Abstract
Migration has been hypothesised to be selective on health but this healthy migrant hypothesis has generally been tested at destinations, and for only one type of flow, from deprived to better-off areas. The circulatory nature of migration is rarely accounted for. This study examines the relationship between different types of internal migration and adult mortality in Health and Demographic Surveillance System (HDSS) populations in West, East, and Southern Africa, and asks how the processes of selection, adaptation and propagation explain the migration-mortality relationship experienced in these contexts. The paper uses longitudinal data representing approximately 900 000 adults living in nine sub-Saharan African HDSS sites of the INDEPTH Network. Event History Analysis techniques are employed to examine the relationship between all-cause mortality and migration status, over periods ranging from 3 to 14 years for a total of nearly 4.5 million person-years. The study confirms the importance of migration in explaining variation in mortality, and the diversity of the migration-mortality relationship over a range of rural and urban local areas in the three African regions. The results confirm that the pattern of migration-mortality relationship is not exclusively explained by selection but also by propagation and adaptation. Consequences for public health policy are drawn.
Keywords: Internal migration, Sub-Saharan Africa, Mortality, Health and demographic surveillance system, INDEPTH network
1. Introduction
Internal migration, understood as a change in usual residence within a country, is a much more common event than other demographic phenomena such as death or birth, especially with secular fertility decline. In the mid-2000s, the median Aggregate Crude Migration Intensity (ACMI), a measure of all permanent changes of address within a country, was 7.5% for 1-year period in a range of 45 countries around the world (Bell et al., 2015), and this excludes international migrations which are estimated at only 0.12% a year, i.e. 60 times less than internal migration (Abel and Sander, 2014). To give a sense of scale, the world crude birth rate was only 2% a year and the world crude death rate less than 1% (United Nations Population Division, 2014). Across the 45 selected countries for which data were available, only four had an 1-year ACMI smaller than 2% (Bell et al., 2015).
Migration is not only a major demographic event, but it also has the potential to influence other demographic events. In this paper, we investigate the relationship between internal migration and health, using mortality as major indicator of health. This relationship is important because health status may both impede and stimulate migration, while migration, often motivated by economic benefits, can result in negative health outcomes, possibly leading to death (Gerritsen et al., 2013). Although studies abound on mortality and to a lesser extent on migration, their relationship has been far less investigated. Where the migration-mortality relationship has been investigated, international migration has been the focus, notably to explain the “Latino paradox” whereby migrants from Latin America have demonstrated a survival advantage in USA despite their lower socio-economic status (Abraído-Lanza et al., 1999). This paradox may or may not present in the same way in the case of internal migration but, any effect of this relationship would likely have a much higher impact on survival since internal migration is experienced by almost every person over their lifetime (Abel and Sander, 2014; Bell et al., 2015).
In this paper, we revisit the theory about the migration-mortality relationship, accounting for different types of migration flow and for the level of health risk in origin and destination areas. Using information collected on migration status and duration of residence, we design a method to identify a set of hypotheses attached to the migration-mortality relationship, and apply this method to interpreting data collected in nine district populations located in West, East, and Southern Africa that present different patterns of mortality and migration. By identifying the most likely explanation for the divergent patterns seen in these different settings, we aim to better identify the categories of migrants at higher risks, in order to identify the target populations for local health interventions.
2. Literature review
The migration-mortality relationship is not foreign to the broader issue of epidemiological transition. Rather than review the role of migration in this transition, this section will build on previous reviews on the subject (Collinson et al., 2014). In the context of low- and middle-income countries (LMICs), the health transition has been at the same time spectacular in its speed and more heterogeneous than in higher-income countries (HICs) (Salomon and Murray, 2002). The transition has led to a general decline in mortality but also, particularly in African countries, to a double burden of disease characterised by the emergence of non-communicable diseases (NCDs) and life-style diseases associated with urbanisation (Ezzati et al., 2005). These coexist with persistent, new and revitalised diseases, such as malaria, HIV/AIDS and TB (Boutayeb, 2006). This double burden runs counter to mortality decline. Whereas urbanisation has generally contributed positively to health in the past, there are concerns that under conditions of slow economic development and weak infrastructure management it could actually drive an increase in cardio-vascular disease (CVD) (Yusuf et al., 2001) as well as in respiratory and diarrheal diseases linked to poor environmental conditions (Harpham, 2009).
Migration plays an important role in sustaining livelihoods in LMIC countries. As people migrate, remittances and information circulate and help to maintain links between sending and receiving communities (White and Lindstrom, 2006). However, migration may improve well-being and at the same time expose migrants to health risks. With respect to mortality, it is not clear whether the net effect of migration is positive or negative, and in which circumstances. Considering the sheer volume of migration and its high sensitivity to livelihood conditions, it is necessary to carefully examine the hypotheses relating to migration and health (for references and glossary of terms used in migrant and health analysis, see Urquia and Gagnon, 2011).
The first and most-utilised hypothesis concerning migration and health is the “healthy (im)migrant” hypothesis. This hypothesis proposes that migrants are selected in their place of origin amongst the more healthy since they must prepare to adapt to their new place of residence. Positive selection on health would then operate through migration. In ordinary migration, because of a high selection effect at origin, the health of migrants can actually be better than that of non-migrants at the destination location. This selection effect could explain the epidemiological paradox that even if originating from places with high health risks, migrants may have better health than the non-migrants in destination areas living in superior (health) conditions (Urquia and Gagnon, 2011).
This would apply provided that the migration conditions are not too stringent, as may be the case for refugees and internally displaced people. The possible effect of the migration conditions is called the disruption effect and is usually attributed to the conditions around the time of migration (just before and just after, the specific time span to be defined by the migration itself). This effect has been particularly studied for reproductive health (Choi, 2014; Goldstein, 1973; Hervitz, 1985; Kulu and Steele, 2013).
The migrants’ health may gradually converge to that of nonmigrants following exposure after migration at the destination. This adaptation effect (also named assimilation effect) is observed over time, i.e. with duration of residence, and can only present if there is a difference between the health of non-migrants and the health of migrants just after their arrival. It is often presented as a loss of (negative or positive) selection effect over time (Urquia and Gagnon, 2011).
Lastly, one cannot exclude that the migration may have no effect at all on the migrant’s health. The health conditions acquired in the place of origin could persist after migration. This is the socialisation effect whereby conditions and behaviours acquired at the place of origin, in particular during childhood, persist in later life whatever the new environment the migrant is exposed to (Kulu, 2005). Adaptation effect may still exist but may not be sufficient to counterbalance the socialisation effect, i.e. the persisting effect of exposure prior to migration. The two effects, adaptation and socialisation, are therefore opposed.
Research into the migration-health relationship often seeks to verify these four effects through empirical analysis. In the remainder of this paper we will refer to the SoSAD hypotheses to discuss the hypotheses that verify Socialisation, Selection, Adaptation and Disruption effects. To note, the SoSAD hypotheses do not only apply to the study of diseases but have been extensively used since the 1960s to analyse reproductive health in relation to migration.
The SoSAD hypotheses have been associated with migration flows from less to more affluent areas, generally from rural to urban areas. These are the most common internal migration flows generally experienced by youth at the beginning of their working lives. Other flows have sometimes been considered and these have prompted the alternative “unhealthy return migrant” hypothesis, i.e. that of negative selection on health. For example, studies in South Africa have shown that prominently rural sending areas experience an excess mortality due to people ‘returning home to die’ (Clark et al., 2007; Collinson et al., 2009). The assumption is that new migrants will be attracted to places with better economic opportunities and living conditions, generally in urban areas, but that some migrants may partake in high risk behaviour (smoking, drinking, unhealthy diets, risky sexual encounters, violence) and may have difficulty accessing health services in these destinations, in particular if they reside in slums. This phenomenon is referred to as the segmented adaptation effect. As a consequence, the migrants will return to their place of origin when their health deteriorates to seek health care and support, thus contributing to higher mortality in rural areas. This return migration is also called the “midnight train” effect after a soul song by this name that tells about a failed musician in Los Angeles who takes the midnight train back to Georgia, his place of origin (Nauman et al., 2015). This return of unhealthy migrants creates the so-called “salmon bias” that leaves the healthier at destinations (Abraído-Lanza et al., 1999; Lu and Qin, 2014).
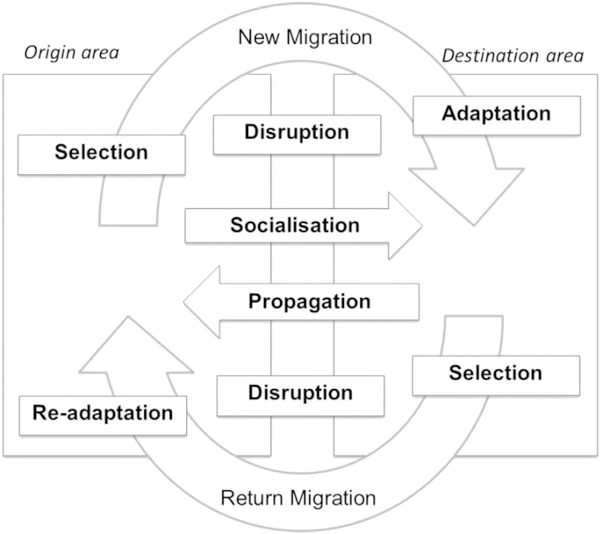
The SoSAD hypotheses are usually intended for new (first-time) migration, but may apply equally to return migration, although not necessarily with the same effect on health. So, it is important to look at bi-directional migration flows between origin and destination areas. For simplicity, we present in Fig. 1 the SoSAD hypotheses for two main migration flows, new migration and return migration. The selection and disruption hypotheses are generally synonymous whatever the direction of migration. However, the equivalent of socialisation, which refers mainly to behaviours and health conditions acquired during childhood, differs in the case of return migration, i.e. after the migrant spent some time at destination. We will refer to the propagation effect as the symmetrical effect to socialisation. This propagation (or diffusion) effect is conditional on adaptation to the place of destination and identifies the possibility that behaviour and health conditions at destinations can be spread to origin areas through return migration. After return migration, the migrant may re-adapt to its origin area, hence the readaptation effect.
