Abstract
Polyphenolic compounds, widely present in fruits, vegetables, and cereals, have potential benefits for human health and are protective agents against the development of chronic/degenerative diseases including cancer. More recently these bioactive molecules have been gaining great interest as anti-inflammatory and immunomodulatory agents, mainly in neoplasia where the pro-inflammatory context might promote carcinogenesis. Colorectal cancer (CRC) is considered a major public healthy issue, a leading cause of cancer mortality and morbidity worldwide. Epidemiological, pre-clinical and clinical investigations have consistently highlighted important relationships between large bowel inflammation, gut microbiota (GM), and colon carcinogenesis. Many experimental studies and clinical evidence suggest that polyphenols have a relevant role in CRC chemoprevention, exhibit cytotoxic capability vs. CRC cells and induce increased sensitization to chemo/radiotherapies. These effects are most likely related to the immunomodulatory properties of polyphenols able to modulate cytokine and chemokine production and activation of immune cells. In this review we summarize recent advancements on immunomodulatory activities of polyphenols and their ability to counteract the inflammatory tumor microenvironment. We focus on potential role of natural polyphenols in increasing the cell sensitivity to colon cancer therapies, highlighting the polyphenol-based combined treatments as innovative immunomodulatory strategies to inhibit the growth of CRC.
Keywords: polyphenols, immunomodulation, inflammation, gut microbiota, colorectal cancer, colorectal cancer therapy
Introduction
Colorectal cancer is the world's second deadliest cancer after lung (1), more than half (55%) of the cases of CRC occur in developed regions, but developing countries are catching up. As their economies grow, so does the incidence of colorectal cancer. The scientific data show that no correct dietary habits and life style may affect the risk/progression of inflammation-related disease such as CRC (2–8). In inflammatory bowel disease (IBD) chronic inflammation leads to mucosal disruption accompanied by an excessive production of reactive oxygen species (ROS) (9) and may promote cancer onset, progression and metastatic diffusion (10). Apart from IBD, inflammation-related cancer risk factors are high fat/low fiber diet, obesity, and family history of CRC, all linked to an abnormal gut microbial composition (11–14). In sporadic (no-colitis-associated) CRC genetic alterations, such as adenomatous polyposis coli (Apc) mutations, DNA mismatch repair (MMR) deficiency, and microsatellite instability (MSI) are reported (15). Immune microenvironment of MSI primary colon cancer revealed a high infiltration of activated CD8+ CTL (16) and high expression of immune checkpoints, indicating that this subgroup of tumors may represent a target of immune checkpoint blockade (ICB). These results stem from seminal data by Galon et al. demonstrating that the lymphocyte infiltration in the primary CRC is a good prognostic factor (17). Clinical and experimental studies have focused on the complex and essential role of immune responses in CRC. In this scenario the crucial role of gut microbiota in triggering chemokine production leading to T cell recruitment in tumor tissues has been demonstrated (18). Notably dietary bioactive compounds act as anti-tumor agents (19, 20) modulating several molecular targets involved in survival, proliferation, angiogenesis, invasion and metastasis in cancer (21–23). As such several nutrients (24) may affect crucial inflammatory chemokines and cytokines which strongly contribute to the epithelial-mesenchymal transition program involved in cancer invasion, metastasis, and immune escape process (25) also in CRC (26).
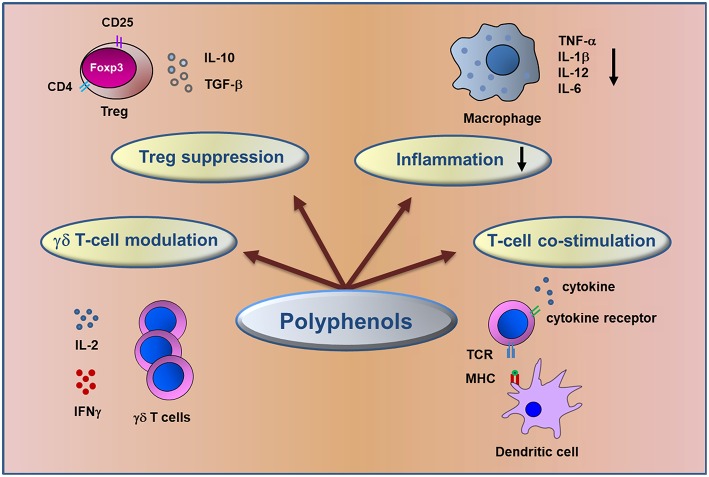
Among bioactive compounds, polyphenols are known as potential anti-inflammatory and anti-tumor agents (Figure 1) and could be good candidates for cancer prevention and treatment (27–29) targeting key molecular pathways involved in colorectal cancer (30–32).
Figure 1.
Schematic representation of immunomodulatory action of dietary polyphenols. The figure summarizes the major mechanisms involved in the control of inflammation and in anti-tumor immune response elicited by polyphenols in CRC.
Epidemiological studies suggest that the Mediterranean Diet (MD) rich in polyphenols, could reduce level of inflammation and oxidative damage and has linked with a relevant reduction in cancer risk mainly in CRC (33, 34).
Considering the role of inflammation in CRC, anti-inflammatory agents such as polyphenols are promising drugs for less toxic clinical intervention. In this review we detail the polyphenol properties, most likely related to their immunomodulatory activities, able to counteract several aspects of the inflammatory process in tumor microenvironment through the modulation of cytokine and chemokine production and in turn immune cell activation (35).
Dietary Polyphenols
Polyphenols are a large group of compounds synthesized by plants for a variety of functions, such as protection against UV radiation, mechanical damage, and microbial infection (36). Different classes and subclasses of polyphenols generate a large structural variability as a function of their number of phenol rings in combination with one or more hydroxyl compounds (37). Polyphenols present in fruits, vegetables, and cereals have emerged as one of the main families of natural compounds, most of them have been considered functional foods with potential biological activities in many pathologies, such as cancer (38–40), diabetes (41), obesity and inflammation-related diseases (42–44), neurodegenerative disorders (45, 46), and cardiovascular diseases (47). The main groups of dietary polyphenols promoting beneficial effects on human health are: phenolic acids, flavonoids, stilbenes, and lignans (see http://phenol-explorer.eu/compounds/classification for an update classification).
They are potential anti-inflammatory and anti-cancer agents, especially in anatomical districts such as colon, where the activity of dietary bioactive compounds is relevant.
Cross Talk Between Polyphenols and Gut Microbiota
After oral assumption, dietary polyphenols are recognized by the human body as xenobiotics and only a small amount is hydrolyzed in active compounds and absorbed in the small intestine (48). The remaining polyphenols accumulate in the large intestinal lumen where they might be hydrolyzed by the enzymatic activities of the gut microbial community into various metabolites before absorption. It is becoming clear that the GM, after degradation of food macromolecules (49), plays a crucial role in the maturation, development, and function of the host immune system (18, 50–52). Nevertheless, a continuous dialogue between microbiota and innate and adaptive immunity (53) regulates intestinal tissue homeostasis. When this functional control is lost, dysbiosis occurs leading to inflammatory disorders that might promote tumorigenesis (54–58).
Recently, advances in defining the effects of the microbiota on polyphenol bioavailability and function have been made. Moreover, it has been recognized that polyphenol-rich foods can affect the composition and activity of the microbiota (59, 60). Dietary polyphenols exert a prebiotic-like effect, contribute to maintain the gut health and to reduce levels of inflammation through the stimulation of beneficial bacteria growth and inhibition of pathogenic microbe development (61, 62). The large inter-individual variation of metabolites (30) can be related, at least partly, to differences in the GM composition and therefore in the way the polyphenols are catabolized.
Epidemiological data (33, 63) are concordant in suggesting that the adherence to MD decreases the risk of a variety of cancers. The polyphenol-rich MD modulates multiple processes involved in inflammatory response and carcinogenesis, such as free radical production, nuclear factor kappa-light-chain-enhancer of activated B cells (NF-κB) activation, and the eicosanoid-derived pathways. Thus, an appropriate diet can maintain the equilibrium between the inflammatory pathway and the anti-inflammatory process induced by many dietary compounds including polyphenols (64). Furthermore, great attention has been addressed to the effect that MD has on maintenance of “good” GM (65) and on control of carcinogenesis through specific epigenetic alterations (66).
