Abstract
A modification of range of motion of the knee can significantly change a patient's quality of life. In general, range of motion of 0° to 125° is adequate for most activities of daily life. The rate of knee arthrofibrosis after ligament reconstruction is reported to be between 0% and 4%; after tibial fracture due to high-energy trauma, the rate is about 7%, with an undetermined incidence after limb lengthening. The purpose of this study was to describe a modification of the operative technique of Judet. We describe minimally invasive quadricepsplasty in 4 steps, aiming to obtain an end result with an arc of movement of at least 120° to 130°. We believe that our technique is a good option for the treatment of the stiff knee, having low morbidity and being an easy method to perform.
A modification of range of motion (ROM) of the knee can significantly change a patient's quality of life. In general, ROM of 0° to 125° is adequate for most activities of daily life. Gait analysis has shown that patients require 67° of flexion during the swing phase of gait. A loss of extension of 5° can increase the energy expenditure of the quadriceps muscle and produce a gait alteration.1 The rate of knee arthrofibrosis after ligament reconstruction is reported to be between 0% and 4%2; after tibial fracture due to high-energy trauma, the rate is about 7%,3 with an undetermined incidence after limb lengthening.
Many methods have been used to treat a knee with arthrofibrosis. Bennet first described his method in 1922, followed by Thompson4 (1944) and Judet5 (1959) and their modifications, described by Van Nes6 (1962), Nicoll7 (1963), and Hesketh8 (1963) and, more recently, by Hosalkar et al.9 (2003) and Wang et al.10 (2006). The Thompson quadricepsplasty and Judet quadricepsplasty may be complicated by skin necrosis, loss of full extension, wound dehiscence, and infection associated with large exposures.7, 11, 12 The purpose of this study was to describe a modification of the operative technique of Judet.
