Abstract
Background
Computer navigation and robotic assistance technologies are used to improve the accuracy of component positioning in total knee arthroplasty (TKA), with the goal of improving function and optimizing implant longevity. The purpose of this study was to analyze trends in the use of technology-assisted TKA, identify factors associated with the use of these technologies, and describe potential drivers of cost.
Methods
The Nationwide Inpatient Sample database was used to identify patients who underwent TKA using conventional instrumentation, computer navigation, and robot-assisted techniques between 2005 and 2014. Variables analyzed include patient demographics, hospital and payer types, and hospital charges. Descriptive statistics were used to describe trends. Univariate and multivariate analyses were performed to identify differences between conventional and technology-assisted groups.
Results
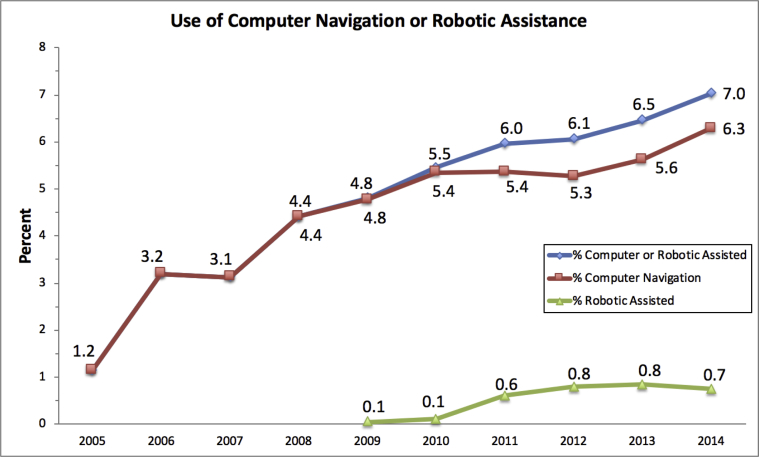
Our analysis identified 6,060,901 patients who underwent TKA from 2005 to 2014, of which 273,922 (4.5%) used computer navigation and 24,084 (0.4%) used robotic assistance. The proportion of technology-assisted TKAs steadily increased over the study period, from 1.2% in 2005 to 7.0% in 2014. Computer navigation increased in use from 1.2% in 2005 to 6.3% in 2014. Computer navigation was more likely to be used in the Western United States, whereas robot-assisted TKAs were more likely to be performed in the Northeast. Increased hospital charges were associated with the use of technology assistance ($53,740.1 vs $47,639.2).
Conclusions
The use of computer navigation and robot-assisted TKA steadily increased over the study period, accounting for 7.0% of TKAs performed in the United States in 2014. Marked regional differences in the use of these technologies were identified. The use of these technologies was associated with increased hospital charges.
Keywords: Computer navigation, Technology assistance, Total knee arthroplasty, Trends, TKA
Introduction
Although total knee arthroplasty (TKA) has shown excellent long-term survivorship in multiple studies [1], [2], [3], efforts to improve longevity and functional outcomes continue. Computer-assisted surgery and, more recently, robot-assisted surgery have been introduced with the goal of improving implant positioning. Improved positioning may in turn translate to improved survivorship, as varus tibial component alignment greater than 3 degrees has been associated with early failure [4], [5]. As the use of technology-assisted surgery has increased over the past 2 decades, multiple studies have demonstrated improved mechanical alignment with the use of computer navigation and robot-assisted surgeries [6], [7], [8], [9], [10], [11], [12], [13], [14], [15], [16], [17]. However, studies have not been conclusive regarding the effects of technology assistance on revision rate, patient-reported outcomes, and complication rates [12], [18], [19], [20], [21], [22], [23], [24], [25], [26], [27], [28], [29], [30], [31], [32], [33], [34], [35], [36], [37], [38]. Given the lack of conclusive data, the debate concerning the value of technology-assisted TKA and its cost-effectiveness continues.
Until recently, nationwide data regarding the use of computer-assisted and robot-assisted arthroplasty were unavailable. Recent revisions of the International Classification of Diseases, Ninth Revision, (ICD-9) procedure codes provided codes for computer-assisted surgery (00.3) and robot-assisted surgery (17.4). The computer-assisted code was released on October 1, 2004, making 2005 the first complete year of data. The robot-assisted code was released on October 1, 2008, making 2009 the first complete year of data. Two recent studies have examined the use of technology-assisted joint replacement surgery with conflicting results. Gholson et al. [39] reported a 38.3% decrease in computer-navigated TKA utilization between 2010 and 2014 using the National Surgical Quality Improvement Program (NSQIP) database. In contrast, Boylan et al. [40] reported yearly increases in technology-assisted total hip and total knee replacements from 2008 to 2015 using the New York Statewide Planning and Research Cooperative System database and saw an increase in the use of these technologies from 2.8% to 8.6% during the study period. However, both studies relied on databases that encompass a biased sampling of national practice trends. The NSQIP database is comprised of a nonrandom sampling of voluntary hospitals, whereas the New York Statewide Planning and Research Cooperative System database is limited by its inherent geographical bias. To date, no study has examined these trends using a sampling of all United States hospitals.
The purpose of this study is to present an analysis of trends in technology-assisted TKA using a representative sampling of all United States inpatient discharges. This study quantifies the recent increased use of computer-navigated and robot-assisted TKAs using a large United States database, identifies factors associated with the use of technology assistance, and describes potential drivers of hospital charges.
Material and methods
Data collection
This study used the Nationwide Inpatient Sample (NIS) database from 2005 through 2014 to identify all patients who underwent a primary TKA. The NIS is part of the Healthcare Cost and Utilization Project sponsored by the Agency for Healthcare Research and Quality and comprises the largest nationwide all-payer hospital inpatient care database in the United States, representing an approximate 20% sampling of all hospital discharges. As the NIS database includes no protected health information, this study was deemed exempt by our institutional review board. No external funding was used to support this investigation.
