Abstract
Aims:
This study was designed to examine the roles of neighborhood social cohesion and parenting stress in influencing maternal mental health outcomes among primarily low-income, unmarried, urban mothers.
Methods:
Structural equation modeling was utilized with cross-sectional Fragile Families and Child Wellbeing Study data (N=3,876) to test the hypotheses that neighborhood social cohesion would be associated with depression and anxiety among mothers with children age 3 and that this relationship would be mediated by parenting stress.
Results:
The mediation model demonstrated good fit (χ2 (796) = 3169.07, p <.001; CFI = 0.96; RMSEA = 0.028 [90% CI: 0.027, 0.029]). Parenting stress partially mediated the effect of social cohesion on maternal depression (indirect effect: −0.04, p < 0.001) and anxiety (indirect effect: −0.05, p < 0.001); higher reported neighborhood social cohesion was associated with lower parenting stress, which was associated with a decreased likelihood of maternal anxiety and depression.
Conclusion:
Efforts to bolster neighborhood social cohesion may improve maternal mental health outcomes by reducing parenting stress.
Keywords: Anxiety, depression, mothers, neighborhood, parenting, psychological stress, social environment, social capital
Introduction
Maternal depression and anxiety are endemic and have substantial individual, familial, and societal consequences. Given that treatment rates for maternal depression and anxiety are low, efforts toward prevention and amelioration of these conditions, outside of traditional medical and mental health facilities—via increased understanding of contextual factors influencing maternal depression and anxiety—is needed. In this study, we sought to examine the roles of neighborhood social cohesion and parenting stress in influencing maternal mental health outcomes.
Maternal Depression and Anxiety
Maternal depression and anxiety are increasingly recognized as a substantial public health challenge. A United States’ (US) epidemiological survey found that more than 10% of mothers (with children age 18 or younger) met the criteria for major depressive disorder within the previous year; approximately half reported receiving treatment (Ertel, Rich-Edwards, & Koenen, 2011). The prevalence of maternal anxiety has been less studied—particularly outside of the perinatal period—but is gaining recent attention in the literature as a frequent and growing problem. Paul and colleagues (2013) reported that postpartum anxiety is a common phenomenon experienced at higher rates than depression among mothers immediately after childbirth and consistently through six months postpartum. Studies show that 3.7 – 20% of women experience postpartum anxiety and that maternal anxiety and depression often occur together (Leach, Poyser, & Fairweather-Schmidt, 2017; Warnock, Craig, Bakeman, Castral, & Mirlashari, 2016). If left untreated, maternal depression and anxiety can result in mothers’ severe psychosocial impairment (Lindahl, Pearson, & Colpe, 2005; Wisner et. al., 2013), mortality (Oates, 2003), compromised mother-child relationships (O’Higgins, Roberts, Glover, & Taylor, 2013), arrested child development (Apter-Levy, Feldman, Vakart, Ebstein, & Feldman, 2013; Beck, 1998; Gress-Smith, Leucken, Lemery-Chalfant, & Howe, 2012; Stewart, 2007) poor mental health in offspring (Glover, 2014; Goodman et al., 2011; Nilsen, Gustavson, Kjeldsen, Røysamb, & Karevold, 2013), loss of productivity, and significant social and economic consequences (Sontag-Padilla, Schultz, Reynolds, Lovejoy, & Firth, 2013).
Neighborhood Social Cohesion, Parenting Stress, and Mental Health
Neighborhood social cohesion refers to the level of trusting relationships and collective social norms among individuals in a shared community (Kawachi, & Berkman, 2000; Sampson, Raudenbush, & Earls, 1997). Social cohesion has been described as multi-faceted and inclusive of a social order, shared values and civic culture, an interactive social network, and a source of connection, belonging, identity, and solidarity (Forrest & Kearns, 2001). Such positive social connections are well-known to support mental health (Kawachi & Berkman, 2001). While higher levels of social cohesion may provide protection against poor mental health in high-poverty neighborhoods (Fone et al., 2014), reports of neighborhood social cohesion tend to be lower among mothers reporting higher levels of neighborhood social disorder (Franco et al., 2010; Wilmot & Dauner, 2017) and higher levels of parenting stress (Maguire-Jack & Wang, 2016)
Parenting stress refers to processes and subsequent reactions that result from attempting to manage the challenges and burdens of parenthood (Deater-Deckard, 2008). Research using 2003–2004 National Survey of Children’s Health data found at least one parent reporting high parenting stress in approximately 13% of households (Raphael, Zhang, Lius, & Giardino, 2010). While some parenting stress is normal and expected, persistent and high levels of parenting stress have been implicated in various negative outcomes, such as increased risk for maternal depression and anxiety (Leigh & Milgrom, 2008; Nam, Wikoff, & Sherraden, 2015; Quittner, Glueckauf, & Jackson, 1990; Vismara et al., 2016). It is essential to note that parenting stress may be particularly salient for lower-income and single-parent households (Parkes, Sweeting, & Wight, 2015; Raphael et al., 2010) and those experiencing economic hardship—difficulty paying bills or affording basic needs (Williams, Cheadler, & Goosby, 2015). One study using Fragile Families and Child Wellbeing Study data found that urban mothers with young children had an increased likelihood of depression if they reported higher levels of economic hardship and parenting stress (Manuel, Martinson, Bledsoe-Mansori, & Bellamy, 2012). Emotional and instrumental support from partners was associated with a significant reduction in odds of experiencing maternal depression. The authors call for broader efforts toward bolstering social and community support, while also working to reduce parents’ chronic economic and parenting stress that disproportionately burden low-income families.