Operative Technique
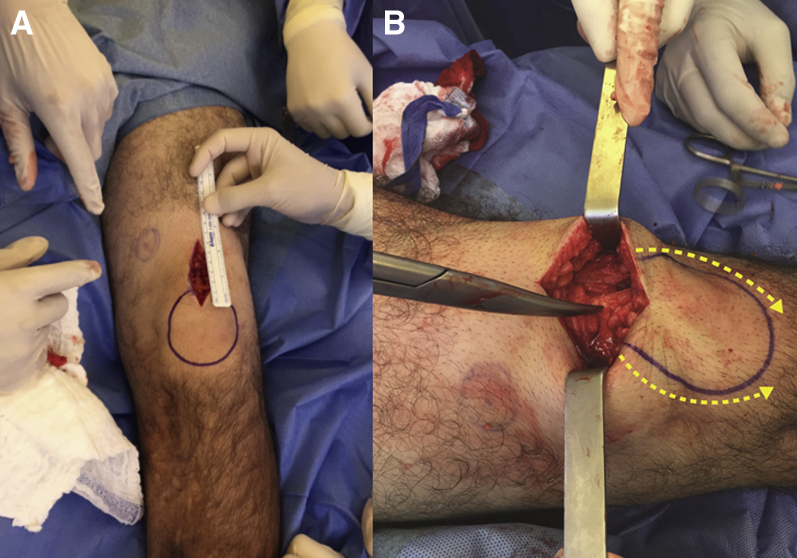
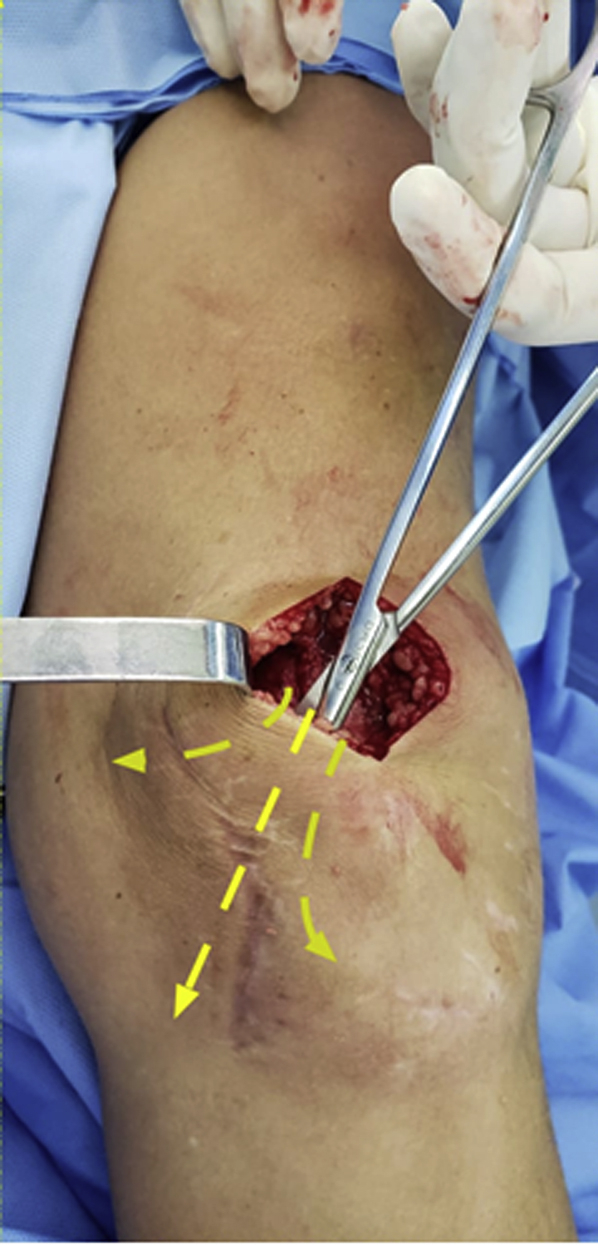
A 6-cm-long median incision is made extending proximally from the superior pole of the patella (Fig 1A), and the rectus femoris is seen generally involved by fibrotic tissue. In the first step, by use of blunt curved dissection scissors, a parapatellar lateral and medial arthrotomy is made by incising the lateral and medial retinaculum, from the top of the patella down the lower pole (Fig 1B).
Fig 1.
(A) The patient is placed in the supine decubitus position, and a 6-cm-long median incision is made extending proximally from the superior pole of the patella. (B) In the first step, by use of a blunt curved dissection scissor, a parapatellar lateral and medial arthrotomy is made by incising the lateral and medial retinaculum (yellow dotted arrows), from the top of the patella down the lower pole (right knee).
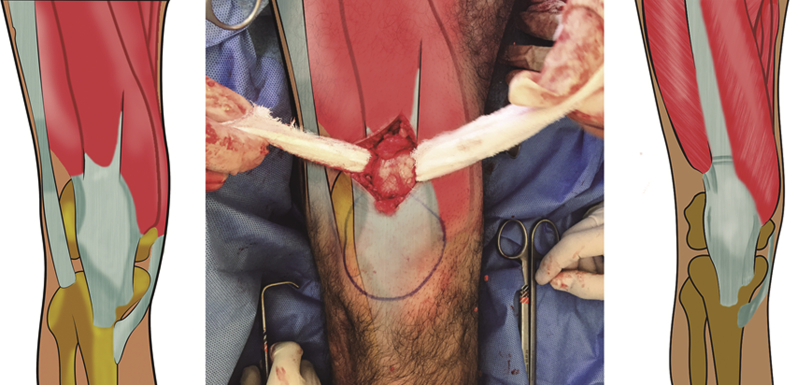
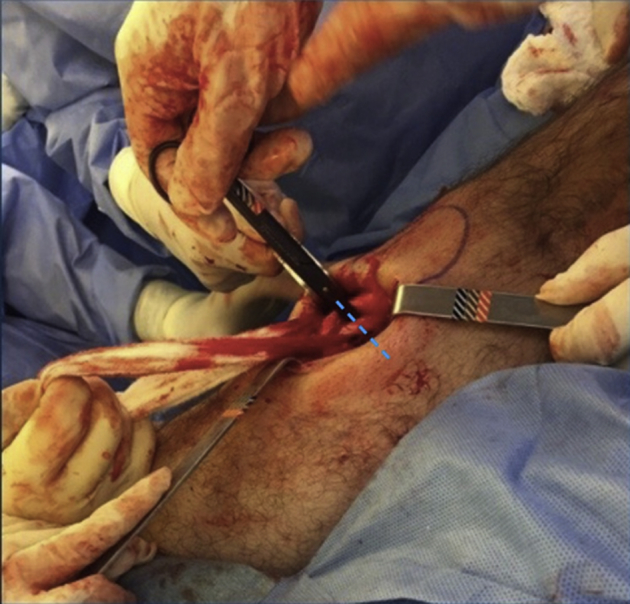
The second step consists of breaking the adhesions within the suprapatellar pouch and patellofemoral compartment, by use of blunt capsule scissors and sometimes a small osteotome. The third step consists of isolating the rectus femoris from the vastus medialis, vastus lateralis, and vastus intermedius (Fig 2). Once the rectus is isolated, the tendon of the vastus intermedius is transected adjacent to its patellar insertion with a scalpel (Fig 3). The fourth step is to release subcutaneous adhesions around the anterior and lateral aspect of the thigh with blunt scissors (Fig 4). Adhesion sites are shown in Figure 5.
