Abstract
This study investigated the relationship of childhood adversity and adult sleep quality in 327 college students (91 males), with a mean age of 18.9 years (SD = 2.1); and also examined whether neuroticism significantly mediated the observed association. Regression findings indicate that the relationship between childhood adversity and adult sleep quality is significant, and that there is a stronger association in men. Furthermore, a bootstrapping approach to testing the significance of the indirect effect (i.e., mediation) indicated that neuroticism mediated this relationship in both men and women. These data suggest that otherwise healthy young adults with a history of childhood adversity are at increased risk for sleep disturbance. Neuroticism may represent a potential target for change in future insomnia interventions, particularly in adults with a history of childhood adversity.
Adverse childhood experiences (ACEs), such as physical, sexual, and emotional abuse and neglect, are common and often associated with health and behavioral problems in children (Dubowitz, Papas, Black, & Starr, 2002; Flaherty et al., 2006; Thompson et al., 2005). Consequences of these experiences may endure—ACEs are associated with a host of physical and psychological problems later in life, including increased rates of depression and other psychiatric disorders (Chapman et al., 2004; Felitti et al., 1998), substance use (Kendler et al., 2000), obesity (Felitti et al., 1998; Thomas, Hypponen, & Power, 2008), heart disease (Felitti et al., 1998), increased health care utilization (Chartier, Walker, & Naimark, 2007), and suicide attempts (Dube et al., 2001). In fact, roughly one fourth of adult psychiatric disorders and as many as one half of all suicide attempts are attributable to ACEs (Afifi et al., 2008).
One of the most ubiquitous symptoms to emerge after exposure to a traumatic event is sleep disruption—evidence suggests that trauma exposure may confer risk for sleep difficulties even in the absence of a full-fledged posttraumatic stress disorder (PTSD) diagnosis (Mellman, Aigbogun, Graves, Lawson, & Alim, 2008; Ohayon & Shapiro, 2000; J. Rosen, Reynolds, Yeager, Houck, & Hurwitz, 1991). Most of these investigations have focused on traumatic events that have occurred during adulthood. Some investigators have also examined sleep in children exposed to a traumatic event (Chemtob, Nomura, & Abramovitz, 2008; Mongillo, Briggs-Gowan, Ford, & Carter, 2009), but few studies have examined sleep in adults who have experienced childhood adversity. Evidence of such a relationship would suggest long-lasting effects of adverse experiences on sleep. Two recent studies by Bader and colleagues utilized wrist actigraphy and polysomnography to examine objective sleep disturbance in adults with primary insomnia with and without ACEs (Bader, Schafer, Schenkel, Nissen, Kuhl, et al., 2007; Bader, Schafer, Schenkel, Nissen, & Schwander, 2007). In these small samples (N = 39 and N = 59, respectively), ACEs were found to correlate with worse sleep, including lower sleep efficiency and a greater number of movements during sleep. Another recent study found an association between childhood adversity and self-reported adult sleep quality in a large epidemiological sample, which remained significant even after adjusting for depressive symptoms and recent stressors (Koskenvuo, Hublin, Partinen, Paunio, & Koskenvuo, 2010). However, this investigation did not employ empirically validated measures of ACEs and sleep quality, and participants were not directly queried about exposure to childhood maltreatment including abuse and neglect. Because the effects of abuse, neglect, and other interpersonal insults have been found to be more pernicious than non-interpersonal events (Luthra et al., 2009; Resnick, Kilpatrick, Dansky, Saunders, & Best, 1993), it is desirable to explicitly assess these types of events in studies of childhood adversity. This study would permit partial replication of the previous findings, using a larger sample than that of the studies by Bader and colleagues (Bader, Schafer, Schenkel, Nissen, Kuhl, et al. (2007) and Bader, Schafer, Schenkel, Nissen, and Schwander (2007)); a sample of young adults more proximal to the events in question; and empirically validated measures of sleep quality and ACEs involving abuse and neglect.
Many studies have found that the female gender is associated with increased vulnerability to unfavorable psychosocial outcomes following traumatic events (Fisher et al., 2009; Haatainen et al., 2003; Kessler, Sonnega, Bromet, Hughes, & Nelson, 1995; Stein, Walker, & Forde, 2000). Of the three aforementioned studies on ACEs and adult sleep in the extant literature, two studies reported no gender differences (Bader, Schafer, Schenkel, Nissen, Kuhl, et al., 2007; Bader, Schafer, Schenkel, Nissen, & Schwander, 2007), and one study found the ACEs–adult sleep association to be stronger in women than in men when adjusting for work status and health behaviors (Koskenvuo et al., 2010). The putative female vulnerability to adverse outcomes following ACEs is again tested in this study.
A final aim of this study was to examine one potential pathway by which childhood adversity may exert its influence on adult sleep quality. We chose to examine neuroticism, which refers to one’s general proneness to negative emotions. Neuroticism is one of five core personality domains that emerges during late childhood and becomes increasingly stable into adulthood (Costa & McCrae, 1988; Lamb, Chuang, Wessels, Broberg, & Hwang, 2002). Thus, neuroticism emerges, on average, at the chronological midpoint between ACEs and adult sleep, supporting its exploration as a potential mediator of the ACEs–adult sleep quality relationship. We examined neuroticism, relative to other variables of interest, as it is considered a latent factor underlying the development and maintenance of a range of psychiatric disorders, including anxiety and depression (Brown, 2007). There is evidence from animal (Carroll et al., 2007; Holmes et al., 2005) and clinical studies (Glaser, van Os, Portegijs, & Myin-Germeys, 2006; McFarlane et al., 2005; Roy, 2002) of an association between ACEs and neuroticism in adulthood. Neuroticism has also been implicated in poor sleep (Gau, 2000; Soehner, Kenned, & Monk, 2007; Vincent, Cox, & Clara, 2009; Williams & Moroz, 2009). To our knowledge, there are no published studies examining whether neuroticism mediates the childhood adversity–adult sleep relationship. However, in previous work, the association between ACEs and sleep outcomes was found in individuals without current psychopathology (Bader, Schafer, Schenkel, Nissen, Kuhl, et al., 2007; Bader, Schafer, Schenkel, Nissen, & Schwander, 2007) and while adjusting for current depressive symptoms (Koskenvuo et al., 2010), suggesting that the effects of neuroticism may not fully account for this relationship. Although there may be other variables involved in the association, we would hypothesize that neuroticism partially, but significantly, mediates the ACEs–adult sleep relationship.
