Abstract
A prenatal care provider’s recommendation for maternal vaccines is one of the strongest predictors of vaccine acceptance during pregnancy. Aside from basic talking points, few resources exist to help obstetric care providers effectively navigate conversations with vaccine hesitant patients. This paper describes the development and acceptability of “VaxChat,” an hour-long, evidence-based video tutorial aimed at improving obstetric care providers’ ability to promote maternal vaccines. Between June and November 2017, 62 obstetric care providers registered to receive continuing medical education credit for viewing VaxChat. Of the post-tutorial responses received, over 90% said VaxChat increased their knowledge of what to say to vaccine hesitant patients, increased their confidence in addressing vaccinations with their pregnant patients, and will help them improve their practice culture regarding maternal vaccine promotion. Eighty percent intend to change how they approach vaccine conversations. These data suggest VaxChat may be a welcome complement to existing provider-to-patient talking points.
Keywords: maternal vaccination, nfluenza, Tdap, provider-patient communication, vaccine hesitancy, provider education
Introduction
In 2018 in the United States (U.S.), maternal immunization rates for influenza and tetanus, diphtheria and acellular pertussis (Tdap) vaccines were estimated to be 50% and 54%, respectively.1 In February 2015, the U.S. National Vaccine Advisory Committee released a report enumerating specific areas for action for improving uptake of recommended vaccines during pregnancy.2 Two of their five recommendations focused on improving vaccine-related communication with pregnant women: enhancing communication to address the safety and effectiveness of currently recommended vaccines and maximizing obstetrical care provider interpersonal communication through recommendation and administration of recommended vaccines. Given that a strong provider recommendation has been shown repeatedly to be one of the most influential factors in a woman’s decision to accept and obtain maternal vaccines,3–9 enhancing obstetric care providers’ ability to converse with patients about immunizations is an important area for intervention. While static vaccine-related provider-to-patient talking points have been developed for maternal vaccine promotion,10 VaxChat is the first tutorial known to explicitly educate providers on how, when, and why to employ specific evidence-based communication strategies regarding maternal vaccination with pregnant women.11 This paper describes the development and provider acceptability of the VaxChat tutorial.
Methods
The VaxChat educational tutorial was developed as the primary obstetric provider-focused component of the P3+ maternal vaccine promotion study (P3+ study). The P3+ study is an NIH-funded cluster-randomized trial aimed at evaluating the effectiveness of a suite of interventions at the patient-, provider- and practice-levels on acceptance of maternal and infant vaccines. The practice and provider interventions were implemented in 11 intervention group practices in Georgia and Colorado. Ten practices without provider- and practice- level interventions served as controls. Full details of the study design, intervention package components, and its effectiveness on vaccine-related outcomes will be made available upon study completion.
Theoretical underpinnings and content of the VaxChat tutorial
The VaxChat tutorial is grounded in five theoretical constructs from established behavioral frameworks and theories, each relating to vaccine promotion in distinct, evidence-based ways. These include disease salience,12,13 myth correction,14 nudge theory,15–18 presumptive communication19,20 and motivational interviewing (MI).21,22 [Table 1] Disease salience ensures providers clearly convey the severity of vaccine-preventable diseases in ways that appropriately inform the obstetric patient without unduly scaring her. Effectively conveying disease salience entails realizing when and how to pivot to discussing disease risks. Myth correction involves learning the psychology behind effectively debunking a myth and the pitfalls of lingering in conversation about a myth for too long. Nudge theory, as aligned with behavioral economics, leverages the power of defaults such as subtle conversational cues or practice-level adaptations that make vaccine acceptance the established norm.
Table 1.