Fig 2.
Isolation of rectus femoris in a left knee. Once the rectus is isolated, the vastus intermedius tendon is transected adjacent to its patellar insertion.
Fig 3.
Once the rectus is isolated, the vastus intermedius tendon is transected (blue line) adjacent to its patellar insertion with a scalpel; right knee.
Fig 4.
In the fourth step, subcutaneous adhesions around the anterior and lateral aspect of the thigh are released with a blunt scissor (yellow dotted arrows); left knee.
Fig 5.
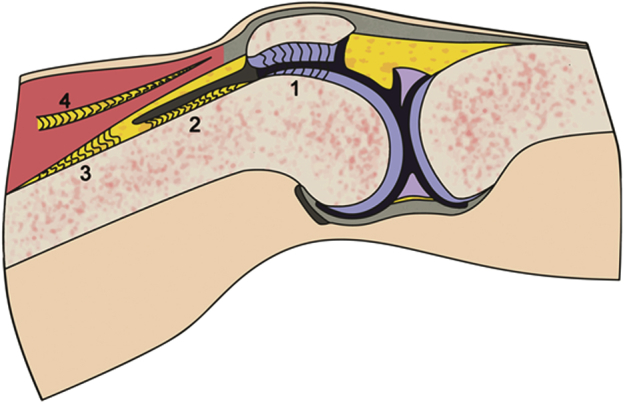
Adhesions on knee: patella (1), suprapatellar pouch and patellofemoral compartment (2), rectus femoris (3), and subcutaneous adhesions (4).
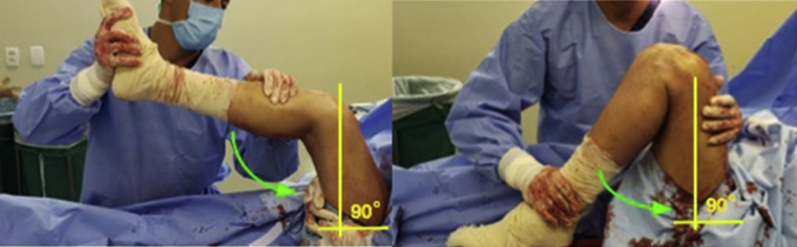
After the aforementioned steps, with the hip in 90° of flexion, gentle manipulation of the knee in flexion is made until maximum flexion is achieved (Fig 6). Our goal is at least 120° to 130°. We recommend that the surgeon place his or her index finger on the patellar tendon during this step so that it is possible to feel any initial ruptures on this tendon. The last step is closure of the skin with heavy nonabsorbable sutures such as Ethibond (Ethicon) (Fig 7), as shown in Video 1.
Fig 6.
With the hip in 90° of flexion, gentle manipulation of the knee in flexion (arrows) is made until maximum flexion is achieved. The surgeon should remember to leave the hip in flexion to avoid complications due to excessive tension on the quadriceps; left knee.
Fig 7.

In the last step, closure of the skin is performed with heavy nonabsorbable sutures such as Ethibond; right knee.
A femoral catheter is left in the operated leg for continuous femoral nerve analgesia (Fig 8). A continuous passive motion machine (model 325; Stryker) is used for 2 days, 24 hours a day, while the patient is supervised by the medical and physiotherapy team.
Fig 8.

A femoral catheter is left in the operated leg, on the same side as the procedure, for continuous femoral nerve analgesia for at least 24 hours; left leg.
The patient must be seen weekly for the first month and taught how to maintain ROM (Fig 6) when physiotherapy is impossible. Pearls and pitfalls associated with our technique are shown in Table 1, and advantages and disadvantages are shown in Table 2.
Table 1.