Our study hypotheses were as follows:
H1: There will be a significant, inverse relationship between childhood adversity and adult sleep quality.
H2: The relationship will be stronger in women than in men.
H3: Neuroticism will mediate this relationship.
We tested these hypotheses in a sample of undergraduate men and women.
METHOD
Participants
Participants were 327 undergraduate students (236 females and 91 males) at San Diego State University (SDSU). These students completed self-report questionnaires during the first month of the semester in a mass testing session for course credit. Students were then invited to participate in additional testing that involved completion of computer tasks and additional questionnaires (including those examined for this study) if they either (a) were considered “normal” on trait anxiety (i.e., they scored within the 40th-60th percentile during the mass testing session on a measure of trait anxiety not used in this study) or (b) were considered “high trait anxious” by virtue of scoring at or above the 80th percentile on trait anxiety. This selection process was related to hypotheses for a larger study. Two hundred sixty participants (79.5%) had scores in the “normal” range, with the remaining 20.5% (67 participants) in the “high” range. The study was approved by the Human Research Protections Programs of SDSU and the University of California, San Diego; and participants gave informed, written consent to participate.
Measures
ACEs.
The 28-item Childhood Trauma Questionnaire (CTQ) contains five domains that assess levels of physical abuse, emotional abuse, sexual abuse, physical neglect, and emotional neglect experienced during childhood (Bernstein et al., 1994; Bernstein et al., 2003). These domains sum to yield a total score (CTQ Total). Higher scores indicate more extensive endorsement of abuse or neglect. The CTQ has demonstrated adequate internal consistency and test–retest reliability (Bernstein et al., 2003).
Sleep quality.
The Pittsburgh Sleep Quality Index (PSQI; Buysse, Reynolds, Monk, Berman, & Kupfer, 1989) was used to assess sleep quality. The PSQI is a widely used and well-validated 19-item self-report measure of sleep quality. It contains seven subscales measuring domains such as subjective sleep quality, sleep latency, sleep duration, and sleep disturbance, which combine to yield a global composite score of sleep quality over the past week. Global sleep quality scores are continuous (range = 0–21), with high scores (≥6) reflecting poor sleep quality (Buysse et al., 1989). These guidelines were used to categorize participants as either “good sleepers” or “poor sleepers” for some analyses. The PSQI has been demonstrated to have high internal consistency (Cronbach’s α = 0.83), test–retest reliability (0.85–0.87), and convergent validity (Buysse et al., 1989).
Neuroticism.
The Revised NEO Personality Inventory (NEO PI–R) is a 240-item measure of five broad personality domains: neuroticism, extraversion, openness to experience, agree-ableness, and conscientiousness. The NEO PI–R also measures six subordinate domains known as facets for each of the personality domains. It has demonstrated good internal consistency, test–retest reliability, and validity (Costa & McCrae, 1992). For this study, neuroticism was the only domain of interest. T scores were derived from college-age, sex-specific norms (Costa & McCrae, 1992).
Statistical Analysis
All statistical analyses were conducted using Statistical Package for the Social Sciences Version 15.0 (SPSS, Inc., Chicago, IL). Group differences (at an alphalevel of p ≤ .05) on demographic variables, CTQ Total and subscale scores, and neuroticism were assessed by sleep status (good sleepers vs. poor sleepers as defined by global PSQI score) and gender using chi-square or independent-sample t test analyses as appropriate.
A hierarchical linear regression approach was employed to test the first two study hypotheses. First, to assess the relationship between ACEs and sleep quality (H1), linear regression analyses were run with CTQ Total as the predictor and global PSQI score as the outcome variable. Next, to test a possible moderating effect of gender on the relationship between ACEs and sleep quality (H2), CTQ Total and gender were entered on Step 1 of a hierarchical linear regression model (female gender was coded “0,” and male gender was coded “1”). A Gender × CTQ Total interaction term was entered on Step 2. If a significant interaction effect was detected, subsequent analyses would be stratified by gender.
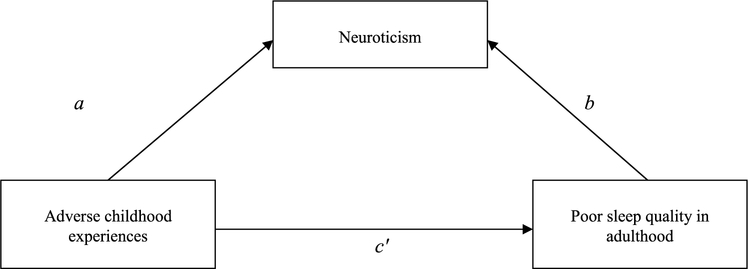
Neuroticism’s role as a potential mediator was assessed by directly testing the significance of its effect (i.e., the indirect effect of X on Y) on the CTQ–PSQI relationship (H3). This indirect effect, as depicted in Figure 1, is quantified as the product of unstandardized regression coefficients for the CTQ–neuroticism relation (Path a) and the neuroticism–PSQI relation (Path b), or ab. In this study, the significance of the indirect effect (ab) was tested using a bootstrapping approach, as recommended by Hayes and colleagues (Hayes, 2009; Preacher & Hayes, 2004). Bootstrapping is a nonparametric method considered to have several advantages over other approaches to testing mediation, such as the “causal effects” approach popularized by Baron and Kenny (1986), which suffers from low power; and the Sobel test, which relies on an assumption that the sampling distribution of the indirect effect is normal (MacKinnon, Lockwood, Hoffman, West, & Sheets, 2002). In bootstrapping, the study sample is re-sampled with replacement multiple times, such that an observation that appears only once in the original sample could potentially appear more than once in a given re-sample. Following recommendations by Hayes, 5,000 bootstrap re-samples were generated in this study. This procedure yields an inference about the size of the indirect effect, a standard error estimate (mean of the standard deviation across the 5,000 re-samples), and 95% confidence intervals based on the distribution of the 5,000 samples. If the confidence interval does not include zero, the indirect effect (i.e., mediation) is considered significant. Finally, for purposes of interpretability and practical significance, an estimation of the effect size of the indirect effect was calculated using methods developed by Fairchild, MacKinnon, Taborga, and Taylor (2009).
