Abstract
Background:
Substance use disorders (SUDs) have been assumed to be rare in individuals with autism spectrum disorder (ASD). Recent research suggests that the rates of SUD among individuals with ASD may be higher than assumed although reliable data on the prevalence of SUD in ASD are lacking. Typical interventions for SUD may be particularly unsuitable for people with ASD but research on intervention and therapy are limited.
Methods:
This study addresses ways of improving services for individuals with ASD and SUD by enhancing the competence of professionals in ordinary SUD outpatient clinics. Three therapists were given monthly ASD education and group supervision. The participants were ordinary referred patients who wanted to master their problems with alcohol or drugs. Four patients, all men diagnosed with ASD and intelligence quotient (IQ) ⩾ 70 completed the treatment. The participants were given cognitive behavioural therapy (CBT) modified for their ASD over a minimum of 10 sessions. The therapies lasted between 8 and 15 months. Standardised assessments were conducted pre- and post-treatment.
Results:
Post-treatment, 2 participants had ended their drug and alcohol abuse completely, 1 had reduced his abuse, and 1 still had a heavy abuse of alcohol. Physical well-being was the most prevalent reported positive aspect of drug or alcohol use, whereas the experience of being left out from social interaction was the most frequent negative aspects of intoxication.
Conclusions:
CBT may represent a promising treatment option for individuals with ASD and SUD. The results suggest that patients’ symptoms can be reduced by providing monthly ASD education and group supervision to therapists in ordinary SUD outpatient clinics. This group of patients need more sessions than other client groups, the therapy has to be adapted to ASD, ie, direct, individualised, and more extensive. Moreover, the patients need psychoeducation on ASD generally, social training, and support to organise several aspects of their lives and some patients need more support than can be provided in an outpatient clinic.
Keywords: autism spectrum disorders, substance abuse disorder, treatment
According to the United Nations Office on Drugs and Crime,1 approximately 29.5 million people, or 0.6% of the global adult population, have a substance use disorder (SUD). There are a number of mental health conditions that are particularly associated with high rates of SUD, including personality disorders (25%-51%), affective disorders (16%-35%), anxiety (16%-18%), schizophrenia (47%), bipolar disorder (56%), and post-traumatic stress disorder (PTSD; 37%).2–5 Certain developmental disorders, notably attention deficit hyperactivity disorder (ADHD), are also overrepresented in treatment-seeking SUD populations.6–8 For example, a recent meta-analysis showed a 23% comorbidity of ADHD in an adult mixed SUD population, ranging from 10% to 54% in different studies.7 In contrast, among individuals with autism spectrum disorder (ASD), SUD has generally been assumed to be relatively uncommon.9–11 ASD is a neurodevelopmental disorder characterised by deficits in social interaction and communication together with a restricted repertoire of activities and interests.12,13 Because of their social and communication deficits, many adolescents and adults with ASD have very limited social networks outside their family14,15 and it has been suggested that this may be a protective factor for SUD10 and that young people with ASD are less likely to be influenced by their peers when it comes to experimenting with alcohol or drugs.9
Nevertheless, recent research suggests that the rates of SUD among individuals with ASD may be higher than is often assumed.16 A recent systematic review of the literature17 identified 18 studies that examined the association between ASD and SUD. A total of 11 papers specifically explored the frequency of SUD in ASD but reported that the rates ranged widely, from 0.7% to 36%, and most studies involved highly selected samples, such as offenders or patients in mental hospitals. Sample sizes were variable and age, intellectual level, and sex distribution of participants varied between samples. Few studies reported formal diagnostic criteria for SUD, and definitions of SUD ranged from ‘having experienced trouble with alcohol or drugs’ to ‘current substance addiction’. Such inconsistencies limit comparisons between studies, but although there are difficulties in establishing an overall estimate for the co-occurrence of ASD and SUD, most existing research suggests that the rates are lower than those in the general population. In contrast, a recent Swedish study, based on register data, found that there was a much higher risk of SUD among individuals with ASD than among non-ASD controls (odds ratio [OR] = 2.6; 95% confidence interval = 2.4-2.9).18 The risk was particularly high in individuals with ASD and comorbid ADHD (OR = 8.3; 95% confidence interval = 7.4-9.2), but there was no increased risk for individuals with ASD and intellectual disability (ID) (OR = 1.1; 95% confidence interval = 0.9-1.3). Other studies suggest that SUD is more likely to occur in individuals with ASD who are more socially outgoing, or of higher intelligence than those who are more socially withdrawn or of lower ability.17,19 Only 1 study has compared the prevalence of SUD among individuals with ADHD or ASD. In this sample, comorbidity was almost twice as high in ADHD (58%) as in ASD (30%).19
The high frequency of anxiety and other psychiatric disorders among individuals with ASD has been proposed as a principal reason for their use of alcohol or illegal drugs.20,21 Other reasons for drug or alcohol use, reported by individuals with ASD, include a reduction in social inhibition, the ability to forget problems and/or to attain peace of mind, to get through the day, or to overcome frustration. Kronenberg et al22 emphasise, however, that although substance use was reported to solve ASD-related problems in the short term, in the longer term substance abuse increased already-impaired functioning. Substance abuse may represent a particular vulnerability factor for individuals with ASD, as intoxication may further decrease the ability to anticipate the consequences of their behaviour and make it even more difficult to behave according to formal and informal laws.23
The lack of reliable data on the prevalence of SUD in ASD is paralleled by a lack of intervention research. In the above-mentioned review,17 no studies of specific treatment strategies were found; moreover, typical interventions for SUD, for example, group therapy, may be particularly unsuitable for people with ASD. In general, about 50% of individuals seeking treatment for SUD drop out before completing treatment,24 and to reduce drop-out and enhance therapeutic effects, there is a need to develop individualised treatment for those patient groups who do not benefit from regular SUD treatment programmes. The special characteristics of individuals with ASD suggest that this may be a subgroup particularly in need of adjusted SUD treatment.
