hospitalized and colonized by drug resistant microbes. Early studies suggest that E. coli isolates recovered from the stools of healthy children have significantly higher rates of multi-drug resistances in China in comparison to the developed countries [4]. Similar observation in rest of Asia and South America, thus accentuate the threat of widespread drug resistance and the urgent need of implementation of future preventive measures and planning strict policy of antibiotic usage [5]. Moreover, co-evolution of virulence factors with antibiotic resistance genes have eventually contributed to the adaptive potential of these resistant microbes and long-term survival [6, 7].
Interestingly, existence of antibiotic resistance has started from the era of penicillin discovery, prompting the start of a national surveillance program namely ‘Resistance Map’ (www.resistancemap.org) demonstrating the occurrence of resistance two decades back involving India and China as the main contributors [8–10]; {Figure A to D in S1 Fig}. In India, very high resistance was reported against ampicillin and nalidixic acid along with an increased resistance to third generation cephalosporins, fluoroquinolone and carbapenems in E. coli [11].
Mobile genetic elements like integrons contain many antibiotic resistance determinants in E. coli. Integrons can also be defined as the systems for site-specific recombination found in transposons, plasmids and chromosomes [12]. Gene cassettes with multiple antibiotic resistance genes in the form of clusters can be found in integrons which contribute majorly to the development of multiple antibiotic resistances [13].
The rapid spread of β-lactamases resistance, led by mobile genetic elements, amongst susceptible bacteria and acquisition of plasmid-mediated β-lactamases such as extended-spectrum β-lactamases–ESBL (TEM, SHV, CTX-M and OXA), and class C plasmid-mediated AmpC β-lactamases–ABL (ACT, CMY and DHA) amongst E. coli are well documented [14–16]. Metallo-β-lactamases—MBL (VIM, IMP and the recent NDM), have further led to limitations in the treatment options [17]. ESBL producers are no longer associated with hospital infections only rather community acquired isolates are now adding to burden of drug resistance [18]. Phenotypic methods have poor detection performance; consequently rampant misidentification of the drug resistant genes have led to the current disastrous therapeutic failure in life threatening infections [19, 20].
Genetic elements involving sul1, sul2 and sul3 genes [21–26] and tetA (A), tetB (B), tetC (A), tetD (A), tetE (A) and tetG (A) genes are other important targets conferring resistance to Sulphonamides and Tetracyclines respectively [27, 28]; and mutations in the quinolone resistance-determining region (QRDR) of gyrA or gyrB subunits of DNA gyrAse and parC genes or parE subunits of topoisomerase IV for fluoroquinolones resistance have also been described in several infections leading to treatment collapse [29–39]. Further, alterations in drug targets causing decreased cellular accumulation of quinolones and accompanied major multidrug efflux pump, AcrAB, may be contributing further to fluoroquinolone resistance [40–46].
The E. coli populations categorized into eight major phylogenetic groups namely A, B1, B2, C, D, E, F (belonging to E. coli sensustricto) and clade I (belonging to Escherichia clade) [47] have a vast genetic substructure within the species.
In view of the recent progression of antibiotic resistance in children under five, not only in clinical but also in community settings; we carried out this study to find the prevalence of different antibiotic resistance genes, to analyze point mutation in QRDR of fluoroquinolones and to detect the distribution of these resistance genes in different phylogroups.
Materials and methods
Study design
During the study period (July 2013 to July 2015), a total of 120 stool samples were collected from children up to five years of age. Each group included 40 subjects and were categorized as diarrhoeal (O), non-diarrhoeal (I) and healthy (C). The subjects were provided with relevant information about the study and were included with written informed consent from their parents/guardians. The study was approved by the Institutional Ethics Committee for Human Research (IEC-HR) of the University College of Medical Sciences (University of Delhi), Delhi and was carried out in accordance with its recommendations.
Sample collection and processing
Conventional biochemical tests were used to identify the recovered E. coli [48] before performing the PCR for the 16SrRNA gene, which was also used as an internal quality control [49]. Antibiotic resistance was determined by the agar diffusion method (Kirby-Bauer method) using 16 antibiotics (HiMedia Laboratories, Mumbai, India) under four different classes namely aminoglycosides, fluoroquinolones, β-lactams and quinolones. The E. coli isolates were classified as sensitive or resistant according to CLSI guidelines at 24 hours of incubation at 37°C [48, 50, 51].
DNA extraction, primers and analysis
DNA was extracted using the commercial kit (Real Biotech Corporation, Taiwan) and conventional PCR was performed for identification of genes associated with antibiotic resistance, single nucleotide polymorphism (SNP) and phylogenetic groups. Primers used are described in Table 1 [22,35,36,49,52–58].
Table 1. Details of the primers used.
| Multiplex PCR | Gene | Primer sequence (5’–3’) | PCR product (bp) | Annealing temperature (°C) | Reference |
|---|---|---|---|---|---|
| Aminoglycoside adenylyl transferases | AadA (aadA1 or aadA2) |
GCTCTTCAGCAATATCACGG GCAGCGCAATGACATTCTTG |
282 | 60 | [52] |
| SNP Detection | |||||
| DNA gyrase | GyrA |
CTCCTCCCAGACCAAAGACA TCACGACCGATACCACAGCC- |
447 | 60 | [35, 36] |
| DNA topoisomerase IV | ParC |
AAACCTGTTCAGCGCCGCATT GTGGTGCCGTTAAGCAAA |
395 | 54 | [35, 36] |
| Antibiotic Resistance Genes | |||||
| Tetracycline |
TetA-F TetA-R |
GTAATTCTGAGCACTGTCGC CTGCCTGGACAACATTGCTT |
937 | 62 | [53] |
| Sulphonamides |
Sul1-F Sul2-R |
TGGTGACGGTGTTCGGCATTC GCGAGGGTTTCCGAGAAGGTG |
789 | 63 | [22] |
| Gentamicin |
AacC1-F AacC1-R |
ACCTACTCCCAACATCAGCC ATATAGATCTCACTACGCGC |
169 | 60 | [54] |
| Tetracycline |
TetB-F TetB-R |
CTCAGTATTCCAAGCCTTTG CTAAGCACTTGTCTCCTGTT |
416 | [54] | |
| Tetracycline |
TetC-F TetC-R |
TCTAACAATGCGCTCATCGT GGTTGAAGGCTCTCAAGGGC |
570 | [54] | |
| ESBL | TEM |
AGTGCTGCCATAACCATGAGG CTGACTCCCCGTCGTGTAGATA |
431 | [55] | |
| SHV |
GATGAACGCTTTCCCATGATG CGCTGTTATCGCTCATGGTAA |
214 | |||
| OXA |
ATTATCTACAGCAGCGCCAGTG TGCATCCACGTCTTTGGTG |
296 | |||
| CTX-M |
GACAAAGAGAGTGCAACGGATG TCAGTGCGATCCAGACGAAA |
501 | |||
| MBL | blaNDM-1 |
ATTAGCCGCTGCATTGAT CATGTCGAGATAGGAAGTG |
154 | 55 | [56] |
| blaIMP |
TTGACACTCCATTTACAG GATTGAGAATTAAGCCACTCT |
139 | [57] | ||
| blaVIM |
GATGGTGTTTGGTCGCATA CGAATGCGCAGCACCAG |
390 | |||
| ABL | CMY |
GCTGCTCAAGGAGCACAGGAT CACATTGACATAGGTGTGGTGC |
520 | 60 | [58] |
| DHA |
AACTTTCACAGGTGTGCTGGGT CCGTACGCATACTGGCTTTGC |
405 | |||
| ACT-1 |
TCGGTAAAG CCGATGTTG CGG CTT CCA CTG CGG CTG CCA GTT |
302 | |||
| Reference gene | 16SrRNA |
CCCCCTGGACGAAGACTGAC ACCGCTGGCAACAAAGGATA |
401 | [49] | |
All the isolates were screened for phylogenetic groups A, B1, B2, C, D, E, F and Clade I using quadruplex multiplex PCR as described by Clermont et al. [47]. The presence of chuA gene represents groups B2 and D and absence represents groups A and B1. Group B2 and group D are being differentiated by yjaA gene.