FIGURE 1.
Simple mediation model depicting direct and indirect effects of adverse childhood experiences (ACEs) on adult sleep quality. The indirect effect (Path ab) represents the effect of the proposed mediator, neuroticism. The direct effect (Path c′) shows the effects of ACEs on adult sleep quality with the indirect effect (ab) removed.
RESULTS
Demographic and Clinical Characteristics
CTQ Total, neuroticism, and global PSQI scores for females, males, and the total sample are presented in Table 1. There were no significant gender differences on any study variables. In the total sample, 52.5% of study participants (53.2% of females and 50.6% of males χ2(1, 326) = 0.18, p = .669, were considered poor sleepers.
TABLE 1.
Demographic and Clinical Characteristics of the Sample
| Variable | Total Sample | Females | Males |
|---|---|---|---|
| Age: M (SD) | 18.9 (2.1) | 19.0 (2.3) | 18.7 (1.1) |
| Gender (% of total sample) | 327 | 236 (72.2) | 91 (27.8) |
| Ethnicity (%)a | |||
| Caucasian | 173 (52.9) | 130 (55.1) | 43 (47.3) |
| Latino | 65 (19.9) | 45 (19.1) | 20 (22.0) |
| Asian | 57 (17.4) | 40 (16.9) | 17 (18.7) |
| Other | 32 (9.8) | 21 (8.9) | 11 (12.1) |
| CTQ Total (SD) | 35.6 (12.5) | 36.5 (12.8) | 35.9 (12.6) |
| Neuroticism (SD) | 50.1 (10.5) | 49.9 (9.4) | 50.0 (10.2) |
| PSQI global (SD) | 6.2 (3.0) | 6.0 (3.2) | 6.1 (3.1) |
| Poor sleepers (% of total) | 169 (52.5) | 134 (53.2) | 45 (50.6) |
Note. CTQ = Childhood Trauma Questionnaire; PSQI = Pittsburgh Sleep Quality Index.
Percentages may not equal 100 due to missing data.
Good Sleepers Versus Poor Sleepers
Comparisons of clinical characteristics for poor sleepers relative to good sleepers are displayed in Table 2. There were significant differences on CTQ Total score, t(318) = −3.99, p < .001; and neuroticism, t(317) = −7.21, p < .001, indicating more ACEs and higher neuroticism for poor sleepers. For descriptive purposes, CTQ subscale findings are also presented. Poor sleepers were more likely to have experienced several types of ACEs compared to good sleepers.
TABLE 2.
Between-Group Differences on CTQ and Neuroticism for Good Sleepers Versus Poor Sleepers
| Variable | Good sleepers: PSQI ≤ 5 | Poor sleepers: PSQI ≥ 5 | p |
|---|---|---|---|
| CTQ Total score (SD) | 32.9 (11.0) | 38.4 (13.4) | < .001 |
| CTQ subscales (%) | |||
| Emotional abuse | 21.7 | 40.2 | < .001 |
| Physical abuse | 19.7 | 28.4 | ns |
| Sexual abuse | 13.2 | 14.8 | ns |
| Emotional neglect | 23.0 | 39.1 | .002 |
| Physical neglect | 10.5 | 26.2 | < .001 |
| Neuroticism | 46.0 (9.1) | 53.6 (9.7) | < .001 |
Note. CTQ = Childhood Trauma Questionnaire; PSQI = Pittsburgh Sleep Quality Index.
Regression Analyses Testing H1 and H2
Table 3 displays findings for the linear regression analyses that include the total sample. The model displayed in Table 3a tests the bivariate association between CTQ Total and global PSQI (H1). CTQ Total was significantly correlated with global PSQI (β = .26), t(318) = 4.81, p < .001. R2 was .07, suggesting that CTQ Total explained a small, but significant, amount of variance in sleep quality. The model displayed in Table 3b tests whether gender moderates the CTQ Total–global PSQI relationship (H2). The full model containing main and interaction effects was significant, F(3,316) = 9.65, p < .001. Step 2, which contained the interaction term, explained significantly more variance than the main effects model, F(1,316) = 5.25, p = .023 (R2 change = .02). The Gender × CTQ Total interaction term was significant (β = .518), t(316) = 2.29, p = .023, indicating that the CTQ Total–global PSQI association is stronger in men.
TABLE 3a.
Linear Regression Analyses Estimating the Relationship Between CTQ Total and Global PSQI
| Dependent Variable | Predictor | R2 | F | B | SE B | β | p |
|---|---|---|---|---|---|---|---|
| Global PSQI | CTQ | .07 | 23.17 | .06 | .01 | .26 | <.001 |
Note. CTQ = Childhood Trauma Questionnaire; PSQI = Pittsburgh Sleep Quality Index.
TABLE 3b.
Multiple Linear Regression Analyses Estimating Main and Interactions Effects for CTQ Total and Gender on Global PSQI
| Dependent Variable | Predictor | R2 | F | B | SE B | β | p |
|---|---|---|---|---|---|---|---|
| Global PSQI | Step 1: CTQ | .07 | 11.70 | 0.06 | 0.01 | .26 | <.001 |
| Gender | −0.20 | 0.37 | −.03 | .599 | |||
| Step 2: CTQ | .08 | 9.65 | −0.02 | 0.04 | −.09 | .581 | |
| Gender | −2.61 | 1.12 | −.38 | .020 | |||
| CTQ × Gender | 0.07 | 0.03 | .52 | .023 |
Note. CTQ = Childhood Trauma Questionnaire; PSQI = Pittsburgh Sleep Quality Index.