Kronenberg et al20,22,25 have provided valuable information for better understanding the needs of patients with co-occurring ASD and SUD, but they did not test specific interventions. The authors note that the needs of patients with ASD and SUD are more extensive and more severe than those of individuals with SUD and ADHD or other psychiatric diagnoses, and that SUD treatment requires medical, psychological, and social interventions, as well as support for housing, education, transportation, and legal services. Furthermore, they argue that intervention approaches should be instructive and directive.
Cognitive behavioural therapy (CBT) does seem to have promise in treating other comorbid disorders in ASD, for example, anxiety.26–29 There is, however, a general consensus that CBT has to be adjusted to the communication and comprehension difficulties and specific needs that characterise individuals with ASD. There is a particular need to deal with the social problems more generally. To minimise stress and anxiety, a rehabilitation plan should include strategies similar to those typically recommended for people with ASD, such as the incorporation of familiar routines and activities, and staff-client interaction should uphold structure and predictability.30
To provide adequate services to individuals with ASD and SUD, there is a need to develop guidelines and recommendations for treatment. This study is, to our knowledge, the first publication reporting experiences from treating this group in a systematic way. Based on recommendations from previous ASD and SUD reports20,22,25 together with studies on treatment of psychiatric disorders in ASD,27–29 CBT was chosen as the main intervention strategy and therapy was provided individually in an outpatient clinic to a small group of referred patients with ASD and SUD.
This study addresses ways of improving services for individuals with ASD and SUD by enhancing the competence of professionals in ordinary SUD outpatient clinics. The outcome of individually focused CBT for individuals with SUD and ASD is also explored. The aims were to explore the individuals’ explanations for drug and alcohol abuse, to educate and support therapists in conducting CBT with these individuals, to explore necessary adjustments to therapeutic techniques, and to monitor outcome by standardised assessment instruments and by patients’ own evaluation.
Method
Participants
A total of 3 therapists in an ordinary SUD outpatient clinic were recruited to the project. The therapists were 2 psychiatric nurses and 1 psychologist and all the three had extensive clinical experience with SUD patients and had training in CBT. They were given monthly group education and supervision by a psychologist with long experience in the field of autism. The main themes of supervision were the characteristics of ASD and discussions on how to conduct therapy and adjust CBT to the needs of individuals with ASD.
All patients were referred by their family doctor to the clinic because they wanted to overcome their problems with alcohol or drugs. To enhance the number of patients with ASD, the project was advertised through websites and flyers at SUD outpatient clinics, ASD services, and user organisations. The inclusion criteria were as follows:
Previous diagnosis of ASD according to International Statistical Classification of Diseases and Related Health Problems, 10th Revision (ICD-10; WHO, 1992)
Intellectual ability within the normal range, ie, intelligence quotient (IQ) ⩾ 70;
Aged over 16 years;
Able to attend weekly outpatient sessions.
In total, 7 patients (6 men and 1 woman) were recruited to the study, but 3 individuals ended treatment before it was finished and before assessments were completed. The reasons for drop-out were as follows: sudden death just when treatment started, 1 therapist ended her participation in the study, and 1 patient was misdiagnosed with ASD. Thus, the final sample consisted of 4 patients, all men, aged between 22 and 44 years (mean: 31.4 years). All four were previously diagnosed with Asperger syndrome by specialists in mental health services. In addition, they all scored above cut-off on the autism spectrum quotient (AQ)31 (mean: 31.8; range: 23-42) and all had an IQ within the normal range (mean: 110.8; range: 102-125). The 4 participants were also diagnosed with anxiety and depression as co-occurring psychiatric disorders. One individual was in regular employment, one had been offered a place on a work preparation scheme, and two were without any regular daily activity. Two participants had their own apartments, one lived with his parents and siblings, and one lived in a sheltered home. Pre-treatment drug use included amphetamines, cocaine, alcohol, and benzodiazepines; three participants had used a wide mix of substances; one was dependent on alcohol.
Details on the drug and alcohol use pre- and post-treatment for the 4 patients who completed the treatment are presented in Table 1. Based on ICD-10,12 Patient 1 was diagnosed with F15.2 Other stimulant dependence and F13.2 Sedative, hypnotic, or anxiolytic dependence. He used drugs on a daily basis. Patient 2 was diagnosed with F10.2 Alcohol dependence. He had used alcohol for 10 years when the project began and drank 12 to 16 bottles of beer (0.5l) 3 to 4 days a week. Patient 3 was diagnosed with F11.22 Opioid dependence and F13.21 Sedative, hypnotic, or anxiolytic dependence in remission. Patient 4 was diagnosed with F12.2 Cannabis dependence. He started with drugs 10 years ago and used drugs on a daily basis. Mean age of onset was 19.5 years (Patient 1: 27 years, Patient 2: 19 years, Patient 3: 16 years, Patient 4: 16 years old). Mean duration of drinking/using drugs was 14.3 years (Patient 1: 9 years, Patient 2: 11 years, Patient 3: 28 years, Patient 4: 9 years.)
Table 1.
