Abstract
Background
Asthma is a common chronic disease worldwide. Inhalers are often prescribed to help control asthma symptoms, improve quality of life and reduce the risk of exacerbations or flare‐ups. However, evidence suggests that many people with asthma do not use their inhaler correctly. It is therefore important to evaluate whether interventions aimed specifically at improving technique are effective and safe, and whether use of these interventions translates into improved clinical outcomes.
Objectives
To assess the impact of interventions to improve inhaler technique on clinical outcomes and safety in adults and children with asthma.
Search methods
We searched the Cochrane Airways Trials Register, which contains records compiled from multiple electronic and handsearched resources. We also searched trial registries and reference lists of primary studies. We conducted the most recent search on 23 November 2016.
Selection criteria
We included studies comparing a group of adults or children with asthma receiving an inhaler technique intervention versus a group receiving a control or alternative intervention. We included parallel and cluster‐randomised trials of any duration conducted in any setting, and planned to include only the first phase of any cross‐over trials identified. We included studies reported as full‐text articles, those published as abstracts only and unpublished data.
Data collection and analysis
Two review authors screened the search results for eligible studies. We extracted outcome data, assessed risk of bias in duplicate and resolved discrepancies by involving another review author. We grouped studies making similar comparisons by consensus (e.g. all those comparing enhanced inhaler technique education vs usual care) and conducted meta‐analyses only if treatments, participants and the underlying clinical question were similar enough for pooling to make sense. We analysed dichotomous data as odds ratios, and continuous data as mean differences or standardised mean differences, all with random‐effects models. We described skewed data narratively. We graded the results and presented evidence in 'Summary of findings' tables for each comparison. Primary outcomes were inhaler technique, asthma control and exacerbations requiring at least oral corticosteroids (OCS).
Main results
This review includes 29 parallel randomised controlled trials (RCTs) (n = 2210), although not all reported relevant or useable data. All participants had asthma, and follow‐up ranged from 2 to 26 weeks. Most studies were at low or unclear risk of selection and attrition biases and at high risk for biases associated with blinding. We considered most of the evidence to be of low quality owing to these biases and to imprecision in the estimates of effect.
We classified studies into three comparisons: enhanced face‐to‐face training session(s), multi‐media‐delivered inhaler training (e.g. DVD, computer app or game) and technique feedback devices. Differences between interventions, populations and outcome measures limited quantitative analyses, particularly for exacerbations, adverse events, unscheduled visits to a healthcare provider and absenteeism from work or school.
Enhanced inhaler technique education and multi‐media training improved technique in most studies immediately after the intervention and at follow‐up, although the variety of checklists used meant that this was difficult to assess reliably. For both adults and children, how and when inhaler technique was assessed appeared to affect whether inhaler technique improved and by how much.
Analyses of the numbers of people who demonstrated correct or 'good enough' technique were generally more useful than checklist scores. Adult studies of enhanced education showed benefit when this metric was used at 2 to 26 weeks' follow‐up (odds ratio (OR) 5.00, 95% confidence interval (CI) 1.83 to 13.65; 258 participants; three studies; 31 per 100 with correct technique in the control group compared with 69 (95% CI 45 to 86) in the education group; moderate‐quality evidence). A similar result was seen in studies looking at feedback devices at four weeks' follow‐up (OR 4.80, 95% CI 1.87 to 12.33; 97 participants; one study; 51 per 100 with correct technique in the control group compared with 83 (95% CI 66 to 93) in the feedback group; low‐quality evidence). However, the benefit of multi‐media training for adults even immediately after the intervention was uncertain (OR 2.15, 95% CI 0.84 to 5.50; 164 participants; two studies; I² = 49%; 30 per 100 in the control group with correct technique compared with 47 (95% CI 26 to 70) in the multi‐media group; moderate‐quality evidence). Evidence tended to be less clear for children, usually because results were based on fewer and smaller studies.
Some studies did not report exacerbations in a way that allowed meta‐analysis; others provided inconclusive results. Inhaler technique interventions provided some benefit for asthma control and quality of life but generally did not lead to consistent or important clinical benefits for adults or children. Confidence intervals included no difference or did not reach a threshold that could be considered clinically important. Responder analyses sometimes showed improvement among more people in the intervention groups, even though the mean difference between groups was small. We found no evidence about harms.
