Abstract
Background:
It is important to restore horizontal and vertical stability to the acromioclavicular (AC) joint when treating dislocations of this joint. Most surgical stabilization techniques of the AC joint have primarily addressed the coracoclavicular ligament complex; however, these techniques may not satisfactorily restore horizontal stability to the AC joint.
Purpose:
To evaluate the strength and bidirectional stability of 3 AC joint stabilizing techniques in a cadaveric model.
Study Design:
Controlled laboratory study.
Methods:
A total of 24 cadaveric shoulders were randomly allocated to 3 treatment groups. For each group, a standardized AC joint stabilizing procedure was performed, and the specimens were potted for mechanical testing. The following reconstruction techniques were used: a single clavicular tunnel for group A, a double clavicular tunnel for group B, and a double clavicular tunnel plus suture fixation across the AC joint for group C. The specimens underwent cyclic loading in the horizontal and vertical planes and then load to failure. Eight control specimens also underwent cyclic loading in both planes. Construct stiffness during cyclic loading, change in displacement after cyclic loading in both planes, load to failure in the vertical plane, and mode of failure were evaluated, and stiffness was compared among the treatment groups as well as with a control group.
Results:
There was a decrease in joint stiffness for all groups, including controls, during the cyclic loading. Compared with controls, all 3 treatment groups demonstrated equivalent stiffness and displacement in the vertical plane. In the horizontal plane, all 3 treatment groups demonstrated decreased stiffness, increased displacement, or both when compared with controls. When groups were compared, no treatment arm proved superior regarding stiffness or displacement in either plane. Load-to-failure testing of the 3 treatment groups in the vertical plane demonstrated construct strength and stiffness comparable with reports for the native AC joint. The mode of failure was predominantly fracture at the point of fixation to the testing apparatus.
Conclusion:
There was no difference in bidirectional strength and stability between the single– and double–clavicular tunnel techniques of coracoclavicular reconstruction. The addition of a stabilizing suture across the AC joint does not improve horizontal stability in the absence of repair of the AC joint capsule and deltotrapezial fascia.
Clinical Relevance:
This laboratory study provides further evidence of the importance of the AC joint capsule and associated soft tissues in affording horizontal stability to that joint. Information from this and subsequent studies utilizing a bidirectional model can influence the choice of surgical procedure in the clinical treatment of AC joint dislocations.
Keywords: acromioclavicular joint, stabilization, vertical, horizontal, cortical button
Although most acromioclavicular (AC) joint injuries can be managed nonoperatively, there is a subset that benefits from surgical stabilization. A multitude of surgical treatments for AC joint dislocation are described, with the principle behind the operation being to restore the anterior strut of the shoulder girdle. Although the AC joint is a stabilizer, its movements are complex, involving vertical, horizontal, and rotational components.9 The AC joint as well as its capsular ligaments, along with the coracoclavicular (CC) ligament complex, need to be considered. For patients with AC joint dislocations, the AC joint has been variously treated with repair, debridement, or excision.5 The CC ligament complex has been treated with direct repair,2 indirect repair through approximation of the clavicle and coracoid process,3,6,12,14,20 reconstruction of the ligaments,7,8,10,11,17–19 or a combination of these.4,15,16,21 Some procedures combine treatments for both the AC joint and the CC ligaments,1 while others focus on one part or the other.
Biomechanical studies have demonstrated the relative importance of the CC ligament complex to vertical stability of the AC joint, while the AC joint capsule is more important regarding horizontal stability.9 In the acute setting, reducing and stabilizing the AC joint, in combination with approximating the clavicle and coracoid process, allows both ligament complexes to heal and restore joint stability and function. In delayed or chronic cases, reconstruction of the ligaments is likely to be required, whether that be the CC ligaments, the AC joint capsule, or both. The time frame for when an acute injury becomes chronic is not well defined.