Patients’ alcohol and drug use pre- and post-treatment.
| Patient | Pre-treatment |
Post-treatment |
||||
|---|---|---|---|---|---|---|
| Positive about using drug (out of 68) | Negative about using drugs (out of 68) | Thoughts about drug use (out of 10) | Positive about using drug (out of 68) | Negative about using drugs (out of 68) | Thoughts about drug use (out of 10) | |
| 1 (DUDIT-E) | 46 | 16 | 5 | 26 | 34 | 7 |
| 2 (Alcohol-E) | 19 | 28 | 4 | 19 | 32 | 4 |
| 3 (DUDIT-E) | 41 | 13 | 5 | 24 | 15 | 8 |
| 4 (DUDIT-E) | 30 | 22 | 4 | * | ||
Alcohol-E, Alcohol Use Disorders Identification Test – Extended; DUDIT-E, Drug Use Disorder Identification Test – Extended.
Alcohol-E is reported for the patient with alcohol dependency.
DUDIT-E is reported for the patients with drug use.
Significance level cannot be computed because there are less than 5 records.
Missing data – Patient 4 totally ended his drug use, but DUDIT-E was not completed.
Pre- and post-treatment assessment
The following assessments were performed before treatment. IQ was assessed by the WAIS-III32 or the WAIS (Wechsler Abbreviated Scale of Intelligence).33 The latter covers the age range from 6 to 89 years and has been found to correlate well with WAIS-III.34 The AQ30 is a frequently used instrument for assessing autism symptoms among individuals with intellectual functioning within the normal range. The AQ has been found to have excellent test-retest reliability (scores from the first and second AQs did not differ statistically, t(16) = 0.3, P = .75, and were strongly correlated). Reasonable face validity and construct validity have also been demonstrated. The internal consistency of items in each subscale has been found to be moderate to high (0.65, 0.77, 0.65, 0.63, 0.67). The Hopkins Symptom Checklist-25 (HSCL-25)35 was used to assess psychiatric comorbidity because this instrument is part of routine practice at the SUD outpatient clinic involved. HSCL-25 includes 25 questions and assesses anxiety, depression, and somatisation which are the psychiatric disorders most likely to co-occur with ASD. HSCL is a well-known and widely used screening instrument and it has been demonstrated in several populations that the total score is highly correlated with severe emotional distress of unspecified diagnosis, and the depression score is correlated with major depression as defined by the Diagnostic and Statistical Manual of Mental Disorders (4th ed.; DSM-IV).36 Drug Use Disorder Identification Test – Extended (DUDIT-E)37 and Alcohol Use Disorders Identification Test – Extended (Alcohol-E)38,39 were used to assess drug and alcohol use before and after treatment and positive and negative experiences with intoxication. These screening tools have moderate to high accuracy for identification of dependency diagnoses. The Alcohol Use Disorders Identification Test (AUDIT) has demonstrated association with alcohol problem severity, whereas the DUDIT has demonstrated association with drug and legal problem severity. The DUDIT has satisfactory measures of reliability and validity for use as a clinical or research tool. Internal consistency reliability estimates (Cronbach α) are generally >0.90. Most studies also revealed favourable sensitivity (ranging from 0.85 to 1.00) and specificity (ranging from 0.75 to 0.92) in a variety of populations.40
The Global Assessment of Functioning (GAF)41 is part of routine practice at the SUD outpatient clinic and was used to assess psychosocial functioning before and after treatment. The GAF is well known internationally and widely used for scoring the severity of illness in psychiatry. In Norway, the GAF is mandatory in all mental health services despite reported problems with both reliability and validity. Overall reliability can be good, but concurrent validity and predictive validity have been found to be more problematic and few empirical results for GAF sensitivity have been reported.42 We used the version in which symptoms (GAF-S) and functioning (GAF-F) are rated separately. The Motivational Interview (MI)43 is also part of routine practice at the clinic and was used to identify the patients’ goals for and anticipations of therapy and to develop an individualised plan in collaboration with the patients. Post-treatment, the Patient Satisfaction Questionnaire (PSQ-18)44 was used to assess patients’ own evaluation of the treatment. All subscales in PSQ-18 have demonstrated acceptable internal consistency reliability, and the short form is substantially correlated with the long form of the questionnaire as well as with multiple scales assessing satisfaction with treatment.
To obtain information on the therapeutic experience of treating patients with ASD and SUD and the challenges of adapting CBT to patients with ASD, the therapists were interviewed individually post-treatment about what they experienced as challenging, what the differences were between patients with ASD and SUD compared with patients with SUD only, and about their suggestions and recommendations for other clinicians who may be treating SUD in individuals with ASD.
Intervention
The primary treatment components in CBT include psychoeducation, cognitive restructuring, relaxation strategies, exposure, and response prevention. The treatment aims at changing ways of thinking and teaching new strategies for self-monitoring and coping. The participants were offered CBT over a minimum of 10 sessions. The CBT treatment was modified to meet the communication and comprehension difficulties that characterise autism, and substantially expanded to address ASD-related clinical characteristics such as social functioning, adaption and self-care, and circumscribed interests and stereotypies according to recommendations by Wood et al.45 The therapy was provided as part of regular clinical practice. The length of each session varied. Because this was an explorative study, specific manuals were not used, but the therapists selected materials and exercises from different available CBT manuals and adjusted these to individuals’ needs and difficulties.
The study initially aimed to explore the outcome of treatment by CBT over 10 to 20 sessions. However, the time to establish contact and to assess and complete the different elements of the treatment was more time-consuming than anticipated. Most participants had additional problems that had to be dealt with, such as organising their daily life and living conditions and problems in completing education or getting a job. Thus, it was not considered ethical to end treatment after 20 sessions and up to 40 sessions were found to be necessary.
Ethical issues
Informed consent was obtained from all the patients. Data were anonymised and processed without name, identification number, or other directly recognisable types of information. The project was approved by the Privacy Protection Supervisor (local institutional review board [IRB]) at Oslo University Hospital, Oslo, Norway. Approval #2013/17582. To preserve anonymity, the results are presented mainly on a group level.