Authors' conclusions
Although interventions to improve inhaler technique may work in some circumstances, the variety of interventions and measurement methods used hampered our ability to perform meta‐analyses and led to low to moderate confidence in our findings. Most included studies did not report important improvement in clinical outcomes. Guidelines consistently recommend that clinicians check regularly the inhaler technique of their patients; what is not clear is how clinicians can most effectively intervene if they find a patient's technique to be inadequate, and whether such interventions will have a discernible impact on clinical outcomes.
Plain language summary
Strategies to help people with asthma use their inhaler correctly
Background to the question
Many asthma drugs are taken by an inhaler, which deposits the drug directly into the lungs. It is important that the inhaler is taken properly, so the patient gets the most benefit. Taken properly, asthma drugs can improve symptoms and reduce attacks.
Lots of people do not use their devices correctly. This means that the drug is not delivered properly to the lungs, and as a result, asthma may not be as well controlled as it should be. People also tell us that they can have more than one type of inhaler, so it is confusing to know what to do.
We wanted to find out whether teaching people with asthma how to use their inhalers works, and whether this leads to better control of symptoms and fewer attacks. It may seem obvious, but it is important that doctors and nurses know how best to help people with asthma.
Study characteristics
We found 29 studies involving 2210 people with asthma. Studies lasted between 2 and 26 weeks. Studies reported inhaler technique on a range of different checklists.
We grouped studies into three types: studies testing enhanced face‐to‐face training session(s), studies using multi‐media to deliver inhaler training (e.g. a video, computer app or game) and studies testing devices that give people visual or audio feedback about technique.
Studies tested different types of training and used different measures to gauge success, meaning that we could not bring data together. This was particularly true when we tried to assess effects on asthma attacks, adverse events, visits to a healthcare provider and absences from work or school.
Key results
Both face‐to‐face and multi‐media inhaler training improved inhaler technique in most studies, although results varied depending on how and when each technique was assessed.
Some studies reported the number of people who had correct or 'good enough' technique. More people had correct or 'good enough' technique after face‐to‐face training and with feedback devices. But the benefit of multi‐media training for adults was uncertain.
Interventions that provide inhaler training may bring some benefit for quality of life and asthma control among adults and children, but results were varied and studies were small.
Children may receive some benefit but results tended to be less clear for children because fewer and smaller studies have included children as participants.
Quality of the evidence
For studies like these, it is not possible to blind people to their assigned group. This may bias how people behave or respond to questionnaires, which reduced our confidence in the findings. We were uncertain about other results because studies did not provide enough data to show clear benefit.
Conclusions
We cannot say for sure what is the best way to help people learn how to use their inhaler properly. It is important that patients understand how their inhaler works, so they should ask their doctor or nurse for help.
We also use Cochrane Reviews to make suggestions for future research. We suggest that trials should last longer than six months and should report adherence information. The most useful information reported was the number of people who had 'good enough' inhaler technique, so we urge future trials to report this as well.
Summary of findings
Background
Description of the condition
Asthma is one of the most common chronic diseases in the world. It affects more than 300 million adults and children, and its prevalence is rising. By 2025, it is estimated that a further 100 million people may be affected by asthma. Asthma is thought to be responsible for approximately 1% of the disability‐adjusted life‐years lost globally, and for one in 250 deaths, which makes effective treatment an international priority (Masoli 2004). Although previously asthma was thought to be a disease primarily of high‐income countries, it is now recognised that much of the global asthma burden affects low‐ and middle‐income countries (Asher 2006). Asthma is estimated to be the 14th most important disease in the world in terms of extent and duration of disability (Global Asthma Network 2014). Asthma is characterised by chronic inflammation of the airways, leading to symptoms that include cough, wheeze, chest tightness and shortness of breath, which typically vary over time. People with asthma may experience a short‐term worsening of symptoms, known as a ‘flare‐up’, an ‘attack’ or an ‘exacerbation’, which may be life‐threatening (GINA 2016).
Inhalation therapy is the most effective treatment for almost all people with asthma (Dekhuijzen 2007). More than 50 years has passed since the first inhalers for asthma were introduced for routine clinical use (Crompton 2006a). The major advantage of the inhaled route is that the drug is delivered directly to the airways, where it has a rapid onset of action with a minimal dose, thus limiting systemic side effects. Inhalers are also portable and compact, which makes them suitable for ambulatory therapy (McFadden 1995).