For the CC ligament complex, cortical buttons with pulley sutures have gained in popularity owing to their minimally invasive technique. Early iterations were troubled by complications, including button migration, suture breakage, and fracture through drill holes in the coracoid or clavicle. Ideally, these issues have been addressed with design changes in the buttons and sutures and through technique modifications to allow for smaller drill holes into the bones. Additionally, the advent of a 2-tunnel technique allows for anatomic placement of the suture pulleys to replicate the structure of the native CC ligaments.3,14,20
For the AC joint itself, an elegant biomechanical study5 demonstrated decreased horizontal stability, with increasing resection of the distal clavicle, indicating that reduction is preferable to excision regarding stability. Persistent horizontal instability is a recognized complication of AC joint reconstruction surgery. The question of whether anatomic CC ligament reconstruction alone will facilitate horizontal stability is the subject of recent publications.2,13
The purpose of this biomechanical cadaveric study was to evaluate the horizontal and vertical stability of 3 techniques of surgery for AC joint dislocation as compared with the native AC joint. Each construct incorporates increasing complexity, and our hypothesis was that with increasing complexity, vertical and horizontal stability will be improved. In particular, we aimed to compare bidirectional stability in the single–clavicular tunnel technique versus the double–clavicular tunnel technique. Furthermore, we included a group that also underwent direct AC joint stabilization to assess its additional benefit to stability over the CC stabilization alone.
Methods
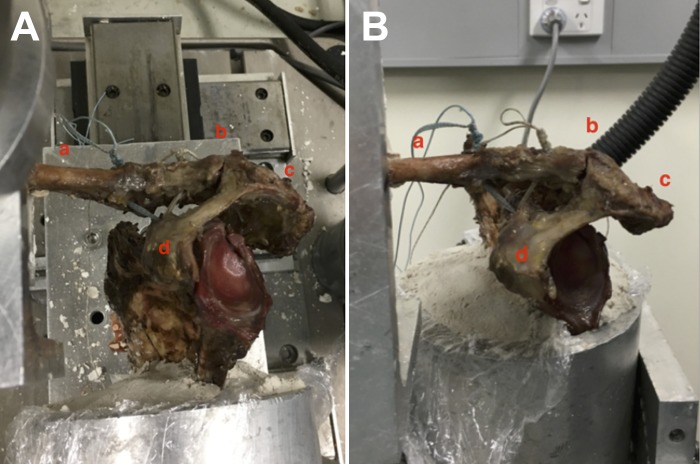
A total of 24 fresh-frozen cadaveric shoulders sourced from the University of Melbourne Department of Anatomy were randomized into 3 treatment groups; 8 shoulders were utilized as controls prior to randomization. Each specimen was dissected free of all soft tissues, leaving the AC joint capsule and the CC ligaments intact. The medial half of the clavicle was then potted with dental cement into a 67-mm aluminum cube mounted on the testing apparatus. Care was taken to ensure that the AC joint was aligned to the sides of the cube to facilitate testing in the horizontal and vertical planes. The inferior half of the scapula was then cemented into a cylindrical aluminum pot mounted onto a platform designed to hinge 90° to facilitate testing in the 2 planes (Figure 1).
Figure 1.
Group B specimen (double clavicular tunnel) potted and mounted for (A) horizontal and (B) vertical testing in the materials testing machine. a, clavicle; b, acromioclavicular joint; c, acromion; d, coracoid.
Treatment Groups
After randomization, each specimen was potted and placed in the anatomic position within the testing apparatus. The AC capsule and the CC ligaments were divided and the assigned surgical reconstruction performed as described here (Figure 2).
Figure 2.
Surgical stabilization techniques for the 3 treatment arms: group A, single clavicular tunnel; group B, double clavicular tunnel; and group C, double clavicular tunnel plus acromioclavicular (AC) suture.