Results
Four participants completed the treatment. They were provided with 30 to 40 sessions each, and in addition there were failed appointments, collaboration meetings with local professionals, care staff, and family member, and phone calls. Therapy lasted between 8 and 25 months (mean = 17 months). Post-treatment, 2 participants had ended their drug and alcohol abuse completely, 1 had reduced his abuse, and 1 remained heavily dependent on alcohol. More details on the patients’ alcohol and drug use are presented in Table 1. Most patients changed positively their thoughts about drugs and alcohol from pre- to post-treatment, but unfortunately data were missing from one of the completers, and significance level could not be computed because there were fewer than 5 records.
Among the positive and negative aspects of drug and alcohol use reported pre-treatment, physical well-being was described as the most positive aspect by 3 participants. One participant reported psychological well-being as the most positive. The experience of being excluded from social interactions was reported as the most negative aspect of intoxication by 2 participants. One participant reported crime and violence involvement as a negative aspect of drug or alcohol use, and one also reported that drug and alcohol use might reduce physical health. Examples are listed in Table 2.
Table 2.
Positive and negative aspects of intoxication; explanations given by the participants (N = 4).
| Why do you use drugs or alcohol? | Why do you want to stop using drugs or alcohol? |
|---|---|
| I drink to reduce my anxiety and improve my social skills and concentration. | I started using drugs to find peace and reduce pain. Now I have lost both my family and my job. |
| Then I am able to socialise with others. | I still feel socially excluded. |
| I drink to get peace and forget problems and conflicts. | When I have been out on town, I have been arrested by the police. |
| I feel normal when I am intoxicated. | I check all the time in the mirror to find out if have been injured by my drug use. |
| I get free from worrying and bad thoughts. I get through the day. | I drink when I am out together with colleagues from work, but I find it difficult to control my drinking and get very drunk and have experienced events that I regret afterword. |
| All my problems were solved when I started with marihuana – I became myself. | I feel ill physically and it is bad for my body. |
| I am not able to anticipate a life without marihuana. | |
| I get more social, think clearer, and get peace of mind. |
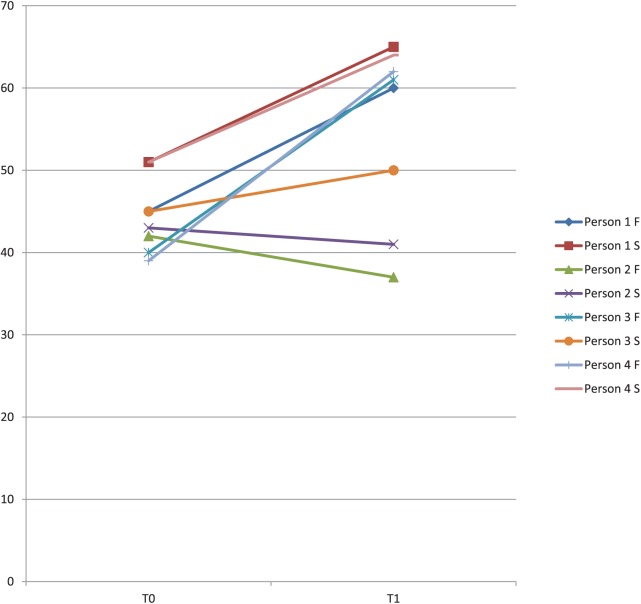
Pre- and post-treatment functioning (GAF) are presented in Figure 1. Participants 1 and 4 showed improvement in both functioning and symptoms (Person 1 F: T0 = 45 and T1 = 60; Person 1 S: T0 = 51 and T1 = 65; Person 4 F: T0 = 39 and T1 = 64, Person 4 S: T0 = 51 and T1 = 64). Participant 3 showed improvement in functioning (Person 3 F: T0 = 40 and T1 = 61) but only slight improvement in symptoms (Person 3 S: T0 = 45 and T1 = 50). Participant 2 showed a decline in functioning accompanied by a slight decline in symptoms (Person 2 F: T0 = 42 and T1 = 37; P2 S: T0 = 43 and T1 = 41).
Figure 1.
Global Assessment of Functioning (GAF) pre- and post-treatment functioning and symptoms.
N = 4, GAF-F = functioning and GAF-S = symptoms, pre-treatment ratings = T0, post-treatment ratings = T1.
GAF-F: T0 - Min = 39, Max = 45, median = 41, standard deviation = 2.65; T1 - Min = 37, Max = 62, median = 60.5, standard deviation = 12.03. The median difference between GAF-F T0 and T1 calculated by Wilcoxon signed rank test is 0.144, P < .05.
GAF-S: T0 - Min = 43, Max = 51, Median = 48, standard deviation = 4.12; T1 - Min = 41, Max = 65, median = 57, standard deviation = 11.58. The median difference between GAF-S T0 and T1 calculated by Wilcoxon signed rank test is 0.144, P < .05.
The patients’ evaluation of therapy was assessed by PSQ-1843 which include 8 questions that are rated from 1 to 4 (1 = not satisfied, 4 = very satisfied). Although there is variation, in general the ratings are high with a mean item score of 3.3 and a mean total score of 26.5 (max rate = 32).
