Abstract
Introduction:
Little is known about what factors predict student engagement in learning communities (LCs). At our institution, we recently converted from an informal, unfunded program with volunteer mentors and no participation requirement to a formal, funded program with a structured curriculum, dedicated mentors, and required attendance. We sought to identify factors that predict student engagement in this new program.
Methods:
Medical students from all 4 years were invited to complete a survey that included self-rating of their level of engagement with their LC. We hypothesized that student engagement would be (1) higher in the new, formal program compared with the informal program; (2) lower among older students; and (3) higher among students who value collective activities for stress management.
Results:
In total, 75% of students completed the survey. Students who participated in the formal LC program reported significantly higher engagement than those who experienced the informal version. Older, out-of-state, and underrepresented in medicine (URiM) students reported lower levels of engagement compared with younger, in-state, and non-URiM students, but gender and campus assignment were not associated with level of engagement. Students who valued participation in extracurricular activities, service work, and time with friends or family all had higher levels of engagement in LCs compared with those who valued more solitary activities.
Discussion:
The formal, structured LC program was associated with higher levels of engagement than the informal program, and engagement was maintained throughout the 4-year curriculum. Subgroups of students reported lower engagement in LCs, and future research is needed to better understand and address this variability in engagement. This study is limited by the fact that students are only surveyed once annually, at a single institution, and our measure of engagement is brief and dependent on student self-report. In addition, it is not possible to discern from this study which components of the formal LC program were most strongly associated with high engagement.
Keywords: engagement, learning communities
Introduction
Learning communities (LCs) are intentionally created groups of students and/or faculty who are actively engaged in learning from each other.1,2 Medical schools have adopted LCs in increasing numbers in recent years as a way to address the need for longitudinal relationships between students and faculty in small groups, promote professional identity formation, improve the learning environment, and decrease student social isolation.3–6 Addressing these needs through LCs requires not only change to the structure of a school’s educational program but also change in the culture of the school. Such cultural changes are often motivational in nature and rely heavily on student engagement in LCs during all years of the curriculum.1,7 “Engagement” in higher education refers to the time and energy students devote to a given learning activity, and growing evidence identifies engagement as a critical component of the learning process.8,9 Learning communities are grounded in social learning theory, which posits that learning takes place in a social context and that new behaviors are adopted through observation and imitation of others, suggesting that the benefit to students from LCs depends, in part, on their level of engagement.10,11
Understanding what predicts LC engagement is an important first step in improving engagement and ultimately understanding whether LCs are meeting their intended goals, yet little is known about predictors of student engagement in LCs. Rosenbaum et al12 describe lower levels of engagement among third- and fourth-year medical students (MS3s and MS4s) compared with first- and second-year medical students (MS1s and MS2s), which they attribute to conflicts with their clinical responsibilities. Another explanation could be that older students have differing personal responsibilities and resources compared with younger students, and so are less likely to engage in school-related community. It remains unclear whether level of training or age is associated with varying levels of engagement in LCs. Bicket et al7 describe the reasons students engaged in leadership of LCs, citing commitment to their institution, a belief in the value of such a program, excitement about starting a new program, a desire to give back, and the opportunity to collaborate with talented peers and faculty. It is not known if students who are not in LC leadership positions are driven to engage in LCs by the same or different reasons. The purpose of this study was to identify predictors of student engagement in LCs. We hypothesized that (1) student engagement would be higher in the newly redesigned and formal program, (2) engagement would be lower among older students, and (3) engagement would be higher among students who value collective or social activities for stress management.
Methods
At the University of Alabama at Birmingham School of Medicine, students are assigned to an LC upon matriculation, and they remain in their LC for the duration of their time in school. Each LC includes about 15 students from each year of medical school (MS1-MS4), for a total of approximately 60 students in each LC. In 2015, the school administration opted to provide funding for our LC program, allowing us to redesign the program in its entirety. Prior to the change, the program was rather informal, relying on voluntary participation from both students and faculty with sessions scheduled by the individual LC at variable times and without a structured curriculum. The sessions, which were designed by a staff member in the Medical Student Services office and facilitated by student leaders, focused on community-building and wellness. Sessions often included a social event, such as dinner or game night. Faculty mentors rarely attended, and student attendance was also variable. With funding, a centralized LC leadership team was established who created a structured curriculum delivered by paid, trained faculty mentors, and LCs were formally integrated into the academic program of the school. Our LC curriculum covers ethics, medical professionalism, and strategies for wellness. Curricular content is delivered in class with an 80% attendance requirement. Learning communities also offer voluntary social events, team competitions, service days, and opportunities to mentor or be mentored. Most LC programming at our institution depends on cooperative activities involving groups of students. Social events include students from all 4 classes in the LC at the same time, but classroom sessions often include students from only 1 or 2 classes at a time to ensure we can discuss topics appropriate to stage of training and maintain manageable group size.