To better understand the effects of gender on the CTQ–PSQI relationship, subsequent analyses were stratified by gender.
Tests of Mediation (H3)
Table 4 displays results for tests of the indirect effect of CTQ Total on PSQI in men and women, respectively. Note that a formal p value is not shown, as this test relies on an assumption of normality of the sampling distribution of ab and, as such, is not reported in favor of a bootstrapping approach to testing indirect effects, which does not make this assumption (Preacher & Hayes, 2008). As the confidence intervals for ab do not include zero, it can be concluded that neuroticism significantly mediates the relationship between CTQ Total and global PSQI in both men and women.
TABLE 4.
Test of the Significance of Neuroticism as a Mediator of the Childhood Adversity–Adult Sleep Quality Relationship in Men and Women (5,000 Bootstraps)
| 95% Confidence Interval | ||||
|---|---|---|---|---|
| Variable | Point Estimate of the Indirect Effect (ab) | SE | Lower | Upper |
| Men | .041 | .016 | .015 | .079 |
| Women | .024 | .006 | .012 | .038 |
Note. P values for the indirect effect are not reported here as it assumes a normal sampling distribution of the indirect effect, which tends to be skewed (MacKinnon, Lockwood, Hoffman, West, & Sheets, 2002). Significance of indirect effect is instead determined by the 95% confidence interval. ab = indirect effect.
Interpretability and Practical Significance of the Indirect Effect
To translate the indirect effect into a value with practical significance, an estimate of effect size, R2, was calculated for women and men using methods developed by Fairchild et al. (2009) to gauge the proportion of variance accounted for in an outcome variable by the indirect effect. In women, R2 was .029, indicating that 2.9% of the variance in PSQI is accounted for by the indirect effect of CTQ through neuroticism. As the R2 for the full model in women was .211, the proportion of variance accounted for in the model by the indirect effect of neuroticism was .029/.211 = .137; that is, 13.7% of the variance in the full model is through the mediated effect. In men, R2 of the indirect effect was .137, indicating that 13.7% of the variance in PSQI is accounted for by the indirect effect of neuroticism. The R2 for the full model in men was .293, and the proportion of variance accounted for in the model by the indirect effect of neuroticism was .137/.293 = .468; indicating that 46.8% of the variance in the full model is due to the mediated effect. Thus, a sizeable portion of the variance in adult sleep quality is explained by the mediating effect of neuroticism.
DISCUSSION
The goal of this study was to examine the relationship between ACEs and adult sleep, the role of gender, and the extent to which this putative relation may be mediated by neuroticism in a young adult sample. These findings suggest that there is a significant relationship between childhood adversity and adult sleep, that there are gender differences in this relationship, and that it is partially mediated by neuroticism.
As predicted in H1, a statistically significant inverse relationship was detected between ACEs and adult sleep quality in the total sample. This is notable, as few previous studies have examined the relationship between ACEs and adult sleep (Bader, Schafer, Schenkel, Nissen, Kuhl, et al., 2007; Bader, Schafer, Schenkel, Nissen, & Schwander, 2007; Koskenvuo et al., 2010). This study, which features a relatively large sample size and uses empirically validated self-report measures, corroborates the previous findings. Taken together, these data suggest that the repercussions of childhood adversity extend into early adulthood. This sample primarily consisted of college freshman, with a mean age of 18.9 years, and so one could infer that the reported ACEs occurred in the fairly recent past for participants who endorsed these events. Thus, it is unclear whether the same strength of association would be found in an older sample of adults more temporally distant from ACEs. Nonetheless, these findings are clinically significant in light of data suggesting that the presence of current sleep disturbance signifies increased risk of future onset of psychiatric disorders, such as depression and anxiety (Chang, Ford, Mead, CooperPatrick, & Klag, 1997; Johnson, Roth, & Breslau, 2006; Ohayon & Roth, 2003). The presence of both ACEs and sleep problems could conceivably confer even greater risk for these outcomes.
H2 specified that the relationship between ACEs and adult sleep quality would be stronger in women. Contrary to our predictions, these data suggest that the ACEs–sleep relationship is more robust in men. This gender difference emerged despite the fact that there were no significant differences between men and women on any of the self-report measures included in this analysis. This is also in contrast to the three published studies on ACEs and adult sleep, of which two studies found no gender differences (Bader, Schafer, Schenkel, Nissen, Kuhl, et al., 2007; Bader, Schafer, Schenkel, Nissen, & Schwander, 2007), and one study found the relationship to be stronger in women relative to men when adjusting for work status and health behaviors (Koskenvuo et al., 2010). It may be that methodological differences between the studies, including variables assessed, led to these disparate results. This finding is also in contrast with much of the broader literature on gender differences in trauma sequelae, which suggests that adverse outcomes following trauma exposure are either more prevalent or more severe in women (Fisher et al., 2009; Haatainen et al., 2003; Kessler et al., 1995; Stein et al., 2000). However, some investigations have found no differences between men and women, particularly once the higher prevalence of reported sexual abuse in women is taken into account (L. N. Rosen & Martin, 1996; Roy & Janal, 2006; Young, Harford, Kinder, & Savell, 2007). One study actually found increased rates of depression and anxiety symptoms in men receiving treatment for sexual abuse relative to female patients (Gold, Lucenko, Elhai, Swingle, & Sellers, 1999). On the other hand, a recent meta-analysis concluded that women fared worse even when type of abuse was taken into account (Tolin & Foa, 2006). Thus, general conclusions regarding gender differences in trauma sequelae are not possible at this time, although one might question the assumption of female vulnerability to adverse outcomes following ACEs in all instances. With regard to sleep outcomes in particular, it appears that healthy young adults with histories of ACEs are at increased risk for sleep disturbance, and these findings suggest that the risk for men may equal or exceed that for women.