Variables
We selected patients of all ages who underwent a primary TKA from 2005 to 2014. Patients were identified using the ICD-9 procedure code 81.54 (TKA). A subcohort of patients who underwent a computer-assisted TKA was identified using the following ICD-9 procedure modifier codes (Supplemental Table 1): computer-assisted surgery with computed tomography/computed tomography angiography (00.31), computer-assisted surgery with magnetic resonance/magnetic resonance angiography (00.32), computer-assisted surgery with fluoroscopy (00.33), imageless computer-assisted surgery (00.34), computer-assisted surgery with multiple data sets (00.35), and other computer-assisted surgery (00.39). A second subcohort of patients who underwent a robot-assisted surgery was identified using the following ICD-9 procedure modifier codes: open robot-assisted procedure (17.41) and other unspecified robot-assisted procedure (17.49).
Variables analyzed in this study included age, gender, race, primary health insurance, total number of chronic conditions, hospital location and teaching status, hospital bed size, geographic region of hospital, median household income, and hospital charge. Hospital charges were adjusted for inflation and expressed in 2014 terms using data obtained from the United States Bureau of Labor Statistics (https://data.bls.gov/cgi-bin/cpicalc.pl). The NIS database contains data on total charges for each hospital in the database, which represents the amount that hospitals billed for services, but does not reflect how much hospitals received in payment. Charge information is obtained on all patients, regardless of payer, including persons covered by Medicare, Medicaid, private insurance, and the uninsured.
Statistical analysis
Statistical analyses were performed using Stata version 13 (StataCorp LP, College Station, TX). Descriptive statistical methods were used to describe trends in utilization over time. Univariate statistics were used to compare the computer navigation and robotic assistance cohorts with patients who underwent TKA using conventional techniques without technology assistance. A Pearson's chi-squared test was used for categorical variables and a Student t-test was used for continuous variables. Differences identified between the cohorts on univariate analysis with a P value ≤.1 were used to create a multivariate model. A multiple logistic regression analysis was used to account for potentially confounding factors.
Results
Our analysis identified 6,060,901 patients who underwent TKA from 2005 to 2014, of which 273,922 (4.5%) used computer navigation and 24,084 (0.4%) used robotic assistance (Table 1). The prevalence of computer navigation in TKA increased from 1.2% in 2005 to 6.29% in 2014. The prevalence of robotic assistance in TKA increased from 0.1% in 2009 to 0.8% in 2013, followed by a slight decrease to 0.7% in 2014 (Fig. 1). Technology-assisted TKA, whether using computer navigation or robotic assistance, has steadily increased over the study period, reaching a peak of 7.0% in 2014 in the final year of study, from 1.2% in 2005.
Table 1.
A comparison of patient and hospital characteristics between conventional and technology-assisted total knee arthroplasty groups.
| Variable | Conventional |
Technology-assisted |
P value | ||
|---|---|---|---|---|---|
| N | % | N | % | ||
| N | 5,762,895 | 95.1% | 298,006 | 4.9% | |
| Computer navigation | 273,922 | 4.5% | |||
| Robotic | 24,084 | 0.4% | |||
| Age (y), mean ± standard deviation | 66.2 ± 0.0 | 66.2 ± 0.0 | .6779 | ||
| Gender (%) | <.0001 | ||||
| Female | 2,130,217 | 37.0% | 115,503 | 38.8% | |
| Male | 3,632,678 | 63.0% | 182,503 | 61.2% | |
| Number of comorbidities, mean ± standard deviation | 4.8 ± 0.0 | 4.8 ± 0.0 | .0015 | ||
| Race (%) | <.0001 | ||||
| White | 4,962,160 | 83.4% | 214,508 | 84.0% | |
| Black | 359,016 | 7.5% | 13,660 | 5.4% | |
| Hispanic | 254,389 | 5.3% | 14,740 | 5.8% | |
| Asian or Pacific Islander | 57,912 | 1.2% | 3985 | 1.6% | |
| Native American | 22,182 | 0.5% | 2217 | 0.9% | |
| Other | 107,237 | 2.2% | 6239 | 2.4% | |
| Primary payment (%) | <.0001 | ||||
| Medicare | 3,187,362 | 55.4% | 164,462 | 55.5% | |
| Medicaid | 168,722 | 2.9% | 7381 | 2.5% | |
| Private | 2,177,405 | 37.9% | 113,158 | 38.2% | |
| Self-pay | 25,620 | 0.5% | 992 | 0.3% | |
| No charge | 4991 | 0.1% | 152 | 0.1% | |
| Other payment | 187,423 | 3.3% | 10,444 | 3.5% | |
| Median household income | <.0001 | ||||
| 0-25th Percentile | 1,145,151 | 22.1% | 64,837 | 22.7% | |
| 25-50th Percentile | 1,402,665 | 27.1% | 78,068 | 27.3% | |
| 50-75th Percentile | 1,371,236 | 26.5% | 76,279 | 26.7% | |
| 75-100th Percentile | 1,259,765 | 24.3% | 67,022 | 23.4% | |
| Hospital location/teaching status | <.0001 | ||||
| Rural | 708,635 | 12.3% | 26,141 | 8.8% | |
| Urban, nonteaching | 2,586,961 | 45.1% | 152,979 | 51.4% | |
| Urban, teaching | 2,445,646 | 42.6% | 118,733 | 39.9% | |
| Hospital size | <.0001 | ||||
| Small | 1,080,749 | 18.8% | 66,373 | 22.3% | |
| Medium | 1,480,850 | 25.8% | 81,213 | 27.3% | |
| Large | 3,179,644 | 55.4% | 150,267 | 50.5% | |
| Region of hospital | <.0001 | ||||
| Northeast | 960,982 | 16.7% | 64,837 | 22.7% | |
| Midwest | 1,626,934 | 28.2% | 78,068 | 27.3% | |
| South | 2,104,748 | 36.5% | 76,279 | 26.7% | |
| West | 1,070,232 | 18.6% | 67,022 | 23.4% | |
| Total hospital charge(s), median | $47,639.2 | $53,740.1 | <.0001 | ||
Figure 1.