Because the new, formal model of the LC program was rolled out incrementally, in 2016 it applied only to MS1 and MS2 students, in 2017 MS3s were also included, and in 2018, all 4 years were in the formal model. Thus, some upper-class students completing the survey had only experienced the informal model. This allowed for comparison between the formal and informal models.
The study was approved by the Institutional Review Board for Human Use at the University of Alabama at Birmingham. Data were collected over 3 years of a multiyear longitudinal project examining various aspects of health, wellness, and burnout in medical students. The surveys included an item assessing self-rated LC engagement (ie, “Overall, how would you rate your engagement and involvement in your learning community?”), intentionally chosen to capture students’ subjective sense of engagement, as opposed to simply participation. The item was rated on a 10-point (1-10) Likert-type scale, with anchors denoting that 1 signified “not very engaged,” 5 was “somewhat engaged,” and 10 was “very engaged.” A 10-point scale was chosen to allow for a more detailed snapshot of student engagement, which was felt more likely to show differences among students.
In addition to collection and tabulation of basic demographic variables, a variable denoting membership in a racial or ethnic group considered to be underrepresented in medicine (URiM) was calculated. Students were coded as belonging to the URiM group if they endorsed one of the following racial or ethnic identities (either singly or in combination with others): African American, Hispanic/Latino, American Indian/Alaska Native, or Native Hawaiian/Pacific Islander. Age was dichotomized younger than 25 and 25 or older. Students were coded as being assigned to the main (Birmingham) campus or 1 of 3 regional campuses (although all students complete their first and second years on the main campus). Preferred methods of stress management were assessed with the following question: “When it comes to managing stress and staying healthy, how important are each of the following to you?” Respondents were asked to rank the extent to which they valued each activity (time with family, time with friends, physical exercise, religion/spiritual pursuits, relaxation/meditation, reflection/journaling, extracurricular activities in school, hobbies outside of school, and service/charitable work) on a 0 to 5 Likert-type scale.
All students were invited to complete the survey in January or February of 2016, 2017, and 2018. At that point in the curriculum, MS1 and MS2 students were taking organ-based modules, with MS2s still a few months away from taking Step 1 of the United States Medical Licensing Examination (USMLE). MS3s were in clerkships and MS4s were taking electives and completing residency interviews. Surveys were distributed via email using a unique link for each student to prevent duplicate responses, but no unique identifier was included as a part of the final data set. Emails inviting participation were sent in advance of LC sessions (MS1 and MS2) or scheduled class meetings (MS3 and MS4) in which dedicated time was provided to complete the survey. Students had the option of completing the survey on their own time outside of the sessions if they preferred. Paper copies were available during the dedicated time for those who did not have electronic access or preferred paper administration. Participation in the survey was voluntary, confidential, and not linked to any course or curricular requirement. Consent was obtained from all participants at each survey administration via an initial informed consent page with options to opt out or proceed with the survey.
Statistical analysis
Statistical analyses were conducted using Stata, Version 15.1 (StataCorp, College Station, TX, USA). Predictors of self-rated LC engagement were examined using 3 ordered logistic regression models. The first model compared engagement under the formal versus informal LC programs controlling for curricular year. The second model examined demographic predictors of engagement in the formal LC program, including age, gender, in-state residency, curricular year, campus (main vs regional), and URiM status. The third model examined self-rated preferred stress management strategies as predictors of LC engagement, controlling for demographic predictors identified in the second model. Given that several individual class cohorts completed the survey in more than 1 curricular year, the regression analyses were conducted using robust standard errors with class cohort as a clustering variable.