Recently, the association between microbiota and different stages of CRC and the role of microbiota in the therapeutic response including that of the immune checkpoint-blocking therapy has shown to be highly relevant (67).
Polyphenols as Immunomodulatory Agents
Growing evidence clearly indicates that diet influences the innate and adaptive arms of the immune system (Figure 1) (68). Innate immune cells, such as macrophages, myeloid-derived suppressor, dendritic and natural killer cells and adaptive immune cells (T and B lymphocytes) may infiltrate the tumor tissues impacting the immune microenvironment and the clinical outcome (49). Several investigations have reported the antitumor effect of polyphenols through the modulation of T lymphocyte functionality to recognize and lyse tumor cells enhancing the immune response and counteracting the immune escape, a cancer progression hallmark (69, 70).
Among polyphenol studies, the dose dependent therapeutic efficacy of resveratrol has been demonstrated in an animal model of ulcerative colitis. Resveratrol, a flavonoid stilbene compound, treatment is associated with the regulation of T regulatory (Treg)/T helper 17 (Th17) balance and the level of plasma and intestinal mucosal cytokines including interleukin 10 (IL-10), transforming growth factor-beta1 (TGF-β1), interleukin 6 (IL-6), and interleukin 17 (IL-17) (71).
Curcumin, a no-flavonoid compound, suppressed the development of Dextran Sulfate Sodium (DSS)-induced colitis in a mouse model through the inhibition of NF-κB activation and the induction of mucosal Treg cells. Treatment with nanoparticles of curcumin induced an alteration of the gut microbial structure and a change in the level of fecal short chain fatty acids, indicating nanoparticles curcumin as a therapeutic option for the treatment of IBD diseases (72).
Trans-Scirpusin A (TSA), a resveratrol oligomer, has been reported to inhibit the growth of colorectal cancer in in vivo model. Among different mechanisms involved in its antitumor efficacy, TSA overcomes the tumor-associated immunosuppressive microenvironment by reducing the number of CD25-FoxP3 regulatory T cells and myeloid-derived suppressor cells (73).
Dietary anti-inflammatory polyphenols, such as chlorogenic acid and resveratrol, significantly suppressed the secretion of several cytokines (interferon gamma IFN-γ, tumor necrosis factor alfa TNF-α), reduced the colonic infiltration of CD3+T cells producing these cytokines and neutrophils in colitis and in colitis-associated to CRC experimental model (74, 75). In mouse C57BL/6J-Min/+, bearing a germline Apc mutation, a classical model of familial adenomatous polyposis (FAP) and sporadic colorectal cancer, administration of curcumin increases mucosal CD4+ T and B cells and contributes to prevent adenoma formation (76). Apple polyphenolic extracts (77), soy and sulforaphane flavonoid compounds (78, 79) reduce pro-inflammatory cytokine expression (IL-1β, TNF-α, IL-6, IL-17, and IFN-γ) in the context of a chemically induced colitis. The immunomodulatory activity of cocoa, a flavonoid compound, has been demonstrated to affect the gut immune responses in young rats by increasing the percentage of γδ T cells and lowering the effect of IgA (80).
It has been demonstrated an important role of chemokine receptor 3 (CXCR3) and its ligands in both inflammation and colorectal cancer (81). Recently it has been shown that resveratrol trihydroxy trans stilbene (TS) is able to hamper the suppressive ability of Treg by increasing CXCR3 in CD8+ Tregs facilitating Teff recruitment with a reduction of number and size of tumors (82). Dendritic cells (DCs) play a relevant role in cancer by exerting both pro-tumorigenic and anti-tumorigenic functions depending on the local environment (83) having an impact upon clinical outcome in CRC patients (84). Furthermore, Kajihara et al. analyzed the potential role of a dendritic-based cancer immunotherapy treatment in patients with recurrent or metastatic CRC (85). The potential effects of polyphenols on the function of DCs, the most effective antigen-presenting cells, with the capacity to shift immune response toward tolerance or immune activation (86, 87) has been highlighted in different studies. In particular protocatechuic acid, an anthocyanin flavonoid metabolite, has been demonstrated to have a main regulatory effect on the functional activation of DCs, suggesting the potential therapeutic application of this dietary compound against inflammatory conditions (88).
Quercetin and piperine, a flavonoid and no-flavonoid compound, when combined represent an effective and potent anti-inflammatory strategy to treat acute colitis in mice. This anti-inflammatory effect was mediated by impaired DC immune responses (89). Moreover, quercetin has been shown to suppress the secretion of TNF-α and interfere with the onset of IBD (90).
Polyphenols and Inflammation
Chronic inflammation characterized by the continuous presence of inflammatory cells and inflammatory mediators is known to play a key role in the development of various cancers. A long-standing chronic inflammation is a key predisposing factor of CRC in IBD since an excessive ROS production present in the inflamed mucosa alters important cellular functions and damages intestinal mucosa (91–93).
For several years, polyphenols have been extensively studied for their ability to scavenge free-radicals endogenously generated (94) or formed by radiation and xenobiotics (95).
Polyphenols have anti-inflammatory effect and their antioxidant properties are mainly mediated by ability to down-regulate the nuclear factor NF-kB, modulating crucial cell signaling pathways involved in inflammation and cancer (96–100).
Evaluating the polyphenolic fraction of olive oil, a principal component of MD, Serra et al. reported the inhibition of some crucial colonic inflammatory processes mediated by NF-kB, inducible nitric oxide synthases (iNOS), IL-8 and IL-6, thus proposing olive oil as a major dietary compound able to prevent and counteract the progression of IBD (101).
Green tea polyphenols ameliorate antioxidant response, decrease inflammatory markers (TNF-α, IL-6, and serum amyloid A), attenuate the pathological lesions and preserve colonic microstructure in a similar manner of sulfasalazine, the standard-of-care agent in IBD as shown in DSS mice (102). Several studies have demonstrated that cocoa exhibits a potential anti-inflammatory effects in in vitro and in vivo CRC models and might be a promising dietary preventive compound. Experiments performed in TNF-α stimulated colon cancer Caco-2 cells demonstrated that cocoa polyphenols down-regulate inflammatory marker expression by suppressing NF-kB nuclear translocation and c-Jun N-terminal kinase (JNK) phosphorylation. A cocoa-rich diet decreased the nuclear level of NF-kB and the expression of cyclooxigenase-2 (COX-2) and nitric oxide (NO) synthase pro-inflammatory enzymes, in a colon carcinogenic rat model (98, 99). Moreover, recent findings demonstrated that cocoa suppresses the development of colitis-associated tumorigenesis by modulating NF-kB/IL-6/Signal transducer and activator of transcription 3 (STAT3) signaling pathways and also induces apoptosis by activating caspase-3 in a mouse model (103).
Evidence has been provided that pomegranate phenolic extract (PE) and/or its microbiota derived metabolite-urolithin-A (UROA), have antioxidant, anti-inflammatory, and anticancer properties as showed by Larrosa et al. (104). They demonstrated that pomegranate could prevent colon inflammation before and during colitis disease in rats. PE and UROA decreased inflammation markers (iNOS, COX-2, prostaglandin E synthase, and prostaglandin E2) in colonic mucosa and could have a beneficial effect on the gut microbiota.
Flavanol extract from Chaenomeles japonica, a Japanese fruit, inhibited COX-2, matrix metalloproteinase-9 (MMP-9), and NF-kB expression indicating a cytotoxic anti-inflammatory and anti-metastatic activities toward the colon cancer SW-480 cells (105).
A recent study has shown that sugarcane extracts, containing a potent reservoir of polyphenols, provide anti-inflammatory activity by decreasing NF-kB phosphorylation and subsequently reduced expression of IL-8 signaling in lipopolysaccharide-stimulated colon cancer cells (106).