Fig. 1.
Interaction between migration and health before and after new migration or return migration.
There is an ambiguity with regards to the interplay between the environment and the behaviour of the migrants. For example, one may consider the exposure to a specific environment as fairly homogenous, while migrants may have different behaviours (segmented adaptation) that lead to negative selection by return migration or to positive selection through permanent settlement in the host area. The alternative explanation is that the environment is heterogeneous, exposing migrants to different risks depending on where they reside, while migrants may be uniformly positively selected through migration.
3. Interpreting migration-mortality relationship in local context
3.1. Why migration matters for monitoring health at local level
Districts are often highly affected by changes in migration trends, depending on the local economic context and on the larger regional, national, or even international environment. The migratory balance can change sign from one year to the next. Epidemiological changes usually occur at a slower pace but may be dramatically affected by migration trends. A health district officer may therefore see unexpected changes in the prevalence of mortality that do not necessarily relate to local health determinants and policy. Comparing local death statistics with regional or national estimates might not be very helpful for this district officer if she cannot attribute changes to either local or larger context. However, with simple variables on migration status and duration of exposure in and out of the district, the methodological framework proposed below will help her to identify selection, adaptation and propagation effects that might drive local public health policy towards the correct targets.
Monitoring local mortality trends can be achieved through regular vital statistics when available, i.e. in developed countries, or with a health and demographic surveillance system (HDSS) circumscribed to a local area in the case of LMICs. HDSSs have been developed in areas, usually the size of an administrative district, where population vital registration is absent or weak. The HDSS platform generates prospective, longitudinal data on demographic and health dynamics and captures all vital events such as births, death and in- or out-migrations within the surveillance population. The HDSS begins with a baseline census of the full population and subsequently tracking of individual’s demographic events, on an on-going basis, at prescribed intervals within the study population (see Sankoh and Byass, 2012 for more details of the HDSS methodology).
3.2. Identifying selection and exposure effects
Although HDSS platforms offer detailed longitudinal data on demographic events, information is usually lacking on the exact circumstances surrounding the in- and out-migration, as well as detail concerning the risk exposure outside of the surveillance area. However, migration status and duration of exposure can be precisely identified for each individual during the observation period in the surveillance area. This is possible since in-migration (of both new and return migrants) and out-migration is captured in prospective, longitudinal datasets that are regularly updated. Table 1 will be used to classify the expected differences in mortality risk between non-migrants (the reference category), new in-migrants, and return migrants, depending on short or longer exposure in the HDSS, as well as longer exposure outside the HDSS in the case of return migrants. Table 1 also presents the three expected effects of propagation/socialisation, selection and adaptation/re-adaptation, evaluated net of one another.
Table 1.
Expected mortality differences between migrants and non-migrants for different combinations of selection and exposure effects.
| (1) | (2) | (3) | (4) | (5) | (6) | (7) | (8) | (9) | (10) | (11) | (12) | (13) | (14) | (15) | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Case of return migrants | |||||||||||||||
| Expected difference in mortality risk between return migrants and non-migrants: | |||||||||||||||
| Short exposure in | > | > | > | > | > | > | = | = | = | < | < | < | < | < | < |
| Long exposure in | = | > | = | > | = | > | = | = | = | = | < | = | < | = | < |
| Long exposure outside | = | = | < | < | > | > | = | < | > | = | = | < | < | > | > |
| Selection effect | neg | neg | neg | neg | neg | neg | none | none | none | pos | pos | pos | pos | pos | pos |
| Re-adaptation effect (i.e. convergence with non-migrants) | yes | no | yes | no | yes | no | n.t. | n.t. | n.t. | yes | no | yes | no | yes | no |
| Propagation effect (i.e. origin conditions persist at destination) | no | no | pos | pos | neg | neg | no | pos | neg | no | no | pos | pos | neg | neg |
| Case of new migrants | |||||||||||||||
| Assumed difference in health risks exposure before (B) and after (A) migration | B = A | B = A | B < A | B < A | B > A | B > A | B=A | B < A | B > A | B=A | B = A | B<A | B < A | B > A | B > A |
| Expected difference in mortality risk after migration between new migrants and non-migrants: | |||||||||||||||
| Short exposure in | > | > | = | = | ≫ | ≫ | = | < | > | < | < | ≪ | ≪ | = | = |
| Long exposure in | = | > | < | = | > | ≫ | = | < | > | = | < | < | ≪ | > | = |
| Selection effect | neg | neg | neg | neg | neg | neg | none | none | none | pos | pos | pos | pos | pos | pos |
| Inferred adaptation effect (i.e. convergence with non-migrants) | yes | no | yes | no | yes | no | n.t. | n.t. | n.t. | yes | no | yes | no | yes | no |
| Inferred socialisation effect (i.e. persistence of exposure B) | no | no | pos | pos | neg | neg | no | pos | neg | no | no | pos | pos | neg | neg |
n.t.: not testable. pos: positive. neg: negative. In bold: assumption of no difference in health risks before and after migration in rural areas.
In the absence of direct information on the selection process and on health risks exposure before and after migration, the table identifies all possible combinations of selection effect amongst migrants. Each combination of selection and exposure effects generates a particular set of relative risks. Table 1 identifies every possible combination of relative mortality risk whose direction can be negative, positive or equal to that of nonmigrants.
The length of exposure (short or long) before and after a migration is important to establish the direction or presence of the effects of propagation, and (re-)adaptation. For return migrants, we can control for the exposure out of the site before return migration, in addition to short- and long-term exposure in the site after return migration. For new migrants, we control the exposure in the site following entry by migration. The only SoSAD hypothesis concerning mortality that we cannot test is that of disruption, because we cannot measure mortality before and after migration for the same individuals. Therefore, Table 1 does not include the disruption hypothesis depicted in Fig. 1.
The respective effects of selection, adaptation and propagation are easier to understand for return migrants. The propagation effect is determined on the basis of a “long exposure out”, i.e. the health risks brought about by exposure in the location before return migration, while the selection effect is determined after return migration and is expressed as the difference in mortality between return migrants and non-migrants in the location. This selection effect can be ascertained shortly after the migration event (i.e.: following a “short exposure in”) and it is established by examining the differences in mortality risk between return migrants and non-migrants in the population. The re-adaptation effect is ascertained after a longer duration following the migration event (the effect of “long exposure in”). This effect is established by examining whether mortality of return migrants has gradually converged to that of non-migrants.
For new migrants to the HDSS, the effect of adaptation and selection are the same as in the case of return migration. However, since we do not have information on the exposure before the new migration, captured as the socialisation effect, we have to consider the possible differences in health risk exposure before and after the migration. We use these to infer a socialisation effect which we view as being synonymous to the propagation effect in return migrants.
3.3. Interpreting results
As explained above, Table 1 shows the expected direction of the relationship between migrants and non-migrants with respect to mortality risk when different situations obtain. Any of the theoretical premises described above can be present and this table provides an interpretative device that indicates which theoretical premise, or combinations thereof, would be most likely to provide the observed results. More description is given below for return migrants and for new in-migrants.
3.3.1. For return migrants
Columns 1–6 present the possible combinations of exposure effects that may be present where return migrants are negatively selected on health. Negative selection is identified when a return migrant’s risk of mortality, following a short exposure in the HDSS, is greater than that of a permanent resident. This is attributed to conditions acquired at the migration destination. Following a longer exposure in the HDSS, the risk of mortality for return migrants might remain higher or might converge to the same risk as that of the permanent residents. This re-adaptation effect is deemed either negative or positive accordingly. For return migrants, the relative risk of mortality following a long exposure outside the HDSS can be contrasted with the risk of mortality following an exposure outside the HDSS of shorter duration. Following a longer exposure outside the HDSS, the risk of mortality amongst return migrants may be the same, greater than or less than that of return migrants with a shorter outside exposure. This is the propagation effect that would be deemed ‘not present’, ‘positive’ or ‘negative’ accordingly.
Columns 7–9 present the possible combinations of effects where no selection is identified (i.e. the mortality risk of return migrants with a short exposure in the HDSS equal to the mortality risk of permanent residents in the HDSS). In the case of no selection effect, the re-adaptation effect is not testable by definition. The effect of long versus short exposure outside the HDSS for return migrants is determined in the same way as previously. Longer versus shorter exposure may result in mortality risk that is equal, less than or greater than permanent residents, and the propagation effect determined as ‘no effect’, ‘positive effect’ or ‘negative effect’.
The final set of expected combinations for return migrants are presented in Columns 10–15. These relate to the instances where return migrants are positively selected on health (i.e. their risk of mortality following a short exposure in the HDSS is lower than that of the permanent residents). After a longer exposure in the HDSS, the risk of mortality may either converge to, or remain lower than, that of the permanent residents. Re-adaptation is present only in the case of the risk following a longer exposure in the HDSS being equal to that of permanent residents (i.e. where the risk of mortality remains lower amongst return migrants, re-adaptation is assumed to not have taken place). The propagation effect is determined in the same way as described for other cases.
3.3.2. For new in-migrants
The above approach differs in the case of new (in-)migrants to the HDSS, because the exposure prior to entering the HDSS is long and its effect cannot be measured directly. Therefore, only the effect of short and long exposure following migration into the HDSS is available to identify the three hypotheses for in-migrants. The interpretation of exposure in the site is conditional on knowledge of the difference in health risks before migration (labelled ‘B’) and after migration (labelled ‘A’). The expected direction of the difference in health risks before and after migration for new migrants is the same as the effect of long exposure outside for return migrants. Therefore, for in-migrants, both the “short exposure in” and “long exposure in” effects are the compound of the selection effect and the difference in health risks before and after migration i.e. the selection and adaptation effects are not discriminated from the socialisation effect.
Where health environments are assumed equal (i.e. B = A), there is no expected socialisation effect and the effect of short and long exposure in the HDSS site on health risk is the same as that described for return migrants. Where migrants are negatively selected on health (columns 1 and 2), their risk of mortality following a short exposure in the HDSS is expected to be greater than that of permanent residents. After a long exposure in the HDSS, a migrant’s mortality risk may converge to that of permanent residents or remain higher (corresponding to a presence or absence of adaptation effect). Where no selection effect is present (column 7), a short or long exposure in the HDSS predicts no differences in mortality risk between in-migrants and permanent residents, and adaptation is not testable. In the case of positive selection (columns 10 and 11), the mortality risk amongst in-migrants can be expected to be lower than the resident population following a short exposure in the HDSS. Following a longer exposure the mortality risk is expected to converge to that of the resident population (an adaptation effect) or remain lower (no adaptation effect).