The five theoretical underpinnings of the VaxChat tutorial and their applicability to maternal vaccine promotion
| Theoretical construct | Premise | Applicability to maternal vaccine promotion |
|---|---|---|
| Disease salience | Making individuals aware of the severity of diseases and their susceptibility to them | Ensuring women are informed of the risks vaccine-preventable diseases pose to themselves and their infants |
| Nudge theory | Utilization of indirect suggestions to influence behavior change and decision-making | Use of pro-vaccination defaults in provider-to-patient conversations (e.g. presumptive communication) and adoption of practice-level adaptations (e.g. standing orders) that promote vaccination as the norm |
| Myth correction | Knowing when and how to correct myths or misperceptions without inadvertently reinforcing myths | Educating providers on when to avoid lingering in a conversation about a myth and how to effectively debunk the myth if necessary |
| Presumptive communication | A communication technique that assumes acceptance or agreement with a desired outcome | Provider initiation of all vaccine-related conversations assumes the patient will accept the vaccine |
| Motivational interviewing | A provider-directed, yet client-centered approach to clinical discourse that is grounded in provider empathy, mutual trust, and patient self-efficacy and autonomy. | Can help vaccine hesitant patients articulate their concerns, remain open to advice, and consider changing their mind on vaccine receipt |
Presumptive communication can be considered one form a “nudge,” but holds particular salience for vaccine promotion. Under the presumptive communication approach, vaccine conversations are initiated under the assumption that the patient will accept the vaccine. For instance, instead of saying, “Would you like your Tdap vaccine today?” a provider using the presumptive approach would state, “It’s time for your Tdap vaccine today.” This reframing conveys vaccination is the standard, putting the onus on the patient to opt-out of the assumed norm of vaccine receipt. While the presumptive approach can be used to initiate vaccine conversations with all patients, the principles espoused in MI can be effective with patients who resist. Motivational interviewing is more participatory, eliciting behavior change through provider-directed, yet client-centered discourse grounded in the principles of provider empathy, mutual trust and patient self-efficacy and autonomy.23 MI can help hesitant individuals articulate their concerns, remain open to the provider’s professional advice, and find the motivation to consider changing their stance on vaccine receipt.
Development of VaxChat also was informed by three additional considerations. Vaccine strategies promoted in the tutorial were: 1) evidence-based,24 2) explained how to address common vaccine-related myths, and 3) conveyed that convincing a reluctant individual to accept a vaccine goes beyond information provision and involves connecting with a patient’s underlying values or worldviews.25 The tutorial describes findings from studies in vaccine promotion20,26,27 while integrating relevant lessons from related fields including psychology,12,14,28,29 sociology,30 behavioral economics,31 and persuasion theory.32 Presenting evidence-based vaccine promotion strategies, in combination with insights and lessons derived from proximal fields, makes this tutorial unique in its approach.
The hour-long tutorial includes a video-recorded welcome and introduction, a narrated slide-based tutorial covering evidence-based strategies for clinical vaccine promotion, and three video-recorded vignettes illustrating application of the strategies in realistic clinical scenarios.33 The introduction and narration are provided by a maternal vaccine promotion researcher who introduces herself in her professional capacity and in her role as a mother. Presenting her dual roles conveys trust and empathy, as well as relatability as a scientific colleague, a mother, and an obstetric patient. Following the introduction, the narrated slide-based portion of the tutorial begins with an explanation of why making prenatal care providers confident communicators about vaccines is important, and it emphasizes that all topics covered are evidence-based. When lessons are derived from original research studies, the studies are referenced and key findings summarized to impress their clinical effectiveness upon the viewers.
The evidence-based vaccine promotion strategies that the VaxChat tutorial covers are presentedin 10 key points organized into 3 modules: message framing, message content, and practice culture. [Figure 1] We chose this organizational structure to maximize impact on our target audience of practicing obstetric care providers. Clinicians on our tutorial development team suggested that vaccine providers are typically interested in what to say, how to say it, and in what context. The tutorial defines message framing as the structure of message delivery and message content as what a provider says to a patient and when. Practice culture refers to the strategies and policies implemented at the practice-level that support and bolster provider efforts to encourage vaccine acceptance.
Figure 1.