Furthermore, low-income families are frequently exposed to greater levels of neighborhood disadvantage which has been related to reduced financial and social support (Turney & Harknett, 2010). The literature is rich in terms of highlighting the negative impact of neighborhood disadvantage and disorder on both parenting stress and parental depression particularly for low-income parents (Cassells & Evans, 2017). Parenting stress, in poor and disorganized neighborhoods, may trigger parents’ psychological distress and hypervigilant parenting in an effort to maintain children’s safety; parents’ perceived neighborhood stress may also have an enduring influence on both parenting and parents’ distress over time (Cassell & Evans, 2017). What is less researched, however, is how positive neighborhood factors, such as social cohesion, may bolster against both parenting stress and parental psychological distress. Moreover, the majority of maternal mental health research focuses on the perinatal period, while there is limited examination of maternal depression and anxiety after children pass infancy. Thus, this study sought to examine whether or not higher levels of perceived neighborhood social cohesion is directly associated with reduced maternal depression and anxiety, among primarily low-income, unmarried women with young children (age three)—in and of itself—but also by reducing parenting stress.
Theoretical Framework
The theoretical approach to this study was informed by Pearlin’s stress process model (1989; 1990) which focuses attention to the structural origins of stressors (e.g. racism, classism and low socioeconomic status) as they relate to health outcomes and disparities. In this view, we would expect that primarily low-income, single mothers would be experiencing increased levels of stress. Additionally, low neighborhood social cohesion may serve as a kind of structural stressor that contributes to parenting stress and poor health outcomes. By taking a strengths-based approach, we sought to examine whether or not higher levels of reported neighborhood social cohesion would be associated with reduced parenting stress and better maternal mental health outcomes. Previous research has suggested that more positive relationships between neighbors and perceived trust in a community—neighborhood social cohesion—can result in increased mutual aid, such as assisting with childcare, and providing emotional and concrete support (Brisson, 2015; Maguire-Jack & Showalter, 2016). In turn, neighborhood social cohesion may reduce parenting stress and subsequent mental health challenges.
The Present Study
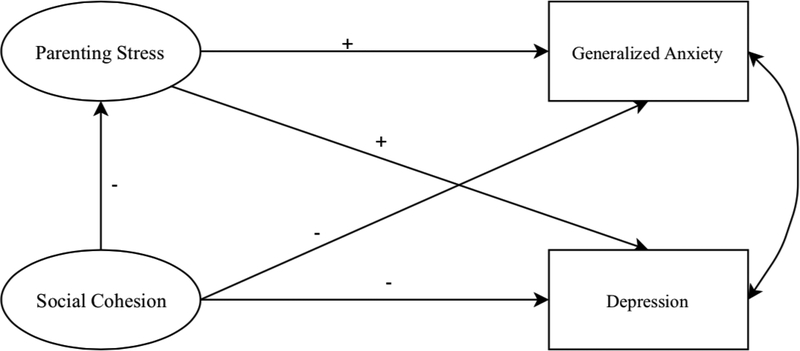
To gain improved understanding of the influences of social cohesion on mental health among mothers of young children (age three), this study answers two research questions: (1) Is neighborhood social cohesion associated with maternal depression and anxiety? (2) Is the association between neighborhood social cohesion and mothers’ depression and anxiety mediated by parenting stress? We hypothesized that higher levels of perceived neighborhood social cohesion would be associated with less maternal depression and anxiety and that parenting stress would mediate this association. See Figure 1 for the conceptual framework that guided the study.
Figure 1.
Conceptual model
Materials and Methods
Source of Data and Sample
This study is a secondary data analysis using data from the core mother survey of the Fragile Families and Child Wellbeing Study (FFCWS)—a longitudinal study that consists of six waves of data and follows a large cohort of children and their parents. This project was exempt from IRB review as the data are absent of identifiers and are publicly available. The original core mother survey included 4,898 mothers who were recruited from 20 large US cities from 1998 – 2000. Data collected included information on demographic characteristics, mothers’ relationships, mothers’ and children’s health status, parenting behaviors, and neighborhood characteristics at the focal child’s birth, and again at ages 1, 3, 5, 9 and 15. The current study used cross-sectional data from the core mother survey at child’s age three. We were interested in the maternal mental health experiences of mothers with young children—age 3—as opposed to those with children 1 year postpartum because there is less research on this time point in the life course. Additionally, FFCWS age three data represents the only wave where all variables of interest were measured. Because neighborhood social cohesion, depression, anxiety, and parenting stress were not consistently measured at each wave, a longitudinal design could not be used to answer the research questions. Using pairwise deletion to deal with missing data, our final sample included 3,876 mothers.
Measures
Social Cohesion.
Mothers’ perception of social cohesion was measured with the Social Cohesion and Trust Scale (Sampson et al., 1997). The 5-item scale consists of statements measuring perceived neighborhood social cohesion such as “people in this neighborhood can be trusted,” “people in this neighborhood generally don’t get along with each other” and “people in this neighborhood do not share the same values”. Mothers reported their perceived social cohesion on a 5-point agreement scale from “strongly agree” to “strongly disagree.” Three positively worded items were reverse coded so that higher scores indicated better social cohesion. The internal consistency of this scale was good (α = 0.80).
Major Depression.