The percent of total knee arthroplasties performed using computer navigation or robotic assistance from 2005 to 2014.
Univariate results
Both conventional and technology-assisted TKA cohorts were similar in age (average, 66.2 years) and the number of comorbidities (average 4.8 chronic conditions) (Table 1). Patients in both conventional and technology-assisted groups were predominantly male, 62.7% and 61.2%, and white, 83.4% and 84.0%, respectively. Medicare beneficiaries made up approximately 55% of knee arthroplasty patients in both cohorts, with private insurance being the next highest payer at nearly 38%. This payer distribution remained consistent over the course of the study, with Medicare beneficiaries comprising roughly 53%-57% of technology-assisted knee arthroplasty patients over the last 8 years of study, and private insurance made up 36%-41% of technology-assisted arthroplasties. Patients were well distributed across household income quartiles in both cohorts.
Differences in hospital factors were noted across conventional and technology-assisted groups. Most notably, the highest volume of TKAs was performed in the South, with approximately 36% of total knee arthroplasties in the conventional cohort. However, hospitals in the West and Northeast were more likely to use computer navigation or robotic assistance. TKAs performed in the West and Northeast comprised a greater proportion of technology-assisted TKAs than would be expected given the geographic breakdown seen in conventional TKAs (Table 1). Conversely, hospitals in the South were less likely to use technology assistance, with only 26.7% of technology-assisted TKAs performed in the South compared with 36.5% of conventional TKAs.
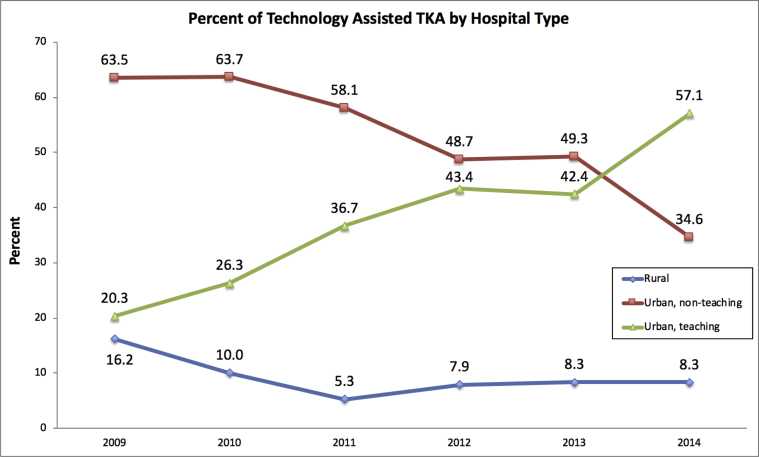
Over the entire study period, urban nonteaching hospitals accounted for 51.4% of all technology-assisted TKAs. However, there has been a notable increasing trend in technology-assisted TKAs performed at urban teaching hospitals from 2009 to 2014 (Fig. 2). In the final year of the study, 57.1% of technology-assisted TKAs were performed in urban teaching centers and 36.6% in urban nonteaching hospitals.
Figure 2.
The use of technology-assisted TKAs by hospital location/teaching status from 2009 to 2014.
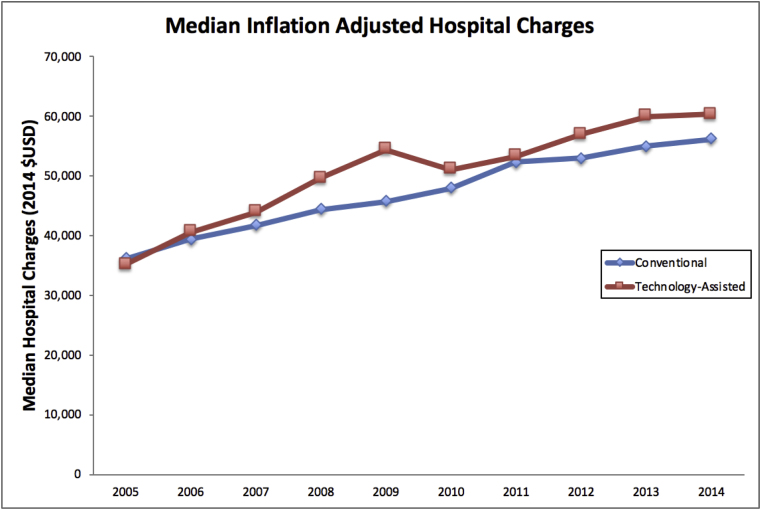
The median hospital charge over the entire study period was significantly more for TKAs performed using computer guidance or robotic assistance than for conventional TKAs ($53,740.1 vs $47,639.2) (Table 1). Charges were nearly identical in 2005 for conventional and technology-assisted TKA ($36,182.8 vs $35,195.9, respectively), but charges for technology-assisted TKA exceeded conventional TKA in 2014 ($59,128.2 vs 68,262.9) (Fig. 3).
Figure 3.
The median inflation-adjusted hospital charges for total knee arthroplasty performed by conventional or technology-assisted techniques from 2005 to 2014.
Multivariate results
A multivariate analysis was conducted for the 2014 data to reveal independent predictors of computer navigation and robotic assistance utilizations. Black (relative risk [RR]: 0.67, 95% confidence interval [CI]: 0.55-0.83, P < .0001) and Asian or Pacific Islander (RR: 0.59, CI: 0.39-0.90, P < .0001) patients were less likely to undergo TKA using computer navigation than white patients (Table 2). There were no significant differences between Hispanic, Native American, and white patients. In addition, patients with Medicaid (RR: 0.55, CI: 0.41-0.74, P < .0001) were less likely to undergo a computer-navigated procedure. Computer navigation for TKA was more likely to be performed in the West region of the country than the Northeast (RR: 1.56, CI: 1.37-1.77, P < .0001), with the Northeast still more likely to use technology assistance than the South or midwest. Urban hospitals were found to be independent predictors of computer navigation utilization (Table 2).