Edible mushroom (Pleurotus eryngii), rich in polyphenols, has been shown to inhibit the production of pro-inflammatory molecules, such as ROS and NO in RAW264.7 macrophage cell line and to induce an anti-proliferative effect on HCT116 colon cancer cells (107). All these results indicate the relevance of dietary polyphenol intake derived from food throughout the world.
The consumption of many varieties of plant derivatives is very ancient remedy against all kinds of ailments. Since ancient times folk medicine has made use of plants like Opuntia ficus indica and Ceratonia Siliqua and recently their polyphenolic extracts have received much attention for their antioxidant, anti-inflammatory, immunomodulatory and anticancer properties. Aboura et al. demonstrated the protective effects of polyphenol-rich infusions from C. Siliqua leaves on inflammation either in in vitro and in vivo experimental models, reducing pro-inflammatory cytokine expression (such as TNF-α, IL-1β, and IL-6), and NO production (108). The anti-inflammatory activity of Garcinia Kola (109) and Ocimum Gratissimum (110) polyphenolic extracts is exerted by reducing TNF-α and pro-inflammatory cytokine production in a rat colitis experimental model.
Potential Role of Polyphenols in CRC Prevention and Therapy
Decades of research on bioactive compounds have highlighted the beneficial effects of anti-inflammatory polyphenols not only in preventing cancer, but also in potentiating the efficacy of chemo/radiotherapy and reducing the risk of tumor recurrence (111).
Primary prevention of colon cancer, using dietary agents, boasts a widespread use in healthy populations (112) and in IBD patients at high risk of developing CRC (113).
Protective effects of apple and berry fruits against colon cancer have been demonstrated in in vivo studies. The Apc Min+ mouse model has been used to show the chemopreventive effects of Annurca apple polyphenol extract, which decreased polyp numbers and size, in animals fed a balanced-diet and also counteracted the tumorigenic effect of a diet rich in fats (114).
The chemopreventive effect of black raspberries (BRB) in DSS-mice was mediated by the downregulation of the pro-inflammatory cytokine expression including TNF-α and IL-1β (115) and the decrease of COX-2 and plasma prostaglandin E2 levels. Furthermore, Pan et al. performed a comprehensive analysis of BRB metabolic profiles correlated with a decrease of polyp number and size in Apc Min+ mice (116).
Consistent with the well-known antioxidant and anti-inflammatory properties of resveratrol (117) Cui et al. reported a decrease of colon inflammation score through the down regulation of mucosal and/or systemic TNF-α and IFN-γ expression in a mouse model of colitis (75). IL-10-deficient mouse, a well-documented model for colitis-associated cancer, was used to investigate the chemopreventive properties of curcumin which has been shown to have anti-inflammatory, anti-oxidative and anti-proliferative properties. The chemopreventive effect of curcumin reduced colonic tumor burden and was associated with the maintenance of a high microbial diversity (118).
Polyphenols may also behave as pro-oxidants (119, 120), triggering ROS-mediated cancer cell death (121, 122), affecting tumor cell behavior based on differential redox status of cancer cells comparing with normal ones (123). Cocoplum (Chrysobalanus icaco L.) anthocyanin-rich tropical fruit exerts anti-inflammatory activity through the reduction of TNF-α, IL-1β, IL-6, and NF-κB expressions and pro-oxidant effect on HT-29 human colorectal adenocarcinoma cells (124).
Conventional radio/chemotherapeutic treatment may induce immunogenic cell death (ICD), essential for activation of a T cell dependent immune response specific for dead cell-derived antigens. The improved efficacy of cancer therapy when tumor cells undergo an ICD (125–127) leads to the stimulation of T cells by DC through capture, processing, and presentation of antigens to naïve CD4+ and CD8+ T cells, which in turn elicit an antitumor response (128). In CRC patients clinical applications of therapeutic drugs have been greatly restricted due to the acquired chemoresistance as well as side-effect toxicity (129). These limitations highlight the need for development of novel anti-tumor strategies that may enhance chemosensitivity of tumor cells and reduce toxicity (130).
The concept of combined therapy of anti-cancer drugs with natural compounds has become a very promising approach in designing effective clinical trials. Evidence is emerging that conventional chemotherapy in CRC significantly benefits through combined treatment with some natural dietary polyphenols (131–135). Indeed several studies have demonstrated the effective and enhanced anticancer activity of 5-Fluorouracil (5-FU) in combination with natural compounds and suggested the possibility of reducing dose-related toxicity and resistance to this drug (136, 137). This effect has been demonstrated by Hakim et al. who combined treatment of Gelam honey and ginger (Zingiber officinale) phenolic acid rich-extracts to enhance the chemotherapeutic effect of 5-FU against a colon adenocarcinoma cell line (138).
In recent years several studies have demonstrated the presence and the relevance of cancer stem cells (CSC) in different tumors including CRC (139–141). These cells are hypothesized to be responsible for tumor relapse and resistance to conventional therapies. Novel anticancer strategies have been designed to selectively target CSC and in this scenario natural polyphenols might have a relevant role.
Shakibaei et al. illustrated interesting effects of curcumin in enhancing chemosensitization to 5-FU-based chemotherapy by targeting the CSC subpopulation (142). Dietary bioactive polyphenolic metabolites derived from pomegranate and berries reduced the number and size of CSC colonspheres and modulated chemotherapy resistance (143).
Given that gastrointestinal cancer cells are poorly responsive to ionizing radiation treatment, novel radiosensitizer agents are required to improve the efficacy of CRC radiotherapy. Fisetin, a dietary flavonoid, has been demonstrated to enhance the radiosensitivity of p53-mutant HT-29 human colorectal cancer cells by increasing radiation induced DNA double strand breaks (144).
Conclusions
The current review reports recent epidemiological and experimental data supporting the bright future of dietary polyphenols as chemopreventive, anti-inflammatory, immunomodulatory, and anticancer agents in CRC (Figure 1). The polyphenol-rich diet not only may represent a chemopreventive treatment but also has important function on immune system by promoting symbiont and commensal bacterial populations, increases reciprocal interaction between host and microbiota which in turn have important effects on immune function Evidence underlines the use of polyphenols as sensitizers of chemo/radiotherapies paving the way for new combined strategies able to minimize toxicity and side effects of conventional treatment in oncological patients. In the new era of precision medicine it would be important to consider the oxidative status prior to polyphenol supplementation or dietary advice. Recent advance in metabolomics might reveal individual oxidative bio-signatures of cancer patients leading to a personalized treatment approach.
Further studies are needed to deeply evaluate the immunomodulatory role of polyphenols to improve the efficacy of novel treatment such as immune checkpoint blockade, a new reality in oncology.
Author Contributions
SM and AM have made a substantial, direct and intellectual contribution to the article designing. PN contributed to the writing and revised the article. All authors have reviewed and approved the final version of the manuscript for publication.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We apologize to those authors whose work could not be cited due to a space limitation.
Footnotes
Funding. PN is supported by AIRC (IG #19822; 5 × mille #12182).
