Abstract
The inveterate patellar dislocation is an uncommon entity. The most frequent findings correspond to a misaligned valgus associated with lateral patellar dislocation. When severe knee osteoarthritis is present, total knee arthroplasty is an option, whether it is associated or not with realignment of the extensor apparatus. We present a review of published literature on correction of inveterate patellar dislocation associated with knee arthritis and our surgical technique with a case of inveterate patellar dislocation associated with tricompartmental knee osteoarthritis, in which a total knee arthroplasty was performed associated with proximal and distal realignment of the extensor apparatus. Total knee arthroplasty is a useful procedure in knee osteoarthritis associated with inveterate patellar dislocation, which can be associated with techniques on the extensor apparatus to achieve an adequate patellar alignment.
Keywords: Inveterate patellar dislocation, knee osteoarthritis, knee arthroplasty
Introduction
The inveterate dislocation of patella is an uncommon entity, for which the cause is still unknown. It usually presents late accompanied by knee arthritis [1], [2], [3].
The most frequently findings correspond to a misaligned valgus of the affected limb associated with lateral dislocation of patella [1], [2], [3].
The susceptibility to inveterate patellar dislocation is enhanced by inadequate treatment after the initial trauma in case of posttraumatic inveterate patellar dislocation, anatomic predisposition, ligament laxity, or familial predisposition [4], [5], [6], [7], [8], [9], [10].
Several techniques have been described to reconstruct the dislocated extensor apparatus, including the Elmslie-Trillat procedure, proximal patellar quadricepsplasty, and medial patellofemoral ligament reconstruction [11], [12], [13], [14]. When severe knee osteoarthritis is present, total knee arthroplasty is a treatment option, which may or may not be associated with realignment of the extensor apparatus to achieve an adequate valgus correction and obtain a correct soft tissue balance [15], [16].
Available literature consists of a number of case reports that report many techniques to provide an adequate treatment for patients with inveterate patellar dislocation.
This article reviews the current literature and describes a surgical technique for an inveterate patellar dislocation associated with tricompartmental arthritis of the knee, in which a total knee arthroplasty was performed associated with a proximal and distal realignment of the extensor apparatus.
Case history
A 73-year-old female presented to our institution with a long history of knee pain and limping. She had a history of bilateral hip dysplasia and bilateral total hip arthroplasties performed 33 years before. No other personal and familial morbid medical history was reported. A physical examination revealed valgus malalignment of her right knee, medial instability, and lateral patellar dislocation. She did not achieve active full extension (−10°) and had flexion of 80°. Radiographs showed tricompartmental right knee arthritis, a mechanical valgus axis of 13.9°, an anatomical valgus axis of 23.6°, and a lateral articular pseudofacet. (Fig. 1). Total right knee arthroplasty plus proximal and distal realignment of the extensor apparatus was indicated.
Figure 1.
Right knee preoperative images. (a) Long standing view. (b) Anteroposterior view. (c) Lateral view (patella not visualized). (d) Rosenberg view. (e) Axial view (dislocated patella articulating with lateral pseudofacet).
Informed consent for the procedure and publication was obtained and documented.