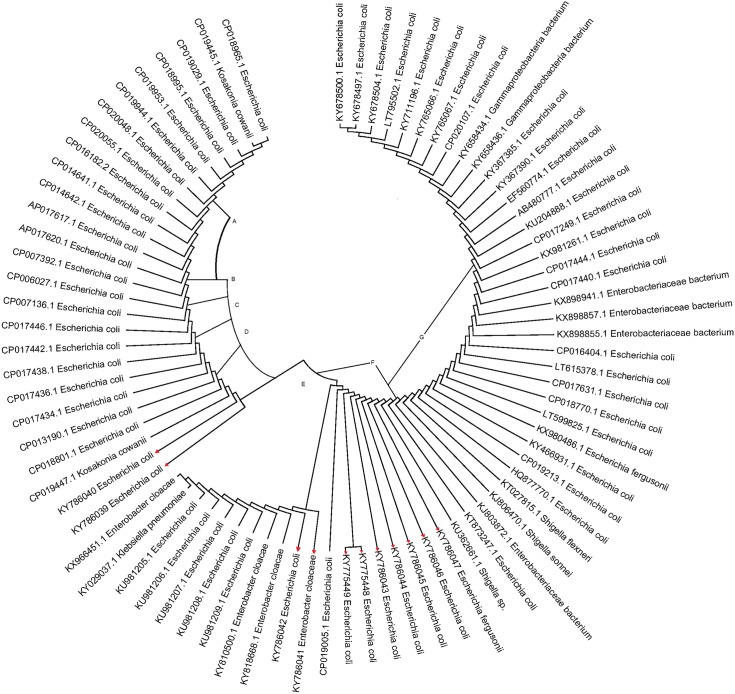
Sequences of PCR product analyzed, commercially by Helix Biosciences (Bangalore, India), were matched with nucleotide sequences available at GenBank using the BLAST program to identify the most similar sequences [59]. Few of the sequences identified from the current study were submitted to the GenBank database and accession numbers obtained. Multiple alignments of sequenced nucleotides were carried out using Clustal W2 (version 2.0.10). Neighbor-joining method was used to construct tree in MEGA 6.0 [60, 61].
Statistical analysis
Statistical analysis was done using Sigma Stat Statistics Software (SPSS) package. The Chi-square test and Fisher’s exact test were used to determine the statistical significance of data. The p-value < 0.05 was considered significant.
Results
Isolation of antibiotic resistant genes and SNP
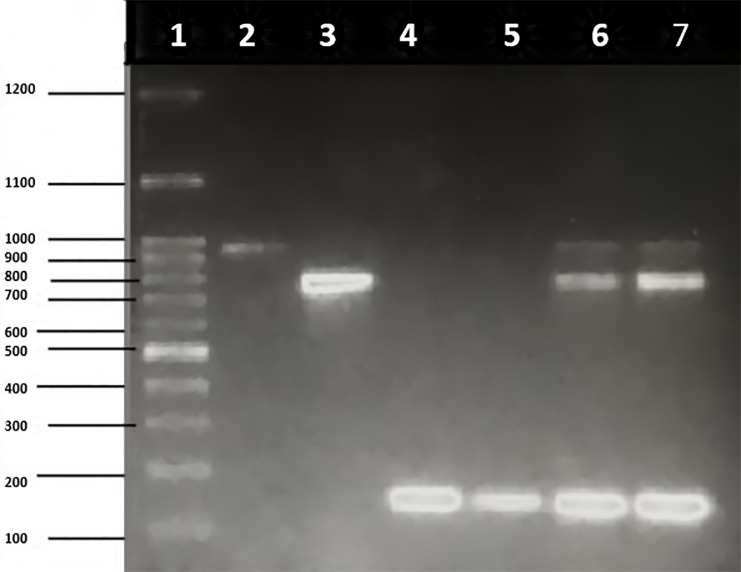
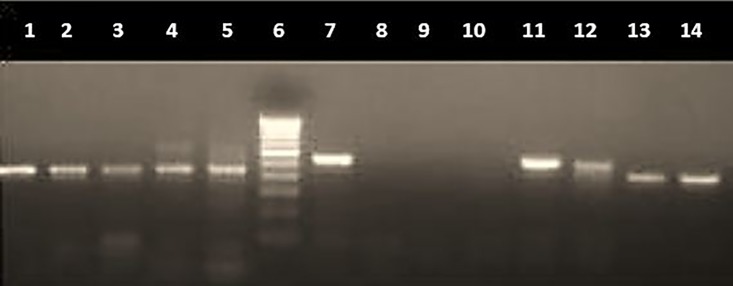
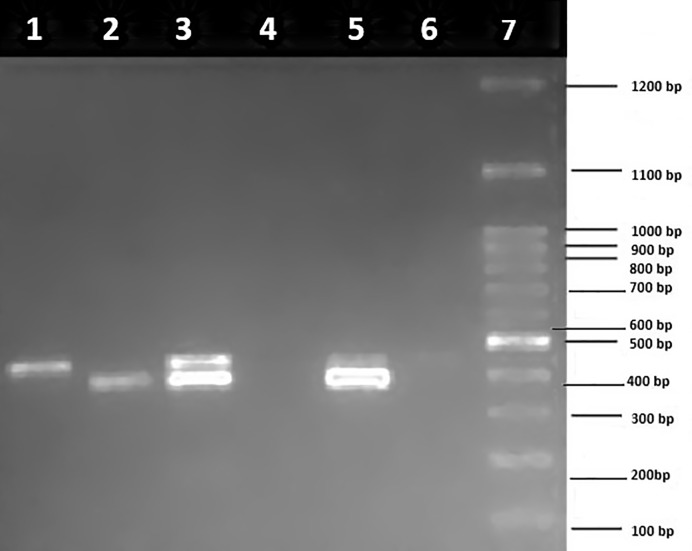
Owing to the scarcity of detailed studies on the prevalence of antimicrobial resistance patterns in paediatric age group in India, screening of diarrheagenic E. coli for the presence of virulence genes and drug resistance genes was performed in our previous study [48]. Multiplex PCR for antibiotic resistance genes showed presence of tetA, sul1 and AacC1 as shown in Fig 1, and tetB and tetC as shown in Fig 2. PCR for SNP targeting QRDR of fluoroquinolones (gyrA and parC) was also performed (Figs 3 and 4).
Fig 1. Multiplex PCR for antibiotic resistance genes (tetA, sul1 and AacC1) on 1.5% agarose gel.
Lane 1: molecular weight marker (100 bp), lane 2: tetA (937 bp), lane 3: sul1 (789 bp), lane 4–5: AacC1 (169 bp), lane 6–7: tetA + sul1 + AacC1.
Fig 2. PCR for antibiotic resistance genes (tetB and tetC) on 1.5% agarose gel.
Lane 1–3: tetB (416 bp), lane 4–5: tetB + tetC (570 bp), lane 6: molecular weight marker (100 bp), lane 7: tetC, lane 8–10: negative isolates, lane 11–12: tetC and lane 13–14: tetB.
Fig 3. PCR for single nucleotide polymorphism (SNP) of fluoroquinolones (gyrA and parC) on 1.5% agarose gel.
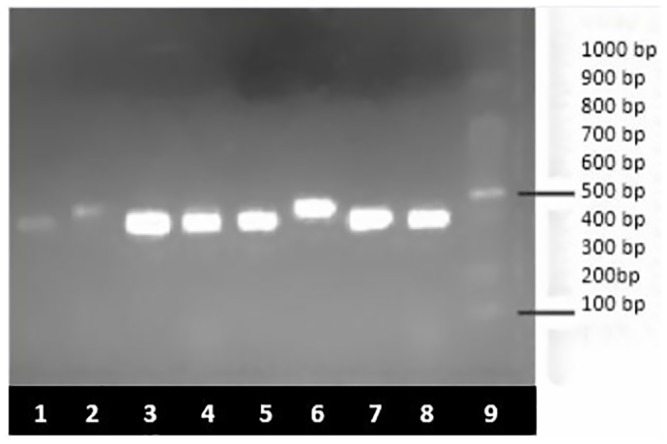
Lane: 1, 3–5, 7–8; parC (395 bp), lane 2 and 6: gyrA (447 bp) and lane 9: molecular weight marker (100 bp).
Fig 4. Multiplex PCR for single nucleotide polymorphism (SNP) of fluoroquinolones (gyrA and parC) on 1.5% agarose gels.
Lane 1: gyrA (447 bp), lane 2: parC (395 bp), lane 3: gyrA + parC, lane 4: negative control, lane 5: gyrA + parC, lane 6: negative control, and lane 7: molecular weight marker (100 bp).
Detection of genes conferring resistance to β-lactamases, tetracycline, gentamicin, and sulphonamide
The distribution of various antibiotic resistance genes in three subject groups analyzed by multiplex PCR is shown in Table 2. High frequency of resistance was detected against ampicillin, sulfonamides and tetracycline. Briefly, Significant antibiotic resistance gene frequency was detected in case of CMY (15%), aacC1 (19.16%) and gyrA + parC (2.5%). Sul1 gene was found prevalent 57 (47.5%) followed by TEM, SHV, tetA and aacC1 (Table 2). Tetracycline resistance gene tetA and class 1 integrons usually share the same conjugative plasmid [62]. The prevalence of sul1 gene in our integron-positive healthy isolates was 47.5% higher than earlier published report [63] suggesting that commensal strains could also harbor these resistance determinants. A significant association between resistance to aminoglycosides tested (gentamicin) and the presence of integron indicate the presence of aminoglycoside resistance genes within integron structures, including aadA and aacA1 [64].
