Abstract
Background
The growing field of personal sensing harnesses sensor data collected from individuals’ smartphones to understand their behaviors and experiences. Such data could be a powerful tool within mental health care. However, it is important to note that the nature of these data differs from the information usually available to, or discussed with, health care professionals. To design digital mental health tools that are acceptable to users, understanding how personal sensing data can be used and shared is critical.
Objective
This study aimed to investigate individuals’ perspectives about sharing different types of sensor data beyond the research context, specifically with doctors, electronic health record (EHR) systems, and family members.
Methods
A questionnaire assessed participants’ comfort with sharing six types of sensed data: physical activity, mood, sleep, communication logs, location, and social activity. Participants were asked about their comfort with sharing these data with three different recipients: doctors, EHR systems, and family members. A series of principal component analyses (one for each data recipient) was performed to identify clusters of sensor data types according to participants’ comfort with sharing them. Relationships between recipients and sensor clusters were then explored using generalized estimating equation logistic regression models.
Results
A total of 211 participants completed the questionnaire. The majority were female (171/211, 81.0%), and the mean age was 38 years (SD 10.32). Principal component analyses consistently identified two clusters of sensed data across the three data recipients: “health information,” including sleep, mood, and physical activity, and “personal data,” including communication logs, location, and social activity. Overall, participants were significantly more comfortable sharing any type of sensed data with their doctor than with the EHR system or family members (P<.001) and more comfortable sharing “health information” than “personal data” (P<.001). Participant characteristics such as age or presence of depression or anxiety did not influence participants’ comfort with sharing sensed data.
Conclusions
The comfort level in sharing sensed data was dependent on both data type and recipient, but not individual characteristics. Given the identified differences in comfort with sensed data sharing, contextual factors of data type and recipient appear to be critically important as we design systems that harness sensor data for mental health treatment and support.
Keywords: mHealth, privacy, personal sensing, digital mental health, depression, anxiety, mobile phone
Introduction
Personal sensing, also referred to as context sensing and digital phenotyping [1], is the acquisition and use of data from networked sensors (as in a smartphone) for the detection of behaviors, psychological states, and environmental conditions [2]. Personal sensing shows great promise within mental health research [3]. Sensed data have already been used in a number of mental health conditions including schizophrenia [4], bipolar disorder [5], social anxiety [6], and depression [7]. For example, in schizophrenia, changes in mobility and social behavior, measured using global positioning system (GPS) and communication log data, were found to proceed clinical relapse [4]. Mobility and location data, measured using information extracted from GPS data [8,9] or the number of cell tower connections [5], have also been reported to identify and predict episodes of depression in bipolar disorder and are associated with severity of unipolar depression symptoms [9-11]. Sleep duration can also be successfully inferred using sensed data acquired from smartphones [12-14] and is related to depression severity [15]. Finally, data on subjectively reported mood, collected via ecological momentary assessments, that often accompany sensed data have demonstrated validity, correlating highly with clinician-assessed mood scales [5]. However, as demonstrations of the potential of sensed data to support mental health care and behavior change increase, questions arise regarding the acceptability of collecting different types of sensed data and the people who have access to that information.
Attitudes about privacy related to digitally collected data are theorized to rely on two major variables: contextual factors and individual characteristics. Research indicates that contextual factors may be the primary influence on people’s reasoning about privacy [16,17]. A robust framework—privacy as contextual integrity—defines the contextual factors that influence people’s privacy judgements and willingness to share data, such as data type and sensitivity, data use, transmission principles and constraints (eg, confidentiality or anonymity), and data recipient [18,19]. In mental health research, the sensitivity of data is high [20]. The types of data collected for mental health are broad, ranging from mood, communication logs, and social activity to GPS data. Finally, within the mental health field, potential data recipients beyond researchers include doctors, electronic health record (EHR) systems, and family members. Importantly, the digital data privacy literature emphasizes the need for individuals to understand (and preferably control) who has access to their personal data [16,21,22].
Despite the importance of privacy considerations in personal sensing, few studies have explored how contextual factors such as data type or recipient influence the acceptability and appropriate use of smartphone sensor data in the treatment and management of mental health. The closest example is Klasnja and colleagues’ [23] study of sensed data related to physical activity. Participants’ concerns about personal sensing varied depending on the type of sensor data collected. Accelerometer data were not considered sensitive, so their daily recording and storage were not of concern. However, perspectives on the collection and storage of GPS data were mixed, and raw audio data were considered very sensitive, with most participants indicating that they would not allow continuous recording. Although these results lend support to the privacy as contextual integrity framework and provide insight into privacy perspectives in personal sensing, many contextual factors differ between sensed data collected for physical activity and mental health purposes, which potentially impact the extensibility of the findings to the mental health context.