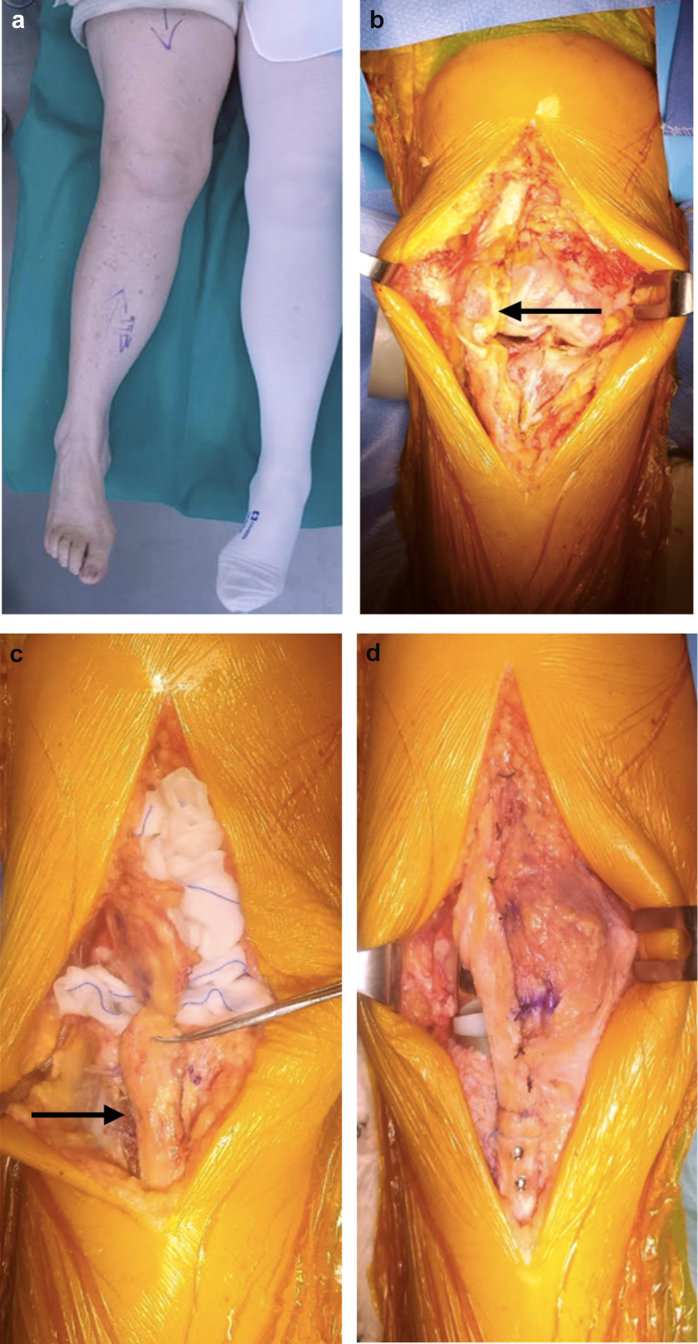
The patient was positioned supine, and a tourniquet was applied and inflated in her right thigh. A midline incision with deep dissection and medial parapatellar arthrotomy was made. Quadriceps hypoplasia and lateralization of the vastus medialis were noted together with a laterally dislocated patella, contacting the lateral wall of the lateral femoral condyle in the pseudoarticular facet. Tricompartmental knee osteoarthritis was observed with abundant marginal osteophytes on the femur and tibia. Regular femoral and tibial cuts were performed and Stryker Scorpio NRG, posterior stabilized (Stryker, Mahwah, NJ) prosthesis was used. The femoral cut was made in 5° of valgus, and the tibial cut was made in 3° of tibial slope. The definitive tibial component was #5, the definitive femoral component was #6, with a resurface and medialized patellar insert. Each component was cemented.
Then, an osteotomy of the anterior tuberosity of the tibia was performed, extending 5 cm distal to the joint line, and was medialized 1 cm and fixed with 2 screws (DePuy Synthes small fracgment, Westchester, PA). Satisfactory patellar realignment was obtained, but with a tendency for patellar tilt, so it was decided to perform a proximal realignment with an advance of the vastus medialis over the patella, using the Insall technique, [17] because of its poor quality. Appropriate patellar tracking and flexion-extension stability were checked. The patella was realigned in the center of the femoral component, and the valgus was corrected (Fig. 2).
Figure 2.
Right knee intraoperative images. (a) Positioning. (b) Direct view of the inveterate patellar dislocation. (c) Medialization of the anterior tuberosity of the tibia. (d) Patella realigned in the center of femur.