Table 2. Distribution of various antibiotic resistance genes in three groups.
| Genes | Group-1 n (%) |
Group-2 n (%) |
Group-3 n (%) |
Total n (%) |
p-value |
|---|---|---|---|---|---|
| TEM | 19(47.5) | 14(35) | 16(40) | 49 (40.83) | 0.519 |
| SHV | 14(35) | 14(35) | 11(27.5) | 39 (32.5) | 0.710 |
| CTX-M | 7(17.5) | 8(20) | 8(20) | 23(19.16) | 0.947 |
| OXA | 9 (22.5) | 7 (17.5) | 7 (17.5) | 23 (19.16) | 0.806 |
| NDM-1 | 11 (27.5) | 5 (12.5) | 6 (15) | 22(18.33) | 0.178 |
| IMP | 12 (32.5) | 5 (12.5) | 6 (15) | 23(19.16) | 0.098 |
| VIM | 8 (20) | 7 (17.5) | 7 (17.5) | 22(18.33) | 0.945 |
| ACT | 6 (15) | 8 (20) | 6 (15) | 20 (16.66) | 0.786 |
| DHA | 4 (10) | 2 (5) | 3 (7.5) | 9 (7.5) | 0.697 |
| CMY | 11 (27.5) | 4 (10) | 3 (7.5) | 18 (15) | 0.024* |
| sul1 | 22 (55) | 16 (40) | 19 (47.5) | 57 (47.5) | 0.405 |
| tetA | 13 (32.5) | 6 (15) | 5 (12.5) | 24 (20) | 0.051 |
| aacC1 | 12 (30) | 9 (22.5) | 2 (5) | 23 (19.16) | 0.014* |
| tetB | 5 (12.5) | 4 (10) | 3 (7.5) | 12 (10) | 0.757 |
| tetC | 6 (20) | 5 (12.5) | 1 (2.5) | 12 (10) | 0.143 |
| gyrA | 6 (15) | 4 (10) | 4 (10) | 14 (11.66) | 0.723 |
| parC | 2 (5) | 1 (2.5) | 0 | 3 (2.5) | 0.358 |
| gyrA + parC | 3 (7.5) | 0 | 0 | 3 (2.5) | 0.046* |
*significant p-value. Gene frequencies are present as absolute numbers with percentage in parentheses
SNPs in gyrA (A660-T660) and parC (C330-T330) were detected in 11.66% and 2.5% isolates, respectively. Among all Nalidixic acid and Ciprofloxacin resistant isolates, 29.78% isolates showed point mutation for gyrA gene, while 27.27% isolates showed point mutation for parC and 5.17% isolates showed mutation for both gyrA and parC. However, no mutation was detected in QRDR of gyrA and parC in 28/48 (58.33%) and 5/11 (45.45%) isolates, respectively; although these isolates were found resistant against Nalidixic acid and Ciprofloxacin, phenotypically {S1 and S2 Tables}.
A multiple logistic regression model was prepared to detect certain independent predictors of antibiotic resistance in three groups (Table 3). It was observed that all independent predictors of antibiotic-resistant genes except sul1 showed strong association with development of antibiotic resistance (p-value < 0.05). Coefficient of adjusted odds ratio was 0.819 times higher in sul1 as compared to other genes for which it was in the range of 0.004–0.477.
Table 3. Multiple logistic regression models exploring certain independent predictors of antibiotic resistance.
| Predictors of antibiotic resistance genes | n = 120 | p-value | Adjusted Odds ratio | 95% CI (Lower) |
95% CI (Upper) |
|---|---|---|---|---|---|
| Sul1 | |||||
| Present | 57 | 0.438 | 0.819 | 0.492 | 1.362 |
| Absent | 63 | 1 | |||
| TetA | |||||
| Present | 24 | 0.000* | 0.063 | 0.033 | 0.118 |
| Absent | 96 | 1 | |||
| TetB | |||||
| Present | 12 | 0.000* | 0.60 | 0.24 | 1.48 |
| Absent | 108 | 1 | |||
| TetC | |||||
| Present | 12 | 0.000* | 0.012 | 0.005 | 0.028 |
| Absent | 108 | 1 | |||
| aaCa | |||||
| Present | 23 | 0.000* | 0.057 | 0.029 | 0.107 |
| Absent | 97 | 1 | |||
| TEM | |||||
| Present | 49 | 0.004* | 0.477 | 0.284 | 0.798 |
| Absent | 71 | 1 | |||
| SHV | |||||
| Present | 39 | 0.000* | 0.227 | 0.131 | 0.389 |
| Absent | 81 | 1 | |||
| CTX | |||||
| Present | 23 | 0.000* | 0.057 | 0.029 | 0.107 |
| Absent | 97 | 1 | |||
| OXA | |||||
| Present | 23 | 0.000* | 0.057 | 0.029 | 0.107 |
| Absent | 97 | 1 | |||
| NDM-1 | |||||
| Present | 22 | 0.000* | 0.031 | 0.015 | 0.063 |
| Absent | 98 | 1 | |||
| IMP | |||||
| Present | 23 | 0.000* | 0.031 | 0.015 | 0.063 |
| Absent | 97 | 1 | |||
| VIM | |||||
| Present | 22 | 0.000* | 0.027 | 0.013 | 0.056 |
| Absent | 98 | 1 | |||
| ACT | |||||
| Present | 20 | 0.000* | 0.021 | 0.009 | 0.044 |
| Absent | 100 | 1 | |||
| CMY | |||||
| Present | 18 | 0.000* | 0.021 | 0.009 | 0.044 |
| Absent | 102 | 1 | |||
| DHA | |||||
| Present | 9 | 0.000* | 0.004 | 0.001 | 0.011 |
| Absent | 111 | 1 | |||
*statistically significant
Note: The y variable is antibiotic resistance whereas the variables mentioned as predictors are the independent (x) variables in the multiple logistic regression models.
16SrRNA sequencing
Few positive isolates were sequenced and submitted to NCBI (accession numbers: gyrA KY753823 and parC KY753821). Alignment of the gyrA (DNA GyrAse) gene sequence conferring resistance to Nalidixic acid and alignment of the parC (DNA topoisomerase) gene sequence conferring resistance to Ciprofloxacin is shown in Figs 5 and 6 [55–57,65,66]. The 16SrRNA was amplified using universal primers and the nucleotide sequences of the 16SrRNA of all the isolates were submitted to NCBI and following accession numbers were obtained: KY775448, KY775449, KY786039, KY786040, KY786041, KY786042, KY786043, KY786044, KY786045, KY786046, and KY786047.
Fig 5. Sequence alignment of the gyrA (DNA gyrase) gene sequence (5) that confers resistance to quinolones (Nalidixic acid).
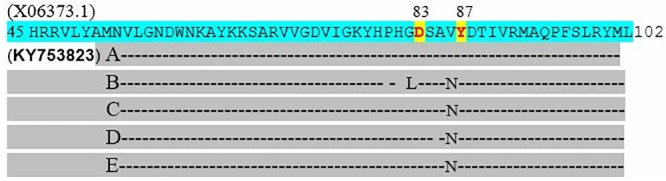
Quinolone resistance determining regions (QRDR) were amplified by PCR and sequenced using the primers [56, 57]. The substitution was seen at position 83 (confers high-level resistance) and 87 (confers low-level resistance) as described by [55, 63]. This amino substitution does not alter the stereochemical structure greatly and is therefore unlikely to confer resistance to quinolones on its own. The gyrA reference sequence (X06373.1) was obtained from the NCBI database and accession number KY753823 was generated from the study.
Fig 6. Sequence alignment of the parC (DNA topoisomerase) gene sequence (5) that confers resistance to quinolones (Ciprofloxacin).
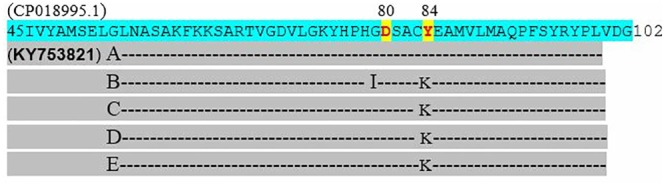
Quinolone resistance determining regions (QRDR) were amplified by PCR and sequenced using the primers [55, 56]. The substitution was seen at position 80 (responsible for quinolone resistance) and 84 (increase affinity to ciprofloxacin by producing positively charged amino acid) as described by [55, 63]. This amino substitution does not alter the stereochemical structure greatly and is therefore unlikely to confer resistance to quinolones on its own. The parC reference sequence (CP018995.1) was obtained from the NCBI database and accession number KY753821 was generated from the study.