In addition to contextual factors, individual characteristics of users may influence attitudes towards privacy. Although, to our knowledge, no research has assessed differences in perspectives of sensed data privacy between people living with and those not living with a mental health condition, research indicates that data privacy and confidentiality are among the primary concerns of individuals with a mental health condition when considering the use of apps to support their mental health [24,25]. Research also suggests that older individuals may have more concerns about the collection and sharing of sensed data than younger people [26]. In a study of app privacy permissions, including access to sensors, participants characterized as “unconcerned” by permissions (those who had a high comfort level with sharing sensitive information across numerous settings) were more likely to be younger. Characteristics of the individual should therefore be considered in conjunction with context when exploring perspectives regarding sensed data sharing in mental health.
As advances in personal sensing aim to integrate the passive identification of behavioral indicators of common mental health disorders such as depression and anxiety with existing mental health services, it is critical to understand how context and individual characteristics influence individuals’ perspectives regarding the use and sharing of sensed data. Understanding such perspectives is vital to guiding the design and successful implementation of digital mental health systems. The aims of this study were (1) to investigate the acceptability of sharing sensed mental health data beyond researchers, specifically with doctors, EHR systems, and family members; (2) to determine the acceptability of use of different types of sensed data beyond the research context by doctors, EHR systems, and family members; and (3) to explore the impact of age and presence of anxiety or depression on the acceptability of sharing data.
Methods
Participants
Data were collected from a convenience sample of individuals participating in a 6-week personal sensing study that required them to download an app that collected mobile sensor data including activity, light, GPS location, and communication logs, and to complete daily questionnaires regarding sleep and wake times [12]. In that study, participants were eligible if they were aged 18 years or above, were able to read and understand English, owned an Android smartphone, and had access to Wi-Fi connectivity for at least a 3-hour period each day. Participants were excluded if they were diagnosed with any psychotic disorder or screened positive for a substance use disorder (Alcohol Use Disorder Identification Test [27] score ≥16 or Drug Abuse Screening Test-10 [28] score ≥6), suicidal ideation (Patient Health Questionnaire - 9 item [PHQ-9] [29], item 9 rating ≥1 or Beck Depression Inventory-II [30], item 9 rating ≥2), or bipolar disorder (mood disorder questionnaire [31] question 1 rating ≥7, endorsed question 2, and responded 2 or 3 for question 3). Individuals who shared their smartphone with others were also excluded.
Based on the results of the PHQ-9 and Generalized Anxiety Disorder - 7 item (GAD-7) [32] screening questionnaires, participants were selected to create roughly four equal groups across depression and anxiety symptoms: nondepressed or anxious (PHQ-9 score<10; GAD-7 score<10), depressed (PHQ-9 score ≥ 10; GAD-7 score <10), anxious (PHQ-9 score <10; GAD-7 score ≥10), and depressed and anxious (PHQ-9 score ≥ 10; GAD-7 score ≥10).
The study was approved by the Northwestern University Institutional Review Board. Participant responses from only the screening and baseline questionnaire were considered in this study. Within the larger study, participants were compensated for their participation. Compensation depended on both the length of their participation in the study and the number of daily questionnaires answered, and ranged between US $25 and US $270.40.
Measures
Demographic information (for example, age and sex) and data on the presence of depression or anxiety, determined using the PHQ-9 and GAD-7, were collected by self-report.
The acceptability of sharing sensed data was measured through a series of questions with regard to three potential recipients: the participant’s doctor, representing a known individual in the health care system; the participant’s EHR system, a generic destination in the health care system that would broaden access to potentially unknown people; and the participant’s family members. Response options were recorded on an ordinal scale:
0 - I would not use any app that gave these data to my doctor/electronic health record/family member;
1 - I’d be uncomfortable but would consider using an app that did this;
2 - It wouldn’t matter to me;
3 - I’d like an app that gave these data to my doctor/electronic health record/family members.
Participants rated their comfort with sharing five classes of sensed activities or states (physical activity, sleep, mood, social activity, and location [places visited and patterns of movement]) and one raw sensed data type (communication logs [number of calls made or texts sent]), with each of the three recipients.
Data Analysis
Given the ordinal (0, 1, 2, and 3) nature of the responses on the acceptability scale and the relatively limited sample size, it was not appropriate to treat these data as continuous. Although these outcomes are appropriate for ordinal logistic regression, we did not assume proportional odds for our models, and hence, survey responses were dichotomized to indicate whether the participant was comfortable sharing their data. Responses 0 and 1 (I would not use any app that gave these data to my doctor/electronic health record/ family member and I’d be uncomfortable but would consider using an app that did this, respectively) were coded as not comfortable, and responses 2 and 3 (It wouldn’t matter to me and I’d like an app that gave these data to my doctor/electronic health record/ family members, respectively) were coded as comfortable.