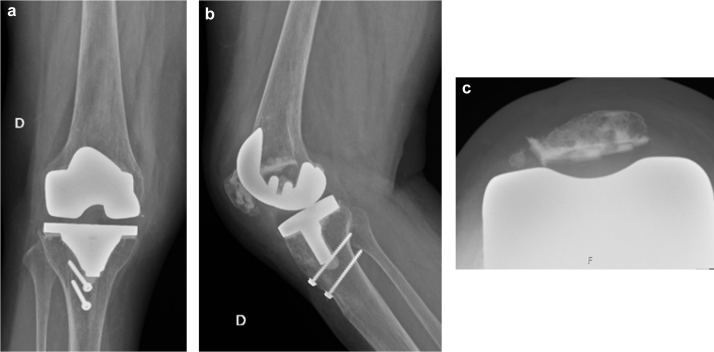
In the immediate postoperative period, a continuous passive mobilization machine was used, and a knee brace limiting the motion from 0° to 30° was employed. In addition, walking with 2 crutches was recommended. At 3 months of evolution, the medializing osteotomy of the anterior tuberosity of the tibia was healed without complications. (Fig. 3).
Figure 3.
Right knee postoperative images. (a) Anteroposterior view. (b) Lateral view. (c) Axial view (centered patella).
Two years after surgery, the patient ambulated without limping, with a range of motion of 0°-100°, without joint pain, and without new episodes of patellar instability or dislocation.
Discussion
The inveterate dislocation of patella is an alteration in the knee where it remains permanently dislocated, even in extension and when fixed to the lateral femoral condyle, as was the case of our patient. However, the etiology remains unknown.
Adults, with valgus axis, can evolve with tricompartmental knee osteoarthritis. In these patients with inveterate dislocation of patella who develop knee arthritis, arthroplasty seems to be a good treatment option once the symptoms and pain affect the usual activities.
In the literature, there are few case reports in which the inveterate patellar dislocation evolves with knee osteoarthritis (Table 1).
Table 1.
Summary of published literature on correction of inveterate patellar dislocation associated with knee arthritis.
| Author | N (knees) | Intervention | Follow-up (mo) | Postoperative outcome | Comments |
|---|---|---|---|---|---|
| Marmor [18] | 2 | TKR | 48 | Painless function, stability, and quadriceps strength | Correction of the dislocated patella and extensor mechanism was not attempted |
| Pradhan [19] | 2 | TKR | 72 | Pain | Revision at 14 months |
| Bullek [20] | 5 | TKR | 40 | HSS Score, Knee Society knee Score | Modified proximal realignment |
| Bergquist [21] | 1 | TKR | 24 | Knee Society knee Score | Release of the lateral retinaculum, proximal extensor mechanism realignment, and patellar resurfacing |
HSS, Hospital for Special Surgery Score.
Marmor [18] was the first to report the knee arthroplasty for treatment in patients with inveterate patellar dislocation; he reported a case of bilateral total knee arthroplasty (TKA) for the treatment of congenital dislocation of the patella. Correction of the dislocated patella and extensor mechanism was not attempted in either knee. He recommended avoidance of reconstruction of the extensor mechanism in adult patients with congenital dislocation of the patella if knee function is preserved. However, only a short-term follow-up was described, and the effects of the neglected patellar stability on the components are unknown.
Pradhan et al [19] also reported that total knee arthroplasty was performed in patients with inveterate patellar dislocation. The results were good, but they did not report the functional long-term results.
Bullek [20] reported 5 total knee replacements (TKR) in 3 patients with congenital dislocation of the patella and 1 with dislocation of the patella caused by juvenile rheumatoid arthritis. The dislocation was treated by a modified proximal realignment and achieved good results.
Bergquist [21] reported a TKR for a patient who had congenital patellar dislocation by a modified lateral release and an overlap of the vastus medialis obliquus, with good results in the medium term.