Group A: Single Clavicular Tunnel
The AC joint was manually reduced and held while a 2.4-mm drill bit was passed vertically through the center of the clavicle, 30 mm from the distal end, and through the coracoid at its base. A Nitinol wire was passed through both tunnels in an antegrade fashion, with the loop exiting under the coracoid. A cortical button (Dog-Bone; Arthrex Inc) was preloaded with 2 strands of 2-mm suture tape (FiberTape; Arthrex Inc) and the suture tails shuttled through the bone tunnels in a retrograde fashion with the Nitinol wire. The cortical button was pulled under the coracoid process and positioned to obtain maximal bone contact. The tails of the 2 suture tapes were then threaded through a second cortical button, which was reduced onto the superior surface of the clavicle and positioned for optimal cortical contact. Each suture tape was then tied over the clavicular button with 6 half-hitch throws to fix the reduced AC joint.
Group B: Double Clavicular Tunnel
The AC joint was manually reduced and held while a 2.4-mm drill bit was used to create 2 vertical tunnels in the clavicle: one at 20 mm from the distal end and a second at 45 mm from the distal end. The drill was then used to create a 2.4-mm vertical tunnel through the base of the coracoid process. A cortical button was preloaded with 2 strands of 2-mm suture tape. A Nitinol wire was then passed through the coracoid tunnel to shuttle the 4 suture ends through the coracoid, and the button was positioned under the coracoid with maximal cortical contact. The Nitinol wire was then passed through the more lateral clavicular tunnel, and the tails of 1 strand of suture tape were shuttled through the tunnel. This process was repeated through the medial tunnel for the tails of the second strand of suture tape. The tails of each suture tape were then threaded through separate cortical buttons, and the buttons were reduced onto the clavicle with maximal cortical contact. Each suture tape was then tied over its own button with 6 half-hitch throws to fix the reduced AC joint.
Group C: Double Clavicular Tunnel Plus AC Suture
For this group, all the steps for group B were performed. Additional fixation was then applied across the AC joint itself. A 2.4-mm vertical tunnel was drilled through the acromion midway across its width and in line with the center of the clavicle. A Nitinol loop was passed through this tunnel and into the subacromial space. One of the tails of the lateral suture tape was taken laterally over the AC joint and then passed around the lateral edge of the acromion to the undersurface. This tail was passed through the Nitinol loop and shuttled through to the superior surface of the acromion. The other tail of the lateral suture tape was then drawn laterally over the AC joint and tied to its partner on the superior surface of the acromion with 6 half-hitch throws. This resulted in 2 strands of suture tape bridging the superior aspect of the AC joint at its midpoint, perpendicular to its long axis.
Testing Protocol
To evaluate the stability of the AC joint, each reconstructed joint underwent cyclic loading and load to failure with an Instron materials testing machine (models 3521 and 8874). Cyclic loading included anterior, posterior, and superior translation of the clavicle relative to the acromion, while the load-to-failure testing was completed in the superior plane. For cyclic load testing, a 70-N load was used on all samples over 500 cycles at 1 Hz. These parameters were consistent with other published biomechanical studies on AC joints.1,4,13,20 Horizontal plane (anterior and posterior stability) cyclic testing was undertaken first, followed by vertical plane (superior stability) cyclic testing and finally vertical load-to-failure testing.
For the 8 control specimens, the identical cyclic loading protocol was undertaken in both planes, but load to failure was not examined, as this was previously reported.
The cyclic testing protocol for both planes was identical. Once positioned and secured in the testing machine, the displacement and load of the specimen were recorded when in its native (zero) position. The clavicle was then displaced in one direction until there was a 70-N load applied relative to the zero position. This displacement was recorded, and the same load was then applied in the opposite direction and that displacement recorded. The specimen was then returned to the zero position and loaded cyclically in displacement control at a rate of 1 Hz. The amplitude of the displacement cycle was set according to the predetermined displacement measured in response to the 70-N load.
After the cyclic load testing in the vertical plane was completed, the AC joint was returned to the native position. This was the starting position for the load to failure of the joint. The Instron materials testing machine software (WaveMatrix) was used to steadily increase the displacement at 0.2 mm/s, pulling the clavicle superiorly while the scapula remained fixed to the table.13 The testing machine continuously records the changes in the load and displacement, from which the maximum load and stiffness of the joint can be determined. Failure was defined as a drop in the load required to maintain the change on displacement. Mode of failure for each specimen was documented.