First, we performed a series of three principal component analyses, one for each data recipient, to identify clusters of sensor data types according to participants’ comfort with sharing them. Second, we determined relationships between recipients and the types of sensor data using generalized estimating equation logistic regression models of each participant’s 18 dichotomized responses (3 types of recipients × 6 types of sensor data, which were clustered into two groups based on the principal component analysis results). Third, we explored the influence of age and mental health on participants’ comfort with sharing sensed data by adding age, depression (defined as PHQ-9 score ≥ 10 and GAD-7 score <10), and anxiety (defined as PHQ-9 score <10 and GAD-7 score ≥10) as covariates in the model. Models were assessed using analysis of variance and Wald tests. All analyses were performed using R (v3.4.3; R Foundation for Statistical Computing, Vienna, Austria) with a type I error rate of 0.05.
Results
Participants
A total of 211 eligible participants were enrolled and completed the privacy survey. The majority were female (171/211; 81.0%), and the mean (SD) age was 38 (10.32) years, ranging from 18 to 66 years. A total of 83% (176/211) of participants identified as Caucasian; 13.3% (28/211), as African American; and 9.0% (19/211), as Hispanic or Latino. Further details of the sample are shown in Table 1.
Table 1.
Participant characteristics.
| Characteristic | Statistics | |
| Gender, n (%) | ||
| Male | 36 (17.1) | |
| Female | 171 (81.0) | |
| Another | 3 (1.4) | |
| Age (years), mean (SD) | 38.09 (10.32) | |
| Race and ethnicitya, n (%) | ||
| Black or African American | 28 (13.3) | |
| American Indian or Alaska native | 6 (2.8) | |
| Asian | 10 (4.7) | |
| White | 176 (83.4) | |
| Hispanic or Latino | 19 (9.0) | |
| Highest level of education, n (%) | ||
| Some high school | 4 (1.9) | |
| Completed high school | 25 (11.8) | |
| Some college | 77 (36.5) | |
| Completed associate’s or bachelor’s degree | 77 (36.5) | |
| Master’s degree | 23 (10.9) | |
| Doctoral degree or professional doctorate | 5 (2.4) | |
| Employment status, n (%) | ||
| Employed | 130 (61.6) | |
| Unemployed | 44 (20.9) | |
| Disability | 17 (8.1) | |
| Retired | 4 (1.9) | |
| Other | 16 (7.6) | |
| Mental health status, n (%) | ||
| Healthy (PHQ-9b score<10 and GAD-7c score<10) | 59 (28.0) | |
| Depressed (PHQ-9 score≥10 and GAD-7 score<10) | 55 (26.1) | |
| Anxious (PHQ-9 score<10 and GAD-7 score≥10) | 44 (20.9) | |
| Depressed and anxious (PHQ-9 score≥10 and GAD-7 score≥10) | 53 (25.1) | |
aRace and ethnicity categories are not mutually exclusive.
bPHQ-9: Patient Health Questionnaire - 9 item.
cGAD-7: Generalized Anxiety Disorder - 7 item.
Sensor Data Type
Principal component analyses were performed on participant responses to their comfort level with sharing the six types of sensor data with each of the three data recipients. Although sensor clusters were largely consistent across data recipients, the relative strengths of each variable across recipients differed. The two clusters extracted across each of the recipients could best be described as “health information,” including sleep, mood, and physical activity, and “personal data,” including communication logs, location, and social activity.
For doctor recipients, the two principle components explained 74.8% of the variability in the responses (Figure 1). Participants were most comfortable sharing health information with doctors and least comfortable sharing personal data, particularly communication logs and location. The same two components for the EHR system explained 76.8% of the variability in the responses (Figure 1). Participants were least comfortable sharing personal data with their EHR system. For family members, the two components explained 80.5% of the responses (Figure 1); however, the two groups were less distinct in terms of comfort with sharing personal data with family members than with doctors or EHR systems.
Figure 1.
