Abstract
Background
The explicit use of theory in research helps expand the knowledge base. Theories and models have been used extensively in HIV‐prevention research and in interventions for preventing sexually transmitted infections (STIs). The health behavior field uses many theories or models of change. However, many educational interventions addressing contraception have no explicit theoretical base.
Objectives
To review randomized controlled trials (RCTs) that tested a theoretical approach to inform contraceptive choice and encourage or improve contraceptive use.
Search methods
To 1 November 2016, we searched for trials that tested a theory‐based intervention for improving contraceptive use in PubMed, CENTRAL, POPLINE, Web of Science, ClinicalTrials.gov, and ICTRP. For the initial review, we wrote to investigators to find other trials.
Selection criteria
Included trials tested a theory‐based intervention for improving contraceptive use. Interventions addressed the use of one or more methods for contraception. The reports provided evidence that the intervention was based on a specific theory or model. The primary outcomes were pregnancy and contraceptive choice or use.
Data collection and analysis
We assessed titles and abstracts identified during the searches. One author extracted and entered the data into Review Manager; a second author verified accuracy. We examined studies for methodological quality.
For unadjusted dichotomous outcomes, we calculated the Mantel‐Haenszel odds ratio (OR) with 95% confidence interval (CI). Cluster randomized trials used various methods of accounting for the clustering, such as multilevel modeling. Most reports did not provide information to calculate the effective sample size. Therefore, we presented the results as reported by the investigators. We did not conduct meta‐analysis due to varied interventions and outcome measures.
Main results
We included 10 new trials for a total of 25. Five were conducted outside the USA. Fifteen randomly assigned individuals and 10 randomized clusters. This section focuses on nine trials with high or moderate quality evidence and an intervention effect. Five based on social cognitive theory addressed preventing adolescent pregnancy and were one to two years long. The comparison was usual care or education. Adolescent mothers with a home‐based curriculum had fewer second births in two years (OR 0.41, 95% CI 0.17 to 1.00). Twelve months after a school‐based curriculum, the intervention group was more likely to report using an effective contraceptive method (adjusted OR 1.76 ± standard error (SE) 0.29) and using condoms during last intercourse (adjusted OR 1.68 ± SE 0.25). In alternative schools, after five months the intervention group reported more condom use during last intercourse (reported adjusted OR 2.12, 95% CI 1.24 to 3.56). After a school‐based risk‐reduction program, at three months the intervention group was less likely to report no condom use at last intercourse (adjusted OR 0.67, 95% CI 0.47 to 0.96). The risk avoidance group (abstinence‐focused) was less likely to do so at 15 months (OR 0.61, 95% CI 0.45 to 0.85). At 24 months after a case management and peer‐leadership program, the intervention group reported more consistent use of hormonal contraceptives (adjusted relative risk (RR) 1.30, 95% CI 1.06 to 1.58), condoms (RR 1.57, 95% CI 1.28 to 1.94), and dual methods (RR 1.36, 95% CI 1.01 to 1.85).
Four of the nine trials used motivational interviewing (MI). In three studies, the comparison group received handouts. The MI group more often reported effective contraception use at nine months (OR 2.04, 95% CI 1.47 to 2.83). In two studies, the MI group was less likely to report using ineffective contraception at three months (OR 0.31, 95% CI 0.12 to 0.77) and four months (OR 0.56, 95% CI 0.31 to 0.98), respectively. In the fourth trial, the MI group was more likely than a group with non‐standard counseling to initiate long‐acting reversible contraception (LARC) by one month (OR 3.99, 95% CI 1.36 to 11.68) and to report using LARC at three months (OR 3.38, 95% CI 1.06 to 10.71).
Authors' conclusions
The overall quality of evidence was moderate. Trials based on social cognitive theory focused on adolescents and provided multiple sessions. Those using motivational interviewing had a wider age range but specific populations. Sites with low resources need effective interventions adapted for their settings and their typical clients. Reports could be clearer about how the theory was used to design and implement the intervention.
Keywords: Adolescent; Adult; Female; Humans; Male; Pregnancy; Health Behavior; Models, Theoretical; Condoms; Condoms/statistics & numerical data; Contraception; Contraception/methods; Contraception/statistics & numerical data; Contraceptive Agents; Contraceptive Agents/administration & dosage; Contraceptive Devices, Female; Contraceptive Devices, Female/statistics & numerical data; HIV Infections; HIV Infections/prevention & control; Motivational Interviewing; Pregnancy in Adolescence; Pregnancy in Adolescence/prevention & control; Randomized Controlled Trials as Topic; Sexually Transmitted Diseases; Sexually Transmitted Diseases/prevention & control; Unsafe Sex
Plain language summary
Improving birth control use with programs based on theory
Background
Theories and models help explain how behavior change occurs. HIV‐prevention research has used theories and models. Programs to prevent sexually transmitted infections (STIs) are often based on behavioral science. The health field has used many theories and models of change. However, programs that address birth control often have no stated theory base.
Methods
We did computer searches for randomized trials until 1 November 2016. Programs included must have tested a theory‐based program for improving birth control use. We excluded trials focused on high‐risk groups and efforts to prevent infections. Programs addressed the use of one or more birth control methods. The reports showed that the theory or model was part of the program design. The main outcomes were pregnancy and birth control use.
Results
We added 10 new trials for a total of 25. Five came from countries other than the USA. This section focuses on nine trials with good quality results and programs that worked. Five had programs based on social cognitive theory (SCT) and four used motivational interviewing (MI). The SCT studies addressed teen pregnancy and lasted one to two years. They included home‐based sessions for adolescent mothers, school‐based programs to prevent pregnancy and HIV, and community‐based case management. Compared to usual services for adolescent mothers, a program group had fewer second births. The other four trials showed more use of effective birth control or use of condoms at last sex among adolescents in school or in the community, The MI studies focused on individuals from a wide age range. Compared to a group with handouts only in three studies, the MI group had more use of effective birth control or less use of ineffective birth control. In another study, the MI group had more women who started using long‐acting birth control than those with usual counseling.
Authors' conclusions
The overall quality of results for our review was moderate. Trials based on SCT focused on teens and provided many sessions. Those using MI had a wider age range but special populations. Sites with low resources need programs than can work in their settings and with their usual clients. Reports could be clearer about how the theory was used to design and conduct the program.
Summary of findings
for the main comparison.
| Behavioral intervention based on social cognitive theory compared with usual care or education for improving contraceptive use | ||||
|
Patient or population: adolescents and women with need for contraception Settings: clinic or home Intervention: behavioral intervention based on social cognitive theory Comparison: usual care or education | ||||
| Outcomes | Relative effect (95% CI) | Participants (studies) | Quality of the evidence (GRADE) | Comments |
| Second birth in 2 years | OR 0.41 (0.17 to 1.00) | Black 2006 | High | Home‐based curriculum (19 sessions) to delay second birth vs usual care; adolescent mothers |
| Consistency of hormonal contraceptive use at: 12 months; 18 months; 24 months |
Reported adjusted RR:
1.46 (1.13 to 1.89); 1.36 (1.02 to 1.83); 1.30 (1.06 to 1.58) |
Sieving 2013 | Moderate | Case management and leadership (18 months) vs usual care; adolescent girls |
| Consistency of condom use at: 12 months; 24 months |
Reported adjusted RR: 1.45 (1.26 to 1.67); 1.57 (1.28 to 1.94) |
|||
| Consistency of dual method use (OCs + condoms) at: 12 months; 24 months |
Reported adjusted RR: 1.58 (1.03 to 2.43); 1.36 (1.01 to 1.85) |
|||
| Use of effective contraceptive method:
at 7 months after baseline (after year 1 sessions); at 19 months after baseline (12 months after year 2 sessions) |
Reported adjusted OR ± SE: 1.62 ± 0.22 (P = 0.03); 1.76 ± 0.29 (P = 0.05) |
Coyle 2001 | Moderate | School‐based curriculum (20 sessions) to prevent pregnancy and HIV/STI vs usual education; grade 9 students |
| Condom use at last sex: at 7 months after baseline; at 19 months after baseline |
Reported adjusted OR ± SE: 1.91 ± 0.27 (P = 0.02); 1.68 ± 0.25 (P = 0.04) |
|||
| Frequency of sex without condom in past 3 months: at 7 months after baseline; at 19 months after baseline |
Reported ratio of adjusted means ± SE: 0.50 ± 0.31 (P = 0.03); 0.63 ± 0.23 (P = 0.05) |
|||
| Condom use at last sex (at 6 months after baseline) | Reported adjusted OR 2.12 (1.24 to 3.56) | Coyle 2006 | Moderate | School‐based curriculum (14 sessions) to prevent pregnancy and HIV/STI vs usual activities; alternative high school students Included Theory of Planned Behavior (+ earlier Theory of Reasoned Action) |
| Less frequent sex without condom in past 3 months (at 6 months after baseline) | Reported adjusted MD −1.09 ± SE 0.36; P = 0.002 | |||
| Risk avoidance group, unprotected sex at last sex: at 3 months; > 15 months |
Reported adjusted OR: 0.70 (0.52 to 0.93); 0.61 (0.45 to 0.85) |
Markham 2012 | Moderate | School‐based curriculum (24 sessions) to prevent pregnancy and HIV/STI (through risk avoidance or risk reduction) vs usual education; grade 7 and 8 students Included Theory of Planned Behavior |
| Risk reduction group, unprotected sex at last sex; sex without condom in past 3 months (at 3 months) |
Reported adjusted OR: 0.67 (0.47 to 0.96); 0.59 (0.36 to 0.95) |
|||
| CI: confidence interval; MD: mean difference; OR: odds ratio; RR: risk ratio; SE: standard error | ||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||
2.
| Motivational interviewing (MI) compared with usual care or handouts for improving contraceptive use | ||||
|
Patient or population: women with need for contraception Settings: clinics primarily Intervention: motivational interviewing Comparison: usual care or handouts | ||||
| Outcomes | Relative effect (95% CI) | Participants (studies) | Quality of the evidence (GRADE) | Comments |
| Less use of ineffective contraception: at 1 month; at 4 months |
OR 0.49 (0.28 to 0.87); OR 0.56 (0.31 to 0.98) |
Ceperich 2011 | Moderate | Prevent alcohol‐exposed pregnancy; 1 MI session vs handout; college women, 18 to 24 years old |
| Use of effective contraception in past 3 months: at 3 months; at 9 months |
OR 2.12 (1.53 to 2.92); OR 2.04 (1.47 to 2.83) |
Floyd 2007 | Moderate | Prevent alcohol‐exposed pregnancy; 5 counseling sessions (4 MI + 1 contraceptive) vs pamphlets; women, 18 to 44 years old, from various settings |
| Less use of ineffective contraception (at 3 months) | OR 0.31 (0.12 to 0.77) | Rendall‐Mkosi 2013 | Moderate | Prevent alcohol‐exposed pregnancy; 5 MI sessions vs handouts; women, 18 to 44 years old, from clinics and farms |
| LARC uptake by 4 weeks; LARC use at 3 months |
OR 3.99 (1.36 to 11.68); OR 3.38 (1.06 to 10.71) |
Whitaker 2016 | Moderate | Prevent pregnancy after abortion; 1 MI session vs usual care only; women, 15 to 29 years old, seeking abortion |
|
CI: confidence interval; MI: motivational interviewing; OR: odds ratio; RR: risk ratio LARC: long‐acting reversible contraceptive | ||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||
Background
Description of the condition
Theories and models are useful in identifying factors that influence health behavior and may be modifiable. The intentional testing of theory in research helps expand the knowledge base (Johnston 2008). Interventions based on theory and behavioral change methods are associated with greater intervention effect (Glanz 2010; Webb 2010). Theories and models have been used extensively in HIV research (Fishbein 2000; Albarracín 2005) and in interventions for reducing risk behaviors or promoting sexual health (Tyson 2014; Bailey 2015). Health education interventions may not have an explicit theoretical premise (Borrelli 2011; Amini 2015). Increasingly though, theories and models are being used in designing and implementing health promotion interventions, as the usefulness of theory becomes more apparent (Bailey 2015).
Description of the intervention
Behavioral theory has been used since the 1950s to explain health behavior and guide interventions (Glanz 2010). Many commonly used theories and models in health behavior are based on a social cognition approach (de Wit 2004; Conner 2005). These include the Health Belief Model, Social Cognitive Theory, the Theory of Reasoned Action along with the later Theory of Planned Behavior, and Protection Motivation Theory. Underlying many of the social cognition models is expectancy‐value theory (de Wit 2004; Conner 2005). While individuals make subjective assessments of probability (expectancy) and value (utility), those assessments are combined in a rational way for decision‐making. Such principles may not be sufficient to explain how individuals make decisions (Conner 2005).
According to the Health Belief Model (HBM), one of the earlier theories in health behavior, individuals will take some action to prevent illness if they believe they are susceptible, if the consequences of the illness are severe, and if the benefits of action outweigh the costs (Janz 2002). Like the HBM, the Theory of Reasoned Action (Ajzen 1980; Terry 1993) and the Theory of Planned Behavior (Montaño 2002) assume a rational approach to engaging in new behaviors. However, they emphasize understanding attitudes toward the new health behavior rather than attitude towards the illness itself. The Theories of Reasoned Action (TRA) and of Planned Behavior (TPB) focus on behavioral intention as the best predictor of the behavior. Rational models may not be the most useful in trying to change behavior related to sexual health (Bailey 2015). The Social Cognitive Theory (SCT) states that current behaviors, thoughts and emotions, and environment all interact to affect new behavior (Bandura 1986; Baranowski 2002). The SCT contributed the construct of self‐efficacy, that is, confidence in one’s ability to undertake a specific behavior. Self‐efficacy has been incorporated into several theories and is sometimes used on its own. Having drawn on several theories, the Transtheoretical Model (TTM) (Prochaska 1992) and the AIDS Risk Reduction Model (Catania 1990) suggest that individuals move through different stages before they can maintain complex health behaviors. These models suggest that tailoring interventions could help individuals move from thinking about a new behavior, to trying it, and eventually to adherence. The Information‐Motivation‐Behavior Skills (IMB) Model placed increased attention of the role of motivation in achieving behavior change (Fisher 1992). The strategy of motivational interviewing (MI) helps individuals identify and verbalize their reasons or motivations for change (Miller 2009). From a theoretical standpoint, MI interventions are client‐centered and use techniques that help clients talk about the changes that they would like to see (Miller 2009). MI techniques were first used during counseling sessions to treat heavy drinking. Over three decades, MI has been applied to a wide range of behaviors, and has been used in combination with other theories such as the TTM. I‐Change, an integrated model for explaining the change process, includes principles and constructs from multiple sources, including the Theory of Planned Behavior, SCT, the TTM, the Health Belief Model, and goal‐setting theories (DeVries 2013).
The published reports of intervention research often provide insufficient information to assess the relevance of the intervention to the problem and the adequacy of implementation (intensity and duration). An effort is underway to extend the Consolidated Standards of Reporting Trials Statement for social and psychological interventions (CONSORT‐SPI) (Montgomery 2013). A tool to assess the fidelity of health behavior interventions was developed for clinical trials (Borrelli 2011). The framework can be useful in reviewing educational interventions. Domains of treatment fidelity include having a curriculum or treatment manual, specifying training of providers, assessing delivery of intervention, and assessing participants' receipt of treatment and ability to use the treatment skills. A Cochrane group developed similar criteria for assessing the integrity of health promotion and public health interventions (Armstrong 2007).
Why it is important to do this review
In this update of our 2013 version, we focus on randomized controlled trials that tested a theory‐based intervention to improve contraceptive use. When we developed the initial review in 2008, theory‐based interventions for contraception had not been systematically examined. One review of interventions to reduce unintended pregnancies among adolescents abstracted the theoretical basis, but not all the strategies addressed specific contraceptive methods (DiCenso 2002). Another discussed the need for learning what types of decision aids for health care work better with certain groups of people, but did not address any theoretical basis (O'Connor 2003). Halpern 2013 studied strategies to improve adherence to hormonal contraceptive regimens. Of trials that tested strategies for communicating contraceptive effectiveness, none had an explicit theoretical base (Lopez 2013). An updated review examined interventions to prevent unintended pregnancies among adolescents (Oringanje 2016). The types of interventions included behavior change programs, but the review did not address theories or models underpinning the programs.
Objectives
To review randomized controlled trials that tested a theoretical approach to inform contraceptive choice and encourage or improve contraceptive use.
Methods
Criteria for considering studies for this review
Types of studies
We included randomized controlled trials (RCTs) that tested an intervention with a theoretical basis for improving contraceptive use for contraception. RCTs were individually randomized or cluster randomized. The use of theories or models had to be explicit, that is, the theory or model had to be named in the report. In addition, the intervention description should have had some evidence of incorporating the theoretical basis, e.g. the constructs used to develop a counseling program.
We excluded trials that focused on preventing sexually transmitted infections (STI) or HIV without also addressing pregnancy prevention. The motivation to prevent disease may differ from that to prevent pregnancy, and consequently the types of theories and models used could also differ. We had included such studies in the initial review but decided to focus on the original intent for the first update.
Types of participants
We included the women in the trials who were users or potential users of the contraceptive methods. We excluded trials that focused on women who are HIV‐positive or high‐risk groups, such as sex workers or women with a known psychiatric or substance abuse disorder.
Types of interventions
The intervention had to address the use of one or more contraceptive methods intended to prevent pregnancy. Any hormonal or non‐hormonal contraceptive could have been the focus, such as oral contraceptives or intrauterine contraception. The theoretical base may have been, but was not limited to, a theory or model of education, communication, or behavior change. The theory‐based intervention could have been compared with a different theory‐based intervention, an intervention without an explicit theoretical base, or usual care. We excluded studies with an intervention focused on abstinence or postponing sexual intercourse for adolescents if they did not include a contraception component.
Types of outcome measures
Primary outcomes
Included trials had to report at least one of the primary outcomes, as the review focuses on affecting contraceptive use.
Pregnancy (test or self‐report)
Contraceptive use, including initiation or change
Adherence to contraceptive regimen
Contraceptive continuation
Because the review included studies assessing contraception initiation or change, we did not have a minimum time frame for outcome assessment. In 2016 we added a minimum of three months after the intervention began for contraceptive adherence and continuation. We still included any time frame for uptake. For pregnancy, we set the minimum time as six months after the intervention began. We also added criteria for high quality evidence, i.e. 6 months for contraceptive use and 12 months for pregnancy. The longer time frames provide more meaningful outcome measures.
Secondary outcomes
Knowledge of contraceptive effectiveness
Attitude about contraception in general or about a specific contraceptive method
In 2016 we added criteria for assessment of these outcomes, i.e. the minimum time frame was three months or more after the baseline. For high quality evidence, we required at least six months.
Search methods for identification of studies
Electronic searches
To 1 November 2016, we searched MEDLINE via PubMed, the Cochrane Central Register of Controlled Trials (CENTRAL), POPLINE, and Web of Science for trials that tested an intervention with a theoretical basis for addressing contraceptive use. We searched for recent clinical trials through ClinicalTrials.gov and the International Clinical Trials Registry Platform (www.who.int/ictrp/en). Appendix 1 shows the most recent search strategies. Appendix 2 has the strategies for previous searches.
Searching other resources
We examined reference lists of relevant articles and reviews for additional trials. For the initial review, we wrote to investigators for information about other published or unpublished trials not discovered in our search.
Data collection and analysis
Selection of studies
We assessed for inclusion all titles and abstracts identified during the literature search with no language limitation. One author reviewed the search results and identified reports for inclusion or exclusion. A second author also examined the reports identified for appropriate categorization. For studies that appeared eligible for this review, we obtained and examined the full‐text articles. We resolved discrepancies by discussion.
Data extraction and management
Two authors conducted the data extraction. One author entered the data into Review Manager 5 (RevMan 2014), and a second author checked accuracy. These data included the study characteristics, risk of bias, and outcomes. The authors resolved discrepancies through discussion.
We extracted the theoretical basis of the experimental intervention which could be derived from, for example, the fields of education, communication, or behavioral change. The use of theory or models had to be explicit; the theory or model had to be named in the report. In addition, the intervention description should have had some evidence of the theoretical basis, for example what principles or constructs were used to develop a counseling session. The identified theoretical basis can be found in Table 3, along with the constructs or principles reportedly used in the intervention design and implementation.
2. Theoretical basis.
| Study | Theory or model | Principles or constructs |
| Social cognitive theory (SCT) | ||
| Black 2006 | Social cognitive theory | Skills, cultural norms, goal‐setting, self‐efficacy, modeling, family support, mentoring relationships |
| Sieving 2013 | Social cognitive theory; resilience paradigm | Environmental (relationships, involvement, norms), personal (expectations), behavioral (skills) |
| Wight 2002 | Social cognitive theory plus health education principles used by teachers | Self‐efficacy, intentions, behavior planning, normative influence, social and communication skills, gender norms, power |
| Coyle 2001 | Social cognitive theory, social influence theory; models of school change | Knowledge, self‐efficacy, communicate, perceived risks and barriers, perceived peer norms; school organization, staff development, school environment, parent education |
| Coyle 2006 | Social cognitive theory; Theory of Reasoned Action; Theory of Planned Behavior (TPB) | Knowledge, attitudes, norms, self‐efficacy, sense of vulnerability, risk, skills |
| Tortolero 2010 | Social cognitive theory, social influence models, and theory of triadic influence | Unclear how used in design other than formative guidance in curriculum development; outcomes assessed relevant concepts Markham 2012, which used this curriculum, was more explicit about theory base |
| Markham 2012 | Social cognitive theory; Theory of Planned Behavior | SCT: personal, environmental, behavioral influences TPB: behavioral and normative beliefs, intentions, behavior Activities to affect behavioral knowledge, self‐efficacy, behavioral and normative beliefs, intentions, environmental factors |
| Raj 2016 | Social cognitive theory; Theory of Gender and Power | Perceive positive outcomes, self‐efficacy, supportive environment; gender power dynamics, social norms, decision making |
| Motivational interviewing (MI) | ||
| Ceperich 2011 | Motivational interviewing | Risk behavior; exercises (decisional balance, development of goal statements and change plans); feedback using "elicit‐provide‐elicit strategy" |
| Floyd 2007 | Motivational interviewing; Transtheoretical model (TTM) | Client‐centered, decisional balance, readiness to change, goal statements and change plans, personalized feedback, problem‐solving, commitment to change |
| Kirby 2010 | Motivational interviewing | Careful and nonjudgmental listening, summarizing, expressing empathy; perceived advantages and disadvantages of behavior change, behavioral expectancies, perceived barriers, reinforcement |
| Petersen 2007 | Motivational interviewing | Empathy, self‐efficacy, perceived barriers, motivation, stage of adopting, improving communication |
| Rendall‐Mkosi 2013 | Motivational interviewing based on Floyd 2007, which also used TTM | Build rapport, assess readiness to change and confidence in ability, develop change plan, implement plan, review counseling experience and progress |
| Whitaker 2016 | Motivational interviewing | Reflective listening; collaborative discussion of benefits and drawbacks of contraceptive methods; avoidance of confrontation |
| Boyer 2005 | Information‐Motivation‐Behavioral Skills Model | Knowledge, attitudes, skills (communication and condom use), risks, decisions |
| Transtheoretical model | ||
| Barnet 2009 | Transtheoretical model; MI; SCT (parenting curriculum from Black 2006) | Stage of change, intentions, behavior; risk, motivation, change |
| Davidson 2015 | Transtheoretical model | Assumed precontemplation or contemplation for LARC Increase awareness, weigh pros and cons, gain self‐efficacy; patient narrative with interview questions according to TTM |
| Gold 2016 | Transtheoretical model; MI | TTM: stages of change, decisional balance, self‐efficacy, processes of change MI as counseling strategy: express empathy, develop discrepancy, roll with resistance, support self‐efficacy; discuss feedback and develop plan |
| Peipert 2008 | Transtheoretical model | Stages of change (contemplation, preparation, action, maintenance); decisional balance, self‐efficacy, change processes |
| Additional theories and models | ||
| Schinke 1981 | Cognitive and behavioral training; problem‐solving schema | Decisions, worth and payoff of options, planning, communicate, coach, feedback, contracting |
| Stanton 2004 | Protection Motivation Theory | Threat appraisal: extrinsic and intrinsic rewards, perceived severity and vulnerability; coping appraisal: self‐efficacy, response efficacy, response cost |
| Berenson 2012 | Health Belief Model | Cues, perceived risk, impact (consequences), benefits of action |
| Gilliam 2014 | Human‐centered design (HCD); Theory of Planned Behavior | HCD: iterative process, rapid low‐fidelity prototyping; stakeholder participation TPB: basis for design unclear; video testimonials, added during testing phase, addressed normative and control beliefs; intended app to raise LARC awareness and interest |
| Taylor 2014 | I‐Change, integrated model | Motivation (affected by predisposing, awareness, information factors), intention (influenced by ability and barriers), behavior |
| Schuler 2015 | C‐Change, social and behavioral change model | Concepts of enabling environment, community organization and services, interpersonal factors, self; issues of information, motivation, ability to act, norms |
MI: motivational interviewing SCT: social cognitive theory TPB: Theory of planned behavior TTM: Transtheoretical model
Intervention fidelity
We used an existing framework to assess the quality of the educational intervention (Borrelli 2011). This framework was developed for assessing treatment fidelity in public health trials of health behavior change. The principles were relevant for this systematic review of behavior change interventions. We examined the trial reports for evidence of intervention (or treatment) fidelity. Domains of treatment fidelity are study design, training of providers, delivery of treatment, receipt of treatment, and enactment of treatment skills. We list the criteria of interest for our review below.
Study design: had a curriculum or treatment manual
Prior training of providers: specified providers' credentials
Project‐specific training: provided standardized training for the intervention
Delivery: assessed providers' adherence to the protocol
Receipt: assessed clients' understanding and skills regarding the intervention (added in 2013)
Information on intervention fidelity came from the primary reports and related design articles (Table 30). For the assessment of evidence quality, we downgraded trials that met fewer than four of the five listed criteria.
1. Intervention fidelity.
| Studya | Curriculum or manual | Provider credentials | Training for intervention | Assessed adherence to protocol | Assessed intervention receipt | Fidelity criteriab |
| Barnet 2009 | Computer‐assisted motivational intervention (CAMI) for study; counseling 20‐min stage‐matched MI; parenting curriculum (Black 2006) | African American paraprofessional women from participants' communities with empathetic qualities, rapport with adolescents, knowledge of community | 2.5 days on Transtheoretical model, motivational interviewing (MI), and CAMI | First 4 months: counselors met biweekly with MI supervisor, who discussed audiotapes, provided feedback |
Not specific: stage‐matched MI |
4 |
| Berenson 2012 | 'Standardization of counseling techniques' (lower literacy handouts, key points, review instructions) | Not specific: Research assistants (RA) | Investigator trained RA in contraceptive counseling | Audio record some sessions for each RA; review for key points | Develop cue for pill‐taking, discuss risks and benefits of pill use, develop plan for side effects, practice condom application | 4 |
| Black 2006 | Curriculum with 19 lessons; order could vary after 2 sessions | 2 Black women, college‐educated, in their 20s, single mothers living independently | Extensive training provided |
Not specific: weekly supervisory sessions |
_ | 4 |
| Boyer 2005 | 4 sessions with educational objectives and strategies; activities and materials | Not specific: research assistants |
Not specific: Trained |
_ | Last session involved describing, practicing, discussing | 2 |
| Ceperich 2011 | Semi‐structured counseling manual with activities and materials | 4 counselors (master's degree in psychology or social work); supervisors experienced in MI training and supervision | Training in motivational interviewing (MI) and counseling manual; reviewed, practiced MI twice per month | Sessions audio‐taped, used in supervision sessions; adjustments made if drifting noted | Sessions involved participant in summarizing, self‐assessment, readiness for change | 5 |
| Coyle 2001 | 20 lessons; grades 9 and 10 (10 lessons each year) | School teachers; in‐class peer leaders for selected activities | Teachers had initial training and ongoing technical support | _ | In‐class peer leaders for some activities, role playing; homework (student‐parent, local resources) | 4 |
| Coyle 2006 | 14‐session curriculum; 9 class lessons and 5 units of service‐learning; pilot‐tested twice | Experienced health educators | Trained to implement; practiced during pilot | _ | Experiential activities, e.g. creating posters, role playing, group discussion, guided skill practice | 4 |
| Davidson 2015 | 3‐segment video for tablet computer | Developers: unspecified for content (presume investigators) + end users; edited by videographers; pilot‐tested | Standard delivery via video | Participants viewed video | _ | 4 |
| Floyd 2007 | Intervention had been tested in feasibility study | 21 counselors (master's level or above) and 6 contraceptive care providers (physicians and family planning nurse practitioners) | _ | Counselors supervised by Project Research team | Participants involved in goals‐setting, change plans, problem solving | 4 |
| Gilliam 2014 | iOS app (15 min) for tablet; designed for project |
Not specific for initial prototype (input from clinicians); tested with women similar to clients; university programmers built iOS prototype |
Standard delivery via app | No information on how women used app | Assessed contraceptive knowledge & LARC interest (post‐intervention; app group only) | 3 |
| Gold 2016 | Computer‐assisted motivational intervention (CAMI); didactic education (DEC) had 3 modules | Developers: unspecified (investigators likely); CAMI counselor not specified; DEC counselor, bachelor's degree layperson |
Standard CAMI delivery; not specified for CAMI counselor |
No information | Participant involved in developing plan for safe behavior; assessed CAMI feasibility and acceptability | 3 |
| Kirby 2010 | Motivational interviewing (MI) guide and training materials | Clinic staff with training on family planning methods, adolescent risk behavior, and counseling | Call content + 3 sessions on MI; observed ≥ 4 calls | Counselors were observed for ≥ 4 calls before conducting solo calls | Interview methods engaged participant in decision‐making | 5 |
| Markham 2012 | 24 sessions (12 per year), 50 min each; based on existing middle school program | Hired for program; most were African American or Hispanic with college degrees; experienced working with adolescents | 5‐day training; skilled trainers modeled lessons, provided teaching practice | Not specific: technical support during implementation | Assessed knowledge and self efficacy about sex and condom use | 4 |
| Peipert 2008 | Computer‐delivered; participants counseled about computer use | Computer‐delivered | Program based on prior system; tested to provide intended feedback | Pre‐tested for delivery of feedback as intended | _ | 4 |
| Petersen 2007 | _ | Experienced health educators trained for this project | 30 to 40 hours | Random observation of sessions and feedback from project manager | Booster session addressed progress and barriers to risk reduction | 4 |
| Raj 2016 | Curriculum 3 sessions with modules | Developers, research team (social science & public health); providers, village health care providers (allopathic or non‐allopathic) | 3 days, FP counseling, gender equity, & partner violence; 2 half‐day boosters | Self‐report only | Review barriers identified, assess discussion of FP with spouse, review FP goals | 4 |
| Rendall‐Mkosi 2013 | Manual developed and used to guide MI sessions: flip chart with alcohol and contraceptive information | Trained lay counselors | _ | Quality control via regular meetings of MI trainer and lay counselor | Participants involved in behavior change plans, implementation, problem solving | 4 |
| Schinke 1981 | 14 group sessions (50 min) for cognitive and behavioral training | Female and male graduate students, 3 to 4 years counseling experience but not with teenagers regarding sex | _ | _ | Sessions involved problem solving, role play, rehearsal | 3 |
| Schuler 2015 | Manual adapted from several sources; 6 sessions with defined activities | APROFAM educators (trained facilitators | Trained to use manual (not specific) | _ | Sessions involved games, role play discussion; study assessed attitudes and knowledge | 4 |
| Sieving 2013 | Case management: monthly core topics each 6 months Peer leadership: training with 15‐session curriculum, group teaching practicum; service learning with standard curriculum |
Case managers (CM) + intervention coordinators: women, aged 22 to 50 years, diverse ethnic and racial backgrounds, bachelor's or master's degree in related field, experience with youth programs |
Not specific for intervention coordinators. CM received training for program and in youth development |
Not specific for intervention coordinators. CM had practice and feedback on strategies, coaching during first group |
CM: adolescent's needs guided specific topics covered | 4 |
| Stanton 2004 | Standard curricula for 3 components, with activities and materials | _ | _ | _ | Involves making decisions, setting goals; includes discussion, homework, role play | 2 |
| Taylor 2014 | 12 weekly lessons with topics and activities; developed with formative research | 2 pairs, young, male and female trained facilitators | _ | _ | Lessons were interactive (role play, discussions, debates, videos) | 3 |
| Tortolero 2010 | 24 lessons (45 min) developed with qualitative work and participatory methods | Trained facilitators | _ | _ | Sessions had computer‐based activities with quizzes, serials with on‐line student feedback, discussion | 3 |
| Whitaker 2016 | Counseling session with 2‐page guide and pictorial guide of FP methods | Counselors (MD‐investigator; licensed social worker) | 2 sessions @ 3 h MI with demonstrations & role play; 5 h encounter & feedback; videotaped; evaluated for competency | Not after training (encounters with professional standardized patients) |
Related to receipt: participant's confidence and readiness to use FP; participant chooses method and helps develop strategy to obtain it; satisfaction with counseling |
4 |
| Wight 2002 | Resource pack of 20 lessons, piloted twice and revised; pilot test had evaluation with teachers and students and lesson observation | Classroom teachers | 5 days | Process evaluation: extent + quality of delivery; who led sessions | Interaction on video with discussion; how to obtain condoms, practice use | 5 |
aIntervention information was assessed with 5 criteria from Borrelli 2011. Those criteria were relevant to completed, rather than ongoing, interventions. bNumber of criteria met by the study, according to information in the reports.