Phylogenetic analysis
Eleven isolates from the current study were used to construct a phylogenetic tree along with other sequences from database for 16SrRNA as described in detail previously by Shashi and Kumar [67] (Fig 7). Significant diversity was evident among these isolates. The phylogenetic tree showed that all the isolates could be grouped into seven phylogroups on the basis of approximately 98% similarity among them (Fig 7). Briefly, the prevalence of phylogenetic group B2 was 36.66%, followed by groups B1, A, F, D, E and C in our study (Table 4). Similar pattern was observed in the healthy isolates with the prevalence of group B2, followed by B1, F and A. All the isolates were assigned a phylogroup except 11 isolates which remained unclassified. None of the isolates recovered from diarrheagenic cases or healthy controls belonged to phylogroup Clade I.
Fig 7. Phylogenetic analysis based on the sequences of 16SrRNA gene sequence of 11 diarrheagenic E. coli (DEC) isolates and 70 sequences retrieved from NCBI.
The accession number of each strain is mentioned in the tree. Eleven isolates identified by this study are highlighted in red.
Table 4. Distribution of various phylogenetic groups in three study populations.
| Phylogroup | Group-1 n (%) |
Group-2 n (%) |
Group-3 n (%) |
Total n (%) |
p-value |
|---|---|---|---|---|---|
| A | 7 (17.5) | 5 (12.5) | 7 (17.5) | 19 (15.83) | 0.778 |
| B1 | 9 (22.5) | 6 (15) | 11 (27.5) | 26 (21.66) | 0.393 |
| B2 | 17 (4/2.5) | 15 (37.5) | 12 (30) | 44 (36.66) | 0.505 |
| C | 1 (2.5) | 1 (2.5) | 1 (2.5) | 3 (2.5) | 1.000 |
| D | 3 (7.5) | 1 (2.5) | 2 (5) | 6 (5) | 0.590 |
| E | 1 (2.5) | 1 (2.5) | 2 (5) | 4 (3.33) | 0.772 |
| F | 3 (7.5) | 3 (7.5) | 2 (5) | 8 (6.66) | 0.874 |
| Clade 1 | 0 | 0 | 0 | 0 | N.A |
| Unclassified | 4 (10) | 4 (10) | 3 (7.5) | 11 (9.16) | 0.904 |
Gene frequencies are present as absolute numbers with percentage in parentheses
Discussion
Antibiotic resistance in bacteria is not only a serious global health problem worldwide but also it renders most of the antibiotics ineffective. The threat is compounded with the continuous spread of drug resistance and enhanced survival potential of such bacterial strains [68, 69]. Since, changes at the gene level like compensatory or suppressor mutations may favor the survival of resistant microbe, the selection of the most virulent and resistant pathogens depends upon the antimicrobial selective pressure [69, 70]. We attempted to analyze the acquisition of point mutations in gyrA and parC genes in QRDR; tetracycline, sulphonamide and gentamicin resistance genes in isolates of E. coli. Tetracycline resistance gene tetA and class 1 integrons are normally present on the same conjugative plasmid [63], but the acquisition of gentamicin resistance genes is unclear. The prevalence of sul1 gene in isolates recovered from healthy subjects samples was 47.5% higher when compared with an early report, suggesting that the commensal strains may also transfer these resistance determinants to neighboring susceptible commensals [64].
Enzymes DNA gyrase, encoded by gyrA and gyrB, and DNA topoisomerase, encoded by parC and parE, are important for bacterial replication and thus primary targets of quinolones. Mutation in the parC gene confers resistance to the secondary class of fluoroquinolones. We observed less prevalence of parC mutation in fluoroquinolones/ciprofloxacin resistant isolates in our population, in contrast to earlier reports [42, 71–74].
An SNP prevalence of 11.66% and 2.5% isolates was detected in gyrA and parC gene respectively, corroborating the findings of previous studies [33, 42, 70, 75–77]. Interestingly, most of the ESBL-producing isolates in our study were resistant to ciprofloxacin having mutations in gyrA/parC genes demonstrating underlying causes of fluoroquinolone resistance [78–80].
It is well-known that E. coli is no longer restricted to the hospital environment [81]. The β-lactamase genes harboring MDR strains are found in healthy children raising an underlying threat of widespread circulation of resistant strains in the community [82, 83]. The genes located on transmissible plasmid along with other antibiotic resistance genes enables an easy dissemination in the environment and amongst hospitalized patients [84]. The VIM encoding integron structure acquired during the hospital stay may also colonize in patients and retain as reservoirs [85]. The emergence of the CMY gene has also been reported in E. coli along with other diverse genera of the Enterobacteriaceae [86]. Several other factors like overcrowding, availability of antibiotics, low level of hygiene and weak hospital antibiotic policies are also responsible for their extensive clonal dissemination [87].
All antibiotic resistant genes, except sulphonamide, appear as important predictors of drug resistance in paediatric population. Low frequency of occurrence of genes of tetracycline, aminoglycosides and other β-lactamases genes perform well as indicators of emerging resistance in children, unlike the sulphonamide resistance which was uniform in all the study groups. Majority of the ESBLs found in E. coli are derivatives of TEM or SHV enzymes while CTX-M and OXA-type beta-lactamase occur less frequently [88, 89].
The ABLs (AmpC β-lactamases) is one of the prevalent mechanisms of β-lactam resistance after ESBLs in E. coli and emerged as an important health problem in the recent years [90, 91]. There are various factors which are associated with development of quinolone resistance, including chromosomal mutations, acquisition of plasmid-mediated genes and decreased uptake of the antimicrobials [92]. We observed occurrence of multiple transferrable resistance genes in E coli. This bacteria being an essential gut microflora, may facilitate the promulgation of resistance determinants to other microbiome and its prolonged survival helps create a huge reservoir of drug resistant microbes [93].
The E. coli phylogroups have different ecological niches, biological characteristics and ability to cause disease. Early reports suggested a link between phylogeny and virulence determinants [94], that are often carried by strains of phylogenetic groups B2 and D [95, 96]. Due to the small number of subjects, the phylogenetic analysis of the isolates did not show any significant difference between the phylogroups. Variations in environmental conditions and host genetic factors may be the responsible for the contrasting findings from other reports [97, 98]. Our results showed the preponderance of phylogenetic group B2 (36.66%) similar to previous reports [97, 98]. Groups B1, A, F, D, E and C were found to have 21.66%, 15.83%, 5.83%, 5%, 3.33% and 2.5% isolates, respectively. We also found commensal phylogroups A and B1 in agreement with previous studies showing that diarrheagenic E. coli isolates are included in phylogroups A, B1, and D [99, 100]. A total of 11 isolates (9.16%) remained unidentified as they were negative for all the genes by quadruplex PCR. The ecological distribution of phylogenetic groups of human E. coli isolates are thus variable and dynamic, influenced by factors such as host genetic makeup, dietary conditions, use of medications, and geographical circumstances often useful in describing the profile of the particular community [82, 83].
We could also reveal 5% isolates associated with phylogroup D that is linked with the spread of AmpC- mediated antibiotic resistance (especially CMY-2 type) [101–104]. Further, this group is also involved in the spread of CTX-M genes [105–107]. The existence of more than 40% of our isolates under phylogroups B2 and D is worth noting as these are associated with ESBLs and AmpCs expressing E. coli strains linked with higher virulence characteristics as described in early studies on phylogroups A and B1 [103, 108, 109]. Although, little is known about the association of MBL resistance with phylogroups in E. coli, phylogroups B1 and D are thought to be associated with NDM-1 type [110–114]. The study highlights that children harbor pathogenic as well as commensal strains of E. coli in alarming abundance and their co-existence in similar niches enable them to maintain a continuous circulation of gene transfer. This observation draws attention to an urgent need for preventing future catastrophe. Bacterial populations in the human gut are complex and share a similar ecology, giving them abundant opportunity for the transfer of genetic material [115].
The current scientific advances have created a wide area of interest amongst scientists to understand the spread of antibiotic resistance genes, and the field of metagenomics have enabled them to create a database of gut commensal resistome from healthy individuals from different countries. Documented evidences state that countries with relatively reserved policies of antibiotic use in humans and animals (like Denmark) have observed lower levels of antibiotic resistance genes in human gut microbiota than in people from countries where antibiotic use is considerably higher (like Spain and China) [116]. Therefore, it is high time to raise awareness amongst health care providers and develop country wise national policies for rationale use of antibiotics in humans especially amongst the vulnerable pediatric population to combat the menace of drug resistance [116, 117].