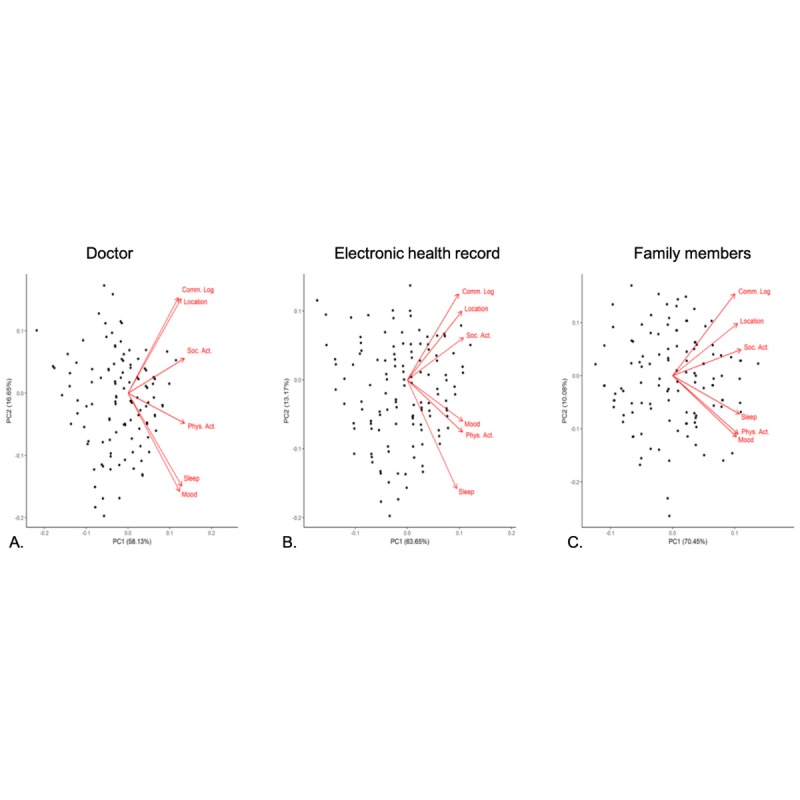
Principal component analysis of participant comfort with sharing data from six different sensors with their doctor, electronic health record, and family members. Comm Log; communications log; PC: principal component; Phys Act: physical activity; Soc Act: social activity.
Sensor Data Sharing
Comfort level in sharing the different types of sensor data with each of the three recipient groups is displayed in Table 2. On the whole, participants indicated they were comfortable sharing their sensor data apart from communication logs and location data, and the comfort levels were higher when such data were shared with their doctor than with their family members.
Table 2.
Participants’ comfort level sharing various sensor data with different recipients. The values indicate participants who were comfortable with sharing data.
| Sensor data type | Doctor, n (%) | Electronic health record, n (%) | Family members, n (%) |
| Sleep | 188 (89.1) | 183 (86.7) | 135 (64.0) |
| Mood | 173 (82.0) | 151 (71.6) | 108 (51.2) |
| Physical activity | 162 (76.8) | 152 (72.0) | 109 (51.7) |
| Communication logs | 135 (64.0) | 110 (52.1) | 115 (54.5) |
| Location | 122 (57.8) | 105 (49.8) | 97 (46.0) |
| Social activity | 154 (73.0) | 129 (61.1) | 116 (55.0) |
Generalized estimating equation logistic regression models were fit on the binary outcome of participants’ comfort with sharing sensor data, with the type of sensor data, the recipient of sensor data, presence of depression, presence of anxiety, and age (modeled continuously) used as covariates. The interaction of depression and anxiety was considered, but was not significant (P=.25). As responses on the sensor data type were highly correlated, the type was grouped according to the results of the principal component analyses mentioned above, with sleep, mood, and physical activity combined as “health information” and communication logs, location, and social activity grouped as “personal data.” Data recipient was a significant predictor of a participant’s comfort with sharing data (P<.001; Table 3). Individuals were significantly more comfortable sharing their sensed data with their doctor than with family members (P<.001) or their EHR system (P<.001), regardless of the data type. As suggested by the principal component analyses, overall, participants were significantly more likely to be comfortable sharing “health information” than “personal data” (P<.001). The model results also indicated a significant interaction between data type and recipient (P<.001). Comfort with sharing data was more strongly associated with data recipient for health information than for personal data, such that the difference in comfort with sharing data between doctors and family members was greater for health information than for personal data. We failed to detect any difference in comfort with sharing data with regard to depression (P=.12), anxiety (P=.14), or age (P=.67) in our study.
Table 3.
Model summary of participants’ comfort with sharing “health information” (sleep, mood, and physical activity) and “personal data” (communication logs, location data, and social activity) with their doctor, the electronic health record system, or family members.
| Covariate | Estimate | SE | Wald statistic | Pr(>|W|) |
| Intercept | 0.745 | 0.468 | 2.529 | .112 |
| Age | –0.002 | 0.011 | 0.041 | .840 |
| Anxiety | 0.309 | 0.211 | 2.158 | .142 |
| Depression | –0.333 | 0.214 | 2.416 | .120 |
| Health informationa | 0.953 | 0.126 | 57.621 | <.001b |
| Personal data: Recipient - EHRc,d | –0.451 | 0.074 | 36.722 | <.001b |
| Personal data: Recipient - familye | –0.554 | 0.108 | 26.460 | <.001b |
| Health information: Recipient - EHRc | 0.086 | 0.103 | 0.690 | .406 |
| Health information: Recipient - familye | –0.801 | 0.141 | 32.453 | <.001b |
aHealth information versus personal data.
bThese values are significant.
cEHR versus doctor as recipient.
dEHR: electronic health record.
eFamily versus doctor as recipient.