Finally, H3, which stated that neuroticism would mediate the relationship between childhood adversity and sleep quality, was supported by these findings. The mediating effect of neuroticism was significant and accounted for 2.9% of the variance in adult sleep quality in women and as much as 13.7% of the variance in adult sleep quality in men. These findings would perhaps suggest gender differences in the extent to which neuroticism mediates the ACEs–sleep quality relationship; however, as we had no hypotheses regarding strength of mediation in men versus women (which would be consistent with mediated moderation or moderated mediation models; e.g., Muller, Judd, & Yzerbyt, 2005), this was not tested statistically in this study. What can be said, based on these findings, is that neuroticism appears to have a significant role in the pathway from ACEs to adult sleep problems in both men and women. Extrapolating to clinical populations, neuroticism may represent a potential future target for treatment, as it is possible that interventions that change one’s general tendency to experience negative affect (or, conversely, that succeed in increasing positive emotions) may lead to improvements in sleep in individuals with a history of ACEs. For example, perhaps cognitive behavioral therapy for insomnia could be augmented to include elements that also target neuroticism. Indeed, whereas neuroticism is generally considered to be a stable personality trait in adulthood, change in levels of neuroticism during treatment has been found to be associated with improved outcomes (Quilty, Meusel, & Bagby, 2008).
Although these findings indicate that neuroticism partially mediates the ACEs–adult sleep quality relationship, what additional mechanisms might explain the association? Although a full discussion of putative mechanisms is beyond the scope of this study, there are some key possibilities that are worth mentioning. First, several neurobiological mechanisms are likely involved (although some of these may actually represent neural substrates of neuroticism). Early adversity has been linked to alterations of the hypothalamic–pituitary–adrenal (HPA) axis (Heim et al., 2000; MacMillan et al., 2009), serotonergic abnormalities (Bhansali, Dunning, Singer, David, & Schmauss, 2007; Kaufman et al., 2004), and differences in amgydala activity (Law, Pei, Feldon, Pryce, & Harrison, 2009; Sabatini et al., 2007). These systems are closely tied to the regulation of sleep, and there is evidence that each is also involved in sleep disruption (Barrett et al., 2009; Benca, Obermeyer, Shelton, Droster, & Kalin, 2000; Hatzinger, Hemmeter, Brand, Ising, & Holsboer-Trachsler, 2004; Mehlman et al., 2000). Second, the presence of physical disorders may impact the relationship between ACEs and adult sleep. ACEs are associated with increased prevalence of physical disorders in adulthood, and physical disorders are, in turn, linked with poor sleep quality (Stein, Belik, Jacobi, & Sareen, 2008). Consequences of physical disorders, such as chronic pain or breathing difficulties, have the potential to impact sleep quality. Third, an environmental explanation has been posited, which states that children who grow up with exposure to ACEs are more likely to live in chaotic family environments where few stable routines, such as regular bed times, bedtime rituals, and so forth, exist (Gregory, Caspi, Moffitt, & Poulton, 2006). Thus, these individuals, having never been taught good sleep hygiene, may continue to engage in behaviors incongruent with good sleep quality even as adults. Further research will be necessary to clarify these and other possible mechanisms involved in the ACEs–sleep quality relationship.
These findings should be interpreted in light of a number of significant limitations. First, this study was done using a relatively homogenous university student sample. Therefore, caution should be used in generalizing these findings to other age groups, to the general population, or to patient populations. Because these participants were selected based on being in the “high” or “normal” range on trait anxiety, these findings may also not be representative of a general undergraduate sample. Second, the association between ACEs and adult sleep quality found here is only one “snapshot” of the relationship in young adults. This tells us little about the strength of the association at earlier or later points in life, or whether these gender differences seen here persist over time—for example, it is quite possible that the ACEs–sleep quality relationship becomes stronger in women at a later point in life, which would be consistent with previous research that has found a stronger relationship in adult women relative to men. Longitudinal studies would be necessary to investigate the trajectory of these relationships over longer periods. Third, these findings rely on self-report measures, including retrospective reports of ACEs that may have occurred many years prior to this assessment. However, here the young ages of the participants may be advantageous; they are less temporally removed from the time of the ACEs relative to most adult samples, and so their memory and self-reports of ACEs may be even more reliable. Furthermore, previous research suggests that retrospective reports of childhood maltreatment are valid and may actually provide an underestimation of the incidence of moderate to severe ACEs (Hardt & Rutter, 2004).
In conclusion, results suggest that childhood trauma is associated with poor sleep quality in adulthood among young men and women. This relationship may be stronger in men, and neuroticism partially mediates the association. Future studies that investigate these associations in a more diverse sample with regard to age and over longer follow-up periods would strengthen these findings. In addition, future investigators may wish to examine whether associations with adult sleep vary by type of ACEs. This study suggests that even otherwise healthy young adults who have experienced ACEs may be experiencing current sleep disturbance and, thus, may be at increased risk for psychiatric disorders in the future. If these findings are replicated, neuroticism may represent an additional target for change in interventions to improve sleep.
ACKNOWLEDGMENTS
This work was funded by the following: National Institutes of Mental Health (NIMH) Grant #T32 MH018399 (Holly J. Ramsawh); National Institute of Aging Grant #R01 AG008415 and the VA Center for Stress and Mental Health (Sonia Ancoli-Israel); and NIMH Grant #K24 MH064122 (Murray B. Stein). Dr. Ancoli-Israel receives or has received research funding from the following: Sepracor, Inc. and Litebook, Inc. She currently serves or has served as a consultant on the Scientific Advisory Board for the following: Ferring Pharmaceuticals, Inc.; GlaxoSmithKline; Merck; NeuroVigil, Inc.; Orphagen Pharmaceuticals; Pfizer; Respironics; Sanofi-Aventis; Sepracor, Inc.; and Schering-Plough. Dr. Stein receives or has in the past three years received research support from the following: Eli Lilly and Company, GlaxoSmithKline, and Hoffmann-La Roche Pharmaceuticals. He is currently or in the past 3 years has been a consultant for the following: AstraZeneca; BrainCells, Inc.; Bristol-Myers Squibb; Comprehensive NeuroScience; Eli Lilly and Company; Forest Laboratories; Hoffmann-La Roche Pharmaceuticals; Jazz Pharmaceuticals; Johnson & Johnson; Mindsite; Pfizer; Sepracor, Inc.; and Transcept Pharmaceuticals, Inc.