Ten evidence-based key points emphasized in VaxChat educational tutorial
The video-recorded vignettes demonstrate how to use the multiple strategies described during the didactic portion of the tutorial as research in other arenas has revealed success in affecting behavior change when communication strategies are explicitly illustrated in realistic scenarios.33,34 The first scenario depicts a pregnant woman expressing concerns about harming the baby. She is specifically concerned about the vaccines’ safety on her growing fetus. In the second scenario, a patient believes the myth that vaccines cause autism. This patient is very vaccine hesitant and is more interested in “natural” approaches to health and wellness. The final vignette illustrates a situation in which a woman’s husband is skeptical of maternal vaccination, thus the scene depicts a physician navigating a joint appointment with the woman and her husband. In this scenario, the couple expresses hesitancy to deviate from the opinions and conventions of their friends and family. All three of the vignettes illustrate patient concerns encountered routinely by obstetric care providers.35
Incentives and tutorial deployment
To incentivize viewership of VaxChat, we obtained continuing medical education (CME) and continuing nursing education (CNE) accreditation for the tutorial via the Emory University CME/CNE offices. For physicians, viewing the tutorial was also one required component to obtain maintenance of certification (MOC) Part IV credit via the American Board of Obstetricians and Gynecologists, an additional incentive provided to physicians from intervention group practices participating in the P3+ study.
The VaxChat educational tutorial was made available to all clinical staff within the 11 intervention practices in June 2017. A designated “immunization champion” staff member at each practice was responsible for notifying colleagues about the availability of the tutorial. These immunization champions provided the tutorial login and CME/CNE credit acquisition information to clinical staff within their practice and encouraged participation during the course of module’s availability. The study protocol and intervention package (including the VaxChat tutorial) was reviewed and approved by the Emory Institutional Review Board.
The stated learning objectives of the tutorial were to: 1) learn the theories and strategies of effective communication about vaccines with all pregnant patients, 2) understand how to implement those communication strategies, and 3) learn practice-level strategies to standardize vaccination in the obstetric care setting. To obtain CME/CNE credit, each provider was prompted to answer 10 evaluation questions at the end of the tutorial; these questions were the only interactive questions included in the tutorial. These questions were as follows: two Likert-scale questions, “The presentation was well organized,” and “The presentation met its stated learning objectives,” each with response options strongly disagree, disagree, neutral, agree and strongly agree; “Was the presentation free of commercial bias” (Yes/No); three scaled questions, “This activity increased my knowledge of what to say to vaccine hesitant patients,” “This activity increased my confidence in addressing vaccinations with my pregnant patients,” and “This activity will help me improve my practice culture regarding maternal vaccine promotion,” with response options “None,” “Somewhat,” and “Significantly.” Three additional dichotomous questions were asked including “Do you intend to change the way you approach conversations with vaccine hesitant patients,” Are there any barriers to prevent changes, and if so, how will your address these,” and “Do you intend to change your practice flow or culture in regards to maternal vaccine promotion?” The final question was an open-ended question asking, “What other learning opportunities do you feel are needed?”
Results
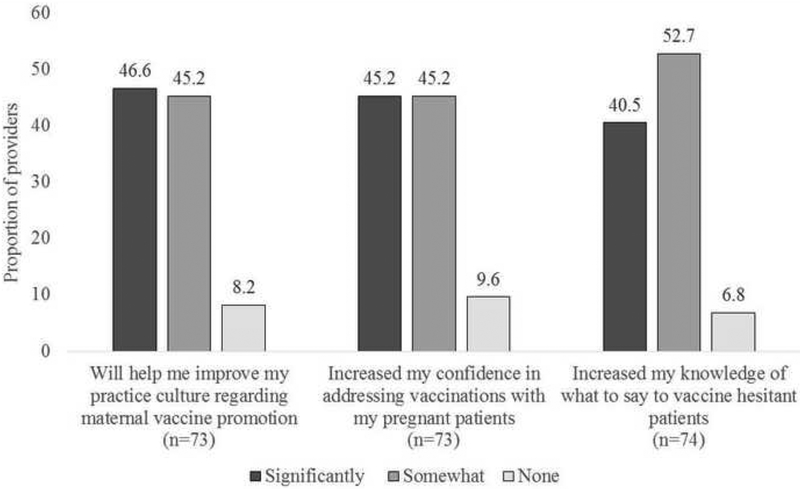