Discussion
Principal Findings
This study explored the attitudes of participants toward sharing of personal data gathered from smartphone sensors with three potential data recipients in the context of mental health care involving the use of digital interventions. We found that the level of comfort with sharing sensed data was dependent on both data type and recipient, but not individual characteristics. This result is in accordance with the contextual integrity framework [18,33], which states that privacy expectations are influenced by contextual factors such as data type and sensitivity, the relationship between the individual and the data recipient, and context-specific information norms [33]. We found that participants had similar levels of comfort with sharing sleep, mood, and physical activity data (“health information”) and were more comfortable sharing them than communication logs, location, and social activity data (“personal data”). Moreover, participants were significantly more comfortable sharing sensed data with their doctor than with the EHR system or family members.
This difference between comfort in sharing data with doctors and that in sharing data with the EHR system particularly emphasizes the nuanced role that the data recipient plays in privacy concerns. The difference is possibly dependent on the existing relationship between the individual and the data recipient, and the important role of trust in privacy [33]. Participants may attribute more trust to a specific person with whom a relationship discussing health has been established (ie, their doctor), rather than the health system more generally, represented by the EHR system. Indeed, previous research has shown that when a trusting relationship is not established, participants resist sharing sensed physical activity data with health providers [34]. In our study, the fact that participants did not always extend trust and willingness to share their data with the EHR system may indicate that they have concerns about who can access their data.
The role of the recipient in comfort with data sharing, therefore, has important implications for the use of apps that acquire and transmit sensed information related to mental health, especially given the variety of people who are often involved in mental health treatment and management. Providers as well as technological system designers must be aware that although individuals may be comfortable sharing their sensed data with their doctor, they may not be comfortable sharing it more widely, even with people who are already involved in their mental health management such as other health professionals, via the EHR system, or family members. As apps are integrated into clinical care, upfront and ongoing conversations regarding the distribution of sensed data will become increasingly critical, as will provider education about sensed data and the ability for providers and individuals to manage sharing options.
In line with contextual integrity, participants’ comfort with sharing sensed data significantly differed by data type. The way in which these different data types fit within existing information norms in the doctor-patient context could possibly explain the observed differences. Sleep, mood, and physical activity data types may closely align with doctor-patient information norms, as they are often discussed with providers. On the other hand, the data types that participants were least comfortable in sharing—communication logs, location, and social activity—are not commonly discussed with doctors. Thus, discussing these data types may violate existing norms and therefore be less willingly shared with providers.
Another explanation for the observed difference in comfort with sharing across data types is that communication logs, location, and social activity data may carry additional sensitivities. For example, just four points of GPS data can reveal the identity of up to 95% of individuals [35]; personal communications document a wider variety of behaviors, habits, and beliefs than data like sleep patterns, and sharing social activity data might put the privacy of other individuals at risk. Such differences related to data type, information norms, and the unique sensitivities associated with certain data are critical to understand and heed as we begin to create systems that harness sensor data for mental health treatment and support.
Comfort with data sharing could not be predicted based on the individual characteristics of age and presence of depression or anxiety, supporting an important tenet of contextual integrity: Contextual factors more strongly influence individuals’ privacy preferences than individual characteristics [36]. The lack of differences in comfort with sharing sensed data between individuals with depression or anxiety and those without a mental health condition found in our study is interesting and important, given the stigmatized nature of these common mental health conditions [37] and the risks associated with sharing. However, further research should aim to elucidate whether any differences in the nature of concerns regarding data privacy exist between people with common mental health disorders and those without such disorders, in order to mitigate any specific concerns of this population.
Irrespective of people’s mental health status, ethicists have raised concerns that personal sensing projects challenge traditional research ethics’ tenets of informed consent and risk mitigation, because data collection is both unobtrusive (easily forgotten and not easily avoided) and pervasive (recording many aspects of a participants’ daily habits for long periods) [19,38], and the inferential harms of passively collected data are often poorly understood [39]. Our findings suggest that personal sensing projects should use contextual factors to guide research design and should revise participant consent processes to address these ethical concerns. For example, individuals should be afforded the opportunity to select specific allowances for data sharing based on factors such as type, purpose, recipient, and sensitivity, rather than providing a blanket consent. Further, researchers should not assume that the acceptability of using sensed data is easily generalized between different research contexts or types of data collected without first considering the comparability of the contextual norms (roles, data types, transmission principles, and uses). Beyond these considerations, data collectors must also ensure protections, such as data deletion, deidentification, and restrictions on sharing.
Limitations
Although this study reveals important differences in the comfort level of individuals sharing sensed data based on the recipient and data type, a number of limitations should be considered when interpreting the results. First, survey participants consented to participate in a wider study that collected data from a number of smartphone sensors over a 6-week period. Therefore, the views of individuals who were deeply uncomfortable with sharing sensed data were likely not represented within the sample. This sampling bias reduces the generalizability of these findings to the general population. However, these findings do represent sensitivities of people who are open to using personal sensing apps. As a further caution to generalizability, we note that the majority of the sample comprised white, employed, and well educated people. Given that privacy is experienced by different populations in distinct ways [40], further work should examine privacy associated with mental health across a broader section of the community.