In the post-treatment interview, the therapists noted that the therapy was more time-consuming because the patients with ASD required several sessions to complete assessments and to establish goals for the treatment; all the other elements of therapy also took longer than usually recommended. In addition, they described therapy with these individuals as challenging and quite different from therapy with other SUD patients. In particular, the patients’ communication style often made the therapists feel helpless and as if they were losing control, and this led to their shifting towards a more structured and directive therapeutic approach. Obtaining support from each other and the supervisor was considered essential for several reasons: to learn how to structure sessions most effectively; to continue therapy without becoming dispirited by apparent lack of success; to explore ways of presenting psychoeducative elements and how to adjust strategies to ASD characteristics. All agreed that knowledge of and experience with ASD is crucial to help these patients overcome their problems with alcohol and drugs. Likewise, collaboration with family and local professionals should be established early in the therapeutic process because individuals need help with many other aspects of their lives, such as housing, getting a job, and establishing social contacts with peers who are not involved in drug or alcohol abuse. Loneliness was described as a significant problem for these patients. In addition, establishing contact with local support services early in the therapy may help avoid patients feeing rejected or disappointed when the course of therapy is completed. Clinical recommendations based on interviews with the therapists are listed in Table 3. Adjustments to traditional CBT are listed in Appendix 1.
Table 3.
Clinical recommendations – important factors in therapy for ASD and SUD.
| Therapy course and structure Therapy for this group is more complex than simply following a manual. The therapy has to be more detailed and thorough; length of sessions and duration of treatment usually need to be increased. To optimise predictability for the patient, sessions should, as far as possible, be at a fixed time each week. It is important to discuss the likely duration of intervention at the beginning of the therapy. The therapy has to be structured, direct, and concrete, and supplemented with written guidance. Written plans, notes, and/or homework assignments are an essential adjunct to therapy. The use of a motivational interview is useful for making a plan for treatment and outcome. Psychoeducation about ASD characteristics and how they may impact on each individual is important. Stability is vital – changing therapist is very challenging for patients. Ending treatment is difficult because the patient may feel rejected. |
| Therapist characteristics Therapists should have previous experience of conducting CBT. It is preferable for the therapist to have had have previous experience of working with individuals with ASD. Therapists have to be persevering and patient and recognise that they may feel incompetent in dealing with the challenges of autism. They may also experience a strong emotional commitment to their patient. Flexibility and creativity are vital therapeutic techniques. |
| Patient characteristics Some patients believe that they are drug experts although they seldom are. Some patients stop using drugs immediately although this can imply a health risk. Most patients have a challenging communication style and may take control over the sessions. |
| Collaboration/external support Some patients will need more support than can be provided in an outpatient clinic. Supervision by experienced clinicians is vital, as is collaboration with colleagues. The therapist should be able to support the patient after ending the therapy – and offer follow-up sessions as needed. It is crucial to establish collaborations with other relevant services and with the family. It is important to help the patient establish relationships with local support professional before ending therapy. Most patients need help with more than SUD; housing, employment, social contacts, etc. |
ASD, autism spectrum disorder; CBT, cognitive behavioural therapy; SUD, substance use disorder.
Discussion
To our knowledge, this study represents the first report on treating SUD in individuals with ASD in a systematic way. The findings suggest that SUD treatment for individuals with ASD can work if therapists are provided with ASD-specific education and specialist, monthly group supervision. Individually tailored treatment based on CBT comprising 30 to 40 sessions was associated with some improvement in 3 of the 4 participants who completed the treatment. Two patients ended their use of drugs and alcohol completely, and three of the four participants showed improvement in functioning and symptoms. However, 3 of the 7 participants initially referred to the study dropped out, which is comparable with SUD treatment generally.23 The patient who did not improve was referred to further treatment because he needed more support than could be provided in an outpatient clinic. Thus, to minimise drop-out rates and ensure a better outcome, a range of services adjusted to the needs of people with ASD are needed.
The main explanations for their drug use reported by the participants in this study involved physical and psychological well-being. As previously suggested,20,22,23 this may be a form of ‘self-medication’ and a means of attempting to cope with social difficulties and dealing with anxiety and depression. However, as noted by Kronenberg et al,20 such strategies tend to be unsuccessful in the longer term. Among the negative aspects of drug use reported by the participants was the exclusion from social interactions, and Butwicka et al18 have also described increased social isolation as a result of drug use by people with ASD. In addition, 1 participant reported becoming involved in crime and violence as a negative aspect of drug use, and this may be associated with the relatively high prevalence of SUD in cohorts of offenders with ASD.46,47 Overall, substance abuse seems to contribute to already-impaired functioning and may represent a particular vulnerability factor. Intoxication may further decrease the ability of individuals with ASD to anticipate the consequences of their behaviour and make it even more difficult to act appropriately and acceptably in social situations.23
The therapists noted that the therapy was more demanding than with other SUD patients, which corresponds to the experiences described by Kronenberg et al.20,22,25 Among the modifications they reported was the need to be more structured and to use more directive strategies; SUD therapy also had to be individualised, more extensive, and composed of more sessions than with other patient groups. This is in line with the general consensus that CBT needs to be specially adapted to meet the communication and comprehension difficulties and specific needs of individuals with ASD.26–29,30,45 March48 argues for widening the access to CBT for individuals with disabilities and for moving away from manual-based CBT towards a more individualised and personalised approach that accounts for comorbidity and individual needs. Therefore, a specific manual was not used in this study. Due to the large variability in the group, treatment plans were individually developed and different materials and exercises from available CBT manuals were adjusted to the individuals’ needs and difficulties. There is reason to assume that a general CBT manual for SUD treatment in individuals with ASD will not be expedient because individual adaptations will always be necessary. In this study, the participants also needed psychoeducation about ASD generally and help organise many other aspects of their lives, including housing, employment, social contacts, and leisure activities without the use of drugs in addition to CBT.