Major depression was assessed using the Composite International Diagnostic Interview-Short Form (CIDI-SF), Section A (Kessler et al., 1998). According to the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) criteria for major depressive episode, participants who endorsed having two weeks of dysphoria or anhedonia symptoms were asked seven follow-up questions related to depressive symptoms. The scores were summed and constructed as a binary variable: “Mother meets depression criteria” (1 = Yes for scores > 3; 0 = No for scores ≤ 3).
Generalized Anxiety Disorder.
Generalized anxiety disorder was measured using a short form of the CIDI-SF scale. Mothers reported their individual worrisome or anxious symptoms such as irritability, having trouble falling asleep, and tiring easily that lasted for at least six months. Responses that endorsed all of the following four criteria: sufficient duration of anxiety (at least six months); worry about more than one thing; lack of control of their anxieties; and showing at least three of the seven physiological symptoms asked in the survey equated to “mother meets anxious criteria.” This variable was constructed as a binary variable (1 =Yes; 0 = No).
Parenting stress.
Parenting stress was measured using a self-reported 12-item scale. The 12 items (e.g. “Do you often have the feeling that you cannot handle things very well?”, “Do you feel alone and without friends?”, “Are you less interested in people than you used to be?”) were adapted from the Home Observation for Measurement of the Environment (HOME) Inventory (Caldwell & Bradley, 1984). Mothers indicated their capability of handling the parent role on a 5-point response scale (1=strongly agree to 5=strongly disagree). All twelve items were reverse coded so that higher scores indicated higher parental stress and more negative feelings toward parenting. Cronbach’s α was 0.87 for this study sample.
Control variables.
Control variables included demographic variables such as race (White, Black, Hispanic, Other), mother’s education, immigration status, mother’s relationship status with focal child’s biological father when child was born and at child’s age three (1 = married; 0= not married), marital status at child’s age three, number of children under age 18 in the household, child’s gender and temperament at age one, and household poverty at child’s age three. Meeting the criteria for major depressive episode (1= Yes; 0 = No) and generalized anxiety disorder (1 = Yes; 0 = No) at child’s age one were also were also included as control variables, as a previous history of depression and anxiety is a risk factor for later depression and anxiety (Delaney, 2017).
Analysis Plan
Structural Equation Modeling (SEM) was conducted using MPlus 8.0 (2017). In the models, neighborhood social cohesion and parenting stress represented latent variables. Maternal depression and anxiety were observed, binary variables. First, the direct relationships between social cohesion and maternal depression and generalized anxiety disorder were examined. Then, following the mediation test approach suggested by Baron and Kenny (1986), the mediation model was performed to test parenting stress as the mediator of the relationship (see Figure 1). First, the direct effects of social cohesion were tested. Second, the indirect effects from social cohesion to the mediator (parenting stress) and then to the outcomes—maternal depression and anxiety—were estimated. The Bootstrap estimation procedure was conducted to estimate the significance of the indirect effects. Since chi-square is highly sensitive to large sample sizes, it may not be a good model fit indicator for this study sample; thus it is reported alongside alternate fit indices. Model fit was evaluated using the Comparative Fit Index (CFI), Root Mean Square Error of Approximation (RMSEA) and its confidence intervals (CI), and Weighted Root Mean Square Residual (WRMR). A CFI above 0.95, RMSEA less than or equal to 0.05 (RMSEA CI lower value near 0, upper value ≤ .05), and WRMR below 1.0 indicates acceptable model fit (Hu & Bentler, 1999; MacCallum, Browne, & Sugawara, 1996; Yu, 2002). Because the WRMR is a relatively newer fit statistic and has received limited research (Muthén, 1998 – 2004), we do not rely heavily on this parameter. Missing data was handled using pairwise deletion and the weighted least square parameter estimator (WLSMV) was used as appropriate for ordinal and non-normal data.
Results
Sample Characteristics
Demographic characteristics of the sample (N = 3,876) are summarized in Table 1. Participants’ average age was 28. About half of the participants were Black (48%), followed by Hispanic (25.90%), White (22.50%), and Other (3.60%); 30.75% of the mothers reported not completing a high school education. Approximately one-quarter of the participants married their child’s biological father (25.59%) and participants reported having approximately two children under age 18 living with them. In the previous wave (child’s age one), 15.45% of respondents met the criteria for major depressive episode and 3.17% met the criteria for generalized anxiety disorder. At child’s age three, 20.6% of mothers met the criteria major depression and 4.6% of mothers met the criteria for generalized anxiety disorder. The correlation between study variables are presented in Table 2. The correlation between social cohesion and parenting stress was −0.21.
Table 1.
Participant Characteristics (N=3,876)
| M (SD) | Range | % | |
|---|---|---|---|
| Age | 28.17 (6.05) | 16–50 | |
| Number of children under 18 in household | 2.32 (1.34) | 0–10 | |
| Race | |||
| White | 22.50 | ||
| Black | 48.00 | ||
| Hispanic | 25.90 | ||
| Other | 3.60 | ||
| Education | |||
| Less than high school completion | 32.75 | ||
| High school or equivalent | 30.75 | ||
| Some college | 25.00 | ||
| College schools | 7.80 | ||
| Graduate schools | 3.70 | ||
| Relationship with Child’s Father | |||
| Married | 25.59 | ||
| Not married | 74.41 | ||
| Maternal Anxiety | |||
| Child’s age one | 3.17 | ||
| Child’s age three | 4.60 | ||
| Maternal Depression | |||
| Child’s age one | 15.45 | ||
| Child’s age three | 20.60 |
Table 2.