Today, commonly used inhaled therapies include short‐acting beta‐agonists (SABAs, e.g. salbutamol); short‐acting muscarinic antagonists (SAMAs, e.g. ipratropium); long‐acting beta‐agonists (LABAs, e.g. salmeterol); long‐acting muscarinic antagonists (LAMAs, e.g. tiotropium); and inhaled corticosteroids (ICSs, e.g. beclomethasone) (BNF 2016). These medications can be used as required to relieve acute symptoms of asthma (e.g. SABAs, SAMAs) or for daily maintenance to prevent worsening of symptoms (i.e. ICS with LABA or LAMA as an add‐on) (BTS/SIGN 2014). Sustained use of ICSs reduces airway inflammation, improves symptoms and reduces asthma‐related morbidity and mortality (Barnes 2003; Bårnes 2015).
The first inhalation devices for asthma were pressurised metered dose inhalers (pMDIs), which were introduced in the 1950s; today, many devices are available and different techniques are required for their proper use (Crompton 2006a; GINA 2016). Inhaler devices can be divided into two main groups: pMDIs and dry powder inhalers (DPIs). pMDIs require the patient to co‐ordinate pressing down on the inhaler canister whilst initiating a slow and deep inhalation, and DPIs require a rapid and forcible inhalation. Both inhaler types require a full exhalation before use, and breath‐holding is recommended after use (Haughney 2010). For those who find the co‐ordination required to use a pMDI difficult, a modified 'breath‐actuated' pMDI can be prescribed or an add‐on device can be used with the inhaler, such as a ‘spacer’ or a ‘holding chamber’. Spacers provide the added advantage of improving delivery of the drug to the appropriate portion of the airway while preventing oropharyngeal deposition, which is particularly important for ICSs (GINA 2016). Some experts recommend that a spacer device should be used universally for children five years of age or younger (Sanchis 2013; GINA 2016). The best choice of inhaler depends on patient factors such as age, co‐ordination and lung function, as well as on patient preference and local availability and cost (Haughney 2010; GINA 2016).
Description of the intervention
An intervention to improve inhaler technique may take many forms, but these interventions broadly fall into three categories: technological adaptations or interventions; education of the healthcare provider; and education of the patient or caregiver (Inhaler Error Steering Committee 2013). However, in reality, any given intervention is unlikely to fall neatly into any single category; for example, a device that provides feedback on inhaler technique may have the dual effect of providing education to the patient and healthcare provider. Interventions may promote self‐management by the patient, monitoring by the healthcare provider or both. They may be delivered face‐to‐face, in writing or through the use of visual or technological aids.
Several currently available inhaler ‘training tools’ could fall under the ‘technological’ umbrella. These devices have various purposes, which include giving feedback to the patient or healthcare provider about inhaler technique and allowing the patient to ‘practise’ the correct technique; helping to identify the best type of inhaler for that patient; or testing the inhalation capacity and co‐ordination of the patient (Lavorini 2010).
In addition, inhalers themselves may be developed to be easier to use; of note, the newer DPIs may be associated with better adherence (Roy 2011), which may be a result of ease of use, and breath‐actuated pMDIs should be considered for those who struggle with co‐ordination (Levy 2013). Simple technological devices such as ‘spacers’ may also improve technique and drug delivery for some patients (McFadden 1995). However, the literature does not suggest that one type of inhaler is consistently associated with a better technique than any other (van Beerendonk 1998). A 2001 Health Technology Assessment report concluded that no consistent advantage is offered by one type of inhaler over another after proper training, and so the cheapest option should be selected in most cases (Brocklebank 2001). More recently, a 'real‐world' cost‐effectiveness analysis based on routine observational data compared outcomes for patients initiated on ICS via a pMDI, a breath‐actuated inhaler pMDI or a DPI. Findings suggest that the real‐world effectiveness of ICS inhalers varies (which may be attributed in part to technique) and that both subsequent healthcare usage costs and the cost of the inhaler should be taken into account when prescribing (Kemp 2010).
Education of both healthcare professionals and patients about correct technique may be delivered in several ways. Multi‐media training tools may comprise Internet‐based or DVD video clips that demonstrate correct inhaler use, as well as interactive components such as games or quizzes (Navarre 2007; Lavorini 2010; Poureslami 2012). Indeed, it has been demonstrated that education delivered via the Internet can be as effective, at least in the short term, as face‐to‐face training for healthcare professionals (Erikson 2003; Toumas 2009).