Where the environment before migration carries lower mortality risks than the destination environment (i.e. B < A), a positive socialisation effect can be inferred. In cases where the selection effect of new in-migrants is negative (columns 3 and 4) the mortality risk of in-migrants after a short exposure in the HDSS will equate to that of permanent residents, i.e. the effects of a better prior health environment and negative selection will equalise the risk. A longer exposure can result in either equal mortality risks across both groups (where no adaptation effect is inferred) or lower mortality risk amongst the in-migrant group (where adaptation is assumed to have cancelled out the selection effect leaving the environment effect only). In cases of no selection (column 8), the migrant’s better health environment before migration creates a lower mortality risk for in-migrants following a short and long exposure in the HDSS compared to permanent residents and the adaptation effect is not testable. Where in-migrants are positively selected on health, and the prior health environment is better (columns 12 and 13), the mortality risks following a short and long exposure in the HDSS will be lower than the resident population. However, where the degree/magnitude of risk following a longer exposure is reduced an adaptation effect can be inferred (column 12).
Finally, if the health environment prior to migration carries higher mortality risks than the destination environment (i.e., B > A), a negative socialisation effect is inferred. Where this is coupled with negative selection (columns 5 and 6), the mortality risk amongst migrants following both a short and a long exposure in the HDSS will be higher than for the resident population. Where the degree/magnitude of higher risk is reduced over time, an adaptation effect may be inferred (column 5). In the case of no selection effect amongst in-migrants (column 9), the mortality risks relative to permanent residents of the HDSS will be higher after both a short and a long exposure in the HDSS, and the adaptation effect is not testable. In the case of a positive selection effect amongst in-migrants, the relative mortality risk amongst migrants is assumed to be equal following a short exposure in the HDSS, i.e. the effects of a worse prior health environment and positive selection will even out the risk. The mortality risk will either remain equal following a migrant’s longer exposure in the HDSS, in which case no adaptation effect is inferred, or migrants’ mortality risks may be higher than the resident population, in which case adaptation is assumed to have cancelled out the selection effect leaving the environment effect only.
3.4. Limits to interpretation
It is reasonable to assume that in relation to rural HDSSs, new migrants generally come from neighbouring areas with the same level of health risks as the HDSS area. In this case, the assumption of no difference in health risks before and after migration (i.e. B = A), is sensible. The combination of selection and adaptation hypotheses can thus be uniquely identified in columns 1, 2, 7, 10, and 11. However, in urban areas, the assumption is less valid because new migrants may come either from rural areas or from urban areas, which are very heterogeneous. Consequently health risks exposure may be higher before migration (B > A), risks may be equal (B = A), or health risks exposure may be lower prior to migration (B < A).
The literature on new migration (Urquia and Gagnon, 2011) has largely assumed the combination of positive selection of migrants (healthy migrant hypothesis) moving to better-off areas from areas with adverse health conditions (negative socialisation hypothesis) and integrating after some time to become undistinguishable from non-migrants (convergence hypothesis) (column 14). Return migration is assumed to be associated with positive propagation effect, re-adaptation and negative selection in the “midnight train” case (column 3) or with positive selection in the opposite case (column 12). However, there are potentially twelve other combinations, when one considers the possibilities of no selection effect, no socialisation/propagation, and no (re-)adaptation (as outlined in Table 1). The observed patterns are expected to be much more diverse than those in the literature.
It is possible that the migration-mortality relationships are not only generated by the combination of selection and exposure, but also by other processes unaddressed, and therefore uncontrolled for in this paper. In addition, Table 1 only indicates the direction of the effects, not their magnitude. Any departure from the proposed patterns in Table 1 will be interpreted as a failure to explain the migration-mortality relationships with selection and exposure effects using the proposed theoretical framework.
Consequently, the specific objectives of the study are as follows:
To confirm the diversity of the migration-mortality relationships over a range of countries and residence types in Western, Eastern and Southern parts of Africa;
To confirm that the pattern of migration-mortality relationships is mainly generated by the combination of three processes: selection, adaptation, and socialisation/propagation;
To identify the most likely explanation for the patterns of mortality in contexts characterised by high mobility, and to check whether they conform to the well-known healthy migrant and unhealthy return migrant hypotheses;
To help local health authorities to identify the categories of migrants for targeted interventions.
4. Data and methods
4.1. Study population
The paper uses data from nine HDSS sites that are members of the International Network for the Demographic Evaluation of Populations and Their Health (INDEPTH). The INDEPTH network brings together HDSS member centres located in LMICs, and provides a streamlined, standardised approach to addressing health-related research questions using the HDSS platform (for more details concerning the methods and objectives of the INDEPTH organisation see Sankoh and Byass, 2012). The HDSS sites included in this study are located in four sub-Saharan African countries in the Western, Eastern and Southern regions of the continent, and they represent a mix of settlement types across the urban rural continuum. The sites are Nanoro, Nouna and Ouagadougou in Burkina Faso; Kilifi, Kisumu and Nairobi in Kenya; Manhiςa in Mozambique; Agincourt and Africa Centre in South Africa. To note, the present study does not aim to cover all existing situations on the continent, nor does it pretend to be representative. The situations are as illustrative as they can be considering the available data. Our hope is that these situations are diverse enough to inspire the analysis of other health issues in local areas where migration is important.
The HDSS sites included in this study were selected to present a set of illustrative contexts across the Western, Eastern and Southern regions of the continent and comprised those sites that met the eligibility criteria for participation in the study. These sites represent one or more sub-district populations of their countries, in relation to which a detailed examination of migration and mortality dynamics across different contexts can be conducted. This study follows from an investigation of the patterns of migration by age and sex and an exploration of education as a determinant of migration in these HDSS populations (see Ginsburg et al., 2016). Exhaustive migration and mortality data are collected through a standardised system of continuous registration of events (Sankoh and Byass, 2012). Internal and external consistency checks were performed on dates, order of events, frequency of events, rates, etc. Data from all sites were processed using the same procedures thus ensuring strict comparability from data collection to data analysis. The characteristics of the HDSS sites included in the study are outlined in Table 2 with respect to migration-related characteristics of the analytical sample and in Appendix 1 for other variables. Seven of the sites are rural or mostly rural, while the Nairobi HDSS and the Ouagadougou HDSS, comprising non-contiguous areas, are urban.
Table 2.
Migration-related characteristics of the analytical sample by HDSS site over the respective analysis periods.
| Nanoro HDSS |
Nouna HDSS |
Ouagadougou HDSS |
Kilifi HDSS |
Kisumu HDSS |
Nairobi HDSS |
Africa centre HDSS |
Agincourt HDSS |
Manhiςa HDSS |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| % Person years |
% Person years |
% Person years |
% Person years |
% Person years |
% Person years |
% Person years |
% Person years |
% Person years |
||||||||||
| Male | Female | Male | Female | Male | Female | Male | Female | Male | Female | Male | Female | Male | Female | Male | Female | Male | Female | |
| Permanent Resident | 32,179 | 53,491 | 168,474 | 144,158 | 58,798 | 56,165 | 318,513 | 412,786 | 294,542 | 360,534 | 86,579 | 56,708 | 118,221 | 172,872 | 100,591 | 146,649 | 99,371 | 180,212 |
| 87% | 87% | 67% | 57% | 84% | 81% | 57% | 57% | 75% | 75% | 44% | 41% | 66% | 69% | 56% | 53% | 58% | 67% | |
| In-migrant | ||||||||||||||||||
| 6 – 24 months in HDSS | 3422 | 6163 | 18 244 | 29 353 | 8771 | 9941 | 77.490 | 95,949 | 26,746 | 39,179 | 43,899 | 32,375 | 13,353 | 16,774 | 15,845 | 31,433 | 13,070 | 16,352 |
| 9% | 10% | 7% | 12% | 12% | 14% | 14% | 13% | 7% | 8% | 22% | 24% | 7% | 7% | 9% | 11% | 8% | 6% | |
| 25 – 59 months in HDSS | 1208 | 2152 | 23,245 | 36,835 | 2843 | 3215 | 77,762 | 102,454 | 27,287 | 35,804 | 34,295 | 24,273 | 15,060 | 19,870 | 21,935 | 42,405 | 16,287 | 20,589 |
| 3% | 3% | 9% | 15% | 4% | 5% | 14% | 14% | 7% | 7% | 17% | 18% | 8% | 8% | 12% | 15% | 10% | 8% | |
| 60 + months in HDSS | n.a. | n.a. | 19,171 | 28,895 | n.a. | n.a. | 48,866 | 71,873 | 12,555 | 14,781 | 12,177 | 8730 | 11,388 | 15,922 | 24,304 | 42,167 | 13,359 | 17,842 |
| 8% | 11% | 9% | 10% | 3% | 3% | 6% | 6% | 6% | 6% | 13% | 15% | 8% | 7% | |||||
| Return migrant | ||||||||||||||||||
| 6 – 24 months in HDSS | n.a. | n.a. | 7356 | 4710 | n.a. | n.a. | 17,693 | 18,773 | 15,197 | 15,733 | 9027 | 6665 | 9295 | 10,658 | 6966 | 4759 | 10 901 | 12 258 |
| 3% | 2% | 3% | 3% | 4% | 3% | 5% | 5% | 5% | 4% | 4% | 2% | 6% | 5% | |||||
| 25 – 59 months in HDSS | n.a. | n.a. | 9232 | 4989 | n.a. | n.a. | 13,919 | 15 409 | 13 692 | 13 172 | 8348 | 6037 | 8457 | 10 464 | 6615 | 4808 | 11,552 | 14,286 |
| 4% | 2% | 2% | 2% | 3% | 3% | 4% | 4% | 5% | 4% | 4% | 2% | 7% | 5% | |||||
| 60 + months in HDSS | n.a. | n.a. | 6262 | 3244 | n.a. | n.a. | 3658 | 4920 | 3902 | 3733 | 2922 | 2173 | 3559 | 4855 | 4563 | 3435 | 6714 | 9148 |
| 2% | 1% | 1% | 1% | 1% | 1% | 1% | 2% | 2% | 2% | 3% | 1% | 4% | 3% | |||||
| Exposure 36 + months for return migrants only | n.a. | n.a. | 5979 | 3668 | n.a. | n.a. | 9752 | 8738 | 5282 | 4666 | 2299 | 1485 | 5039 | 5602 | 11,470 | 6777 | 6741 | 7265 |
| 2% | 1% | 2% | 1% | 1% | 1% | 1% | 1% | 3% | 2% | 6% | 2% | 4% | 3% | |||||
4.2. Data and variables
As part of the routine HDSS data collection activities, conducted at least once, on average twice a year, reliable dates of all events representing entry into, or exit from households within the geographical boundaries of the HDSS are gathered. These events include enumeration at the inception of the HDSS (through a baseline census or subsequent expansion of the study area), births, deaths, in-migration, out-migration, internal moves (i.e. moves within the boundaries of the study area involving changes of residence from one household to another), and end of observation (an event signalling the last round of reliable data collection). In an HDSS each and every individual that has once been documented as a resident can be traced from any entry event (enumeration, birth, in-migration) to any exit event (death, out-migration, end of observation) allowing the construction of complete migratory histories from first entry event to last exit event. Individuals can exit and re-enter the HDSS as they are traced with a unique identifier. Standard statistical techniques can now easily handle left-censoring and observation gaps.