Assessment of risk of bias in included studies
We examined the trials for methodological quality, according to recommended principles (Higgins 2011), and entered the information into the 'Risk of bias' tables. We considered study design, randomization method, allocation concealment, blinding, and losses to follow‐up and early discontinuation. For individually randomized trials, adequate methods for allocation concealment include a centralized telephone system and the use of sequentially numbered, opaque, sealed envelopes (Schulz 2002). In cluster randomized trials, clusters are usually randomized all at once, making allocation concealment less of an issue (Campbell 2012; Higgins 2011). However, selection bias may be introduced when individuals are approached for consent after the cluster has been randomized. We presented limitations in design in Risk of bias in included studies and considered them in interpreting the results.
Measures of treatment effect
Outcomes listed in the Characteristics of included studies address the primary and secondary outcomes for this review. Trials reports may have included other outcomes of interest to the investigators.
For unadjusted dichotomous outcomes, we calculated the Mantel‐Haenszel odds ratio (OR) with 95% confidence interval (CI). This applied to an individually randomized trial or a cluster randomized trial that did not adjust for clustering. An example is the proportion of adolescents who used a condom with the last sexual intercourse. Fixed effect and random‐effects give the same result if no heterogeneity exists, as when a comparison includes only one study. We did not have unadjusted continuous outcomes.
Cluster randomized trials may use a variety of strategies to account for the clustering. When available, we used adjusted measures that the investigators considered the primary effect measures. The adjusted odds ratio (OR) is commonly provided for dichotomous outcomes when analyses are obtained using cluster‐adjusted logit models with or without covariates. If an appropriate adjusted OR was unavailable from the report, we considered other effect measures, for example adjusted risk ratio, adjusted difference in proportions, or regression coefficient (adjusted beta). For continuous outcomes, we used the adjusted mean difference (MD), the adjusted beta, or other measure obtained from cluster‐adjusted linear models. Where the investigators used multivariate models, we did not analyze the treatment effect as that would usually require individual participant data. Rather we presented the results from adjusted models as reported by the investigators.
Unit of analysis issues
We included cluster RCTs for which the analysis appeared to account for the cluster effects. Cluster RCTs used various methods of accounting for the clustering, such as multilevel modeling. We give the specific methods in the results for each trial. Most reports did not provide sufficient information to calculate the effective sample size, so we did not analyze the data in this review. For those studies, we present the results as reported by the investigators. Stanton 2004 reported the intraclass correlation coefficients for each outcome and the number of clusters. We calculated the design effects and then effective sample sizes, according to recommended methods (Higgins 2011).
Dealing with missing data
If reports were missing data needed for analysis, we wrote to the study investigators. Responses and any data provided are shown in Characteristics of included studies. We limited our data requests to studies less than 10 years old. Investigators are unlikely to have access to data for older studies.
We wrote to trial investigators to request missing statistics, such as sample sizes for analysis and actual proportions or means for outcomes presented in figures. However, we limited our requests to studies less than 10 years old, as well as trials that had a report within the past five years. Investigators are unlikely to have access to data from older studies. In some cases, we had obtained information from investigators for earlier work that included the studies. If we could not analyze the data due to missing data, we presented the results as reported by the investigators.
Assessment of heterogeneity
We did not combine data from studies with different interventions. Therefore, we were not able to conduct any meta‐analysis due to the variety of behavioral interventions. Heterogeneity is not an issue when a comparison has a single study.
Data synthesis
To assess the quality of evidence and address confidence in the effect estimates, we applied principles from GRADE (Higgins 2011; GRADE 2013). If meta‐analysis is not viable because of varied interventions or outcome measures, a typical 'Summary of findings' table is not feasible. We provide a 'Summary of findings' table for the main results, although we did not conduct a formal GRADE assessment for all outcomes (GRADE 2013).
We assessed the body of evidence based on the quality of evidence from the included trials. Evidence quality includes the design, implementation, and reporting of the intervention and of the trial. The information on intervention fidelity is part of the overall assessment. We considered RCTs to be high quality and then downgraded the evidence based on the criteria below.
Intervention fidelity information for fewer than four criteria
Inadequate randomization sequence generation or allocation concealment, or no information provided for either one
Follow‐up less than 6 months for contraceptive use or less than 12 months for pregnancy
Loss to follow‐up greater than 20%
In 2016, we added the criterion for follow‐up time and deleted the earlier one for self‐reported outcomes; contraceptive use is generally by self‐report. In addition, we lowered the cutoff for losses from 25% to 20%. We examined the trials that provided evidence of moderate quality and showed an intervention effect.
Results
Description of studies
Results of the search
The 2013 search produced 589 citations: 540 references from the database searches, 5 from other sources, and 44 trials from searches of the clinical trials sites. Three new trials were included along with secondary articles from three previously included trials. We excluded nine studies after reviewing the full text. The remaining references were discarded after reviewing the titles and abstracts or trial summaries.
In 2016, the database searches yielded 445 unduplicated references (Figure 1). Another six items came from other sources, i.e. reference lists or other projects for a new total of 451. We removed 70 references electronically or by hand, leaving 381 unduplicated references. After reviewing the full text of 22 articles, we excluded 8 that did not meet the eligibility criteria (7 primary reports plus 1 secondary article). This total does not include the two trials from a previous version of this review that we excluded in this update. We included 14 items, i.e. 10 primary reports from studies that met the criteria plus 4 secondary references. Searches of clinical trials listing produced 62 unduplicated trials. They were either not eligible or from completed studies we had already considered.
1.
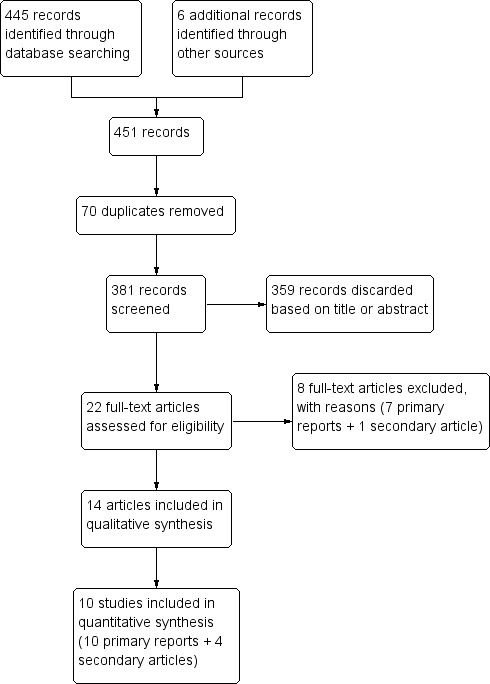
Study flow diagram.
Included studies
In 2016, we included 10 new trials for a total of 25 (Table 3); 15 randomly assigned individuals and 10 assigned groups (cluster randomized trials). Twenty were conducted in the USA; the other locations were Scotland (Wight 2002), Guatemala (Schuler 2015), India (Raj 2016), and South Africa (Rendall‐Mkosi 2013; Taylor 2014). Participants were generally recruited from primary care sites, family planning clinics, community‐based organizations, and schools.
Trial reports were published from 2001 to 2016, except for one from 1981. Sample sizes for the individual‐randomized trials ranged from 36 to 1155. The cluster‐randomized trials ranged from 817 to 9645 individuals, and the number of clusters ranged from 20 to 35. The effective sample sizes would be smaller due to the assignment of groups rather than individuals.
Most studies provided multiple sessions or contacts with participants. Many interventions involved group sessions, including the school‐based programs. Five studies had a single session for individuals (Petersen 2007; Ceperich 2011; Gilliam 2014; Davidson 2015; Whitaker 2016); four of those focused on young women ranging from 15 to 30 years old. Overall, 12 studies targeted adolescents and 7 included both adolescents and young women.
Intervention focus
Twelve trials focused on contraception: delaying second births (Black 2006; Barnet 2009); reducing risk for alcohol‐exposed pregnancy (Floyd 2007; Ceperich 2011; Rendall‐Mkosi 2013); preventing unplanned pregnancy (Schinke 1981; Gilliam 2014; Taylor 2014; Davidson 2015; Schuler 2015; Raj 2016; Whitaker 2016)
Eleven studies addressed preventing HIV or STI as well as pregnancy (Coyle 2001; Wight 2002; Boyer 2005; Coyle 2006; Petersen 2007; Peipert 2008; Kirby 2010; Tortolero 2010; Berenson 2012; Markham 2012; Gold 2016)
Two addressed multiple risks including sexual risk behavior (Stanton 2004; Sieving 2013)
Outcome measures
Eleven trials assessed pregnancy or births. Seven of those had an objective measure: pregnancy test (Boyer 2005; Petersen 2007; Peipert 2008; Raj 2016), observation of a second child (Black 2006), or record review (Barnet 2009; Berenson 2012). The other four trials used self‐reported pregnancy (Stanton 2004; Coyle 2006; Kirby 2010; Taylor 2014). One had self‐reported pregnancy in the original paper (Wight 2002), but a later article provided data from national records on conceptions and abortions by age 20.
The other outcomes assessed included use of non‐condom or hormonal or effective contraceptives, condom use, and dual‐method use.
Excluded studies
In some cases, the full text indicated that assignment was not random. For some cluster randomized trials, the analysis did not appear to account for clustering effects.
Other reasons for exclusions were that the intervention focused on preventing STI or HIV and did not have a contraception component, the target population was a high‐risk group, the intervention had no explicit theoretical or model base, the study did not have a primary outcome for this review, or the report did not provide outcome data for both study arms.
In 2010, we specified the intervention had to have a contraception component, and excluded 14 of the original trials focusing on STI or HIV prevention (Stanton 1996; Boekeloo 1999; Kalichman 1999; Shain 1999; Hoffman 2003; DiClemente 2004; Jemmott 2005; Morrison‐Beedy 2005; Peragallo 2005; DiIorio 2006; Kiene 2006; Villarruel 2006; Jemmott 2007; Roye 2007).
In 2016, we excluded two previously included trials (Ross 2007; Cowan 2010). After closer examination for another review, the intervention in Ross 2007 did not appear to include contraception. The study focused on prevention of STI, although a later cross‐sectional survey included use of modern contraception as an outcome. For Cowan 2010, nearly half the cohort migrated out of the area. The investigators and data and safety monitoring board changed the design to a cross‐sectional survey, which would otherwise not have been eligible.
Risk of bias in included studies
We looked for evidence of intervention fidelity (Table 30), which we included in the assessment of evidence quality (Table 4). Figure 2 illustrates our assessments of risk of bias for the overall review; Figure 3 provides our assessment for each study.
3. Summary of evidence quality.
| Study | Intervention fidelity < 4 items | Randomization and allocation concealment | Follow‐up period | Loss > 20% | Evidence qualitya |
| Social cognitive theory | |||||
| Black 2006 | _ | _ | _ | _ | High |
| Coyle 2001 | _ | _ | _ | −1 | Moderate |
| Coyle 2006 | _ | _ | _ | −1 | Moderate |
| Markham 2012 | _ | _ | _ | −1 | Moderate |
| Raj 2016 | _ | _ | _ | _ | High |
| Sieving 2013 | _ | −1 | _ | _ | Moderate |
| Tortolero 2010 | −1 | _ | _ | _ | Moderate |
| Wight 2002 | _ | _ | _ | −1 | Moderate |
| Motivational interviewing or IMB model | |||||
| Boyer 2005 | −1 | _ | _ | −1 | Low |
| Ceperich 2011 | _ | _ | −1 | _ | Moderate |
| Floyd 2007 | _ | _ | _ | −1 | Moderate |
| Kirby 2010 | _ | _ | _ | −1 | Moderate |
| Petersen 2007 | _ | _ | _ | _ | High |
| Rendall‐Mkosi 2013 | _ | _ | _ | −1 | Moderate |
| Whitaker 2016 | _ | _ | −1 | _ | Moderate |
| Transtheoretical model | |||||
| Barnet 2009 | _ | _ | _ | _ | High |
| Davidson 2015 | _ | _ | −1 | _ | Moderate |
| Gold 2016 | −1 | _ | _ | −1 | Low |
| Peipert 2008 | _ | _ | −1 | −1 | Low |
| Additional theories or models | |||||
| Berenson 2012 | _ | −1 | _ | −1 | Low |
| Gilliam 2014 | −1 | _ | −1 | _ | Low |
| Schinke 1981 | −1 | −1 | _ | _ | Low |
| Schuler 2015 | _ | _ | −1 | −1 | Low |
| Stanton 2004 | −1 | _ | _ | −1 | Low |
| Taylor 2014 | −1 | _ | _ | −1 | Low |
aGrades could be high (RCT), moderate, low, or very low. RCTs downgraded (−1) one level for following: (a) intervention fidelity information for < 4 criteria; (b) randomization sequence generation and allocation concealment: no information on either, or one inadequate; (c) follow‐up < 6 months for contraceptive use or < 12 months for pregnancy; (d) losses > 20%.
2.
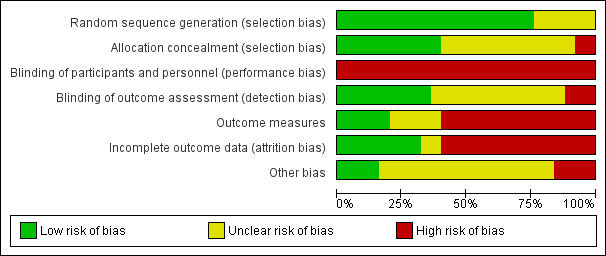
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies
3.
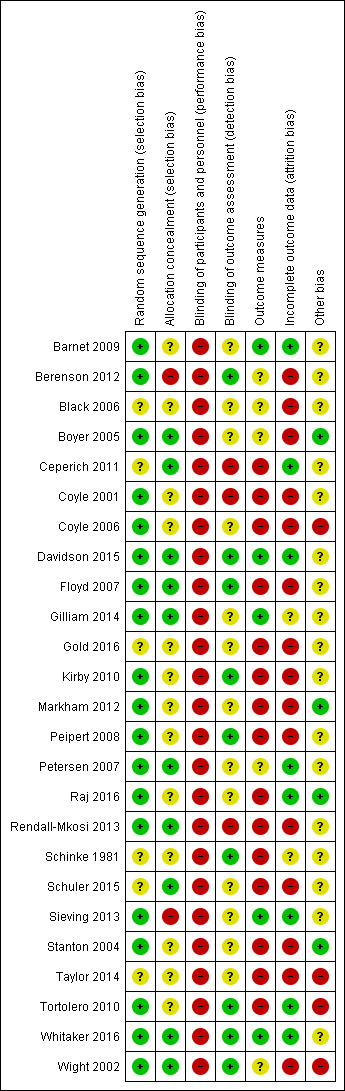
Risk of bias summary: review authors' judgements about each risk of bias item for each included study
Allocation
Of 25 included trials, three provided no information on the randomization sequence generation (Schinke 1981; Ceperich 2011; Schuler 2015). Five trials mentioned stratification (Black 2006; Peipert 2008; Kirby 2010; Taylor 2014; Gold 2016).
Of the 14 individually randomized trials, seven provided some detail on allocation concealment (Floyd 2007; Petersen 2007; Ceperich 2011; Rendall‐Mkosi 2013; Gilliam 2014; Davidson 2015; Whitaker 2016). Peipert 2008 referred to concealment but the information was limited. The investigator for Sieving 2013 communicated that they did not use any allocation concealment.
The cluster randomized trials identified the clusters prior to randomization; individuals meeting the inclusion criteria were eligible. We considered the allocation concealment unclear if the report did not indicate whether the recruiters of individuals or the potential participants were aware of the cluster allocation prior to the consent process.
Blinding
Double‐blinding is often not feasible for participants or providers in educational interventions, but the assessors could be blinded to study arm. Eleven trial reports mentioned using blinding. Counselors and clinicians were unaware of allocation in three trials (Gilliam 2014; Davidson 2015; Whitaker 2016). The assessors or interviewers were masked to the participant's assignment in eight studies (Schinke 1981; Wight 2002; Floyd 2007; Peipert 2008; Kirby 2010; Tortolero 2010; Berenson 2012; Whitaker 2016).
Several trials mentioned no use of blinding (Ceperich 2011; Gold 2016; Raj 2016) or noted the difficulty in blinding field workers (assessors) in a rural community (Rendall‐Mkosi 2013).
Incomplete outcome data
Loss to follow‐up was 20% or more for 13 trials: Wight 2002 (31%); Stanton 2004 (40%); Boyer 2005 (38% to 55%); Coyle 2006 (44%); Floyd 2007 (29%); Peipert 2008 (26%); Kirby 2010 (25%); Berenson 2012 (44%); Markham 2012 (27% to 31%); Rendall‐Mkosi 2013 (23% and 26%); Taylor 2014 (11% and 23%); Schuler 2015 (46%); Gold 2016 (34% and 45%). High losses to follow‐up threaten validity (Strauss 2005).
Differential losses between treatment and control groups did not appear to be a major factor. Most trials had similar losses across treatment arms, and one reported the losses did not differ significantly. However, losses in Taylor 2014 were 11% intervention and 23% control.
Selective reporting
In Black 2006, contraceptive use was presented by second birth rather than by randomized group. The investigators presented combined percentages, but claimed there were no differences by second birth or not. However, mothers who did not have a second infant were slightly more likely to plan to use contraceptive at next intercourse.
Effects of interventions
The results are grouped according to the type of theory or model that guided the experimental intervention (Table 3). While several studies used the same theoretical basis for their experimental interventions, the actual programs differed in structure and emphasis, as noted in the Description of studies.
Social Cognitive Theory (SCT)
Eight trials were based on Social Cognitive Theory (Bandura 1986) or SCT plus another theory or model.
Primarily SCT
Three trials based on Social Cognitive Theory (SCT) or Social Learning Theory (SLT) examined a theory‐based intervention versus usual care (or program). One assigned schools to conditions in Scotland, while two USA trials randomized individuals. The participants were adolescents in all three studies. The interventions provided multiple sessions and lasted 18 months to two years.
A cluster randomized trial used a school‐based curriculum. Wight 2002 was based on SLT and incorporated educational principles familiar to teachers to enhance acceptability. The 7616 participants were 13 to 15 years old and attending state schools in Scotland. The program included active learning and skill development in 20 sessions over two years. The control group received the usual sex education. To assign schools to treatment groups, the investigators selected an allocation from the set of 20,000 possible allocations, which provided the best balance of school‐level measures. To analyze the outcome of unwanted pregnancy, the investigators used a random effects logistics regression. For the other outcomes they used a randomization test, based on all the possible allocations from which they selected the final allocation. The investigators based the analysis of behavioral outcomes at six months on a subsample of those who were sexually experienced, a variable that the intervention could affect. Since they did not include all students in the randomized groups, those comparisons were not randomized comparisons. At six months postprogram (or 24 months from baseline), the intervention and comparison groups did not differ significantly for oral contraceptive (OC) use during last intercourse or self‐reported unwanted pregnancy (Analysis 1.1), first intercourse without condom use or no condom use during most recent intercourse (Analysis 1.2). By linking records from the National Health Service, the investigators examined pregnancies by age 20, approximately 4.5 years after the intervention. The termination data included live births, stillbirths, abortions, and miscarriages. The groups did not differ significantly in conceptions or terminations (Analysis 1.3).
1.1. Analysis.
Comparison 1 Pregnancy prevention curriculum versus usual sex education, Outcome 1 Pregnancy and oral contraceptive use at 6 months postprogram (24 months).
| Pregnancy and oral contraceptive use at 6 months postprogram (24 months) | ||||||
|---|---|---|---|---|---|---|
| Study | Outcome | Gender | N | Intervention Reported % (n) | Control Reported % (n) | Reported adjusted difference (95% CI) |
| Wight 2002 | Unwanted pregnancy (self report) | Young women | 2117 | 4.0% (48) | 3.8% (35) | 1.0 (0.6 to 1.8) |
| Wight 2002 | OC use during last sex | Young men | 876 | 18.7% (79) | 21.2% (96) | ‐2.5 (‐8.0 to 2.9) |
| Wight 2002 | OC use during last sex | Young women | 1269 | 30.4% (196) | 28.0% (175) | 2.4 (‐4.1 to 8.9) |
1.2. Analysis.
Comparison 1 Pregnancy prevention curriculum versus usual sex education, Outcome 2 Condom use at 6 months postprogram (24 months).
| Condom use at 6 months postprogram (24 months) | ||||||
|---|---|---|---|---|---|---|
| Study | Outcome | Gender | N | Intervention Reported % (n) | Control Reported % (n) | Reported adjusted difference (95% CI) |
| Wight 2002 | First‐time sex without condom after 1st program year | Young men | 2323 | 5.2% (57) | 5.7% (70) | ‐0.5 (‐2.5 to 1.5) |
| Wight 2002 | First‐time sex without condom after 1st program year | Young women | 2629 | 9.7% (127) | 9.1% (120) | 0.6 (‐1.9 to 3.1) |
| Wight 2002 | No condom during last sex | Young men | 876 | 33.6% (142) | 34.9% (158) | ‐1.3 (‐5.9 to 3.3) |
| Wight 2002 | No condom during last sex | Young women | 1269 | 44.9% (289) | 44.0% (275) | 0.9 (‐5.7 to 7.4) |
1.3. Analysis.
Comparison 1 Pregnancy prevention curriculum versus usual sex education, Outcome 3 Outcomes by age 20 (women, 4.5 years postprogram).
| Outcomes by age 20 (women, 4.5 years postprogram) | ||||
|---|---|---|---|---|
| Study | Outcome | Intervention rate/1000 | Control rate/1000 | Reported adjusted difference (95% CI) |
| Wight 2002 | Termination events | 126.6 | 112.0 | 15.7 (‐10.7 to 42.1) |
| Wight 2002 | Conception events (live births, stillbirths, therapeutic terminations, miscarriages) | 300.2 | 273.8 | 31.9 (‐16.1 to 79.9) |
| Wight 2002 | Had > 1 termination | 108.9 | 104.3 | 5.6 (‐16.0 to 27.2) |
| Wight 2002 | Had > 1 conception | 222.6 | 216.8 | 9.7 (‐21.8 to 41.2) |
In Black 2006 (N = 181), the intervention group had multiple contacts over two years. The home‐based curriculum for new adolescent mothers included a maximum of 19 lessons. Content included information about access to birth control and condoms provided at each visit. The adolescents in the treatment group were less likely to have had a second birth within two years than the usual care group (OR 0.41, 95% CI 0.17 to 1.00) (Analysis 2.1). Second births were assessed during home visits. Report had results for contraceptive use by second birth and not by randomized group.
2.1. Analysis.
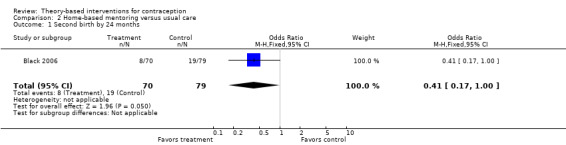
Comparison 2 Home‐based mentoring versus usual care, Outcome 1 Second birth by 24 months.
For Sieving 2013 (N = 253), the 18‐month intervention involved case management as well as a peer‐leadership program for sexually active adolescent girls. Besides SCT, the investigators used a resilience paradigm and principles of social connectedness. They adjusted the analysis for baseline values and intercorrelation among participants recruited from the same clinic using a generalized estimating equation model. Compared with the control group, the intervention group reported greater consistency of use for the outcomes below.
Condoms at 12 and 24 months: reported adjusted relative risk (RR) 1.45 (95% CI 1.26 to 1.67); RR 1.57 (95% CI 1.28 to 1.94) (Analysis 3.1)
Hormonal contraceptives: at 12 months, RR 1.46 (95% CI 1.13 to 1.89); at 18 months, RR 1.36 (95% CI 1.02 to 1.83); at 24 months, RR 1.30 (95% CI 1.06 to 1.58) (Analysis 3.2)
Dual methods (OCs plus condoms): at 12 months, RR 1.58 (95% CI 1.03 to 2.43); at 24 months, RR 1.36 (95% CI 1.01 to 1.85) (Analysis 3.3)
3.1. Analysis.
Comparison 3 Case management + peer leadership versus usual care, Outcome 1 Consistency of condom use.
| Consistency of condom use | ||
|---|---|---|
| Study | Assessment | Reported adjusted relative risk (95% CI) |
| Sieving 2013 | 12 months | 1.45 (1.26 to 1.67) |
| Sieving 2013 | 18 months | 1.10 (0.73 to 1.68) |
| Sieving 2013 | 24 months | 1.57 (1.28 to 1.94) |
3.2. Analysis.
Comparison 3 Case management + peer leadership versus usual care, Outcome 2 Consistency of hormonal contraceptive use.
| Consistency of hormonal contraceptive use | ||
|---|---|---|
| Study | Assessment | Reported adjusted relative risk (95% CI) |
| Sieving 2013 | 12 months | 1.46 (1.13 to 1.89) |
| Sieving 2013 | 18 months | 1.36 (1.02 to 1.83) |
| Sieving 2013 | 24 months | 1.30 (1.06 to 1.58) |
3.3. Analysis.
Comparison 3 Case management + peer leadership versus usual care, Outcome 3 Consistency of dual‐method use.
| Consistency of dual‐method use | ||
|---|---|---|
| Study | Assessment | Reported adjusted relative risk (95% CI) |
| Sieving 2013 | 12 months | 1.58 (1.03 to 2.43) |
| Sieving 2013 | 18 months | 1.08 (0.78 to 1.50) |
| Sieving 2013 | 24 months | 1.36 (1.01 to 1.85) |
At 30 months in Sieving 2013, the intervention group reported more consistent use of condoms (reported adjusted risk ratio (ARR) 1.67, 95% CI 1.39 to 2.00) and dual methods (reported ARR 2.28, 95% CI 1.31 to 3.97) (Analysis 3.4). The groups did not differ significantly for hormonal methods. The study arms did not differ significantly for desire to use contraception at 12, 18, or 24 months (Analysis 3.5).
3.4. Analysis.
Comparison 3 Case management + peer leadership versus usual care, Outcome 4 Months of consistent use in past 7 months (at 30 months).
| Months of consistent use in past 7 months (at 30 months) | |||
|---|---|---|---|
| Study | Method | N | Reported adjusted risk ratio (95% CI) |
| Sieving 2013 | Condoms | 199 | 1.67 (1.39 to 2.00) |
| Sieving 2013 | Hormonal methods | 198 | 1.52 (0.85 to 2.71) |
| Sieving 2013 | Dual methods (hormonal + condoms) | 198 | 2.28 (1.31 to 3.97) |
3.5. Analysis.
Comparison 3 Case management + peer leadership versus usual care, Outcome 5 Attitude: desire to use contraception.
| Attitude: desire to use contraception | ||
|---|---|---|
| Study | Assessment | Reported adjusted OR (95% CI) |
| Sieving 2013 | 12 months | 1.62 (0.81 to 3.27) |
| Sieving 2013 | 18 months | 1.18 (0.96 to 1.46) |
| Sieving 2013 | 24 months | 1.17 (0.77 to 1.77) |
SCT plus another theory or model
The interventions in five trials were based on social cognitive theory plus another theory or model. All randomized clusters rather than individuals. The four school‐based programs for adolescents took place in the USA; one lasted 5 to 7 weeks while the others were provided over two school years. The fifth study took place in India with young couples. The intervention involved three sessions.
The school‐based curriculum in Coyle 2001 incorporated social cognitive theory, social influence theory, and models of school change. The 20 randomized schools had 3869 students who completed baseline surveys. The intervention addressed using condoms and other contraception and included 20 sessions, divided between grades 9 and 10. The program also included school organization activities and parent education. The comparison group received the standard five‐session curriculum and some school activities. The locations were in southeast Texas and northern California (USA). This cluster randomized trial accounted for the cluster effects in the analysis by using multilevel models adjusted for baseline responses for outcomes, geographic area, and unspecified covariates related to the outcome and intervention condition. The investigators conducted assessments immediately after intervention years 1 and 2 as well as 12 months after year 2. The intervention group had more favorable outcomes than the comparison group. Results below are from assessments at 7 and 19 months after baseline (i.e. after year 1 sessions and 12 months after year 2 sessions), unless otherwise specified.
Intervention group versus comparison group
Was more likely to report using an effective method of contraception at last intercourse (condoms, OCs, or both): reported adjusted OR 1.62 ± standard error (SE) 0.22 (P = 0.03); reported adjusted OR 1.76 ± SE 0.29 (P = 0.05) (Analysis 4.1).
Was more likely to report using a condom during last intercourse: reported adjusted OR 1.91 ± SE 0.27 (P = 0.02); reported adjusted OR 1.68 ± SE 0.25 (P = 0.04) (Analysis 4.2).
Was more likely to report a lower frequency of sex without condom use in the past three months: reported ratio of adjusted means 0.50 ± SE 0.31 (P = 0.03); reported ratio of adjusted means 0.63 ± SE 0.23 (P = 0.05) (Analysis 4.2).
Had a higher mean for positive attitudes about condoms 7 months after baseline (reported MD 0.10 ± SE 0.03; P < 0.01) and year 2 (reported MD 0.07; P < 0.01) and 19 months after baseline (reported MD 0.07 ± SE 0.02; P = 0.01) (Analysis 4.3).
4.1. Analysis.
Comparison 4 Curriculum to prevent pregnancy, HIV, and STI versus standard sex education, Outcome 1 Effective protection against pregnancy.
| Effective protection against pregnancy | |||||
|---|---|---|---|---|---|
| Study | Outcome | Assessment | N | Reported adjusted OR ± SE | Reported P |
| Coyle 2001 | Use of effective protection against pregnancy at last sex (condom, OCs, or both) | After 9th‐grade lessons (7 months after baseline) | 998 | 1.62 ± 0.22 | 0.03 |
| Coyle 2001 | _ | After 10th‐grade lessons (19 months after baseline) | _ | 1.40 (no SE reported) | 0.38 |
| Coyle 2001 | _ | 12 months after year 2 (31 months after baseline) | 549 | 1.76 ± 0.29 | 0.05 |
4.2. Analysis.
Comparison 4 Curriculum to prevent pregnancy, HIV, and STI versus standard sex education, Outcome 2 Condom use.
| Condom use | |||||
|---|---|---|---|---|---|
| Study | Outcome | Assessment | N | Reported adjusted effect ± SE | Reported P |
| Coyle 2001 | Condom use at first sex (initiators only) | After 9th‐grade lessons (7 months after baseline) | 285 | OR 0.68 ± 0.48 | 0.42 |
| Coyle 2001 | _ | After 10th‐grade lessons (19 months after baseline) | _ | OR 1.23 (no SE reported) | 0.52 |
| Coyle 2001 | _ | 12 months after year 2 (31 months after baseline) | 733 | OR 1.44 ± 0.27 | 0.17 |
| Coyle 2001 | Condom use at last sex | After 9th‐grade lessons | 1018 | OR 1.91 ± 0.27 | 0.02 |
| Coyle 2001 | _ | After 10th‐grade lessons | _ | OR 1.51 (no SE reported) | 0.26 |
| Coyle 2001 | _ | 12 months after year 2 | 549 | OR 1.68 ± 0.25 | 0.04 |
| Coyle 2001 | Frequency of sex without condom in past 3 months | After 9th‐grade lessons | 963 | Ratio of adjusted means (RM) 0.50 ± 0.31 | 0.03 |
| Coyle 2001 | _ | After 10th‐grade lessons | _ | RM 0.69 (no SE reported) | 0.14 |
| Coyle 2001 | _ | 12 months after year 2 | 1371 | RM 0.63 ± 0.23 | 0.05 |
4.3. Analysis.
Comparison 4 Curriculum to prevent pregnancy, HIV, and STI versus standard sex education, Outcome 3 Attitudes toward condoms.
| Attitudes toward condoms | ||||
|---|---|---|---|---|
| Study | Assessment | N | Reported adjusted MD ± SE | Reported P |
| Coyle 2001 | After 9th‐grade lessons (7 months after baseline) | 3510 | 0.10 ± 0.03 | < 0.01 |
| Coyle 2001 | After 10th‐grade lessons (19 months after baseline) | _ | 0.07 (no SE reported) | < 0.01 |
| Coyle 2001 | 12 months after year 2 (31 months after baseline) | 3751 | 0.07 ± 0.02 | 0.01 |
For Coyle 2006, the school‐based curriculum was based on SCT and the Theory of Planned Behavior, which extended the earlier Theory of Reasoned Action. The program included nine sessions of skill‐based learning plus five service‐learning activities in 24 alternative day schools in northern California (USA). The comparison group received the usual prevention activities for HIV, STI, and pregnancy. The schools served high school students with severe discipline issues, substance use, or chronic absenteeism. This cluster RCT accounted for the cluster effects in the analysis by using multilevel models adjusted for baseline responses on outcomes and unspecified covariates related to the outcome and intervention condition. The study included 988 participants. The investigators based the analysis of behavioral outcomes on a subsample that reported ever having sex, a variable that the intervention could affect. Since they did not include all those randomized, we did not consider the comparisons to be randomized comparisons. The assessments at 6, 12, and 18 months after baseline were conducted about 5, 11, and 17 months postprogram.