Results
Survey response rates and characteristics of survey respondents are detailed in Table 1. Overall, 2180 surveys were distributed over the 3 annual administrations. A total of 1636 surveys were completed, yielding an overall response rate of 75%. Response rates varied by class, with MS4 students consistently having the lowest response rate (56.6%). Demographic characteristics of respondents were consistent with the characteristics of the student body as a whole. Men comprised 52.1% of the sample, consistent with the slight overrepresentation of men in recent classes. The percentage of URiM respondents (8.7%) fell at the lower end of proportions in recent classes (8%-15%). The proportion of respondents assigned to the main campus (54.4%) was consistent with typical campus assignments (usually 53%). The student body as a whole typically consists of 80% to 90% in-state students, consistent with 81.2% of in-state respondents.
Table 1.
Respondent characteristics by curricular year.
| MS1 | MS2 | MS3 | MS4 | Total | |
|---|---|---|---|---|---|
| Surveys distributed | 569 | 555 | 533 | 523 | 2180 |
| Surveys completed | 438 | 425 | 477 | 296 | 1636 |
| Response rate | 77.0% | 76.6% | 89.5% | 56.6% | 75.0% |
| Age | |||||
| Younger than 25 | 341 (77.9%) | 271 (63.8%) | 140 (29.4%) | 5 (1.7%) | 757 (46.3%) |
| 25 and older | 96 (21.9%) | 154 (36.2%) | 337 (70.6%) | 291 (98.3%) | 878 (53.7%) |
| Gender (men) | 228 (52.1%) | 216 (50.8%) | 246 (51.5%) | 162 (54.7%) | 852 (57.1%) |
| URiM | 45 (10.3%) | 37 (8.7%) | 39 (8.2%) | 22 (7.4%) | 143 (8.7%) |
| Campus (main)a | 233 (50.9%) | 233 (54.8%) | 258 (54.1%) | 166 (56.1%) | 890 (54.4%) |
| In-state | 356 (81.3%) | 337 (79.3%) | 378 (79.2%) | 257 (86.8%) | 1328 (81.2%) |
Abbreviation: URiM, underrepresented in medicine.
Percentages reflect proportion of completed surveys, with the exception of response rate, which reflects the proportion of distributed surveys that were completed.
All students complete the preclinical curriculum on the main campus regardless of campus assignment. Clerkships are completed at the main campus or 1 of 3 regional campuses.
Ratings of LC engagement by curricular year and survey year are presented in Figure 1. Engagement was generally high for students participating in the formal program compared with those participating in the informal program. Mean LC engagement was lower in MS3 and MS4 respondents compared with MS1 and MS2 respondents in survey year 1, but increased as the formal program was expanded into the MS3 and MS4 years.
Figure 1.
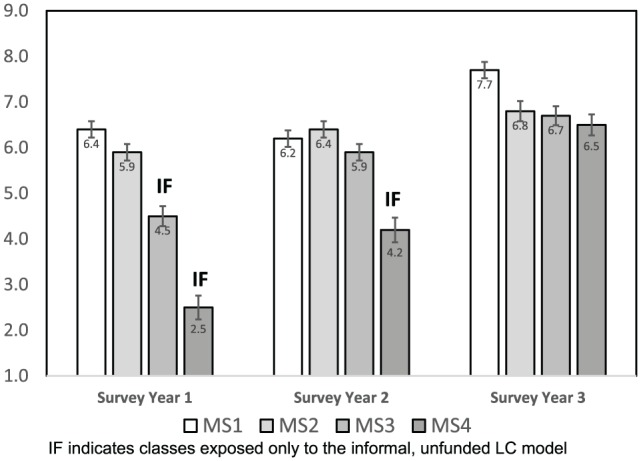
Mean ratings of LC engagement (1-10) by survey year. The formal, funded LC program was implemented for MS1 and MS2 students in survey year 1. It was extended into the MS3 year in survey year 2, and the MS4 year in survey year 3. LC indicates learning community.
Formal vs informal
Results of the ordinal logistic regression analysis examining LC engagement under the formal and informal programs are presented in Table 2. Participation in the formal LC program at the time of survey completion was a robust predictor of higher engagement (P < .001), controlling for curricular year.
Table 2.