The therapists also noted the difficulties patients had in understanding the nature of the therapeutic relationship and their tendency to view the therapist as their personal friend. At the same time, the therapists felt an emotional involvement with their clients and were strongly motivated to help them. They recommend that therapists should have some previous experience of working with people with ASD before delivering SUD therapy to this group; they also highlighted the need for specific support and supervision during therapy. Thus, to enhance the access to adjusted SUD treatment for individuals with ASD, this study indicates that therapists need specific training and supervision and collaboration with other therapists with similar patients. Development of specialised professional networks and tertiary services may be the ways of providing therapists with sufficient support and education.
Although the responses were variable, participants mostly evaluated the therapy as satisfactory which further suggests that CBT may represent a promising treatment option for individuals with ASD and SUD. The frequency of SUD among individuals with ASD is currently unknown, and although SUD screening is increasingly an integral part of clinical guidelines for many mental health conditions, it is not yet part of routine clinical psychiatric assessment for individuals with ASD.49 It is therefore likely that the comorbidity is significantly underdiagnosed, particularly among higher functioning individuals with ASD who are at a greater risk of using alcohol or illegal substances.16 The participants in this study were all high functioning and this corresponds with previous suggestions that SUD may be more likely to occur in individuals with ASD who are more socially outgoing, or of higher intelligence than those who are more socially withdrawn or of lower ability.16,18
An unusual phenomenon was identified in this study which may be a particular characteristic to be aware of in individuals with ASD and SUD. Thus, both participants who ended their drug use completely did it in their ‘own way’, ie, they stopped their drug use suddenly and did not follow a recommended reduction plan. This may be related to ASD characteristics such as inflexibility and literal comprehension. In addition, most participants thought that they were drug experts and reported that they provided advice to others about doses and combination of drugs. However, as therapists discovered during psychoeducation about drugs, such expertise was much exaggerated.
Limitation
Sample size in this study was very small and the study does not include a control group, so caution is needed when interpreting the results. Further limitations were homogeneity of ethnicity, sex, and intellectual ability; thus, the experiences may not apply to more heterogeneous groups of clients with ASD and SUD. More studies are needed to explore ways of improving access to SUD treatment for individuals with ASD, as well as optimal ways of delivering CBT and SUD treatment to this group.
Conclusions
CBT may represent a promising treatment option for individuals with ASD and SUD. This explorative study suggests that patients’ symptoms can be reduced by providing monthly ASD education and group supervision to therapists in ordinary SUD outpatient clinics. As reported by other researchers, this group of patients need more sessions than other client groups and the therapy has to be direct, individualised, and more extensive. The patients need psychoeducation on ASD generally, together with social training and support to organise several aspects of their lives like housing, employment, social contacts, and leisure activities without the use of drugs. Some patients, too, need more support than can be provided in an outpatient clinic, and this highlights the need for a greater range of SUD services to meet the needs of individuals with ASD. More research is indicated in this field, as well as improved professional training and cooperation between services.
Acknowledgments
The project represents collaboration between the National Advisory Unit on SUD treatment, NevSom – Norwegian Centre of Expertise for Neurodevelopmental disorders and Hypersomnias, and SUD Outpatient Clinics at Oslo University Hospital. The essential contribution made by the therapists and by the patients with ASD and SUD and their families and caregivers is gratefully acknowledged. We appreciate the support and contribution from dedicated professionals and user representatives in the reference group. Thank you to Professor Emeritus Patricia Howlin at Institute of Psychiatry, London, UK, for contributing in a final discussion on the manuscript and help with language.
Appendix
Appendix 1.
Adjustments to traditional CBT.
| The cognitive components have to be adapted to individuals cognitive/language level and language style |
| The therapy has to be individualised |
| More structured and greater use of directive strategies |
| Longer treatment sessions and longer duration of therapy than with other patient groups |
| Increased time spent on emotional education and stress management |
| Use of the individuals’ special interests as a starting point |
| Increased use of visual strategies |
| The use of drawings or cartoons to aid visualisation of concepts/make them more concrete |
| Provision of specific social training |
| Involvement of parents and other caregivers |
| Psychoeducation about ASD generally is often needed |
| Help to organise many other aspects of the patients’ lives, including housing, employment, social contacts, and leisure activities without the use of drugs |
Footnotes
Declaration of conflicting interests:The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding:The author(s) received no financial support for the research, authorship, and/or publication of this article.
Author Contributions: SBH and EAA contributed to the conceptualisation and design of the study. SBH and ARB contributed to the collection and processing of data. SBH and ARB wrote the first and final drafts of the manuscript. EAA critically revised the final manuscript. All authors have made substantial contributions to the conception and design or acquisition of data and have been involved in drafting the manuscript or revised it critically. All authors have approved the final article.