References
- 1.Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. (2018) 68:394–424. 10.3322/caac.21492 [DOI] [PubMed] [Google Scholar]
- 2.Montenegro MF, Sanchez-del-Campo L, Fernandez-Perez MP, Saez-Ayala M, Cabezas-Herrera J, Rodriguez-Lopez JN. Targeting the epigenetic machinery of cancer cells. Oncogene. (2015) 34:135–43. 10.1038/onc.2013.605 [DOI] [PubMed] [Google Scholar]
- 3.Sapienza C, Issa JP. Diet, nutrition, and cancer epigenetics. Annu Rev Nutr. (2016) 36:665–81. 10.1146/annurev-nutr-121415-112634 [DOI] [PubMed] [Google Scholar]
- 4.Bishop KS, Ferguson LR. The interaction between epigenetics, nutrition and the development of cancer. Nutrients. (2015) 7:922–47. 10.3390/nu7020922 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Aggarwal BB, Danda D, Gupta S, Gehlot P. Models for prevention and treatment of cancer: problems vs promises. Biochem Pharmacol. (2009) 78:1083–94. 10.1016/j.bcp.2009.05.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lavalette C, Adjibade M, Srour B, Sellem L, Fiolet T, Hercberg S, et al. Cancer-specific and general nutritional scores and cancer risk: results from the prospective nutrinet-sante cohort. Cancer Res. (2018) 78:4427–35. 10.1158/0008-5472.CAN-18-0155 [DOI] [PubMed] [Google Scholar]
- 7.Vineis P, Wild CP. Global cancer patterns: causes and prevention. Lancet. (2014) 383:549–57. 10.1016/S0140-6736(13)62224-2 [DOI] [PubMed] [Google Scholar]
- 8.Mantovani A, Allavena P, Sica A, Balkwill F. Cancer-related inflammation. Nature. (2008) 454:436–44. 10.1038/nature07205 [DOI] [PubMed] [Google Scholar]
- 9.Rogler G. Chronic ulcerative colitis and colorectal cancer. Cancer Lett. (2014) 345:235–41. 10.1016/j.canlet.2013.07.032 [DOI] [PubMed] [Google Scholar]
- 10.Hanahan D, Weinberg RA. Hallmarks of cancer: the next generation. Cell. (2011) 144:646–74. 10.1016/j.cell.2011.02.013 [DOI] [PubMed] [Google Scholar]
- 11.Morrison DS, Parr CL, Lam TH, Ueshima H, Kim HC, Jee SH, et al. Behavioural and metabolic risk factors for mortality from colon and rectum cancer: analysis of data from the Asia-Pacific Cohort Studies Collaboration. Asian Pac J Cancer Prev. (2013) 14:1083–7. 10.7314/APJCP.2013.14.2.1083 [DOI] [PubMed] [Google Scholar]
- 12.Dabritz J, Menheniott TR. Linking immunity, epigenetics, and cancer in inflammatory bowel disease. Inflamm Bowel Dis. (2014) 20:1638–54. 10.1097/MIB.0000000000000063 [DOI] [PubMed] [Google Scholar]
- 13.Favoriti P, Carbone G, Greco M, Pirozzi F, Pirozzi RE, Corcione F. Worldwide burden of colorectal cancer: a review. Updates Surg. (2016) 68:7–11. 10.1007/s13304-016-0359-y [DOI] [PubMed] [Google Scholar]
- 14.Belkaid Y, Harrison OJ. Homeostatic immunity and the microbiota. Immunity. (2017) 46:562–76. 10.1016/j.immuni.2017.04.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Raskov H, Pommergaard HC, Burcharth J, Rosenberg J. Colorectal carcinogenesis–update and perspectives. World J Gastroenterol. (2014) 20:18151–64. 10.3748/wjg.v20.i48.18151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Llosa NJ, Cruise M, Tam A, Wicks EC, Hechenbleikner EM, Taube JM, et al. The vigorous immune microenvironment of microsatellite instable colon cancer is balanced by multiple counter-inhibitory checkpoints. Cancer Discov. (2015) 5:43–51. 10.1158/2159-8290.CD-14-0863 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Galon J, Costes A, Sanchez-Cabo F, Kirilovsky A, Mlecnik B, Lagorce-Pages C, et al. Type, density, and location of immune cells within human colorectal tumors predict clinical outcome. Science. (2006) 313:1960–4. 10.1126/science.1129139 [DOI] [PubMed] [Google Scholar]
- 18.Roy S, Trinchieri G. Microbiota: a key orchestrator of cancer therapy. Nat Rev Cancer. (2017) 17:271–85. 10.1038/nrc.2017.13 [DOI] [PubMed] [Google Scholar]
- 19.Sung B, Prasad S, Yadav VR, Lavasanifar A, Aggarwal BB. Cancer and diet: how are they related? Free Radic Res. (2011) 45:864–79. 10.3109/10715762.2011.582869 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bishayee A, Sethi G. Bioactive natural products in cancer prevention and therapy: progress and promise. Semin Cancer Biol. (2016) 40–41:1–13. 10.1016/j.semcancer.2016.08.006 [DOI] [PubMed] [Google Scholar]
- 21.Colotta F, Allavena P, Sica A, Garlanda C, Mantovani A. Cancer-related inflammation, the seventh hallmark of cancer: links to genetic instability. Carcinogenesis. (2009) 30:1073–81. 10.1093/carcin/bgp127 [DOI] [PubMed] [Google Scholar]
- 22.Inacio Pinto N, Carnier J, Oyama LM, Otoch JP, Alcantara PS, Tokeshi F, et al. Cancer as a proinflammatory environment: metastasis and cachexia. Mediat Inflamm. (2015) 2015:791060. 10.1155/2015/791060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Grivennikov SI, Greten FR, Karin M. Immunity, inflammation, and cancer. Cell. (2010) 140:883–99. 10.1016/j.cell.2010.01.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sauer S, Plauth A. Health-beneficial nutraceuticals-myth or reality? Appl Microbiol Biotechnol. (2017) 101:951–61. 10.1007/s00253-016-8068-5 [DOI] [PubMed] [Google Scholar]
- 25.Sistigu A, Di Modugno F, Manic G, Nistico P. Deciphering the loop of epithelial-mesenchymal transition, inflammatory cytokines and cancer immunoediting. Cytokine Growth Factor Rev. (2017) 36:67–77. 10.1016/j.cytogfr.2017.05.008 [DOI] [PubMed] [Google Scholar]
- 26.Becht E, de Reynies A, Giraldo NA, Pilati C, Buttard B, Lacroix L, et al. Immune and stromal classification of colorectal cancer is associated with molecular subtypes and relevant for precision immunotherapy. Clin Cancer Res. (2016) 22:4057–66. 10.1158/1078-0432.CCR-15-2879 [DOI] [PubMed] [Google Scholar]
- 27.Chikara S, Nagaprashantha LD, Singhal J, Horne D, Awasthi S, Singhal SS. Oxidative stress and dietary phytochemicals: role in cancer chemoprevention and treatment. Cancer Lett. (2018) 413:122–34. 10.1016/j.canlet.2017.11.002 [DOI] [PubMed] [Google Scholar]
- 28.Yang CS, Wang X, Lu G, Picinich SC. Cancer prevention by tea: animal studies, molecular mechanisms and human relevance. Nat Rev Cancer. (2009) 9:429–39. 10.1038/nrc2641 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Elshaer M, Chen Y, Wang XJ, Tang X. Resveratrol: an overview of its anti-cancer mechanisms. Life Sci. (2018) 207:3409. 10.1016/j.lfs.2018.06.028 [DOI] [PubMed] [Google Scholar]
- 30.Alam MN, Almoyad M, Huq F. Polyphenols in colorectal cancer: current state of knowledge including clinical trials and molecular mechanism of action. Biomed Res Int. (2018) 2018:4154185. 10.1155/2018/4154185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tse G, Eslick GD. Cruciferous vegetables and risk of colorectal neoplasms: a systematic review and meta-analysis. Nutr Cancer. (2014) 66:128–39. 10.1080/01635581.2014.852686 [DOI] [PubMed] [Google Scholar]
- 32.Shafiee G, Saidijam M, Tavilani H, Ghasemkhani N, Khodadadi I. Genistein induces apoptosis and inhibits proliferation of HT29 colon cancer cells. Int J Mol Cell Med. (2016) 5:178–91. 10.22088/acadpub.bums.5.3.178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Schwingshackl L, Hoffmann G. Adherence to Mediterranean diet and risk of cancer: a systematic review and meta-analysis of observational studies. Int J Cancer. (2014) 135:1884–97. 10.1002/ijc.28824 [DOI] [PubMed] [Google Scholar]