In this study, the focus is on migration events that involve the crossing the geographical boundaries of the HDSS site (in either an inward or an outward direction). Moves that are internal to the HDSS are excluded from the migration definition, as are moves that take place between areas outside of the boundaries of the HDSS. Across HDSS sites, definitions of in- and out-migration may differ in relation to the time threshold used to determine HDSS membership (varying from 3 to 6 months of residence within the boundaries of the HDSS). In this study, a consistent residency threshold of 6 months was selected to determine residency across all HDSS sites. A new in-migrant is an individual who has entered and resided in the HDSS area for at least 6 months, while an out-migrant is a resident who moved away from the HDSS area for at least 6 months. For both new in-migrants and return migrants, exposure time following entry into the HDSS is categorised into durations of 6–24 months; 25–59 months and 60 + months. Return migrant exposure outside the HDSS discriminates between long exposure (taken at >36 months) and short exposure (<36 months).
4.3. Statistical analysis
The study uses Event History Analysis (EHA) techniques to analyse the relationship between migration and mortality. This technique requires that the data be checked for consistency and transformed into a biographical “residency episode” structure (Gerritsen et al., 2013). This structure implies that all events (such as births, deaths, in- and out-migration) for individuals are recorded sequentially with dates attached to each event. The models treat time continuously and allow for the analysis of repeatable migration events per individual. The analyses presented in this paper are based on data starting in 1998 or the earliest reliable year for migration analysis until 2012 (see Appendix 2 for the different periods covered for each site).
Cox semi-parametric proportional hazards models were produced for each site to examine in-migration and return migration status as a determinant of death. These models control for age in the non-parametric part of the Cox model, and migration status, grouped calendar years and education as covariates. Models were stratified by sex to control for gender compositional effects. All analyses were performed using Stata version 14.
5. Results
5.1. Descriptive results
The rates of out-migration by site were analysed and reported on in a previous study (see Ginsburg et al., 2016). Across the same group of HDSS sites, between 7 and 21 per 100 PYAR of these HDSS populations were found to have out-migrated between years 2009–2011, while between 7 and 27 per 100 PYAR of individuals in-migrated over this period. Both in- and out-migration rates were found to vary by age group with the highest rates observed in early adult years (ages 15–29) for both males and females across all HDSS sites (Ginsburg et al., 2016).
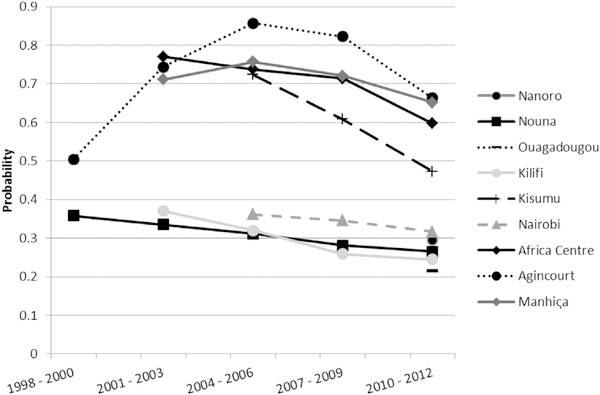
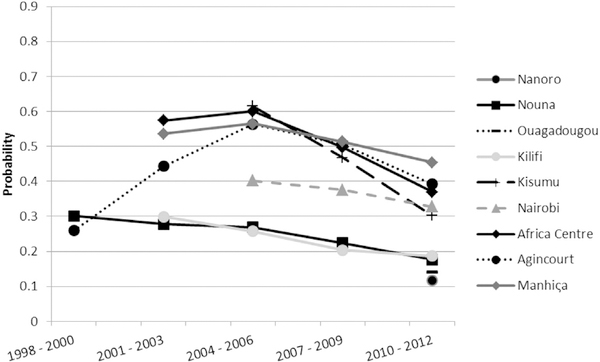
The probability to die between ages 15 and 60 (45q15) for males and females is presented for each HDSS site by period in Figs. 2 and 3. In the 2010–2012 period, for which data is available for all sites, Southern Africa sites experience the highest probability of male adult mortality over time, with probabilities between ages 15 and 60 being 0.66 and 0.65 for Agincourt and Manhiça, closely followed by the Africa Centre at 0.60. Similarly, Southern African sites report the highest probabilities of mortality in females: 0.45 for Manhiça, 0.39 for Agincourt and 0.37 for the Africa Centre. Lowest probabilities of mortality are evident within the Burkina Faso HDSS sites and Kilifi in East Africa. In all sites for which data is available from the year 2000 onwards the probability is declining for both males and females.
Fig. 2.
Probability of death between ages 15 and 60 (45q15) by HDSS site for males.
Fig. 3.
Probability of death between ages 15 and 60 (45q15)by HDSS site for females.
5.2. Regression results
5.2.1. Rural Southern Africa
With respect to the Agincourt HDSS, significant differences are observed between permanent residents and first time entering in-migrants in the initial two years following in-migration. Similarly, in the case of both male and female return migrants, the probability of death in the HDSS is 4.99 times higher for males and 5.39 times higher for females within two years following return, as compared with permanent residents. Conversely in the Africa Centre HDSS, the effect of return migration is far less in magnitude for females (1.36 times higher between 6 and 24 months following return to the HDSS) and not apparent amongst males. The higher relative risk of mortality for female return migrants reduces the longer the duration spent in Africa Centre HDSS. Results from the Manhiça HDSS indicate that male and female first time in-migrants to the HDSS have a significantly higher risk of death within two years following their entry in the HDSS (1.41 times the risk for males and 1.45 times for females); however this risk reduces with length of stay in the HDSS. To note, risks within the first two years following return do not differ by gender for Agincourt and Manhiça HDSSs, but they do differ for the Africa Centre.
The only case where a socialisation/propagation effect can be seen is amongst return migrants to the Agincourt HDSS. All other HDSSs in the sample show no evidence of these effects. The propagation effect in combination with the negative selection effect results in particularly high mortality for return migrants as compared to non-migrants. This stands in sharp contrast to the absence of any migration effect for in-migrants. Here the “midnight train” or negative selection effect (unhealthy return migrant) is compounded with a propagation effect resulting in migrants returning home with higher health risks acquired outside the study area.
The results of the Africa Centre HDSS reveal no migration effect whatsoever for males. This means that both in-migrant and return migrant males are moving from areas with similar exposures to the HDSS resident population and there is no selection effect (Table 3). Female return migrants, however, show a negative selection effect. Female in-migrants in Africa Centre HDSS are the only group amongst all the African HDSS under study that present a pattern that does not conform to any combination displayed in Table 1. This group experiences lower mortality for short exposure in the site but higher mortality after 5 years of residence: this reversal of trends after long exposure in the site is not predicted by our hypotheses and would therefore need further investigation.
Table 3.
Cox proportional hazards models – Southern African Rural HDSSs.