Table 2.
Independent factors associated with computer navigation TKA utilization.
| Variable | Relative risk | Confidence interval | P value |
|---|---|---|---|
| Age | 1.01 | 1.00-1.01 | .03 |
| Female gender (reference: male) | 0.98 | 0.90-1.07 | .62 |
| Number of comorbidities | 1.01 | 1.00-1.03 | .13 |
| Race (reference: white) | |||
| Black | 0.67 | 0.55-0.83 | <.0001 |
| Hispanic | 0.93 | 0.78-1.11 | .42 |
| Asian or Pacific Islander | 0.59 | 0.39-0.90 | .01 |
| Native American | 1.36 | 0.78-2.37 | .28 |
| Other | 2.24 | 1.85-2.71 | <.0001 |
| Primary payment (reference: Medicare) | |||
| Medicaid | 0.55 | 0.41-0.74 | <.0001 |
| Private | 1.07 | 0.96-1.20 | .22 |
| Self-pay | 1.22 | 0.67-2.24 | .51 |
| Median household income (reference: first quartile) | |||
| 25-50th Percentile | 0.97 | 0.86-1.10 | .66 |
| 50-75th Percentile | 0.90 | 0.80-1.02 | .11 |
| 75-100th Percentile | 0.72 | 0.63-0.82 | <.0001 |
| Hospital location/teaching status (reference: rural) | |||
| Urban, nonteaching | 0.64 | 0.55-0.74 | <.0001 |
| Urban, teaching | 0.65 | 0.57-0.75 | <.0001 |
| Hospital size (reference: small) | |||
| Medium | 0.85 | 0.77-0.95 | <.0001 |
| Large | 0.65 | 0.59-0.72 | <.0001 |
| Region of hospital (reference: Northeast) | |||
| Midwest | 0.65 | 0.56-0.74 | <.0001 |
| South | 0.72 | 0.63-0.81 | <.0001 |
| West | 1.56 | 1.37-1.77 | <.0001 |
Robot-assisted TKA was more likely to be performed on patients with fewer comorbidities (RR: 0.90, CI: 0.88-0.93, P < .0001) and less likely to be performed on female patients (RR: 0.80, CI: 0.71-0.90, P < .0001) (Table 3). Hispanic (RR: 1.56, CI: 1.26-1.95, P < .0001) and Native American patients (RR: 2.41, CI: 1.13-5.14, P = .022) were more likely to receive a robot-assisted TKA. Patients with Medicaid (RR: 0.54, CI: 0.3-0.85, P = .008) were again less likely to have a robotic procedure, whereas patients with private insurance (RR: 1.24, CI: 1.06-1.45, P-.008) were more likely. Upper quartile median household income trended toward increasing likelihood of robot-assisted TKA (RR: 1.21, CI: 1.00-1.46, P = .052). Urban nonteaching hospital (RR: 2.14, CI: 0.1.57-2.91, P < .0001) was an independent predictor of robotic assistance; however, the previously seen increased prevalence of technology assistance in the West was not seen (Table 3).
Table 3.
Independent factors associated with robot-assisted TKA utilization.
| Variable | Relative risk | Confidence interval | P value |
|---|---|---|---|
| Age | 0.99 | 0.98-0.99 | .001 |
| Female gender (reference: male) | 0.80 | 0.71-0.90 | <.0001 |
| Number of comorbidities | 0.90 | 0.88-0.93 | <.0001 |
| Race (reference: white) | |||
| Black | 0.85 | 0.65-1.10 | .214 |
| Hispanic | 1.56 | 1.26-1.95 | <.0001 |
| Asian or Pacific Islander | 1.11 | 0.67-1.83 | .693 |
| Native American | 2.41 | 1.13-5.14 | .022 |
| Other | 1.01 | 0.71-1.43 | .977 |
| Primary payment (reference: Medicare) | |||
| Medicaid | 0.54 | 0.35-0.85 | .008 |
| Private | 1.24 | 1.06-1.45 | .008 |
| Self-pay | 0.22 | 0.03-1.62 | .139 |
| Median household income (reference: first quartile) | |||
| 25-50th Percentile | 0.83 | 0.69-1.01 | .067 |
| 50-75th Percentile | 1.17 | 0.97-1.40 | .099 |
| 75-100th Percentile | 1.21 | 1.00-1.46 | .052 |
| Hospital location/teaching status (reference: rural) | |||
| Urban, nonteaching | 2.14 | 1.57-2.91 | <.0001 |
| Urban, teaching | 1.15 | 0.85-1.57 | .363 |
| Hospital size (reference: small) | |||
| Medium | 0.56 | 0.49-0.65 | <.0001 |
| Large | 0.42 | 0.36-0.49 | <.0001 |
| Region of hospital (reference: Northeast) | |||
| Midwest | 0.21 | 0.16-0.27 | <.0001 |
| South | 0.63 | 0.54-0.74 | <.0001 |
| West | 0.53 | 0.44-0.64 | <.0001 |
A regression analysis was performed to look for drivers of high costs in 2014 (Table 4). A “high-cost” discharge was defined as hospital charges in the 90th percentile and above for our data set, equaling costs greater than $94,963. The cost was much more likely to be high in the West (RR: 5.49, CI: 5.16-5.83, P < .0001) and South (RR: 1.46, CI: 1.37-1.55, P < .0001) compared to the Northeast. The cost was also more likely to be high in urban centers, both teaching (RR: 2.58, CI: 2.34-2.85, P < .0001) and nonteaching hospitals (RR: 2.42, CI: 2.20-2.68, P < .0001). Interestingly, the use of computer navigation was associated with increasing cost (RR: 1.26, CI: 1.12-1.43, P < .0001); however, the use of robotic assistance was not (RR: 1.08, CI: 0.90-1.31, P = .410).
Table 4.