REFERENCES
- Afifi TO, Enns MW, Cox BJ, Asmundson GJG, Stein MB, & Sareen J (2008). Population attributable fractions of psychiatric disorders and suicide ideation and attempts associated with adverse childhood experiences. American Journal of Public Health, 98, 946–952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bader K, Schafer V, Schenkel M, Nissen L, Kuhl HC, & Schwander J (2007). Increased nocturnal activity associated with adverse childhood experiences in patients with primary insomnia. Journal of Nervous and Mental Disease, 195, 588–595. [DOI] [PubMed] [Google Scholar]
- Bader K, Schafer V, Schenkel M, Nissen L, & Schwander J (2007). Adverse childhood experiences associated with sleep in primary insomnia. Journal of Sleep Research, 16, 285–296. [DOI] [PubMed] [Google Scholar]
- Baron RM, & Kenny DA (1986). The moderator mediator variable distinction in social psychological research—Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology, 51, 1173–1182. [DOI] [PubMed] [Google Scholar]
- Barrett CE, Noble P, Hanson E, Pine DS, Winslow JT, & Nelson EE (2009). Early adverse rearing experiences alter sleep–wake patterns and plasma cortisol levels in juvenile rhesus monkeys. Psychoneuroendocrinology, 34, 1029–1040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benca RM, Obermeyer WH, Shelton SE, Droster J, & Kalin NH (2000). Effects of amygdala lesions on sleep in rhesus monkeys. Brain Research, 879, 130–138. [DOI] [PubMed] [Google Scholar]
- Bernstein DP, Fink L, Handelsman L, Foote J, Lovejoy M, Wenzel K, et al. (1994). Initial reliability and validity of a new retrospective measure of child abuse and neglect. American Journal of Psychiatry, 151, 1132–1136. [DOI] [PubMed] [Google Scholar]
- Bernstein DP, Stein JA, Newcomb MD, Walker E, Pogge D, Ahluvalia T, et al. (2003). Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child Abuse and Neglect, 27, 169–190. [DOI] [PubMed] [Google Scholar]
- Bhansali P, Dunning J, Singer SE, David L, & Schmauss C (2007). Early life stress alters adult serotonin 2C receptor pre-mRNA editing and expression of the alpha subunit of the heterotrimeric G-protein Gq. Journal of Neuroscience, 27, 1467–1473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown TA (2007). Temporal course and structural relationships among dimensions of temperament and DSM–IV anxiety and mood disorder constructs. Journal of Abnormal Psychology, 116, 313–328. [DOI] [PubMed] [Google Scholar]
- Buysse DJ, Reynolds CF, Monk TH, Berman SR, & Kupfer DJ (1989). The Pittsburgh Sleep Quality Index—A new instrument for psychiatric practice and research. Psychiatry Research, 28, 193–213. [DOI] [PubMed] [Google Scholar]
- Carroll JC, Boyce-Rustay JM, Millstein R, Yang R, Wiedholz LM, Murphy DL, et al. (2007). Effects of mild early life stress on abnormal emotion-related behaviors in 5-HTT knockout mice. Behavior Genetics, 37, 214–222. [DOI] [PubMed] [Google Scholar]
- Chang PP, Ford DE, Mead LA, CooperPatrick L, & Klag MJ (1997). Insomnia in young men and subsequent depression—The Johns Hopkins Precursors Study. American Journal of Epidemiology, 146, 105–114. [DOI] [PubMed] [Google Scholar]
- Chapman DP, Whitfield CL, Felitti VJ, Dube SR, Edwards VJ, & Anda RF (2004). Adverse childhood experiences and the risk of depressive disorders in adulthood. Journal of Affective Disorders, 82, 217–225. [DOI] [PubMed] [Google Scholar]
- Chartier MJ, Walker JR, & Naimark B (2007). Childhood abuse, adult health, and health care utilization: Results from a representative community sample. American Journal of Epidemiology, 165, 1031–1038. [DOI] [PubMed] [Google Scholar]
- Chemtob CM, Nomura Y, & Abramovitz RA (2008). Impact of conjoined exposure to the World Trade Center attacks and to other traumatic events on the behavioral problems of preschool children. Archives of Pediatrics and Adolescent Medicine, 162, 126–133. [DOI] [PubMed] [Google Scholar]
- Costa PT, & McCrae RR (1988). Personality in adulthood—A 6-year longitudinal study of self-reports and spouse ratings on the NEO Personality Inventory. Journal of Personality and Social Psychology, 54, 853–863. [DOI] [PubMed] [Google Scholar]
- Costa PT, & McCrae RR (1992). Revised NEO Personality Inventory and NEO Five Factor Inventory professional manual. Odessa, FL: Psychological Assessment Resources. [Google Scholar]
- Dube SR, Anda RF, Felitti VJ, Chapman DP, Williamson DF, & Giles WH (2001). Childhood abuse, household dysfunction, and the risk of attempted suicide throughout the life span—Findings from the adverse childhood experiences study. Journal of the American Medical Association, 286, 3089–3096. [DOI] [PubMed] [Google Scholar]
- Dubowitz H, Papas MA, Black MM, & Starr RH (2002). Child neglect: Outcomes in high-risk urban preschoolers. Pediatrics, 109, 1100–1107. [DOI] [PubMed] [Google Scholar]
- Fairchild AJ, MacKinnon DP, Taborga MP, & Taylor AB (2009). R-2 effect-size measures for mediation analysis. Behavior Research Methods, 41, 486–498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, et al. (1998). Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults—The adverse childhood experiences (ACE) study. American Journal of Preventive Medicine, 14, 245–258. [DOI] [PubMed] [Google Scholar]