- 34.Schwingshackl L, Schwedhelm C, Galbete C, Hoffmann G. Adherence to mediterranean diet and risk of cancer: an updated systematic review and meta-analysis. Nutrients. (2017) 9:10. 10.3390/nu9101063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ghiringhelli F, Rebe C, Hichami A, Delmas D. Immunomodulation and anti-inflammatory roles of polyphenols as anticancer agents. Anticancer Agents Med Chem. (2012) 12:852–73. 10.2174/187152012802650048 [DOI] [PubMed] [Google Scholar]
- 36.Watson RR. Polyphenols in Plants: Isolation, Purification and Extract Preparation. Amsterdam: Elsevier Science; (2014). [Google Scholar]
- 37.Ding S, Jiang H, Fang J. Regulation of immune function by polyphenols. J Immunol Res. (2018) 2018:1264074. 10.1155/2018/1264074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Zhou Y, Zheng J, Li Y, Xu DP, Li S, Chen YM, et al. Natural polyphenols for prevention and treatment of cancer. Nutrients. (2016) 8:8. 10.3390/nu8080515 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Mileo AM, Di Venere D, Linsalata V, Fraioli R, Miccadei S. Artichoke polyphenols induce apoptosis and decrease the invasive potential of the human breast cancer cell line MDA-MB231. J Cell Physiol. (2012) 227:3301–9. 10.1002/jcp.24029 [DOI] [PubMed] [Google Scholar]
- 40.Visioli F, De La Lastra CA, Andres-Lacueva C, Aviram M, Calhau C, Cassano A, et al. Polyphenols and human health: a prospectus. Crit Rev Food Sci Nutr. (2011) 51:524–46. 10.1080/10408391003698677 [DOI] [PubMed] [Google Scholar]
- 41.Dragan S, Andrica F, Serban MC, Timar R. Polyphenols-rich natural products for treatment of diabetes. Curr Med Chem. (2015) 22:14–22. 10.2174/0929867321666140826115422 [DOI] [PubMed] [Google Scholar]
- 42.Wang S, Moustaid-Moussa N, Chen L, Mo H, Shastri A, Su R, et al. Novel insights of dietary polyphenols and obesity. J Nutr Biochem. (2014) 25:1–18. 10.1016/j.jnutbio.2013.09.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ali F, Ismail A, Kersten S. Molecular mechanisms underlying the potential antiobesity-related diseases effect of cocoa polyphenols. Mol Nutr Food Res. (2014) 58:33–48. 10.1002/mnfr.201300277 [DOI] [PubMed] [Google Scholar]
- 44.Magrone T, Russo MA, Jirillo E. Cocoa and dark chocolate polyphenols: from biology to clinical applications. Front Immunol. (2017) 8:677. 10.3389/fimmu.2017.00677 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hossen MS, Ali MY, Jahurul MHA, Abdel-Daim MM, Gan SH, Khalil MI. Beneficial roles of honey polyphenols against some human degenerative diseases: a review. Pharmacol Rep. (2017) 69:1194–205. 10.1016/j.pharep.2017.07.002 [DOI] [PubMed] [Google Scholar]
- 46.Bhullar KS, Rupasinghe HP. Polyphenols: multipotent therapeutic agents in neurodegenerative diseases. Oxid Med Cell Longev. (2013) 2013:891748. 10.1155/2013/891748 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Yamagata K, Tagami M, Yamori Y. Dietary polyphenols regulate endothelial function and prevent cardiovascular disease. Nutrition. (2015) 31:28–37. 10.1016/j.nut.2014.04.011 [DOI] [PubMed] [Google Scholar]
- 48.Cardona F, Andres-Lacueva C, Tulipani S, Tinahones FJ, Queipo-Ortuno MI. Benefits of polyphenols on gut microbiota and implications in human health. J Nutr Biochem. (2013) 24:1415–22. 10.1016/j.jnutbio.2013.05.001 [DOI] [PubMed] [Google Scholar]
- 49.Tap J, Furet JP, Bensaada M, Philippe C, Roth H, Rabot S, et al. Gut microbiota richness promotes its stability upon increased dietary fibre intake in healthy adults. Environ Microbiol. (2015) 17:4954–64. 10.1111/1462-2920.13006 [DOI] [PubMed] [Google Scholar]
- 50.Macpherson AJ, Harris NL. Interactions between commensal intestinal bacteria and the immune system. Nat Rev Immunol. (2004) 4:478–85. 10.1038/nri1373 [DOI] [PubMed] [Google Scholar]
- 51.Pickard JM, Chervonsky AV. Intestinal fucose as a mediator of host-microbe symbiosis. J Immunol. (2015) 194:5588–93. 10.4049/jimmunol.1500395 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Yang Y, Xu C, Wu D, Wang Z, Wu P, Li L, et al. gammadelta T cells: crosstalk between microbiota, chronic inflammation, and colorectal cancer. Front Immunol. (2018) 9:1483. 10.3389/fimmu.2018.01483 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Rescigno M. Intestinal microbiota and its effects on the immune system. Cell Microbiol. (2014) 16:1004–13. 10.1111/cmi.12301 [DOI] [PubMed] [Google Scholar]
- 54.Biragyn A, Ferrucci L. Gut dysbiosis: a potential link between increased cancer risk in ageing and inflammaging. Lancet Oncol. (2018) 19:e295–e304. 10.1016/S1470-2045(18)30095-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Zitvogel L, Galluzzi L, Viaud S, Vetizou M, Daillere R, Merad M, et al. Cancer and the gut microbiota: an unexpected link. Sci Transl Med. (2015) 7:271ps1. 10.1126/scitranslmed.3010473 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Sheflin AM, Whitney AK, Weir TL. Cancer-promoting effects of microbial dysbiosis. Curr Oncol Rep. (2014) 16:406. 10.1007/s11912-014-0406-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Sun J, Kato I. Gut microbiota, inflammation and colorectal cancer. Genes Dis. (2016) 3:130–43. 10.1016/j.gendis.2016.03.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Jahani-Sherafat S, Alebouyeh M, Moghim S, Ahmadi Amoli H, Ghasemian-Safaei H. Role of gut microbiota in the pathogenesis of colorectal cancer; a review article. Gastroenterol Hepatol Bed Bench. (2018) 11:101–9. [PMC free article] [PubMed] [Google Scholar]
- 59.Kawabata K, Yoshioka Y, Terao J. Role of intestinal microbiota in the bioavailability and physiological functions of dietary polyphenols. Molecules. (2019) 24:2. 10.3390/molecules24020370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Ricciardiello L, Bazzoli F, Fogliano V. Phytochemicals and colorectal cancer prevention–myth or reality? Nat Rev Gastroenterol Hepatol. (2011) 8:592–6. 10.1038/nrgastro.2011.149 [DOI] [PubMed] [Google Scholar]
- 61.Chow HH, Hakim IA. Pharmacokinetic and chemoprevention studies on tea in humans. Pharmacol Res. (2011) 64:105–12. 10.1016/j.phrs.2011.05.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Ju S, Ge Y, Li P, Tian X, Wang H, Zheng X, et al. Dietary quercetin ameliorates experimental colitis in mouse by remodeling the function of colonic macrophages via a heme oxygenase-1-dependent pathway. Cell Cycle. (2018) 17:53–63. 10.1080/15384101.2017.1387701 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Farinetti A, Zurlo V, Manenti A, Coppi F, Mattioli AV. Mediterranean diet and colorectal cancer: a systematic review. Nutrition. (2017) 43–44:83–88. 10.1016/j.nut.2017.06.008 [DOI] [PubMed] [Google Scholar]