Correlation Matrix for the Study Variables
| Social Cohesion | Parenting Stress | Depression | Anxiety | |
|---|---|---|---|---|
| Social Cohesion | 1.00 | |||
| Parenting Stress | −0.21 | 1.00 | ||
| Depression | −0.11 | 0.23 | 1.00 | |
| Anxiety | −0.08 | 0.23 | 0.67 | 1.00 |
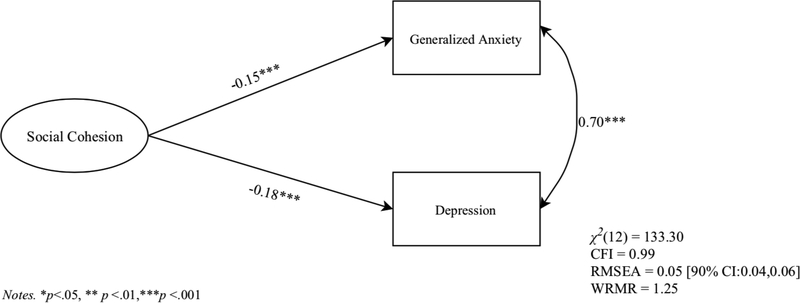
The Direct Effects
The direct relationships between social cohesion and generalized maternal anxiety and depression are displayed in Figure 2. The direct effect model produced good model fit: χ2 (12) = 133.30; CFI = 0.99; RMSEA = 0.05 [90% CI: 0.04, 0.06]; WRMR = 1.25. The results indicated that mothers living in neighborhoods with higher social cohesion were less likely to meet the criteria for generalized anxiety disorder (b = −0.15, p < 0.001) and major depressive episode (b = −0.18, p < 0.001). Generalized maternal anxiety was highly correlated with maternal depression (r = 0.70, p < 0.001).
Figure 2.
Observed path model of the direct effects of social cohesion on maternal anxiety and depression.
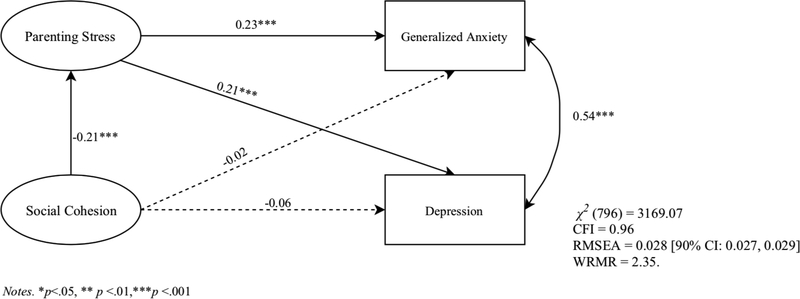
The Indirect Effects of Parenting Stress
According to the results of the mediation model, the direct relationship between social cohesion and generalized maternal anxiety and depression was mediated by mothers’ parenting stress (Figure 3). The mediation model yielded good model fit: χ2 (796) = 3169.07, p <.001; CFI = 0.96; RMSEA = 0.028 [90% CI: 0.027, 0.029]; WRMR = 2.35. The factor loadings of the two latent variables, social cohesion and parenting stress, ranged from .53 to .87 and were considered acceptable (Malakouti, Fatollahi, Mirabzadeh, Salavati, & Zandi, 2006; Stevens, 1992). The results showed that the relationship between social cohesion and generalized maternal anxiety was mediated by parenting stress (indirect effect: −0.05, p < 0.001) (Table 3). Social cohesion had no significant direct effects on generalized maternal anxiety (b = −0.02, p = 0.96). However, as perceived neighborhood social cohesion increased, parenting stress decreased (b = −0.21, p <0.001), which decreased maternal anxiety (b = 0.23, p < 0.001).
Figure 3.
Observed path model of the direct and indirect effects of social cohesion on maternal anxiety and depression.
Table 3.
Direct and Indirect Effects of Social Cohesion on Maternal Anxiety and Depression (N=3,876)
| β | |
|---|---|
| Social Cohesion on Maternal Anxiety | |
| Direct | −0.02 |
| Total indirect (By Parenting Stress) | −0.05*** |
| Social Cohesion on Maternal Depression | |
| Direct | −0.06 |
| Total indirect (By Parenting Stress) | −0.04*** |
Note. β = standardized coefficient
p < .05
p < .01
p < .001
Social cohesion did not have a significant direct effect on maternal depression (b = −0.06, p = 0.10). Parenting stress partially mediated the effect of social cohesion on maternal depression (indirect effect: −0.04, p < 0.001) (Table 3). These results indicated that higher social cohesion was associated with reduced parenting stress (b = −0.21, p < 0.001) which in turn significantly reduced maternal depression (b = 0.21, p < 0.001).
Discussion
Study results supported our hypotheses that neighborhood social cohesion would be associated with maternal depression and anxiety and that this relationship would be mediated by parenting stress, using a large secondary data set of primarily low-income, unmarried mothers of young children. More specifically, findings showed that as neighborhood social cohesion increased, parenting stress decreased, and that was associated with lower rates of maternal anxiety and depression.
This study extends upon previous research demonstrating that neighborhood factors play a significant role in parenting stress and mental health outcomes (Barnhart & Maguire-Jack, 2016; Franco et al., 2010; Mair, Roux, & Galea, 2008; Rios, Aiken, & Zautra, 2011). Together, these studies confirm associations between lower neighborhood social cohesion, increased neighborhood disorder and increased parenting stress and maternal depression. This study’s novel contribution lies in examining parenting stress as a mediator between neighborhood social cohesion and maternal depression and anxiety. Furthermore, our study adds to the literature by analyzing the complex relationships between multiple variables—neighborhood social cohesion, parenting stress, and maternal depression and anxiety—simultaneously. Using SEM to test these complicated phenomena over more commonly used statistical methods that do not allow for examining mediation relationships with multiple dependent variables was advantageous. The study results provide improved understanding of the relationships between social cohesion, parenting stress, and maternal mental health among primarily low-income, unpartnered mothers.