The study arms did not differ significantly for self‐reported pregnancy or using an effective method of pregnancy prevention at last sex (Analysis 5.1; Analysis 5.2).
At 5 months but not 11 or 17 months, the intervention group was more likely than the usual‐activity group to report having used a condom during last intercourse (reported adjusted OR 2.12, 95% CI 1.24 to 3.56) (Analysis 5.3) and less frequent sex without a condom in the past three months (reported adjusted MD −1.09 ± SE 0.36; P = 0.002) (Analysis 5.4).
The intervention group had a higher mean for condom knowledge at 5 months (reported MD 0.055 ± SE 0.028; P = 0.05) and at 17 months (reported adjusted MD 0.060 ± 0.030; P = 0.04) (Analysis 5.5).
The two groups did not differ significantly in their attitudes about condoms (Analysis 5.6).
5.1. Analysis.
Comparison 5 Curriculum to prevent HIV, STI, and pregnancy versus usual prevention activities (in alternative schools), Outcome 1 Pregnancy (self report).
| Pregnancy (self report) | ||||
|---|---|---|---|---|
| Study | Assessment (postprogram) | N | Reported adjusted OR (95% CI) | Reported P |
| Coyle 2006 | 5 months | 308 | 0.61 (0.33 to 1.12) | 0.11 |
| Coyle 2006 | 11 months | _ | 1.15 (no CI reported) | 0.66 |
| Coyle 2006 | 17 months | _ | 0.84 (no CI reported) | 0.61 |
5.2. Analysis.
Comparison 5 Curriculum to prevent HIV, STI, and pregnancy versus usual prevention activities (in alternative schools), Outcome 2 Effective pregnancy prevention at last sex.
| Effective pregnancy prevention at last sex | |||
|---|---|---|---|
| Study | Assessment (postprogram) | N | Reported adjusted OR (95% CI) |
| Coyle 2006 | 5 months | 527 | 1.15 (0.78 to 1.70) |
| Coyle 2006 | 11 months | 460 | 1.12 (0.74 to 1.66) |
| Coyle 2006 | 17 months | 417 | 0.77 (0.49 to 1.23) |
5.3. Analysis.
Comparison 5 Curriculum to prevent HIV, STI, and pregnancy versus usual prevention activities (in alternative schools), Outcome 3 Condom use at last sex.
| Condom use at last sex | |||
|---|---|---|---|
| Study | Assessment (postprogram) | N | Reported adjusted OR (95% CI) |
| Coyle 2006 | 5 months | 469 | 2.12 (1.24 to 3.56) |
| Coyle 2006 | 11 months | 386 | 0.88 (0.50 to 1.55) |
| Coyle 2006 | 17 months | 359 | 1.00 (0.49 to 2.02) |
5.4. Analysis.
Comparison 5 Curriculum to prevent HIV, STI, and pregnancy versus usual prevention activities (in alternative schools), Outcome 4 Frequency of sex without condom use in past 3 months.
| Frequency of sex without condom use in past 3 months | ||||
|---|---|---|---|---|
| Study | Assessment (postprogram) | N | Reported adjusted MD ± SE | Reported P |
| Coyle 2006 | 5 months | 412 | ‐1.09 ± 0.36 | 0.002 |
| Coyle 2006 | 11 months | 328 | 0.18 ± 0.34 | 0.6 |
| Coyle 2006 | 17 months | 289 | 0.38 ± 0.39 | 0.33 |
5.5. Analysis.
Comparison 5 Curriculum to prevent HIV, STI, and pregnancy versus usual prevention activities (in alternative schools), Outcome 5 Condom knowledge.
| Condom knowledge | ||||
|---|---|---|---|---|
| Study | Assessment (postprogram) | N | Reported adjusted MD ± SE | Reported P |
| Coyle 2006 | 5 months | 532 | 0.055 ± 0.028 | 0.05 |
| Coyle 2006 | 11 months | 449 | 0.026 ± 0.029 | 0.4 |
| Coyle 2006 | 17 months | 411 | 0.060 ± 0.030 | 0.04 |
5.6. Analysis.
Comparison 5 Curriculum to prevent HIV, STI, and pregnancy versus usual prevention activities (in alternative schools), Outcome 6 General attitudes toward condoms.
| General attitudes toward condoms | ||||
|---|---|---|---|---|
| Study | Assessment (postprogram) | N | Reported adjusted MD ± SE | Reported P |
| Coyle 2006 | 5 months | 527 | 0.086 ± 0.061 | 0.16 |
| Coyle 2006 | 11 months | 451 | 0.035 ± 0.052 | 0.5 |
| Coyle 2006 | 17 months | 413 | ‐0.044 ± 0.066 | 0.5 |
Two USA studies used variations of the same curriculum and provided 24 sessions across grades 7 and 8.
The Tortolero 2010 curriculum was based in SCT, social influence models, and theory of triadic influence (TTI). TTI identifies three levels of influence on behavior: proximal, distal, and ultimate (Flay 2009). The theory integrates concepts and principles from other models to explain and predict the behavior and to identify actions to guide intervention development. The focus in Tortolero 2010 was on delaying sexual behavior, although the intervention addressed a range of contraceptive methods and their relative effectiveness (see Characteristics of included studies). The comparison group had the usual health classes, which varied by school. The study included 1307 participants across the 10 schools randomized. In the analysis, the investigators used multilevel models that included the baseline measures of the dependent variable plus covariates judged to be potential confounders. However, they based the analysis of behavioral outcomes on a subsample that reported ever having sex, so the comparisons were not randomized comparisons. The study groups did not differ significantly in reported condom use at last sex, sex without a condom in the last three months, or sex without effective pregnancy prevention in the last three months (Analysis 6.1). For condom knowledge, the intervention group had a higher reported mean (2.41 ± SD 0.79) than the comparison group (2.25 ± SD 0.95) (reported P ≤ 0.01) (Analysis 6.2). This analysis of knowledge included all those randomized.
Markham 2012 included the risk reduction (RR) intervention from Tortolero 2010, which encouraged abstinence until older, and a comparison group with the usual health classes that varied by school. The study was based in SCT and the Theory of Planned Behavior. An additional third arm for risk avoidance (RA) focused on abstinence until marriage. The intervention addressed a range of contraceptive methods and their relative effectiveness (see Characteristics of included studies). The 15 randomized schools included 1742 participants. The analysis involved generalized linear models with covariates (gender, race or ethnicity, age at baseline, family structure, time between measures, school‐level sexual experience at baseline, and baseline measure for psychosocial outcomes). The estimated standard errors were adjusted for intraclass correlation via random‐effects models. Results are from the 2012 and 2014 reports.
At 3 months and after 15 months postprogram, the risk avoidance group was less likely than the control group to report unprotected vaginal sex at last intercourse (reported adjusted ORs 0.70 (95% CI 0.52 to 0.93) and 0.61 (95% CI 0.45 to 0.85), respectively) (Analysis 7.1). Protected sex included using a condom or abstaining from sex. The RA and control groups did not differ significantly for vaginal sex without a condom in the last three months (Analysis 7.2) or for general condom knowledge (Analysis 7.3).
At three months postprogram, the risk reduction group was less likely than the control group to report unprotected sex at last vaginal intercourse (reported adjusted OR 0.67, 95% CI 0.47 to 0.96) (Analysis 7.1). Also at three months postprogram, the RR group was less likely to report vaginal sex without a condom in the last three months (reported adjusted OR 0.59, 95% CI 0.36 to 0.95) (Analysis 7.2). The RR group had a higher score for general condom knowledge at 3 months and after 15 months postprogram (reported adjusted MD 0.09 and 0.10, respectively; P < 0.01) (Analysis 7.3).
6.1. Analysis.
Comparison 6 HIV, STI, and pregnancy prevention versus usual health classes, Outcome 1 Contraception use.
| Contraception use | ||||
|---|---|---|---|---|
| Study | Outcome | Assessment after baseline | N | Reported adjusted risk ratio (95% CI) |
| Tortolero 2010 | Condom use at last vaginal sex | 24 months (3 months postprogram) | 166 | 1.04 (0.87 to 1.25) |
| Tortolero 2010 | Vaginal sex without condom in last 3 months | 24 months (3 months postprogram) | 166 | 0.92 (0.71 to 1.19) |
| Tortolero 2010 | Vaginal sex without effective pregnancy prevention in last 3 months | 24 months (3 months postprogram) | 162 | 0.83 (0.51 to 1.35) |
6.2. Analysis.
Comparison 6 HIV, STI, and pregnancy prevention versus usual health classes, Outcome 2 Condom knowledge.
| Condom knowledge | ||||||
|---|---|---|---|---|---|---|
| Study | Assessment | N | Intervention Reported mean ± SD | Comparison Reported mean ± SD | Reported difference in adjusted mean | Reported P |
| Tortolero 2010 | 24 months after baseline (3 months postprogram) | 893 | 2.41 ± 0.79 | 2.25 ± 0.95 | 0.16 | < 0.01 |
7.1. Analysis.
Comparison 7 Education for sexual risk avoidance versus risk reduction versus usual health education, Outcome 1 Unprotected sex (no condom) at last vaginal sex.
| Unprotected sex (no condom) at last vaginal sex | ||||
|---|---|---|---|---|
| Study | Comparison | Assessment (postprogram) | N | Reported adjusted OR (95% CI) |
| Markham 2012 | Risk avoidance vs control | 3 months (9th grade) | 843 | 0.70 (0.52 to 0.93) |
| Markham 2012 | _ | > 15 months (10th grade) | 777 | 0.61 (0.45 to 0.85) |
| Markham 2012 | Risk reduction vs control | 3 months (9th grade) | 725 | 0.67 (0.47 to 0.96) |
| Markham 2012 | _ | > 15 months (10th grade) | 677 | 0.71 (0.38 to 1.34) |
7.2. Analysis.
Comparison 7 Education for sexual risk avoidance versus risk reduction versus usual health education, Outcome 2 Vaginal sex without condom in last 3 months.
| Vaginal sex without condom in last 3 months | ||||
|---|---|---|---|---|
| Study | Comparison | Assessment (postprogram) | N | Reported adjusted OR (95% CI) |
| Markham 2012 | Risk avoidance vs control | 3 months (9th grade) | 741 | 0.97 (0.74 to 1.28) |
| Markham 2012 | _ | > 15 months (10th grade) | 638 | 0.66 (0.44 to 1.00) |
| Markham 2012 | Risk reduction vs control | 3 months (9th grade) | 619 | 0.59 (0.36 to 0.95) |
| Markham 2012 | _ | > 15 months (10th grade) | 550 | 0.98 (0.66 to 1.47) |
7.3. Analysis.
Comparison 7 Education for sexual risk avoidance versus risk reduction versus usual health education, Outcome 3 General condom knowledge.
| General condom knowledge | |||||
|---|---|---|---|---|---|
| Study | Comparison | Assessment (postprogram) | N | Reported adjusted MD | Reported P value |
| Markham 2012 | Risk avoidance vs control | 3 months (9th grade) | 894 | 0.00 | NS |
| Markham 2012 | _ | > 15 months (10th grade) | 833 | 0.03 | NS |
| Markham 2012 | Risk reduction vs control | 3 months (9th grade) | 780 | 0.09 | < 0.01 |
| Markham 2012 | _ | > 15 months (10th grade) | 717 | 0.10 | < 0.01 |
The pregnancy prevention intervention of Raj 2016 was based on SCT and the Theory of Gender and Power (TGP). According to TGP, gender‐based power issues are reinforced by social norms. The dynamics are associated with male control over reproductive issues including contraceptive use. The intent was to provide counseling that could lead to gender equity, including a respected male leading the group. Raj 2016 involved 1081 couples from 50 geographic clusters in rural areas of India. Husbands were 18 to 30 years old. Men were the focus for two sessions on family planning and male involvement, and couples were involved in the third session. The comparison group was referred to the government health system for the usual family planning services. At 9 and 18 months, the randomized groups did not differ significantly for use of a modern contraceptive method (Analysis 8.1) nor for pregnancy (Analysis 8.2). Urine tests for pregnancy were done at baseline and 18 months, while 9‐month data came from self‐reports.
8.1. Analysis.
Comparison 8 Family planning and gender equity program versus usual services, Outcome 1 Use of modern contraceptive in past 3 months.
| Use of modern contraceptive in past 3 months | |||
|---|---|---|---|
| Study | Assessment | N | Reported adjusted OR (95% CI) |
| Raj 2016 | 9 months | 898 | 1.57 (0.995 to 2.49) |
| Raj 2016 | 18 months | 891 | 1.58 (0.999 to 2.50) |
8.2. Analysis.
Comparison 8 Family planning and gender equity program versus usual services, Outcome 2 Pregnancy.
| Pregnancy | ||||
|---|---|---|---|---|
| Study | Assessment | N | Reported adjusted OR (95% CI) Self report | Reported adjusted OR (95% CI) Self report or HCG test |
| Raj 2016 | 9 months | 898 | 1.36 (0.92 to 2.00) | _ |
| Raj 2016 | 18 months | 891 | 0.95 (0.62 to 1.47) | 1.03 (0.69 to 1.53) |
IMB model (Information‐Motivation‐Behavioral Skills) or motivational interviewing
IMB model
Boyer 2005 used the IMB model to address preventing STIs and unplanned pregnancy among US Marine recruits. The participants were 2157 women from about 30 platoons (number not specified). This cluster RCT assigned platoons to the treatment and comparison groups. The intervention involved four group sessions on preventing STI and unplanned pregnancy. The comparison group participated in a program of similar format but the content addressed nutrition and physical activity. The investigators accounted for the cluster effects in the analysis; they calculated robust standard errors using the Huber‐White sandwich estimator in regression models assessing intervention effectiveness. The study groups did not differ significantly in unplanned pregnancy (tested) or inconsistent condom use by 14 months (Analysis 9.1).
9.1. Analysis.
Comparison 9 Group risk reduction versus group health promotion, Outcome 1 Outcomes at 14 months.
| Outcomes at 14 months | |||
|---|---|---|---|
| Study | Outcome | Experimental Reported % | Control Reported % |
| Boyer 2005 | Unplanned pregnancy (tested) | 6.7 | 7.3 |
| Boyer 2005 | Inconsistent condom use | 72.8 | 76.5 |
Motivational interviewing
Six studies were based primarily on motivational interviewing (MI). They focused on individuals of varying ages, and the number of sessions ranged from one to five. Two other studies, based on the Transtheoretical model, also incorporated MI into computer‐assisted interventions (Barnet 2009; Gold 2016). The six MI trials here randomized individuals to the intervention and comparison groups. One was conducted in South Africa (Rendall‐Mkosi 2013) and the other five were from the USA.
Three studies addressed reducing risk for alcohol‐exposed pregnancy among women engaged in risky drinking. Two used the same basic program, which involved multiple sessions over two or three months for women of reproductive age (Floyd 2007; Rendall‐Mkosi 2013). One provided a single session for university women (Ceperich 2011).
Floyd 2007 incorporated elements of the Stages of Change from the Transtheoretical model (TTM) into four MI sessions; the intervention also included a contraceptive counseling session. The 840 participants were 18 to 44 years old and from various clinics and treatment centers. The intervention involved five sessions over 14 weeks: four MI sessions on risky drinking and one contraceptive counseling visit. The control group received pamphlets on alcohol use and women's health. The MI group was more likely than the control to have used effective contraception during the three months prior to the follow‐up interviews at three months (OR 2.12, 95% CI 1.53 to 2.92) and nine months (OR 2.04, 95% CI 1.47 to 2.83) (Analysis 10.2).
Ceperich 2011 had a single session lasting about an hour for 224 university students. The control group received a pamphlet on women's health. Women in the MI group were less likely than those in the control group to report using ineffective contraception at one month (OR 0.49, 95% CI 0.28 to 0.87) and at four months (OR 0.56, 95% CI 0.31 to 0.98) (Analysis 10.1).
The focus in Rendall‐Mkosi 2013 was also on reducing risk for alcohol‐exposed pregnancy. The study was conducted in South Africa with 165 participants, 18 to 44 years old. The women were recruited from clinics and from farms within the study area. The intervention was based on that in Floyd 2007 but with contraception integrated into the five MI sessions. Both the intervention and comparison groups received a pamphlet on preventing fetal alcohol syndrome and a handbook on women's health. At three months, the MI group was less likely to use ineffective contraception than the comparison group (OR 0.31, 95% CI 0.12 to 0.77), but the difference was not significant at 12 months (Analysis 11.1).
10.2. Analysis.
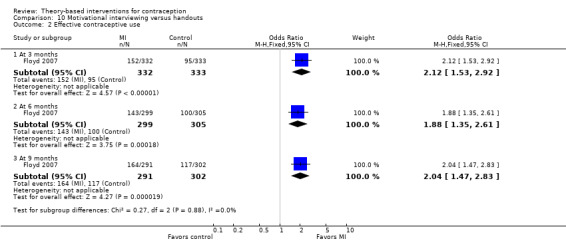
Comparison 10 Motivational interviewing versus handouts, Outcome 2 Effective contraceptive use.
10.1. Analysis.
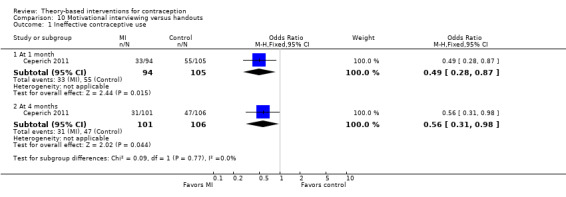
Comparison 10 Motivational interviewing versus handouts, Outcome 1 Ineffective contraceptive use.
11.1. Analysis.
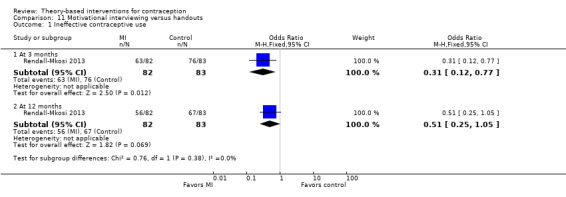
Comparison 11 Motivational interviewing versus handouts, Outcome 1 Ineffective contraceptive use.
Three trials addressed pregnancy prevention, two of which also included STI prevention. They focused on young people (14 to 29 years range) or women 16 to 44 years old. The number of contacts ranged from one in‐person session to nine phone calls over 12 months.
Petersen 2007 addressed preventing pregnancy and STI through an MI session in person and a 'booster' session two months later, in person or by telephone. The 764 women, 16 to 44 years old, were from primary care clinics. The comparison group received brief general counseling on women's health. The primary outcome was improving level of contraceptive use or maintaining a high level of contraceptive use. The groups were not significantly different in contraceptive use at the follow‐up visits at 2, 8, and 12 months (Analysis 12.1). Pregnancy (tested) was not significantly different between the two groups at 12 months (Analysis 12.2).
In Kirby 2010, the focus was also on preventing pregnancy and STI among adolescents. The intervention involved MI during phone calls to improve contraceptive use for young women aged 14 to 18 years (N = 805). After the initial clinic visit, nine calls could be provided in 12 months, monthly for the first six months and then every other month. The comparison group had usual care from the reproductive health clinic, e.g. calls to report abnormal results or respond to patients' inquiries. Only 30% of calls were completed (mean of 2.7 per participant). The regression analyses treated time either continuously or discreetly, and controlled for baseline values and other significant covariates. The intervention and control groups did not differ significantly at 6, 12, or 18 months in the reported percentages for hormonal contraceptive use at last sex (Analysis 13.1), condom use at last sex (Analysis 13.2), or use of hormonal contraceptive or condom at last sex (Analysis 13.3). The investigators provided additional results. Self‐reported pregnancy did not differ significantly for the two groups at study end (Analysis 13.4). Pregnancy rates from clinic charts were much lower than those from self‐report, but participants did not necessarily use the same clinic.
The pilot study of Whitaker 2016 focused on preventing pregnancy after abortion. The 60 participants were 15 to 29 years old and presenting for abortion. Davidson 2015 had a similar focus and target audience but had a different theoretical base. In Whitaker 2016, the one MI session involved seven steps, e.g. developing rapport and assessing readiness to use contraception. Also included was a pictorial guide of contraceptive methods by effectiveness. Both the MI and comparison groups received usual care, i.e. non‐standardized counseling. The primary outcome was use of long‐acting reversible contraception (LARC), i.e. intrauterine contraception or implants. Within four weeks of abortion, uptake of LARC was more likely for the MI group than the comparison group (OR 3.99, 95% CI 1.36 to 11.68) (Analysis 14.1), although the groups did not differ significantly for use of any effective method (Analysis 14.1). Similarly, the MI group was more likely to use LARC at three months (OR 3.38, 95% CI 1.06 to 10.71), but use of any effective method did not differ significantly between the groups (Analysis 14.2). Among those using an effective contraceptive method at three months, the MI and usual care groups did not differ significantly for satisfaction with method (Analysis 14.3).
12.1. Analysis.
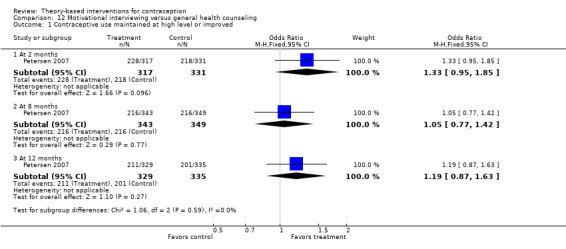
Comparison 12 Motivational interviewing versus general health counseling, Outcome 1 Contraceptive use maintained at high level or improved.
12.2. Analysis.
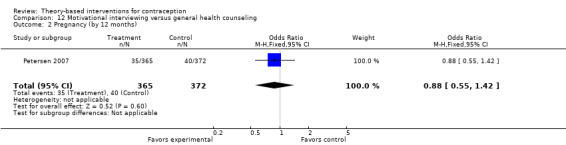
Comparison 12 Motivational interviewing versus general health counseling, Outcome 2 Pregnancy (by 12 months).
13.1. Analysis.
Comparison 13 Motivational phone calls versus usual care, Outcome 1 Hormonal contraceptive use at last sex.
| Hormonal contraceptive use at last sex | ||||
|---|---|---|---|---|
| Study | Assessment | Intervention Reported % | Control Reported % | Reported P |
| Kirby 2010 | 6 months | 44% | 44% | NS |
| Kirby 2010 | 12 months | 43% | 43% | NS |
| Kirby 2010 | 18 months | 43% | 42% | NS |
13.2. Analysis.
Comparison 13 Motivational phone calls versus usual care, Outcome 2 Condom use at last sex.
| Condom use at last sex | ||||
|---|---|---|---|---|
| Study | Assessment | Intervention Reported % | Control Reported % | Reported P |
| Kirby 2010 | 6 months | 53% | 60% | NS |
| Kirby 2010 | 12 months | 55% | 57% | NS |
| Kirby 2010 | 18 months | 58% | 55% | NS |
13.3. Analysis.
Comparison 13 Motivational phone calls versus usual care, Outcome 3 Use of hormonal contraceptive or condom at last sex.
| Use of hormonal contraceptive or condom at last sex | ||||
|---|---|---|---|---|
| Study | Assessment | Intervention Reported % | Control Reported % | Reported P |
| Kirby 2010 | 6 months | 82% | 84% | NS |
| Kirby 2010 | 12 months | 80% | 81% | NS |
| Kirby 2010 | 18 months | 79% | 78% | NS |
13.4. Analysis.
Comparison 13 Motivational phone calls versus usual care, Outcome 4 Pregnancy by 18 months.
| Pregnancy by 18 months | |||
|---|---|---|---|
| Study | Intervention (self report) Reported % | Control (self report) Reported % | Reported P |
| Kirby 2010 | 27% | 23% | NS |
14.1. Analysis.
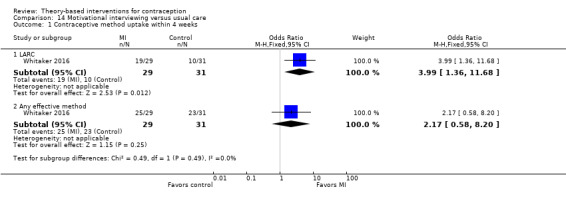
Comparison 14 Motivational interviewing versus usual care, Outcome 1 Contraceptive method uptake within 4 weeks.
14.2. Analysis.
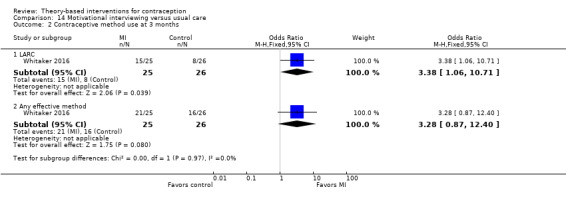
Comparison 14 Motivational interviewing versus usual care, Outcome 2 Contraceptive method use at 3 months.
14.3. Analysis.
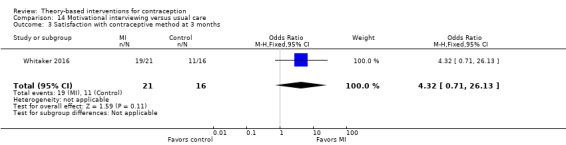
Comparison 14 Motivational interviewing versus usual care, Outcome 3 Satisfaction with contraceptive method at 3 months.
Transtheoretical model
The interventions in four trials incorporated the Transtheoretical model; two also used motivational interviewing as a counseling strategy (Barnet 2009; Gold 2016). They randomized individuals and were conducted in the USA. All used some type of technology to deliver the intervention to the individuals. The age range varied as did the number of sessions provided.
For Peipert 2008, a tailored intervention based on the Transtheoretical model was compared with enhanced standard care. Participants were 542 women, 13 to 35 years old, from various clinics. The computer‐delivered intervention had three tailored sessions for the experimental group and one non‐tailored session for the comparison group. At 24 months, the groups were not significantly different for any dual‐method use (Analysis 15.1), consistent condom use (Analysis 15.2), or unplanned pregnancy (tested) (Analysis 15.3). The investigators had reported differences between the groups after adjusting for a propensity score that included covariates and two‐way interactions. A secondary paper from 2011 examined dual‐method use with adjusted analyses. By 24 months, the intervention group was no more likely than the comparison group to have initiated or sustained dual‐method use (Analysis 15.4).
Barnet 2009 used several theories or models in an intervention to prevent rapid repeat births. Participants were pregnant adolescents from prenatal clinics (N = 237). The computer‐assisted motivational intervention (CAMI) was based on the Transtheoretical model (stages of change). The CAMI software used participants' responses to sexual and risk behavior questions to determine their stage of change. Then CAMI counselors used motivational interviewing for contraception counseling, which was matched to the participant's stage of change. SCT was the basis of the parenting curriculum, which came from Black 2006; it included contraception and was provided to the CAMI+ group. The home‐visiting intervention had multiple components, including case management. A CAMI‐only group had CAMI as a single‐component home‐based intervention. The control group had usual care. The groups were not significantly different for repeat births by 24 months from index birth (Analysis 16.1). Births were assessed through Vital Statistics; 100% of the index births were located. Abortion information was obtained at the follow‐up interview. According to the investigators, the percentages for reported abortions did not differ significantly across the groups: CAMI+ 22%, CAMI‐only 20%, and usual care 21%.
Davidson 2015 focused on preventing pregnancy (N = 191), using the Transtheoretical model. Participants were 18 to 29 years old and presenting for abortion. The intervention group viewed a three‐segment video (on a tablet computer) designed to encourage LARC use. A health care provider delivered one segment and peers provided the other two. The comparison group viewed a video of a physician speaking about stress management. Both groups received usual care after the assigned video. Contraceptives were free of charge, including LARC, an injection of depot medroxyprogesterone acetate, or a one‐month supply of the contraceptive pill, patch, or ring. LARC initiation was assessed by record review after the visit. The groups did not differ for LARC initiation overall (Analysis 17.1) nor for LARC initiation by type (Analysis 17.2).
The intervention in Gold 2016 was based on principles from the Transtheoretical model. The focus was on preventing pregnancy and STI through condom use. The trial included 572 young women, 13 to 21 years old. The intervention group had a computer‐assisted motivational intervention (CAMI) with three counseling sessions over six months. The comparison group received didactic educational counseling (DEC) over three sessions. The study arms did not differ in reporting unprotected sex at three, six, or nine months (Analysis 18.1).
15.1. Analysis.
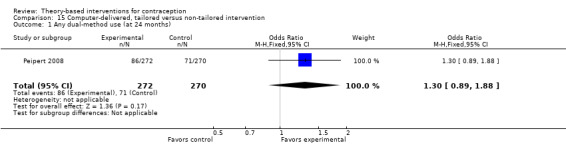
Comparison 15 Computer‐delivered, tailored versus non‐tailored intervention, Outcome 1 Any dual‐method use (at 24 months).
15.2. Analysis.
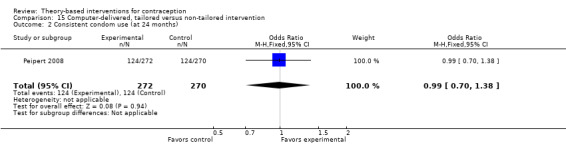
Comparison 15 Computer‐delivered, tailored versus non‐tailored intervention, Outcome 2 Consistent condom use (at 24 months).
15.3. Analysis.
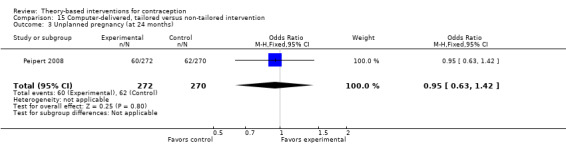
Comparison 15 Computer‐delivered, tailored versus non‐tailored intervention, Outcome 3 Unplanned pregnancy (at 24 months).
15.4. Analysis.
Comparison 15 Computer‐delivered, tailored versus non‐tailored intervention, Outcome 4 Dual‐method use at 24 months, adjusted.
| Dual‐method use at 24 months, adjusted | ||||
|---|---|---|---|---|
| Study | Measure | Intervention Reported % | Comparison Reported % | Reported adjusted relative risk (95% CI) |
| Peipert 2008 | Initiated | 82 | 68 | 1.52 (0.96 to 2.41) |
| Peipert 2008 | Sustained | 19 | 24 | 0.89 (0.45 to 1.75) |
16.1. Analysis.
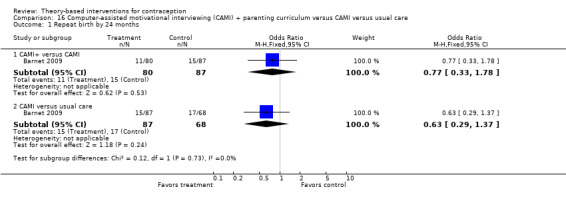
Comparison 16 Computer‐assisted motivational interviewing (CAMI) + parenting curriculum versus CAMI versus usual care, Outcome 1 Repeat birth by 24 months.
17.1. Analysis.
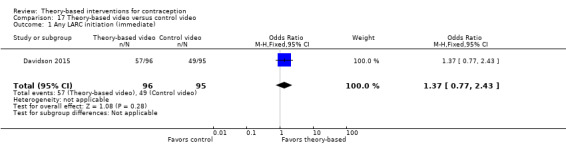
Comparison 17 Theory‐based video versus control video, Outcome 1 Any LARC initiation (immediate).
17.2. Analysis.
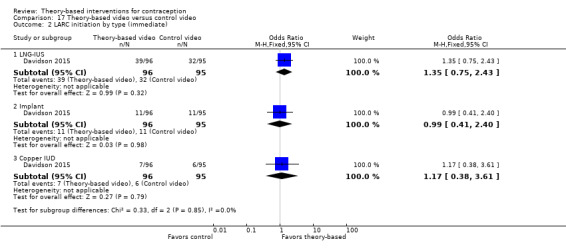
Comparison 17 Theory‐based video versus control video, Outcome 2 LARC initiation by type (immediate).