- 64.Soldati L, Di Renzo L, Jirillo E, Ascierto PA, Marincola FM, De Lorenzo A. The influence of diet on anti-cancer immune responsiveness. J Transl Med. (2018) 16:75. 10.1186/s12967-018-1448-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Ostan R, Lanzarini C, Pini E, Scurti M, Vianello D, Bertarelli C, et al. Inflammaging and cancer: a challenge for the Mediterranean diet. Nutrients. (2015) 7:2589–621. 10.3390/nu7042589 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Hardy TM, Tollefsbol TO. Epigenetic diet: impact on the epigenome and cancer. Epigenomics. (2011) 3:503–18. 10.2217/epi.11.71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Kroemer G, Zitvogel L. Cancer immunotherapy in 2017: the breakthrough of the microbiota. Nat Rev Immunol. (2018) 18:87–8. 10.1038/nri.2018.4 [DOI] [PubMed] [Google Scholar]
- 68.Nosrati N, Bakovic M, Paliyath G. Molecular mechanisms and pathways as targets for cancer prevention and progression with dietary compounds. Int J Mol Sci. (2017) 18:10. 10.3390/ijms18102050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Bhattacharyya S, Md Sakib Hossain D, Mohanty S, Sankar Sen G, Chattopadhyay S, Banerjee S, et al. Curcumin reverses T cell-mediated adaptive immune dysfunctions in tumor-bearing hosts. Cell Mol Immunol. (2010) 7:306–15. 10.1038/cmi.2010.11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Zou T, Yang Y, Xia F, Huang A, Gao X, Fang D, et al. Resveratrol inhibits CD4+ T cell activation by enhancing the expression and activity of Sirt1. PLoS ONE. (2013) 8:e75139. 10.1371/journal.pone.0075139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Yao J, Wei C, Wang JY, Zhang R, Li YX, Wang LS. Effect of resveratrol on Treg/Th17 signaling and ulcerative colitis treatment in mice. World J Gastroenterol. (2015) 21:6572–81. 10.3748/wjg.v21.i21.6572 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Ohno M, Nishida A, Sugitani Y, Nishino K, Inatomi O, Sugimoto M, et al. Nanoparticle curcumin ameliorates experimental colitis via modulation of gut microbiota and induction of regulatory T cells. PLoS ONE. (2017) 12:e0185999. 10.1371/journal.pone.0185999 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Hong EH, Heo EY, Song JH, Kwon BE, Lee JY, Park Y, et al. Trans-scirpusin A showed antitumor effects via autophagy activation and apoptosis induction of colorectal cancer cells. Oncotarget. (2017) 8:41401–11. 10.18632/oncotarget.17388 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Zhang Z, Wu X, Cao S, Cromie M, Shen Y, Feng Y, et al. Chlorogenic acid ameliorates experimental colitis by promoting growth of akkermansia in mice. Nutrients. (2017) 9:7. 10.3390/nu9070677 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Cui X, Jin Y, Hofseth AB, Pena E, Habiger J, Chumanevich A, et al. Resveratrol suppresses colitis and colon cancer associated with colitis. Cancer Prev Res. (2010) 3:549–59. 10.1158/1940-6207.CAPR-09-0117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Churchill M, Chadburn A, Bilinski RT, Bertagnolli MM. Inhibition of intestinal tumors by curcumin is associated with changes in the intestinal immune cell profile. J Surg Res. (2000) 89:169–75. 10.1006/jsre.2000.5826 [DOI] [PubMed] [Google Scholar]
- 77.Skyberg JA, Robison A, Golden S, Rollins MF, Callis G, Huarte E, et al. Apple polyphenols require T cells to ameliorate dextran sulfate sodium-induced colitis and dampen proinflammatory cytokine expression. J Leukoc Biol. (2011) 90:1043–54. 10.1189/jlb.0311168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Wang B, Wu C. Dietary soy isoflavones alleviate dextran sulfate sodium-induced inflammation and oxidative stress in mice. Exp Ther Med. (2017) 14:276–82. 10.3892/etm.2017.4469 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Wagner AE, Will O, Sturm C, Lipinski S, Rosenstiel P, Rimbach G. DSS-induced acute colitis in C57BL/6 mice is mitigated by sulforaphane pre-treatment. J Nutr Biochem. (2013) 24:2085–91. 10.1016/j.jnutbio.2013.07.009 [DOI] [PubMed] [Google Scholar]
- 80.Ramiro-Puig E, Perez-Cano FJ, Ramos-Romero S, Perez-Berezo T, Castellote C, Permanyer J, et al. Intestinal immune system of young rats influenced by cocoa-enriched diet. J Nutr Biochem. (2008) 19:555–65. 10.1016/j.jnutbio.2007.07.002 [DOI] [PubMed] [Google Scholar]
- 81.Ma B, Khazali A, Wells A. CXCR3 in carcinoma progression. Histol Histopathol. (2015) 30:781–92. 10.14670/HH-11-594 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Abron JD, Singh NP, Murphy AE, Mishra MK, Price RL, Nagarkatti M, et al. Differential role of CXCR3 in inflammation and colorectal cancer. Oncotarget. (2018) 9:17928–36. 10.18632/oncotarget.24730 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Legitimo A, Consolini R, Failli A, Orsini G, Spisni R. Dendritic cell defects in the colorectal cancer. Hum Vaccin Immunother. (2014) 10:3224–35. 10.4161/hv.29857 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Malietzis G, Lee GH, Jenkins JT, Bernardo D, Moorghen M, Knight SC, et al. Prognostic value of the tumour-infiltrating dendritic cells in colorectal cancer: a systematic review. Cell Commun Adhes. (2015) 22:9–14. 10.3109/15419061.2015.1036859 [DOI] [PubMed] [Google Scholar]
- 85.Kajihara M, Takakura K, Kanai T, Ito Z, Saito K, Takami S, et al. Dendritic cell-based cancer immunotherapy for colorectal cancer. World J Gastroenterol. (2016) 22:4275–86. 10.3748/wjg.v22.i17.4275 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.del Corno M, Scazzocchio B, Masella R, Gessani S. Regulation of dendritic cell function by dietary polyphenols. Crit Rev Food Sci Nutr. (2016) 56:737–47. 10.1080/10408398.2012.713046 [DOI] [PubMed] [Google Scholar]
- 87.Deng Z, Rong Y, Teng Y, Mu J, Zhuang X, Tseng M, et al. Broccoli-derived nanoparticle inhibits mouse colitis by activating dendritic cell AMP-activated protein kinase. Mol Ther. (2017) 25:1641–54. 10.1016/j.ymthe.2017.01.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Del Corno M, Varano B, Scazzocchio B, Filesi C, Masella R, Gessani S. Protocatechuic acid inhibits human dendritic cell functional activation: role of PPARgamma up-modulation. Immunobiology. (2014) 219:416–24. 10.1016/j.imbio.2014.01.007 [DOI] [PubMed] [Google Scholar]
- 89.Cavalcanti E, Vadrucci E, Delvecchio FR, Addabbo F, Bettini S, Liou R, et al. Administration of reconstituted polyphenol oil bodies efficiently suppresses dendritic cell inflammatory pathways and acute intestinal inflammation. PLoS ONE. (2014) 9:e88898. 10.1371/journal.pone.0088898 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.De Santis S, Kunde D, Serino G, Galleggiante V, Caruso ML, Mastronardi M, et al. Secretory leukoprotease inhibitor is required for efficient quercetin-mediated suppression of TNFalpha secretion. Oncotarget. (2016) 7:75800–9. 10.18632/oncotarget.12415 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Ghattamaneni NKR, Panchal SK, Brown L. Nutraceuticals in rodent models as potential treatments for human Inflammatory Bowel Disease. Pharmacol Res. (2018) 132:99–107. 10.1016/j.phrs.2018.04.015 [DOI] [PubMed] [Google Scholar]