This study asked general questions about individuals’ willingness to share sensed data and did not explore richer contextual factors such as perceived benefits or risks that are often considered by individuals when making decisions about privacy [39]. Therefore, the behavior and decisions made by individuals when deciding whether to share sensed data may vary from what is outlined here. The importance of richly contextualizing information about the collection of sensed data for mental health was highlighted by a recent study [34] on veterans with posttraumatic stress disorder. Researchers found that the lack of clarity of purpose was a primary reason given by participants for not using a wearable fitness tracker to support treatment. Lack of purpose also contributed to uncertainty and increased discomfort about the collection of sensed GPS and Bluetooth data in a feasibility study of a passive data–collection app [41]. Individuals’ existing beliefs about the importance of privacy and data control have also been shown to interact with contextual factors when people make privacy decisions [36]. These beliefs were not explored in the current study. Future research that more richly contextualizes the collection and sharing of sensed data and explores existing beliefs using vignettes, semistructured interviews, or other contextualized methods would provide deeper insight into why the reported differences in comfort with sharing sensed data exist.
Finally, considering the importance of context in our study, it is worth noting that the data in this study were collected before a number of highly publicized data privacy scandals took place, most notably, that of Cambridge Analytica, in which data were misused, and that of Strava, where released data had unforeseen consequences for disclosure. These events brought to light the importance of contextual factors such as unforeseen harms and data re-identification, purpose, and recipient. Individuals’ attitudes toward passive data collection may have since changed, again highlighting the need for further contextualized research regarding the privacy of sensed data for mental health.
Conclusions
In line with the contextual integrity framework, participants’ comfort with sharing sensed data was dependent on the type of data collected and the intended recipient of those data. Given these differences, research and treatment protocols and systems designed to use sensed data must consider differences in individuals’ comfort depending on contextual factors. These differences represent important considerations, as systems are developed to integrate sensed data into health systems and use these data to encourage behavior change and mental health management. The reported insights will help establish data sharing norms for personal sensing and manage or mitigate privacy concerns as we develop systems to collect, share, and use sensed data to support mental health treatment.
Acknowledgments
This research was supported by the National Institute of Mental Health (R01 MH111610 and P20 MH090318 to DM).
Abbreviations
- EHR
electronic health record
- GAD-7
Generalized Anxiety Disorder - 7 item
- GPS
global positioning system
- PHQ-9
Patient Health Questionnaire - 9 item
Footnotes
Conflicts of Interest: None declared.
References
- 1.Jain SH, Powers BW, Hawkins JB, Brownstein JS. The digital phenotype. Nat Biotechnol. 2015;33(5):462–3. doi: 10.1038/nbt.3223. [DOI] [PubMed] [Google Scholar]
- 2.Schatz BR. National Surveys of Population Health: Big Data Analytics for Mobile Health Monitors. Big Data. 2015;3(4):219–229. doi: 10.1089/big.2015.0021. http://europepmc.org/abstract/MED/26858915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Insel TR. Digital Phenotyping: Technology for a New Science of Behavior. JAMA. 2017;318(13):1215–1216. doi: 10.1001/jama.2017.11295. [DOI] [PubMed] [Google Scholar]
- 4.Barnett I, Torous J, Staples P, Sandoval L, Keshavan M, Onnela J. Relapse Prediction in Schizophrenia Through Digital Phenotyping: A Pilot Study. Neuropsychopharmacology. 2018;43(8):1660–1666. doi: 10.1038/s41386-018-0030-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Faurholt-Jepsen M, Frost M, Vinberg M, Christensen EM, Bardram JE, Kessing LV. Smartphone Data as Objective Measures of Bipolar Disorder Symptoms. Psychiatry Res. 2014;217(1-2):124–7. doi: 10.1016/j.psychres.2014.03.009. [DOI] [PubMed] [Google Scholar]