Independent factors associated with high-cost computer-navigated total knee arthroplasty.
| Variable | Relative risk | Confidence interval | P value |
|---|---|---|---|
| Age | 0.99 | 0.99-1.00 | <.0001 |
| Female gender (reference: male) | 0.95 | 0.91-0.98 | .010 |
| Number of comorbidities | 1.08 | 1.08-1.09 | <.0001 |
| Race (reference: white) | |||
| Black | 1.66 | 1.56-1.78 | <.0001 |
| Hispanic | 1.79 | 1.68-1.90 | <.0001 |
| Asian or Pacific Islander | 1.62 | 1.44-1.82 | <.0001 |
| Native American | 0.69 | 0.49-0.95 | .030 |
| Other | 2.13 | 1.86-2.04 | <.0001 |
| Primary payment (reference: private insurance) | |||
| Medicare | 1.06 | 1.01-1.11 | .020 |
| Medicaid | 1.03 | 0.94-1.13 | .530 |
| Self-pay | 0.62 | 0.45-0.87 | .010 |
| Median household income (reference: first quartile) | |||
| 25-50th Percentile | 0.90 | 0.85-0.95 | <.0001 |
| 50-75th Percentile | 1.03 | 0.98-1.09 | .270 |
| 75-100th Percentile | 1.25 | 1.18-1.32 | <.0001 |
| Hospital location/teaching status (reference: rural) | |||
| Urban, nonteaching | 2.58 | 2.34-2.85 | <.0001 |
| Urban, teaching | 2.42 | 2.20-2.68 | <.0001 |
| Hospital Size (reference: small) | |||
| Medium | 1.45 | 1.38-1.52 | <.0001 |
| Large | 1.12 | 1.07-1.17 | <.0001 |
| Region of hospital (reference: Northeast) | |||
| Midwest | 0.79 | 0.74-0.86 | <.0001 |
| South | 1.46 | 1.37-1.55 | <.0001 |
| West | 5.49 | 5.16-5.83 | <.0001 |
| Computer navigation | 1.26 | 1.12-1.43 | <.0001 |
| Robotic assistance | 1.08 | 0.90-1.31 | .410 |
Discussion
The use of computer navigation and robotic assistance during TKA steadily increased from 2005 to 2014, accounting for approximately 1 in 14 TKAs (7.0%) performed in the United States in 2014. Most technology-assisted TKAs were performed in urban hospitals, on patients of white race, who were Medicare beneficiaries. Medicaid was found to be an independent factor associated with a decreased likelihood of using either computer navigation and robotic assistance. Finally, surgeons in the Western United States were most likely to adopt computer navigation, whereas robot-assisted TKA was adopted mostly by surgeons in the Northeastern United States. The present study is the first, to our knowledge, that reports on these trends and associations using a national sampling of all geographical regions, containing all insurance providers. As such, the findings reported herein are likely the most representative data of the United States to date.
The mean hospital charge for a TKA has increased by 52.4% in the past 15 years [41]. With osteoarthritis being the single most expensive condition reported by Medicare, total hip and total knee arthroplasties are among the largest surgical expenditures in Medicare patients [42]. Our study demonstrated an increase in median hospital charges for technology-assisted TKAs, with computer navigation independently associated with high hospital charges. Though the prevalence of computer navigation and robotic assistance is relatively low, the increasing use of these technologies, as evidenced in our study, can contribute to rising health-care costs, particularly for payers who base hospital reimbursement as a proportion of hospital charges rather than those who use a bundled payment model.
The contribution of technology assistance to costs will continue to be of importance when assessing bundles for comprehensive joint care. In particular, computer-navigated TKAs have been shown to have little to no effect on hospital length of stay [20], [39], suggesting that these technologies may be ineffective at mitigating increased hospital charges through shorter inpatient hospital stays. However, if these technologies are able to improve TKA survivorship, these costs may be offset by a decrease in future revisions. However, conclusive data regarding the relationship between computer navigation and TKA implant longevity are lacking [28].
In our study, computer navigation was independently associated with higher hospital charges; however, robotic assistance was not. There are recent data to suggest robot-assisted TKA may lead to decreased facility and index costs [43]. Although computer navigation has not consistently shown decreased inpatient length of stay, recent data suggests robotic assisted TKA may be associated with less trauma, resulting in decreased lengths of stay Kayani et al. [44] demonstrated a decrease of approximately 30 hours in inpatient stay with robotic assistance compared with conventional techniques. However, the findings by Kayani et al. must be verified by others before robotic assistance can be recommended as a cost saving measure.
Computer navigation and robotic assistance have been shown to improve consistency of implant positioning, decrease outliers, and reduce intraoperative malalignment. However, data showing improved clinical outcomes are conflicting. The New Zealand registry data found no difference in revision rates with computer navigation vs conventional techniques [32]. However, in a larger study from the Australian National Joint Replacement Registry, De Steiger et al. [28] found a roughly 13% decrease in the revision rate over 9 years with computer navigation in patients <65 years old but were unable to demonstrate a benefit in patients >65 years of age. This difference was attributed to decreased rates of revision due to aseptic loosening. In this study, the revision rates diverged more in the latter years of the 9-year study period, highlighting the possibility of a greater benefit in survivorship with longer follow-up. Of note, the use of computer navigation in the Australian registry increased to 22.8% of primary TKAs in 2012, which is far larger than rates seen in the United States as demonstrated in the present study. A study by Schnurr et al. [31] similarly found decreased revision rates in the early 2-4 years of the postoperative period, again attributed to decreased rates of aseptic loosening. However, this study is limited by its retrospective nature, single-institution analysis, and short-term follow-up. The effect of technology assistance on revision rates in TKA is of critical importance and warrants future study; however, this analysis was outside the scope of this study.