Stiffness was the primary outcome measurement recorded to evaluate joint stability in the vertical and horizontal planes. Force and displacement measurements were taken at baseline, throughout the cyclic testing, and at the conclusion of the loading cycles. During cyclic loading, mean stiffness and maximal load were continuously recorded for statistical analysis. After 500 cycles, a further measurement of displacement for a 70-N load was recorded for each specimen.
During the load-to-failure testing, ultimate tensile strength was measured, with the mode of failure of each construct.
Statistical Analysis
We summarized continuous and discrete variables by means and standard deviations or by medians and interquartile ranges as appropriate. For each plane, stiffness was analyzed with a linear random intercept model. Treatment group and cycle number at 6 time points were treated as categorical variables, and an interaction between treatment group and cycle number was included. Pairwise comparisons were made between predicted marginal means for each group in each plane. The Bonferroni correction was made for multiple comparisons.
Sample size calculation was determined by assuming a difference of 5 mm between groups to be significant, corresponding to a change in stiffness of 4 N/mm. To detect this difference with a power of 80% and an alpha of .05, 8 specimens were required in each group. Displacement after loading was analyzed with simple linear regression. Load to failure was analyzed with the Kruskal-Wallis test. All analyses were performed with Stata (v 14; StataCorp).
Results
Mean Stiffness During Cyclic Loading
In the anterior direction, none of the 3 treatments replicated the mean stiffness of the controls (Table 1 and Figure 3). In the posterior direction, group A and group C replicated the controls but group B did not. On pairwise comparisons, there was no evidence of any difference in construct stiffness among any of the 3 constructs in the anterior or posterior direction (Table 2).
TABLE 1.
Stiffness at Cycle 300a
| Anterior | Posterior | Superior | |
|---|---|---|---|
| Group A | 5.01 ± 1.98 | 7.97 ± 2.71 | 13.51 ± 7.85 |
| Group B | 3.36 ± 1.99 | 6.49 ± 3.86 | 11.80 ± 4.57 |
| Group C | 5.65 ± 8.42 | 9.52 ± 6.18 | 13.36 ± 4.20 |
| Control | 14.17 ± 8.56 | 13.72 ± 4.18 | 12.99 ± 6.80 |
aValues are reported in N/mm as mean ± SD.
Figure 3.

Mean stiffness during cyclic loading for each group.
TABLE 2.
Pairwise Comparisons for Stiffnessa
| Pairwise Comparison | Stiffness | P Valueb |
|---|---|---|
| Anterior | ||
| B vs A | –1.65 (–9.89 to 6.58) | ≥.999 |
| C vs A | 0.63 (–7.60 to 8.86) | ≥.999 |
| Control vs A | 9.15 (0.92 to 17.38) | .02 |
| C vs B | 2.28 (–5.95 to 10.5) | ≥.999 |
| Control vs B | 10.8 (2.57 to 19.03) | .003 |
| Control vs C | 8.52 (0.29 to 16.75) | .04 |
| Posterior | ||
| B vs A | –1.49 (–7.50 to 4.52) | ≥.999 |
| C vs A | 1.55 (–4.45 to 7.56) | ≥.999 |
| Control vs A | 5.75 (–0.25 to 11.75) | .07 |
| C vs B | 3.04 (–2.97 to 9.04) | ≥.999 |
| Control vs B | 7.24 (2.28 to 13.24) | .009 |
| Control vs C | 4.2 (–1.80 to 10.20) | .390 |
| Superior | ||
| B vs A | –1.71 (–9.99 to 6.57) | ≥.999 |
| C vs A | –0.15 (–8.43 to 8.13) | ≥.999 |
| Control vs A | –0.52 (–8.80 to 7.77) | ≥.999 |
| C vs B | 1.56 (–6.72 to 9.85) | ≥.999 |
| Control vs B | 1.2 (–7.09 to 9.48) | ≥.999 |
| Control vs C | –0.37 (–8.65 to 7.92) | ≥.999 |
aData reported in N/mm as mean (95% CI).
bBonferroni correction.