The osteotomy of the anterior tuberosity of the tibia is also effective for distal realignment, but it has a risk of nonunion, fracture, and alteration of soft tissues [1], and on the other hand, it may interfere with the proper placement of the prosthesis.
In our case, we performed a proximal realignment with advancement of the vastus medialis obliquus over the patella and also distal realignment, with medialization of the anterior tuberosity of the tibia, which consolidated without complications.
In the medium-term follow-up, the patient returned to her usual activities without pain or limping, with adequate ranges of movement of her joint.
Current controversies and future considerations
The inveterate patellar dislocation is an uncommon entity, and the most frequent findings correspond to a misaligned valgus associated with lateral patellar dislocation; the total knee arthroplasty is an option when severe knee osteoarthritis is present. One controversy to highlight is when distal, proximal, or both realignments are needed. The patient ended up having successful surgery and recovery with the total knee replacement associated with proximal and distal realignment of the extensor apparatus. For future work, greater number of cases and longer follow-up are needed to evaluate the functional results and survival of the prosthetic components in these complex pathologies.
Summary
In conclusion, total knee arthroplasty is a useful procedure in knee osteoarthritis associated with inveterate dislocation of patella, which can be associated with some technique on the extensor apparatus to achieve an adequate patellar alignment. However, a greater number of cases and longer follow-up will be needed to evaluate the functional results and survival of the prosthetic components in these complex pathologies.
Key Points.
-
•
The inveterate patellar dislocation presents with a misaligned valgus tibiofemoral joint associated with lateral patellar dislocation, noted on the Merchant knee radiograph.
-
•
When severe symptomatic knee osteoarthritis is present, TKA is an option for treatment.
-
•
Adequate patellar alignment with reduction of the patellofemoral joint is an appropriate goal of surgery.
-
•
To achieve an adequate patellar alignment, a proximal, distal, or combined realignment should be considered.
-
•
The surgeon should be prepared to perform each of these options at the time of TKA.
Footnotes
One or more of the authors of this article have disclosed potential or pertinent conflicts of interest, which may include receipt of payment, either direct or indirect, institutional support, or association with an entity in the biomedical field which may be perceived to have potential conflict of interest with this work. For full disclosure statements refer to https://doi.org/10.1016/j.artd.2018.04.003.
Appendix A. Supplementary data
References
- 1.Yamanaka H., Kawamoto T., Tamai H. Total knee arthroplasty in a patient with bilateral congenital dislocation of the patella treated with a different method in each knee. Case Rep Orthop. 2015;2015:890315. doi: 10.1155/2015/890315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Oh K.-J., Yoon J.-R., Yang J.-H. Total knee arthroplasty in a pseudoachondroplastic dwarfism patient with bilateral patellar dislocation. Knee. 2013;20(1):45. doi: 10.1016/j.knee.2012.10.012. [DOI] [PubMed] [Google Scholar]
- 3.Dao Q., Chen D.B., Scott R.D. Proximal patellar quadricepsplasty realignment during total knee arthroplasty for irreducible congenital dislocation of the patella: a report of two cases. J Bone Joint Surg. 2010;92(14):2457. doi: 10.2106/JBJS.H.00812. [DOI] [PubMed] [Google Scholar]