- Fisher H, Morgan C, Dazzan P, Craig TK, Morgan K, Hutchinson G, et al. (2009). Gender differences in the association between childhood abuse and psychosis. British Journal of Psychiatry, 194, 319–325. [DOI] [PubMed] [Google Scholar]
- Flaherty EG, Thompson R, Litrownik AJ, Theodore A, English DJ, Black MM, et al. (2006). Effect of early childhood adversity on child health. Archives of Pediatrics and Adolescent Medicine, 160, 1232–1238. [DOI] [PubMed] [Google Scholar]
- Gau SF (2000). Neuroticism and sleep-related problems in adolescence. Sleep, 23, 495–502. [PubMed] [Google Scholar]
- Glaser JP, van Os J, Portegijs PJM, & Myin-Germeys I (2006). Childhood trauma and emotional reactivity to daily life stress in adult frequent attenders of general practitioners. Journal of Psychosomatic Research, 61, 229–236. [DOI] [PubMed] [Google Scholar]
- Gold SN, Lucenko BA, Elhai JD, Swingle JM, & Sellers AH (1999). A comparison of psychological psychiatric symptomatology of women and men sexually abused as children. Child Abuse and Neglect, 23, 683–692. [DOI] [PubMed] [Google Scholar]
- Gregory AM, Caspi A, Moffitt TE, & Poulton R (2006). Family conflict in childhood: A predictor of later insomnia. Sleep, 29, 1063–1067. [DOI] [PubMed] [Google Scholar]
- Haatainen KM, Tanskanen A, Kylma J, Honkalampi K, Koivumaa-Honkanen H, Hintikka J, et al. (2003). Gender differences in the association of adult hopelessness with adverse childhood experiences. Social Psychiatry and Psychiatric Epidemiology, 38, 12–17. [DOI] [PubMed] [Google Scholar]
- Hardt J, & Rutter M (2004). Validity of adult retrospective reports of adverse childhood experiences: Review of the evidence. Journal of Child Psychology and Psychiatry, 45, 260–273. [DOI] [PubMed] [Google Scholar]
- Hatzinger M, Hemmeter UM, Brand S, Ising M, & Holsboer-Trachsler E (2004). Electroencephalographic sleep profiles in treatment course and long-term outcome of major depression: Association with DEX/CRH-test response. Journal of Psychiatric Research, 38, 453–465. [DOI] [PubMed] [Google Scholar]
- Hayes AF (2009). Beyond Baron and Kenny: Statistical mediation analysis in the new millennium. Communication Monographs, 76, 408–420. [Google Scholar]
- Heim C, Newport DJ, Heit S, Graham YP, Wilcox M, Bonsall R, et al. (2000). Pituitary–adrenal and autonomic responses to stress in women after sexual and physical abuse in childhood. Journal of the American Medical Association, 284, 592–597. [DOI] [PubMed] [Google Scholar]
- Holmes A, le Guisquet AM, Vogel E, Millstein RA, Leman S, & Belzung C (2005). Early life genetic, epigenetic and environmental factors shaping emotionality in rodents. Neuroscience and Biobehavioral Reviews, 29, 1335–1346. [DOI] [PubMed] [Google Scholar]
- Johnson EO, Roth T, & Breslau N (2006). The association of insomnia with anxiety disorders and depression: Exploration of the direction of risk. Journal of Psychiatric Research, 40, 700–708. [DOI] [PubMed] [Google Scholar]
- Kaufman J, Yang BZ, Douglas-Palumberi H, Houshyar S, Lipschitz D, Krystal JH, et al. (2004). Social supports and serotonin transporter gene moderate depression in maltreated children. Proceedings of the National Academy of Sciences USA, 101, 17316–17321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendler KS, Bulik CM, Silberg J, Hettema JM, Myers J, & Prescott CA (2000). Childhood sexual abuse and adult psychiatric and substance use disorders in women—An epidemiological and Cotwin control analysis. Archives of General Psychiatry, 57, 953–959. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Sonnega A, Bromet E, Hughes M, & Nelson CB (1995). Posttraumatic stress disorder in the National Comorbidity Survey. Archives of General Psychiatry, 52, 1048–1060. [DOI] [PubMed] [Google Scholar]
- Koskenvuo K, Hublin C, Partinen M, Paunio T, & Koskenvuo M (2010). Childhood adversities and quality of sleep in adulthood: A population-based study of 26,000 Finns. Sleep Medicine, 11, 17–22. [DOI] [PubMed] [Google Scholar]
- Lamb ME, Chuang SS, Wessels H, Broberg AG, & Hwang CP (2002). Emergence and construct validation of the Big Five factors in early childhood: A longitudinal analysis of their ontogeny in Sweden. Child Development, 73, 1517–1524. [DOI] [PubMed] [Google Scholar]
- Law AJ, Pei Q, Feldon J, Pryce CR, & Harrison PJ (2009). Gene expression in the anterior cingulate cortex and amygdala of adolescent marmoset monkeys following parental separations in infancy. International Journal of Neuropsychopharmacology, 12, 761–772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luthra R, Abramovitz R, Greenberg R, Schoor A, Newcorn J, Schmeidler J, et al. (2009). Relationship between type of trauma exposure and posttraumatic stress disorder among urban children and adolescents. Journal of Interpersonal Violence, 24, 1919–1927. [DOI] [PubMed] [Google Scholar]
- MacKinnon DP, Lockwood CM, Hoffman JM, West SG, & Sheets V (2002). A comparison of methods to test mediation and other intervening variable effects. Psychological Methods, 7, 83–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacMillan HL, Georgiades K, Duku EK, Shea A, Steiner M, Niec A, et al. (2009). Cortisol response to stress in female youths exposed to childhood maltreatment: Results of the Youth Mood Project. Biological Psychiatry, 66, 62–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McFarlane A, Clark CR, Bryant RA, Williams LM, Niaura R, Paul RH, et al. (2005). The impact of early life stress on psychophysiological, personality and behavioral measures in 740 non-clinical subjects. Journal of Integrative Neuroscience, 4, 27–40. [DOI] [PubMed] [Google Scholar]