- 6.Chow PI, Fua K, Huang Y, Bonelli W, Xiong H, Barnes LE, Teachman BA. Using Mobile Sensing to Test Clinical Models of Depression, Social Anxiety, State Affect, and Social Isolation Among College Students. J Med Internet Res. 2017;19(3):e62. doi: 10.2196/jmir.6820. http://www.jmir.org/2017/3/e62/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mohr DC, Zhang M, Schueller SM. Personal Sensing: Understanding Mental Health Using Ubiquitous Sensors and Machine Learning. Annu Rev Clin Psychol. 2017;13:23–47. doi: 10.1146/annurev-clinpsy-032816-044949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Osmani V. Smartphones in Mental Health: Detecting Depressive and Manic Episodes. IEEE Pervasive Comput. 2015 Jul;14(3):10–13. doi: 10.1109/MPRV.2015.54. [DOI] [Google Scholar]
- 9.Saeb S, Zhang M, Karr CJ, Schueller SM, Corden ME, Kording KP, Mohr DC. Mobile Phone Sensor Correlates of Depressive Symptom Severity in Daily-Life Behavior: An Exploratory Study. J Med Internet Res. 2015;17(7):e175. doi: 10.2196/jmir.4273. http://www.jmir.org/2015/7/e175/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Canzian L, Musolesi M. Trajectories of Depression: Unobtrusive Monitoring of Depressive States by Means of Smartphone Mobility Traces Analysis. Proceedings of the 2015 ACM international joint conference on pervasive and ubiquitous computing; Sept 7-11; Osaka, Japan. ACM Press; 2015. [Google Scholar]
- 11.Saeb S, Lattie EG, Schueller SM, Kording KP, Mohr DC. The Relationship Between Mobile Phone Location Sensor Data and Depressive Symptom Severity. PeerJ. 2016;4:e2537. doi: 10.7717/peerj.2537. doi: 10.7717/peerj.2537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Saeb S, Cybulski TR, Schueller SM, Kording KP, Mohr DC. Scalable Passive Sleep Monitoring Using Mobile Phones: Opportunities and Obstacles. J Med Internet Res. 2017;19(4):e118. doi: 10.2196/jmir.6821. http://www.jmir.org/2017/4/e118/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Doryab A, Min J, Wiese J, Zimmerman J, Hong J. Detection of Behavior Change in People with Depression. AAAI workshop: Modern Artificial Intelligence for Health Analytics; Jul 27-28; Quebec, Canada. 2014. [Google Scholar]
- 14.Rabbi M, Ali S, Choudhury T, Berke E. Passive and In-situ Assessment of Mental and Physical Well-being using Mobile Sensors. Proc ACM Int Conf Ubiquitous Comput. 2011;2011:385–394. doi: 10.1145/2030112.2030164. http://europepmc.org/abstract/MED/25285324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wang R, Chen F, Chen Z, Li T, Harari G, Tignor S, Zhou X, Ben-Zeev D, Campbell A. StudentLife: Assessing Mental Health, Academic Performance and Behavioral Trends of College Students using Smartphones. Proceedings of the 2014 ACM International Joint Conference on Pervasive and Ubiquitous Computing; Sept 13-17; Seattle, WA. StudentLife: 2014. [Google Scholar]
- 16.Adams A. Users' Perception of privacy in Multimedia Communication. CHI'99 Extended Abstracts on Human Factors in Computing Systems; May 15-20; Pittsburgh, PA. 1999. [Google Scholar]
- 17.Barth A, Datta A, Mitchell J, Nissenbaum H. Privacy and Contextual Integrity: Framework and Applications. Proceedings of the 2006 IEEE Symposium on Security and Privacy; May 21-24; Berkeley/Oakland, CA. 2006. [Google Scholar]
- 18.Nissenbaum H. Privacy in Context: Technology, Policy, and the Integrity of Social Life. Stanford, CA: Stanford University Press; 2009. [Google Scholar]
- 19.Zimmer M. Addressing Conceptual Gaps in Big Data Research Ethics: An Application of Contextual Integrity. Social Media+Society. 2018;4(2):1–11. doi: 10.1177/2056305118768300;4. [DOI] [Google Scholar]
- 20.Dehling T, Gao F, Schneider S, Sunyaev A. Exploring the Far Side of Mobile Health: Information Security and Privacy of Mobile Health Apps on iOS and Android. JMIR Mhealth Uhealth. 2015;3(1):e8. doi: 10.2196/mhealth.3672. http://mhealth.jmir.org/2015/1/e8/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pentland A, Lazer D, Brewer D, Heibeck T. Using Reality Mining to Improve Public Health and Medicine. Stud Health Technol Inform. 2009;149:93–102. [PubMed] [Google Scholar]
- 22.Shilton K. Four Billion Little Brothers? Commun ACM. 2009 Nov 01;52(11):48. doi: 10.1145/1592761.1592778. [DOI] [Google Scholar]
- 23.Klasnja P, Consolvo S, Choudhury T, Beckwith R, Hightower J. Exploring Privacy Concerns About Personal Sensing. Proceedings of the 7th International Conference on Pervasive Computing; May 11-14; Nara, Japan. 2009. [Google Scholar]