Formal program as a predictor of LC engagement (n = 1623).
| Predictor | Coefficient | P |
|---|---|---|
| Curricular year | ||
| MS2 | –0.32 | .394 |
| MS3 | –0.22 | .387 |
| MS4 | –0.55 | .379 |
| Formal program | 1.75 | <.001 |
Abbreviation: LC, learning community.
Values in bold indicate P < .05.
Demographics
Demographic predictors of LC engagement in the formal program are presented in Table 3. Learning community engagement in students 25 years or older was significantly lower than engagement among students under 25 years old (P < .001). In-state students also rated their engagement in LCs as higher than out-of-state students (P = .02). Underrepresented in medicine status was associated with lower LC engagement (P = .02)
Table 3.
Demographic predictors of engagement in the formal LC program.
| Predictor | Coefficient | P |
|---|---|---|
| Age (25 or older) | –0.32 | <.001 |
| Gender (male) | –0.14 | .236 |
| In-state | 0.08 | .022 |
| Curricular year | ||
| MS2 | –0.30 | .458 |
| MS3 | –0.19 | .668 |
| MS4 | –0.03 | .934 |
| Campus (main) | –0.02 | .665 |
| URiM | –0.22 | .022 |
Abbreviations: LC, learning community; URiM, underrepresented in medicine.
Values in bold indicate P < .05.
Approaches to stress management
Results of the regression analysis examining preferred approaches to stress management as predictors of engagement are presented in Table 4. Several approaches to stress management were associated with higher LC engagement, including time with family (P = .009), time with friends (P = .002), extracurricular activities in school (P < .001), and service/charitable work (P = .003). None of the predictors were associated with lower LC engagement.
Table 4.
Preferred methods of stress management as predictors of engagement in the formal LC program.
| Predictor | Coefficient | P |
|---|---|---|
| Age (25 or older) | –0.22 | .026 |
| In-state | 0.05 | .148 |
| URiM | –0.21 | .021 |
| Time with family | 0.05 | .009 |
| Time with friends | 0.34 | .002 |
| Physical exercise | 0.05 | .317 |
| Religion/spiritual/faith | 0.04 | .052 |
| Relaxation/meditation | –0.02 | .749 |
| Reflection/journaling | 0.09 | .129 |
| Extracurricular activities in school | 0.27 | <.001 |
| Hobbies outside of school | –0.06 | .318 |
| Service/charitable work | 0.05 | .003 |
Abbreviations: LC, learning community; URiM, underrepresented in medicine.
Values in bold indicate P < .05.
Discussion
As hypothesized, self-rated engagement in the formal LC program was significantly higher than in the informal program, even when controlling for variability in engagement based on curricular year. These findings are consistent with the recommendations of experts in the field,1 and comparable with those of Rosenbaum et al,12 who reported improved connectedness among students and an increase in participation in various activities under a funded LC program. This study was not designed to identify which specific components of the new program were most highly associated with engagement, but it seems likely that multiple programmatic changes that occurred simultaneously when we adopted the formal program could be implicated, such as dedicated faculty mentors, protected time in the schedule, more frequent social events, and a formal, structured curriculum. One possible alternative interpretation of the increase in engagement is that our formal program, like those at many other institutions,4 included some curricular elements with a minimum attendance requirement. Students might self-rate engagement simply based on their required attendance. However, this seems unlikely as ratings of engagement improved over time and varied across the full range of the scale, and thus do not appear to reflect merely LC time spent in class. It may be that a minimum requirement for attendance creates more consistent exposure to aspects of the program that might promote further engagement (eg, funded social activities, trained faculty mentors with protected time, and structured opportunities for service).
Unlike the findings of Rosenbaum et al,12 engagement among MS3 and MS4 students was not lower than MS1 and MS2 students, which is encouraging given the fact that our LC program, like many, places students from different classes in the same LC, with the goal of encouraging near-peer mentoring and longitudinal cohesiveness in LCs.13 This difference may be explained by programmatic variability, as the University of Iowa Program depended primarily on participation in voluntary extracurricular activities, which can be difficult for clinical students to attend due to schedule constraints, while students at our institution are excused from clinical duties to attend LC sessions. In addition, we intentionally tailor curricular content to focus on topics that are relevant to stage of training, for example, sessions are tied to basic science coursework in the preclinical years, to clinical care in the MS3 year, and to the residency application process in the MS4 year.