Face‐to‐face education or coaching is another commonly used strategy for improving inhaler technique. This may be done as part of a comprehensive asthma management package and can be delivered to, or by, a variety of healthcare professionals, including nurses, pharmacists and physicians (Verver 1996; Basheti 2005; Basheti 2008; Armour 2013). Studies have shown that even brief interventions can substantially improve medical professionals’ knowledge about correct technique (Basheti 2009; Kim 2009). Trials of telephone interventions aimed at patients have yielded mixed results (Bynum 2001; Nelson 2011).
How the intervention might work
The breadth of interventions available to improve inhaler technique means that no single mechanism has been identified by which clinical outcomes might benefit. Some technological interventions may allow optimisation of the choice of inhaler for a patient by characterising the patient's breathing pattern, thus improving technique, or by allowing a patient to hone his or her technique at home or with the assistance of a healthcare professional (Lavorini 2010). Attempts to minimise the number of different types of inhalers prescribed for one patient may also improve technique; studies suggest that both adults and children who are prescribed more than one type of inhaler, especially a mixture of pMDIs and DPIs, are more likely to make inhaler errors (van der Palen 1999; Alotabi 2011).
Other interventions may ensure that a patient is following the correct sequence of steps for proper use; physical demonstration appears superior to verbal or written instructions alone (Basheti 2005; Bosnic‐Anticevich 2010), and a multi‐media presentation may be superior to written information alone (Savage 2003). This suggests that being able to watch and copy as the correct technique is demonstrated in person or via a video clip or the Internet is an important requirement for the intervention in many cases.
Children present a unique challenge, and evidence suggests that even after training, their inhaler technique may remain inadequate for effective drug delivery (Kamps 2000). Some studies suggest that repeated training with reinforcement is important (Deerojanawong 2009), that audiovisual training alone is insufficient and that children show the greatest improvement when they receive individual training with follow‐up at home (Agertoft 1998).
Knowledge of how a technique is assessed and recorded is important for determining whether or not an intervention has worked. As anticipated, we found that not all studies used a validated measurement instrument (Rootmensen 2010). We considered how each trial that contributed to this Cochrane Review assessed technique and how this impacted our confidence in this outcome.
Why it is important to do this review
As many as 70% to 80% of people with asthma are unable to use their inhaler device correctly (GINA 2016); poor technique has been associated with age, sex, educational level and emotional problems (Rootmensen 2010). Studies suggest that up to 67% of clinicians cannot describe the steps involved or cannot demonstrate correct inhaler use. Furthermore, of the approximate USD 50 billion spent annually on inhalers (for all respiratory conditions) in the USA, USD 7 to 15 billion is wasted owing to improper use (Fink 2005). Mistakes in inhaler use have been associated with poor clinical outcomes in asthma, including more frequent emergency department (ED) visits; hospitalisations; prescriptions of oral steroids and antimicrobials; and poorer asthma control as assessed by the Asthma Control Questionnaire (ACQ), the Asthma Instability Score (AIS) and the Asthma Therapy Assessment Questionnaire (ATAQ) (Giraud 2001; Melani 2011; Al‐Jahdali 2013; Westerik 2016). A similar association is seen in children (Capanoglu 2015). Evidence suggests that even after a successful intervention, many patients revert to incorrect use within a short time (Price 2002; Crompton 2006b).
International and national guidelines highlight that assessment of inhaler technique is an essential component of asthma care, especially for patients with inadequate control (BTS/SIGN 2014; GINA 2016). Recently, the Aerosol Drug Management Improvement Team (ADMIT) published a series of papers that focus on the need to improve inhalation technique in Europe (ADMIT 2016). In summary, the ADMIT reports suggest that specific education for patients and clinicians on correct technique for inhaler use is needed and should be repeated frequently; devices that provide ‘feedback’ about appropriate technique are useful; information about the correct technique for each device should be easily accessible; and standardised prescribing throughout Europe is preferable (Crompton 2006b; Dekhuijzen 2007). The Global Allergy and Asthma European Network (GA²LEN) initiative, which focusses on problematic severe asthma in children, calls for repeated checking of an individual's inhaler technique (Hedlin 2010). This inevitably raises the question of what is the most effective way to correct and improve improper technique.