In the superior direction, there was no evidence of difference in stiffness between the controls and 3 treatment groups (Table 1). Pairwise comparisons showed no evidence of any difference in construct stiffness among any of the 3 constructs in the superior direction (Table 2).
All specimens demonstrated a decrease in mean construct stiffness during cyclic loading, and most of this change was seen in the first 100 cycles (Figure 3). In group C, there was 1 specimen that was much stiffer than the others in that group. This had the potential to skew the mean results for that treatment group.
Displacement After Cyclic Loading
For anterior displacement, there was no difference among any of the treatment groups after cyclic loading. When compared with controls in the anterior direction, displacement was greater for treatment group B (P = .04) but not for group A (P = .32) or group C (P = .09) (Table 3). For posterior displacement, there was no difference among any of the treatment groups after cycling loading. When compared with controls in the posterior direction, displacement was greater for treatment group B (P = .008) but not for group A (P = .22) or group C (P = .81). For superior displacement, there was no difference among any of the treatment groups or between the treatment groups and the controls.
TABLE 3.
Displacement After Cyclinga
| Displacement After Cycling | P Valueb | |
|---|---|---|
| Anterior | ||
| Control | 7.33 (4.26 to 10.40) | |
| A | 14.06 (7.56 to 20.57) | |
| B | 17.18 (8.13 to 20.00) | |
| C | 15.97 (11.63 to 20.83) | |
| Pairwise comparison | ||
| A vs control | 6.73 (–2.73 to 16.20) | .32 |
| B vs control | 9.85 (0.39 to 19.32) | .04 |
| C vs control | 8.64 (–0.82 to 18.1) | .09 |
| B vs A | 3.12 (–6.62 to 12.86) | ≥.999 |
| C vs A | 1.91 (–7.83 to 11.65) | ≥.999 |
| C vs B | –1.21 (–10.95 to 8.53) | ≥.999 |
| Posterior | ||
| Control | 5.65 (4.61 to 6.69) | |
| A | 9.05 (7.25 to 10.85) | |
| B | 11.12 (7.89 to 14.34) | |
| C | 8.03 (5.43 to 10.63) | |
| Pairwise comparison | ||
| A vs control | 3.4 (–0.98 to 7.78) | .22 |
| B vs control | 5.46 (1.08 to 9.85) | .008 |
| C vs control | 2.38 (–2.0 to 6.76) | .81 |
| B vs A | 2.07 (–2.44 to 6.57) | ≥.999 |
| C vs A | –1.02 (–5.52 to 3.49) | ≥.999 |
| C vs B | –3.08 (–7.59 to 1.42) | .38 |
| Superior | ||
| Control | 6.85 (4.4 to 9.31) | |
| A | 6.91 (4.26 to 9.56) | |
| B | 6.47 (4.54 to 8.39) | |
| C | 5.95 (4.0 to 7.91) | |
| Pairwise comparison | ||
| A vs control | 0.06 (–4.38 to 4.49) | ≥.999 |
| B vs control | –0.38 (–4.82 to 4.05) | ≥.999 |
| C vs control | –0.9 (–5.33 to 3.53) | ≥.999 |
| B vs A | –0.44 (–5.0 to 4.12) | ≥.999 |
| C vs A | –0.96 (–5.52 to 3.60) | ≥.999 |
| C vs B | –0.52 (–5.08 to 4.04) | ≥.999 |
aData reported in millimeters as mean (95% CI).
bBonferroni correction.
Load to Failure
Loading of the 3 treatment groups to failure revealed no difference in ultimate tensile strength among them (P = .81) (Table 4). The mode of failure for 22 specimens was related to the potting rather than the surgical reconstruction. In 15 specimens, the clavicle fractured at the point of insertion into the cement pot. In a further 7 specimens, the scapula fractured or migrated at the interface with the cement pot. In 2 of the 24 cases, there was pull-through of the Dog-Bone at the coracoid. Both cases of coracoid button migration were in group C.