| Africa centre HDSS |
Agincourt HDSS |
Manhiςa HDSS |
||||
|---|---|---|---|---|---|---|
| All deaths |
All deaths |
All deaths |
||||
| Male | Female | Male | Female | Male | Female | |
| Permanent resident (Ref) | 1 | 1 | 1 | 1 | 1 | 1 |
| In-migrant | ||||||
| 6 – 24 months in HDSS | 0.94 (0.83–1.05) | 0.85** (0.75–0.97) | 1.37*** (1.20–1.56) | 1.26*** (1.12–1.43) | 1.41*** (1.26–1.58) | 1.45*** (1.27–1.65) |
| 25 – 59 months in HDSS | 0.86** (0.76–0.97) | 1.09 (0.97–1.23) | 1.08 (0.95–1.23) | 1.14** (1.02–1.27) | 1.12** (1.01–1.25) | 1.19*** (1.06–1.35) |
| 60 + months in HDSS | 1.02 (0.88–1.18) | 1.19** (1.03–1.38) | 0.88* (0.77–1.01) | 1.03 (0.92–1.15) | 0.97 (0.86–1.09) | 1.11 (0.98–1.27) |
| Return migrant | ||||||
| 6 – 24 months in HDSS | 1.18* (1.00–1.40) | 1.36*** (1.14–1.62) | 4.99*** (4.36–5.70) | 5.39*** (4.55–6.37) | 1.27*** (1.10–1.48) | 1.58*** (1.36–1.84) |
| 25 – 59 months in HDSS | 1.08 (0.91–1.29) | 1.23** (1.03–1.48) | 1.23** (1.04–1.45) | 1.53*** (1.22–1.92) | 1 (0.86–1.15) | 1.47*** (1.28–1.69) |
| 60 + months in HDSS | 0.98 (0.75–1.27) | 1.22 (0.95–1.58) | 0.97 (0.81–1.17) | 0.85 (0.62–1.16) | 1.08 (0.91–1.29) | 1.05 (0.87–1.27) |
| Return Migrant Exposure < 36months (Ref) | 1 | 1 | 1 | 1 | 1 | 1 |
| 36 + months away | 0.98 (0.78–1.24) | 1.14 (0.90–1.45) | 1.40*** (1.23–1.59) | 1.33*** (1.11–1.59) | 1.16* (0.98–1.39) | 1.17 (0.96–1.42) |
| Period | ||||||
| 1 Jan 1998–1 Jan 2001 (1998) | n.a. | n.a. | 0.78*** (0.69–0.90) | 0.74*** (0.65–0.85) | n.a. | n.a. |
| 1 Jan 2001–1 Jan 2004 (2001) | 1.06 (0.95–1.18) | 1.34*** (1.21–1.50) | 1.44*** (1.28–1.61) | 1.20*** (1.07–1.35) | 1.12** (1.02–1.23) | 1.29*** (1.17–1.42) |
| 1 Jan 2004–1 Jan 2007 (2004) | 1.31*** (1.18–1.45) | 1.75*** (1.58–1.93) | 1.91*** (1.72–2.13) | 1.56*** (1.40–1.74) | 1.24*** (1.14–1.36) | 1.39*** (1.27–1.51) |
| 1 Jan 2007–1 Jan 2010 (2007) | 1.25*** (1.13–1.38) | 1.41*** (1.27–1.56) | 1.70*** (1.53–1.89) | 1.30*** (1.17–1.45) | 1.13*** (1.04–1.23) | 1.20*** (1.10–1.31) |
| 1 Jan 2010–1 Jan 2013 (2010) (Ref) | 1 | 1 | 1 | 1 | 1 | 1 |
| Education | ||||||
| No Formal (Ref) | 1 | 1 | 1 | 1 | 1 | 1 |
| Some primary | 1.19*** (1.06–1.34) | 1.03 (0.92–1.15) | 0.96 (0.87–1.06) | 0.90* (0.82–1.00) | 0.83*** (0.77–0.90) | 1.02 (0.95–1.10) |
| Some secondary | 0.85** (0.75–0.96) | 0.88** (0.78–0.99) | 0.85*** (0.76–0.94) | 0.89** (0.80–1.00) | 0.59*** (0.52–0.68) | 0.53*** (0.43–0.65) |
| Some tertiary | 0.36*** (0.31–0.41) | 0.30*** (0.26–0.35) | 0.41*** (0.33–0.50) | 0.51*** (0.41–0.62) | n.a. | n.a. |
| Unknown | 7.02*** (6.12–8.05) | 10.60*** (9.26–12.14) | 3.08*** (2.49–3.81) | 3.00*** (2.34–3.84) | 0 (0.00–0.00) | 0 (0.00–0.00) |
| Observations | 132,397 | 178,581 | 334,011 | 486,753 | 161,391 | 254,925 |
| Wald Chi-square | 1793 | 2238 | 2067 | 970.8 | 195.2 | 237 |
| Log likelihood | −26421 | −30511 | −22910 | −25463 | −30180 | −34677 |
| Subjects | 38,234 | 46,303 | 40,818 | 55,904 | 37,663 | 48,787 |
| Time at risk | 179,333 | 251,414 | 180,818 | 275,656 | 171,254 | 270,686 |
| Failures | 3593 | 3860 | 3198 | 3143 | 3966 | 4203 |
p < 0.01
p < 0.05
p < 0.1.
n.a. = not applicable.
In the Manhiça HDSS in Mozambique, the dominant pattern is that of negative selection with (re-)adaptation, and no social-isation/propagation effect. The “unhealthy migrant” hypothesis applies in Manhiça to both in-migrants and return migrants. The number of female return migrants was too low to compute meaningful regression analysis coefficients.
5.2.2. Rural East Africa
The results from the Kisumu HDSS reveal both first time in-migrants and return migrants have a higher risk of mortality within the first two years following entry into the HDSS as compared with non-migrants, with the risk for females being higher than for males (for first-time in-migrants 1.80 and 1.35 times the risk respectively). The risk of mortality declines with duration of residence in the HDSS. Conversely, in-migrants and return migrants to the Kilifi HDSS are positively selected on health with lower risk of mortality within two years following entry to the HDSS (Table 4)(male return migrants have 0.56 and females 0.62 times the risk of death during this period).
Table 4.
Cox proportional hazards models – East African Rural HDSSs.
| Kilifi HDSS |
Kisumu HDSS |
|||
|---|---|---|---|---|
| All deaths |
All deaths |
|||
| Male | Female | Male | Female | |
| Permanent resident (Ref) | 1 | 1 | ||
| In-migrant | ||||
| 6 – 24 months in HDSS | 0.59*** (0.53–0.66) | 0.58*** (0.52–0.64) | 1.35*** (1.23–1.49) | 1.80*** (1.64–1.97) |
| 25 – 59 months in HDSS | 0.67*** (0.60–0.74) | 0.74*** (0.67–0.82) | 1.12** (1.01–1.24) | 1.26*** (1.13–1.40) |
| 60 + months in HDSS | 0.96 (0.85–1.08) | 1.12* (1.00–1.25) | 0.95 (0.81–1.12) | 1.17* (0.99–1.39) |
| Return migrant | ||||
| 6 – 24 months in HDSS | 0.56*** (0.44–0.71) | 0.62*** (0.49–0.77) | 1.36*** (1.17–1.57) | 1.53*** (1.31–1.79) |
| 25 – 59 months in HDSS | 0.76** (0.61–0.96) | 0.86 (0.68–1.07) | 1.40*** (1.21–1.62) | 1.13 (0.94–1.36) |
| 60 + months in HDSS | 0.75 (0.49–1.13) | 0.92 (0.63–1.34) | 1.15 (0.87–1.52) | 1.12 (0.79–1.60) |
| Return migrant exposure < 36months (Ref) | 1 | 1 | 1 | 1 |
| 36 + months away | 0.96 (0.71–1.29) | 1.11 (0.83–1.48) | 1.04 (0.81 – 1.33) | 0.88 (0.64–1.23) |
| Period | ||||
| 1 Jan 1998–1 Jan 2001 (1998) | n.a. | n.a. | n.a. | n.a. |
| 1 Jan 2001–1 Jan 2004 (2001) | 0.97 (0.88–1.07) | 1.06 (0.96–1.16) | n.a. | n.a. |
| 1 Jan 2004–1 Jan 2007 (2004) | 1.16*** (1.06–1.27) | 1.31*** (1.20–1.42) | 1.80*** (1.68–1.92) | 2.21*** (2.07–2.36) |
| 1 Jan 2007–1 Jan 2010 (2007) | 1.00 (0.91–1.09) | 0.98 (0.90–1.06) | 1.39*** (1.31 – 1.48) | 1.57*** (1.48–1.68) |
| 1 Jan 2010–1 Jan 2013 (2010) (Ref) | 1 | 1 | 1 | 1 |
| Education | ||||
| No Formal (Ref) | 1 | 1 | 1 | 1 |
| Some primary | 0.89** (0.81–0.99) | 1.05 (0.94–1.17) | 0.70*** (0.63–0.78) | 0.81*** (0.75–0.87) |
| Some secondary | 0.83** (0.71–0.96) | 0.91 (0.73–1.14) | 0.53*** (0.47–0.60) | 0.55*** (0.49–0.62) |
| Some tertiary | 0.72** (0.56–0.93) | 0.66* (0.42–1.06) | 0.36*** (0.30–0.43) | 0.32*** (0.24–0.43) |
| Unknown | 4.10*** (3.77–4.47) | 8.38*** (7.80–9.01) | 0.75*** (0.66–0.85) | 0.92* (0.84–1.01) |
| Observations | 2,382,427 | 3097 890 | 292,304 | 352,742 |
| Wald Chi-square | 2033 | 3974 | 623.3 | 969 |
| Log likelihood | −34689 | −39304 | −53320 | −56146 |
| Subjects | 145,669 | 168,010 | 98,838 | 123,054 |
| Time at risk | 557,901 | 722,164 | 393,920 | 482,936 |
| Failures | 4145 | 4548 | 6345 | 6396 |
p < 0.01
p < 0.05
p < 0.1.
n.a. = not applicable.
The gender difference in mortality pattern is negligible in these two sites. The difference by migration status is also absent: the effects are the same for in-migrants and return migrants. Both sites show (re-)adaptation effect but no socialisation/propagation effect, meaning that migrants faced similar health risks where they migrated from to the non-migrants in the site. However Kisumu and Kilifi HDSS differ markedly in terms of the selection hypothesis: it is positive in the case of Kilifi (conforming to the “healthy migrant” hypothesis) and negative in the case of Kisumu (conforming to the “unhealthy migrant” hypothesis). The situation in Kisumu HDSS in Kenya is very similar to that of Manhiça HDSS in Mozambique, while the Kilifi HDSS situation is unique among the African sites under study.
5.2.3. Rural West Africa
In Burkina Faso (Table 5), males returning to the Nouna HDSS, or entering the Nouna HDSS for the first time are positively selected on health with their risk of mortality being 0.61 and 0.75 times the risk of non-migrants respectively. For females, no significant relationship between mortality and migrant status is observed.
Table 5.