Conclusion
The spread of antimicrobial resistance has emerged as an important public health problem especially in resource limited countries where lack of strict adherence to antibiotic policy has created a challenge for the clinicians to treat serious infections essentially in prolonged hospitalized patients. Our phylogenetic analysis identified 40% of the isolates grouped as B2 and D which mostly harbor ESBL and ABL expressing E. coli strains. Mankind has partly been responsible for creating such an environment for the microbial world to develop armamentarium for challenging the antimicrobial agents. Gut flora is the first line of defense, and harboring drug-resistant pathogens will be detrimental not only to that individual but will be a threat to the community. Antibiotic resistance has extended from hospital to community settings as well, suggesting that healthy children may also contribute to the development of MDR in E. coli. Our observation in pediatric population is a grim reality to the development, dissemination and carriage of antibiotic resistant bugs not only in the gut of diarrhoeal children but also in healthy children of our community. Active AMR surveillance and stewardship programs needs to be implemented in all hospitals to minimize further danger.
Supporting information
The data used to create this figure can be accessed at the Center for Disease Dynamics, Economics & Policy (CDDEP) Resistance Map website at http://resistancemap.cddep.org/resmap/c/in/India.
(PDF)
(PDF)
(PDF)
Acknowledgments
The Council of Scientific and Industrial Research (CSIR), Pusa, New Delhi is acknowledged for providing Senior Research Fellowship [08/532(0007)/2011-EMR-I] to TS. The authors wish to thank all the children and their parents for providing the samples. The authors are grateful to Dr. Shaun Cochrane, Ph.D. graduate from NIHR, MRC, London, for reviewing the manuscript.
Data Availability
All relevant data are within the manuscript and its Supporting Information files.
Funding Statement
The author(s) received no specific funding for this work.
References
- 1.Ramana J, Tamanna. Db Diarrhea: The database of pathogen proteins and vaccine antigens from diarrheal pathogens. Infect Genet Evol. 2012;12: 1647–1651. 10.1016/j.meegid.2012.08.002 [DOI] [PubMed] [Google Scholar]
- 2.FDA. National Antimicrobial Resistance Monitoring System-Enteric Bacteria (NARMS): 2010 Executive Report. Rockville, MD: U.S: Department of Health and Human Services, Food and Drug Administration, 2012. [Google Scholar]
- 3.Hammerum AM, Heuer OE. Human Health Hazards from Antimicrobial Resistant Escherichia coli of Animal Origin. Clin Infect Dis. 2009;48: 916–921. 10.1086/597292 [DOI] [PubMed] [Google Scholar]
- 4.Lester SC, Pla MP, Wang F, Schael IP, Jiang H, and O’Brien TF. The Carriage of Escherichia coli Resistant to Antimicrobial Agents by Healthy Children in Boston, in Caracas, Venezuela, and in Qin Pu, China. N Engl J Med. 1990; 323: 285–289. 10.1056/NEJM199008023230501 [DOI] [PubMed] [Google Scholar]
- 5.Nys S, Okeke IN, Kariuki S, Dinant GJ, Driessen C, Stobberingh EE. Antibiotic resistance of faecal Escherichia coli from healthy volunteers from eight developing countries. JAntimicrob Chemother. 2004;54: 952–955. [DOI] [PubMed] [Google Scholar]
- 6.Galán JC, Candelas FG, Rolain JM and Cantón R. Antibiotics as selectors and accelerators of diversity in the mechanisms of resistance: from the resistome to genetic plasticity in the β-lactamases world. Front Microbiol. 2013;4: 1–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Aarestrup FM, Wegener HC, Collignon P. Resistance in bacteria of the food chain: Epidemiology and control strategies. Expert Rev Anti Infect Ther. 2008;6: 733–750. 10.1586/14787210.6.5.733 [DOI] [PubMed] [Google Scholar]
- 8.Levy SB, Bonnie M. Antibacterial resistance worldwide: Causes, challenges and responses. Nat Med. 2004;10: S122–S129. 10.1038/nm1145 [DOI] [PubMed] [Google Scholar]
- 9.Center for Disease Dynamics Economics & Policy, State of the World’s Antibiotics, CDDEP. 8 (2015) 30–34. https://www.cddep.org/wp-content/uploads/2017/06/swa_executive_summary_edits_2016.pdf
- 10.Van Boeckel TP, Brower C, Gilbert M, Grenfell BT, Levin SA, Robinson TP et al. Global trends in antimicrobial use in food animals. Proc Natl Acad Sci. 2015;112: 5649–5654. 10.1073/pnas.1503141112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Laxminarayan R and Chaudhury RR. Antibiotic Resistance in India: Drivers and Opportunities for Action. PLoS Med. 2016; 13(3):e1001974 10.1371/journal.pmed.1001974 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rowe-Magnus DA and Mazel D. Integrons: natural tools for bacterial genome evolution. Current opinion in microbiology. 2001; 4: 565–569. [DOI] [PubMed] [Google Scholar]
- 13.Rowe-Magnus DA and Mazel D. Resistance gene capture. Current opinion in microbiology.1999; 2: 483–488. [DOI] [PubMed] [Google Scholar]
- 14.Agrawal P, Ghosh AN, Kumar S, Basu B and Kapila K. Prevalence of extended-spectrum β-lactamases among Escherichia coli and Klebsiella pneumoniae isolates in a tertiary care hospital. Indian Journal of Pathology and Microbiology. 2008;51: 139 [DOI] [PubMed] [Google Scholar]
- 15.Jacoby GA. AmpC beta-lactamases. Clin. Microbiol. Rev. 2009; 22: 161–182. 10.1128/CMR.00036-08 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Queenan AM and Bush K. Carbapenemases: the versatile b-lactamases. Clin Microbiol. 2007; 20: 440–458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jacoby GA and Munoz-Price LS. The new β-lactamases. New England Journal of Medicine, 2005; 352: 380–391. 10.1056/NEJMra041359 [DOI] [PubMed] [Google Scholar]
- 18.Pitout JD and Laupland KB. Extended-spectrum β-lactamase-producing Enterobacteriaceae: an emerging public-health concern. The Lancet infectious diseases. 2008; 8: 159–166. 10.1016/S1473-3099(08)70041-0 [DOI] [PubMed] [Google Scholar]
- 19.Pai H., Kang C.I., Byeon J.H., Lee K.D., Park W.B., Kim H.B., Kim E.C., Oh M.D. & Choe K.W. Epidemiology and clinical features of bloodstream infections caused by AmpC-type beta-lactamase-producing Klebsiella pneumoniae. Antimicrob. Agents Chemother. 2004; 48: 3720–3728. 10.1128/AAC.48.10.3720-3728.2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Park YS, Yoo S, Seo MR, Kim JY, Cho YK and Pai H. Risk factors and clinical features of infections caused by plasmid-mediated AmpC beta lactamase- producing Enterobacteriaceae. Int. J. Antimicrob. Agents. 2009; 34: 38–43. 10.1016/j.ijantimicag.2009.01.009 [DOI] [PubMed] [Google Scholar]
- 21.Hall RM, Collis CM. Mobile gene cassettes and integrons: capture and spread of genes by site-specific recombination. Mol Microbiol. 1995;15: 593–600. [DOI] [PubMed] [Google Scholar]
- 22.Mazel D, Dychinco B, Webb V, Davies J. Antibiotic resistance in the ECOR collection: integrons and identification of a novel aad gene. Antimicrob Agents Chemother. 2000;44: 1568–1574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gupta K, Hooton TM, Stamm WE. Increasing antimicrobial resistance and the management of uncomplicated community-acquired urinary tract infections. Ann Intern Med. 2001;135: 41–50. [DOI] [PubMed] [Google Scholar]
- 24.Schwarz S, Chaslus-Dancla E. Use of antimicrobials in veterinary medicine and mechanisms of resistance. Vet Res. 2001;32: 201–225. 10.1051/vetres:2001120 [DOI] [PubMed] [Google Scholar]
- 25.Enne VI, Delsol AA, Davis GR, Hayward SL, Roe JM, Bennett PM. Assessment of the fitness impacts on Escherichia of acquisition of antibiotic resistance genes encoded by different types of genetic element. J. AntimicrobChemother. 2005;56: 544–551. [DOI] [PubMed] [Google Scholar]
- 26.Perreten V, Boerlin P.A New Sulfonamide Resistance Gene (sul3) in Escherichia coli Is Widespread in the Pig Population of Switzerland. Antimicrob Agents Chemother. 2003;47: 1169–1172. 10.1128/AAC.47.3.1169-1172.2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Blake DP, Humphry RW, Scott KP, Hillman K, Fenlon DR, Low JC. Influence of tetracycline exposure on tetracycline resistance and the carriage of tetracycline resistance genes within commensal Escherichia coli populations. J ApplMicrobiol. 2003;94: 1087–1097. [DOI] [PubMed] [Google Scholar]