TABLE 4.
Ultimate Load to Failurea
| Ultimate Load | P Valueb | |
|---|---|---|
| Treatment group | .81 | |
| A | 335.6 (280.7-431.36) | |
| B | 361.8 (302.9-527.6) | |
| C | 387.7 (249.38-456.76) |
aData reported in newtons as median (interquartile range).
bKruskal-Wallis test.
Discussion
This study demonstrated no difference in bidirectional strength and stability between the single– and the double–clavicular tunnel techniques of CC reconstruction. The addition of a stabilizing suture across the AC joint did not improve horizontal stability in the absence of repair of the AC joint capsule and deltotrapezial fascia.
In 2006, Mazzocca and colleagues13 published the first biomechanics study testing stability of the AC joint in the vertical and horizontal directions. Interestingly, this work reported good horizontal stability after surgical reconstruction of the CC ligament complex in isolation. This finding was somewhat surprising, as it contradicted other authors who suggested that horizontal stability is conferred through the AC capsule and ligaments.9 Our intention in undertaking this research was to determine whether we could reproduce those findings. We also chose to include a treatment group with a suture bridging the AC joint in addition to the CC ligament reconstruction to determine what effect this would have on horizontal stability.
We chose to use stiffness as our primary outcome measure, as this had been cited as a possible reason for the bidirectional stability reported by Mazzocca et al.13 Additionally, we included a control group in our study to demonstrate the efficacy of our experimental model and to provide comparative stiffness for the treatment groups. This ensured that we were not overtightening the repairs.
For the treatment groups involving CC ligament reconstruction alone, with a single- or double-tunnel technique, stiffness in the vertical plane closely represented that among the intact controls. In the horizontal plane, however, stiffness was significantly less than that of the controls. When an AC joint suture was added to the double-tunnel technique, no improvement in stiffness was seen in the horizontal or vertical direction. Interestingly, our results demonstrated that the single-tunnel technique required more force per unit displacement than the double-tunnel technique in the horizontal plane. This implies that the single-tunnel technique is equivalent to the double-tunnel technique for vertical stability and better than the double-tunnel technique for horizontal stability but still inferior to the native joint in the horizontal plane. Given our sample size, however, we cannot be definitive about this.
The results of mean displacement after cyclic loading for each group indicate that suture creep or stretch is unlikely to be relevant when tying suture tape over cortical buttons out to 500 cycles. In the horizontal plane, there was increased displacement for all treatment groups when compared with the native joint, except for group C posteriorly. This result may have been skewed by an outlier within group C, with markedly higher stiffness than the rest of the group (Figure 3). Vertical displacement after cyclic loading did not demonstrate any difference, either between groups or as compared with the controls. If suture lengthening, stretch, or creep was a factor, one would expect increased displacement in all directions after cyclic loading.
The stiffness and displacement results indicate that for each construct tested, vertical stability was achieved but not horizontal stability. This is despite 2 treatment groups incorporating an “anatomic” CC ligament reconstruction. We conclude from our study that surgically addressing the CC ligament complex alone does not provide horizontal stability for the disrupted AC joint. We also conclude that an additional, simple suture across the AC suture does not improve horizontal stability. It is our postulate that a more robust intervention directly to the AC joint, in addition to CC stabilization, is required to produce bidirectional stability at the AC joint. We cannot, however, conclude this from our research, as the AC joint capsule and deltotrapezial fascia were completely excised for this study, and so no direct repair of this tissues was attempted.
Regarding load to failure, our study demonstrated similar median superior load to failure for each surgical intervention. This correlates well with reported load to failure for the native AC joint, indicating satisfactory overall construct strength with a single- or double-tunnel technique. There were no fractures related to the drill holes in either bone, but in 2 cases, the coracoid cortical button migrated into the coracoid, leading to failure. This represents a significant decrease in construct-related failures as compared with previous cortical button techniques. It is our opinion that the decrease in bone-related failures is due to a combination of the smaller drill hole required for this technique, as well as the design of the cortical button, spreading the load over a larger surface area.