Pearls and Pitfalls
| Pearls | Pitfalls |
|---|---|
| The surgeon should place the hip at 90° before trying to flex the knee. | Insufficient release of subcutaneous adhesions can occur. |
| Silence is recommended in the OR during knee flexion so that is possible to hear the rupture of the adherences. | Femoropatellar osteophytes might be present. |
| The surgeon should leave his or her finger on the patellar tendon so that it is possible to feel any possible ruptures during flexion of the knee. | Bleeding can disrupt visualization. |
OR, operating room.
Table 2.
Advantages and Disadvantages
| Advantages | Disadvantages |
|---|---|
| Less bleeding than classic techniques | Difficulty releasing proximal adhesions |
| Low chance of fibrosis postoperatively | |
| Low amount of damage to tissues |
Discussion
Judet5 (1959) and Nicoll7 (1963) (Nicoll, 1963) described several components that can limit flexion of the knee, including adhesions from the deep surface of the patella to the femoral condyles, fibrosis and shortening of the lateral expansions of the vastus muscles and their adherence to the femoral condyles, fibrosis of the vastus intermedius, and shortening of the rectus femoris muscle. We have also noticed that deep skin adhesions on the distal portion of the thigh play a relevant role in the pathology.
Khakharia et al.13 reviewed 16 patients treated with limited quadricepsplasty. The mean age was 23 years and mean final flexion was 125°, but they used their technique only in cases resulting from femoral lengthening complications. They had 1 case of extensor lag and did not recommend the procedure for chronic cases.
Wang et al.10 developed a mini-incision operation for the treatment of severe arthrofibrosis. Their study included 22 patients whose mean age was 37 years. The mean flexion gain by the end of the study was 88°. A length of the quadriceps tendon was made in 16 patients, resulting in an extension lag in all 16 cases; this resolved between 3 and 6 months postoperatively in 15 cases but persisted in 1 case.
Hahn et al.14 described modified Thompson quadricepsplasty. The operation was performed in 20 patients with a mean age of 37 years, and the final mean gain in ROM was 67.6°. A Z-plasty of the rectus femoris was performed in 4 cases, resulting in an extension lag in 2.
We believe that our technique is a good option for the treatment of the stiff knee, having low morbidity and being an easy method to learn. In associated with these characteristics, the technique offers a minimally invasive approach to a broad spectrum of indications and is not limited to 1 type of knee stiffness. However, it is important to be alert to the risk of fracture of the patella and rupture of the patellar and quadriceps tendons. We highly recommend that patients follow a physiotherapy regimen after surgery.
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Minimally invasive quadricepsplasty. Rigidity in knee extension may occur after fracture and surgery performed on the lower limbs, leading to significant functional disability in these patients. In this patient, we observed a middle-third fracture of the femur that was extremely consolidated. The knee in question did not show radiologic signs of osteoarthrosis, presenting an arc of movement from 0° to 20°. A median longitudinal incision of 6 cm is made, beginning at the upper pole of the patella. We perform the procedure without limb ischemia. We perform careful hemostasis. We identify the rectus femoris tendon usually encased by fibrous tissue. In the first step, with a blunt curved shear, a lateral arthrotomy is performed with release of the retinaculum, from the upper pole of the patella to the inferior pole. In the second step, we release the adhesions in the suprapatellar bursa and in the patellofemoral compartment. After this step, we perform the same medial sequence. Step 3 consists of isolating the rectus femoris from the vastus medialis and vastus lateralis. Afterward, we identify the limit between the vastus tendon and the rectus femoris, isolating the rectus femoris with a compress. After we ensure the correct identification of the tendons, we section the vastus intermedius tendon adjacent to its patellar insertion, releasing it laterally and medially. In step 4, we perform release of subcutaneous adhesions around the anterior and lateral aspect of the thigh. After all the aforementioned steps, with the hip in 90° of flexion, gentle and gradual manipulation of the knee is performed until we reach the maximum flexion possible, our goal being at least 120° to 130°. The skin is then closed with nonabsorbable sutures such as No. 5 Ethibond.