- 28.Wilkerson C, Samadpour M, Kirk NV, Roberts MC. Antibiotic Resistance and Distribution of Tetracycline Resistance Genes in Escherichia coli O157: H7 Isolates from Humans and Bovines. Antimicrob Agents Chemother. 2004;48: 1066–1067. 10.1128/AAC.48.3.1066-1067.2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Baum HV, Marre R. Antimicrobial resistance of Escherichia coli and therapeutic implications. Int J Med Microbiol. 2005; 295: 503–511. 10.1016/j.ijmm.2005.07.002 [DOI] [PubMed] [Google Scholar]
- 30.Oethinger M, Conrad S, Kaifel K, Cometta A, Bille J, Klotz G et al. Molecular epidemiology of fluoroquinolone-resistant Escherichia coli bloodstream isolates from patients admitted to European cancer centres. Antimicrob Agents Chemother. 1996;40: 387–392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Evans WE, Relling MV. Pharmacogenomics: Translating functional genomics into rational therapeutics. Science. 1999; 286: 487–491. [DOI] [PubMed] [Google Scholar]
- 32.Namboodiri SS, Opintan JA, Lijek RS, Newman MJ, Okeke IN. Quinolone resistance in Escherichia coli from Accra, Ghana. BMC Microbiol.2011; 11:44 10.1186/1471-2180-11-44 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cambau E, Bordon F, Collatz E, Gutmann L. Novel gyrA point mutation in a strain of Escherichia coli resistant to fluoroquinolones but not to nalidixic acid. Antimicrob Agents Chemother.1993; 37:1247–1252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Heisig P, Schedletzky H, Paul HF. Mutations in the gyrA gene of a highly fluoroquinolone-resistant clinical isolate of Escherichia coli. Antimicrob Agents Chemother. 1993;37: 696–701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Vila J, Ruiz J, Marco F, Barcelo A, Goni P, Giralt E, De Anta TJ. Association between double mutation in gyrA gene of ciprofloxacin-resistant clinical isolates of Escherichia coli and MICs, Antimicrob Agents Chemother. 1994;38: 2477–2479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Vila J, Ruiz J, Goñi P, De Anta MT. Detection of mutations in parC in quinolone-resistant clinical isolates of Escherichia coli. Antimicrob Agents Chemother. 1996;40: 491–493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Martínez LM, Cano EC, Martínez JMR, Calvo J, Pascual A. Plasmid-mediated quinolone resistance. Expert Rev Anti InfectTher. 2008;6: 685–711. [DOI] [PubMed] [Google Scholar]
- 38.Giraud E, Sétrin SL, Flaujac G, Cloeckaert A, Moulin MD, Dancla EC, Characterization of high-level fluoroquinolone resistance in Escherichia coli O78:K80 isolated from turkeys. J AntimicrobChemother. 2001;47: 341–343. [DOI] [PubMed] [Google Scholar]
- 39.Everett MJ, Jin YF, Ricci V, Piddock LJ. Contributions of individual mechanisms to fluoroquinolone resistance in 36 Escherichia coli strains isolated from humans and animals. Antimicrob Agents Chemother. 1996;40: 2380–2386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Yoshida H, Kojima T, Yamagishi JI, and Nakamura S. Quinolone-resistant mutations of the gyrA gene of Escherichia coli. Mol Gen Genet. 1988;211: 1–7. [DOI] [PubMed] [Google Scholar]
- 41.Conrad S, Oethinger M, Kaifel K, Klotz G, Marre R, Kern WV. gyrA Mutations in high-level fluoroquinolone-resistant clinical isolates of Escherichia coli. Bact. 1996;9: 443–455. [DOI] [PubMed] [Google Scholar]
- 42.Heisig P. Genetic evidence for a role of parC mutations in development of high-level fluoroquinolone resistance in Escherichia coli. 1996;40: 879–885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hooper DC. Mechanisms of fluoroquinolone resistance. Drug Resist Updat. 1999;2: 38–55. 10.1054/drup.1998.0068 [DOI] [PubMed] [Google Scholar]
- 44.Oethinger M, Kern WV, Jellen-Ritter AS, McMurry LM, Levy SB. Ineffectiveness of topoisomerase mutations in mediating clinically significant fluoroquinolone resistance in Escherichia coli in the absence of the AcrAB efflux pump. Antimicrob Agents Chemother. 2000;44: 10–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hopkins KL, Davies RH, Threlfall EJ. Mechanisms of quinolone resistance in Escherichia coli and Salmonella: Recent developments. Int JAntimicrob Agents. 2005;25: 358–373. [DOI] [PubMed] [Google Scholar]
- 46.Wang H, Dzink-Fox J. Genetic Characterization of Highly Fluoroquinolone-Resistant Clinical Escherichia coli Strains from China: Role of acrR Mutations. Antimicrob Agents. 2001;45: 1515–1521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Clermont O, Christenson JK, Denamur E, Gordon DM. The Clermont Escherichia coli phylo-typing method revisited: Improvement of specificity and detection of new phylo-groups. Environ Microbiol Rep. 2013;5: 58–65. 10.1111/1758-2229.12019 [DOI] [PubMed] [Google Scholar]
- 48.Singh T, Das S, Ramachandran VG, Wani S, Shah D, Maroof KA et al. Distribution of integrons and phylogenetic groups among enteropathogenic Escherichia coli isolates from children < 5 Years of Age in Delhi, India. Front Microbiol. 2017;8: 561–574. 10.3389/fmicb.2017.00561 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wang G, Clark CG, Rodgers F G. Detection in Escherichia coli of the Genes Encoding the Major Virulence Factors, the Genes Defining the O157: H7 Serotype and Components of the Type 2 Shiga Toxin Family by Multiplex PCR. J ClinMicrobiol. 2002;40: 3613–3619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Bauer AW, Kirby WMM, Sherris JC, Turck AM. Antibiotic Susceptibility Testing by a Standardized Single Disk Method. Am J ClinPathol. 1966;45: 493–496. [PubMed] [Google Scholar]
- 51.CLSI, Methods for Dilution Antimicrobial Susceptibility Tests for Bacteria That Grow Aerobically, Approv. Stand Ed. CLSI Doc M07-A10. (2015) 1–87. https://clsi.org/media/1632/m07a10_sample.pdf [Google Scholar]
- 52.Hollingshead S, Vapnek D. Nucleotide sequence analysis of a gene encoding a streptomycin/spectinomycin adenylyl transferase. Plasmid. 1985;13: 17–30. [DOI] [PubMed] [Google Scholar]
- 53.Guardabassi L, Dijkshoorn L, Collard JM, Olsen JE, Dalsgaard A. Distribution and in-vitro transfer of tetracycline resistance determinants in clinical and aquatic Acinetobacter strains. J Med Microbiol. 2000;49: 929–936. 10.1099/0022-1317-49-10-929 [DOI] [PubMed] [Google Scholar]
- 54.Choi SM, Kim SH, Kim HJ, Lee DG, Choi JH, Yoo JH et al. Multiplex PCR for the Detection of Genes Encoding Aminoglycoside Modifying Enzymes and Methicillin Resistance among Staphylococcus Species. J Korean Med Sci. 2003;18: 631–636. 10.3346/jkms.2003.18.5.631 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Kim J, Jeon S, Rhie H, Lee B, Park M, Lee H et al. Rapid Detection of Extended-Spectrum β-Lactamase (ESBL) for Enterobacteriaceae by use of a Multiplex PCR-based Method. Infect Chemother. 2009;41: 181–184. [Google Scholar]
- 56.Naas T, Ergani A, Carrër A, Nordmann P. Real-time PCR for detection of NDM-1 carbapenemase genes from spiked stool samples. Antimicrob Agents Chemother. 2011;55: 4038–4043. 10.1128/AAC.01734-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Dallenne C, Costa A, Decré D, Favier C, Arlet G. Development of a set of multiplex PCR assays for the detection of genes encoding important β-lactamases in Enterobacteriaceae. J AntimicrobChemother. 2010;65: 490–495. [DOI] [PubMed] [Google Scholar]
- 58.Anand M, Madhan S, Anil K, Jose H, Dilip M. Phenotypic & molecular characterization of AmpC beta-lactamases among Escherichia coli, Klebsiella spp. &Enterobacter spp. from five Indian Medical Centers. Indian J Med. Res. 2012;135: 359–364. [PMC free article] [PubMed] [Google Scholar]