Cox proportional hazards models – West African Rural HDSSs.
| Nanoro HDSS |
Nouna HDSS |
|||
|---|---|---|---|---|
| All deaths |
All deaths |
|||
| Male | Female | Male | Female | |
| Permanent resident (Ref) | 1 | 1 | 1 | 1 |
| In-migrant | ||||
| 6 – 24 months in HDSS | 1.11 (0.69–1.79) | 0.96 (0.56–1.67) | 0.75*** (0.60–0.93) | 0.92 (0.77–1.10) |
| 25 – 59 months in HDSS | 1.34 (0.66–2.71) | 0.53 (0.19–1.51) | 0.85* (0.71–1.02) | 0.97 (0.83–1.13) |
| 60 + months in HDSS | n.a. | n.a. | 0.86 (0.71–1.03) | 0.87 (0.72–1.04) |
| Return migrant | ||||
| 6 – 24 months in HDSS | n.a. | n.a. | 0.61** (0.42–0.90) | 0.89 (0.63–1.26) |
| 25 – 59 months in HDSS | n.a. | n.a. | 0.56*** (0.40–0.78) | 0.57*** (0.38–0.84) |
| 60 + months in HDSS | n.a. | n.a. | 0.51*** (0.36–0.73) | 0.73 (0.49–1.08) |
| Return Migrant Exposure < 36months (Ref) | 1 | 1 | 1 | 1 |
| 36 + months away | n.a. | n.a. | 1.11 (0.76–1.63) | 1.17 (0.78–1.75) |
| Period | ||||
| 1 Jan 1998–1 Jan 2001 (1998) | n.a. | n.a. | 0.83** (0.71–0.96) | 1.02 (0.87–1.19) |
| 1 Jan 2001–1 Jan 2004 (2001) | n.a. | n.a. | 0.83*** (0.72–0.95) | 1.10 (0.95–1.27) |
| 1 Jan 2004–1 Jan 2007 (2004) | n.a. | n.a. | 0.92 (0.81–1.05) | 1.17** (1.02–1.35) |
| 1 Jan 2007–1 Jan 2010 (2007) | n.a. | n.a. | 1.04 (0.91–1.18) | 1.12 (0.97–1.30) |
| 1 Jan 2010–1 Jan 2013 (2010) (Ref) | 1 | 1 | 1 | 1 |
| Education | ||||
| No Formal (Ref) | 1 | 1 | 1 | 1 |
| Some primary | 0.99 (0.60–1.63) | 1.03 (0.47–2.29) | 1.37*** (1.15–1.63) | 1.23 (0.94–1.60) |
| Some secondary | 0.22*** (0.07–0.69) | 0.63 (0.19–2.03) | 1.17 (0.87–1.57) | 0.79 (0.47–1.32) |
| Some tertiary | 0.94 (0.23–3.84) | 0 (0.00–0.00) | 0.61 (0.15–2.46) | 0.00 (0.00–0.00) |
| Unknown | 1.47 (0.71–3.07) | 3.11*** (1.73–5.58) | 4.64*** (4.20–5.12) | 4.55*** (4.13–5.03) |
| Observations | 48,198 | 85,165 | 369,512 | 383,136 |
| Wald Chi-square | 13.95 | 14.92 | 1035 | 1056 |
| Log likelihood | −1607 | −1532 | −16135 | −14960 |
| Subjects | 14,863 | 24,204 | 45,864 | 51,906 |
| Time at risk | 36,808 | 61,807 | 251 985 | 2,52,185 |
| Failures | 272 | 238 | 2130 | 1948 |
p < 0.01
p < 0.05
p < 0.1.
n.a. = not applicable.
There is a sharp contrast between males and females in Nouna HDSS: females show no migration effect, whereas males show a positive selection effect that persists over time, i.e. with no (re-)adaptation effect. In Nanoro, there is no selection effect for both males and females and therefore adaptation is not testable.
5.2.4. Urban sites: Ouagadougou and Nairobi
With respect to the Ouagadougou HDSS, male first time entering migrants have 0.61 times the risk of death within two years following entry to the HDSS as compared to non-migrants. The risk converges to that of non-migrants after some years. This pattern is only compatible with no difference in health risks before and after migration, i.e. with positive selection, adaptation and no socialisation effect. This is also the case for male in-migrants in Nairobi HDSS (relative risks of 0.77 times that of non-migrants within two years of entry).
The number of return migrants is too low in the Ouagadougou HDSS to include in an analysis due to the site’s more recent inception date. Males returning to the Nairobi HDSS present the opposite risks to in-migrants: their risk of death is 1.31 times higher than non-migrants in the HDSS, while the risk converges to that of non-migrants thereafter. This pattern is compatible with negative selection, re-adaptation and no propagation effect.
To note, for both males in Ouagadougou and Nairobi, the observed patterns are only compatible with no difference in health risks before and after migration. In other words, migrants faced similar health risks where they migrated from as the non-migrants in these two sites (Table 6). This is also the case of females in Nairobi but there exists a doubt about females in Ouagadougou: the absence of migration effect for female in-migrants is compatible with all situations of difference in health risks before and after migration. However, there is little reason to believe that female migrants were subjected to very different health risks than male migrants. Therefore, assuming no socialisation, the pattern of female in-migration is compatible with no selection effect, and therefore not testable adaptation effect.
Table 6.
Cox proportional hazards models – Urban HDSSs.
| Ouagadougou HDSS |
Nairobi HDSS |
|||
|---|---|---|---|---|
| All deaths |
All deaths |
|||
| Male | Female | Male | Female | |
| Permanent resident (Ref) | 1 | 1 | 1 | 1 |
| In-migrant | ||||
| 6 – 24 months in HDSS | 0.61** (0.38–0.97) | 0.93 (0.59–1.47) | 0.77*** (0.65–0.90) | 1.25** (1.05–1.50) |
| 25 – 59 months in HDSS | 1.12 (0.62–2.00) | 0.96 (0.45–2.04) | 0.91 (0.78–1.07) | 1.01 (0.83–1.24) |
| 60 + months in HDSS | n.a. | n.a. | 0.81* (0.63–1.03) | 0.91 (0.67–1.23) |
| Return migrant | ||||
| 6 – 24 months in HDSS | n.a. | n.a. | 1.31** (1.04–1.65) | 1.16 (0.85–1.58) |
| 25 – 59 months in HDSS | n.a. | n.a. | 1.10 (0.86–1.40) | 0.98 (0.70–1.35) |
| 60 + months in HDSS | n.a. | n.a. | 1.32 (0.92–1.89) | 1.39 (0.91–2.14) |
| Return migrant exposure < 36months (Ref) | 1 | 1 | 1 | 1 |
| 36 + months away | n.a. | n.a. | 1.46* (0.99–2.15) | 1.36 (0.77–2.40) |
| Period | ||||
| 1 Jan 1998–1 Jan 2001 (1998) | n.a. | n.a. | n.a. | n.a. |
| 1 Jan 2001–1 Jan 2004 (2001) | n.a. | n.a. | n.a. | n.a. |
| 1 Jan 2004–1 Jan 2007 (2004) | n.a. | n.a. | 1.05 (0.91–1.20) | 1.33*** (1.13–1.57) |
| 1 Jan 2007–1 Jan 2010 (2007) | n.a. | n.a. | 1.07 (0.94–1.21) | 1.03 (0.88–1.20) |
| 1 Jan 2010–1 Jan 2013 (2010) (Ref) | 1 | 1 | 1 | 1 |
| Education | ||||
| No formal (Ref) | 1 | 1 | 1 | 1 |
| Some primary | 1.13 (0.84–1.51) | 1.13 (0.75–1.69) | 0.95 (0.76–1.19) | 0.90 (0.73–1.11) |
| Some secondary | 1.14 (0.82–1.58) | 0.7 (0.41–1.19) | 0.62*** (0.49–0.79) | 0.55*** (0.43–0.70) |
| Some tertiary | 0.96 (0.52–1.80) | 0.36 (0.05–2.60) | 0.60* (0.33–1.08) | 0.15* (0.02–1.07) |
| Unknown | 1.43 (0.93–2.20) | 1.59* (0.99–2.54) | 1.70** (1.08–2.69) | 1.69* (0.95–3.03) |
| Observations | 40,696 | 40,882 | 370,927 | 266,241 |
| Wald Chi-square | 7.587 | 8.546 | 105.7 | 82.57 |
| Log likelihood | −2050 | −1268 | −12214 | −7698 |
| Subjects | 33,377 | 34,174 | 67,859 | 50,049 |
| Time at risk | 70,412 | 69,321 | 197,246 | 136,962 |
| Failures | 317 | 195 | 1511 | 992 |
p < 0.01
p < 0.05
p < 0.1.
n.a. = not applicable.
Contrary to males, female in-migrants in Nairobi HDSS show a negative selection effect, the risk of mortality within the first two years is 1.25 times the risk for a permanent resident, but their risk converge to that of non-migrants thereafter (adaptation effect).
6. Discussion and conclusion
The results confirm the diversity of the migration-mortality relationship over a range of rural and urban local areas in three African regions (South, East and West). The selection and exposure effects are very diverse across the continent and within each country. No single pattern fits all situations: only two sites (Manhiça and Kisumu HDSS) present with similar situations although being very distant. Gender differences are absent in about half the sites. The results also confirm that the pattern of migration-mortality relationship is mainly generated by the combination of three processes: selection, adaptation and propagation. Out of 32 observed patterns there is only one (female in-migrants in Africa Centre HDSS) that does not conform to the expected combination. Therefore, the proposed theoretical framework proves valid. A limited set of variables easily extracted from longitudinal data (migration status and duration of residence in and out of the study site) is sufficient and quite effective in interpreting the data at hand. However, an important limitation is that for in-migrants into rural HDSSs, prior knowledge of origin areas (assumed difference in health risks before and after first in-migration) is necessary for interpreting data that are covering destination, but not origin.
With regards to the selection hypothesis, the results present a range of situations summarized in Table 7 for rural HDSSs and in Table 8 for urban HDSSs. The healthy in-migrant hypothesis is confirmed in four sites out of eight for males (Kilifi, Nouna, Ouagadougou and Nairobi HDSSs) and in only one site for females (Kilifi HDSS). It is contradicted in three sites (Agincourt, Manhiça and Kisumu HDSSs, for both males and females) while migration has no effect for in-migrants in two sites for males (Africa Centre and Nanoro HDSSs), and three sites for females (Nouna, Nanoro and Ouagadougou HDSSs).
Table 7.