The hypothesis that older students would report lower engagement and involvement in LCs (controlling for curricular year) was also supported. Older medical students do report having a different subjective experience, as well as different responses to stress, than younger medical students.14 It may be that the content and structure of LCs appeal less to older students, perhaps because they have less need for the professionalism or wellness topics discussed in class or for the social benefits of extracurricular LC events. Alternatively, older students may simply have less time to devote to voluntary activities due to competing interests. Questions about family were added beginning in the second year of the study and were thus not included in formal analyses here. However, data from those 2 years confirm higher rates of marriage in the older group (33.1% compared with 10.8% of younger students) and higher likelihood of having children in the older group (8.7% compared with 0.8% of younger students).
Two unexpected demographic characteristics were also associated with engagement, and both merit discussion. In-state students reported higher engagement in LCs, which may reflect preexisting social relationships (eg, students who attended the same high school or undergraduate institution) or commonality of cultural background. Underrepresented in medicine students reported lower engagement, which should be interpreted cautiously given the relatively small number of URiM students in our sample (which can amplify response bias). However, there are several reports in the literature that URiM medical students may be less socially connected, which would support our finding of lower levels of engagement in LCs.14,15 Inclusivity in LCs is obviously of the utmost importance, and barriers to inclusivity can occur at many levels, including curricular content, faculty mentor characteristics, student leader characteristics, dynamics between students, and the nature of social events. As aggregate assessments such as surveys may fail to capture the concerns of specific groups, we plan to pursue alternate approaches relying on qualitative methodologies to better understand this finding. LC leaders need to consider the needs of, and seek input from, a wide variety of subgroups when developing their programs.
We found support for our hypothesis that engagement would be higher among students who place value on cooperative activities for management of stress. This lends some support to the notion that it is the social and community-based aspects of the LC program that drive engagement for many students. That said, there is a significant proportion of students who prefer to manage their stress with activities that are more solitary, such as journaling or meditation, and we would not recommend LCs avoid these activities simply because these students tend to be less engaged. In fact, the opposite is probably true: LC programs probably should include more such activities to enhance engagement among these students. We do find it encouraging that these “solitary activity” students did not have lower engagement, suggesting that LCs still have the potential to appeal to a wide variety of students in spite of their strong “group activity” orientation.
Study limitations
Several limitations of this study should be considered, including the fact that students are only surveyed annually, so changes in engagement over the course of the year cannot be captured. In addition, because it is only at 1 institution, results may not be generalizable. One of the strengths of this study is the large multiyear sample, but this comes at the expense of using a brief and subjective self-rating of LC engagement. This does not allow for nuanced exploration of engagement, nor do we have corresponding objective measures of engagement (attendance at events, etc) that can be linked with the anonymous survey data. We are also not able to link academic metrics for the same reason, and thus cannot address the academic characteristics associated with LC engagement. As mentioned previously, multiple intertwined interventions were adopted as a part of the redesigned, formal LC model, so it is not possible to tell which component was the most important in achieving higher levels of engagement (ie, protected faculty time, dedicated curricular time, curricular content, social events, etc). Finally, our sample may be large, but key groups of students (eg, older students, URiM students) comprise relatively small subsamples.
Implications for LCs and future directions
The formal LC program garnered more student engagement than the informal program, but it is essential to point out that funding alone cannot achieve this. With funding came centralized program leadership, a curriculum with required participation, consistency of implementation, integration into medical school events, and longitudinal access to trained faculty mentors with protected time. Funding may also be a proxy for other less tangible aspects of institutional commitment and support. Provision of funding in the absence of broader institutional commitment or readiness for change may not yield the same results. Future investigations should examine which of these components are essential for building student engagement.
Our data suggest that LC programming can be implemented in a way that cultivates engagement of a diverse range of students in all 4 years. Younger students who value social activities may be the “low hanging fruit” of LC engagement, but our data suggest that it may be more challenging to engage older, out-of-state, and URiM students, as well as those who prefer solitary activities for stress management. There is so much variability between LC programs at different institutions that meeting the needs of each of these groups will likely be achieved in different ways depending on the program and the needs of these different populations. At our institution, it seems possible that making LCs mandatory was actually helpful in driving engagement among third- and fourth-year students. Further study is needed to better understand how to meet the needs of these students.