18.1. Analysis.
Comparison 18 Computer‐assisted motivational intervention versus didactic counseling, Outcome 1 Unprotected sex.
| Unprotected sex | |||
|---|---|---|---|
| Study | Assessment | Intent to treat Reported OR (95% CI) | As treated Reported OR (95% CI) |
| Gold 2016 | 3 months (2nd session) | 0.60 (0.33 to 1.11) | 0.91 (0.51 to 1.60) |
| Gold 2016 | 6 months (3rd session) | 0.48 (0.24 to 0.95) | 0.67 (0.37 to 1.26) |
| Gold 2016 | 9‐month follow‐up | 1.12 (0.37 to 3.36) | 1.26 (0.69 to 2.29) |
Additional theories and models
Six trials had interventions based on other theories or models. The conceptual basis may overlap conceptually with those above. Three USA studies randomized individuals (Schinke 1981; Berenson 2012; Gilliam 2014). The other three randomized communities or schools in the USA (Stanton 2004), South Africa (Taylor 2014), or Guatemala (Schuler 2015).
Several trials were based on social cognition models other than SCT. Two provided multiple group sessions for adolescents. The pregnancy prevention program of Schinke 1981 focused on cognitive and behavioral training and used a problem‐solving schema. Content included sexuality, birth control, and pregnancy. This USA trial randomized 36 high school sophomores in one school to study groups. Contact included 14 sessions of 50 minutes each. The control group only received the assessments. The report provided results of t‐tests and did not clearly define the outcome variables. We did not request details due to the age of the publication. At the six‐month follow‐up, the students who received the training had a higher mean than the control group for "more habitual contraception" (reported t (32) = 2.38; P < 0.05), "greater protection at last intercourse" (reported t (32) = 3.26; P < 0.005), and less reliance on "inadequate birth control" (reported t (32) = 4.35; P < 0.001) (Analysis 19.1). The intervention group also had better attitudes toward family planning (reported t (32) = 2.08; P < 0.05) (Analysis 19.1). At the post‐test, the intervention group had higher mean scores than the control group for knowledge of human reproduction (reported t (34) = 3.40; P < 0.002) and of birth control (reported t (34) = 2.63; P < 0.02) (Analysis 19.2).
19.1. Analysis.
Comparison 19 Pregnancy prevention education versus no education, Outcome 1 Contraceptive use and attitudes at 6 months.
| Contraceptive use and attitudes at 6 months | ||||
|---|---|---|---|---|
| Study | Outcome | N | Reported t statistic | Reported P |
| Schinke 1981 | More habitual contraception | 32 | 2.38 | < 0.05 |
| Schinke 1981 | Greater protection at last sex | 32 | 3.26 | < 0.005 |
| Schinke 1981 | Less reliance on inadequate birth control | 32 | 4.35 | < 0.001 |
| Schinke 1981 | Attitudes toward family planning | 32 | 2.08 | < 0.05 |
19.2. Analysis.
Comparison 19 Pregnancy prevention education versus no education, Outcome 2 Contraception knowledge at post‐test.
| Contraception knowledge at post‐test | ||||
|---|---|---|---|---|
| Study | Outcome | N | Reported t statistic | Reported P |
| Schinke 1981 | Knowledge of human reproduction | 34 | 3.40 | < 0.002 |
| Schinke 1981 | Knowledge of birth control | 34 | 2.63 | < 0.02 |
Stanton 2004 used Protection Motivation Theory (Rogers 1983), which includes components of the Health Belief Model as well as self‐efficacy (Conner 2005). This cluster randomized trial in the USA provided multiple intervention sessions for 817 participants. The three study groups were: (1) an eight‐week youth intervention (Y), also known as Focus on Kids; (2) the youth program and a short parent program (Y + P); or (3) the youth and parent interventions plus booster sessions for the youth program (Y + P + B). We calculated the design effects with the intraclass correlation coefficients for each outcome and the number of clusters provided in the report. We used these design effect estimates to obtain the effective sample sizes for our analyses. At the 24‐month follow‐up, the Y + P group was less likely than the Y group to report having been pregnant or gotten someone pregnant (OR 0.24, 95% CI 0.10 to 0.56), as was the Y + P compared with the Y + P + B (OR 0.27, 95% CI 0.11 to 0.66) (Analysis 20.1). In contrast, the groups did not differ significantly in the proportions who reported use of contraception or condom during last sex.
20.1. Analysis.
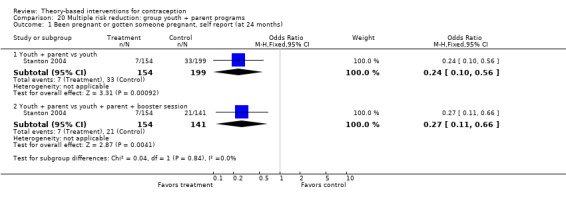
Comparison 20 Multiple risk reduction: group youth + parent programs, Outcome 1 Been pregnant or gotten someone pregnant, self report (at 24 months).
Another two trials focused on individual young women to encourage contraceptive adherence or LARC uptake. In Berenson 2012, the Health Belief Model provided the basis of the intervention to prevent STI and pregnancy. Participants were young women, 16 to 24 years old, attending reproductive health clinics (N = 1155). The three study arms were special counseling about OCs plus follow‐up phone calls (C + P), special clinic counseling about OC use, and standard clinic services. Below is a summary of results.
-
Special counseling plus phone calls (C + P) versus special counseling only
The C + P group was more likely to report consistent OC use at three months (OR 1.41, 95% CI 1.06 to 1.87) and at six months (OR 1.39, 95% CI 1.03 to 1.87) (Analysis 21.1).
At three months, inconsistent condom users in the C + P group were more likely to report condom use at last sex (OR 1.45, 95% CI 1.03 to 2.03) (Analysis 21.5).
The two arms did not differ significantly for reported use of dual methods at any time point (Analysis 21.3; Analysis 21.4) or for pregnancy at 12 months (from medical records) (Analysis 21.7).
The C + P group was more likely to report they would recommend OC use to a friend at three months (OR 1.52, 95% CI 1.11 to 2.09) and at six months (OR 1.68, 95% CI 1.20 to 2.36) (Analysis 21.8).
The group with special counseling only did not differ significantly from the standard care group for most outcomes (Analysis 21.2; Analysis 21.4; Analysis 21.6; Analysis 21.7). The exception was recommending OC use to a friend; the counseling‐only group was less likely than the standard care group to do so at six months (OR 0.65, 95% CI 0.46 to 0.91) (Analysis 21.9)
21.1. Analysis.
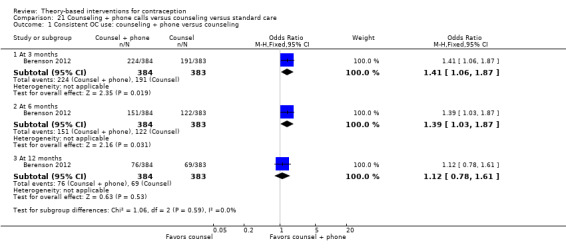
Comparison 21 Counseling + phone calls versus counseling versus standard care, Outcome 1 Consistent OC use: counseling + phone versus counseling.
21.5. Analysis.
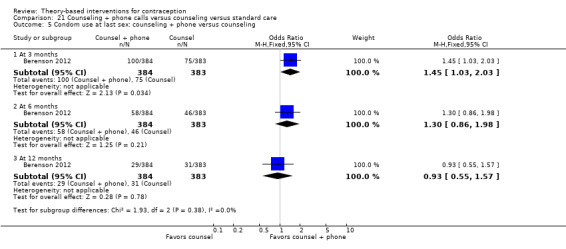
Comparison 21 Counseling + phone calls versus counseling versus standard care, Outcome 5 Condom use at last sex: counseling + phone versus counseling.
21.3. Analysis.
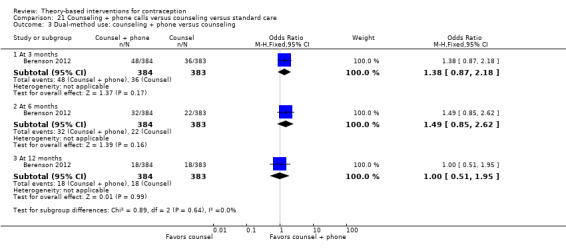
Comparison 21 Counseling + phone calls versus counseling versus standard care, Outcome 3 Dual‐method use: counseling + phone versus counseling.
21.4. Analysis.
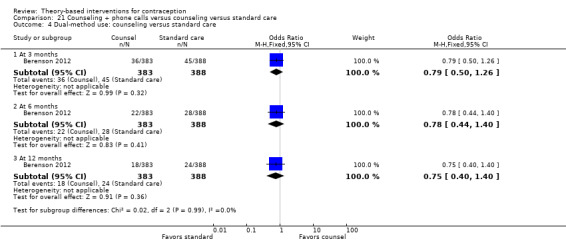
Comparison 21 Counseling + phone calls versus counseling versus standard care, Outcome 4 Dual‐method use: counseling versus standard care.
21.7. Analysis.
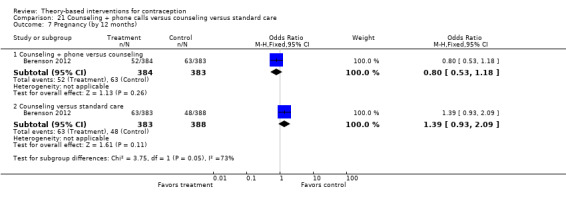
Comparison 21 Counseling + phone calls versus counseling versus standard care, Outcome 7 Pregnancy (by 12 months).
21.8. Analysis.
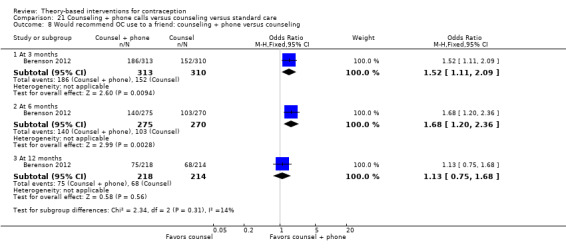
Comparison 21 Counseling + phone calls versus counseling versus standard care, Outcome 8 Would recommend OC use to a friend: counseling + phone versus counseling.
21.2. Analysis.
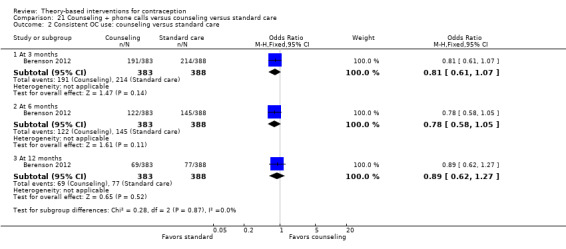
Comparison 21 Counseling + phone calls versus counseling versus standard care, Outcome 2 Consistent OC use: counseling versus standard care.
21.6. Analysis.
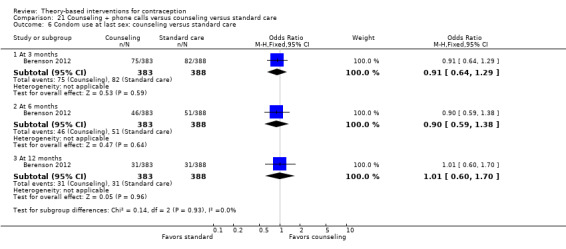
Comparison 21 Counseling + phone calls versus counseling versus standard care, Outcome 6 Condom use at last sex: counseling versus standard care.
21.9. Analysis.
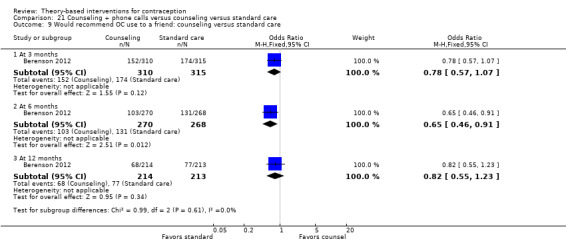
Comparison 21 Counseling + phone calls versus counseling versus standard care, Outcome 9 Would recommend OC use to a friend: counseling versus standard care.
Gilliam 2014 focused on preventing pregnancy, especially through selection of LARC. The 60 participants were aged 15 to 30 years and seeking contraceptive services. The intervention was an iOS application based on principles of 'human‐centered design' and the Theory of Planned Behavior. Content included information on LARC as well as the full range of contraceptive options. The intervention group used the app for a maximum of 15 minutes prior to standard care, which included contraceptive counseling and receipt of chosen method or prescription. The comparison group had standard care only. The study arms did not differ significantly for selection of any LARC or IUC by one month (Analysis 22.1).
22.1. Analysis.
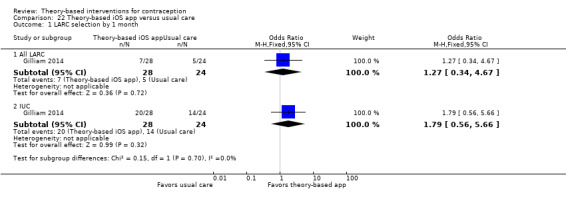
Comparison 22 Theory‐based iOS app versus usual care, Outcome 1 LARC selection by 1 month.
Two trials used integrated models. The conceptual framework for Taylor 2014 was the I‐Change model, an integration of ideas from the Theory of Planned Behavior, SCT, TTM, Health Belief Model, and goal setting theories (DeVries 2013). Schuler 2015 used a social and behavioral change model known as C‐Change, which appeared to incorporate elements of the Health Belief model and SCT.
The pregnancy prevention intervention of Taylor 2014 involved 12 weekly interactive sessions. Participants were in the first year of high school (grade 8) in KwaZulu‐Natal, South Africa. The study randomized 16 schools and had 816 participants. The special intervention addressed choice, body development, contraception, and parenthood. Both the intervention and comparison groups received the compulsory program on life skills plus media messages about teen pregnancy. The analysis corrected for cluster effect; multivariate linear and logistic regression models included covariates such as age, gender, socioeconomic status, and sexual experience. The investigators based the analysis of behavioral outcomes on a subsample that reported ever having sex, a variable that the intervention could affect. Since they did not include all those randomized, the comparisons were not randomized comparisons. The study groups did not differ significantly in self‐reported pregnancy (Analysis 23.1), and the groups did not differ for attitudes toward teen pregnancy (Analysis 23.2). The experimental group was more likely than the control group to report having any condom use (reported adjusted beta 0.98 ± SE 0.37; reported P < 0.01) (Analysis 23.1). The two groups did not differ significantly for condom use consistency (Analysis 23.2).
In Schuler 2015, the focus was on improving gender attitudes and communication about reproductive health (RH), including family planning. Participants (N = 1122) came from 30 communities in Guatemala. The intervention involved six sessions provided over one month on gender inequality and barriers to RH. The control group received the delayed intervention. The investigators used a difference in difference approach to compare changes from baseline; the study arms did not differ significantly in use of modern contraceptives at follow‐up (two months after baseline) (Analysis 24.1). However, the intervention group was more likely to have had an increase in knowledge of modern contraceptive methods among the women (reported adjusted OR 2.48, 95% CI 1.09 to 5.64) (Analysis 24.2) and among the men (4.47, 95% CI 1.96 to 10.18) (Analysis 24.3).
23.1. Analysis.
Comparison 23 Pregnancy prevention program versus usual life skills program, Outcome 1 Dichotomous outcomes (8 months after baseline).
| Dichotomous outcomes (8 months after baseline) | ||||||
|---|---|---|---|---|---|---|
| Study | Outcome | N (ever had sex) | Experimental Reported % (n) | Control Reported % (n) | Reported adjusted beta ± SE | Reported P |
| Taylor 2014 | Been pregnant or caused pregnancy | 129 | 6.3% (5) | 4.4% (2) | 0.27 ± 2.99 | NS |
| Taylor 2014 | Condom use (any) | 129 | 54.2% (39) | 36.7% (11) | 0.98 ± 0.37 | < 0.01 |
23.2. Analysis.
Comparison 23 Pregnancy prevention program versus usual life skills program, Outcome 2 Scale outcomes (8 months after baseline).
| Scale outcomes (8 months after baseline) | ||||||
|---|---|---|---|---|---|---|
| Study | Outcome | N | Experimental Reported mean ± SD | Control Reported mean ± SD | Reported adjusted beta ± SE | Reported P |
| Taylor 2014 | Condom use consistency (4‐point scale) | 129 | 2.34 ± 1.29 | 2.66 ± 1.28 | ‐0.25 ± 0.21 | NS |
| Taylor 2014 | Attitude toward teen pregnancy (pro) | 679 | 2.26 ± 0.82 | 2.45 ± 0.85 | ‐0.13 ± 0.13 | NS |
| Taylor 2014 | Attitude toward teen pregnancy (con) | 679 | 3.81 ± 0.87 | 3.83 ± 0.93 | 0.01 ± 0.09 | NS |
24.1. Analysis.
Comparison 24 Social and behavioral change model (gender equity + FP) versus delayed intervention, Outcome 1 Use of modern contraceptive methods at 2 months.
| Use of modern contraceptive methods at 2 months | ||||
|---|---|---|---|---|
| Study | Group | N | Reported adjusted OR (95% CI) | Reported P |
| Schuler 2015 | Intervention (follow‐up ‐ baseline) | _ | 1.79 (1.06 to 3.03) | 0.031 |
| Schuler 2015 | Control (follow‐up ‐ baseline) | _ | 1.24 (0.68 to 2.26) | 0.472 |
| Schuler 2015 | Difference in difference | 292 | 1.45 (0.65 to 3.22) | 0.350 |
24.2. Analysis.
Comparison 24 Social and behavioral change model (gender equity + FP) versus delayed intervention, Outcome 2 Knowledge of modern contraceptive methods (women at 2 months.
| Knowledge of modern contraceptive methods (women at 2 months | |||
|---|---|---|---|
| Study | Group | N | Reported adjusted OR (95% CI) |
| Schuler 2015 | Intervention (follow‐up ‐ baseline) | _ | 4.28 (2.39 to 7.66) |
| Schuler 2015 | Control (follow‐up ‐ baseline) | _ | 1.73 (0.97 to 3.08) |
| Schuler 2015 | Difference in difference | 334 | 2.48 (1.09 to 5.64) |
24.3. Analysis.
Comparison 24 Social and behavioral change model (gender equity + FP) versus delayed intervention, Outcome 3 Knowledge of modern contraceptive methods (men at 2 months.
| Knowledge of modern contraceptive methods (men at 2 months | |||
|---|---|---|---|
| Study | Group | N | Reported adjusted OR (95% CI) |
| Schuler 2015 | Intervention (follow‐up ‐ baseline) | _ | 6.11 (3.40 to 10.98) |
| Schuler 2015 | Control (follow‐up ‐ baseline) | _ | 1.37 (0.77 to 2.44) |
| Schuler 2015 | Difference in difference | 267 | 4.47 (1.96 to 10.18) |
Discussion
Summary of main results
We summarized results for each study in Table 5, which also has the quality of evidence assessment from Table 4. Overall, eight studies based the intervention on social cognitive theory or SCT plus another theory or model, six used motivational interviewing and one used the related Information‐Motivation‐Behavioral Skills model, four had the Transtheoretical model as the basis, and six used a variety of other theories (Table 5). In this section we focus on nine studies that provided high or moderate quality evidence for our review and also showed an intervention effect.
4. Outcome summary by theory base and evidence quality.
| Studya | Pregnancies or births | Contraceptive use (non‐condom) | Condom use | Dual‐method use | Evidence qualityb |
| Social cognitive theory | |||||
| Black 2006 | Repeat pregnancy | _ | _ | _ | High |
| Sieving 2013 | _ | Hormonal consistency | Consistency | Consistency (OCs + condoms) | Moderate |
| Wight 2002 | NS | NS | NS | _ | Moderate |
| Coyle 2001 | _ | Effective method | Last sex; past 3 mo | _ | Moderate |
| Coyle 2006 | NS | NS | Last sex; past 3 mo | _ | Moderate |
| Tortolero 2010 | _ | _ | NS | _ | Moderate |
| Markham 2012 | _ | _ | RA: last sex; NS, past 3 mo RR: last sex; past 3 mo |
_ | Moderate |
| Raj 2016 | NS | NS | _ | _ | High |
| Motivational interviewing or IMB model | |||||
| Boyer 2005 | NS | _ | NS | _ | Low |
| Floyd 2007 | _ | Effective | _ | _ | Moderate |
| Ceperich 2011 | _ | Less ineffective | _ | _ | Moderate |
| Rendall‐Mkosi 2013 | _ | Less ineffective | _ | _ | Moderate |
| Petersen 2007 | NS | NS | _ | _ | High |
| Kirby 2010 | NS | NS | NS | _ | Moderate |
| Whitaker 2016 | _ | LARC; NS, effective method | _ | _ | Moderate |
| Transtheoretical model | |||||
| Peipert 2008 | NS | _ | NS | NS | Low |
| Barnet 2009 | NS | _ | _ | _ | High |
| Davidson 2015 | _ | NS | _ | _ | Moderate |
| Gold 2016 | _ | _ | NS | _ | Low |
| Additional theories or modelsc | |||||
| Schinke 1981 | _ | Habitual; less inadequate | _ | _ | Low |
| Stanton 2004 | Pregnancy, self‐report | NS | NS | _ | Low |
| Berenson 2012 | NS | C+P: OCs consistently C: NS |
C+P: last sex C: NS |
NS | Low |
| Gilliam 2014 | _ | NS | _ | _ | Low |
| Taylor 2014 | _ | _ | Any; NS, consistent | _ | Low |
| Schuler 2015 | _ | NS | _ | _ | Low |
aTable has primary outcomes for this review by theory or model base; for explanation of comparison groups or outcomes, see Characteristics of included studies bFrom Table 4 cCognitive and behavioral training (Schinke 1981); Protection Motivation Theory (Stanton 2004); Health Belief Model (Berenson 2012); human‐centered design and Theory of Planned Behavior (Gilliam 2014); integrated model, I‐Change (Taylor 2014); social and behavioral change model, C‐Change (Schuler 2015) C+P and C: counseling + phone calls group and counseling‐only group IMB: Information‐Motivation‐Behavioral Skills model LARC: long‐acting reversible contraception NS: no significant difference between study groups
Of the trials based on social cognitive theory, five had some positive results for the intervention group (Table 1). All focused on adolescents, were one to two years in length, and were conducted in the USA. A home‐based curriculum for adolescent mothers was primarily based on SCT (Black 2006). Four used SCT plus another theory or model. The interventions included a curriculum for prevention of pregnancy and HIV/STI among public school students (Coyle 2001) and a similar program for alternative day schools (Coyle 2006), school programs for risk avoidance and risk reduction (regarding adolescent pregnancy and STI/HIV transmission) (Markham 2012), and a case‐management and peer leadership program for high‐risk adolescents (Sieving 2013). Compared with the usual care or standard education group in these trials, the intervention group had fewer second births to adolescent mothers (Black 2006), more use of effective contraceptives (Coyle 2001; Sieving 2013), and more use of condoms (Coyle 2001; Coyle 2006; Markham 2012; Sieving 2013) and dual methods (Sieving 2013).
Of trials that used motivational interviewing as the basis for the intervention, four showed a significant difference between study arms (Table 2). Three focused on reducing risk for alcohol‐exposed pregnancy among women engaged in risky drinking and one focused on pregnancy prevention after abortion through LARC use in particular. The time frames for assessment ranged from one to nine months. Participants were young women in two trials (ages 18 to 24 and 15 to 29 years) and women 18 to 44 years in the other two studies. Three were conducted in the USA and one was from South Africa. Two trials provided one MI session each, and the other trials provided four and five MI sessions, respectively. Compared with a group that received handouts only (three trials) or routine counseling (one study), the MI group reported more use of effective contraception (Floyd 2007), less use of ineffective contraception (Ceperich 2011; Rendall‐Mkosi 2013), and more initiation and use of LARC (Whitaker 2016).
Studies using other theories or models did not provide high or moderate quality evidence or did not show an intervention effect (Table 5). Four trials using the Transtheoretical model did not show any intervention effect. All six trials that used other theories or models had low quality evidence for our review.
Overall completeness and applicability of evidence
Trials were generally conducted in community settings, schools, or clinics. Most provided multiple sessions or contacts. Nearly all included pregnancy prevention as an objective and the majority focused on contraceptive use (non‐condom). Eleven also addressed preventing HIV or STI, and two addressed multiple risks. Five trials took place outside the USA.
Twelve trials focused on adolescents and all provided multiple sessions or contacts. Seven of the 12 were school‐based. The interventions in seven were based on social cognitive theory; the other five used various models. Seven studies included young women as well as adolescents and were also based on a range of theories and models. Four of the seven provided one educational session. Another six trials included a wider age range of women, i.e. those of reproductive age. Four of the six used motivational interviewing or the IMB model, and five had multiple sessions.
Some of the effective interventions were targeted to higher risk groups and may not be applicable to a general audience. Of the five programs for adolescents that showed a difference between study arms, two were intended for higher risk teenagers and one was developed for low‐income adolescent mothers. In addition, three of the four effective MI interventions focused on women engaged in risky drinking.
Applicability of the successful interventions to traditional contraceptive counseling may be limited. The shortest intervention that showed an effect was 60 to 75 minutes in duration; most involved multiple sessions. Contraceptive counseling typically focuses on individual women. Contact time might be a few minutes within a clinic visit or a separate session of 10 to 15 minutes. In such situations, expectations for behavior change has to be limited.
As noted earlier, theories and models have been used extensively in HIV and STI research. Comparable high‐quality research on behavior change had been limited for reproductive health. This update shows an increased number recently for family planning; we found 10 new eligible studies since the 2013 update. In a USA study about reproductive counseling, in‐depth interviews indicated that most clinicians believed they influenced their patients through their medical authority and the presentation of information (Henderson 2011). The investigators noted that views were not consistent with current thinking about behavior change and patient‐centered counseling. Effective interventions are needed, including some that can be adapted to clinical settings.
Quality of the evidence
We considered the overall quality of evidence to be moderate for our review. Of 25 trials, 4 provided evidence of high quality according to our criteria, 12 were moderate quality, and 9 had low quality evidence (Table 4). Of 13 trials with effective interventions, 9 were high or moderate quality. The major reason for downgrading was high loss to follow‐up. The study arms generally had similar losses (Incomplete outcome data). Losses may be more likely with a focus on adolescents and a relatively long follow‐up period.
Some reports did not provide sufficient information to fully assess trial quality, as design information was lacking. Within the studies with a priori sample size estimations, sample size was sufficient to detect differences in behavior. However, half the studies did not report a priori calculations. Two individually randomized trials were reportedly powered to detect a difference in pregnancy and one cluster RCTs was powered to detect a difference in abortion rate several years postprogram.
The primary outcomes for our review were generally self‐reported, i.e. contraceptive use. Because of social desirability and other types of information bias, self‐reports are not the most reliable indicators of behavior. Two trials used medical records for LARC uptake, i.e. IUC or implant insertion. Other types of contraceptive use can be assessed more objectively in clinical trials, e.g. on‐time injections or electronic pill counts. However, such methods are less feasible when the intervention is a program rather than a drug or device; the participants may be using a wide range of contraceptives. For pregnancy, rates are preferable to self‐report, especially if the incidence is likely to be high enough to detect differences between groups. Seven trials used objective means to assess pregnancies: four conducted pregnancy tests, one observed the presence of second births, and two checked records for relevant births.
All studies provided information on the fidelity of implementation; we used five criteria from Borrelli 2011 that were relevant to completed interventions. The type and amount of information reported varied (Table 30). Eighteen trials met at least four of the five criteria we used. Areas most often lacking information were training for the intervention and means to assess adherence to the protocol.
Effectiveness may be limited when the theory or model is partially implemented. Some trials appeared to use parts of theories or models, i.e. specific principles or constructs, rather than the full theory. When trials combined models, we usually could not determine what parts were used and what may have worked. For some trials, the emphasis was likely on the intervention rather than a particular theory or model, as most theories had been examined previously. We required the intervention to have evidence of incorporating constructs or principles from the theory or model. However, we could not always discern whether the theory drove the intervention development or if a theory or model was chosen to complement an intervention idea. The information was not sufficient in many cases to assess theory implementation.
Potential biases in the review process
We tried to identify the primary theoretical basis and group the results accordingly; other researchers might have synthesized the results differently. For example, some trials incorporated elements of the Transtheoretical model and used principles of motivational interviewing to varying degrees. In addition, the main social cognition models have considerable overlap in their principles and constructs (Conner 2005). The ecological approach of C‐Change, used in one trial here, appeared to have elements from other social cognition models.
In some trials, certain intervention components may have been emphasized rather than the overall theory. Further inquiries to the investigators and review of intervention materials might have provided more information for analysis and interpretation. However, a full assessment of theory implementation was beyond the scope of this review. Response rates to inquiries for further information varies, as does the quantity and quality of information provided.
Agreements and disagreements with other studies or reviews
A systematic review examined motivational interviewing to reduce pregnancy risk (Wilson 2015). The eight RCTs, also in our review, were either based on MI principles or on the TTM with the MI approach. The conclusions were similar to ours: the interventions led to more effective contraceptive use in the short term only. Also, the programs had no effect on subsequent pregnancy.
Many of the studies in our review that had an effect on pregnancy or contraceptive use were based on SCT or on SCT and another theory. Others showed a change in knowledge or attitude related to the intervention and no effect on action, i.e. contraceptive use. Those interventions were based on SCT, another social cognition model, or an integrated model. Even limited interventions can result in short‐term changes. A feasibility study tested an online video about IUDs, which was based on social cognitive theory (Garbers 2015). Participants had a significant increase in IUD knowledge and were more likely to obtain an IUD in the next few months than before viewing the video. A non‐randomized study from Iran had a more intensive intervention based on BASNEF, a model with elements of SCT and the Theory of Planned Behavior (Sarayloo 2015). The educational program included four weekly sessions and two review sessions. The intervention group had a greater improvement in contraceptive use after the program, as well as changes in knowledge and attitude.
In our review, interventions based on the TTM had no effect on contraceptive use or pregnancy. The four trials ranged in evidence quality from high to low. Three of the interventions were computer‐assisted, though two also had in‐person educational sessions. One provided an educational video on a tablet computer. A non‐randomized study in Iran used the TTM to implement a contraceptive education program (Kamalikhah 2015). Intervention groups were based on the participants' stage of change. Both groups showed improvement in practices related to family planning, such as communicating with their spouse, but only the experimental group had a significant improvement in contraception use. A systematic review found that the TTM was the most commonly used theory or model in Iran for interventions to increase physical activity (Abdi 2015). Most of the studies did not address maintenance of the behavior, though. From Northern Ethiopia, a cross‐sectional study used the TTM to examine male involvement in family planning in the context of stage of change (Berhane 2015). The TTM may be more useful in identifying stages of change than in designing interventions to encourage change.
A cumulative scientific approach could benefit the health behavior field (Johnston 2008) and may lead to an integrated model of health behavior (Conner 2005). I‐Change is an integrated model used in Taylor 2014 that incorporates principles from various theories and models (DeVries 2013). Discerning what works may become more difficult with an increasing number of operative principles. Comparisons of theories or models for their relative utility could be helpful in designing programs for contraception behavior change. Using structural equation modeling, Espada 2016 found the Theory of Planned Behavior explained the frequency of condom use among adolescents better than Social Cognitive Theory or the Information‐Motivation‐Behavioral skills model.
Authors' conclusions
Implications for practice.
Interventions with a theoretical base help explain behavior change. Counseling often focuses on information transfer rather than how people learn, think, and behave. We found 10 new theory‐based interventions for this update. From the overall review of 25 trials, 9 had good quality evidence and an intervention effect. Five were based on social cognitive theory (SCT); they focused on adolescents and provided multiple sessions over one to two years. Four were implemented in school classes or another group format and may be applicable to settings other than clinics. Four trials using motivational interviewing (MI) had a wider age range and provided one to five sessions. Three of the MI studies focused on reducing alcohol‐exposed pregnancy and one on preventing pregnancy after abortion. The MI format may be appropriate for clinics, but the interventions should be tested with more diverse populations.
Implications for research.
The use of theory was more widespread than we found previously. Many reports could have been clearer about how the theory or model was used in designing and implementing the intervention. We had some difficulty identifying what worked when studies used parts of theories or combined models. Testing of single theories would be helpful as would comparisons of two theories. The majority of trials provided evidence of high or moderate quality by our criteria, and half of those showed an intervention effect. The programs based on social cognitive theory were multifaceted and those using motivational interviewing addressed special populations. Clinics and sites with few resources need effective interventions that can be adapted for their settings and that may be effective with their typical clients.