Long-term follow-up studies of TKAs performed using conventional techniques call into question the importance of a neutral mechanical axis and suggest other factors may contribute to patient outcomes and long-term revision rates [45], [46]. However, regardless of the mechanical axis target, proponents of technology assistance believe that decreasing the number of outliers may reduce early failures, improve implant longevity, and lead to improved patient-reported outcomes [12], [33], [35]. A study by Browne et al. [20] found computer-assisted TKAs had fewer cardiac complications, decreased length of stay, and trended toward fewer postoperative hematomas than conventional TKAs. Liow et al. [47] found subtle improvements in patients' quality of life with robotic assistance in a study of 60 TKAs. Kayani et al. [44] provided data supporting earlier functional recovery with robot-assisted surgery. Other studies have demonstrated increased operative times with computer navigation compared with conventional techniques [19], [23]. However, a meta-analysis by Bauwens et al. [18], including over 3,400 patients who underwent a computer-navigated TKA, revealed no conclusive impact of technology assistance on functional outcomes, radiographic accuracy, and total complication rates.
Our study has several strengths, including a large sample size, geographic representation of all regions of the United States, and the inclusion of all payer types, making our results generalizable. Gholson et al. [39] published computer navigation use rates using the NSQIP database over a 5-year period and concluded that the use of computer navigation was decreasing. However, the NSQIP database includes a different annualized sampling of hospitals as new hospitals continue to enroll. As such, temporal trends identified in the NSQIP database may not accurately mirror practice trends in the United States. In contrast, our study showed an increasing use of both computer navigation and robotic assistance, using a database that captures 20% representative sampling of all inpatient discharges. Boylan et al. [40] published similar trends using a New York database from 2008 to 2015 and found results consistent with our findings.
Our study has several limitations. First, this study relies on an administrative database, which relies on accurate coding. Although this is an intrinsic source of potential error, studies have shown that the NIS database captures accurate patient demographic and procedural data [48], [49]. The NIS database has been shown to underestimate comorbidities such as obesity and inpatient complications such as sepsis; however, our study did not rely on comorbidities or complications to describe temporal trends [48], [49]. The use of voluntary ICD-9 modifier codes may have led to underreporting of computer navigation and robotic assistance. However, these technologies can be used to justify increased hospital charges. As such, hospital billers may have a financial incentive to accurately capture these codes. Although same-day total joint arthroplasties are of increasing national interest, outpatient TKAs are not captured in this study given the NIS database only includes inpatient data. Finally, our study identified several univariate and multivariate associations with these technologies; however, no causal conclusions can be derived from these associations.
Conclusions
This study provides national estimates of the use of computer navigation and robotic assistance in total knee arthroplasties and demonstrates regional and demographic differences associated with these technologies. During the study period, a marked increase in the use of these technologies was observed. The use of these technologies is more prevalent in urban hospitals on Medicare beneficiaries and is associated with increased hospital charges. Further studies are needed to justify the clinical use of computer navigation and robotic assistance given the increase in the use and associated costs.
Footnotes
One or more of the authors of this article have disclosed potential or pertinent conflicts of interest, which may include receipt of payment, either direct or indirect, institutional support, or association with an entity in the biomedical field which may be perceived to have potential conflict of interest with this work. For full disclosure statements refer to https://doi.org/10.1016/j.artd.2019.01.002.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.artd.2019.01.002.
Appendix A. Supplementary data
References
- 1.Hopley C.D., Crossett L.S., Chen A.F. Long-term clinical outcomes and survivorship after total knee arthroplasty using a rotating platform knee prosthesis: a meta-analysis. J Arthroplasty. 2013;28:68. doi: 10.1016/j.arth.2012.04.026. e1-e3. [DOI] [PubMed] [Google Scholar]
- 2.Ritter M.A., Meneghini R.M. Twenty-year survivorship of cementless anatomic graduated component total knee arthroplasty. J Arthroplasty. 2010;25:507. doi: 10.1016/j.arth.2009.04.018. [DOI] [PubMed] [Google Scholar]
- 3.Bae D.K., Song S.J., Park M.J. Twenty-year survival analysis in total knee arthroplasty by a single surgeon. J Arthroplasty. 2012;27:1297.e1. doi: 10.1016/j.arth.2011.10.027. [DOI] [PubMed] [Google Scholar]
- 4.Berend M.E., Ritter M.A., Meding J.B. Tibial component failure mechanisms in total knee arthroplasty. Clin Orthop Relat Res. 2004;428:26. doi: 10.1097/01.blo.0000148578.22729.0e. [DOI] [PubMed] [Google Scholar]
- 5.Jeffery R.S., Morris R.W., Denham R.A. Coronal alignment after total knee replacement. J Bone Joint Surg Br. 1991;73:709. doi: 10.1302/0301-620X.73B5.1894655. [DOI] [PubMed] [Google Scholar]