The percentage of mothers in our sample who met criteria for a major depressive episode at child’s age three was 20.6, much higher than epidemiological surveys reporting a 8.5% annual prevalence among adult women (SAMHSA, 2017) and 10.0% among mothers specifically (Ertel et al., 2011). Conversely, the percentage of mothers in our sample meeting criteria for generalized anxiety disorder at child’s age three was 4.6%, which coincides with a 12-month prevalence rate of 4.0% in the US adult population as reported by Ruscio and colleagues (2017). Despite this, it is important to note that some literature shows higher rates of depression and anxiety among low-income women when compared to the general population. A recent study of a racially and ethnically diverse sample of low-income women found that 45% met the criteria for major depression (Mersky, Janczewski, & Nitkowski, 2018). Researchers also using FFCWS data found that the poorest mothers were the most likely to experience anxiety and that their symptoms were associated with increased odds of economic instability (Baer, Kim, & Wilkenfeld, 2012). Along with the current study, such findings provide further credence to the assertion that mental health problems are largely influenced by the social and economic environment.
Implications for Practice and Policy
To reduce parenting stress and improve maternal mental health outcomes, it may be prudent to focus efforts toward increasing neighborhood social cohesion. Social programming and opportunities for social interaction are needed, perhaps even more so in communities experiencing lower levels of neighborhood social cohesion. Starting in the perinatal and early postpartum period, healthcare and social service providers can connect mothers with local parenting groups and social programs. As the relationships between neighborhood social cohesion and maternal health outcomes may be reciprocal, such interventions may simultaneously increase opportunities for social engagement and cohesion and reduce symptoms of anxiety and depression via increased social support (Dennis & Kingston, 2008; Small, Taft, & Brown, 2011). Providers should emphasize the importance of social support and connection for mothers and discuss ways they can develop their social networks. This may be particularly salient for low-income and unpartnered mothers to reduce parenting in isolation (Stewart et al., 2009). Increasing social cohesion and reducing social isolation may result in improved mental health and perceived well-being outcomes (Cacioppo & Cacioppo, 2014; Erdem, Van Lenthe, Prins, Voorham, & Burdorf, 2016).
On the macro level, there exists a need to advocate for social, political, and environmental policies and conditions that recognize the important influence of neighborhood social context on health and that support efforts to boost neighborhood social cohesion. In their paper explaining the relationship between social cohesion and neighborhoods, Forrest and Kearns (2001) describe eight dimensions of social capital—empowerment; participation; associational activity and common purpose; supporting networks and reciprocity; collective norms and values; trust; safety; and belonging—which can be used to create and enrich neighborhood social cohesion and policies and practices to support it. Suggestions include involving residents in establishing programs, activities, security measures, and policies and their related processes, providing support to community groups, and promoting community interests. These ideas can also be tailored in order to provide increased support to parents in a community. Finally, there are numerous neighborhood contextual factors (e.g. neighborhood safety, presence of sidewalks, recreation areas, and grocery stores) that can influence self-reported neighborhood social cohesion. Such neighborhood-level factors must be considered in order to best facilitate increased opportunities for social and civic engagement, and to grow trust and interaction among community members. Investment in neighborhood social cohesion may facilitate a reduction in maternal parenting strain and an improvement in mental health.
Limitations
This study uses data collected from 2001 – 2003. Thus, findings may not be reflective of current rates and patterns of maternal depression and anxiety, or experiences of parental stress and neighborhood social cohesion. Given that participants were primarily unmarried mothers, study results may not generalize to other types of family structures. For instance, it may be possible that single female-headed households are more influenced by neighborhood social cohesion and parenting stress than male-headed households or households where there are multiple caregivers sharing parenting roles because of gendered relationships between the social environment and well-being. Women who perceived neighborhood problems and less social support and networks in the community are significantly more likely than men with similar perceptions to report poorer health (Molinari, Ahern, & Hendryx, 1998). Moreover, mothers are more likely than fathers to multitask across roles at work and at home, which is associated with increased stress (Offer & Schneider, 2011). This study focused on anxiety and depression outcomes among mothers who are raising young children, which can represent a critical period of high parenting stress (Crnic, Gaze, & Hoffman, 2005). Further studies investigating the mental health of mothers of children in other developmental periods are needed.
Furthermore, the cross-sectional design of the study is a limitation. While significant relationships have been confirmed between these variables, results do not imply causation. It is possible that mothers who are depressed and anxious—as a side effect of these conditions—are more likely to experience more parental stress and perceive lower social cohesion; similarly, mothers who are not depressed or anxious may be more likely to perceive higher degrees of neighborhood social cohesion and less parenting stress. Improved mental health can lead to improved parenting and the ability to positively contribute to better neighborhood social cohesion. Future studies may investigate relationships between these constructs using a longitudinal, time-series design. Lastly, all variables in this study were self-reported by mothers, which may have potential bias. Future studies might consider using more objective data in combination with mothers’ reports to examine the relationship among social cohesion, parenting stress, and maternal mental health.