Better alignment of objectives, interventions, and outcomes would help in categorizing studies and interpreting results. Most studies had pregnancy prevention as an objective, often in addition to preventing STI and HIV. Fewer than half assessed pregnancy as an outcome, and about a third did not have contraceptive use as an outcome. In contrast, we found (and excluded) many studies that assessed pregnancy or contraceptive use as an outcome but did not appear to address contraception in the intervention.
What's new
| Date | Event | Description |
|---|---|---|
| 1 November 2016 | New search has been performed | Search updated |
| 29 September 2016 | New citation required but conclusions have not changed | Effective interventions with moderate quality evidence: Social Cognitive Theory with multiple sessions for adolescents; motivational Interviewing with special populations |
| 17 August 2016 | Amended | Added 10 new trials (Tortolero 2010; Markham 2012; Rendall‐Mkosi 2013; Gilliam 2014; Taylor 2014; Davidson 2015; Schuler 2015; Gold 2016; Raj 2016; Whitaker 2016) and additional data for previously included study (Sieving 2013) |
| 15 August 2016 | Amended | Added 'Summary of findings' tables |
History
Protocol first published: Issue 3, 2008 Review first published: Issue 1, 2009
| Date | Event | Description |
|---|---|---|
| 3 July 2013 | New search has been performed | Searches updated. |
| 30 May 2013 | New citation required but conclusions have not changed | Three new trials included (Berenson 2012; Cowan 2010a; Sieving 2013). Secondary papers from previously included trials added: Ceperich & Ingersoll, 2011 (Ceperich 2011; Peipert et al, 2011 (Peipert 2008); Doyle et al, 2010 (Ross 2007a); Henderson et al, 2006 (Wight 2002). Intervention fidelity (Table 30): added criterion and ratings. Evidence quality ratings (Table 5): included more design and fidelity information. |
| 10 December 2010 | New citation required and conclusions have changed | Revised review to focus on interventions that had identified contraception content as well as outcome of pregnancy, repeat birth, or contraceptive use other than condoms. For specifics, see Criteria for considering studies for this review and Excluded studies. Two new trials were included (Barnet 2009; Kirby 2010). |
| 9 November 2010 | New search has been performed | Searches were updated |
| 21 April 2008 | Amended | Converted to new review format. |
| 17 April 2008 | New citation required and conclusions have changed | Substantive amendment |
Acknowledgements
From FHI 360, Carol Manion helped design and implement the initial literature searches. Kenneth Schulz provided consultation on methodological issues for the initial review.
David A Grimes, formerly of FHI 360, was an author of earlier versions of this review. In 2008 and 2010, he consulted on inclusion criteria and conducted the secondary data extraction for the outcomes.
Appendices
Appendix 1. Search 2016
MEDLINE via PubMed (1 April 2013 to 1 November 2016)
("Contraception"[Mesh] OR "Contraception Behavior"[Mesh] OR "Contraceptive Agents"[Mesh] OR "Contraceptive Devices"[Mesh] OR contracept*[tiab] OR "family planning"[tiab] OR condom*[tiab] OR "protected sex"[tiab] OR "unprotected sex"[tiab]) AND (theor*[tiab] OR model[tiab] OR models[tiab] OR principle*[tiab] OR construct*[tiab] OR framework[tiab] OR "motivational interview*"[tiab] OR tailored[ti]) AND (educat*[tiab] OR counsel*[tiab] OR communicat*[tiab] OR behavioral[tiab] OR psycho‐social[tiab] OR psychosocial[tiab] OR use[tiab] OR uptake[tiab] OR continuation[tiab]) AND ( ( Clinical Trial[ptyp] OR Clinical Study[ptyp] OR Comparative Study[ptyp] OR Evaluation Studies[ptyp] OR Multicenter Study[ptyp] ) )
CENTRAL (2 June 2016 (Cochrane Library Issue 5, 2016))
contracept* OR "family planning" OR condom OR protected OR unprotected in Title AND (theory OR theories OR theoret* OR model OR models OR principle* OR construct* OR framework*) in Abstract AND (counsel* OR communicat* OR educat* OR intervention OR uptake OR use OR continuation OR behavioral OR psycho‐social OR psychosocial) in Abstract Search limits: Trials Publication year: 2013 to 2016
POPLINE (2 June 2016)
Keywords: Contraception AND All fields: theor* OR model OR principle* OR construct* OR framework AND Keywords: Education OR Counseling AND Behavior change AND Interventions Years: From 2013 to 2016
Web of Science (2 June 2016)
TOPIC:(contracept* OR family planning) AND TOPIC: (theor* OR model* OR principle* OR construct* OR framework) AND TOPIC: (educat* OR counsel* OR behavioral OR psychosocial OR intervention) Refined by: RESEARCH AREAS: ( HEALTH CARE SCIENCES SERVICES OR OBSTETRICS GYNECOLOGY OR PUBLIC ENVIRONMENTAL OCCUPATIONAL HEALTH ) AND RESEARCH DOMAINS: ( SCIENCE TECHNOLOGY ) AND DOCUMENT TYPES: ( CLINICAL TRIAL ) Timespan: 2013‐2016.Search language=Auto
ClinicalTrials.gov (1 March 2013 to 6 June 2016)
Search terms: (theory OR model OR principles OR constructs OR framework) AND ((contraception OR contraceptive) OR pregnancy OR condom) Study type: Interventional studies Outcome measures: pregnancy OR birth OR births OR condom use OR unprotected sex OR protected sex
ICTRP (1 January 2013 to 6 June 2016)
Title: contraception OR contraceptive OR pregnancy Intervention: theory OR model OR principles OR constructs OR framework Recruitment status: all
Appendix 2. Previous searches
2013
MEDLINE via PubMed (01 June 2010 to 03 July 2013)
("Contraception"[Mesh] OR "Contraception Behavior"[Mesh] OR "Contraceptive Agents"[Mesh] OR "Contraceptive Devices"[Mesh] OR condom*[tiab] OR protected[tiab] OR unprotected[tiab]) AND (theor* OR model* OR principle* OR construct* OR framework* OR behavioral OR psycho‐social OR psychosocial) AND (educat* OR counsel* OR communicat* OR information disseminat* OR intervention* OR choice OR choose OR use OR continuation) Limits Activated: Clinical Trial, Randomized Controlled Trial
CENTRAL (2010 to 27 May 2013)
contracept* in Title, Abstract or Keywords AND (theory OR theories OR theoret* OR model* OR principle* OR construct* OR framework* OR behavioral OR psycho‐social OR psychosocial) in Title, Abstract or Keywords AND (counsel* OR communicat* OR educat* OR information disseminat* OR intervention OR choice OR choose OR use OR continuation) in Title, Abstract or Keywords Limits Activated: Trials
POPLINE (2010 to 28 March 2013)
All Fields: (contraceptive methods chosen, contraceptive continuation, contraceptive usage determinants) AND (behavioral, psycho‐social, psychosocial, theor*, model*, principle*, construct*, framework*) AND (educat*, counsel*, communicat*, information disseminat*, intervention*)
PsycINFO (01 June 2010 to 19 March 2013)
(contraception OR contraceptive OR contraceptives OR birth control) AND (theory OR theories OR theoret* OR model* OR principle* OR construct* OR framework* OR behavioral OR psycho‐social OR psychosocial) AND (educat* OR counsel* OR communicat* OR information disseminat* OR intervention* OR choice OR choose OR use OR continuation) Empirical study
ClinicalTrials.gov (01 June 2010 to 01 May 2013)
Search terms: theor* OR model* OR principle* OR construct* OR framework* OR behavioral OR psycho‐social OR psychosocial OR motivational Study type: Interventional studies Intervention: Contracept* OR condom* OR protected OR unprotected Outcomes: pregnancy OR pregnant* OR birth* OR condom OR contracept*
ICTRP (01 June 2010 to 28 March 2013)
1) Title: contracept* or 2) Condition: contracept* Intervention: theor* OR model* OR principle* OR construct* OR framework* OR behavioral OR psycho‐social OR psychosocial Recruitment status: all
2008 and 2010
MEDLINE via PubMed (to 8 November 2010)
("Contraception"[Mesh] OR "Contraception Behavior"[Mesh] OR "Contraceptive Agents"[Mesh] OR "Contraceptive Devices"[Mesh] OR condom*[tiab] OR protected[tiab] OR unprotected[tiab]) AND (theor* OR model* OR principle* OR construct* OR framework* OR behavioral OR psycho‐social OR psychosocial) AND (educat* OR counsel* OR communicat* OR information disseminat* OR intervention* OR choice OR choose OR use OR continuation) Limits Activated: Clinical Trial, Randomized Controlled Trial
CENTRAL (to 8 November 2010)
contracept* in Title, Abstract or Keywords AND (theory OR theories OR theoret* OR model* OR principle* OR construct* OR framework* OR behavioral OR psycho‐social OR psychosocial) in Title, Abstract or Keywords AND (counsel* OR communicat* OR educat* OR information disseminat* OR intervention OR choice OR choose OR use OR continuation) in Title, Abstract or Keywords Limits Activated: Trials
POPLINE (to 8 November 2010)
(contraceptive methods chosen, contraceptive continuation, contraceptive usage determinants) & (behavioral/psycho‐social/psychosocial/ theor*/ model*/ principle*/ construct*/ framework*) & (educat*/ counsel*/ communicat*/ information disseminat*/ intervention*)
EMBASE (to 8 November 2010)
contracept? AND (theory OR theories OR theoret? OR model? OR principle? OR construct? OR framework?) AND (behavioral OR psycho‐social OR psychosocial) AND (educat? OR choice OR choos? OR counsel? OR communicat? OR information()disseminat? OR intervention? OR use OR continuation)
PsycINFO (to 8 November 2010)
(contraception OR contraceptive OR contraceptives OR birth control) AND (theory OR theories OR theoret* OR model* OR principle* OR construct* OR framework* OR behavioral OR psycho‐social OR psychosocial) AND (educat* OR counsel* OR communicat* OR information disseminat* OR intervention* OR choice OR choose OR use OR continuation)
ClinicalTrials.gov (to 9 November 2010)
Search terms: theor* OR model* OR principle* OR construct* OR framework* OR behavioral OR psycho‐social OR psychosocial Intervention: Contracept* OR condom* OR protected OR unprotected Outcomes: pregnancy OR pregnant* OR birth* OR condom OR contracept* Study type: interventional studies
ICTRP (to 7 February 2011)
Title or Condition: contracept* Intervention: theor* OR model* OR principle* OR construct* OR framework* OR behavioral OR psycho‐social OR psychosocial
Data and analyses
Comparison 1. Pregnancy prevention curriculum versus usual sex education.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Pregnancy and oral contraceptive use at 6 months postprogram (24 months) | Other data | No numeric data | ||
| 2 Condom use at 6 months postprogram (24 months) | Other data | No numeric data | ||
| 3 Outcomes by age 20 (women, 4.5 years postprogram) | Other data | No numeric data |
Comparison 2. Home‐based mentoring versus usual care.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Second birth by 24 months | 1 | 149 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.41 [0.17, 1.00] |
Comparison 3. Case management + peer leadership versus usual care.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Consistency of condom use | Other data | No numeric data | ||
| 2 Consistency of hormonal contraceptive use | Other data | No numeric data | ||
| 3 Consistency of dual‐method use | Other data | No numeric data | ||
| 4 Months of consistent use in past 7 months (at 30 months) | Other data | No numeric data | ||
| 5 Attitude: desire to use contraception | Other data | No numeric data |
Comparison 4. Curriculum to prevent pregnancy, HIV, and STI versus standard sex education.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Effective protection against pregnancy | Other data | No numeric data | ||
| 2 Condom use | Other data | No numeric data | ||
| 3 Attitudes toward condoms | Other data | No numeric data |
Comparison 5. Curriculum to prevent HIV, STI, and pregnancy versus usual prevention activities (in alternative schools).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Pregnancy (self report) | Other data | No numeric data | ||
| 2 Effective pregnancy prevention at last sex | Other data | No numeric data | ||
| 3 Condom use at last sex | Other data | No numeric data | ||
| 4 Frequency of sex without condom use in past 3 months | Other data | No numeric data | ||
| 5 Condom knowledge | Other data | No numeric data | ||
| 6 General attitudes toward condoms | Other data | No numeric data |
Comparison 6. HIV, STI, and pregnancy prevention versus usual health classes.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Contraception use | Other data | No numeric data | ||
| 2 Condom knowledge | Other data | No numeric data |
Comparison 7. Education for sexual risk avoidance versus risk reduction versus usual health education.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Unprotected sex (no condom) at last vaginal sex | Other data | No numeric data | ||
| 2 Vaginal sex without condom in last 3 months | Other data | No numeric data | ||
| 3 General condom knowledge | Other data | No numeric data |
Comparison 8. Family planning and gender equity program versus usual services.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Use of modern contraceptive in past 3 months | Other data | No numeric data | ||
| 2 Pregnancy | Other data | No numeric data |
Comparison 9. Group risk reduction versus group health promotion.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Outcomes at 14 months | Other data | No numeric data |
Comparison 10. Motivational interviewing versus handouts.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Ineffective contraceptive use | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.1 At 1 month | 1 | 199 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.49 [0.28, 0.87] |
| 1.2 At 4 months | 1 | 207 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.56 [0.31, 0.98] |
| 2 Effective contraceptive use | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 2.1 At 3 months | 1 | 665 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.12 [1.53, 2.92] |
| 2.2 At 6 months | 1 | 604 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.88 [1.35, 2.61] |
| 2.3 At 9 months | 1 | 593 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.04 [1.47, 2.83] |
Comparison 11. Motivational interviewing versus handouts.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Ineffective contraceptive use | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.1 At 3 months | 1 | 165 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.31 [0.12, 0.77] |
| 1.2 At 12 months | 1 | 165 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.51 [0.25, 1.05] |
Comparison 12. Motivational interviewing versus general health counseling.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Contraceptive use maintained at high level or improved | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.1 At 2 months | 1 | 648 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.33 [0.95, 1.85] |
| 1.2 At 8 months | 1 | 692 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.05 [0.77, 1.42] |
| 1.3 At 12 months | 1 | 664 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.19 [0.87, 1.63] |
| 2 Pregnancy (by 12 months) | 1 | 737 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.88 [0.55, 1.42] |
Comparison 13. Motivational phone calls versus usual care.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Hormonal contraceptive use at last sex | Other data | No numeric data | ||
| 2 Condom use at last sex | Other data | No numeric data | ||
| 3 Use of hormonal contraceptive or condom at last sex | Other data | No numeric data | ||
| 4 Pregnancy by 18 months | Other data | No numeric data |
Comparison 14. Motivational interviewing versus usual care.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Contraceptive method uptake within 4 weeks | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.1 LARC | 1 | 60 | Odds Ratio (M‐H, Fixed, 95% CI) | 3.99 [1.36, 11.68] |
| 1.2 Any effective method | 1 | 60 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.17 [0.58, 8.20] |
| 2 Contraceptive method use at 3 months | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 2.1 LARC | 1 | 51 | Odds Ratio (M‐H, Fixed, 95% CI) | 3.38 [1.06, 10.71] |
| 2.2 Any effective method | 1 | 51 | Odds Ratio (M‐H, Fixed, 95% CI) | 3.28 [0.87, 12.40] |
| 3 Satisfaction with contraceptive method at 3 months | 1 | 37 | Odds Ratio (M‐H, Fixed, 95% CI) | 4.32 [0.71, 26.13] |
Comparison 15. Computer‐delivered, tailored versus non‐tailored intervention.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Any dual‐method use (at 24 months) | 1 | 542 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.30 [0.89, 1.88] |
| 2 Consistent condom use (at 24 months) | 1 | 542 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.99 [0.70, 1.38] |
| 3 Unplanned pregnancy (at 24 months) | 1 | 542 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.95 [0.63, 1.42] |
| 4 Dual‐method use at 24 months, adjusted | Other data | No numeric data |
Comparison 16. Computer‐assisted motivational interviewing (CAMI) + parenting curriculum versus CAMI versus usual care.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Repeat birth by 24 months | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.1 CAMI+ versus CAMI | 1 | 167 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.77 [0.33, 1.78] |
| 1.2 CAMI versus usual care | 1 | 155 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.63 [0.29, 1.37] |
Comparison 17. Theory‐based video versus control video.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Any LARC initiation (immediate) | 1 | 191 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.37 [0.77, 2.43] |
| 2 LARC initiation by type (immediate) | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 2.1 LNG‐IUS | 1 | 191 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.35 [0.75, 2.43] |
| 2.2 Implant | 1 | 191 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.99 [0.41, 2.40] |
| 2.3 Copper IUD | 1 | 191 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.17 [0.38, 3.61] |
Comparison 18. Computer‐assisted motivational intervention versus didactic counseling.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Unprotected sex | Other data | No numeric data |
Comparison 19. Pregnancy prevention education versus no education.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Contraceptive use and attitudes at 6 months | Other data | No numeric data | ||
| 2 Contraception knowledge at post‐test | Other data | No numeric data |
Comparison 20. Multiple risk reduction: group youth + parent programs.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Been pregnant or gotten someone pregnant, self report (at 24 months) | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.1 Youth + parent vs youth | 1 | 353 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.24 [0.10, 0.56] |
| 1.2 Youth + parent vs youth + parent + booster session | 1 | 295 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.27 [0.11, 0.66] |
| 2 Used contraception at last sex (at 24 months) | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 2.1 Youth + parent vs youth | 1 | 337 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.35 [0.81, 2.25] |
| 2.2 Youth + parent vs youth + parent + booster session | 1 | 282 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.72 [0.43, 1.21] |
| 3 Used condom at last sex (at 24 months) | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 3.1 Youth + parent vs youth | 1 | 334 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.25 [0.76, 2.04] |
| 3.2 Youth + parent vs youth + parent + booster session | 1 | 279 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.92 [0.53, 1.61] |
20.2. Analysis.
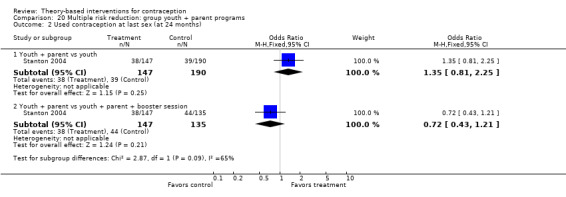
Comparison 20 Multiple risk reduction: group youth + parent programs, Outcome 2 Used contraception at last sex (at 24 months).
20.3. Analysis.
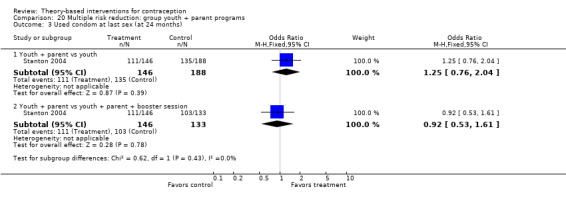
Comparison 20 Multiple risk reduction: group youth + parent programs, Outcome 3 Used condom at last sex (at 24 months).
Comparison 21. Counseling + phone calls versus counseling versus standard care.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Consistent OC use: counseling + phone versus counseling | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.1 At 3 months | 1 | 767 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.41 [1.06, 1.87] |
| 1.2 At 6 months | 1 | 767 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.39 [1.03, 1.87] |
| 1.3 At 12 months | 1 | 767 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.12 [0.78, 1.61] |
| 2 Consistent OC use: counseling versus standard care | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 2.1 At 3 months | 1 | 771 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.81 [0.61, 1.07] |
| 2.2 At 6 months | 1 | 771 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.78 [0.58, 1.05] |
| 2.3 At 12 months | 1 | 771 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.89 [0.62, 1.27] |
| 3 Dual‐method use: counseling + phone versus counseling | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 3.1 At 3 months | 1 | 767 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.38 [0.87, 2.18] |
| 3.2 At 6 months | 1 | 767 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.49 [0.85, 2.62] |
| 3.3 At 12 months | 1 | 767 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.00 [0.51, 1.95] |
| 4 Dual‐method use: counseling versus standard care | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 4.1 At 3 months | 1 | 771 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.79 [0.50, 1.26] |
| 4.2 At 6 months | 1 | 771 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.78 [0.44, 1.40] |
| 4.3 At 12 months | 1 | 771 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.75 [0.40, 1.40] |
| 5 Condom use at last sex: counseling + phone versus counseling | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 5.1 At 3 months | 1 | 767 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.45 [1.03, 2.03] |
| 5.2 At 6 months | 1 | 767 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.30 [0.86, 1.98] |
| 5.3 At 12 months | 1 | 767 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.93 [0.55, 1.57] |
| 6 Condom use at last sex: counseling versus standard care | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 6.1 At 3 months | 1 | 771 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.91 [0.64, 1.29] |
| 6.2 At 6 months | 1 | 771 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.90 [0.59, 1.38] |
| 6.3 At 12 months | 1 | 771 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.01 [0.60, 1.70] |
| 7 Pregnancy (by 12 months) | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 7.1 Counseling + phone versus counseling | 1 | 767 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.80 [0.53, 1.18] |
| 7.2 Counseling versus standard care | 1 | 771 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.39 [0.93, 2.09] |
| 8 Would recommend OC use to a friend: counseling + phone versus counseling | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 8.1 At 3 months | 1 | 623 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.52 [1.11, 2.09] |
| 8.2 At 6 months | 1 | 545 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.68 [1.20, 2.36] |
| 8.3 At 12 months | 1 | 432 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.13 [0.75, 1.68] |
| 9 Would recommend OC use to a friend: counseling versus standard care | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 9.1 At 3 months | 1 | 625 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.78 [0.57, 1.07] |
| 9.2 At 6 months | 1 | 538 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.65 [0.46, 0.91] |
| 9.3 At 12 months | 1 | 427 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.82 [0.55, 1.23] |
Comparison 22. Theory‐based iOS app versus usual care.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 LARC selection by 1 month | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.1 All LARC | 1 | 52 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.27 [0.34, 4.67] |
| 1.2 IUC | 1 | 52 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.79 [0.56, 5.66] |
Comparison 23. Pregnancy prevention program versus usual life skills program.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Dichotomous outcomes (8 months after baseline) | Other data | No numeric data | ||
| 2 Scale outcomes (8 months after baseline) | Other data | No numeric data |
Comparison 24. Social and behavioral change model (gender equity + FP) versus delayed intervention.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Use of modern contraceptive methods at 2 months | Other data | No numeric data | ||
| 2 Knowledge of modern contraceptive methods (women at 2 months | Other data | No numeric data | ||
| 3 Knowledge of modern contraceptive methods (men at 2 months | Other data | No numeric data |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Barnet 2009.
| Methods | Design: individually randomized Location: Baltimore, MD (USA) Time frame: recruitment February 2003 to April 2005 Sample size calculation (and outcome of focus): no mention |
|
| Participants | General with N: 237 pregnant adolescents Source: 5 prenatal care clinics serving low‐income, mainly African American communities Inclusion criteria: 12 to 18 years old; pregnancy ≥ 24 weeks gestation Exclusion criteria: pregnancy did not result in live birth and withdrawn if infant died in neonatal period, since parenting was intervention focus | |
| Interventions | Study focus: prevent rapid repeat births Theory or model: Transtheoretical model for computer‐assisted motivational intervention (CAMI); motivational interviewing on contraception by CAMI counselors; Social Cognitive Theory for parenting curriculum from Black 2006 (included contraception)
Duration: from 6 weeks postpartum to 24 months postpartum; maximum 9 quarterly sessions |
|
| Outcomes | Primary: repeat birth by 24 months postpartum; abortion since index child's birth
Secondary: not applicable (NA) Follow‐up: 24 months Additional data provided by investigator: losses by arm to help interpret abortion information from 24‐month interview |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomly assigned, 'computer‐generated permuted blocks'. Investigator communicated ratio was 3:3:2; with 6 used for intervention groups and 4 for control. Block size of 16 would account for ratio rather than block size of 6 reported in paper. |
| Allocation concealment (selection bias) | Unclear risk | No mention |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Presume no blinding of participants; not feasible due to type of intervention |
| Blinding of outcome assessment (detection bias) | Unclear risk | No mention |
| Outcome measures | Low risk | Repeat birth assessed via Vital Statistics |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Loss to follow‐up: 19% overall loss; group losses 17% CAMI+, 16% CAMI‐only, 24% usual care Investigator provided losses by study arm (counts and %) at 24‐month interview Exclusions after randomization: 1 participant with stillborn infant and 1 whose 2‐month old infant died If participant became pregnant, CAMI stopped because questions on contraception no longer relevant; program did not allow skipping |
| Other bias | Unclear risk | Analysis for cluster randomized trial: NA |
Berenson 2012.
| Methods | Design: individually randomized Location: southeast Texas (USA) Time frame: enrollment from July 2006 to January 2010 Sample size calculation (and outcome of focus): N = 190 in each group (570 total) for 90% power to detect OR of 2.0 for oral contraceptive (OC) continuation after 12 months |
|
| Participants | General with N: 1155 women; 16 to 24 years of age Source: 5 public reproductive health clinics in southeast Texas serving low income women Inclusion criteria: sexually active; non‐pregnant; 16 to 24 years old; requesting OC initiation Exclusion criteria: desire to become pregnant in next year; medical contraindication to OC; current or prior (> 1 month) OC use |
|
| Interventions | Study focus: increasing contraceptive adherence as well as dual‐method use to prevent STI and pregnancy. Theory or model: health belief model
Duration: 6‐month intervention |
|
| Outcomes | Primary: OC adherence (consistent OC use); dual‐method use (consistent OC use and consistent condom use); condom use at last sex (if inconsistent condom user); pregnancy Secondary: NA Follow‐up: by telephone at 3, 6 12 months |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomization scheme (PLAN procedure, SAS Institute) |
| Allocation concealment (selection bias) | High risk | When asked about concealment before assignment, investigator communicated that they did not conceal from researchers but did conceal from participants |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Presume no blinding of participants; not feasible due to type of intervention |
| Blinding of outcome assessment (detection bias) | Low risk | Staff who made assessment phone calls were blinded to intervention group |
| Outcome measures | Unclear risk | Pregnancy by self‐report and medical record review (low risk); contraceptive use by self‐report (high risk) |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Loss to follow‐up by 12 months: 44% counseling, 43% counseling + phone, and 45% standard care. |
| Other bias | Unclear risk | Analysis for cluster randomized trial: NA |
Black 2006.
| Methods | Design: individually randomized Time frame: recruitment September 1997 through December 1999 Location: Baltimore, MD (USA) Sample size calculation (and outcome of focus): no mention |
|
| Participants | General with N: 181 adolescents Source: 3 urban hospitals Inclusion criteria: low income (< 185% poverty level); < 18 years old; first‐time delivery; black race; no indication of cocaine or heroin use in chart; no chronic illness that would interfere with parenting or adolescent development; infant was term (≥ 37 weeks) and > 2500 g; infant had no congenital problem, chronic illness, or disability | |
| Interventions | Study focus: delaying second births; parenting, contraception Theory or model: primarily Social Cognitive Theory
Duration: maximum of 19 visits for intervention group at 2 per month |
|
| Outcomes | Primary: second birth (not pregnancy); contraceptive use (report presented by second birth rather than randomized group)
Secondary: NA Follow‐up assessments: 6, 13, 24 months |
|
| Notes | 2008: unable to obtain information from investigator about contraceptive use by study arm | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | 'Randomization procedure' stratified on maternal age and child's gender |
| Allocation concealment (selection bias) | Unclear risk | No mention |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Presume no blinding of participants; not feasible due to type of intervention |
| Blinding of outcome assessment (detection bias) | Unclear risk | No mention |
| Outcome measures | Unclear risk | Second birth assessed at home visit (low risk); contraceptive use reported by second birth and not randomized group (high risk) |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Loss to follow‐up: overall, 18%; by group, intervention 20% (17/87); control 16% (15/94) Exclusions after randomization: excluded from analysis 32 mothers who did not have 24‐month evaluation (17 treatment and 15 control), because intent was to assess second births. May have had 6‐month or 13‐month evaluations. |
| Other bias | Unclear risk | Analysis for cluster randomized trial: NA |
Boyer 2005.
| Methods | Cluster randomized trial: platoons were assigned to study groups. Number of platoons not specified (likely about 30, given 50 to 75 recruits in each platoon and overall sample size) Location: most likely California and South Carolina (USA) Time frame: recruitment June 1999 to June 2000 Sample size calculation (and outcome of focus): originally 477 per group to assess decreasing STI by 6%. Increased to 568 per group to address cluster effect, then increased to 1000 per group since half of participants would be stationed where STI and pregnancy screening not be possible at follow‐up. |
|
| Participants | General with N: 2157 women Inclusion criteria: female Marine recruits in training Exclusion criteria: no mention | |
| Interventions | Study focus: preventing STI and unplanned pregnancy Theory or model: Information‐motivation‐behavioral (IMB) skills model
Duration: 12‐week intervention |
|
| Outcomes | Primary: unplanned pregnancy (tested); frequency of condom use; frequency of contraceptive use
Secondary: NA Follow‐up: 14 months after baseline |
|
| Notes | Additional data from investigator: number of events and group size for pregnancy and condom use | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random numbers table established before study start |
| Allocation concealment (selection bias) | Low risk | Platoons identified prior to randomization; female Marine recruits in platoons eligible |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Platoons informed of group assignment after enrollment and baseline assessment; blinding not feasible due to type of intervention |
| Blinding of outcome assessment (detection bias) | Unclear risk | No mention |
| Outcome measures | Unclear risk | Unplanned pregnancy by test; contraceptive use by self‐report |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Loss to follow‐up: 38% loss for questionnaire data and 59% loss for pregnancy data (due to deployments); study groups were similar. |
| Other bias | Low risk | Analysis for cluster randomized trial: robust standard errors using Huber‐White sandwich estimator in regression models. Independent variables were intervention group, sexual history, and time between assessments. |
Ceperich 2011.
| Methods | Design: individually randomized Location: Richmond VA (USA) Time frame: no date; recruiting via mailings and posted flyers on campus and in student health center Sample size calculation (and outcome of focus): no mention |
|
| Participants | General with N: 228 female students at urban university Inclusion criteria: 18 to 24 years old; at risk for alcohol‐exposed pregnancy, i.e. had sex with man in past 90 days, use contraception ineffectively (none, incorrect use of effective method, or use of ineffective method), and drinking at risk levels, i.e. ≥ 5 drinks per occasion in past 90 days or ≥ 8 drinks per week on average Exclusion criteria: no mention | |
| Interventions | Study focus: reducing alcohol‐exposed pregnancy risk
Theory or model: motivational interviewing
Duration: 1 session or pamphlet |
|
| Outcomes | Primary: ineffective contraceptive use
Secondary: NA Follow‐up assessments: 1 and 4 months |
|
| Notes | In 2008, investigator communicated that "ineffective methods" included those with high pregnancy rates, such as withdrawal, "natural family planning," and spermicide only | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No mention |
| Allocation concealment (selection bias) | Low risk | Closed envelope |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | After assessment, counselor opened allocation envelope and provided counseling intervention or information‐only condition. Presume no blinding of participants; not feasible due to type of intervention |
| Blinding of outcome assessment (detection bias) | High risk | Questionnaires mailed to participants |
| Outcome measures | High risk | Contraceptive use by self‐report |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Loss to follow‐up: 9% overall; by group, intervention 11% (13/114), control 7% (8/114) |
| Other bias | Unclear risk | Analysis for cluster randomized trial: NA |
Coyle 2001.
| Methods | Design: cluster randomized trial; 20 schools assigned to study groups Location: southeast Texas and northern California, USA Time frame: 1993 to 1996 Sample size calculation (and outcome of focus): no information |
|
| Participants | General with N: 20 public schools; 3869 students in grade 9 Inclusion criteria: school districts served diverse populations (ethnicity and socioeconomic status); areas with high HIV prevalence; close to research team Exclusion criteria: no information | |
| Interventions | Study focus: prevention of HIV, STI, and pregnancy for high school youth Theory or model: Social Cognitive Theory + social influence model and models of school change
Duration: 2‐year program |
|
| Outcomes | Primary: frequency of unprotected sex; condom use during last sex; use of effective contraception during last sex (i.e. condom, birth control pills, or both)
Secondary: attitudes about sex or condom use; HIV/STD knowledge; beliefs; self efficacy; barriers to condom use; HIV/STD risk perceptions Follow‐up: 7 months, i.e. after year 1 lessons (9th grade); 19 months, i.e. after year 2 lessons (10th grade); 31 months, i.e. 12 months after year 2 lessons |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Restricted randomization process to assign schools: schools ranked on index of possible confounders, and adjacent schools in ranking paired and randomly assigned to intervention or control |
| Allocation concealment (selection bias) | Unclear risk | Schools identified prior to randomization. All students in identified grades were eligible. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Presume no blinding of participants or providers; not feasible due to type of intervention |
| Blinding of outcome assessment (detection bias) | High risk | No mention |
| Outcome measures | High risk | Contraceptive use from self‐report |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Loss to follow‐up: 19 months, 17% (immediately after year 2); 31 months, 21% (12 months after year 2) Exclusions after randomization: 346 students left year 1 and did not enroll in Fall year 2; 95 took baseline survey but were grade 11 or 12 |
| Other bias | Unclear risk | Analysis for cluster randomized trial: multilevel models (levels measurement occasion, student, and school); predictor variables, i.e. baseline responses on outcomes, intervention group, geographic area, and "outcome specific covariates" (related to outcome and intervention; unspecified) |
Coyle 2006.