Lewis 2016 developed a model to estimate the impact of poor inhalation technique on the economic burden of asthma and chronic obstructive pulmonary disease (COPD) in three European countries (Spain, Sweden and the United Kingdom). Study authors attributed 2.2% to 2.7% of direct asthma and COPD costs to poor inhalation technique, totaling 105 million euros across the three countries. Inclusion of lost productivity costs in additional analyses revealed that the annual expenditure was increased to 3.3 billion euros in the UK and 6.4 billion euros across all three countries. These figures further highlight the need for effective interventions to improve inhaler technique.
Although the literature provides compelling evidence of the need for good inhaler technique in maintaining asthma control, the most effective ways to improve inhaler technique and thus improve clinical outcomes remain unclear. This Cochrane Review examined the evidence for this question for both adults and children.
Objectives
To assess the impact of interventions to improve inhaler technique on clinical outcomes and safety in adults and children with asthma.
Methods
Criteria for considering studies for this review
Types of studies
We included parallel and cluster‐randomised controlled trials (RCTs) of any duration conducted in any setting. If we identified cross‐over trials, we included only data from the first part of the study because of the potential for carry‐over effects from the intervention.
We included studies reported as full‐text articles, published as abstracts only and described in unpublished data.
Types of participants
We included both adults and children with asthma, diagnosed according to national or international guidelines or by a healthcare professional. We excluded participants with other respiratory comorbidities, including COPD and bronchiectasis. If we identified a study in which only a subset of participants had asthma, we included these participants if we were able to obtain disaggregated data.
We intended to analyse studies aimed solely at children (younger than 12 years) separately from those aimed at adults and adolescents (12 years of age and older). If within each of these comparisons we found trials focused on a more narrow age range (e.g. children younger than five years), we explored this potential source of heterogeneity. If a study recruited both adults and children and did not provide disaggregated data, we were guided by the average age of participants to determine in which comparison we should include the study.
Types of interventions
We included studies that compared an intervention primarily aimed at improving inhaler technique versus any of the following.
Usual care/No additional intervention.
An alternative intervention that did not primarily aim to improve inhaler technique (e.g. asthma education only vs asthma education plus an inhaler technique demonstration).
An alternative intervention of a different type or intensity, also aimed at improving inhaler technique (e.g. written instructions only vs written instructions plus physical demonstration).
It is likely that the effect of the intervention will be systematically different depending on which of these three types of comparison groups each study used, so we meta‐analysed results separately unless we had a justification for pooling data (i.e. if treatments, participants and the underlying clinical question were similar enough for pooling to make sense).
Trial interventions may be delivered to healthcare professionals (e.g. pharmacists, healthcare assistants, nurses, physicians) or directly to patients or their parents/caregivers. Interventions may involve education delivered face‐to‐face or remotely, and may include written, verbal or multi‐media methods of delivery. Interventions may also involve a device or a piece of technology designed to improve inhaler technique.
'Usual care' comprises the treatment that a patient with asthma in this setting would normally receive according to local or national guidelines, or according to the judgement of their healthcare provider. This may include routine advice about inhaler technique but not about the specific intervention that is being studied.
Types of outcome measures
Primary outcomes
Inhaler technique (as assessed/rated by triallist; change from baseline scores preferred if available)
Asthma control (preferably measured on a validated scale, e.g. Asthma Control Questionnaire (ACQ))
Asthma exacerbations requiring at least oral corticosteroids (OCSs)
Secondary outcomes
Quality of life (preferably measured on a validated scale, e.g. Asthma Quality of Life Questionnaire (AQLQ))
Adverse events (including local drug side effects, which can be associated with improper inhaler technique)
Unscheduled visits to healthcare provider (e.g. emergency department (ED), primary care)
Absenteeism from work or school
Reporting of one or more of the outcomes listed here within a study was not an inclusion criterion for the review.
We chose these outcomes to reflect the main aim of the intervention (improved inhaler technique) but also patient‐important clinical outcomes, such as exacerbations and quality of life. Adverse events may be associated with improper inhaler use (e.g. oropharyngeal deposition of ICS) and may decrease post intervention. Alternatively, some participants may have noted an increase in medication side effects as they were not receiving a therapeutic dose of their inhaler previously. We did not anticipate many serious adverse events linked to the intervention and so chose to capture all adverse events.