There are several limitations in the present study. First, this was a laboratory evaluation of the biomechanical strength of the surgical intervention alone. It did not take into account a period of postoperative immobilization after CC ligament repair or reconstruction, which may allow healing of the AC capsule without the need for direct surgical repair. A randomized controlled clinical trial comparing repair of the CC ligament alone and the CC and AC ligaments together would be valuable.
Other limitations include the variability of the cadaveric specimens regarding bone and joint morphology, degenerative joint disease, and bone mineralization. Consequent to this, there was inevitable variability in the potting of specimens directly into the planes of motion of the AC joint.
The stabilization techniques evaluated in this study do not involve biological reconstruction of the CC ligament complex and are therefore appropriate only for the treatment of acute AC joint injuries. The CC stabilization techniques utilized in this study were based on those published by Mazzocca et al,13 with modifications in tunnel diameter and materials used. Also, no distal clavicle excision was undertaken.
Persistent horizontal instability can lead to pain and loss of function, and improved methods of stabilization for the horizontal plane may improve this. It is unknown whether initial stabilization of the AC joint may decrease the incidence or severity of longer-term degenerative changes in that joint.
Conclusion
We can demonstrate no advantage in using a double–clavicular tunnel technique over a single-tunnel technique regarding strength and stability. Neither construct restores stability in the horizontal plane. We recommend that a single–clavicular tunnel technique with a cortical button be combined with restoration of the AC joint capsule and deltotrapezial fascia in the acute surgical treatment of AC joint dislocations to restore vertical and horizontal stability.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: Funding for this study was provided by the Victorian Orthopaedic Research Trust and the Melbourne Orthopaedic Group Research Foundation. Arthrex donated the implants (Dog-Bone cortical buttons), sutures (FiberTape), and surgical equipment (drill bits) used in this study. M.C.E. has received fees for speaking at and organizing educational activities for Arthrex. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from the University of Melbourne Anatomy and Neuroscience Human Ethics Advisory Group (1646969).
References
- 1. Beaver AB, Parks BG, Hinton RY. Biomechanical analysis of distal clavicle excision with acromioclavicular joint reconstruction. Am J Sports Med. 2013;41(7):1684–1688. [DOI] [PubMed] [Google Scholar]
- 2. Beitzel K, Obopilwe E, Apostolakos J, et al. Rotational and translational stability of different methods for direct acromioclavicular ligament repair in anatomic acromioclavicular joint reconstruction. Am J Sports Med. 2014;42(9):2141–2148. [DOI] [PubMed] [Google Scholar]
- 3. Beitzel K, Obopilwe E, Chowaniec DM, et al. Biomechanical comparison of arthroscopic repairs for acromioclavicular joint instability: suture button systems without biological augmentation. Am J Sports Med. 2011;39(10):2218–2225. [DOI] [PubMed] [Google Scholar]
- 4. Beitzel K, Obopilwe E, Chowaniec DM, et al. Biomechanical properties of repairs for dislocated AC joints using suture button systems with integrated tendon augmentation. Knee Surg Sports Traumatol Arthrosc. 2012;20:1931–1938. [DOI] [PubMed] [Google Scholar]
- 5. Beitzel K, Sablan N, Chowaniec DM, et al. Sequential resection of the distal clavicle and its effects on horizontal acromioclavicular joint translation. Am J Sports Med. 2012;40(3):681–685. [DOI] [PubMed] [Google Scholar]