References
- 1.Magit D., Wolff A., Sutton K., Medvecky M.J. Arthrofibrosis of the knee. J Am Acad Orthop Surg. 2007;15:682–694. doi: 10.5435/00124635-200711000-00007. [DOI] [PubMed] [Google Scholar]
- 2.Shelbourne K.D., Nitz P. Accelerated rehabilitation after anterior cruciate ligament reconstruction. Am J Sports Med. 1990;18:292–299. doi: 10.1177/036354659001800313. [DOI] [PubMed] [Google Scholar]
- 3.Egel K.A., Tejwani N.C., Capla E.L., Wolinsky P.L., Koval K.J. Staged management of high-energy proximal tibial fractures (OTA types 41): The results of a prospective, standardized protocol. J Orthop Trauma. 2005;19:448–455. doi: 10.1097/01.bot.0000171881.11205.80. [DOI] [PubMed] [Google Scholar]
- 4.Thompson T. Quadricepsplasty to improve knee function. J Bone Joint Surg. 1944;26:366–379. [Google Scholar]
- 5.Judet R. Mobilization of the stiff knee. J Bone Joint Surg Br. 1959;41:856–857. [Google Scholar]
- 6.Van Nes C.P. Quadricepsplasty. J Bone Joint Surg Br. 1962;44:954. [Google Scholar]
- 7.Nicoll E.A. Quadricepsplasty. J Bone Joint Surg Br. 1963;45:483–490. [PubMed] [Google Scholar]
- 8.Hesketh K.T. Experience with the Thompson quadricepsplasty. J Bone Joint Surg Br. 1963;45:491–495. [PubMed] [Google Scholar]
- 9.Hosalkar H.S., Jones S., Chowdhury M., Hartley J., Hill R.A. Quadricepsplasty for knee stiffness after femoral lengthening in congenital short femur. J Bone Joint Surg Br. 2003;85:261–264. doi: 10.1302/0301-620x.85b2.13144. [DOI] [PubMed] [Google Scholar]
- 10.Wang J.H., Zhao J.Z., He Y.H. New treatment strategy for severe arthrofibrosis of the knee. A review of twenty two cases. J Bone Joint Surg Am. 2006;88:1245–1250. doi: 10.2106/JBJS.E.00646. [DOI] [PubMed] [Google Scholar]
- 11.Ebraheim N.A., DeTroye R.J., Saddemi S.R. Results of Judet quadricepsplasty. J Orthop Trauma. 1993;7:327–330. doi: 10.1097/00005131-199308000-00007. [DOI] [PubMed] [Google Scholar]
- 12.Moore T.J., Harwin C., Green S.A., Garland D.E., Chandler R.W. The results of quadricepsplasty on knee motion following femoral fractures. J Trauma. 1987;27:49–51. doi: 10.1097/00005373-198701000-00009. [DOI] [PubMed] [Google Scholar]
- 13.Khakharia S., Fragomen A.T., Rozbruch S.R. Limited quadricepsplasty for contracture during femoral lengthening. Clin Orthop Relat Res. 2009;467:2911–2917. doi: 10.1007/s11999-009-0951-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hahn S.B., Lee W.S., Han D.Y. A modified Thompson quadricepsplasty for stiff knee. J Bone Joint Surg Br. 2000;82:992–995. doi: 10.1302/0301-620x.82b7.10590. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Minimally invasive quadricepsplasty. Rigidity in knee extension may occur after fracture and surgery performed on the lower limbs, leading to significant functional disability in these patients. In this patient, we observed a middle-third fracture of the femur that was extremely consolidated. The knee in question did not show radiologic signs of osteoarthrosis, presenting an arc of movement from 0° to 20°. A median longitudinal incision of 6 cm is made, beginning at the upper pole of the patella. We perform the procedure without limb ischemia. We perform careful hemostasis. We identify the rectus femoris tendon usually encased by fibrous tissue. In the first step, with a blunt curved shear, a lateral arthrotomy is performed with release of the retinaculum, from the upper pole of the patella to the inferior pole. In the second step, we release the adhesions in the suprapatellar bursa and in the patellofemoral compartment. After this step, we perform the same medial sequence. Step 3 consists of isolating the rectus femoris from the vastus medialis and vastus lateralis. Afterward, we identify the limit between the vastus tendon and the rectus femoris, isolating the rectus femoris with a compress. After we ensure the correct identification of the tendons, we section the vastus intermedius tendon adjacent to its patellar insertion, releasing it laterally and medially. In step 4, we perform release of subcutaneous adhesions around the anterior and lateral aspect of the thigh. After all the aforementioned steps, with the hip in 90° of flexion, gentle and gradual manipulation of the knee is performed until we reach the maximum flexion possible, our goal being at least 120° to 130°. The skin is then closed with nonabsorbable sutures such as No. 5 Ethibond.