- Mehlman PT, Westergaard GC, Hoos BJ, Sallee FR, Marsh S, Suomi SJ, et al. (2000). CSF5-HIAA and nighttime activity in free-ranging primates. Neuropsychopharmacology, 22, 210–218. [DOI] [PubMed] [Google Scholar]
- Mellman TA, Aigbogun N, Graves RE, Lawson WB, & Alim TN (2008). Sleep paralysis and trauma, psychiatric symptoms and disorders in an adult African American population attending primary medical care. Depression and Anxiety, 25, 435–440. [DOI] [PubMed] [Google Scholar]
- Mongillo EA, Briggs-Gowan M, Ford JD, & Carter AS (2009). Impact of traumatic life events in a community sample of toddlers. Journal of Abnormal Child Psychology, 37, 455–468. [DOI] [PubMed] [Google Scholar]
- Muller D, Judd CM, & Yzerbyt VY (2005). When moderation is mediated and mediation is moderated. Journal of Personality and Social Psychology, 89, 852–863. [DOI] [PubMed] [Google Scholar]
- Ohayon MM, & Roth T (2003). Place of chronic insomnia in the course of depressive and anxiety disorders. Journal of Psychiatric Research, 37, 9–15. [DOI] [PubMed] [Google Scholar]
- Ohayon MM, & Shapiro CM (2000). Sleep disturbances and psychiatric disorders associated with posttraumatic stress disorder in the general population. Comprehensive Psychiatry, 41, 469–478. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, & Hayes AF (2004). SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behavior Research Methods Instruments and Computers, 36, 717–731. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, & Hayes AF (2008). Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods, 40, 879–891. [DOI] [PubMed] [Google Scholar]
- Quilty LC, Meusel LAC, & Bagby RM (2008). Neuroticism as a mediator of treatment response to SSRIs in major depressive disorder. Journal of Affective Disorders, 111, 67–73. [DOI] [PubMed] [Google Scholar]
- Resnick HS, Kilpatrick DG, Dansky BS, Saunders BE, & Best CL (1993). Prevalence of civilian trauma and posttraumatic stress disorder in a representative national sample of women. Journal of Consulting and Clinical Psychology, 61, 984–991. [DOI] [PubMed] [Google Scholar]
- Rosen J, Reynolds CF, Yeager AL, Houck PR, & Hurwitz LF (1991). Sleep disturbances in survivors of the Nazi Holocaust. American Journal of Psychiatry, 148, 62–66. [DOI] [PubMed] [Google Scholar]
- Rosen LN, & Martin L (1996). Impact of childhood abuse history on psychological symptoms among male and female soldiers in the U.S. Army. Child Abuse and Neglect, 20, 1149–1160. [DOI] [PubMed] [Google Scholar]
- Roy A (2002). Childhood trauma and neuroticism as an adult: Possible implication for the development of the common psychiatric disorders and suicidal behaviour. Psychological Medicine, 32, 1471–1474. [DOI] [PubMed] [Google Scholar]
- Roy A, & Janal M (2006). Gender in suicide attempt rates and childhood sexual abuse rates: Is there an interaction? Suicide and Life-Threatening Behavior, 36, 329–335. [DOI] [PubMed] [Google Scholar]
- Sabatini MJ, Ebert P, Lewis DA, Levitt P, Cameron JL, & Mirnics K (2007). Amygdala gene expression correlates of social behavior in monkeys experiencing maternal separation. Journal of Neuroscience, 27, 3295–3304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soehner AM, Kenned KS, & Monk TH (2007). Personality correlates with sleep–wake variables. Chronobiology International, 24, 889–903. [DOI] [PubMed] [Google Scholar]
- Stein MB, Belik SL, Jacobi F, & Sareen J (2008). Impairment associated with sleep problems in the community: Relationship to physical and mental health comorbidity. Psychosomatic Medicine, 70, 913–919. [DOI] [PubMed] [Google Scholar]
- Stein MB, Walker JR, & Forde DR (2000). Gender differences in susceptibility to posttraumatic stress disorder. Behaviour Research and Therapy, 38, 619–628. [DOI] [PubMed] [Google Scholar]
- Thomas C, Hypponen E, & Power C (2008). Obesity and type 2 diabetes risk in midadult life: The role of childhood adversity. Pediatrics, 121, E1240–E1249. [DOI] [PubMed] [Google Scholar]
- Thompson R, Briggs E, English DJ, Dubowitz H, Lee LC, Brody K, et al. (2005). Suicidal ideation among 8-year-olds who are maltreated and at risk: Findings from the LONGSCAN studies. Child Maltreatment, 10, 26–36. [DOI] [PubMed] [Google Scholar]
- Tolin DF, & Foa EB (2006). Sex differences in trauma and posttraumatic stress disorder: A quantitative review of 25 years of research. Psychological Bulletin, 132, 959–992. [DOI] [PubMed] [Google Scholar]
- Vincent N, Cox B, & Clara I (2009). Are personality dimensions associated with sleep length in a large nationally representative sample? Comprehensive Psychiatry, 50, 158–163. [DOI] [PubMed] [Google Scholar]
- Williams PG, & Moroz TL (2009). Personality vulnerability to stress-related sleep disruption: Pathways to adverse mental and physical health outcomes. Personality and Individual Differences, 46, 598–603. [Google Scholar]
- Young MS, Harford KL, Kinder B, & Savell JK (2007). The relationship between childhood sexual abuse and adult mental health among undergraduates—Victim gender doesn’t matter. Journal of Interpersonal Violence, 22, 1315–1331. [DOI] [PubMed] [Google Scholar]