- 24.Proudfoot J, Parker G, Hadzi Pavlovic D, Manicavasagar V, Adler E, Whitton A. Community attitudes to the appropriation of mobile phones for monitoring and managing depression, anxiety, and stress. J Med Internet Res. 2010 Dec 19;12(5):e64. doi: 10.2196/jmir.1475. http://www.jmir.org/2010/5/e64/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nicholas J, Boydell K, Christensen H. Beyond Symptom Monitoring: Consumer Needs for Bipolar Disorder Self-management Using Smartphones. Eur Psychiatry. 2017 Dec;44:210–216. doi: 10.1016/j.eurpsy.2017.05.023. [DOI] [PubMed] [Google Scholar]
- 26.Lin J, Liu B, Sadeh N, Hong J. Modeling Users Mobile App Privacy Preferences: Restoring Usability in a Sea of Permission Settings. SOUPS'14 Proceedings of the Tenth USENIX Conference on Usable Privacy and Security; Jul 09-11; Menlo Park, CA. 2014. [Google Scholar]
- 27.Bohn MJ, Babor TF, Kranzler HR. The Alcohol Use Disorders Identification Test (AUDIT): Validation of a Screening Instrument for Use in Medical Settings. J Stud Alcohol. 1995;56(4):423–32. doi: 10.15288/jsa.1995.56.423. [DOI] [PubMed] [Google Scholar]
- 28.Skinner HA. The Drug Abuse Screening Test. Addict Behav. 1982;7(4):363–71. doi: 10.1016/0306-4603(82)90005-3. [DOI] [PubMed] [Google Scholar]
- 29.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: Validity of a Brief Depression Severity Measure. J Gen Intern Med. 2001;16(9):606–13. doi: 10.1046/j.1525-1497.2001.016009606.x. http://europepmc.org/abstract/MED/11556941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Beck A, Steer R, Brown G. Manual for the Beck Depression Inventory-II. San Antonio, USA: Psychological Corporation; 1996. [Google Scholar]
- 31.Hirschfeld RM, Williams JB, Spitzer RL, Calabrese JR, Flynn L, Keck PE, Lewis L, McElroy SL, Post RM, Rapport DJ, Russell JM, Sachs GS, Zajecka J. Development and Validation of a Screening Instrument for Bipolar Spectrum Disorder: The Mood Disorder Questionnaire. Am J Psychiatry. 2000;157(11):1873–5. doi: 10.1176/appi.ajp.157.11.1873. [DOI] [PubMed] [Google Scholar]
- 32.Spitzer RL, Kroenke K, Williams JBW, Löwe B. A Brief Measure for Assessing Generalized Anxiety Disorder: The GAD-7. Arch Intern Med. 2006;166(10):1092–7. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- 33.Nissenbaum H. Privacy as contextual integrity. Wash L Rev. 2004;79:101–139. https://crypto.stanford.edu/portia/papers/RevnissenbaumDTP31.pdf. [Google Scholar]
- 34.Ng A, Reddy M, Zalta AK, Schueller SM. Veterans' Perspectives on Fitbit Use in Treatment for Post-Traumatic Stress Disorder: An Interview Study. JMIR Ment Health. 2018;5(2):e10415. doi: 10.2196/10415. http://mental.jmir.org/2018/2/e10415/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.De Montjoye YA, Hidalgo CA, Verleysen M, Blondel VD. Unique in the Crowd: The Privacy Bounds of Human Mobility. Sci Rep. 2013;3:1376. doi: 10.1038/srep01376. doi: 10.1038/srep01376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Martin K, Shilton K. Why experience matters to privacy: How context-based experience moderates consumer privacy expectations for mobile applications. J Assn Inf Sci Tec. 2015 May 05;67(8):1871–1882. doi: 10.1002/asi.23500. doi: 10.1002/asi.23500. [DOI] [Google Scholar]
- 37.Corrigan P, Watson A. The Paradox of Self-Stigma and Mental Illness. Clinical Psychology: Science and Practice. 2002;9:35–53. doi: 10.1093/clipsy.9.1.35. doi: 10.1093/clipsy.9.1.35. [DOI] [Google Scholar]
- 38.Vitak J, Shilton K, Ashktorab Z. Beyond the Belmont principles: Ethical challenges, practices, and beliefs in the online data research community. Proceedings of the 19th ACM Conference on Computer-Supported Cooperative Work & Social Computing; Feb 27-Mar 02; San Francisco, CA. ACM Press; 2016. [Google Scholar]
- 39.Beckwith R, Mainwaring S. Privacy: Personal information, threats, and technologies. Proceedings International Symposium on Technology and Society, 2005 Weapons and Wires: Prevention and Safety in a Time of Fear ISTAS; Jun 8-10; Los Angeles, CA. 2005. [Google Scholar]
- 40.Marwick A, Boyd D. Understanding Privacy at the Margins. International Journal of Communication. 2018;12:1157–65. https://ijoc.org/index.php/ijoc/article/view/7053/2293. [Google Scholar]
- 41.Boonstra TW, Nicholas J, Wong QJ, Shaw F, Townsend S, Christensen H. Using Mobile Phone Sensor Technology for Mental Health Research: Integrated Analysis to Identify Hidden Challenges and Potential Solutions. J Med Internet Res. 2018;20(7):e10131. doi: 10.2196/10131. http://www.jmir.org/2018/7/e10131/ [DOI] [PMC free article] [PubMed] [Google Scholar]