- 6. Chaudhary D, Jain V, Joshi D, Jain JK, Goyal A, Mehta N. Arthroscopic fixation for acute acromioclavicular joint disruption using the TightRope device. J Orthop Surg (Hong Kong). 2015;23(3):309–314. [DOI] [PubMed] [Google Scholar]
- 7. Clevenger T, Vance RE, Bachus KN, Burks RT, Tashjian RZ. Biomechanical comparison of acromioclavicular joint reconstructions using coracoclavicular tendon grafts with and without coracoacromial ligament transfer. Arthroscopy. 2011;27(1):24–30. [DOI] [PubMed] [Google Scholar]
- 8. Costic RS, Labriola JE, Rodosky MW, Debski RE. Biomechanical rationale for development of anatomical reconstructions of coracoclavicular ligaments after complete acromioclavicular joint dislocations. Am J Sports Med. 2004;32(8):1929–1936. [DOI] [PubMed] [Google Scholar]
- 9. Fukuda K, Craig EV, An KN, Cofield RH, Chao EY. Biomechanical study of the ligamentous system of the acromioclavicular joint. J Bone Joint Surg Am. 1986;68(3):434–440. [PubMed] [Google Scholar]
- 10. Garg R, Adamson GJ, Javidan P, Lee TQ. Biomechanical comparison of an intramedullary and extramedullary free-tissue graft reconstruction of the acromioclavicular joint complex. Clin Orthop Surg. 2013;5(4):298–305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Hou Z, Graham J, Zhang Y, et al. Comparison of single and two-tunnel techniques during open treatment of acromioclavicular joint disruption. BMC Surg. 2014;14:53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Lädermann A, Gueorguiev B, Stimec B, Fasel J, Rothstock S, Hoffmeyer P. Acromioclavicular joint reconstruction: a comparative biomechanical study of three techniques. J Shoulder Elbow Surg. 2013;22(2):171–178. [DOI] [PubMed] [Google Scholar]
- 13. Mazzocca AD, Santangelo SA, Johnson ST, Rios CG, Dumonski ML, Arciero RA. A biomechanical evaluation of an anatomical coracoclavicular ligament reconstruction. Am J Sports Med. 2006;34(2):236–246. [DOI] [PubMed] [Google Scholar]
- 14. Nüchtern JV, Sellenschloh K, Bishop N, et al. Biomechanical evaluation of 3 stabilization methods on acromioclavicular joint dislocations. Am J Sports Med. 2013;41(6):1387–1394. [DOI] [PubMed] [Google Scholar]
- 15. Saier T, Venjakob AJ, Minzlaff P, et al. Value of additional acromioclavicular cerclage for horizontal stability in complete acromioclavicular separation: a biomechanical study. Knee Surg Sports Traumatol Arthrosc. 2015;23(5):1498–1505. [DOI] [PubMed] [Google Scholar]
- 16. Schliemann B, Lenschow S, Schürmann P, et al. Biomechanics of a new technique for minimal-invasive coracoclavicular ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2013;21(5):1176–1182. [DOI] [PubMed] [Google Scholar]
- 17. Shu B, Johnston T, Lindsey DP, McAdams TR. Biomechanical evaluation of a novel reverse coracoacromial ligament reconstruction for acromioclavicular joint separation. Am J Sports Med. 2012;40(2):440–446. [DOI] [PubMed] [Google Scholar]
- 18. Tashjian RZ, Southam JD, Clevenger T, Bachus KN. Biomechanical evaluation of graft fixation techniques for acromioclavicular joint reconstructions using coracoclavicular tendon grafts. J Shoulder Elbow Surg. 2012;21(11):1573–1579. [DOI] [PubMed] [Google Scholar]
- 19. Voss A, Beitzel K, Alaee F, et al. A biomechanical analysis of different clavicular tunnel diameters in anatomic acromioclavicular ligament reconstruction. Arthroscopy. 2016;32(8):1551–1557. [DOI] [PubMed] [Google Scholar]
- 20. Walz L, Salzmann GM, Fabbro T, Eichhorn S, Imhoff AB. The anatomic reconstruction of acromioclavicular joint dislocations using 2 TightRope devices: a biomechanical study. Am J Sports Med. 2008;36(12):2398–2406. [DOI] [PubMed] [Google Scholar]
- 21. Wellmann M, Lodde I, Schanz S, Zantop T, Raschke MJ, Petersen W. Biomechanical evaluation of an augmented coracoacromial ligament transfer for acromioclavicular joint instability. Arthroscopy. 2008;24(12):1395–1401. [DOI] [PubMed] [Google Scholar]