- 6.Anderson K.C., Buehle K.C., Markel D.C. Computer assisted navigation in total knee arthroplasty: comparison with conventional methods. J Arthroplasty. 2005;20:132. doi: 10.1016/j.arth.2005.05.009. [DOI] [PubMed] [Google Scholar]
- 7.Bäthis H., Perlick L., Tingart M. Alignment in total knee arthroplasty. A comparison of computer-assisted surgery with the conventional technique. J Bone Joint Surg Br. 2004;86:682. doi: 10.1302/0301-620x.86b5.14927. [DOI] [PubMed] [Google Scholar]
- 8.Barrett W.P., Mason J.B., Moskal J.T. Comparison of radiographic alignment of imageless computer-assisted surgery vs conventional instrumentation in primary total knee arthroplasty. J Arthroplasty. 2001;26:1273.e1. doi: 10.1016/j.arth.2011.04.037. [DOI] [PubMed] [Google Scholar]
- 9.Chauhan S.K., Scott R.G., Breidahl W. Beaver RJ Computer-assisted knee arthroplasty versus a conventional jig-based technique. J Bone Joint Surg Br. 2004;86:372. doi: 10.1302/0301-620x.86b3.14643. [DOI] [PubMed] [Google Scholar]
- 10.Chin P.L., Yang K.Y., Yeo S.J., Lo N.N. Randomized control trial comparing radiographic total knee arthroplasty implant placement using computer navigation versus conventional technique. J Arthroplasty. 2005;20:618. doi: 10.1016/j.arth.2005.04.004. [DOI] [PubMed] [Google Scholar]
- 11.Clark T.C., Schmidt F.H. Robot-assisted navigation versus computer-assisted navigation in primary total knee arthroplasty: efficiency and accuracy. ISRN Orthop. 2013;2013:794827. doi: 10.1155/2013/794827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Choong P.F., Dowsey M.M., Stoney J.D. Does accurate anatomical alignment result in better function and quality of life? Comparing conventional and computer-assisted total knee arthroplasty. J Arthroplasty. 2009;24:560. doi: 10.1016/j.arth.2008.02.018. [DOI] [PubMed] [Google Scholar]
- 13.Hetaimish B.M., Khan M.M., Simunovic N. Meta-analysis of navigation vs conventional total knee arthroplasty. J Arthroplasty. 2012;27:1177. doi: 10.1016/j.arth.2011.12.028. [DOI] [PubMed] [Google Scholar]
- 14.Matziolis G., Krocker D., Weiss U., Tohtz S., Perka C. A prospective, randomized study of computer-assisted and conventional total knee arthroplasty. Three-dimensional evaluation of implant alignment and rotation. J Bone Joint Surg Br. 2007;89:236. doi: 10.2106/JBJS.F.00386. [DOI] [PubMed] [Google Scholar]
- 15.Hong Y., Jong S., Young S., Hong L., Eun S. Robotic total knee arthroplasty with a cruciate retaining implant: a 10-year follow-up study. Clin Orthop Surg. 2017;9:169. doi: 10.4055/cios.2017.9.2.169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Liow M.H.L., Xia Z., Wong M.K. Robot-assisted total knee arthroplasty accurately restores the joint line and mechanical axis: a prospective randomised study. J Arthroplasty. 2014;29:2373. doi: 10.1016/j.arth.2013.12.010. [DOI] [PubMed] [Google Scholar]
- 17.Decking R., Markmann M., Fuchs J., Puhl W., Scharf H.P. Leg axis after computer-navigated total knee arthroplasty: a prospective randomized trial comparing computer-navigated and manual implantation. J Arthroplasty. 2005;20:282. doi: 10.1016/j.arth.2004.09.047. [DOI] [PubMed] [Google Scholar]
- 18.Bauwens K., Matthes G., Wich M. Navigated total knee replacement. A meta-analysis. J Bone Joint Surg Br. 2007;89:261. doi: 10.2106/JBJS.F.00601. [DOI] [PubMed] [Google Scholar]
- 19.Brown M.L., Reed J.D., Drinkwater C.J. Imageless computer-assisted versus conventional total hip arthroplasty: one surgeon’s initial experience. J Arthroplasty. 2014;29:1015. doi: 10.1016/j.arth.2013.10.007. [DOI] [PubMed] [Google Scholar]
- 20.Browne J.A., Cook C., Hofmann A.A., Bolognesi M.P. Postoperative morbidity and mortality following total knee arthroplasty with computer navigation. Knee. 2010;17:152. doi: 10.1016/j.knee.2009.08.002. [DOI] [PubMed] [Google Scholar]
- 21.Kalairajah Y., Cossey A.J., Verrall G.M., Ludbrook G., Spriggins A.J. Are systemic emboli reduced in computer-assisted knee surgery?: a prospective, randomised, clinical trial. J Bone Joint Surg Br. 2006;88:198. doi: 10.1302/0301-620X.88B2.16906. [DOI] [PubMed] [Google Scholar]
- 22.Deep K., Shankar S., Mahendra A. Computer assisted navigation in total knee and hip arthroplasty. SICOT J. 2017;3:50. doi: 10.1051/sicotj/2017034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Shi J., Wei Y., Wang S. Computer navigation and total knee arthroplasty. Orthopedics. 2014;37:e39. doi: 10.3928/01477447-20131219-15. [DOI] [PubMed] [Google Scholar]
- 24.Kim Y.H., Kim J.S., Yoon S.H. Alignment and orientation of the components in total knee replacement with and without navigation support: a prospective, randomised study. J Bone Joint Surg Br. 2007;89:471. doi: 10.1302/0301-620X.89B4.18878. [DOI] [PubMed] [Google Scholar]
- 25.Kim Y.H., Park J.W., Kim J.S. The clinical outcome of computer-navigated compared with conventional knee arthroplasty in the same patients: a prospective, randomized, double-blind, long-term study. J Bone Joint Surg Am. 2017;99:989. doi: 10.2106/JBJS.16.00791. [DOI] [PubMed] [Google Scholar]
- 26.Aoude A.A., Aldebeyan S.A., Nooh A., Weber M.H., Tanzer M. Thirty-day complications of conventional and computer-assisted total knee and total hip arthroplasty: analysis of 103m855 patients in the American College of Surgeons national surgical quality improvement program database. J Arthroplasty. 2016;31:1674. doi: 10.1016/j.arth.2016.01.042. [DOI] [PubMed] [Google Scholar]
- 27.Cip J., Obwegeser F., Benesch T. Twelve-year follow-up of navigated computer-assisted versus conventional total knee arthroplasty: a prospective randomized comparative trial. J Arthroplasty. 2018;33:1404. doi: 10.1016/j.arth.2017.12.012. [DOI] [PubMed] [Google Scholar]
- 28.De Steiger R.N., Liu Y.L., Graves S.E. Computer navigation for total knee arthroplasty reduces revision rate for patients less than sixty-five years of age. J Bone Joint Surg Am. 2015;97:635. doi: 10.2106/JBJS.M.01496. [DOI] [PubMed] [Google Scholar]