| Methods | Design: cluster randomized trial; 24 schools assigned to intervention or control Location: northern California, USA Time frame: recruited 2000 to 2001 Sample size calculation (and outcome of focus): no information |
|
| Participants | General with N: 24 alternative day schools; 988 students (ages 14 to > 18 years) Inclusion criteria: 4 counties with ethnic diversity and in close proximity to investigators; all enrolled students (generally had severe discipline issues, substance use, or chronic absenteeism) Exclusion criteria: students on extended leave (e.g. maternity or medical); suspended or incarcerated at baseline; functionally dropped out of school | |
| Interventions | Study focus: Prevention of HIV, STI, and pregnancy Theory or model: Social Cognitive Theory + Theory of Planned Behavior (+ earlier Theory of Reasoned Action)
|
|
| Outcomes | Primary: frequency of sex without condom in past 3 months, condom use with last sex, use of effective birth control, pregnancy (self‐report)
Secondary: attitude toward condoms (general, protecting against STDs or pregnancy); knowledge of condoms or HIV and condoms; self efficacy Follow‐up: 6, 12, and 18 months after baseline (about 5, 11, and 17 months postprogram) |
|
| Notes | Report provided effect estimates but not means or frequencies per study group; unable to obtain further information from investigator. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Restricted randomization: schools put into matched sets, matched groups formed with set from each county, and matched groups randomized |
| Allocation concealment (selection bias) | Unclear risk | Schools identified prior to randomization. All students in schools were eligible. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Presume no blinding of participants or providers; not feasible due to type of intervention |
| Blinding of outcome assessment (detection bias) | Unclear risk | No mention |
| Outcome measures | High risk | Self‐report of contraceptive use and pregnancy |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Loss to follow‐up: after baseline 6 months, 27% (immediately postprogram); 12 months, 38% (6 months postprogram); 18 months, 44% (12 months postprogram) Loss by group not reported |
| Other bias | High risk | Analysis for cluster randomized trial: multilevel models (levels student and school); psychosocial outcomes also had survey measurement occasion Predictor variables in models: baseline responses on outcome, intervention group, and “outcome specific covariates” (related to outcome and intervention; unspecified) Analysis of behavioral outcomes based on who had sex (could be affected by intervention), rather than all randomized (high risk) |
Davidson 2015.
| Methods | Design: individually randomized Location: Chicago, IL (USA) Time frame: June to September 2013 Sample size calculation (and outcome of focus): assumed LARC initiation immediately after abortion at 6% control and 21% intervention. To detect 15% increase in LARC initiation (from 6% to 21%) using 2‐sided alpha P = 0.05 and 80% power, 188 subjects needed (94 each arm). Due to protocol violations by interim analysis, recruited 5 additional participants |
|
| Participants | General with N: 191 participants (96 intervention; 95 control)
Inclusion criteria: English‐speaking women 18 to 29 years old; presenting for surgical abortion; not desiring pregnancy in next 12 months Exclusion criteria: nonviable or anomalous pregnancy; pregnancy as result of sexual assault; not English‐speaking |
|
| Interventions | Study focus: pregnancy prevention; initiate LARC after abortion Theory or model: Transtheoretical model (assumed most women seeking abortion in precontemplation or contemplation for LARC)
|
|
| Outcomes | Primary: initiation of LARC Secondary: NA Follow‐up: NA; immediately after abortion |
|
| Notes | Not included in this review: satisfaction (and perceived autonomy) survey regarding usual care counseling for both groups (5 items); groups did not differ significantly | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomization (random.org); 1:1 allocation and blocks of 10 |
| Allocation concealment (selection bias) | Low risk | Sequence entered into software (RedCap), which automatically randomized following baseline survey |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Counselors and clinicians blinded to study arm allocation Presume no blinding of participants; not feasible due to type of intervention |
| Blinding of outcome assessment (detection bias) | Low risk | No mention; initiation of LARC from medical records |
| Outcome measures | Low risk | Contraceptive method selection from chart review |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Loss to follow‐up: NA; method initiation assessed on same day as procedure Excluded after randomization: 1 did not have abortion and 1 ineligible due to age |
| Other bias | Unclear risk | Analysis for cluster randomized trial: NA |
Floyd 2007.
| Methods | Design: individually randomized Location: Florida, Virginia, and Texas (USA) Time frame: recruited July 2002 through January 2004 Sample size calculation (and outcome of focus): N = 60 in each group to detect 30% difference in reduction of problem drinking |
|
| Participants | General with N: 830 women; age 18 to 44 years; at risk for alcohol‐exposed pregnancy Sources: primary care practices; jails; drug and alcohol treatment centers; hospital‐based gynecology clinic; Medicaid health maintenance organization; and media‐recruited sample Inclusion criteria: 18 to 44 years old; no condition causing infertility; not pregnant or planning to get pregnant in 9 months; had vaginal sex in past 3 months (or 3 months prior to jail) with non‐sterile male and without using effective contraception; engaged in risky drinking (≥ 5 drinks in a day or on average ≥ 8 drinks per week); available for follow‐up Exclusion criteria: no mention | |
| Interventions | Study focus: change one or both of the target behaviors, i.e. risky drinking and ineffective contraceptive use Theory or model: motivational interviewing (MI) and Transtheoretical Model (TTM)
Duration: 14 weeks with sessions 2 to 3 weeks apart |
|
| Outcomes | Primary: ineffective contraception use (vaginal sex without contraception or with ineffective contraception, i.e. reported deviation from published guidelines for method use)
Secondary: NA Follow‐up assessments: 3, 6, and 9 months |
|
| Notes | 2016 article by Parrish examined mechanisms of treatment effect | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Data coordinating center used randomization program to generate unique IDs for each site; equal number in each study group |
| Allocation concealment (selection bias) | Low risk | Sequentially‐numbered, sealed, opaque envelopes |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Presume no blinding of participants; not feasible due to type of intervention |
| Blinding of outcome assessment (detection bias) | Low risk | Follow‐up interviews conducted by staff blinded to group assignment |
| Outcome measures | High risk | Contraceptive use from self‐report |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Loss to follow‐up: 29% overall; 30% treatment and 27% control |
| Other bias | Unclear risk | Analysis for cluster randomized trial: NA |
Gilliam 2014.
| Methods | Design: individually randomized Location: Chicago, IL (USA) Time frame: after March 2013 (app usability testing and IRB approval) Sample size calculation (and outcome of focus): 60 chosen to detect increase of 10% (baseline) to 45% (app intervention) in proportion expressing interest in discussing LARC method during visit; 80% power and 2‐sided alpha = 0.05 |
|
| Participants | General with N: 60 women
Inclusion criteria: sexually experienced; English‐speaking women, age 15 to 30 years, presenting for contraceptive services at Chicago Title X clinic Exclusion criteria: currently pregnant; desiring pregnancy within next 12 months; currently using LARC; scheduled for LARC‐related visit; reliance on male partner sterilization for contraception |
|
| Interventions | Study focus: pregnancy prevention; selection of LARC Theory or model: human‐centered design and Theory of Planned Behavior
|
|
| Outcomes | Primary: contraceptive method selected Secondary: NA Follow‐up assessment: 1 month (chart review) |
|
| Notes | Contraceptive knowledge and interest in LARC methods not comparative; pre‐post for intervention group and only at baseline for standard care group | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomization (random.org) |
| Allocation concealment (selection bias) | Low risk | Sequentially numbered opaque envelopes |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Clinic counselors and clinicians blinded to treatment assignment Presume no blinding of participants; not feasible due to type of intervention |
| Blinding of outcome assessment (detection bias) | Unclear risk | No mention; data managed with electronic capture tools (RedCap) |
| Outcome measures | Low risk | Chart review for method selected (1 month after visit) and how provided (dispensed directly, prescribed, referred for follow‐up) |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Loss to follow‐up: none (1‐month chart review) Exclusions after randomization: 3 intervention and 7 control (missing or ineligible age, current implant use, desiring pregnancy, appointment for IUC insertion) |
| Other bias | Unclear risk | Analysis for cluster randomized trial: NA |
Gold 2016.
| Methods | Design: RCT with multi‐site recruitment strategy Location: Pittsburgh PA (USA) Time frame: February 2003 to September 2006 Sample size calculation (and outcome of focus): no mention |
|
| Participants | General with N: 572 female adolescents
Inclusion criteria: 13 to 21 years old; access to telephone; able to sign consent form Exclusion criteria: non‐English speaker; unable to read at sixth‐grade level; blind or visually impaired; another communication barrier; living in group or foster home; currently, or trying to get, pregnant; engaging in exclusively same‐gender sex; IUD or contraceptive implant in place; being sterile |
|
| Interventions | Study focus: decrease unprotected sex and STI Theory or model: Transtheoretical model (TTM) using stages of change, decisional balance, situational self‐efficacy and process of change constructs; motivational interviewing (MI) as counseling strategy
|
|
| Outcomes | Primary: self‐reported rating scales of acceptability and feasibility of CAMI intervention Secondary: unprotected sex (any sex without condom) Follow‐up: 9 months after baseline |
|
| Notes | Investigator communicated that CAMI contraceptive content was tailored based on participant request. Counselors could provide detailed information on specific methods (content similar to DEC) when participants requested it or were offered it and accepted offer. Offered participants pamphlets on all contraceptive methods at all 3 sessions. CAMI content on contraception was shorter than DEC but would expand if participant asked questions or requested more information. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No mention of generation; stratified according to age, race, and sexually active (ever) |
| Allocation concealment (selection bias) | Unclear risk | No mention |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Open according to ClinicalTrials.gov listing; blinding not feasible due to type of intervention |
| Blinding of outcome assessment (detection bias) | Unclear risk | No mention |
| Outcome measures | High risk | Self‐report: sex without condom or not; self‐reported follow‐back calendar |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Loss to follow‐up: CAMI 45% (128/286); control (DEC) 34% (96/286) |
| Other bias | Unclear risk | Analysis for cluster RCT: NA |
Kirby 2010.
| Methods | Design: individually randomized Location: San Francisco, CA (USA) Sample size calculation (and outcome of focus): 80% chance of finding 10% difference in proportion of women who used hormonal contraception for 6 months or longer |
|
| Participants | General with N: 805 females; 14 to 18 years old Source: reproductive health clinic for adolescents and young adults Inclusion criteria: not pregnant or trying to become pregnant; had sex in last 3 months; no consistent hormonal contraception for 3 months and no IUD or contraceptive implant Exclusion criteria: no mention | |
| Interventions | Study focus: improve contraceptive use, reduce unintended pregnancy and STI Theory or model: motivational interviewing, which investigators claimed was built on Health Belief Model
Duration: 12 months |
|
| Outcomes | Primary: hormonal contraceptive use at last sex, condom use at last sex, self‐reported pregnancy
Secondary: NA Follow‐up assessments: 6, 12, 18 months |
|
| Notes | Additional data from investigator: pregnancy rates by group; effect sizes and P values for outcomes without details in report. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number generator; participants were stratified by age |
| Allocation concealment (selection bias) | Unclear risk | No mention |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | None; not feasible due to type of intervention |
| Blinding of outcome assessment (detection bias) | Low risk | Outcome assessor blinded |
| Outcome measures | High risk | Self‐report of contraceptive use and pregnancy |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Loss: based on completed surveys; at 6 months, 22%; 12 months, 26%; 18 months, 25%; reportedly did not differ by group Report does not provide numbers per group at each assessment. |
| Other bias | Unclear risk | Analysis for cluster randomized trial: NA Investigator communicated that analysis involved multiple linear and logistic regression repeated measures, and included adjustments for differences between groups. |
Markham 2012.
| Methods | Design: cluster randomized trial; 15 urban middle schools assigned, 5 to each condition Location: south‐central USA (most investigators based in Houston, TX) Time frame: conducted 2006 to 2010 Sample size estimation and outcome of focus: assumed 15% controls would initiate sex by grade 9, 25% attrition, intra‐school correlations = 0.005, and alpha = 0.05 (two‐tailed); initial sample size 1500 grade 7 students estimated, 80% power to detect 10% pair‐wise differences in sexual initiation between intervention and control conditions at grade 9 follow‐up; recruited to reach quota of 100 students per school |
|
| Participants | General with N: 15 schools; 1742 students Inclusion criteria: grade 7 students in study schools Exclusion criteria: no information |
|
| Interventions | Study focus: reduce risk for adolescent pregnancy and STI/HIV transmission through sexual risk avoidance and risk reduction Theory or model: Social Cognitive Theory and Theory of Planned Behavior 24 sessions of 50 minutes each (12 session grade 7 and 12 sessions grade 8); based on middle‐school program (Tortolero 2010) 1. Risk avoidance (RA): focused on abstinence until marriage 2. Risk reduction (RR): addressed abstinence until older; had activities regarding condom use and contraception use and on advantages and limitations of various contraceptive methods 3. Comparison (C): usual health classes that varied by school |
|
| Outcomes | Primary: delayed sexual initiation for those with no sexual experience Secondary: delayed oral, vaginal, and anal sex specifically; reduced sexual risk (no sex without condom; fewer partners); general condom knowledge; belief about condoms; intent to use condoms Audio‐computer‐assisted self‐interview Follow‐up: 9th grade (2012 report), about 3 months postprogram; October to July of 10th grade (2014 report), > 15 months postprogram |
|
| Notes | Investigator provided information about contraceptive methods addressed in curriculum (see Tortolero 2010) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Multi‐attribute randomization protocol accounting for school size, racial and ethnic composition, and geographic location |
| Allocation concealment (selection bias) | Unclear risk | Schools assigned and randomized; all 7th grade students were eligible |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Presume no blinding of participants or providers; not feasible due to type of intervention |
| Blinding of outcome assessment (detection bias) | Unclear risk | No information; audio‐computer‐assisted self‐interview |
| Outcome measures | High risk | Contraceptive use from self‐report |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Loss to follow‐up: 3 months (9th grade) RA 27%, RR 26%, C 21%; 10th grade follow‐up RA 27%, RR 31%, C 30% |
| Other bias | Low risk | Analysis for cluster randomized trial: non‐response weighting due to nonrandom attrition; generalized linear models with covariates (gender, race or ethnicity, age at baseline, family structure, time between measures, school‐level sexual experience at baseline, and baseline measure for psychosocial outcomes); estimated standard errors adjusted for intraclass correlation via random‐effects models |
Peipert 2008.
| Methods | Design: individually randomized Location: Rhode Island (USA) Time frame: recruitment October 1999 to October 2003 Sample size calculation (and outcome of focus): N = 250 in each group to detect two‐fold increase in dual‐method use and 50% difference in unintended pregnancy |
|
| Participants | General with N: 542 women Source: primary care and family planning clinics Inclusion criteria: 13 to 35 years old; sex with man in past 6 months; desire to avoid pregnancy for 24 months; if age 25 to 35 years, then high‐risk history (unplanned pregnancy, STI, inconsistent contraception use, > 1 sex partner in past 6 months, drug or alcohol abuse) Exclusion criteria: currently using dual methods of contraception consistently and correctly | |
| Interventions | Study focus: STI and pregnancy prevention Theory or model: Transtheoretical model
Duration: depended on study arm |
|
| Outcomes | Primary: dual‐method use (hormonal + barrier; male condoms + female condoms; condoms + spermicide; intrauterine device + barrier); consistent condom use; unplanned pregnancy (tested)
Secondary: NA Follow‐up: 6 and 18 months by phone; 12‐ and 24‐month visits (only 24‐month outcomes reported) |
|
| Notes | Secondary article in 2011 reported on 'sustained' use of dual methods (reported use ≥ 2 follow‐up interviews). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer program; stratified by site and contraceptive use |
| Allocation concealment (selection bias) | Unclear risk | Computer allocated women after collecting baseline information; separate from executor of assignment (phone interviewer and nurse doing exams) |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Presume no blinding of participants; may not have been feasible due to type of intervention |
| Blinding of outcome assessment (detection bias) | Low risk | Follow‐up evaluators 'masked' to allocation as far as possible |
| Outcome measures | High risk | Contraceptive use from self‐report |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Loss to follow‐up: 26% by 24 months (groups had similar losses) 2011 paper: N = 463; 15% had no follow‐up data |
| Other bias | Unclear risk | Analysis for cluster randomized trial: NA Relative risk adjusted for education, substance use, contraceptive use at baseline, stages of change |
Petersen 2007.
| Methods | Design: individually randomized Location: North Carolina (USA) Time frame: enrollment March 2003 to September 2004 Sample size calculation (and outcome of focus): N = 1050 to measure improvements in level of contraceptive use (with 10% loss = 948) |
|
| Participants | General with N: 764 women visiting clinics Source: 3 primary care clinics serving "numerous" counties Inclusion criteria: 16 to 44 years old; at risk of unintended pregnancy (not pregnant and not planning to get pregnant, not using an IUD, and neither woman or her partner sterilized) Exclusion criteria: no mention | |
| Interventions | Study focus: pregnancy and STI prevention counseling Theory or model: motivational interviewing
Duration: 2 treatment sessions and 1 control session |
|
| Outcomes | Primary: contraceptive use improved (nonuser to high or low level, or low level to high), maintained at high level or improved to maintain highest level, or decreased (high to low level, low to nonuse, or maintained at low level or nonuse); consistent condom use; pregnancy (tested)
Secondary: NA Follow‐up assessment: 2, 8, 12 months |
|
| Notes | Additional data provided by investigator: number that completed each follow‐up by study arm (flow diagram of trial participants); pregnancy data by study arm | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random‐numbers table; permuted blocks of 100 |
| Allocation concealment (selection bias) | Low risk | Sealed envelopes (no other detail) |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Presume no blinding of participants; not feasible due to type of intervention |
| Blinding of outcome assessment (detection bias) | Unclear risk | No mention |
| Outcome measures | Unclear risk | Contraceptive use from self‐report; pregnancy tested but no data provided (no significant difference) |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Loss to follow‐up: overall 13% at 12 months (groups were the same) Exclusions after randomization: none apparent; analysis reportedly included 737 with complete follow‐up data |
| Other bias | Unclear risk | Analysis for cluster randomized trial: NA |
Raj 2016.
| Methods | Design: cluster randomized Location: rural areas of Thane district in Maharashtra, India Time frame: March to December 2012 Sample size calculation (and outcome of focus): based on use of modern contraceptive and communication methods; assuming baseline 1000 couples equally distributed across 50 clusters (25 intervention and 25 control); assuming 80% retention by 18‐month follow‐up; needed 800 men. Based on 2‐sided logistic regression with significance level 0.05. Adjusted for design effect to account for correlation of subjects in same village; assuming 20 men enrolled in each village and within‐village correlation 0.10, design effect estimated as 2.9 For modern contraceptive use, 80% power to detect difference as small as 12% between groups (if control is 8%, 10%, or 12% when intervention is 20%, 22%, or 25%) |
|
| Participants | General with N: 1081 couples from 50 geographic clusters
Inclusion criteria for clusters: geographically distinct with natural borders; sufficient distance from other clusters to reduce contamination risk; proximity to public and private health services Inclusion criteria for households: husband 18 to 30 years of age and wife; fluent in Marathi (native language in Maharashtra); residing together for past 3 months with no intention to relocate in next 2 years; both members consent Exclusion criteria: couples reporting infertility, surgical sterilization or exhibiting serious cognitive or health impairment |
|
| Interventions | Study focus: pregnancy prevention Theory or model: Social Cognitive Theory; Theory of Gender and Power
|
|
| Outcomes | Primary: use of modern contraceptive method in past 3 months (pills, IUD, injectable, male or female condoms, or male or female sterilization); pregnancy self‐report (9 and 18 months) and test (18 months) Secondary: NA Follow‐up: 9 and 18 months |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | From 62 geographic clusters of approximately equal size, 50 selected based on ease of reach; randomized using computer‐generated numbers |
| Allocation concealment (selection bias) | Unclear risk | Not specified; research team randomized clusters on 1 day in month prior to enrollment initiation Households within each cluster were screened sequentially for eligibility, unmasked to treatment condition |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Neither participants nor staff masked to treatment condition; not feasible due to type of intervention |
| Blinding of outcome assessment (detection bias) | Unclear risk | No mention; research staff collected data on tablet computers using MSHARE |
| Outcome measures | High risk | Pregnancy: self‐report at 9 and 18 months; combined self‐report and urine (HCG) test results at 18 months Contraceptive use: self‐report |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Loss to follow‐up: 9 months, 16% intervention and 17% control; 18 months, 15% intervention and 19% control No withdrawals from study |
| Other bias | Low risk | Analysis: generalized linear mixed models with cluster as random effect; adjusted for wife's age and education, caste or tribe, number of living sons and of living daughters, pregnancy intent (contraceptive use only) |
Rendall‐Mkosi 2013.
| Methods | Design: individually randomized Location: Bergrivier Municipality, Western Cape, South Africa Time frame: recruited June to November 2007 Sample size calculation (and outcome of focus): anticipated reduction in prevalence for alcohol‐exposed pregnancy risk from 100% to 70% intervention and 90% control with power 0.80. Anticipated minimum 30 in each arm. Because recruitment easier than expected and needed greater power to detect effect size OR 2, continued to randomize 196 among 3 groups (Notes below) |
|
| Participants | General with N: 165 women Sources: primary care clinics and farms within study area Inclusion criteria: age 18 to 44 years; not pregnant; engaged in risky drinking over past 3 months (> 5 drinks at 1 sitting or > 7 drinks in 1 week); ineffective or no contraceptive use; no sterilization or hysterectomy; had vaginal sex in past 3 months; resided within 25‐km radius of main town Exclusion criteria: found to be pregnant |
|
| Interventions | Study focus: reduce risk of alcohol‐exposed pregnancy (AEP) Theory or model: Motivational interviewing (MI)
|
|
| Outcomes | Primary: ineffective contraception (not using any method, using ineffective method (any method other than OCs, injectable, IUC), or incorrect use of such methods) in past 3 months Secondary: NA Follow‐up: 3 and 12 months |
|
| Notes | Third arm for life‐skills arm: stopped after 30 in each group; poor adherence to intervention and difficulty with recruitment | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated |
| Allocation concealment (selection bias) | Low risk | Sealed envelopes to indicate random group allocation prepared in advance |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Presume no blinding of participants or providers; not feasible due to type of intervention |
| Blinding of outcome assessment (detection bias) | High risk | Report states difficult to blind field workers in rural community |
| Outcome measures | High risk | Contraceptive use by self‐report (face‐to‐face interview) |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Loss to follow‐up: 3 months, 30.5% MI and 27% control; 12 months, 26% MI and 23% control |
| Other bias | Unclear risk | Analysis for cluster randomized trial: NA |
Schinke 1981.
| Methods | Design: individually randomized Location: not specified; investigators based in Seattle, WA (USA) Time frame: no information Sample size calculation (and outcome of focus): no information |
|
| Participants | General with N: 36 students in public high school Inclusion criteria: sophomore class students Exclusion criteria: no information | |
| Interventions | Study focus: preventing adolescent pregnancy
Theory or model: cognitive and behavioral training; problem‐solving schema
Duration: 14 group sessions of 50 minutes each |
|
| Outcomes | Primary: "habitual contraception"; "greater protection at last intercourse"; "less reliance on inadequate birth control" (no definitions) Secondary: knowledge of pregnancy prevention (post‐test only); attitudes toward family planning Follow‐up: 6 months | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No mention |
| Allocation concealment (selection bias) | Unclear risk | No mention |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Presume no blinding of participants or providers; not feasible due to type of intervention |
| Blinding of outcome assessment (detection bias) | Low risk | Measures scored by 2 assistants not aware of study conditions or hypotheses |
| Outcome measures | High risk | Contraceptive use from self‐report Investigator communicated that contraceptive outcomes were based on reported behavior; did not request data due to age of study |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Loss to follow‐up: no mention |
| Other bias | Unclear risk | Analysis for cluster randomized trial: NA |
Schuler 2015.
| Methods | Design: cluster RCT; communities assigned Location: western highlands of Guatemala Time frame: workshops March to April 2012 Sample size calculation (and outcome of focus): no mention |
|
| Participants | General with N: 30 communities; 1122 participants completed baseline survey Inclusion criteria for communities: western highlands (5 departments); rural areas where APROFAM (international Planned Parenthood affiliate) provided mobile services and trained volunteers promoting reproductive health Inclusion criteria for participants: live in the community; be married or in civil union; wife 18 to 40 years of age; both members of couple agree to participate; supposed to be well known and respected in community and have good communication with others Exclusion criteria: no mention |
|
| Interventions | Study focus: intervention focus on improving gender attitudes and communication about reproductive health Theory or model: C‐Change social and behavioral change model
|
|
| Outcomes | Primary: gender attitudes (Gender and FP Equity Scale) Secondary: knowledge and use of modern contraceptive methods, i.e. tubal ligation, vasectomy, OCs, emergency contraceptive pills, IUDs, injectables, implants, male and female condoms and spermicide Follow‐up: 2 months after baseline |
|
| Notes | Manual adapted from Stepping Stones, Sakhi Saheli (Population Council), and EngenderHealth Men Investigator communicated that APROFAM implemented FP component using standard material; due to staffing changes, investigators did not have further information |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information on sequence generation; randomly assigned 9 communities from each of 5 departments to 3 study arms (later dropped 3rd arm, service statistics only) |
| Allocation concealment (selection bias) | Low risk | Communities identified prior to assignment; individuals within community were eligible if they met additional criteria |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No mention; blinding not feasible due to type of intervention |
| Blinding of outcome assessment (detection bias) | Unclear risk | No mention |
| Outcome measures | High risk | Self‐report of contraceptive use |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Loss to follow‐up: intervention 45% (269/597); control 44% (213/488) |
| Other bias | Unclear risk | Analysis for cluster RCT: logistic mixed model for contraceptive use and knowledge; models included random effects to account for community‐level randomization and repeated measures; study group and assessment time were fixed effects in model |
Sieving 2013.
| Methods | Design: individually randomized Location: Minneapolis and Saint Paul, MN (USA) Time frame: recruitment April 2007 to October 2008 Sample size calculation (and outcome of focus): no mention |
|
| Participants | General with N: 253 sexually active girls; 13 to 17 years old
Source: 4 school and community‐based clinics Inclusion: clinic visit with negative pregnancy test or treatment for STI; young age; high‐risk sexual and contraceptive behavior; aggressive and violent behavior; behavior indicating school disconnection (behavioral indicators from screening tool) Exclusion: did not understand consent material; married, pregnant, or had given birth |
|
| Interventions | Study focus: reduce pregnancy risk (sexual risk behavior, involvement in violence, school disconnection) Theory or model: SCT and resilience paradigm; principles of social connectedness used, but not cited as guiding theory or model
Duration: 18‐month intervention |
|
| Outcomes | Primary: contraceptive use consistency with most recent sex partner (condoms, hormonal, dual‐method (hormonal + condoms)). Consistency: months used method during sex (every time or most times); range 0 to 7 (past 6 months + current month) Secondary: desire to use contraception (1 item, later dichotomized) Follow‐up assessment: after 12 and 18 months of intervention; 24 months (6‐month follow‐up) Secondary paper (2014) reported months of consistent use in past 7 months; assessed at 30 months |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Investigator communicated they generated list of random numbers for each clinic. Teens were individually randomized within clinics. |
| Allocation concealment (selection bias) | High risk | Not used (investigator communication) |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Presume no blinding of participants; not feasible due to type of intervention |
| Blinding of outcome assessment (detection bias) | Unclear risk | No mention |
| Outcome measures | Low risk | Investigator communicated that "beliefs about birth control" not reported with final outcomes due to space limits and being non‐significant |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Loss: 6% overall (8% intervention and 3% control); 24 months 30 months 7% (18/253) |
| Other bias | Unclear risk | Analysis for cluster randomized trial: NA Models for contraceptive use and attitude: adjusted for baseline measure and clinic Contraceptive use outcomes: adjusted for same sexual partner as baseline and number months had sex with most recent partner |
Stanton 2004.
| Methods | Cluster randomized trial: communities assigned to study groups; 35 sites Location: Baltimore, MD (USA) Time frame: recruitment 1999 to 2000 Sample size calculation (and outcome of focus): no mention Report included intraclass correlation coefficients and number of clusters for use in calculating design effect |
|
| Participants | General with N: 817 youth; African American; 13 to 16 years old Source: low‐income housing developments, tenant associations and local recreation center staff Inclusion criteria: youth living in low‐income communities Exclusion criteria: no mention | |
| Interventions | Study focus: multiple risk reduction, including sexual risk
Theory or model: Protection Motivation Theory
Follow‐up: 6, 12, 18, and 24 months after intervention (only 24‐month data reported) |
|
| Outcomes | Primary: in past 6 months been pregnant or gotten girl pregnant (self‐report), used birth control during last sex (specify a method), or used condom during last sex Secondary: NA | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Use of a random numbers table |
| Allocation concealment (selection bias) | Unclear risk | Randomization of sites occurred after all youths in selected sites identified. All youths meeting inclusion criteria were eligible. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Presume no blinding of participants; not feasible due to type of intervention |
| Blinding of outcome assessment (detection bias) | Unclear risk | No mention |
| Outcome measures | High risk | Contraceptive use and pregnancy from self‐report |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Loss to follow‐up: 40%; groups ranged from 38% to 41% |
| Other bias | Low risk | Analysis for cluster randomized trial: reported intraclass correlation coefficients for each outcome and number of clusters. We calculated design effects, and then effective sample sizes, according to recommended methods (Higgins 2011). |
Taylor 2014.
| Methods | Design: cluster randomized trial; 16 high schools (urban and rural) allocated to conditions Location: KwaZulu‐Natal, South Africa Time frame: 2009 Sample size estimation and outcome of focus: no information |
|
| Participants | General with N: 16 high schools; 816 students Inclusion criteria: 2 of 11 districts (1 urban and 1 rural); 16 of 1580 high schools on Department of Education list; randomly selected grade 8 classes (1st year high school) Exclusion criteria: no information |
|
| Interventions | Study focus: teenage pregnancy prevention Theory or model: I‐Change model from 2005 (DeVries 2013); integration of ideas from Theory of Planned Behavior, Social Cognitive Theory, Transtheoretical Model, Health Belief Model, and goal setting theories
|
|
| Outcomes | Primary: been pregnant or caused pregnancy; condom use (any); condom use consistency as 4‐point scale from 1 (never) to 4 (always) Secondary: attitudes to teen pregnancy (pro and con scales); intent to prevent pregnancy and to use condoms Follow‐up: 4 months postprogram (8 months after baseline) |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No specifics on sequence generation: 16 of 1580 schools selected; geographical stratification; randomly allocated schools to groups |
| Allocation concealment (selection bias) | Unclear risk | Students invited from 1 randomly selected grade 8 class |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Presume no blinding of participants or providers; not feasible due to type of intervention |
| Blinding of outcome assessment (detection bias) | Unclear risk | No mention |
| Outcome measures | High risk | Contraceptive use and pregnancy by self‐report |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Loss to follow‐up: intervention 11% (48/431); control 23% (89/385); differential losses |
| Other bias | High risk | Analysis for cluster randomized trial: multivariate linear and logistic regression models included covariates of age, gender, socioeconomic status, sexual experience, and baseline scores. Analysis of behavioral outcomes based on who had sex (could be affected by intervention), rather than all randomized (high risk) |
Tortolero 2010.