- 92.Kaulmann A, Bohn T. Bioactivity of polyphenols: preventive and adjuvant strategies toward reducing inflammatory bowel diseases-promises, perspectives, and pitfalls. Oxid Med Cell Longev. (2016) 2016:9346470. 10.1155/2016/9346470 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Guan G, Lan S. Implications of antioxidant systems in inflammatory bowel disease. Biomed Res Int. (2018) 2018:1290179. 10.1155/2018/1290179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Lee CY, Nanah CN, Held RA, Clark AR, Huynh UG, Maraskine MC, et al. Effect of electron donating groups on polyphenol-based antioxidant dendrimers. Biochimie. (2015) 111:125–34. 10.1016/j.biochi.2015.02.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Kalaiselvan I, Samuthirapandi M, Govindaraju A, Sheeja Malar D, Kasi PD. Olive oil and its phenolic compounds (hydroxytyrosol and tyrosol) ameliorated TCDD-induced heptotoxicity in rats via inhibition of oxidative stress and apoptosis. Pharm Biol. (2016) 54:338–46. 10.3109/13880209.2015.1042980 [DOI] [PubMed] [Google Scholar]
- 96.Gosslau A, En Jao DL, Huang MT, Ho CT, Evans D, Rawson NE, et al. Effects of the black tea polyphenol theaflavin-2 on apoptotic and inflammatory pathways in vitro and in vivo. Mol Nutr Food Res. (2011) 55:198–208. 10.1002/mnfr.201000165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Zhang H, Tsao R. Dietary polyphenols, oxidative stress and antioxidant and anti-inflammatory effects. Curr Opin Food Sci. (2016) 8:33–42. 10.1016/j.cofs.2016.02.002 [DOI] [Google Scholar]
- 98.Rodriguez-Ramiro I, Ramos S, Lopez-Oliva E, Agis-Torres A, Bravo L, Goya L, et al. Cocoa polyphenols prevent inflammation in the colon of azoxymethane-treated rats and in TNF-alpha-stimulated Caco-2 cells. Br J Nutr. (2013) 110:206–15. 10.1017/S0007114512004862 [DOI] [PubMed] [Google Scholar]
- 99.Rodriguez-Ramiro I, Ramos S, Bravo L, Goya L, Martin MA. Procyanidin B2 and a cocoa polyphenolic extract inhibit acrylamide-induced apoptosis in human Caco-2 cells by preventing oxidative stress and activation of JNK pathway. J Nutr Biochem. (2011) 22:1186–94. 10.1016/j.jnutbio.2010.10.005 [DOI] [PubMed] [Google Scholar]
- 100.Sahu BD, Kumar JM, Sistla R. Fisetin, a dietary flavonoid, ameliorates experimental colitis in mice: relevance of NF-kappaB signaling. J Nutr Biochem. (2016) 28:171–82. 10.1016/j.jnutbio.2015.10.004 [DOI] [PubMed] [Google Scholar]
- 101.Serra G, Incani A, Serreli G, Porru L, Melis MP, Tuberoso CIG, et al. Olive oil polyphenols reduce oxysterols -induced redox imbalance and pro-inflammatory response in intestinal cells. Redox Biol. (2018) 17:348–54. 10.1016/j.redox.2018.05.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Oz HS, Chen T, de Villiers WJ. Green tea polyphenols and sulfasalazine have parallel anti-inflammatory properties in colitis models. Front Immunol. (2013) 4:132. 10.3389/fimmu.2013.00132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Saadatdoust Z, Pandurangan AK, Ananda Sadagopan SK, Mohd Esa N, Ismail A, Mustafa MR. Dietary cocoa inhibits colitis associated cancer: a crucial involvement of the IL-6/STAT3 pathway. J Nutr Biochem. (2015) 26:1547–58. 10.1016/j.jnutbio.2015.07.024 [DOI] [PubMed] [Google Scholar]
- 104.Larrosa M, Gonzalez-Sarrias A, Yanez-Gascon MJ, Selma MV, Azorin-Ortuno M, Toti S, et al. Anti-inflammatory properties of a pomegranate extract and its metabolite urolithin-A in a colitis rat model and the effect of colon inflammation on phenolic metabolism. J Nutr Biochem. (2010) 21:717–25. 10.1016/j.jnutbio.2009.04.012 [DOI] [PubMed] [Google Scholar]
- 105.Owczarek K, Hrabec E, Fichna J, Sosnowska D, Koziolkiewicz M, Szymanski J, et al. Flavanols from Japanese quince (Chaenomeles japonica) fruit suppress expression of cyclooxygenase-2, metalloproteinase-9, and nuclear factor-kappaB in human colon cancer cells. Acta Biochim Pol. (2017) 64:567–76. 10.18388/abp.2017_1599 [DOI] [PubMed] [Google Scholar]
- 106.Bucio-Noble D, Kautto L, Krisp C, Ball MS, Molloy MP. Polyphenol extracts from dried sugarcane inhibit inflammatory mediators in an in vitro colon cancer model. J Proteomics. (2018) 177:1–10. 10.1016/j.jprot.2018.02.009 [DOI] [PubMed] [Google Scholar]
- 107.Hu Q, Yuan B, Xiao H, Zhao L, Wu X, Rakariyatham K, et al. Polyphenols-rich extract from Pleurotus eryngii with growth inhibitory of HCT116 colon cancer cells and anti-inflammatory function in RAW264.7 cells. Food Funct. (2018) 9:1601–11. 10.1039/C7FO01794D [DOI] [PubMed] [Google Scholar]
- 108.Aboura I, Nani A, Belarbi M, Murtaza B, Fluckiger A, Dumont A, et al. Protective effects of polyphenol-rich infusions from carob (Ceratonia siliqua) leaves and cladodes of Opuntia ficus-indica against inflammation associated with diet-induced obesity and DSS-induced colitis in Swiss mice. Biomed Pharmacother. (2017) 96:1022–35. 10.1016/j.biopha.2017.11.125 [DOI] [PubMed] [Google Scholar]
- 109.Farombi EO, Adedara IA, Ajayi BO, Ayepola OR, Egbeme EE. Kolaviron, a natural antioxidant and anti-inflammatory phytochemical prevents dextran sulphate sodium-induced colitis in rats. Basic Clin Pharmacol Toxicol. (2013) 113:49–55. 10.1111/bcpt.12050 [DOI] [PubMed] [Google Scholar]
- 110.Alabi QK, Akomolafe RO, Omole JG, Adefisayo MA, Ogundipe OL, Aturamu A, et al. Polyphenol-rich extract of Ocimum gratissimum leaves ameliorates colitis via attenuating colonic mucosa injury and regulating pro-inflammatory cytokines production and oxidative stress. Biomed Pharmacother. (2018) 103:812–22. 10.1016/j.biopha.2018.04.071 [DOI] [PubMed] [Google Scholar]
- 111.Asensi M, Ortega A, Mena S, Feddi F, Estrela JM. Natural polyphenols in cancer therapy. Crit Rev Clin Lab Sci. (2011) 48:197–216. 10.3109/10408363.2011.631268 [DOI] [PubMed] [Google Scholar]
- 112.Orlich MJ, Singh PN, Sabate J, Fan J, Sveen L, Bennett H, et al. Vegetarian dietary patterns and the risk of colorectal cancers. JAMA Intern Med. (2015) 175:767–76. 10.1001/jamainternmed.2015.59 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Halmos EP, Gibson PR. Dietary management of IBD–insights and advice. Nat Rev Gastroenterol Hepatol. (2015) 12:133–46. 10.1038/nrgastro.2015.11 [DOI] [PubMed] [Google Scholar]
- 114.Fini L, Piazzi G, Daoud Y, Selgrad M, Maegawa S, Garcia M, et al. Chemoprevention of intestinal polyps in ApcMin/+ mice fed with western or balanced diets by drinking annurca apple polyphenol extract. Cancer Prev Res. (2011) 4:907–15. 10.1158/1940-6207.CAPR-10-0359 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Montrose DC, Horelik NA, Madigan JP, Stoner GD, Wang LS, Bruno RS, et al. Anti-inflammatory effects of freeze-dried black raspberry powder in ulcerative colitis. Carcinogenesis. (2011) 32:343–50. 10.1093/carcin/bgq248 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Pan P, Skaer CW, Wang HT, Stirdivant SM, Young MR, Oshima K, et al. Black raspberries suppress colonic adenoma development in ApcMin/+ mice: relation to metabolite profiles. Carcinogenesis. (2015) 36:1245–53. 10.1093/carcin/bgv117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Ko JH, Sethi G, Um JY, Shanmugam MK, Arfuso F, Kumar AP, et al. The Role of resveratrol in cancer therapy. Int J Mol Sci. (2017) 18:12. 10.3390/ijms18122589 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.McFadden RM, Larmonier CB, Shehab KW, Midura-Kiela M, Ramalingam R, Harrison CA, et al. The role of curcumin in modulating colonic microbiota during colitis and colon cancer prevention. Inflamm Bowel Dis. (2015) 21:2483–94. 10.1097/MIB.0000000000000522 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Elbling L, Weiss RM, Teufelhofer O, Uhl M, Knasmueller S, Schulte-Hermann R, et al. Green tea extract and (-)-epigallocatechin-3-gallate, the major tea catechin, exert oxidant but lack antioxidant activities. FASEB J. (2005) 19:807–9. 10.1096/fj.04-2915fje [DOI] [PubMed] [Google Scholar]