Conclusion
This study tested the mediation effects of parenting stress on the relationship between social cohesion and maternal mental health in early childhood. Our findings showed that parenting stress partially mediated the influences of social cohesion on maternal anxiety and depression. Interventions that promote neighborhood social cohesion for mothers with young children may have the potential to foster maternal mental health by reducing parenting stress; likewise interventions to reduce maternal anxiety and depression may also improve neighborhood social cohesion. Professionals working in mental health clinics and obstetric and pediatric offices may consider the role of mothers’ neighborhood conditions in influencing mental health and work to connect mothers with positive social networks to increase reduce isolation and cultivate social cohesion. Perhaps most notably, this study emphasizes the need for macro level work to improve and develop programs and policies that aim to prevent or reduce maternal depression and anxiety among low-income families, while also supporting social engagement and community interests.
Acknowledgements
Research reported in this publication was supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) of the National Institutes of Health under award numbers R01HD36916, R01HD39135, and R01HD40421, as well as a consortium of private foundations. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors
References
- Apter-Levy Y, Feldman M, Vakart A, Ebstein RP, & Feldman R (2013). Impact of maternal depression across the first 6 years of life on the child’s mental health, social engagement, and empathy: the moderating role of oxytocin. American Journal of Psychiatry, 170(10), 1161–1168. [DOI] [PubMed] [Google Scholar]
- Baer JC, Kim M, & Wilkenfeld B (2012). Is it generalized anxiety disorder or poverty? An examination of poor mothers and their children. Child and Adolescent Social Work Journal, 29(4), 345–355. https://link.springer.com/article/10.1007/s10560-012-0263-3 [Google Scholar]
- Barnhart S, & Maguire-Jack K (2016). Single mothers in their communities: The mediating role of parenting stress and depression between social cohesion, social control and child maltreatment. Children and youth services review, 70, 37–45. 10.1016/j.childyouth.2016.09.003 [DOI] [Google Scholar]
- Baron RM, & Kenny DA (1986). The moderator–mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology, 51(6), 1173. [DOI] [PubMed] [Google Scholar]
- Beck CT (1998). The effects of postpartum depression on child development: A meta-analysis. Archives of Psychiatric Nursing, 12(1), 12–20. 10.1016/S0883-9417(98)80004-6 [DOI] [PubMed] [Google Scholar]
- Brisson D (2014). Neighborhood social cohesion. 10.1093/obo/9780195389678-0183 [DOI]
- Cacioppo JT, & Cacioppo S (2014). Social relationships and health: The toxic effects of perceived social isolation. Social and Personality Psychology Compass, 8(2), 58–72. 10.1111/spc3.12087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caldwell BM, & Bradley RH (1984). Home observation for measurement of the environment. Little Rock: University of Arkansas at Little Rock. [Google Scholar]
- Cassells RC, & Evans GW (2017). Ethnic variation in poverty and parenting stress In Parental Stress and Early Child Development (pp. 15–45). Springer International Publishing; https://link.springer.com/chapter/10.1007/978-3-319-55376-4_2 [Google Scholar]
- Chuang YC, Chuang KY, & Yang TH (2013). Social cohesion matters in health. International journal for equity in health, 12, 87. doi: 10.1186/1475-9276-12-87 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crnic KA, Gaze C, & Hoffman C (2005). Cumulative parenting stress across the preschool period: Relations to maternal parenting and child behaviour at age 5. Infant and Child Development: An International Journal of Research and Practice, 14(2), 117–132. [Google Scholar]
- Delaney ME (2017). The relationship between counseling, social support, and depression in mothers of fragile families. Journal of Mental Health Counseling, 39(4), 320–334. 10.17744/mehc.39.4.04 [DOI] [Google Scholar]
- Deater-Deckard K (2008). Parenting stress. New Haven, CT: Yale University Press. [Google Scholar]
- Dennis CL, & Kingston D (2008). A systematic review of telephone support for women during pregnancy and the early postpartum period. Journal of Obstetric, Gynecologic & Neonatal Nursing, 37(3), 301–314. 10.1111/j.1552-6909.2008.00235.x [DOI] [PubMed] [Google Scholar]
- Erdem Ö, Van Lenthe FJ, Prins RG, Voorham TA, & Burdorf A (2016). Socioeconomic inequalities in psychological distress among urban adults: the moderating role of neighborhood social cohesion. PloS one, 11(6), e0157119 10.1371/journal.pone.0157119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ertel KA, Rich-Edwards JW, & Koenen KC (2011). Maternal depression in the United States: Nationally representative rates and risks. Journal of Women’s Health, 20(11), 1609–1617. 10.1089/jwh.2010.2657 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fone D, White J, Farewell D, Kelly M, John G, Lloyd K, ... & Dunstan F (2014). Effect of neighbourhood deprivation and social cohesion on mental health inequality: a multilevel population-based longitudinal study. Psychological Medicine, 44(11), 2449–2460. 10.1017/S0033291713003255 [DOI] [PubMed] [Google Scholar]