- 59.Altschul SF, Madden TL, Schäffer AA, Zhang J, Zhang Z, Miller W et al. Gapped BLAST and PSI-BLAST: A new generation of protein database search programs. Nucleic Acids Res. 1997;25: 3389–3402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Tamura K, Peterson D, Peterson N, Stecher G, Nei M, Kumar S. MEGA5: Molecular evolutionary genetics analysis using maximum likelihood, evolutionary distance, and maximum parsimony methods. Mol Biol Evol. 2011;28: 2731–2739. 10.1093/molbev/msr121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Tamura K, Stecher G, Peterson D, Filipski A, Kumar S. MEGA6: Molecular evolutionary genetics analysis version 6.0. Mol Biol Evol. 2013;30: 2725–2729. 10.1093/molbev/mst197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Rajkumar S, Sistla S, Manoharan M, Sugumar M, Nagasundaram N, Parija SC, et al. Prevalence and genetic mechanisms of antimicrobial resistance in Staphylococcus species: a multicentre report of the Indian Council of Medical Research Antimicrobial Resistance Surveillance Network. Indian J Med Microbiol. 2017;35: 53–60. 10.4103/ijmm.IJMM_16_427 [DOI] [PubMed] [Google Scholar]
- 63.Park YS, Yoo S, Seo MR, Kim JY, Cho YK, Pai H. Risk factors and clinical features of infections caused by plasmid-mediated AmpC β-lactamase-producing Enterobacteriaceae. Int J Antimicrob Agents. 2009;34: 38–43. 10.1016/j.ijantimicag.2009.01.009 [DOI] [PubMed] [Google Scholar]
- 64.Sunde M, Norström M. The prevalence of, associations between and conjugal transfer of antibiotic resistance genes in Escherichia coli isolated from Norwegian meat and meat products. J AntimicrobChemother. 2006;58 741–747. [DOI] [PubMed] [Google Scholar]
- 65.Infante B, Grape M, Larsson M, Kristiansson C, Pallecchi L, Rossolini GM et al. Acquired sulphonamide resistance genes in faecal Escherichia coli from healthy children in Bolivia and Peru. Int J Antimicrob. Agents. 2005;25: 308–312. 10.1016/j.ijantimicag.2004.12.004 [DOI] [PubMed] [Google Scholar]
- 66.FreijoP M, Fluit AC, Schmitz FJ, Verhoef J, Jones ME.Many class I integrons comprise distinct stable structures occurring in different species of Enterobacteriaceae isolated from widespread geographic regions in Europe. Antimicrob Agents Chemother. 1999;43: 686–689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Shahi SK and Kumar A. Isolation and Genetic Analysis of Multidrug Resistant Bacteria from Diabetic Foot Ulcers. Front. Microbiol. 2016; 6:1464 10.3389/fmicb.2015.01464 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Jones KE, Patel NG, Levy MA, Storeygard A, Balk D, Gittleman JL et al. Global trends in emerging infectious diseases. Nature. 2008;451: 990–993. 10.1038/nature06536 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Beceiro A, Tomás M, Bou G. Antimicrobial resistance and virulence: A successful or deleterious association in the bacterial world? Clin Microbiol Rev. 2013;26: 185–230. 10.1128/CMR.00059-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Mathers AJ, Peirano G, Pitout JDD. The role of epidemic resistance plasmids and international high- risk clones in the spread of multidrug-resistant Enterobacteriaceae. Clin Microbiol Rev. 2015;28: 565–591. 10.1128/CMR.00116-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Zechiedrich EL, Cozzarelli NR. Roles of topoisomerase IV and DNA gyrAse in DNA unlinking during replication in Escherichia coli. Genes Dev. 1995; 22:2859–2869. [DOI] [PubMed] [Google Scholar]
- 72.Soto SM, Bosch J, Jimenez De Anta MT, Vila J. Comparative study of virulence traits of Escherichia coli clinical isolates causing early and late neonatal sepsis. J ClinMicrobiol. 2008;46: 1123–1125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Lanata CF, Fischer-Walker CL, Olascoaga AC, Torres CX, Aryee MJ, Black RE. Global Causes of Diarrheal Disease Mortality in Children <5 Years of Age: A Systematic Review. PLoS One. 2013;9: e72788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Kotloff KL, Nataro JP, Blackwelder WC, Nasrin D, Farag TH, Panchalingam S et al. Burden and aetiology of diarrhoeal disease in infants and young children in developing countries (the Global Enteric Multicenter Study, GEMS): A prospective, case-control study. Lancet. 2013;382: 209–222. 10.1016/S0140-6736(13)60844-2 [DOI] [PubMed] [Google Scholar]
- 75.Heisig P, Tschorny R. Characterization of fluoroquinolone-resistant mutants of Escherichia coli selected in vitro. Antimicrob Agents Chemother.1994;38: 1284–1291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Ouabdesselam S, Hooper DC, Tankovic J, Soussy CJ. Detection of gyrA and gyrB mutations in quinolone-resistant clinical isolates of Escherichia coli by single-strand conformational polymorphism analysis and determination of levels of resistance conferred by two different single gyrA mutations. Antimicrob Agents Chemother. 1995;39: 1667–1670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Tavío MM, Vila J, Ruiz J, Martín-Sánchez AM, Jiménez de Anta MT. Mechanisms involved in the development of resistance to fluoroquinolones in Escherichia coli isolates. J AntimicrobChemother. 1999;44: 735–742. [DOI] [PubMed] [Google Scholar]
- 78.Sáenz Y, Zarazaga M, Briñas L, Ruiz-Larrea F, Torres C. Mutations in gyrA and parC genes in nalidixic acid-resistant Escherichia coli strains from food products, humans and animals. J AntimicrobChemother. 2003;51: 1001–1005. [DOI] [PubMed] [Google Scholar]
- 79.Yang H, Chen S, White DG, Zhao S, McDermott P, Walker R, Meng J. Characterization of Multiple—Antimicrobial—Resistant Escherichia coli Isolates from Diseased Chickens and Swine in China. J ClinMicrobiol. 2004;42: 3483–3489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Jurado S, Orden JA, Horcajo P, De La Fuente R, Ruiz-Santa-Quiteria JA, Martínez-Pulgarín S. Characterization of fluoroquinolone resistance in Escherichia coli strains from ruminants. J. Vet. Diagn. Invest. 2008;20: 342–345. 10.1177/104063870802000314 [DOI] [PubMed] [Google Scholar]
- 81.Banerjee R, Strahilevitz J, Johnson JR, Nagwekar PP, Schora DM, ShevrinIet et al. Predictors and Molecular Epidemiology of Community-Onset Extended-Spectrum β-Lactamase–Producing Escherichia coli Infection in a Midwestern Community. Infect Control Hosp. Epidemiol. 2013;34: 947–953. 10.1086/671725 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Zerr DM, Qin X, Oron AP, Adler AL, Wolter DJ, Berry JE et al. Pediatric infection and intestinal carriage due to extended-spectrum- cephalosporin-resistant Enterobacteriaceae, Antimicrob. Agents Chemother. 2014;58: 3997–4004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Yaffee AQ, Roser L, Daniels K, Humbaugh K, Brawley R, Thoroughman D et al. Notes from the Field: Verona Integron-Encoded Metallo-Beta-Lactamase–Producing Carbapenem-Resistant Enterobacteriaceae in a Neonatal and Adult Intensive Care Unit—Kentucky, 2015, 2016. https://www.cdc.gov/mmwr/volumes/65/wr/mm6507a5.htm [DOI] [PubMed]
- 84.Baudry PJ, Mataseje L, Zhanel GG, Hoban DJ, Mulvey MR. Characterization of plasmids encoding CMY-2 AmpC β-lactamases from Escherichia coli in Canadian intensive care units. Diagn Microbiol Infect Dis. 2009;65: 379–383. 10.1016/j.diagmicrobio.2009.08.011 [DOI] [PubMed] [Google Scholar]
- 85.Kumarasamy KK, Toleman MA, Walsh TR, Bagaria J, Butt F, Balakrishnan R et al. Emergence of a new antibiotic resistance mechanism in India, Pakistan, and the UK: A molecular, biological, and epidemiological study. Lancet Infect Dis. 2010;10: 597–602. 10.1016/S1473-3099(10)70143-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Riccio ML, Pallecchi L, Fontana R, Rossolini GM. In70 of plasmid pAX22, a blaVIM-1-containing integron carrying a new aminoglycoside phosphotransferase gene cassette. Antimicrob Agents Chemother. 2001;45: 1249–1253. 10.1128/AAC.45.4.1249-1253.2001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Qin X, Zerr DM, Weissman SJ, Englund JA, Denno DM, Klein EJ et al. Prevalence and mechanisms of broad-spectrum β-lactam resistance in Enterobacteriaceae: A children’s hospital experience. Antimicrob Agents Chemother. 2008;52: 3909–3914. 10.1128/AAC.00622-08 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Nordmann P, Poirel L, Toleman MA, Walsh TR. Does broad-spectrum β-lactam resistance due to NDM-1 herald the end of the antibiotic era for treatment of infections caused by Gram-negative bacteria? J AntimicrobChemother. 2011;66: 689–692. [DOI] [PubMed] [Google Scholar]