- 29.Decking R., Markmann Y., Mattes T., Puhl W., Scharf H.P. On the outcome of computer-assisted total knee replacement. Acta Chir Orthop Traumatol Cech. 2007;74:171. [PubMed] [Google Scholar]
- 30.Ensini A., Catani F., Leardini A., Romagnoli M., Giannini S. Alignments and clinical results in conventional and navigated total knee arthroplasty. Clin Orthop Relat Res. 2006;457:156. doi: 10.1097/BLO.0b013e3180316c92. [DOI] [PubMed] [Google Scholar]
- 31.Schnurr C., Gudden I., Eysel P., Konig D.P. Influence of computer navigation on TKA revision rates. Int Orthop. 2012;36:2255. doi: 10.1007/s00264-012-1606-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Roberts T.D., Clatworthy M.G., Frampton C.M., Young S.W. Does computer assisted navigation improve functional outcomes and implant survivability after total knee arthroplasty? J Arthroplasty. 2015;30(Suppl 1):59. doi: 10.1016/j.arth.2014.12.036. [DOI] [PubMed] [Google Scholar]
- 33.Rebal B.A., Babatunde O.M., Lee J.H. Imageless computer navigation in total knee arthroplasty provides superior short term functional outcomes: a meta-analysis. J Arthroplasty. 2014;29:938. doi: 10.1016/j.arth.2013.09.018. [DOI] [PubMed] [Google Scholar]
- 34.Liodakis E., Antoniou J., Zukor D. Navigated vs conventional total knee arthroplasty: is there a difference in the rate of respiratory complications and transfusions? J Arthroplasty. 2016;31:2273. doi: 10.1016/j.arth.2016.03.051. [DOI] [PubMed] [Google Scholar]
- 35.Huang N.F.R., Dowsey M.M., Ee E. Coronal alignment correlates with outcome after total knee arthroplasty: five-year followup of a randomized controlled trial. J Arthroplasty. 2012;27:1737. doi: 10.1016/j.arth.2012.03.058. [DOI] [PubMed] [Google Scholar]
- 36.Hiscox C.M., Bohm E.R., TUrgeon T.R., Hedden D.R., Burnell C.D. Randomized trial of computer-assisted knee arthroplasty: impact on clinical and radiographic outcomes. J Arthroplasty. 2011;26:1259. doi: 10.1016/j.arth.2011.02.012. [DOI] [PubMed] [Google Scholar]
- 37.Harvie P., Sloan K., Beaver R.J. Computer navigation vs conventional total knee arthroplasty. J Arthroplasty. 2012;27:667.e1. doi: 10.1016/j.arth.2011.08.009. [DOI] [PubMed] [Google Scholar]
- 38.Petursson G., Fenstad A.M., Gøthesen Ø. Computer-assisted compared with conventional total knee replacement: a multicenter parallel-group randomized controlled trial. J Bone Joint Surg Am. 2018;100(15):1265. doi: 10.2106/JBJS.17.01338. [DOI] [PubMed] [Google Scholar]
- 39.Gholson J.J., Duchman K.R., Otero J.E. Computer navigated total knee arthroplasty: rates of adoption and early complications. J Arthroplasty. 2017;32:2113. doi: 10.1016/j.arth.2017.01.034. [DOI] [PubMed] [Google Scholar]
- 40.Boylan M., Suchman K., Vigdorchik J., Slover J., Bosco J. Technology-assisted total hip and knee arthroplasties: an analysis of utilization trends. J Arthroplasty. 2018;33:1019. doi: 10.1016/j.arth.2017.11.033. [DOI] [PubMed] [Google Scholar]
- 41.Molloy I.B., Martin B.I., Moschetti W.E., Jevsevar D.S. Effects of length of stay on the cost of total knee and total hip arthroplasty from 2002 to 2013. J Bone Joint Surg Am. 2017;99:402. doi: 10.2106/JBJS.16.00019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Cutler D., Ghosh K. The potential for cost savings through bundled episode payments. N Engl J Med. 2012;366(12):1075. doi: 10.1056/NEJMp1113361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Cool C.L., Jacofsky D.J., Seeger K.A., Sodhi N., Mont M.A. A 90-day episode-of-care cost analysis of robotic-arm assisted total knee arthroplasty. J Comp Eff Res. 2019 doi: 10.2217/cer-2018-0136. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 44.Kayani B., Konan S., Tahmassebi J., Pietrzak J.R.T., Haddad F.S. Robotic-arm assisted total knee arthroplasty is associated with improved early functional recovery and reduced time to hospital discharge compared with conventional jig-based total knee arthroplasty. Bone Joint J. 2018;100:930. doi: 10.1302/0301-620X.100B7.BJJ-2017-1449.R1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Parratte S., Pagnano M.W., Trousdale R.T., Berry D.J. Effect of postoperative mechanical axis alignment on the fifteen-year survival of modern, cemented total knee replacements. J Bone Joint Surg Am. 2010;92:2143. doi: 10.2106/JBJS.I.01398. [DOI] [PubMed] [Google Scholar]
- 46.Abdel M.P., Ollivier M., Parratte S. Effect of postoperative mechanical axis alignment on survival and functional outcomes of modern total knee arthroplasties with cement: a concise follow-up at 20 years. J Bone Joint Surg Am. 2018;100:472. doi: 10.2106/JBJS.16.01587. [DOI] [PubMed] [Google Scholar]
- 47.Liow M.H.L., Goh G.S., Wong M.K. Robotic-assisted total knee arthroplasty may lead to improvement in quality-of-life measures: a 2-year follow-up of a prospective randomized trial. Knee Surg Sports Traumatol Arthrosc. 2017;25:2942. doi: 10.1007/s00167-016-4076-3. [DOI] [PubMed] [Google Scholar]
- 48.Bohl D.D., Basques B.A., Golinvaux N.S., Baumgaertner M.R., Grauer J.N. Nationwide inpatient sample and national surgical quality improvement program give different results in hip fracture studies. Clin Orthop Relat Res. 2014;472:1672. doi: 10.1007/s11999-014-3559-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Bohl D.D., Russo G.S., Basques B.A. Variations in data collection methods between national databases affect study results: a comparison of the nationwide inpatient sample and national surgical quality improvement program databases for lumbar spine fusion procedures. J Bone Joint Surg Am. 2014;96:e193. doi: 10.2106/JBJS.M.01490. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.