By November 1, 2017, 62 obstetric care providers had registered for CME or CNE credit upon viewing VaxChat. [Table 2] Thirty-three (53%) were from Colorado and 29 (47%) were from Georgia. Data from the post-tutorial questions were provided in aggregate by the Emory University CME/CNE office staff. Data from 76 responses were provided; this number exceeded the number of individuals taking the tutorial due to a requirement to repeat the evaluation questions to obtain the completion certificate again (if misplaced, for instance). Responses were not linked to identifying information, so we were unable to identify and remove duplicates. Of the responses, 93% indicated VaxChat was well-organized, 92% felt it met its stated learning objectives, and 96% believed it to be free of commercial bias. Over 90% said VaxChat increased their knowledge of what to say to vaccine hesitant patients, increased their confidence in addressing vaccinations with their pregnant patients, and will help them improve their practice culture regarding maternal vaccine promotion [Figure 2]. Over eighty percent (82%) indicated they intended to change the way they approach conversations with vaccine-hesitant patients, 87% reported no barriers to preventing changes in how they approach conversations, and 69% indicated an intention to change their practice flow or culture regarding maternal vaccine promotion. Four respondents provided concrete recommendations for further learning opportunities and resources: a desire for web links mentioned in the video for use on their own website, fact sheets or scripts for nursing staff, more education about group-B strep, and patient-focused posters that list statistics regarding pregnancy and newborn disease related to influenza and pertussis.
Table 2.
Location and provider types of VaxChat CME/CNE registrants
| Colorado (n=33) | Georgia (n=29) | Total (n=62) | |
|---|---|---|---|
| Provider type | n (%) | n (%) | n (%) |
| MD/DO | 11 (33.3) | 15 (51.7) | 26 (41.9) |
| Certified Nurse Midwife | 20 (60.6) | 9 (31.0) | 29 (46.8) |
| Nurse Practitioner | 2 (6.1) | 4 (13.8) | 6 (9.7) |
| Medical Assistant | 0 (0.0) | 1 (3.4) | 1 (1.6) |
Abbreviations: MD, Medical Doctor; DO, Doctor of Osteopathy
Figure 2.
Perceptions of clinical utility of the VaxChat educational tutorial among practicing obstetric care providers
Discussion
Obstetric provider endorsement is one of the strongest predictors of vaccine receipt for pregnant women.3–8 For providers, strongly recommending an influenza or a Tdap vaccine to a woman with concerns can prove challenging. Because one size may not fit all when it comes to vaccine promotion, more emphasis needs to be placed on teaching providers evidence-based strategies for how to assess patient concerns and handle conversations accordingly. VaxChat fills this educational void in ways that Vaccine Information Statement (VIS) sheets and other stand-alone talking point lists do not. With over 80% of post-tutorial responses indicating a willingness to change how conversations with vaccine-hesitant patients are approached, VaxChat may be a welcome and broadly scalable provider-level intervention.
There are limitations to this evaluation. First, these data only reflect feedback from obstetric care providers who registered to receive CME or CNE credit for viewing the tutorial. It does not include responses from providers who may have taken the tutorial without seeking educational credit. Second, because the Emory University CME/CNE office could only supply anonymized post-tutorial data in aggregate, we were unable to quantify the number of duplicate responses and remove those associated with individuals who may have taken the post-tutorial questionnaire more than once. Despite the limitations, this study suggests the tutorial was generally well-received and educational.
Through efforts to understand vaccine decision-making, we have come to learn that decisions to accept or refuse vaccines can be influenced by myriad factors including values, worldviews, familial norms, scientific knowledge, public health awareness, misperceptions and provider endorsement. For pregnant women, certain considerations can become more or less important due to the additional desire to protect the developing fetus. VaxChat has the potential to be widely implemented, facilitating obstetric providers in effectively tailoring vaccine-related communication with pregnant women to reduce vaccine hesitancy and increase maternal and infant vaccine uptake.
Funding:
This work was support by the National Institutes of Health [grant number R01AI110482 (All authors)]. The funder had no role in the design and conduct of the study; collection, management, analysis, or interpretation of the data; or preparation, review or approval of the manuscript.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Declaration of interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
- Allison Chamberlain is a paid consultant with the American College of Obstetricians and Gynecologists (ACOG) on vaccine-related topics.