- 89.Sharma J, Sharma M, Ray P. Detection of TEM & SHV genes in Escherichia coli & Klebsiella pneumoniae isolates in a tertiary care hospital from India. Indian J Med Res. 2010;132: 332–336. [PubMed] [Google Scholar]
- 90.Paterson DL, Bonomo RA. Extended-spectrum beta-lactamases: a clinical update. Clin Microbiol Rev. 2005;18: 657–686. 10.1128/CMR.18.4.657-686.2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Verdet C, Benzerara Y, Gautier V, Adam O, Ould-Hocine Z, Arlet G. Emergence of DHA-1-producing Klebsiella spp. in the Parisian region: genetic organization of the ampC and ampR genes originating from Morganella morganii. Antimicrobial agents and chemotherapy. 2006;50: 607–617. 10.1128/AAC.50.2.607-617.2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Hanson N.D. AmpC β-lactamases: what do we need to know for the future? Journal of Antimicrobial Chemotherapy. 2003;52: 2–4. 10.1093/jac/dkg284 [DOI] [PubMed] [Google Scholar]
- 93.Ruiz J. Mechanisms of resistance to quinolones: target alterations, decreased accumulation and DNA gyrase protection. Journal of Antimicrobial Chemotherapy. 2003;51: 1109–1117. 10.1093/jac/dkg222 [DOI] [PubMed] [Google Scholar]
- 94.Ke X, Gu B, Pan S, Tong M. Epidemiology and molecular mechanism of integron-mediated antibiotic resistance in Shigella. Arch Microbiol. 2011;193:767–774. 10.1007/s00203-011-0744-3 [DOI] [PubMed] [Google Scholar]
- 95.Picard B, Garcia JS, Gouriou S, Duriez P, Brahimi N, Bingen E, et al. The link between phylogeny and virulence in Escherichia coli extraintestinal infection? Infect Immun. 1999;67: 546–553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Johnson JR, Delavari P, Kuskowski M, Stell AL. Phylogenetic Distribution of Extraintestinal Virulence-Associated Traits in Escherichia coli. J Infect Dis. 2001;183: 78–88. 10.1086/317656 [DOI] [PubMed] [Google Scholar]
- 97.Escobar-Paramo P, Grenet K, Le Menac’h A, Rode L, Salgado E, Amorin C et al. Large-Scale Population Structure of Human Commensal Escherichia coli Isolates. Appl Environ Microbiol. 2004;70: 5698–5700. 10.1128/AEM.70.9.5698-5700.2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Bailey JK, Pinyon JL, Anantham S, Hall RM. Distribution of human commensal Escherichia coli phylogenetic groups. JClinMicrobiol. 2010;48: 3455–3456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Duriez P, Clermont O, Bonacorsi S, Bingen E, Chaventré A, Elion J Denamur, et al. Commensal Escherichia coli isolates are phylogenetically distributed among geographically distinct human populations. Microbiology. 2001;147: 1671–1676. 10.1099/00221287-147-6-1671 [DOI] [PubMed] [Google Scholar]
- 100.Li B, Sun JY, Han LZ, Huang XH, Fu Q, Ni YX. Phylogenetic groups and pathogenicity island markers in fecal Escherichia coli isolate from asymptomatic humans in china. Appl Environ Microbiol. 2010;76: 6698–6700. 10.1128/AEM.00707-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Brisse S, Diancourt L, Laouénan C, Vigan M, Caro V, Arlet G et al. Phylogenetic distribution of CTX-M- and non-extended-spectrum-β- lactamase-producing Escherichia coli isolates: Group B2 isolates, except clone ST131, rarely produce CTX-M enzymes. JClinMicrobiol. 2012;50: 2974–2981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Alizade H, Ghanbarpour R, Aflatoonian MR. Virulence genotyping of Escherichia coli isolates from diarrheic and urinary tract infections in relation to phylogeny in southeast of Iran. Trop Biomed. 2014;31: 174–182. [PubMed] [Google Scholar]
- 103.Sidjabat HE, Paterson DL, Qureshi ZA, Adams-haduch JM, Keefe AO, Pascual A. Clinical Features and Molecular Epidemiology of CMY-Type β- Lactamase-Producing Escherichia coli. Clin Infect Dis. 2010;48 739–744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Naseer U, Haldorsen B, Simonsen GS, Sundsfjord A. Sporadic occurrence of CMY-2-producing multidrug-resistant Escherichia coli of ST-complexes 38 and 448, and ST131 in Norway. ClinMicrobiol Infect. 2010;16: 171–178. [DOI] [PubMed] [Google Scholar]
- 105.Oteo J, Cercenado E, Cuevas O, Bautista V. AmpC β -lactamases in Escherichia coli: emergence of CMY-2 –producing virulent phylogroup D isolates belonging mainly to to the international clone O25b –ST131. Diagn Microbiol Infect Dis. 2010;67: 270–276. 10.1016/j.diagmicrobio.2010.02.008 [DOI] [PubMed] [Google Scholar]
- 106.Matsumura Y, Nagao M, Iguchi M, Yagi T, Komori T, Fujita N et al. Molecular and clinical characterization of plasmid-mediated AmpC β-lactamase-producing Escherichia coli bacteraemia: A comparison with extended-spectrum β-lactamase-producing and non-resistant E. coli bacteraemia. ClinMicrobiol Infect. 2013;19: 161–168. [DOI] [PubMed] [Google Scholar]
- 107.Coque TM, Novais A, Carattoli A, Poirel L, Pitout J, Peixe J et al. Dissemination of clonally related Escherichia coli strains expressing extended-spectrum beta-lactamase CTX-M-15. Emerg Infect Dis. 2008;14: 195–200. 10.3201/eid1402.070350 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Hansen F, Olsen SS, Heltberg O, Justesen US, Fuglsang-damgaard D, Knudsen JD et al. Characterization of Third-Generation Bloodstream Infections in Denmark. 2014;20: 316–324. [DOI] [PubMed] [Google Scholar]
- 109.Van Der Bij AK, Peirano G, Goessens WHF, Van Der Vorm ER, Van Westreenen M, et al. Clinical and molecular characteristics of extended-spectrum-β- lactamase-producing Escherichia coli causing bacteremia in the Rotterdam Area, Netherlands, Antimicrob. Agents Chemother. 2011;55: 3576–3578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Oteo J, Diestra K, Juan C, Bautista V, Novais A, Pérez-Vázquez M, et al. Extended-spectrum β-lactamase-producing Escherichia coli in Spain belong to a large variety of multilocus sequence typing types, including ST10 complex/A, ST23 complex/A and ST131/B2. Int J Antimicrob Agents. 2009;34: 173–176. 10.1016/j.ijantimicag.2009.03.006 [DOI] [PubMed] [Google Scholar]
- 111.Valverde A, Turrientes MC, Norman F, San Martín E, Moreno L, Pérez-Molina JA et al. CTX-M-15-non-ST131 Escherichia coli isolates are mainly responsible of faecal carriage with ESBL-producing Enterobacteriaceae in travellers, immigrants and those visiting friends and relatives. Clin Microbiol Infect. 2015;21: 252.e1–252.e4. [DOI] [PubMed] [Google Scholar]
- 112.Mushtaq S, Irfan S, Sarma JB, Doumith M, Pike R, Pitout J et al. Phylogenetic diversity of Escherichia coli strains producing NDM-type carbapenemases. JAntimicrobChemother. 2011;66: 2002–2005. [DOI] [PubMed] [Google Scholar]
- 113.Pfeifer Y, Witte W, Holfelder M, Busch J, Nordmann P, Poirel L. NDM-1-producing Escherichia coli in Germany. Antimicrob Agents Chemother. 2011;55: 1318–1319. 10.1128/AAC.01585-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Pallecchi L, Bartoloni A, Fiorelli C, Mantella A, Di Maggio T, Gamboa H et al. Rapid dissemination and diversity of CTX-M extended-spectrum β-lactamase genes in commensal Escherichia coli isolates from healthy children from low-resource settings in Latin America. Antimicrob Agents Chemother. 2007;51: 2720–2725. 10.1128/AAC.00026-07 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Smillie CS, Smith MB, Friedman J, Cordero OX, David LA, Alm EJ. Ecology drives a global network of gene exchange connecting the human microbiome. Nature. 2011;480: 241–244. ( 10.1038/nature10571) [DOI] [PubMed] [Google Scholar]
- 116.Forslund K, Sunagawa S, Kultima JR, Mende DR, Arumugam M, Typas A, Bork P. Country specific antibiotic use practices impact the human gut resistome. Genome Res. 2013; 23: 1163–1169. ( 10.1101/gr.155465.113) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Hu Y, Yang X, Qin J, Lu N, Cheng G, Wu N, et al. Metagenome-wide analysis of antibiotic resistance genes in a large cohort of human gut microbiota. Nat. Commun. 2013; 4: 2151 ( 10.1038/ncomms3151) [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The data used to create this figure can be accessed at the Center for Disease Dynamics, Economics & Policy (CDDEP) Resistance Map website at http://resistancemap.cddep.org/resmap/c/in/India.
(PDF)
(PDF)
(PDF)
Data Availability Statement
All relevant data are within the manuscript and its Supporting Information files.