- Franco LM, Pottick KL, & Huang C-C (2010). Early parenthood in a community context: neighborhood conditions, race-ethnicity, and parenting stress. Journal of Community Psychology, 38, 5, 574–590. http://onlinelibrary.wiley.com/doi/10.1002/jcop.20382/pdf [Google Scholar]
- Glover V (2014). Maternal depression, anxiety and stress during pregnancy and child outcome; what needs to be done. Best Practice & Research Clinical Obstetrics & Gynaecology, 28, 1, 25–35. 10.1016/j.bpobgyn.2013.08.017 [DOI] [PubMed] [Google Scholar]
- Goodman SH, Rouse MH, Connell AM, Broth MR, Hall CM, & Heyward D (2011). Maternal depression and child psychopathology: A meta-analytic review. Clinical Child and Family Psychology Review, 14(1), 1–27. 10.1007/s10567-010-0080-1 [DOI] [PubMed] [Google Scholar]
- Gress-Smith JL, Luecken LJ, Lemery-Chalfant K, & Howe R (2012). Postpartum depression prevalence and impact on infant health, weight, and sleep in low-income and ethnic minority women and infants. Maternal and Child Health Journal, 16(4), 887–893. doi: 10.1007/s10995-011-0812-y [DOI] [PubMed] [Google Scholar]
- Hu LT, & Bentler PM (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal, 6(1), 1–55. 10.1080/10705519909540118 [DOI] [Google Scholar]
- Kawachi I, and Berkman L (2000). Social cohesion, social capital, and health In: Berkman FLF. & Kawachi I (Eds.). Social Epidemiology (pp. 174–190). New York: Oxford University Press. [Google Scholar]
- Kawachi I, & Berkman LF (2001). Social ties and mental health. Journal of Urban Health, 78(3), 458–467. 10.1093/jurban/78.3.458 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Andrews G, Mroczek D, Ustun TB, & Wittchen HU (1998). The World Health Organization Composite International Diagnostic Interview Short-Form (CIDI-SF). International Journal of Methods in Psychiatric Research, 7, 171–185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leach LS, Poyser C, & Fairweather‐Schmidt K (2017). Maternal perinatal anxiety: a review of prevalence and correlates. Clinical Psychologist, 21(1), 4–19. 10.1111/cp.12058 [DOI] [Google Scholar]
- Leigh B, & Milgrom J (2008). Risk factors for antenatal depression, postnatal depression and parenting stress. BMC psychiatry, 8(1), 24 https://bmcpsychiatry.biomedcentral.com/articles/10.1186/1471-244X-8-24 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindahl V, Pearson JL & Colpe L (2005). Prevalence of suicidality during pregnancy and the postpartum. Archives of Women’s Mental Health, 8(2), 77–87. doi: 10.1007/s00737005-0080-1 [DOI] [PubMed] [Google Scholar]
- MacCallum RC, Browne MW, & Sugawara HM (1996). Power analysis and determination of sample size for covariance structure modeling. Psychological Methods, 1, 130–149. doi: 10.1037/1082-989X.1.2.130 [DOI] [Google Scholar]
- Maguire-Jack K, & Showalter K (2016). The protective effect of neighborhood social cohesion in child abuse and neglect. Child abuse & neglect, 52, 29–37. doi: 10.1016/j.chiabu.2015.12.011 [DOI] [PubMed] [Google Scholar]
- Maguire-Jack K & Wang X (2016). Pathways from social cohesion to neglect: the mediating role of social support and parenting stress. Children and Youth Services Review, 66, 28–34. 10.1016/j.childyouth.2016.04.017 [DOI] [Google Scholar]
- Mair CF, Roux AVD, & Galea S (2008). Are neighborhood characteristics associated with depressive symptoms? A critical review. Journal of Epidemiology & Community Health, 62, 940–946. 10.1136/jech.2007.066605 [DOI] [PubMed] [Google Scholar]
- Manuel JI, Martinson ML, Bledsoe-Mansori SE, & Bellamy JL (2012). The influence of stress and social support on depressive symptoms in mothers with young children. Social Science & Medicine, 75, 11, 2013–2020. doi: 10.1016/j.socscimed.2012.07.034 [DOI] [PubMed] [Google Scholar]
- Mersky JP, Janczewski CE, & Nitkowski JC (2018). Poor mental health among low-income women in the US: The roles of adverse childhood and adult experiences. Social Science & Medicine, 206, 14–21. 10.1016/j.socscimed.2018.03.043 [DOI] [PubMed] [Google Scholar]
- Molinari C, Ahern M, & Hendryx M (1998). The relationship of community quality to the health of women and men. Social Science & Medicine, 47, 8, 1113–1120. doi: 10.1016/S0277-9536(98)00114-2 [DOI] [PubMed] [Google Scholar]
- MPlus (Version 8.0). [Computer Software]. (2017). Los Angeles, CA: Muthén & Muthén. [Google Scholar]
- Muthén BO (1998–2004). MPlus technical appendices. Los Angeles, CA: Muthén & Muthén. [Google Scholar]
- Nam Y, Wikoff N & Sherraden MJ (2015). Racial and ethnic differences in parenting stress: evidence from a statewide sample of new mothers. Journal of Child and Family Studies, 24(2): 278–288. 10.1007/s10826-013-9833-z [DOI] [Google Scholar]
- Nilsen W, Gustavson K, Kjeldsen A, Røysamb E, & Karevold E (2013). Pathways from maternal distress and child problem behavior to adolescent depressive symptoms – A prospective examination from 18 months to 17 years of age. Journal of Developmental and Behavioral Pediatrics, 35(5), 303–313 [DOI] [PubMed] [Google Scholar]
- Oates M (2003). Perinatal psychiatric disorders: A leading cause of maternal morbidity and mortality. British Medical Bulletin, 67, 219–229. doi: 10.1093/bmb/ldg011 [DOI] [PubMed] [Google Scholar]
- O’Higgins M, Roberts ISJ, Glover V, & Taylor A (2013). Mother-child bonding at 1 year; associations with symptoms of postnatal depression and bonding in the first few weeks. Archives of women’s mental health, 16(5), 381–389. 10.1007/s00737-013-0354-y [DOI] [PubMed] [Google Scholar]