Summary of the empirical findings of the effects of selection, (re)-adaptation and socialisation/propagation in rural areas.
| Socialisation/Propagation | Adaptation | Negative selection | No selection | Positive selection |
|---|---|---|---|---|
| Negative | Yes | Agincourt ♂ ♀ R | n.a. | |
| No | n.a. | |||
| Not testable | n.a. | n.a. | ||
| None | Yes | Agincourt ♂ ♀ I | n.a. | Kilifi ♂ ♀ I R |
| Manhiça ♂ ♀ I R | ||||
| Kisumu ♂ ♀ I R | ||||
| Africa Centre ♀ R | ||||
| No | n.a. | Nouna ♂ I R | ||
| Not testable | n.a. | Africa Centre ♂ I R | n.a. | |
| Nouna ♀ R | ||||
| Nanoro ♂ ♀ I | ||||
| Positive | Yes | n.a. | ||
| No | n.a. | |||
| Not testable | n.a. | n.a. |
Only “Africa Centre ♀ ” do not fit into this table of expected combination of selection and exposure. n.a.: not applicable. I: in-migrants. R: return migrants. ♂: males. ♀: females.
Table 8.
Summary of the empirical findings of the effects of selection, (re)-adaptation and socialisation/propagation in urban areas.
| Socialisation/Propagation | Adaptation | Negative selection | No selection | Positive selection |
|---|---|---|---|---|
| Negative | Yes | n.a. | ||
| No | n.a. | |||
| Not testable | n.a. | n.a. | ||
| None | Yes | Nairobi ♀ I | n.a. | Ouagadougou ♂ I |
| Nairobi ♂ R | Nairobi ♂ I | |||
| No | n.a. | |||
| Not testable | n.a. | Ouagadougou ♀ I | n. a. | |
| Nairobi ♀ R | ||||
| Positive | Yes | n.a. | ||
| No | n.a. | |||
| Not testable | n.a. | n.a. |
n.a.: not applicable. I: in-migrants. R: return migrants.♂: males. ♀: females.
The pattern amongst return migrants corresponds exactly to that of in-migrants in all sites but the Africa Centre HDSS for females (where the pattern is not consistent with our theoretical framework), as well as the Nairobi HDSS, where male return migrants are negatively selected (as opposed to positive selection observed amongst in-migrants) and female return migrants are not selected (as opposed to negative selection observed amongst in-migrants). The similar patterns for in-migrants and return migrants found in most sites show that the nature of the migration does not markedly influence the interplay between selection and exposure effects. In particular, the “healthy migrant” does not oppose the “unhealthy return migrant” in the same site, except for males in one urban site, the Nairobi HDSS.
Whether positive or negative, selection is always associated with adaptation, except for males in Nouna who experience positive selection and no adaptation. In one case, return migrants in Agincourt, negative selection is associated with negative propagation, making return migration particularly associated with high mortality. At the opposite, 8 out of 32 observed patterns show no effect of migration on mortality, i.e. no selection, adaptation, or socialisation effects.
How might these results impact on the administration of public health services in these HDSS sites, in particular as relating to migrants? Two effects call for particular attention: negative selection and negative socialisation/propagation. Migrants who are negatively selected on health are clearly a concern in Manhiça and Kisumu, whatever the migration status (in- or return migrant) and gender. In the Agincourt HDSS, male and female return migrants should be also targeted, especially since they are vectors of negative propagation in the site. In the Africa Centre HDSS, female return migrants’ health calls for more investigation on why it departs from other patterns. In Nairobi HDSS, the concern is for male return migrants and for female in-migrants. In all these cases but females in Africa Centre, the migrants should be targeted in the first 2 or 3 years after their arrival to the HDSS. After some years, migrants’ risks tend to converge with those of non-migrants. The public health intervention would then help to reduce the risks upon arrival and accelerate the convergence.
Conditional on the validity of our assumption in rural areas of no difference in health risks before and after first in-migration, the negative socialisation/propagation effect is not a concern in any of the rural sites under study, except in Agincourt HDSS for return migrants. The Agincourt HDSS situation probably reflects the propagation of the AIDS epidemic that affected this rural area particularly severely in the years 2000 (Bocquier et al., 2014). There, in the absence of a means to reduce health risks at migrants’ destinations, prevention targeted towards residents who intend to migrate could help reduce health risks taken in these destinations through raising awareness to potential health risks. Contrary to the expected, return migrants to rural areas (presumably returning from more affluent areas, in cities or abroad) do not appear to be vectors of positive propagation, as this effect is not evident in these data. Seeking support for return migrants with long exposure out of the site in the form of local public health policy implementation would be a less effective direction for interventions. Gathering information about health risks at migrants’ destinations would be a more fruitful approach.
Acknowledgements
We greatly value the contribution of each participating HDSS centre in providing data for this multi-centre study (see details below). The Multi-centre Analysis of the Dynamics of Internal Migration And Health (MADIMAH) project has received funds from the Swedish International Development Agency (Sida: 2012–000379), the National Research Foundation, South Africa, the Wallonia-Brussels Federation of Belgium (Grant No: 95284) and the INDEPTH Secretariat. We further acknowledge institutional support from the School of Public Health, Faculty of Health Sciences, University of the Witwatersrand, South Africa; Centre de Recherche en Démographie et Sociétés, Université Catholique de Louvain, Louvain-la-Neuve, Belgium; and the African Population and Health Research Centre, Nairobi, Kenya, as critical bases for the MADIMAH project leadership. We gratefully acknowledge the South African Medical Research Council (SAMRC) for funding Carren Ginsburg’s Career Development Award. Michael White’s participation in this publication was made possible with help from the Lifespan/Tufts/Brown Center for AIDS Research (Grant No: P30AI042853).
The Nanoro HDSS (CRUN) is grateful to the Malaria Clinical Trial Alliance (MCTA) (Grants: IN-MCTA-10012008; IN-MCTA-05092010) and the Institute of Tropical Medicine, Antwerp, through the Belgian Cooperation (Framework Agreement 3-III DGD-ITM 2014–2016), for their financial support. The Nouna HDSS (Centre de Recherche en Santé de Nouna, CRSN) wish to acknowledge the Ministry of Health Burkina Faso, the Ministry of Research of the State of Baden-Wurttemberg and the Institute of Public Health of Heidelberg, as well as the German Research Foundation (DFG) for their financial support under research grant SFB 544. The Ouagadougou HDSS (Observatoire de Population de Ouagadougou, OPO) extends thanks to the Wellcome Trust (Grant No: WT081993MA) for their support. The Kilifi HDSS acknowledges the Wellcome Trust (Grant No: 092654/Z/10/A) for funding data collection activities. The KEMRI-CDC HDSS (Kisumu) acknowledges CDC (USA) for providing funding and KEMRI-CGHR for their support. The Nairobi Urban HDSS (NUHDSS) would like to acknowledge the Rockefeller Foundation, USA, the Wellcome Trust, UK, (Grant No: GR 07830M), the William and Flora Hewlett Foundation, USA, (Grant No: 2015-2530), Comic relief, UK, (Grant No: GR002-12547), Swedish International Development Cooperation (SIDA), (Grant No: 54100029) and the Bill and Melinda Gates Foundation, USA, (Grant No: OPP1021893). The Manhiça HDSS (Centro de Investigação em Saúde de Manhiça, CISM) is grateful to the National Health Institute of Mozambique (INS), the Fundació Clínic per a la Recerca Biomèdica, Universitat de Barcelona, and the Spanish Agency for International Development and Cooperation for their technical and financial support. The Agincourt HDSS gratefully acknowledges the Wellcome Trust, UK, (Grants 058893/Z/99/A; 069683/Z/02/Z; 085477/Z/08/Z), The William and Flora Hewlett Foundation (Grant: 2008-1840), National Institute on Aging (NIA) of the NIH (Grants 1R24AG032112-01; 5R24AG032112-03), and The Andrew W Mellon Foundation, USA. The Africa Centre for Population Health Demographic Surveillance site wishes to acknowledge the financial support received from the Wellcome Trust (Grant No: 097410/Z/11/Z).
Appendix
Appendix 1.
HDSS sites included in this multi-centre analysis.
| HDSS site | Population size (approximate) | Size of site (km2) | Settlement type | Population density estimate (persons per km2) | Inception year | Contiguity and location |
|---|---|---|---|---|---|---|
| West Africa | ||||||
| Nanoro HDSS Burkina Faso | 61,000 | 594.3 | Rural | 102.6 | 2009 | Contiguous site situated in centre of Burkina Faso, 85 km from capital, Ouagadougou |
| Nouna HDSS Burkina Faso | 84,336 | 1756 | (Mostly) Rural | 48 | 1992 | Contiguous site situated north west of Burkina Faso, 300 km from capital, Ouagadougou |
| Ouagadougou HDSS Burkina Faso | 81,717 | 14.73 | Urban | 5547.7 | 2008 | Non-contiguous site comprising three informal areas: Nonghin, Polesgo and Nioko 2, and two formal areas: Kilwin and Tanghin, north ofcity. |
| East Africa | ||||||
| Kilifi HDSS Kenya | 261,919 | 900 | (Mostly) Rural | 291 | 2000 | Contiguous site situated north of Mombasa on Indian Ocean coast of Kenya |
| Kisumu HDSS Kenya | 223,406 | 700 | (Mostly) Rural | 319.2 | 2001 | Contiguous site located in Rarieda, Siaya and Gem districts, northeast of Lake Victoria, Nyanza Province, western Kenya |
| Nairobi HDSS Kenya | 71,000 | 0.97 | Urban | 73,195.9 | 2002 | Non-contiguous site comprising Viwandani and Korogocho slum settlements (7 km apart) in capital, Nairobi |
| Southern Africa | ||||||
| Africa Centre HDSS South Africa | 85,000 | 438 | Rural | 194.1 | 1997 | Contiguous site in the Umkanyakude district of KwaZulu-Natal |
| Agincourt HDSS South Africa | 91,178 | 420 | (Mostly) Rural | 217.1 | 1992 | Contiguous site situated in northeast South Africa close to border with Mozambique |
| Manhiςa HDSS Mozambique | 90,000 | 500 | Rural | 180 | 1996 | Contiguous site located in southern Mozambique, 80 km north of capital, Maputo |
Appendix 2.