The number of schools with LCs is increasing exponentially,4 and for programs to succeed, it is essential to understand how to engage students from diverse backgrounds with varying preferences. Engagement alone is not the most important measure of LC success, and future publications from our group will document student wellness outcomes associated with LCs at our institution. Nonetheless, engagement is a necessary condition for the type of cultural change in medical education that many LC programs seek to achieve.7 When students are highly engaged in LCs, there is tremendous potential to improve student well-being, catalyze essential learning, and transform students into physicians with the skills and values we all hope for in our health care providers.
Acknowledgments
The authors would like to thank Laura Kezar and Craig Hoesley for their tireless support of the learning community (LC) program, as well as Anne Zinski, Nicholas Van Wagoner, and Fredrick Vars for their careful edits of earlier versions of the manuscript.
Footnotes
Funding:This work was supported by a grant from the University of Alabama School of Medicine Dean’s Research Award.
Declaration of conflicting interests:The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Author Contributions: Study design and data collection were overseen by Drs. Baños and Harada. Data analyses were performed by Dr. Baños. All authors participated in the interpretation of results and preparation of the manuscript. All authors reviewed and approved the final manuscript.
ORCID iD: Caroline N Harada  https://orcid.org/0000-0002-3072-4021
https://orcid.org/0000-0002-3072-4021
References
- 1. Fleming A, Cutrer W, Moutsios S, et al. Building learning communities: evolution of the colleges at Vanderbilt University School of Medicine. Acad Med. 2013;88:1246–1251. [DOI] [PubMed] [Google Scholar]
- 2. Lenning OT, Ebbers LH. The Powerful Potential of Learning Communities: Improving Education for the Future. Washington, DC: ERIC Publications; 1999. [Google Scholar]
- 3. Osterberg LG, Goldstein E, Hatem DS, Moynahan K, Shochet R. Back to the future: What learning communities offer to medical education. J Med Educ Curric Dev. 2016;3:67–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Smith S, Shochet R, Keeley M, Fleming A, Moynahan K. The growth of learning communities in undergraduate medical education. Acad Med. 2014;89:928–933. [DOI] [PubMed] [Google Scholar]
- 5. Ferguson KJ, Wolter EM, Yarbrough DB, Carline JD, Krupat E. Defining and describing medical learning communities: results of a national survey. Acad Med. 2009;84:1549–1556. [DOI] [PubMed] [Google Scholar]
- 6. Zhao C, Kuh GD. Adding value: learning communities and student engagement. Res High Educ. 2004;45:115–138. [Google Scholar]
- 7. Bicket M, Misra S, Wright SM, Shochet R. Medical student engagement and leadership within a new learning community. BMC Med Educ. 2010;10:20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Kahu ER. Framing student engagement in higher education. Stud High Educ. 2013;38:758–773. [Google Scholar]
- 9. Kuh GD. What we’re learning about student engagement from NSSE. Change: Mag High Learn. 2003;35:24–32. [Google Scholar]
- 10. Torre DM, Daley BJ, Sebastian JL, Elnicki DM. Overview of current learning theories for medical educators. Am J Med. 2006;119:903–907. [DOI] [PubMed] [Google Scholar]
- 11. Mann KV. Theoretical perspectives in medical education: past experience and future possibilities. Med Educ. 2011;45:60–68. [DOI] [PubMed] [Google Scholar]
- 12. Rosenbaum ME, Schwabbauer M, Kreiter C, Ferguson KJ. Medical students’ perceptions of emerging learning communities at one medical school. Acad Med. 2007;82:508–515. [DOI] [PubMed] [Google Scholar]
- 13. Hafferty FW, Watson KV. The rise of learning communities in medical education: a socio-structural analysis. J Cancer Educ. 2007;22:6–9. [DOI] [PubMed] [Google Scholar]
- 14. Royal KD. Medical students rate black female peers as less socially connected. J Natl Med Assoc. 2018;110:157–162. [DOI] [PubMed] [Google Scholar]
- 15. Vaughan S, Sanders T, Crossley N, O’Neill P, Wass V. Bridging the gap: the roles of social capital and ethnicity in medical student achievement. Med Educ. 2015;49:114–123. [DOI] [PubMed] [Google Scholar]