| Methods | Design: cluster randomized trial; 10 urban middle schools with 5 assigned to each condition Location: Texas, USA Time frame: Fall 2004 to Spring 2006 Sample size estimation and outcome of focus: no mention; investigators state small sample of sexually active youth in grade 7 left little power |
|
| Participants | General with N: 10 middle schools; 1307 students completed baseline survey Inclusion criteria: middle schools selected within urban school district (served low‐income population); students in grade 7 Exclusion criteria: no mention |
|
| Interventions | Study focus: HIV, STI, and pregnancy prevention Theory or model: Social Cognitive Theory; social influence models; theory of triadic influence 1. Intervention: 'It's Your Game' curriculum (12 lessons in 7th grade; 12 lessons in 8th grade); grade 8 addressed pregnancy testing and skills regarding condom and contraceptive use; 6 parent‐child homework activities at each grade level 2. Comparison: regular health classes that varied by school |
|
| Outcomes | Primary: delayed sexual initiation Secondary: condom use; sex without pregnancy prevention Audio‐computer‐assisted self‐interview Investigator communicated that survey listed effective prevention as condoms (male or female), birth control pills, spermicides, IUD, injectable (DMPA), transdermal patch, vaginal ring, tubal ligation, and EC. Follow‐up: grade 9 (24 months after baseline or > 3 months postprogram) |
|
| Notes | Investigator communicated contraceptives in intervention: condoms, birth control pills, injectable (DMPA), vaginal ring, transdermal patch, abstinence or choosing to wait to have sex, spermicides, EC, condom with other method, as well as rhythm method, withdrawal, and hope. Ranked each method by effectiveness and noted whether method was considered effective or ineffective. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Multi‐attribute randomization protocol; took into account size and racial or ethnic composition and geographic location |
| Allocation concealment (selection bias) | Unclear risk | Schools identified prior to randomization; all 7th‐grade students presumably eligible |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Presume no blinding of participants or providers; not feasible due to type of intervention |
| Blinding of outcome assessment (detection bias) | Low risk | Data collectors unaware of study condition |
| Outcome measures | High risk | Contraceptive use from self‐report |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Loss to follow‐up: 7% intervention; 5% comparison Loss overall: 42% intervention; 34% comparison; most withdrew from school or were repeatedly absent |
| Other bias | High risk | Analysis for cluster randomized trial: multilevel models (intraclass correlation from 0 to 0.03); baseline measures of dependent variable plus covariates judged to be potential confounders Analysis of behavioral outcomes based on who had sex (could be affected by intervention), rather than all randomized (high risk) |
Whitaker 2016.
| Methods | Design: individually randomized; pilot Location: urban academic center; investigators in Chicago, IL (USA) Time frame: June to November 2013 Sample size calculation (and outcome of focus): none for pilot study; 60 chosen to estimate LARC uptake in feasible time (30 per arm within standard practice) |
|
| Participants | General with N: 60 women aged 15 to 29 years
Inclusion criteria: English‐speaking; aged 15 to 29 years; presenting for abortion Exclusion criteria: requesting abortion for fetal or maternal medical indications; with pregnancy resulting from sexual assault; desire for repeat pregnancy within 6 months |
|
| Interventions | Study focus: pregnancy prevention after abortion Theory or model: motivational interviewing (MI)
|
|
| Outcomes | Primary: uptake of LARC within 4 weeks of abortion visit including same‐day Secondary: effective contraceptive uptake within 4 weeks of abortion (IUD or hormonal method); method use and satisfaction with method at 3 months Follow‐up: 4 weeks (medical record); 3 months (telephone) |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated scheme with permuted block sizes 4 and 6 |
| Allocation concealment (selection bias) | Low risk | Sequentially numbered, sealed, opaque envelopes |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Clinic staff and physicians not informed of participant's allocation Presume no blinding of participants; not feasible due to type of intervention |
| Blinding of outcome assessment (detection bias) | Low risk | Research assistant, blinded to group allocation, surveyed by telephone; LARC use within 4 weeks from medical record |
| Outcome measures | Low risk | Contraceptive uptake by 4 weeks from medical record for LARC and DMPA; combined hormonal contraception and progestin‐only pills by prescription; at 3 months, method use from self‐report |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Loss to follow‐up: by 3 months, intervention 14% (4/29) and control 16% (5/31) |
| Other bias | Unclear risk | Analysis for cluster randomized trial: NA |
Wight 2002.
| Methods | Design: cluster randomized trial; 25 schools assigned to intervention or control Location: Tayside and Lothian regions, Scotland Time frame: recruited 1996 and 1997 Sample size calculation (and outcome of focus): based on 80% power to detect 33% decrease in abortion rate by age 20 and 28% decrease in sex without condom use for each gender at 6 months; for latter, assumed 27% would have first sex between 14 and 16 years old (survey data) and 60% events with no condom use for overall rate of 16% no condom use at first sex; assumed design effect 1.5 |
|
| Participants | General with N: 25 schools; 8430 participants, 13 to 15 years old Source: schools Inclusion criteria: non‐Catholic state schools within 24 km of main cities in region; students in third year of secondary school Exclusion criteria: pilot schools; teachers excluded 3 students due to learning difficulties | |
| Interventions | Study focus: reduce unsafe sex behavior, unwanted pregnancies, and improve quality of sexual relationships
Theory or model: primarily Social Cognitive Theory + other health education principles
Duration: 2 school years |
|
| Outcomes | Primary: first sex without condom; condom use with last sex; oral contraception with last sex; unwanted pregnancy (self‐report) Outcomes at age 20 from linked National Health Service records (Henderson 2006): overall termination (abortion) and conception (live births, stillbirths, miscarriages, and terminations); 'any' abortion or conception due to some women having > 1 event Secondary: no mention Follow‐up: 6 months after program completion; 4.5 years after intervention (age 20) |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Balanced randomization; assigned schools by selecting allocation from set of 20,000 possible allocations, which provided best balance of school‐level measures |
| Allocation concealment (selection bias) | Low risk | Two groups determined by comparability of school baseline data. One randomization assigned all schools. All students meeting inclusion criteria were eligible. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Presume no blinding of participants or providers; not feasible due to type of intervention |
| Blinding of outcome assessment (detection bias) | Low risk | Data analysis and checking blinded to study arm |
| Outcome measures | Unclear risk | Shorter‐term follow‐up: no objective measure for contraceptive use; pregnancy self‐report (high risk) Long‐term follow‐up: pregnancy and abortion records (low risk) |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Losses: 32% treatment; 29% comparison Exclusions: none apparent |
| Other bias | High risk | Analysis accounted for cluster effects 6‐month outcomes: for pregnancy, used random effects logistic regression; for other outcomes, used randomization test based on all possible allocations from which final allocation selected Analysis of behavioral outcomes at 6 months based on sexually experienced (could be affected by intervention), rather than all randomized (high risk) 4.5‐year outcomes: adjusted for school socioeconomic measure and individual measures of school leaver and social class |
Note: Primary and secondary outcomes refer to this review, and outcomes may have had different priority in trial report. AEP: alcohol‐exposed pregnancy APROFAM: international Planned Parenthood affiliate FP: family planning N: number NA: not applicable SCT: Social Cognitive Theory STD: sexually transmitted disease STI: sexually transmitted infection USAID: US Agency for International Development WHO: World Health Organization
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Bachanas 2012 | Study focus: HIV prevention |
| Barnet 2007 | The experimental intervention (home visiting) focused on parenting and adolescent curricula. For contraception, the home‐visitors "sought to connect adolescents with primary care." Hence, the theoretical basis did not apply to the contraceptive component. |
| Barth 1992 | Some classes were assigned randomly to study groups, while others were assigned based on group size. |
| Boekeloo 1999 | Intervention focused on STI and HIV prevention, emphasized condom use for protection and abstinence as the safest behavior. |
| Brown 2011 | Investigator communicated that study was not randomized. Materials for each condition were distributed ad hoc within each classroom or data collection setting. |
| Carneiro 2011 | No explicit behavioral theory or model |
| Chung‐Park 2008 | Random assignment by group; analysis did not appear to account for clustering effects. |
| Cowan 2010 | Interim survey showed nearly half the cohort migrated out of area. Investigators and data and safety monitoring board changed design to cross‐sectional survey. |
| DiClemente 2004 | Study focus: HIV prevention among female adolescents; no mention of contraception. |
| DiIorio 2006 | Study focus: HIV prevention |
| Eisen 1990 | Random assignment by group; analysis did not appear to account for clustering effects. |
| Ferrer 2011 | Study focus: sexual risk reduction not contraception |
| Gallegos 2008 | Did not have any of the primary outcomes in this review. Study focused on intentions to use condoms and contraceptives, not behavior. |
| Garbers 2012 | Pre‐post design for feasibility study (no comparison group); nested within RCT |
| Hall 2014 | No explicit behavioral theory or model underlying intervention |
| Hanna 1993 | Primary outcome of contraceptive adherence combined pill‐taking and appointment‐keeping. |
| Hoffman 2003 | Study focus: HIV and STI prevention |
| Ickovics 2016 | No mention of contraception in intervention, nor in background articles. Condom use apparently focused on prevention of STI. |
| Ingersoll 2013 | No contraceptive counseling intervention, unlike Ceperich 2011. |
| Ito 2008 | Did not have any of the primary outcomes in this review. |
| James 2006 | No explicit behavioral theory or model |
| Jemmott 2005 | Study focus: HIV and STI risk reduction |
| Jemmott 2007 | Study focus: HIV and STI risk reduction |
| Jewkes 2008 | Focused on preventing HIV infections. |
| Kalichman 1999 | Study focus: HIV prevention via condom use |
| Kamalikhah 2015 | Not RCT according to investigator's communication: 2 health centers identified that served women of similar sociocultural characteristics; investigators reportedly chose 1 as control and the other as intervention |
| Kiene 2006 | Study focus: HIV/AIDS risk reduction via condom use |
| Kiene 2013 | Not RCT; pre‐post assessment of treatment group |
| Kirby 1997 | Classrooms were assigned to study group; analysis did not appear to account for clustering effects. |
| Kraft 2007 | No relevant outcome measure. Report notes that effective contraceptive use did not differ significantly between the study groups; data were not presented. |
| Langston 2010 | No explicit behavioral theory or model |
| Lederman 2003 | No behavioral data were reported, so no primary outcomes for this review were available. Later reports included attitudes and intentions. |
| Lee 2007 | Coin flip determined which rooms were assigned to program first. Even‐numbered rooms were the experimental group and odd‐numbered were the control group. Cluster assignment (by room) not addressed in the analysis. |
| Lee 2011 | Even‐numbered rooms were control group (routine services). Odd‐numbered rooms were experimental; divided into 2 groups (1 to 11; 13 to 23); coin flip determined which would receive the special intervention first (versus pamphlet). Rooms with double occupancy were assigned as a unit. Cluster assignment (by room) not addressed in the analysis. |
| Legardy 2005 | No explicit behavioral theory or model; some constructs were mentioned. |
| Melnick 2008 | Did not have any of the primary outcomes in this review. No explicit behavioral theory or model that might have guided the development of the intervention. Both groups had the same counseling; the 'intensive' intervention also included 3‐month supply of contraceptives. |
| Moberg 1998 | Assignment was not completely random. Schools were randomized to either control or treatment, but the latter had a choice of 2 treatments. Curriculum objectives included not engaging in sex. |
| Morrison‐Beedy 2005 | Study focus: HIV risk reduction |
| Morrison‐Beedy 2013 | Intervention did not specifically address pregnancy prevention or contraception; focus on HIV risk reduction |
| Peragallo 2005 | Study focus: HIV prevention |
| Peskin 2015 | 'It's Your Game (IYG)‐Tech': computer‐based, middle school sexual health education program. Report does not mention contraceptive use as an outcome; condom use assessed but no outcome data provided. |
| Roberto 2007 | Random assignment by group; only 2 schools were randomized so the analysis could not be adjusted for clustering effects. |
| Ross 2007 | No mention of contraception in intervention, including in background article; condom use apparently focused on prevention of STI. Cross‐sectional survey (several years later) included use of modern contraception as outcome. |
| Roye 2007 | Study focus: brief intervention to prevent HIV via condom use (in addition to current use of hormonal contraceptives) |
| Sarayloo 2015 | Not RCT; treatment and control selected from separate health centers to avoid contamination |
| Shain 1999 | Study focus: preventing STI among minority women |
| Sieving 2012 | Pilot study to refine intervention protocols and determine preliminary efficacy. Outcome analysis included participants randomized (phase 1) and nonrandomized (phase 2). |
| Stanton 1996 | Study focus: AIDS prevention |
| Stanton 2005 | Trial had 4 arms (3 program versions and 1 control). Investigators excluded the 1 group (with the interactive televised version) from the analysis. A secondary report from 2006 grouped the 3 intervention arms and compared them to the control. Adjustment for cluster effects was not apparent in the latter report. |
| Stephenson 2004 | No explicit behavioral theory or model |
| Thato 2008 | Curriculum emphasized abstinence (Thai values and culture toward premarital sex and maintaining virginity until marriage). Report did not include any of the primary outcomes for this review. |
| Tortolero 2008 | The investigator communicated that there was no intervention effect and they never published an outcome paper. |
| Villarruel 2006 | Study focus: HIV prevention for Latino youth |
| Vogt 2012 | No relevant outcome |
| Weeks 1997 | Random assignment by group; analysis did not appear to account for cluster effects. |
| Winter 1993 | No explicit behavioral theory or model. Did not have any of the primary outcomes in this review. 'Condom acceptance' was defined by the number of condoms taken at the end of the session rather than reported use. |
| Zimmerman 2008 | Curriculum emphasized abstinence. |
Characteristics of studies awaiting assessment [ordered by study ID]
Gilliam 2016.
| Methods | Design: individually randomized Location: Chicago, IL (USA) Time frame: February 201 to June 2016 Sample size calculation: no information |
| Participants | 22 women Inclusion criteria: African American or Latina; sexually active with male partner in past 6 months; age 15 to 29 years; seeking contraception; English speaking Exclusion criteria: currently pregnant or intending pregnancy in next 6 months; currently using LARC; highly intend to use LARC |
| Interventions | Study focus: contraceptive counseling Theory: not specified
|
| Outcomes | LARC uptake (at initial visit); method satisfaction at 12 weeks; method continuation at 12 weeks |
| Notes | Insufficient information from conference abstract and ClinicalTrials.gov for determining eligibility for review; will consider for inclusion when full report is available |
Contributions of authors
LM Lopez developed the idea, reviewed the search results, conducted the primary data extraction, and drafted the review. She led the updates and revisions through 2016. EE Tolley provided expertise in behavioral science and reviewed the data extracted on theories and constructs. M Chen reviewed the cluster randomized trials for analytical methods, provided expertise on study design, and reviewed the data extracted on evidence quality. In 2013, LL Stockton reviewed search results and extracted and checked data. All authors reviewed and edited the manuscript. In 2016, TW Grey reviewed the search results, conducted the primary and secondary data extraction with LM Lopez, and checked the data in the review text.
Sources of support
Internal sources
No sources of support supplied
External sources
-
National Institute of Child Health and Human Development, USA.
Through 2016: support for conducting the review at FHI 360
-
U.S. Agency for International Development, USA.
Through 2013: support for conducting the review at FHI 360
Declarations of interest
M Chen was involved in the analysis, but not study design, for Schuler 2015. Study was conducted at FHI 360, where review authors are employed, but no others were involved.
LM Lopez, TW Grey, EE Tolley, and LL Stockton have no interests to declare.
New search for studies and content updated (no change to conclusions)
References
References to studies included in this review
Barnet 2009 {published and unpublished data}
- Barnet B, Liu J, DeVoe M, Duggan AK, Gold MA, Pecukonis E. Motivational intervention to reduce rapid subsequent births to adolescent mothers: a community‐based randomized trial. Annals of Family Medicine 2009;7(5):436‐45. [DOI] [PMC free article] [PubMed] [Google Scholar]
Berenson 2012 {published data only (unpublished sought but not used)}
- Berenson AB, Rahman M. A randomized controlled study of two educational interventions on adherence with oral contraceptives and condoms. Contraception 2012;86(6):716‐24. [DOI] [PMC free article] [PubMed] [Google Scholar]
Black 2006 {published data only (unpublished sought but not used)}
- Black MM, Bentley ME, Papas MA, Oberlander S, Teti LO, McNary S, et al. Delaying second births among adolescent mothers: a randomized, controlled trial of a home‐based mentoring program. Pediatrics 2006;118(4):e1087‐99. [DOI] [PubMed] [Google Scholar]
- Black MM, Siegel EH, Abel Y, Bentley ME. Home and videotape intervention delays early complementary feeding among adolescent mothers. Pediatrics 2001;107(5):e67. [DOI] [PubMed] [Google Scholar]
Boyer 2005 {published and unpublished data}
- Boyer CB, Shafer MA, Shaffer RA, Brodine SK, Pollack LM, Betsinger K, et al. Evaluation of a cognitive‐behavioral, group, randomized controlled intervention trial to prevent sexually transmitted infections and unintended pregnancies in young women. Preventive Medicine 2005;40(4):420‐31. [DOI] [PubMed] [Google Scholar]
Ceperich 2011 {published and unpublished data}
- Ceperich SD, Ingersoll KS. Motivational interviewing + feedback intervention to reduce alcohol‐exposed pregnancy risk among college binge drinkers: determinants and patterns of response. Journal of Behavioral Medicine 2011;34(5):381‐95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ingersoll KS, Ceperich SD, Nettleman MD, Karanda K, Brocksen S, Johnson BA. Reducing alcohol‐exposed pregnancy risk in college women: initial outcomes of a clinical trial of a motivational intervention. Journal of Substance Abuse Treatment 2005;29(3):173‐80. [DOI] [PMC free article] [PubMed] [Google Scholar]
Coyle 2001 {published data only}
- Coyle K, Basen‐Engquist K, Kirby D, Parcel G, Banspach S, Collins J, et al. Safer Choices: Reducing teen pregnancy, HIV, and STDs. Public Health Reports 2001;116(Suppl 1):82‐93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coyle K, Basen‐Engquist K, Kirby D, Parcel G, Banspach S, Harrist R, et al. Short‐term impact of Safer Choices: a multicomponent, school‐based HIV, other STD, and pregnancy prevention program. Journal of School Health 1999;69(5):181‐8. [DOI] [PubMed] [Google Scholar]
- Kirby DB, Baumler E, Coyle KK, Basen‐Engquist K, Parcel GS, Harrist R, et al. The "Safer Choices" intervention: its impact on the sexual behaviors of different subgroups of high school students. Journal of Adolescent Health 2004;35(6):442‐52. [DOI] [PubMed] [Google Scholar]
Coyle 2006 {published data only (unpublished sought but not used)}
- Coyle KK, Kirby DB, Robin LE, Banspach SW, Baumler E, Glassman JR. All4You! A randomized trial of an HIV, other STDs, and pregnancy prevention intervention for alternative school students. AIDS Education and Prevention 2006;18(3):187‐203. [DOI] [PubMed] [Google Scholar]
Davidson 2015 {published data only}
- Davidson AS, Whitaker AK, Martins SL, Hill B, Kuhn C, Hagbom‐Ma C, et al. Impact of a theory‐based video on initiation of long‐acting reversible contraception after abortion. American Journal of Obstetrics and Gynecology 2015;212(3):310 e1‐7. [DOI] [PubMed] [Google Scholar]
Floyd 2007 {published data only}
- Floyd RL, Sobell M, Velasquez MM, Ingersoll K, Nettleman M, Sobell L, et al. Preventing alcohol‐exposed pregnancies. A randomized controlled trial. American Journal of Preventive Medicine 2007;32(1):1‐10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ingersoll K, Floyd l, Sobell M, Velasquez MM, Project CHOICES Intervention Research Group. Reducing the risk of alcohol‐exposed pregnancies: a study of a motivational intervention in community settings. Pediatrics 2003;111(5 Part 2):1131‐5. [PubMed] [Google Scholar]
- Velasquez MM, Ingersoll KS, Sobell MB, Floyd RL, Sobell LC, Sternberg K. A dual‐focus motivational intervention to reduce the risk of alcohol‐exposed pregnancy. Cognitive and Behavioral Practice 2010; Vol. 17, issue 2:203‐12. [DOI] [PMC free article] [PubMed]
Gilliam 2014 {published data only}
- Gilliam ML, Martins SL, Bartlett E, Mistretta SQ, Holl JL. Development and testing of an iOS waiting room "app" for contraceptive counseling in a Title X family planning clinic. American Journal of Obstetrics and Gynecology 2014;211(5):481 e1‐8. [DOI] [PubMed] [Google Scholar]
Gold 2016 {published data only}
- Gold MA, Tzilos GK, Stein LA, Anderson BJ, Stein MD, Ryan CM, et al. A randomized controlled trial to compare computer‐assisted motivational intervention with didactic educational counseling to reduce unprotected sex in female adolescents. Journal of Pediatric and Adolescent Gynecology 2016;29(1):26‐32. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kirby 2010 {published and unpublished data}
- Kirby D, Raine T, Thrush G, Yuen C, Sokoloff A, Potter SC. Impact of an intervention to improve contraceptive use through follow‐up phone calls to female adolescent clinic patients. Perspectives on Sexual and Reproductive Health 2010;42(4):251‐7. [NCT00230880] [DOI] [PMC free article] [PubMed] [Google Scholar]
Markham 2012 {published and unpublished data}
- Markham CM, Peskin MF, Shegog R, Baumler ER, Addy RC, Thiel M, et al. Behavioral and psychosocial effects of two middle school sexual health education programs at tenth‐grade follow‐up. Journal of Adolescent Health 2014;54(2):151‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Markham CM, Tortolero SR, Peskin MF, Shegog R, Thiel M, Baumler ER, et al. Sexual risk avoidance and sexual risk reduction interventions for middle school youth: a randomized controlled trial. Journal of Adolescent Health 2012;50(3):279‐88. [DOI] [PMC free article] [PubMed] [Google Scholar]
Peipert 2008 {published data only}
- Peipert J, Redding CA, Blume J, Allsworth JE, Iannuccillo K, Lozowski F, et al. Design of a stage‐matched intervention trial to increase dual method contraceptive use (Project PROTECT). Contemporary Clinical Trials 2007;28(5):626‐37. [DOI] [PubMed] [Google Scholar]
- Peipert JF, Redding CA, Blume JD, Allsworth JE, Matteson KA, Lozowski F, et al. Tailored intervention to increase dual‐contraceptive method use: a randomized trial to reduce unintended pregnancies and sexually transmitted infections. American Journal of Obstetrics & Gynecology 2008;198(6):630.e1‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peipert JF, Zhao Q, Meints L, Peipert BJ, Redding CA, Allsworth JE. Adherence to dual‐method contraceptive use. Contraception 2011;84(3):252‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Petersen 2007 {published and unpublished data}
- Petersen R, Albright J, Garrett JM, Curtis KM. Pregnancy and STD prevention counseling using an adaptation of motivational interviewing: a randomized controlled trial. Perspectives on Sexual and Reproductive Health 2007;39(1):21‐8. [DOI] [PubMed] [Google Scholar]
Raj 2016 {published data only}
- Raj A, Ghule M, Ritter J, Battala M, Gajanan V, Nair S, et al. Cluster Randomized Controlled Trial Evaluation of a Gender Equity and Family Planning Intervention for Married Men and Couples in Rural India. PLoS One 2016;11(5):e0153190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yore J, Dasgupta A, Ghule M, Battala M, Nair S, Silverman J, et al. CHARM, a gender equity and family planning intervention for men and couples in rural India: protocol for the cluster randomized controlled trial evaluation. Reproductive Health 2016;13:14. [DOI] [PMC free article] [PubMed] [Google Scholar]
Rendall‐Mkosi 2013 {published data only}
- Rendall‐Mkosi K, Morojele N, London L, Moodley S, Singh C, Girdler‐Brown B. A randomized controlled trial of motivational interviewing to prevent risk for an alcohol‐exposed pregnancy in the Western Cape, South Africa. Addiction 2013;108(4):725‐32. [DOI] [PubMed] [Google Scholar]
Schinke 1981 {published data only (unpublished sought but not used)}
- Schinke SP, Blythe BJ, Gilchrist LD. Cognitive‐behavioral prevention of adolescent pregnancy. Journal of Counseling Psychology 1981;28(5):451‐4. [Google Scholar]
- Schinke SP, Gilchrist LD, Smith TE, Wong SE. Group interpersonal skills training in a natural setting: an experimental study. Behavior Research and Therapy 1979;17(2):149‐54. [DOI] [PubMed] [Google Scholar]
Schuler 2015 {published data only}
- Schuler SR, Nanda G, Ramírez LF, Chen M. Interactive workshops to promote gender equity and family planning in rural communities of Guatemala: results of a community randomized study. Journal of Biosocial Science 2015;47(5):667‐86. [DOI] [PubMed] [Google Scholar]
- Schuler SR, Ramírez LF. Interactive workshops to promote gender equity and family planning in rural Guatemalan communities: results of a field test. Washington (DC): C‐Change, FHI 360; 2012. [DOI] [PubMed]
Sieving 2013 {published data only}
- Sieving RE, McMorris BJ, Beckman KJ, Pettingell SL, Secor‐Turner M, Kugler K, et al. Prime Time: 12‐month sexual health outcomes of a clinic‐based intervention to prevent pregnancy risk behaviors. Journal of Adolescent Health 2011;49(2):172‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sieving RE, McRee AL, McMorris BJ, Beckman KJ, Pettingell SL, Bearinger LH, et al. Prime time: sexual health outcomes at 24 months for a clinic‐linked intervention to prevent pregnancy risk behaviors. JAMA Pediatrics 2013;167(4):333‐40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sieving RE, McRee AL, Secor‐Turner M, Garwick AW, Bearinger LH, Beckman KJ, et al. Prime Time: long‐term sexual health outcomes of a clinic‐linked intervention. Perspectives on Sexual and Reproductive Health 2014;46(2):91‐100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanner AE, Secor‐Turner M, Garwick A, Sieving R, Rush K. Engaging vulnerable adolescents in a pregnancy prevention program: perspectives of Prime Time staff. Journal of Pediatric Health Care 2010;26(4):254‐65. [DOI] [PMC free article] [PubMed] [Google Scholar]
Stanton 2004 {published data only}
- Stanton B, Cole M, Galbraith J, Li X, Pendleton S, Cottrel L, et al. Randomized trial of a parent intervention: parents can make a difference in long‐term adolescent risk behaviors, perceptions, and knowledge. Archives of Pediatrics & Adolescent Medicine 2004;158(10):947‐55. [DOI] [PubMed] [Google Scholar]
- Stanton BF, Li X, Galbraith J, Cornick G, Feigelman S, Kaljee L, et al. Parental underestimates of adolescent risk behavior: a randomized, controlled trial of a parental monitoring intervention. Journal of Adolescent Health 2000;26(1):18‐26. [DOI] [PubMed] [Google Scholar]
Taylor 2014 {published data only (unpublished sought but not used)}
- Taylor M, Jinabhai C, Dlamini S, Sathiparsad R, Eggers MS, Vries H. Effects of a teenage pregnancy prevention program in KwaZulu‐Natal, South Africa. Health Care for Women International 2014;35(7‐9):845‐58. [DOI] [PubMed] [Google Scholar]
Tortolero 2010 {published and unpublished data}
- Tortolero SR, Markham CM, Peskin MF, Shegog R, Addy RC, Escobar‐Chaves SL, et al. It's Your Game: Keep It Real: delaying sexual behavior with an effective middle school program. Journal of Adolescent Health 2010;46(2):169‐79. [DOI] [PMC free article] [PubMed] [Google Scholar]
Whitaker 2016 {published data only}
- Whitaker AK, Quinn MT, Martins SL, Tomlinson AN, Woodhams EJ, Gilliam M. Motivational interviewing to improve postabortion contraceptive uptake by young women: development and feasibility of a counseling intervention. Contraception 2015;92(4):323‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitaker AK, Quinn MT, Munroe E, Martins SL, Mistretta SQ, Gilliam ML. A motivational interviewing‐based counseling intervention to increase postabortion uptake of contraception: A pilot randomized controlled trial. Patient Education and Counseling 2016 May 9 [Epub ahead of print]. [DOI] [PMC free article] [PubMed]
Wight 2002 {published data only}
- Henderson M, Wight D, Raab GM, Abraham C, Parkes A, Scott S, et al. Impact of a theoretically based sex education programme (SHARE) delivered by teachers on NHS registered conceptions and terminations: final results of cluster randomised trial. British Medical Journal 2006;334(7585):133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wight D, Abraham C. From psychosocial theory to sustainable classroom practice: developing a researchbased teacherdelivered sex education programme. Health Education Research 2000;15(1):25‐38. [DOI] [PubMed] [Google Scholar]
- Wight D, Raab GM, Henderson M, Abraham C, Buston K, Hart G, et al. Limits of teacher delivered sex education: interim behavioural outcomes from randomised trial. British Medical Journal 2002;324(7351):1430. [DOI] [PMC free article] [PubMed] [Google Scholar]
References to studies excluded from this review
Bachanas 2012 {published data only (unpublished sought but not used)}
- Bachanas P. HIV Prevention for PLHIV: Evaluation of an Intervention Toolkit for HIV Care & Treatment Settings. http://clinicaltrials.gov/ct2/show/NCT01256463 (accessed 31 Jul 2012).