- 4.Boring T.H., O'Donoghue D.H. Acute patellar dislocation: results of immediate surgical repair. Clin Orthop Relat Res. 1978:182. [PubMed] [Google Scholar]
- 5.Chen S.C., Ramanathan E.B. The treatment of patellar instability by lateral release. J Bone Joint Surg Br. 1984;66:344. doi: 10.1302/0301-620X.66B3.6725343. [DOI] [PubMed] [Google Scholar]
- 6.Jensen C.M., Roosen J.U. Acute traumatic dislocations of the patella. J Trauma. 1985;25:160. doi: 10.1097/00005373-198502000-00014. [DOI] [PubMed] [Google Scholar]
- 7.McCarroll H.R., Schwartzmann J.R. Lateral dislocation of the patella. Correction by simultaneous transplantation of the tibial tubercle and semitendinosus tendon. J Bone Joint Surg Am. 1945;27:446. [Google Scholar]
- 8.Larsen E., Lauridsen F. Conservative treatment of patellar dislocations. Influence of evident factors on the tendency to redislocation and the therapeutic result. Clin Orthop Relat Res. 1982:131. [PubMed] [Google Scholar]
- 9.Runow A. The dislocating patella. Etiology and prognosis in relation to generalized joint laxity and anatomy of the patellar articulation. Acta Orthop Scand Suppl. 1983;201:1. [PubMed] [Google Scholar]
- 10.Miller G.F. Familial recurrent dislocation of the patella. J Bone Joint Surg Br. 1978;60-B:203. doi: 10.1302/0301-620X.60B2.659465. [DOI] [PubMed] [Google Scholar]
- 11.Langenskiöid A., Ritsilä V. Congenital dislocation of the patella and its operative treatment. J Pediatr Orthop. 1992;12:315. doi: 10.1097/01241398-199205000-00007. [DOI] [PubMed] [Google Scholar]
- 12.Paton R.W., Bonshahi A.Y., Kim W.Y. Congenital and irreducible non-traumatic dislocation of the patella—a modified soft tissue procedure. Knee. 2004;11:117. doi: 10.1016/S0968-0160(03)00074-7. [DOI] [PubMed] [Google Scholar]
- 13.Gordon J.E., Schoenecker P.L. Surgical treatment of congenital dislocation of the patella. J Pediatr Orthop. 1999;19:260. doi: 10.1097/00004694-199903000-00024. [DOI] [PubMed] [Google Scholar]
- 14.Beals R.K., Buehler K. Treatment of patellofemorai instability in childhood with creation of a femoral sulcus. J Pediatr Orthop. 1997;17:516. [PubMed] [Google Scholar]
- 15.Tunay S., Ozkan H., Köse O., Atik A., Basbozkurt M. Total knee arthroplasty in a patient with neglected congenital patellar dislocation. Orthopedics. 2009;32(10):45. doi: 10.3928/01477447-20090818-22. [DOI] [PubMed] [Google Scholar]
- 16.Matsushita T., Kuroda R., Kubo S., Mizuno K., Matsumoto T., Kurosaka M. Total knee arthroplasty combined with medial patellofemoral ligament reconstruction for osteoarthritic knee with preoperative valgus deformity and chronic patellar dislocation. J Arthroplasty. 2011;26(3):505.e17. doi: 10.1016/j.arth.2010.01.101. [DOI] [PubMed] [Google Scholar]
- 17.Insall J., Falvo K.A., Wise D.W. Chondromalacia patellae. A prospective study. J Bone Joint Surg. 1976;58A:1. [PubMed] [Google Scholar]
- 18.Marmor L. Total knee arthroplasty in a patient with congenital dislocation of the patella. Case report. Clin Orthop Relat Res. 1988;226:129. [PubMed] [Google Scholar]
- 19.Pradhan R.L., Watanabe W., Itoi E., Yamada S., Shimada Y., Sat K. Total knee arthroplasty in bilateral congenital dislocation of the patella—a case report. Acta Orthop Scand. 2001;72(4):422. doi: 10.1080/000164701753542113. [DOI] [PubMed] [Google Scholar]
- 20.Bullek D.D., Scuderi G.R., Insall J.N. Management of the chronic irreducible patellar dislocation in total knee arthroplasty. J Arthroplasty. 1996;11:339. doi: 10.1016/s0883-5403(96)80090-8. [DOI] [PubMed] [Google Scholar]
- 21.Bergquist P.E., Baumann P.A., Finn H.A. Total knee arthroplasty in an adult with congenital dislocation of the patella. J Arthroplasty. 2001;16:384. doi: 10.1054/arth.2001.20545. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.