- Parkes A, Sweeting H, & Wight D (2015). Parenting stress and parent support among mothers with high and low education. Journal of Family Psychology : JFP : Journal of the Division of Family Psychology of the American Psychological Association (Division 43), 29(6), 907–918. 10.1037/fam0000129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paul IM, Downs DS, Schaefer EW, Beiler JS, & Weisman CS (2013). Postpartum anxiety and maternal-infant health outcomes. Pediatrics, 131(4), 1–7. doi:10.1542/peds.2012–2147 doi: 10.1542/peds.2012-2147 [DOI] [PubMed] [Google Scholar]
- Quittner AL, Glueckauf RL, & Jackson DN (1990). Chronic parenting stress: Moderating versus mediating effects of social support. Journal of Personality and Social Psychology, 59(6), 1266. doi: 10.1037/0022-3514.59.6.1266 [DOI] [PubMed] [Google Scholar]
- Raphael JL, Zhang Y, Liu H, & Giardino AP (2010). Parenting stress in US families: Implications for paediatric healthcare utilization. Child: Care, Health and Development, 36(2), 216–224. http://onlinelibrary.wiley.com/doi/10.1111/j.1365-2214.2009.01052.x/full [DOI] [PubMed] [Google Scholar]
- Rios R, Aiken LS, & Zautra AJ (2011). Neighborhood contexts and the mediating role of neighborhood social cohesion on health and psychological distress among Hispanic and non-Hispanic residents. Annals of Behavioral Medicine, 43(1), 50–61. 10.1007/s12160-011-9306-9 [DOI] [PubMed] [Google Scholar]
- Ruscio AM, Hallion LS, Lim CC, Aguilar-Gaxiola S, Al-Hamzawi A, Alonso J, ... & De Almeida JMC (2017). JAMA Psychiatry, 74(5), 465–475. doi: 10.1001/jamapsychiatry.2017.0056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sampson RJ, Raudenbush SW, and Earls F (1997). Neighborhoods and violent crime: A multilevel study of collective efficacy. Science, 277(5328), 918–924. doi: 10.1126/science.277.5328.918 [DOI] [PubMed] [Google Scholar]
- Small R, Taft AJ, & Brown SJ (2011). The power of social connection and support in improving health: lessons from social support interventions with childbearing women. BMC Public Health, 11(5), S4 10.1186/1471-2458-11-S5-S4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sontag-Padilla L Schultz D, Reynolds K, Lovejoy SL & Firth R (2013). Maternal depression: Implications for systems serving mother and child. Santa Monica, CA: RAND Corporation, 2013. https://www.rand.org/pubs/research_reports/RR404.html [Google Scholar]
- Stewart MJ, Makwarimba E, Reutter LI, Veenstra G, Raphael D, & Love R (2009). Poverty, sense of belonging and experiences of social isolation. Journal of Poverty, 13(2), 173–195. 10.1080/10875540902841762 [DOI] [Google Scholar]
- Stewart RC (2007). Maternal depression and infant growth: a review of recent evidence. Maternal and Child Nutrition, 3(2), 94–107. doi: 10.1111/j.1740-8709.2007.00088.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration (SAMHSA). (2017). Key substance use and mental health indicators in the United States: Results from the 2016 National Survey on Drug Use and Health (HHS Publication No. SMA 17–5044, NSDUH Series H-52). Rockville, MD: Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration; Retrieved from https://www.samhsa.gov/data/ [Google Scholar]
- Turney K, & Harknett K (2010). Neighborhood disadvantage, residential stability, and perceptions of instrumental support among new mothers. Journal of Family Issues, 31(4), 499–524. 10.1177/0192513X09347992 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vismara L, Rollè L, Agostini F, Sechi C, Fenaroli V, Molgora S, ... & Polizzi C (2016). Perinatal parenting stress, anxiety, and depression outcomes in first-time mothers and fathers: a 3-to 6-months postpartum follow-up study. Frontiers in Psychology, 7(938). https://www.frontiersin.org/articles/10.3389/fpsyg.2016.00938/full [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warnock FF, Craig KD, Bakeman R, Castral T, & Mirlashari J (2016). The relationship of prenatal maternal depression or anxiety to maternal caregiving behavior and infant behavior self-regulation during infant heel lance: an ethological time-based study of behavior. BMC Pregnancy and Childbirth, 16(1), 264 10.1186/s12884-016-1050-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DT, Cheadle JE, & Goosby BJ (2015). Hard times and heart break: Linking economic hardship and relationship distress. Journal of Family Issues, 36(7), 924–950. 10.1177/0192513X13501666 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilmot N & Dauner K (2017). Examination of the influence of social capital on depression in fragile families. Journal of Epidemiology and Community Health, 71(3), 296–302. doi: 10.1136/jech-2016-207544 [DOI] [PubMed] [Google Scholar]
- Wisner KL, Sit DKY, McShea MC, Risso DM, Zoretich RA, Hughes CL, Eng HF, Luther JF, Wisniewski SR, Costantino ML, Confer AL, Moses Kolko EL, Famy CS, & Hanusa BH (2013). Onset timing, thoughts of self-harm, and diagnoses in postpartum women with screen-positive depression findings. JAMA Psychiatry, 70(5), 490–498. doi: 10.1001/jamapsychiatry.2013.8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu CY (2002). Evaluating cutoff criteria of model fit indices for latent variable models with binary and continuous outcomes (Unpublished doctoral dissertation). University of California Los Angeles, Los Angeles, CA. [Google Scholar]