- Kidder DP, Bachanas P, Medley A, Pals S, Nuwagaba‐Biribonwoha H, Ackers M, et al. HIV prevention in care and treatment settings: baseline risk behaviors among HIV patients in Kenya, Namibia, and Tanzania. PloS one. 2013/03/06 2013; Vol. 8, issue 2:e57215. [DOI] [PMC free article] [PubMed]
Barnet 2007 {published data only}
- Barnet B, Liu J, DeVoe M, Alperovitz‐Bichell K, Duggan AK. Home visiting for adolescent mothers: effects on parenting, maternal life course, and primary care linkage. Annals of Family Medicine 2007;5(3):224‐32. [DOI] [PMC free article] [PubMed] [Google Scholar]
Barth 1992 {published data only}
- Barth RP, Fetro JV, Leland N, Volkan K. Preventing adolescent pregnancy with social and cognitive skills. Journal of Adolescent Research 1992;7(2):208‐32. [DOI] [PubMed] [Google Scholar]
- Kirby D, Barth RP, Leland N, Fetro JV. Reducing the Risk: impact of a new curriculum on sexual risk‐taking. Family Planning Perspectives 1991;23(6):253‐63. [PubMed] [Google Scholar]
Boekeloo 1999 {published data only}
- Boekeloo BO, Schamus LA, Simmens SJ, Cheng TL, O'Connor K, D'Angelo LJ. A STD/HIV prevention trial among adolescents in managed care. Pediatrics 1999;103(1):107‐15. [DOI] [PubMed] [Google Scholar]
Brown 2011 {published data only}
- Brown KE, Hurst KM, Arden MA. Improving adolescent contraceptive use: evaluation of a theory‐driven classroom‐based intervention. Psychology, Health & Medicine 2011;16(2):141‐55. [DOI] [PubMed] [Google Scholar]
Carneiro 2011 {published data only}
- Carneiro Gomes Ferreira AL, Impieri Souza A, Evangelista Pessoa R, Braga C. The effectiveness of contraceptive counseling for women in the postabortion period: an intervention study. Contraception 2011;84(4):377‐83. [DOI] [PubMed] [Google Scholar]
Chung‐Park 2008 {published data only}
- Chung‐Park MS. Evaluation of a pregnancy prevention programme using the Contraceptive Behavior Change Model. Journal of Advanced Nursing 2008;61(1):81‐91. [DOI] [PubMed] [Google Scholar]
Cowan 2010 {published data only}
- Cowan FM, Pascoe SJ, Langhaug LF, Dirawo J, Chidiya S, Jaffar S, et al. The Regai Dzive Shiri Project: a cluster randomised controlled trial to determine the effectiveness of a multi‐component community‐based HIV prevention intervention for rural youth in Zimbabwe‐‐study design and baseline results. Tropical Medicine & International Health 2008;13(10):1235‐44. [DOI] [PubMed] [Google Scholar]
- Cowan FM, Pascoe SJ, Langhaug LF, Mavhu W, Chidiya S, Jaffar S, et al. The Regai Dzive Shiri project: results of a randomized trial of an HIV prevention intervention for youth. AIDS 2010;24(16):2541‐52. [DOI] [PMC free article] [PubMed] [Google Scholar]
DiClemente 2004 {published data only}
- DiClemente RJ, Wingood GM, Harrington KF, Lang DL, Davies SL, Hook EW 3rd, et al. Efficacy of an HIV prevention intervention for African‐American adolescent girls: a randomized controlled trial. Journal of the American Medical Association 2004;292(2):171‐9. [DOI] [PubMed] [Google Scholar]
- Wingood GM, DiClemente RJ, Harrington KF, Lang DL, Davies SL, Hook EW 3rd, et al. Efficacy of an HIV prevention program among female adolescents experiencing gender‐based violence. American Journal of Public Health 2006;96(6):1085‐90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wingood GM, DiClemente RJ, Hubbard McCree D, Harrington K, Davies SL. Dating violence and the sexual health of Black adolescent females. Pediatrics 2001;107(5):e72. [DOI] [PubMed] [Google Scholar]
DiIorio 2006 {published data only}
- DiIorio C, Resnicow K, McCarty F, De AK, Dudley WN, Wang DT, et al. Keepin' it R.E.A.L.!: results of a mother‐adolescent HIV prevention program. Nursing Research 2006;55(1):43‐51. [DOI] [PubMed] [Google Scholar]
- DiIorio C, Resnicow K, Thomas S, Wang DT, Dudley WN, Marter DF, et al. Keepin' It R.E.A.L.!: program description and results of baseline assessment. Health Education & Behavior 2002;29(1):104‐23. [DOI] [PubMed] [Google Scholar]
Eisen 1990 {published data only}
- Eisen M, Zellman GL, McAlister AL. A Health Belief Model‐Social Learning Theory approach to adolescents' fertility control: findings from a controlled field trial. Health Education Quarterly 1992;19(2):249‐62. [DOI] [PubMed] [Google Scholar]
- Eisen M, Zellman GL, McAlister AL. Evaluating the impact of a theory‐based sexuality and contraceptive education program. Family Planning Perspectives 1990;22(6):261‐71. [PubMed] [Google Scholar]
Ferrer 2011 {published data only}
- Ferrer RA, Fisher JD, Buck R, Amico KR. Pilot test of an emotional education intervention component for sexual risk reduction. Health Psychology 2011;30(5):656‐60. [DOI] [PubMed] [Google Scholar]
Gallegos 2008 {published data only}
- Gallegos EC, Villarruel AM, Loveland‐Cherry C, Ronis DL, Yan Zhou M. [Intervention to reduce adolescents sexual risk behaviors: a randomized controlled trial]. Salud Pública de México 2008;50:59‐66. [DOI] [PubMed] [Google Scholar]
- Villarruel AM, Zhou Y, Gallegos EC, Ronis DL. Examining long‐term effects of Cuidate‐a sexual risk reduction program in Mexican youth. Revista Panamericana de sSalud Pública. 2010/07/06 2010; Vol. 27, issue 5:345‐51. [DOI] [PubMed]
Garbers 2012 {published data only}
- Garbers S, Meserve A, Kottke M, Hatcher R, Chiasson MA. Tailored health messaging improves contraceptive continuation and adherence: results from a randomized controlled trial. Contraception 2012;86(5):536‐42. [DOI] [PubMed] [Google Scholar]
- Garbers S, Meserve A, Kottke M, Hatcher R, Ventura A, Chiasson MA. Randomized controlled trial of a computer‐based module to improve contraceptive method choice. Contraception 2012;86(4):383‐90. [DOI] [PubMed] [Google Scholar]
Hall 2014 {published data only}
- Castano PM, Bynum JY, Andres R, Lara M, Westhoff C. Effect of daily text messages on oral contraceptive continuation: a randomized controlled trial. Obstetrics and Gynecology 2012;119(1):14‐20. [DOI] [PubMed] [Google Scholar]
- Hall KS, Castano P, Westhoff CL. The influence of oral contraceptive knowledge on oral contraceptive continuation among young women. Journal of Womens Health 2014;23(7):596‐601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall KS, Westhoff CL, Castano PM. The impact of an educational text message intervention on young urban women's knowledge of oral contraception. Contraception 2013;87(4):449‐54. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hanna 1993 {published data only}
- Hanna KM. Effect of nurse‐client transaction on female adolescents' oral contraceptive adherence. IMAGE: Journal of Nursing Scholarship 1993;25(4):285‐290. [DOI] [PubMed] [Google Scholar]
Hoffman 2003 {published data only}
- Ehrhardt AA, Exner TM, Hoffman S, Silberman I, Leu C‐S, Miller S, et al. A gender‐specific HIV/STD risk reduction intervention for women in a health care setting: short‐ and long‐term results of a randomized clinical trial. AIDS Care 2002;14(2):147‐61. [DOI] [PubMed] [Google Scholar]
- Ehrhardt AA, Exner TM, Hoffman S, Silberman I, Yingling S, Adams‐Skinner J, et al. HIV/STD risk and sexual strategies among women family planning clients in New York: Project FIO. AIDS and Behavior 2002;6(1):1‐13. [Google Scholar]
- Hoffman S, Exner TM, Leu CS, Ehrhardt AA, Stein Z. Female‐condom use in a gender‐specific family planning clinic trial. American Journal of Public Health 2003;93(11):1897‐903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller S, Exner TM, Williams SP, Ehrhardt AA. A gender‐specific intervention for at‐risk women in the USA. AIDS Care 2000;12(5):603‐12. [DOI] [PubMed] [Google Scholar]
Ickovics 2016 {published data only}
- Ickovics JR, Earnshaw V, Lewis JB, Kershaw TS, Magriples U, Stasko E, et al. Cluster randomized controlled trial of group prenatal care: perinatal outcomes among adolescents in New York City health centers. American Journal of Public Health 2016;106(2):359‐65. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ingersoll 2013 {published data only}
- Ingersoll KS, Ceperich SD, Hettema JE, Farrell‐Carnahan L, Penberthy JK. Preconceptional motivational interviewing interventions to reduce alcohol‐exposed pregnancy risk. Journal of Substance Abuse Treatment 2013;44(4):407‐16. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ito 2008 {published data only}
- Ito KE, Kalyanaraman S, Ford CA, Brown JD, Miller WC. "Let's Talk About Sex": pilot study of an interactive CD‐ROM to prevent HIV/STIs in female adolescents. AIDS Education and Prevention 2008;20(1):78‐89. [DOI] [PubMed] [Google Scholar]
James 2006 {published data only}
- James S, Reddy P, Ruiter RA, McCauley A, Borne B. The Impact of an HIV and AIDS Life Skills Program on Secondary School Students in KwaZulu‐Natal, South Africa. AIDS Education and Prevention 2006;18(4):281‐94. [DOI] [PubMed] [Google Scholar]
Jemmott 2005 {published data only}
- Jemmott JB 3rd, Jemmott LS, Braverman PK, Fong GT. HIV/STD risk reduction interventions for African American and Latino adolescent girls at an adolescent medicine clinic: a randomized controlled trial. Archives of Pediatrics & Adolescent Medicine 2005;159(5):440‐9. [DOI] [PubMed] [Google Scholar]
Jemmott 2007 {published data only}
- Jemmott LS, Jemmott JB 3rd, O'Leary A. Effects on sexual risk behavior and STD rate of brief HIV/STD prevention interventions for African American women in primary care settings. American Journal of Public Health 2007;97(6):1034‐40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Leary A, Jemmott LS, Jemmott JB. Mediation analysis of an effective sexual risk‐reduction intervention for women: the importance of self‐efficacy. Health Psychology 2008;27(2(Suppl)):S180‐4. [DOI] [PubMed] [Google Scholar]
Jewkes 2008 {published data only}
- Jewkes R, Nduna M, Levin J, Jama N, Dunkle K, Khuzwayo N, et al. A cluster randomized‐controlled trial to determine the effectiveness of Stepping Stones in preventing HIV infections and promoting safer sexual behaviour amongst youth in the rural Eastern Cape, South Africa: trial design, methods and baseline findings. Tropical Medicine and International Health 2006;11(1):3‐16. [DOI] [PubMed] [Google Scholar]
- Jewkes R, Nduna M, Levin J, Jama N, Dunkle K, Puren A, et al. Impact of stepping stones on incidence of HIV and HSV‐2 and sexual behaviour in rural South Africa: cluster randomised controlled trial. BMJ. 2008/08/09 2008; Vol. 337:a506. [DOI] [PMC free article] [PubMed]
- Welbourn A. Stepping Stones: a positive force for change. Reproductive Health Matters 1996;4(7):177‐8. [Google Scholar]
Kalichman 1999 {published data only}
- Kalichman SC, Cherry C, Browne‐Sperling F. Effectiveness of a video‐based motivational skills‐building HIV risk‐reduction intervention for inner‐city African American men. Journal of Consulting and Clinical Psychology 1999;67(6):959‐66. [DOI] [PubMed] [Google Scholar]
Kamalikhah 2015 {published data only (unpublished sought but not used)}
- Kamalikhah T, Rakhshani F, Najarkolaei FR, Avval MG. Evaluation of transtheoretical model‐based family education among females of Zahedan (Southeast of Iran). Iranian Red Crescent Medical Journal 2015;17(10):e18895. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kiene 2006 {published data only}
- Kiene SM, Barta WD. A brief individualized computer‐delivered sexual risk reduction intervention increases HIV/AIDS preventive behavior. Journal of Adolescent Health 2006;39(3):404‐10. [DOI] [PubMed] [Google Scholar]
Kiene 2013 {published data only}
- Kiene SM, Hopwood S, Lule H, Wanyenze RK. An empirical test of the Theory of Planned Behaviour applied to contraceptive use in rural Uganda. Journal of Health Psychology 2013;19(12):1564‐75. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kirby 1997 {published data only}
- Kirby D, Korpi M, Adivi C, Weissman J. An impact evaluation of Project SNAPP: an AIDS and pregnancy prevention middle school program. AIDS Education and Prevention 1997;9(Suppl A):44‐61. [PubMed] [Google Scholar]
Kraft 2007 {published and unpublished data}
- Kraft JM, Harvey SM, Thorburn S, Henderson JT, Posner SF, Galavotti C. Intervening with couples: assessing contraceptive outcomes in a randomized pregnancy and HIV/STD risk reduction intervention trial. Womens Health Issues 2007;17(1):52‐60. [DOI] [PubMed] [Google Scholar]
Langston 2010 {published data only}
- Langston AM, Rosario L, Westhoff CL. Structured contraceptive counseling‐‐a randomized controlled trial. Patient Education and Counseling. 2010/09/28 2010; Vol. 81, issue 3:362‐7. [DOI] [PubMed]
- Westhoff C. Randomized controlled trial of structured contraceptive counseling in adult women. http://clinicaltrials.gov/ct2/show/NCT00746993 (accessed 25 Mar 2010). [NCT00746993] [DOI] [PubMed]
- World Health Organization. Decision‐making tool for family planning clients and providers. http://www.who.int/reproductivehealth/publications/family_planning/9241593229index/en/index.html (accessed 08 Jan 2012).
Lederman 2003 {published data only}
- Lederman RP, Chan W, Roberts‐Gray C. Parent‐Adolescent Relationship Education (PARE): program delivery to reduce risks for adolescent pregnancy and STDs. Behavioral Medicine 2008;33(4):137‐143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lederman RP, Chan W, Roberts‐Gray C. Sexual risk attitudes and intentions of youth aged 12‐14 years: survey comparisons of parent‐teen prevention and control groups. Behavioral Medicine 2004;29(4):155‐63. [DOI] [PubMed] [Google Scholar]
- Lederman RP, Mian TS. The Parent‐Adolescent Relationship Education (PARE) Program: a curriculum for prevention of STDs and pregnancy in middle school youth. Behavioral Medicine 2003;29(1):33‐41. [DOI] [PubMed] [Google Scholar]
Lee 2007 {published data only}
- Lee JT, Yen HW. Randomized controlled evaluation of a theory‐based postpartum sexual health education programme. Journal of Advanced Nursing 2007;60(4):389‐401. [DOI] [PubMed] [Google Scholar]
Lee 2011 {published data only}
- Lee JT, Tsai JL, Tsou TS, Chen MC. Effectiveness of a theory‐based postpartum sexual health education program on women's contraceptive use: a randomized controlled trial. Contraception 2011;84(1):48‐56. [DOI] [PubMed] [Google Scholar]
Legardy 2005 {published data only}
- Legardy JK, Macaluso M, Artz L, Brill I. Do participant characteristics influence the effectiveness of behavioral interventions? Promoting condom use to women. Sexually Transmitted Diseases 2005;32(11):665‐71. [DOI] [PubMed] [Google Scholar]
Melnick 2008 {published data only}
- Melnick AL, Rdesinski RE, Creach ED, Choi D, Harvey SM. The influence of nurse home visits, including provision of 3 months of contraceptives and contraceptive counseling, on perceived barriers to contraceptive use and contraceptive use self‐efficacy. Womens Health Issues. 2008/10/18 2008; Vol. 18, issue 6:471‐81. [DOI] [PMC free article] [PubMed]
Moberg 1998 {published data only}
- Moberg DP, Piper DL. The Healthy for Life project: sexual risk behavior outcomes. AIDS Education and Prevention 1998;10(2):128‐48. [PubMed] [Google Scholar]
Morrison‐Beedy 2005 {published and unpublished data}
- Morrison‐Beedy D, Carey MP, Kowalski J, Tu X. Group‐based HIV risk reduction intervention for adolescent girls: evidence of feasibility and efficacy. Research in Nursing & Health 2005;28(1):3‐15. [DOI] [PMC free article] [PubMed] [Google Scholar]
Morrison‐Beedy 2013 {published data only}
- Morrison‐Beedy D, Jones S H, Xia Y, Tu X, Crean H F, Carey M P. Reducing sexual risk behavior in adolescent girls: results from a randomized controlled trial. Journal of Adolescent Health 2013;52(3):314‐21. [DOI] [PMC free article] [PubMed] [Google Scholar]
Peragallo 2005 {published and unpublished data}
- Peragallo N, Deforge B, O'Campo P, Lee SM, Kim YJ, Cianelli R, et al. A randomized clinical trial of an HIV‐risk‐reduction intervention among low‐income Latina women. Nursing Research 2005;54(2):108‐18. [DOI] [PubMed] [Google Scholar]
Peskin 2015 {published data only}
- Peskin MF, Shegog R, Markham CM, Thiel M, Baumler ER, Addy RC, et al. Efficacy of It's Your Game‐Tech: A Computer‐Based Sexual Health Education Program for Middle School Youth. Journal of Adolescent Health 2015;56(5):515‐21. [DOI] [PMC free article] [PubMed] [Google Scholar]
Roberto 2007 {published data only}
- Roberto AJ, Zimmerman RS, Carlyle KE, Abner EL. A computer‐based approach to preventing pregnancy, STD, and HIV in rural adolescents. Journal of Health Communication 2007;12(1):53‐76. [DOI] [PubMed] [Google Scholar]
Ross 2007 {published data only}
- Doyle AM, Ross DA, Maganja K, Baisley K, Masesa C, Andreasen A, et al. Long‐term biological and behavioural impact of an adolescent sexual health intervention in Tanzania: follow‐up survey of the community‐based MEMA kwa Vijana Trial. PLoS Medicine 2010;7(6):e1000287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes RJ, Changaluchab J, Ross DA, Gavyolec A, Todd J, Obasi AIN, et al. The MEMA kwa Vijana Project: Design of a community randomised trial of an innovative adolescent sexual health intervention in rural Tanzania. Contemporary Clinical Trials 2005;26(4):430‐42. [DOI] [PubMed] [Google Scholar]
- Obasi AI, Cleophas B, Ross DA, Chima KL, Mmassy G, Gavyole A, et al. Rationale and design of the MEMA kwa Vijana adolescent sexual and reproductive health intervention in Mwanza Region, Tanzania. AIDS Care 2006;18(4):311‐22. [DOI] [PubMed] [Google Scholar]
- Ross DA, Changaluchab J, Obasia AIN, Todd J, Plummer ML, Cleophas‐Mazige B, et al. Biological and behavioural impact of an adolescent sexual health intervention in Tanzania: a community‐randomized trial. AIDS 2007;21(14):1943‐55. [DOI] [PubMed] [Google Scholar]
Roye 2007 {published and unpublished data}
- Roye C, Perlmutter Silverman P, Krauss B. A brief, low‐cost, theory‐based intervention to promote dual method use by black and Latina female adolescents: a randomized clinical trial. Health Education & Behavior 2007;34(4):608‐21. [DOI] [PubMed] [Google Scholar]
- Roye CF, Hudson M. Developing a culturally appropriate video to promote dual‐method use by urban teens: rationale and methodology. AIDS Education and Prevention 2003;15(2):148‐58. [DOI] [PubMed] [Google Scholar]
Sarayloo 2015 {published data only}
- Sarayloo K, Moghadam ZB, Mansoure JM, Mostafa H, Mohsen S. The impact of an educational program based on BASNEF model on the selection of a contraceptive method in women. Iranian Journal of Nursing and Midwifery Research 2015;20(2):171‐8. [PMC free article] [PubMed] [Google Scholar]
Shain 1999 {published data only (unpublished sought but not used)}
- Shain RN, Perdue ST, Piper JM, Holden AEC, Champion JD, Newton ER, et al. Behaviors changed by intervention are associated with reduced STD recurrence. Sexually Transmitted Diseases 2002;29(9):520‐9. [DOI] [PubMed] [Google Scholar]
- Shain RN, Piper JM, Newton ER, Perdue ST, Ramos R, Champion JD, et al. A randomized, controlled trial of a behavioral intervention to prevent sexually transmitted disease among minority women. New England Journal of Medicine 1999;340(2):93‐100. [DOI] [PubMed] [Google Scholar]
- Thurman AR, Holden AEC, Shain RN, Perdue S, Piper JM. Preventing recurrent sexually transmitted diseases in minority adolescents. Obstetrics and Gynecology 2008;111(6):1417‐25. [DOI] [PubMed] [Google Scholar]
Sieving 2012 {published data only}
Stanton 1996 {published data only}
- Stanton B, Fang X, Li X, Feigelman S, Galbraith J, Ricardo I. Evolution of risk behaviors over 2 years among a cohort of urban African American adolescents. Archives of Pediatrics & Adolescent Medicine 1997;151(4):398‐406. [DOI] [PubMed] [Google Scholar]
- Stanton BF, Li X, Ricardo I, Galbraith J, Feigelman S, Kaljee L. A randomized, controlled effectiveness trial of an AIDS prevention program for low‐income African‐American youths. Archives of Pediatrics & Adolescent Medicine 1996;150(4):363‐72. [DOI] [PubMed] [Google Scholar]
Stanton 2005 {published data only}
- Stanton B, Guo J, Cottrell L, Galbraith J, Li X, Gibson C, et al. The complex business of adapting effective interventions to new populations: an urban to rural transfer. Journal of Adolescent Health 2005;37(2):163. [DOI] [PubMed] [Google Scholar]
- Stanton B, Harris C, Cottrell L, Li X, Gibson C, Guo J, et al. Trial of an urban adolescent sexual risk‐reduction for rural youth: a promising but imperfect fit. Journal of Adolescent Health 2006;38(1):25‐36. [DOI] [PubMed] [Google Scholar]
Stephenson 2004 {published data only}
- Stephenson JM, Strange V, Forrest S, Oakley A, Copas A, Allen E, et al. Pupil‐led sex education in England (RIPPLE study): cluster‐randomised intervention trial. Lancet 2004;364(9431):338‐46. [DOI] [PubMed] [Google Scholar]
Thato 2008 {published data only}
- Thato R, Jenkins RA, Dusitsin N. Effects of the culturally‐sensitive comprehensive sex education programme among Thai secondary school students. Journal of Advanced Nursing 2008;62(4):457‐69. [DOI] [PubMed] [Google Scholar]
Tortolero 2008 {published data only}
- Tortolero SR, Markham CM, Addy RC, Baumler ER, Escobar‐Chaves SL, Basen‐Engquist KM, et al. Safer choices 2: rationale, design issues, and baseline results in evaluating school‐based health promotion for alternative school students. Contemporary Clinical Trials 2008;29(1):70‐82. [DOI] [PMC free article] [PubMed] [Google Scholar]
Villarruel 2006 {published data only (unpublished sought but not used)}
- Villarruel AM, Jemmott JB 3rd, Jemmott LS, Ronis DL. Predictors of sexual intercourse and condom use intentions among Spanish‐dominant Latino youth: a test of the planned behavior theory. Nursing Research 2004;53(3):172‐81. [DOI] [PubMed] [Google Scholar]
- Villarruel AM, Jemmott JB III, Jemmott LS. A randomized controlled trial testing an HIV prevention intervention for Latino youth. Archives of Pediatrics & Adolescent Medicine 2006;160(8):772‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Villarruel AM, Jemmott LS, Jemmott JB III. Designing a culturally based intervention to reduce HIV sexual risk for Latino adolescents. Journal of the Association of Nurses in AIDS Care 2005;16(2):23‐31. [DOI] [PubMed] [Google Scholar]
Vogt 2012 {published data only}
- Vogt C, Schaefer M. Knowledge matters — Impact of two types of information brochure on contraceptive knowledge, attitudes and intentions. European Journal of Contraception and Reproductive Health Care 2012;17(2):135‐43. [DOI] [PubMed] [Google Scholar]
Weeks 1997 {published data only}
- Levy SR, Perhats C, Weeks K, Handler AS, Zhu C, Flay BR. Impact of a school‐based AIDS prevention program on risk and protective behavior for newly sexually active students. Journal of School Health 1995;65(4):145‐51. [DOI] [PubMed] [Google Scholar]
- Weeks K, Levy SR, Gordon AK, Handler A, Perhats C, Flay BR. Does parental involvement make a difference? The impact of parent interactive activities on students in a school‐based AIDS prevention program. AIDS Education and Prevention 1997;9(Suppl A):90‐106. [PubMed] [Google Scholar]
Winter 1993 {published data only}
- Winter L, Goldy AS. Effects of prebehavioral cognitive work on adolescents' acceptance of condoms. Health Psychology 1993;12(4):308‐12. [DOI] [PubMed] [Google Scholar]
Zimmerman 2008 {published data only}
References to studies awaiting assessment
Gilliam 2016 {published data only}
- Gilliam M, Hebert L, Brown R, Akinola M, Hill B, Whitaker A, et al. Exploring the feasibility and effectiveness of a contraceptive counseling waiting room app [abstract]. Contraception 2016;94(4):412. [Google Scholar]
Additional references
Abdi 2015
- Abdi J, Eftekhar H, Estebsari F, Sadeghi R. Theory‐based interventions in physical activity: a systematic review of literature in Iran. Global Journal of Health Science 2015;7(3):215‐29. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ajzen 1980
- Ajzen I, Fishbein M. Understanding Attitudes and Predicting Social Behavior. Englewood Cliffs, NJ: Prentice Hall, 1980. [Google Scholar]
Albarracín 2005
- Albarracín D, Gillette JC, Earl AN, Glasman LR, Durantini MR. A test of major assumptions about behavior change: a comprehensive look at the effects of passive and active HIV‐prevention interventions since the beginning of the epidemic. Psychological Bulletin 2005;131(6):856‐97. [DOI] [PMC free article] [PubMed] [Google Scholar]
Amini 2015
- Amini M, Djazayery A, Majdzadeh R, Taghdisi MH, Jazayeri S. Effect of school‐based interventions to control childhood obesity: a review of reviews. International Journal of Preventive Medicine 2015;6:68. [DOI] [PMC free article] [PubMed] [Google Scholar]
Armstrong 2007
- Armstrong R, Waters E, Jackson N, Oliver S, Popay J, Shepherd J, et al. Guidelines for Systematic reviews of health promotion and public health interventions. Version 2. Melbourne University: Australia; 2007. goo.gl/PEUHTL (accessed 23 September 2016).
Bailey 2015
- Bailey J, Mann S, Wayal S, Hunter R, Free C, Abraham C, et al. Sexual health promotion for young people delivered via digital media: a scoping review. Public Health Research 2015;3(13):1‐119. [PubMed] [Google Scholar]
Bandura 1986
- Bandura A. Social Foundations of Thought and Action: A Social Cognitive Theory. Englewood Cliffs, NJ: Prentice Hall, 1986. [Google Scholar]
Baranowski 2002
- Baranowski T, Perry CL, Parcel GS. How individuals, environments, and health behavior interact. Social Cognitive Theory. In: Glanz K, Rimer RK, Lewis FM editor(s). Health Behavior and Health Education. Theory, Research, and Practice. 3rd Edition. San Francisco (CA): Jossey‐Bass, 2002:165‐84. [Google Scholar]
Berhane 2015
- Berhane A, Biadgilign S, Berhane A, Memiah P. Male involvement in family planning program in Northern Ethiopia: an application of the Transtheoretical model. Patient Education and Counseling 2015;98(4):469‐75. [DOI] [PubMed] [Google Scholar]
Borrelli 2011
- Borrelli B. The assessment, monitoring, and enhancement of treatment fidelity in public health clinical trials. Journal of Public Health Dentistry. 2011/04/19 2011; Vol. 71, issue s1:S52‐63. [DOI] [PMC free article] [PubMed]
Campbell 2012
- Campbell MK, Piaggo G, Elbourne DR, Altman DG, CONSORT Group. CONSORT 2010 statement: extension to cluster randomized trials. British Medical Journal 2012;345(Sep 4):e5661. [DOI: 10.1136/bmj.e5661] [DOI] [PubMed] [Google Scholar]
Catania 1990
- Catania JA, Kegeles SM, Coates TJ. Towards an understanding of risk behavior: an AIDS Risk Reduction Model (ARRM). Health Education Quarterly 1990;17(1):53‐72. [DOI] [PubMed] [Google Scholar]
Conner 2005
- Conner M, Norman P. Predicting health behaviour: a social cognition approach. In: Conner M, Norman P editor(s). Predicting Health Behaviour. Second Edition. New York: Open University Press, 2005:1‐27. [Google Scholar]
de Wit 2004
- Wit J, Stroebe W. Social cognition models of health behaviour. In: Kaptein A, Weinman J editor(s). Health Psychology. Oxford: Blackwell Publishing, 2004:52‐83. [Google Scholar]
DeVries 2013
- DeVries H. I‐Change Model. www.maastricht‐university.eu/hein.devries/interests/change (accessed 26 July 2016).
DiCenso 2002
- DiCenso A, Guyatt G, Willan A, Griffith WL. Interventions to reduce unintended pregnancies among adolescents: systematic review of randomized controlled trials. British Medical Journal 2002;324(7351):1426. [DOI] [PMC free article] [PubMed] [Google Scholar]
Espada 2016
- Espada JP, Morales A, Guillen‐Riquelme A, Ballester R, Orgiles M. Predicting condom use in adolescents: a test of three socio‐cognitive models using a structural equation modeling approach. BMC Public Health 2016;16:35. [DOI] [PMC free article] [PubMed] [Google Scholar]
Fishbein 2000
- Fishbein M. The role of theory in HIV prevention. AIDS Care 2000;12(3):273‐8. [DOI] [PubMed] [Google Scholar]
Fisher 1992
- Fisher JD, Fisher WA. Changing AIDS‐risk behavior. Psychological Bulletin 1992;111(3):455‐74. [DOI] [PubMed] [Google Scholar]
Flay 2009
- Flay BR, Snyder F, Petraitis J. The Theory of Triadid Influence. In R J DiClemente, MC Kegler, & RA Crosby (Eds), Emerging Theories in Health Promotion Practice and Research (2nd ed., pp 451‐510. New York: Jossey‐Bass. positiveaction.net/research/downloads/emerging‐theories‐health‐promotion‐2009.pdf (accessed 15 November 2016).
Garbers 2015
- Garbers S, Chiasson MA, Baum R, Tobier N, Ventura A, Hirshfield S. "Get It and Forget It:" online evaluation of a theory‐based IUD educational video in English and Spanish. Contraception 2015;91(1):76‐9. [DOI] [PubMed] [Google Scholar]
Glanz 2010
- Glanz K, Bishop DB. The role of behavioral science theory in development and implementation of public health interventions. Annual Review of Public Health 2010;31:399‐418. [DOI] [PubMed] [Google Scholar]
GRADE 2013
- Schünemann H, Brożek J, Guyatt G, Oxman A. GRADE Handbook [updated October 2013]. http://gdt.guidelinedevelopment.org/central_prod/_design/client/handbook/handbook.html (accessed 29 December 2015).
Halpern 2013
- Halpern V, Lopez L, Grimes DA, Stockton LL, Gallo MF. Strategies to improve adherence and acceptability of hormonal methods of contraception. Cochrane Database of Systematic Reviews 2013, Issue 10. [DOI: 10.1002/14651858.CD004317.pub4] [DOI] [PubMed] [Google Scholar]
Henderson 2011
- Henderson JT, Raine T, Schalet A, Blum M, Harper CC. "I Wouldn't Be this Firm if I Didn't Care": Preventive clinical counseling for reproductive health. Patient Education and Counseling 2011;82(2):254‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. handbook.cochrane.org (accessed 16 August 2016).
Janz 2002
- Janz NK, Champion VL, Strecher VJ. The Health Belief Model. In: Glanz K, Rimer BK, Lewis FM editor(s). Health Behavior and Health Education. Theory, Research, and Practice. 3rd Edition. San Francisco (CA): Jossey‐Bass, 2002:45‐66. [Google Scholar]
Johnston 2008
- Johnston M, Dixon D. Current issues and new direction in psychology and health: What happened to behaviour in the decade of behaviour?. Psychology and Health 2008;23(5):509‐13. [DOI] [PubMed] [Google Scholar]
Lopez 2013
- Lopez LM, Steiner MJ, Grimes DA, Schulz KF. Strategies for communicating contraceptive effectiveness. Cochrane Database of Systematic Reviews 2013, Issue 4. [DOI: 10.1002/14651858.CD006964.pub3] [DOI] [PubMed] [Google Scholar]
Miller 2009
- Miller WR, Rose GS. Toward a theory of motivational interviewing. American Psychologist 2009;64(6):527‐37. [DOI] [PMC free article] [PubMed] [Google Scholar]
Montaño 2002
- Montaño DE, Kasprzyk D. The theory of reasoned action and the theory of planned behavior. In: Glanz K, Rimer BK, Lewis FM editor(s). Health Behavior and Health Education. Theory, Research, and Practice. 3rd Edition. San Francisco, CA: Jossey‐Bass, 2002. [Google Scholar]
Montgomery 2013
- Montgomery P, Grant S, Hopewell S, Macdonald G, Moher D, Michie S, et al. Protocol for CONSORT‐SPI: an extension for social and psychological interventions. Implementation Science 2013;8:99. [DOI] [PMC free article] [PubMed] [Google Scholar]
O'Connor 2003
- O'Connor AM, Stacey D, Rovner D, Holmes‐Rovner M, Tetroe J, Llewellyn‐Thomas H, et al. Decision aids for people facing health treatment or screening decisions. Cochrane Database of Systematic Reviews 2003, Issue 1. [DOI: 10.1002/14651858.CD001431] [DOI] [PubMed] [Google Scholar]
Oringanje 2016
- Oringanje C, Meremikwu MM, Eko H, Esu E, Meremikwu A, Ehiri JE. Interventions for preventing unintended pregnancies among adolescents. Cochrane Database of Systematic Reviews 2016, Issue 2. [DOI: 10.1002/14651858.CD005215.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Prochaska 1992
- Prochaska JO, DiClemente CC, Norcross JC. In search of how people change. Applications to addictive behaviors. American Psychologist 1992;47(9):1102‐14. [DOI] [PubMed] [Google Scholar]
RevMan 2014 [Computer program]
- The Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager (RevMan). Version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Rogers 1983
- Rogers RW. Cognitive and physiological processes in fear appeals and attitude change: a revised Theory of Protection Motivation. In: Cacioppi T, Petty RE editor(s). Social Psychology. New York, NY: Guilford Press, 1983. [Google Scholar]
Schulz 2002
- Schulz KF, Grimes DA. Allocation concealment in randomised trials: defending against deciphering. Lancet 2002;359(9306):614‐8. [DOI] [PubMed] [Google Scholar]
Strauss 2005
- Strauss SE, Richardson WS, Glasziou P, Haynes RB. Evidence‐based Medicine: How to Practice and Teach EBM. Third Edition. New York: Churchill Livingstone, 2005. [Google Scholar]
Terry 1993
- Terry DJ, Gallois C, McCamish M. The Theory of Reasoned Action. Its Application to AIDS‐Preventive Behaviour. Oxford, England: Pergamon Press Ltd, 1993. [Google Scholar]
Tyson 2014
- Tyson M, Covey J, Rosenthal HE. Theory of planned behavior interventions for reducing heterosexual risk behaviors: A meta‐analysis. Health Psychology 2014;33(12):1454‐67. [DOI] [PubMed] [Google Scholar]
Webb 2010
- Webb T, Joseph J, Yardley L, Michie S. Using the internet to promote health behavior change: a systematic review andmeta‐analysis of the impact of theoretical basis, use of behavior change techniques, and mode of delivery on efficacy. Journal of Medical Internet Research 2010;12(1):e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wilson 2015
- Wilson A, Nirantharakumar K, Truchanowicz EG, Surenthirakumaran R, MacArthur C, Coomarasamy A. Motivational interviews to improve contraceptive use in populations at high risk of unintended pregnancy: a systematic review and meta‐analysis. European Journal of Obstetrics, Gynecology, and Reproductive biology 2015;191:72‐9. [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Lopez 2009
- Lopez LM, Tolley EE, Grimes DA, Chen‐Mok M. Theory‐based strategies for improving contraceptive use: a systematic review. Contraception 2009;79:411‐7. [DOI] [PubMed] [Google Scholar]