- Kevin Ault is a member of the federal Advisory Committee on Immunization Practices (ACIP) and advises the American College of Obstetricians and Gynecologists (ACOG) on immunization policy.
- Daniel Salmon has done grant and consulting support for Pfizer, Walgreen’s, and Merck.
- Matthew Dudley has received funding support from Walgreen’s.
References
- 1.Kahn KE, Black CL, Ding H, et al. Influenza and Tdap Vaccination Coverage Among Pregnant Women - United States, April 2018. MMWR Morbidity and mortality weekly report. 2018;67(38):1055–1059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.The National Vaccine Advisory Committee: Reducing Patient and Provider Barriers to Maternal Immunizations: Approved by the National Vaccine Advisory Committee on June 11, 2014. Public Health Reports. 2015;130(1):10–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Meharry P, Colson E, Grizas A, Stiller R, Vázquez M. Reasons Why Women Accept or Reject the Trivalent Inactivated Influenza Vaccine (TIV) During Pregnancy. Matern Child Health J. 2013;17(1):156–164. [DOI] [PubMed] [Google Scholar]
- 4.Beel E, Rench M, Montesinos D, Mayes B, Health C. Knowledge and attitudes of postpartum women toward immunization during pregnancy and the peripartum period. Human Vaccines and Immunotherapeutics. 2013;9(9). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Marsh H, Malik F, Shapiro E, Omer S, Frew P. Message Framing Strategies to Increase Influenza Immunization Uptake Among Pregnant African American Women. Matern Child Health J. 2014;18(7):1639–1647. [DOI] [PubMed] [Google Scholar]
- 6.Chamberlain AT, Seib K, Ault KA, et al. Improving influenza and Tdap vaccination during pregnancy: a cluster-randomized trial of a multi-component antenatal vaccine promotion package in late influenza season. Vaccine. 2015; 33(30): 3571–3579. [DOI] [PubMed] [Google Scholar]
- 7.Moniz M, Vitek W, Akers A, Meyn L, Beigi R. Perceptions and acceptance of immunization during pregnancy. J Reprod Med 2013;58:383–388. [PubMed] [Google Scholar]
- 8.Healy CM, Rench MA, Montesinos DP, Ng N, Swaim LS. Knowledge and attitiudes of pregnant women and their providers towards recommendations for immunization during pregnancy. Vaccine. 2015;33(41):5445–5451. [DOI] [PubMed] [Google Scholar]
- 9.Kharbanda EO, Vargas CY, Castaño PM, Lara M, Andres R, Stockwell MS. Exploring pregnant women’s views on influenza vaccination and educational text messages. Preventive Medicine. 2011;52(1):75–77. [DOI] [PubMed] [Google Scholar]
- 10.American College of Obstetricians and Gynecologists. Maternal Immunization Toolkit. Available at: http://immunizationforwomen.org/providers/resources/toolkits/maternalimmunizations.php. Accessed on 12/12/2018.