Non-migration characteristics of the analytical sample by HDSS site over the respective analysis periods.
| Nanoro HDSS |
Nouna HDSS |
Ouagadougou HDSS |
Kilifi HDSS |
Kisumu HDSS |
Nairobi HDSS |
Africa centre HDSS |
Agincourt HDSS |
Manhiςa HDSS |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| % Person years |
% Person years |
% Person years |
% Person Yyears |
% Person years |
% Person years |
% Person Years |
% Person years |
% Person years |
||||||||||
| Male | Female | Male | Female | Male | Female | Male | Female | Male | Female | Male | Female | Male | Female | Male | Female | Male | Female | |
| Period | ||||||||||||||||||
| 1 Jan 1998–1 Jan 2001 | n.a. | n.a. | 29,518 | 29,762 | n.a. | n.a. | n.a. | n.a. | n.a. | n.a. | n.a. | n.a. | n.a. | n.a. | 39 433 | 55 500 | n.a. | n.a. |
| 11.71% | 11.80% | 22% | 20% | |||||||||||||||
| 1 Jan 2001–1 Jan 2004 | n.a. | n.a. | 44 704 | 44 527 | n.a. | n.a. | 107,781 | 137,179 | n.a. | n.a. | n.a. | n.a. | 43 779 | 61 698 | 32 956 | 52 442 | 33 108 | 49 855 |
| 17.74% | 17.66% | 19% | 19% | 24% | 25% | 18% | 19% | 19% | 18% | |||||||||
| 1 Jan 2004–1 Jan 2007 | n.a. | n.a. | 54,232 | 54,325 | n.a. | n.a. | 135,271 | 177,188 | 93,066 | 114,869 | 60,031 | 40,031 | 43 210 | 61 482 | 32 713 | 52 597 | 44 296 | 70 090 |
| 21.52% | 21.54% | 24% | 25% | 24% | 24% | 30% | 29% | 24% | 24% | 18% | 19% | 26% | 26% | |||||
| 1 Jan 2007–1 Jan 2010 | n.a. | n.a. | 59,190 | 59,471 | n.a. | n.a. | 149 931 | 195 821 | 141 468 | 172 354 | 64 977 | 45 185 | 44 969 | 63 771 | 35 327 | 55 600 | 44 556 | 73 172 |
| 23.49% | 23.58% | 27% | 27% | 36% | 36% | 33% | 33% | 25% | 25% | 20% | 20% | 26% | 27% | |||||
| 1 Jan 2010–1 Jan 2013 | 36,808 | 61 807 | 64,341 | 64,100 | 70,412 | 69,321 | 164 918 | 211 977 | 159 386 | 195 713 | 72 238 | 51 746 | 47 375 | 64 463 | 40 389 | 59 518 | 49 294 | 77 569 |
| 100% | 100% | 26% | 25% | 100% | 100% | 30% | 29% | 40% | 41% | 37% | 38% | 26% | 26% | 22% | 22% | 29% | 29% | |
| Education | ||||||||||||||||||
| No Formal | 24 135 | 50 961 | 119 727 | 149 753 | 21 348 | 29 179 | 66 760 | 292 929 | 7640 | 52 595 | 6237 | 9468 | 8916 | 19 976 | 18 910 | 55 734 | 26 841 | 111 548 |
| 66% | 82% | 48% | 59% | 30% | 42% | 12% | 41% | 2% | 11% | 3% | 7% | 5% | 8% | 10% | 20% | 16% | 41% | |
| Some Primary | 5453 | 4235 | 37 542 | 20 998 | 18 497 | 14 720 | 283 779 | 254 246 | 243 840 | 299 926 | 110 180 | 86 218 | 23 215 | 47 039 | 38 862 | 50 950 | 116 683 | 136,597 |
| 15% | 7% | 15% | 8% | 26% | 21% | 51% | 35% | 62% | 62% | 56% | 63% | 13% | 19% | 21% | 18% | 68% | 50% | |
| Some Secondary | 5510 | 3438 | 18 734 | 10 806 | 20 253 | 16 188 | 65 220 | 39 569 | 89 834 | 71 840 | 76 577 | 39 389 | 98 220 | 125 451 | 113 129 | 152 609 | 26 136 | 20 570 |
| 15% | 6% | 7% | 4% | 29% | 23% | 12% | 5% | 23% | 15% | 39% | 29% | 55% | 50% | 63% | 55% | 15% | 8% | |
| Some Tertiary | 357 | 67 | 852 | 150 | 3778 | 1554 | 12 911 | 8291 | 16 186 | 8441 | 2733 | 1037 | 46 617 | 56 347 | 8317 | 14 155 | n.a. | n.a. |
| 1% | 0% | 0% | 0% | 5% | 2% | 2% | 1% | 4% | 2% | 1% | 1% | 26% | 22% | 5% | 5% | |||
| Unknown | 1354 | 3107 | 75 131 | 70 478 | 6536 | 7681 | 129 231 | 127 129 | 36,418 | 50 133 | 1520 | 849 | 2364 | 2600 | 1600 | 2208 | 1594 | 1971 |
| 4% | 5% | 30% | 28% | 9% | 11% | 23% | 18% | 9% | 10% | 1% | 1% | 1% | 1% | 1% | 1% | 1% | 1% | |
n.a. = not applicable.
References
- Abel GJ, Sander N, 2014. Quantifying global international migration flows. Science 343 (6178), 1520–1522. [DOI] [PubMed] [Google Scholar]
- Abraído-Lanza AF, Dohrenwend BP, Ng-Mak DS, Turner JB, 1999. The Latino mortality paradox: a test of the “salmon bias” and healthy migrant hypotheses. Am. J. Public Health 89 (10), 1543–1548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bell M, Charles-Edwards E, Ueffing P, Stillwell J, Kupiszewski M, Kupiszewska D, 2015. Internal migration and development: comparing migration intensities around the world. Popul. Dev. Rev 41 (1), 33–58. [Google Scholar]
- Bocquier P, Collinson M, Clark SJ, Gerritsen A, Kahn K, Tollman SM, 2014. Ubiquitous burden: the contribution of migration to AIDS and Tuberculosis mortality in rural South Africa. Afr. Popul. Stud. 28 (1), 691–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boutayeb A, 2006. The double burden of communicable and non-communicable diseases in developing countries. Trans. R. Soc. Trop. Med. Hyg 100 (3), 191–199. [DOI] [PubMed] [Google Scholar]
- Choi K, 2014. Fertility in the context of Mexican migration to the United States. Demogr. Res 30, 703–738. [Google Scholar]
- Clark S, Collinson M, Kahn K, Drullinger K, Tollman S, 2007. Returning home to die: circular labour migration and mortality in South Africa. Scand. J. Public Health 35 (Suppl. 69), 35–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collinson M, Adazu K, White M, Findley SE, 2009. The Dynamics of Migration, Health and Livelihoods: INDEPTH Network Perspectives. Ashgate, Farnham. [Google Scholar]
- Collinson MA, White MJ, Bocquier P, McGarvey SJ, Afolabi SA, Clark SJ, Kahn K, Tollman SM, 2014. Migration and the epidemiological transition: insights from the Agincourt sub-district of northeast South Africa. Glob. Health Action 7 (23514), 1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ezzati M, Vander Hoorn S, Lawes CMM, Leach R, James WPT, Lopez AD, Rodgers A, Murray CJL, 2005. Rethinking the “diseases of affluence” paradigm: global patterns of nutritional risks in relation to economic development. PLoS Med. 2 (5), e133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gerritsen A, Bocquier P, White M, Mbacke C, Alam N, Beguy D, Odhiambo F, Sacoor C, Phuc HD, Punpuing S, Collinson MA, 2013. Health and demographic surveillance systems: contributing to an understanding of the dynamics in migration and health. Glob. Health Action 6 (21496), 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ginsburg C, Bocquier P, Beguy D, Afolabi S, Augusto O, Derra K, Odhiambo F, Otiende M, Soura A, Zabre P, 2016. Human capital on the move: education as a determinant of internal migration in selected INDEPTH surveillance populations in Africa. Demogr. Res. 34, 845–884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldstein S, 1973. Interrelation between migration and fertility in Thailand. Demography 10 (2), 225–241. [PubMed] [Google Scholar]
- Harpham T, 2009. Urban health in developing countries: what do we know and where do we go? Health & Place 15 (1), 107–116. [DOI] [PubMed] [Google Scholar]
- Hervitz HM, 1985. Selectivity, adaptation, or disruption? a comparison of alternative hypotheses on the effects of migration on fertility: the case of Brazil. Int. Migr. Rev 19 (2), 293–317. [PubMed] [Google Scholar]
- Kulu H, 2005. Migration and fertility: competing hypotheses Re-examined. Eur. J. Popul./Revue Eur. de Demogr 21 (1), 51–87. [Google Scholar]
- Kulu H, Steele F, 2013. Interrelationships between childbearing and housing transitions in the family life course. Demography 50 (5), 1687–1714. [DOI] [PubMed] [Google Scholar]
- Lu Y, Qin L, 2014. Healthy migrant and salmon bias hypotheses: a study of health and internal migration in China. Soc. Sci. Med 102, 41–48. [DOI] [PubMed] [Google Scholar]
- Nauman E, VanLandingham M, Anglewicz P, Patthavanit U, Punpuing S, 2015. Rural-to-urban migration and changes in health among young adults in Thailand. Demography 52 (1), 233–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salomon JA, Murray CJL, 2002. The epidemiologic transition revisited: compositional models for causes of death by age and sex. Popul. Dev. Rev 28 (2), 205–228. [Google Scholar]
- Sankoh O, Byass P, 2012. The INDEPTH Network: filling vital gaps in global epidemiology”. Int. J. Epidemiol 41 (3), 579–588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- United Nations Population Division, 2014. World Population Prospects: the 2012 Revision.
- Urquia ML, Gagnon AJ, 2011. Glossary: migration and health. J. Epidemiol. Community Health:jech 2010,109405. [DOI] [PubMed] [Google Scholar]
- White M, Lindstrom D, 2006. Internal migration In: Poston DL, Micklin M (Eds.), Handbook of Population. Springer, New York, pp. 331–346. [Google Scholar]
- Yusuf S, Reddy S, Ounpuu S, Anand S, 2001. Global burden of cardiovascular diseases: Part I: general considerations, the epidemiologic transition, risk factors, and impact of urbanization. Circulation 104 (22), 2746–2753. [DOI] [PubMed] [Google Scholar]