- 120.Araujo JR, Goncalves P, Martel F. Chemopreventive effect of dietary polyphenols in colorectal cancer cell lines. Nutr Res. (2011) 31:77–87. 10.1016/j.nutres.2011.01.006 [DOI] [PubMed] [Google Scholar]
- 121.Khan HY, Zubair H, Ullah MF, Ahmad A, Hadi SM. A prooxidant mechanism for the anticancer and chemopreventive properties of plant polyphenols. Curr Drug Targets. (2012) 13:1738–49. 10.2174/138945012804545560 [DOI] [PubMed] [Google Scholar]
- 122.Mileo AM, Di Venere D, Miccadei S. Antitumour effects of artichoke polyphenols: cell death and ROS-mediated epigenetic growth arrest. Stem Cell Epigenet. (2016) 2016:3. [Google Scholar]
- 123.Khan HY, Zubair H, Faisal M, Ullah MF, Farhan M, Sarkar FH, et al. Plant polyphenol induced cell death in human cancer cells involves mobilization of intracellular copper ions and reactive oxygen species generation: a mechanism for cancer chemopreventive action. Mol Nutr Food Res. (2014) 58:437–46. 10.1002/mnfr.201300417 [DOI] [PubMed] [Google Scholar]
- 124.Venancio VP, Cipriano PA, Kim H, Antunes LM, Talcott ST, Mertens-Talcott SU. Cocoplum (Chrysobalanus icaco L.) anthocyanins exert anti-inflammatory activity in human colon cancer and non-malignant colon cells. Food Funct. (2017) 8:307–14. 10.1039/C6FO01498D [DOI] [PubMed] [Google Scholar]
- 125.Zitvogel L, Kepp O, Senovilla L, Menger L, Chaput N, Kroemer G. Immunogenic tumor cell death for optimal anticancer therapy: the calreticulin exposure pathway. Clin Cancer Res. (2010) 16:3100–4. 10.1158/1078-0432.CCR-09-2891 [DOI] [PubMed] [Google Scholar]
- 126.Lee CS, Ryan EJ, Doherty GA. Gastro-intestinal toxicity of chemotherapeutics in colorectal cancer: the role of inflammation. World J Gastroenterol. (2014) 20:3751–61. 10.3748/wjg.v20.i14.3751 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Golden EB, Apetoh L. Radiotherapy and immunogenic cell death. Semin Radiat Oncol. (2015) 25:11–7. 10.1016/j.semradonc.2014.07.005 [DOI] [PubMed] [Google Scholar]
- 128.Steinman RM, Banchereau J. Taking dendritic cells into medicine. Nature. (2007) 449:419–26. 10.1038/nature06175 [DOI] [PubMed] [Google Scholar]
- 129.Marin JJ, Sanchez de Medina F, Castano B, Bujanda L, Romero MR, Martinez-Augustin O, et al. Chemoprevention, chemotherapy, and chemoresistance in colorectal cancer. Drug Metab Rev. (2012) 44:148–72. 10.3109/03602532.2011.638303 [DOI] [PubMed] [Google Scholar]
- 130.Redondo-Blanco S, Fernandez J, Gutierrez-Del-Rio I, Villar CJ, Lombo F. New insights toward colorectal cancer chemotherapy using natural bioactive compounds. Front Pharmacol. (2017) 8:109. 10.3389/fphar.2017.00109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Yu Y, Kanwar SS, Patel BB, Nautiyal J, Sarkar FH, Majumdar AP. Elimination of colon cancer stem-like cells by the combination of curcumin and FOLFOX. Transl Oncol. (2009) 2:321–8. 10.1593/tlo.09193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Patel BB, Sengupta R, Qazi S, Vachhani H, Yu Y, Rishi AK, et al. Curcumin enhances the effects of 5-fluorouracil and oxaliplatin in mediating growth inhibition of colon cancer cells by modulating EGFR and IGF-1R. Int J Cancer. (2008) 122:267–73. 10.1002/ijc.23097 [DOI] [PubMed] [Google Scholar]
- 133.Aires V, Limagne E, Cotte AK, Latruffe N, Ghiringhelli F, Delmas D. Resveratrol metabolites inhibit human metastatic colon cancer cells progression and synergize with chemotherapeutic drugs to induce cell death. Mol Nutr Food Res. (2013) 57:1170–81. 10.1002/mnfr.201200766 [DOI] [PubMed] [Google Scholar]
- 134.Abouzeid AH, Patel NR, Rachman IM, Senn S, Torchilin VP. Anti-cancer activity of anti-GLUT1 antibody-targeted polymeric micelles co-loaded with curcumin and doxorubicin. J Drug Target. (2013) 21:994–1000. 10.3109/1061186X.2013.840639 [DOI] [PubMed] [Google Scholar]
- 135.Jeng LB, Kumar Velmurugan B, Chen MC, Hsu HH, Ho TJ, Day CH, et al. Fisetin mediated apoptotic cell death in parental and Oxaliplatin/irinotecan resistant colorectal cancer cells in vitro and in vivo. J Cell Physiol. (2018) 233:7134–42. 10.1002/jcp.26532 [DOI] [PubMed] [Google Scholar]
- 136.Shakibaei M, Mobasheri A, Lueders C, Busch F, Shayan P, Goel A. Curcumin enhances the effect of chemotherapy against colorectal cancer cells by inhibition of NF-kappaB and Src protein kinase signaling pathways. PLoS ONE. (2013) 8:e57218. 10.1371/journal.pone.0057218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Hamaya Y, Guarinos C, Tseng-Rogenski SS, Iwaizumi M, Das R, Jover R, et al. Efficacy of adjuvant 5-fluorouracil therapy for patients with EMAST-positive stage II/III colorectal cancer. PLoS ONE. (2015) 10:e0127591. 10.1371/journal.pone.0127591 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Hakim L, Alias E, Makpol S, Ngah WZ, Morad NA, Yusof YA. Gelam honey and ginger potentiate the anti-cancer effect of 5-FU against HCT 116 colorectal cancer cells. Asian Pac J Cancer Prev. (2014) 15:4651–7. 10.7314/APJCP.2014.15.11.4651 [DOI] [PubMed] [Google Scholar]
- 139.Snyder V, Reed-Newman TC, Arnold L, Thomas SM, Anant S. Cancer stem cell metabolism and potential therapeutic targets. Front Oncol. (2018) 8:203. 10.3389/fonc.2018.00203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Kim TI. Chemopreventive drugs: mechanisms via inhibition of cancer stem cells in colorectal cancer. World J Gastroenterol. (2014) 20:3835–46. 10.3748/wjg.v20.i14.3835 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Munro MJ, Wickremesekera SK, Peng L, Tan ST, Itinteang T. Cancer stem cells in colorectal cancer: a review. J Clin Pathol. (2018) 71:110–6. 10.1136/jclinpath-2017-204739 [DOI] [PubMed] [Google Scholar]
- 142.Shakibaei M, Buhrmann C, Kraehe P, Shayan P, Lueders C, Goel A. Curcumin chemosensitizes 5-fluorouracil resistant MMR-deficient human colon cancer cells in high density cultures. PLoS ONE. (2014) 9:e85397. 10.1371/journal.pone.0085397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Nunez-Sanchez MA, Karmokar A, Gonzalez-Sarrias A, Garcia-Villalba R, Tomas-Barberan FA, Garcia-Conesa MT, et al. In vivo relevant mixed urolithins and ellagic acid inhibit phenotypic and molecular colon cancer stem cell features: a new potentiality for ellagitannin metabolites against cancer. Food Chem Toxicol. (2016) 92:8–16. 10.1016/j.fct.2016.03.011 [DOI] [PubMed] [Google Scholar]
- 144.Chen WS, Lee YJ, Yu YC, Hsaio CH, Yen JH, Yu SH, et al. Enhancement of p53-mutant human colorectal cancer cells radiosensitivity by flavonoid fisetin. Int J Radiat Oncol Biol Phys. (2010) 77:1527–35. 10.1016/j.ijrobp.2010.02.043 [DOI] [PubMed] [Google Scholar]