ORCID iD: Sissel Berge Helverschou  https://orcid.org/0000-0003-3710-6733
https://orcid.org/0000-0003-3710-6733
References
- 1. United Nations Office on Drugs and Crime. World Drug Report 2017 (Report No. 20). Vienna, Austria: United Nations Publication; 2017. [Google Scholar]
- 2. Stinson FS, Grant BF, Dawson DA, Ruan WJ, Huang B, Saha T. Comorbidity between DSM-IV alcohol and specific drug use disorders in the United States: results from the National epidemiologic survey on alcohol and related conditions. Drug Alcohol Depend. 2005;80:105–116. [DOI] [PubMed] [Google Scholar]
- 3. Grant BF, Stinson FS, Dawson DA, et al. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psych. 2004;61:807–816. [DOI] [PubMed] [Google Scholar]
- 4. Regier DA, Farmer ME, Rae DS, et al. Comorbidity of mental disorders with alcohol and other drug abuse. Results from the Epidemiologic Catchment Area (ECA) study. JAMA. 1990;264:2511–2518. [PubMed] [Google Scholar]
- 5. Gielen N, Havermans RC, Tekelenburg M, Jansen A. Prevalence of post-traumatic stress disorder among patients with substance use disorder: it is higher than clinicians think it is. Eur J Psychotraumatol. 2012;3:PMC3415609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. van de Glind G, Konstenius M, Koeter MWJ, et al. Variability in the prevalence of adult ADHD in treatment seeking substance use disorder patients: results from an international multi-centre study exploring DSM-IV and DSM-5 criteria. Drug Alcohol Depend. 2014;134:158–166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. van Emmerik-van Oortmerssen K, van de Glind G, van den Brink W, et al. Prevalence of attention-deficit hyperactivity disorder in substance use disorder patients: a meta-analysis and meta-regression analysis. Drug Alcohol Depend. 2012;122:11–19. [DOI] [PubMed] [Google Scholar]
- 8. Solberg BS, Halmøy A, Engeland A, Igland J, Haavik J, Klungsøyr K. Gender differences in psychiatric comorbidity: a population-based study of 40 000 adults with attention deficit hyperactivity disorder. Acta Psych Scand. 2017;137:176–186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Ramos M, Boada L, Moreno C, Ljlorente C, Romo J, Parellada M. Attitude and risk of substance use in adolescents diagnosed with Asperger syndrome. Drug Alcohol Depend. 2013;133:535–540. [DOI] [PubMed] [Google Scholar]
- 10. Santosh PJ, Mijovic A. Does pervasive developmental disorder protect children and adolescents against drug and alcohol use? Europ J Child and Adoles Psych. 2006;15:183–188. [DOI] [PubMed] [Google Scholar]
- 11. Woodbury-Smith MR, Clare ICH, Holland AJ, Kearns A. High functioning autistic spectrum disorders, offending and other law-breaking: findings from a community sample. J Forensic Psych Psychol. 2006;17:108–120. [Google Scholar]
- 12. World Health Organization. The ICD-10 Classification of Mental and Behavioural Disorders: Clinical Descriptions and Diagnostic Guidelines. Geneva, Switzerland: World Health Organization; 1992. [Google Scholar]
- 13. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Health Disorders, 5th ed. Washington, DC: American Psychiatric Association; 2013. [Google Scholar]
- 14. Brugha TS, McManus S, Bankart J, et al. The epidemiology of autism spectrum disorders in adults in the community in England. Archiv Gen Psych. 2011;68:459–466. [DOI] [PubMed] [Google Scholar]
- 15. Howlin P, Magiati I. Autism spectrum disorder: outcome in adulthood. Neurodevelop Disord. 2017;30:69–76. [DOI] [PubMed] [Google Scholar]
- 16. Rengit AC, McKowen JW, O’Brien J, Howe YJ, McDougle CJ. Brief report: autism spectrum disorder and substance use disorder: a review and case study. J Autism Dev Disord. 2016;46:2514–2519. [DOI] [PubMed] [Google Scholar]
- 17. Arnevik EA, Helverschou SB. Autism spectrum disorder and co-occurring substance use disorder – a systematic review. Subst Abuse. 2016;10:69–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Butwicka A, Långström N, Larsson H, et al. Increased risk for substance use-related problems in autism spectrum disorders: a population-based study. J Autism Develop Disord. 2017;47:80–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Sinzoo B, van den Brinck W, Koeter M, Gorissen van Eenige M, van Wijngaarden-Crers P, van der Gaag RJ. Treatment seeking adults with autism or ADHD and co-morbid substance use disorder: prevalence, risk factors and functional disability. Drug Alcohol Depend. 2009;107:44–50. [DOI] [PubMed] [Google Scholar]
- 20. Kronenberg LM, Goossens PJJ, van Busschah J, van Achterberg T, van den Brinck W. Coping styles in substance use disorders (SUD) patients with and without co-occurring attention deficit / hyperactivity disorders (ADHD) or autism spectrum disorder (ASD). BMC Psychiatry. 2015;15:159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Lalanne L, Weiner L, Trojak B, Berna F, Berschy G. Substance-use disorder in high-functioning autism: clinical and neurocognitive insights from two case reports. BMC Psychiatry. 2015;15:149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Kronenberg LM, Slager-Visscher K, van Achterberg T, van den Brinck W. Everyday life consequences of substance use in adults patients with a substance use disorder (SUD) and co-occurring attention deficit/hyperactivity disorder or autism spectrum disorder (ASD): a patient’s perspective. BMC Psychiatry. 2014;14: 264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Stoddart KP, Bruke L, King R. Asperger Syndrome in Adulthood. A Comprehensive Guide for Clinicians. New York, NY: W.W. Norton & Company; 2012. [Google Scholar]
- 24. Brorson HH, Ajo Arnevik E, Rand-Hendriksen K, Duckert F. Drop-out from addiction treatment: a systematic review of risk factors. Clin Psychol Rev. 2013;33:1010–1024. [DOI] [PubMed] [Google Scholar]