- 11.Ellingson MK, Dudley MZ, Limaye RJ, Salmon DA, O’Leary ST, Omer SB. Enhancing uptake of influenza maternal vaccine. Expert review of vaccines. 2018. (Published ahead of print.) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Witte K Putting the fear back into fear appeals: the extended parallel process model. Commun Monogr. 1992;59:329–349. [Google Scholar]
- 13.Brewer NT, Chapman GB, Gibbons FX, Gerrard M, McCaul KD, Weinstein ND. Meta-analysis of the relationship between risk perception and health behavior: the example of vaccination. Health psychology. 2007;26(2):136–145. [DOI] [PubMed] [Google Scholar]
- 14.Cook J, Lewandowsky S. The Debunking Handbook St. Lucia, Australia: University of Queensland; 2011. [Google Scholar]
- 15.Milkman KL, Beshears J, Choi JJ, Laibson D, Madrian BC. Using implementation intentions prompts to enhance influenza vaccination rates. Proceedings of the National Academy of Sciences of the United States of America. 2011;108(26):10415–10420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chapman GB, Li M, Colby H, Yoon H. Opting in vs opting out of influenza vaccination. JAMA. 2010;304(1):43–44. [DOI] [PubMed] [Google Scholar]
- 17.Thaler RH, S CR. Nudge: improving decisions about health, wealth and happiness. New York (NY): Penguin Books; 2008. [Google Scholar]
- 18.Halpern SD, Ubel PA, Asch DA. Harnessing the power of default options to improve health care. NEJM. 2007;357(13):1340–1344. [DOI] [PubMed] [Google Scholar]
- 19.Brewer NT, Hall ME, Malo TL, Gilkey MB, Quinn B, Lathren C. Announcements Versus Conversations to Improve HPV Vaccination Coverage: A Randomized Trial. Pediatrics. 2017;139(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Opel DJ, Heritage J, Taylor JA, et al. The architecture of provider-parent vaccine discussions at health supervision visits. Pediatrics. 2013;132(6):1037–1046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dempsey AF, Pyrznawoski J, Lockhart S, et al. Effect of a Health Care Professional Communication Training Intervention on Adolescent Human Papillomavirus Vaccination: A Cluster Randomized Clinical Trial. JAMA Pediatr. 2018;172(5):e180016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Reno JE, O’Leary S, Garrett K, et al. Improving Provider Communication about HPV Vaccines for Vaccine-Hesitant Parents Through the Use of Motivational Interviewing. Journal of health communication. 2018;23(4):313–320. [DOI] [PubMed] [Google Scholar]
- 23.Miller RW, Rollnick S. Motivational Interviewing: Preparing People for Change. New York: Guilford Press; 2002. [Google Scholar]
- 24.Mazzoni SE, Brewer SE, Pyrzanowski JL, et al. Effect of a multi-modal intervention on immunization rates in obstetrics and gynecology clinics. American Journal of Obstetrics & Gynecology. 2016;214(5):617.e611–617.e617. [DOI] [PubMed] [Google Scholar]
- 25.Omer SB, Amin AB, Limaye RJ. Communicating about vaccines in a fact-resistant world. JAMA Pediatrics. 2017;171(10):929–930. [DOI] [PubMed] [Google Scholar]
- 26.Nyhan B, Reifler J, Richey S, Freed GL. Effective Messages in Vaccine Promotion: A Randomized Trial. Pediatrics. 2014:e835–842. [DOI] [PubMed] [Google Scholar]
- 27.Sadique MZ, Devlin N, Edmunds WJ, Parkin D. The effect of perceived risks on the demand for vaccination: results from a discrete choice experiment. PloS one. 2013;8(2):e54149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Haidt J The Righteous Mind: why good people are divided by politics and religion. New York: Random House; 2012. [Google Scholar]
- 29.Borrelli B, Riekert KA, Weinstein A, Rathier L. Brief motivational interviewing as a clinical strategy to promote asthma medication adherence. The Journal of allergy and clinical immunology. 2007;120(5):1023–1030. [DOI] [PubMed] [Google Scholar]
- 30.Communication in Medical Care: Interaction between Primary Care Physicians and Patients. Cambridge: Cambridge University Press; 2006. [Google Scholar]
- 31.Kahneman D Thinking, fast and slow (1st ed.). New York: Farrar, Straus and Giroux; 2011. [Google Scholar]
- 32.Hovland CI, Janis IL, Kelley HH. Communication and Persuasion: psychological studies of opinion change. New Haven: Yale University Press; 1953. [Google Scholar]
- 33.Taylor PJ, Russ-Eft DF, Chan DW. A meta-analytic review of behavior modeling training. The Journal of applied psychology. 2005;90(4):692–709. [DOI] [PubMed] [Google Scholar]
- 34.Hillen MA, van Vliet LM, de Haes HCJM, Smets EMA. Developing and administering scripted video vignettes for experimental research of patient–provider communication. Patient Education and Counseling. 2013;91(3):295–309. [DOI] [PubMed] [Google Scholar]
- 35.O’Leary ST, Riley LE, Lindley MC, et al. Obstetrician–Gynecologists’ Strategies to Address Vaccine Refusal Among Pregnant Women. Obstetrics & Gynecology. 2019;133(1): 40–47. [DOI] [PMC free article] [PubMed] [Google Scholar]