- 25. Kronenberg LM, Goossens PJJ, van Etten DM, van Achterberg T, van den Brinck W. Need for care and life satisfaction in adults with and without attention deficit hyperactivity disorder (ADHD) or autism spectrum disorders (ASD). Perspec Psych Care. 2015;51:4–15. [DOI] [PubMed] [Google Scholar]
- 26. Spain D, Sin J, Chalder T, Murphy D, Happé F. Cognitive behaviour therapy for adults with autism spectrum disorders and psychiatric co-morbidity: a review. Res Autism Spect Disord. 2015;9:1151–1162. [Google Scholar]
- 27. Vasa RA, Carroll LM, Nozzolillo AA, et al. A systematic review of treatments for anxiety in youth with autism spectrum disorders. J Autism Dev Disord. 2014;44:3215–3229. [DOI] [PubMed] [Google Scholar]
- 28. Wood JJ, Ehrenreich-May J, Allessandri M, et al. Cognitive behavioural therapy for early adolescents with autism spectrum disorders and clinical anxiety: a radomized, controlled trial. Behav Ther. 2015;46:7–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. White S, Ollendick T, Albano AM, et al. Randomized controlled trial: multimodal anxiety and social skill intervention for adolescents with autism spectrum disorder. J Autism Dev Disord. 2013;43:382–394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Helverschou SB, Utgaard K, Wandaas PC. The challenges of applying and assessing cognitive behavioural therapy for individuals on the autism spectrum in a clinical setting: a case study series. Good Autism Practice. 2013;14:117–127. [Google Scholar]
- 31. Baron-Cohen S, Wheelwright S, Skinner R, Martin J, Clubley E. The autism-spectrum quotient (AQ): evidence from Asperger syndrome/high-functioning autism, males and females, scientists and mathematicians. J Autism Dev Disord. 2001;31:5–17. [DOI] [PubMed] [Google Scholar]
- 32. Wechsler D, Nyman H, Nordvik H. WAIS-III: Wechsler Adult Intelligence Scale: Manual. Norsk Versjon (Norwegian Version). Stockholm, Sweden: Psykologiförlaget; 2003. [Google Scholar]
- 33. Ørbeck B, Sundet KS. WASI Norsk Versjon, Manualsupplement (Norwegian Version of WASI). Stockholm, Sweden: Harcourt Assessment; 2007. [Google Scholar]
- 34. Bosnes O. Norsk versjon av (Norwegian version of) Wechsler Abbreviated Scale of Intelligence: Hvor godt er samsvaret mellom WASI og norsk versjon av (How well correlate WASI and Norwegian version of Wechsler Adult Intelligence Scale-III?). J Norweg Psychol Assoc. 2009;46:564–568. [Google Scholar]
- 35. Derogatis LR, Lipman RS, Rickels K, Uhlenhuth EH, Covi L. The Hopkins Symptom Checklist (HSCL): a measure of primary symptom dimensions. In: Pichot P, Olivier-Martin R. eds. Psychological Measurements in Psychopharmacology. Vol 7 Oxford, UK: S. Karger; 1974:79–110. [DOI] [PubMed] [Google Scholar]
- 36. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th ed. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- 37. Berman AH, Palmstierna T, Kallmen H, Bergman H. The self-report Drug Use Disorders Identification Test-Extended (DUDIT-E): reliability, validity, and motivational Index. J Subst Abuse Treat. 2007;32:357–369. [DOI] [PubMed] [Google Scholar]
- 38. Bergman H, Kallmen H. Alcohol use among Swedes and a psychometric evaluation of the Alcohol Use Disorders Identification Test. Alcohol Alcohol. 2002;37:245–251. [DOI] [PubMed] [Google Scholar]
- 39. Durbeej N, Berman AH, Gumpert C, Palmstierna T, Kristiansson M, Alm C. Validation of the Alcohol Use Disorders Identification Test and the Drug Use Disorders Identification Test in a Swedish sample of suspected offenders with signs of mental health problems results from the mental disorder, substance abuse and crime study. J Subst Abuse Treat. 2010;39:364–377. [DOI] [PubMed] [Google Scholar]
- 40. Hildebrand M. The psychometric properties of the Drug Use Identification Test (DUDIT): a review of recent research. J Subst Abuse Treatment. 2015;53:52–59. [DOI] [PubMed] [Google Scholar]
- 41. Endicott J, Spitzer RL, Fleiss JL, Cohen J. The global assessment scale: a procedure for measuring overall severity of psychiatric disturbance. Arch Gen Psychiatry. 1976;33:766–771. [DOI] [PubMed] [Google Scholar]
- 42. Aas IHM. Global Assessment of Functioning (GAF). Properties and frontier of current knowledge. Ann Gen Psychiatry. 2010;9: 20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Forsberg L, Berman AH, Kallmén H, Hermansson U, Helgason AR. A test of the validity of the motivational interviewing treatment integrity code. Cognitive Behav Ther. 2008;37:183–191. [DOI] [PubMed] [Google Scholar]
- 44. Marshall GN, Hays RD. The Patient Satisfaction Questionnaire Short Form (PSQ-18) (Report No. P-7865). Santa Monica, CA: Rand Corporation; 1994. [Google Scholar]
- 45. Wood JJ, Drahota A, Sze K, Har K, Chiu A, Langer DA. Cognitive behavioral therapy for anxiety in children with autism spectrum disorders: a radomized, controlled trial. J Child Psychol Psych. 2009;50:224–234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Helverschou SB, Rasmussen K, Steindal K, Søndanaa E, Nilsson B, Nøttestad JA. Offending profiles of individuals with ASD: a study of all individuals with ASD examined by the expert forensic psychiatric service in Norway between 2000 and 2010. Autism. 2015;19:850–858. [DOI] [PubMed] [Google Scholar]
- 47. Sondenaa E, Helverschou SB, Steindal K, Rasmussen K, Nilson B, Nottestad JA. Violence and sexual offending behavior in people with autism spectrum disorder who have undergone a psychiatric forensic examination. Psychol Rep. 2014;115:32–43. [DOI] [PubMed] [Google Scholar]
- 48. March JS. The future of psychotherapy for mentally ill children and adolescents. J Child Psychol Psych. 2009;50:170–179. [DOI] [PubMed] [Google Scholar]
- 49. Palmquist E, Claeson AS, Neely G, Stenberg B, Nordin S. Overlap in prevalence between various types of environmental intolerance. Int J Hyg Environ Health. 2014;217:427–434. [DOI] [PubMed] [Google Scholar]