Search methods for identification of studies
Electronic searches
We identified studies from the Cochrane Airways Trials Register, which is maintained by the Information Specialist for the Group. The Cochrane Airways Trials Register includes studies identified from several sources.
Monthly searches of the Cochrane Central Register of Controlled Trials (CENTRAL), through the Cochrane Register of Studies Online (crso.cochrane.org).
Weekly searches of MEDLINE Ovid SP 1946 to date.
Weekly searches of Embase Ovid SP 1974 to date.
Monthly searches of PsycINFO Ovid SP.
Monthly searches of the Cumulative Index to Nursing and Allied Health Literature (CINAHL) EBSCO.
Monthly searches of Allied and Complementary Medicine (AMED) EBSCO.
Handsearches of the proceedings of major respiratory conferences.
Studies included in the Trials Register are identified through search strategies based on the scope of Cochrane Airways. We have provided details of these strategies, as well as a list of handsearched conference proceedings, in Appendix 1. See Appendix 2 for search terms used to identify studies for this review.
We searched the following trials registries.
US National Institutes of Health Ongoing Trials Register ClinicalTrials.gov (www.clinicaltrials.gov).
World Health Organization International Clinical Trials Registry Platform (apps.who.int/trialsearch).
We searched the Cochrane Airways Trials Register and additional sources from inception to the present, with no restriction on language of publication. We conducted the most recent search on 23 November 2016.
Searching other resources
We checked the reference lists of all primary studies and review articles for additional references. We searched relevant manufacturers' websites for trial information.
On 24 November 2016, we searched for errata or retractions from included studies published in full text on PubMed (www.ncbi.nlm.nih.gov/pubmed).
Data collection and analysis
Selection of studies
Two review authors (KK and RN or AM) screened titles and abstracts independently of all studies identified for potential inclusion as a result of the search, and coded them as 'retrieve' (eligible or potentially eligible/unclear) or 'do not retrieve'. We retrieved full‐text study reports/publications; two review authors (RN and KK) independently screened the full‐text reports, identified studies for inclusion and identified and recorded reasons for exclusion of ineligible studies. We resolved disagreements through discussion, or, if required, we consulted a third review author. We identified and excluded duplicates and collated multiple reports of the same study, so that each study, rather than each report, was the unit of interest in the review. We recorded the selection process in sufficient detail to complete a Preferred Reporting Items for Systematic Reviews and Meta‐Analyses (PRISMA) flow diagram and a Characteristics of excluded studies table (Moher 2009).
Data extraction and management
We piloted a data collection form on at least one study included in the review and used it to document study characteristics and outcome data. One review author (RN, KK or AM) extracted the following study characteristics from the included studies.
Methods: study design, total duration of study, details of any 'run‐in' period, number of study centres and locations, study settings, withdrawals, dates of study.
Participants: N, mean age, age range, gender, severity of condition, diagnostic criteria, baseline lung function, smoking history, inclusion criteria, exclusion criteria.
Interventions: intervention, comparison, allowed medications and concomitant interventions, excluded medications and interventions.
Outcomes: primary and secondary outcomes specified and collected, time points reported.
Notes: funding for trial, notable conflicts of interest of trial authors.
Two review authors (RN and KK or AM) independently extracted outcome data from the included studies. We noted in the Characteristics of included studies table if the included trials did not report outcome data in a useable way. We resolved disagreements by reaching consensus or by consulting a third review author. One review author (RN) transferred data into Review Manager (RevMan) (RevMan 2014). We double‐checked that the review author had entered data correctly by comparing data presented in the systematic review versus the study reports. A second review author (KK or RN) spot‐checked study characteristics for accuracy against the trial report.
Assessment of risk of bias in included studies
Two review authors (RN and KK or AM) independently assessed the risk of bias of each included study using the criteria outlined in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). We resolved disagreements by discussion or by consultation with a third review author. We assessed risk of bias according to the following domains.
Random sequence generation.
Allocation concealment.
Blinding of participants and personnel.
Blinding of outcome assessment.
Incomplete outcome data.
Selective outcome reporting.
Other bias.
We graded each potential source of bias as high, low or unclear and provided a quote from the study report and a justification for our judgement in the 'Risk of bias' table. We summarised 'Risk of bias' judgements across different studies for each of the domains listed. We considered blinding separately for different key outcomes when necessary (e.g. for unblinded outcome assessment, risk of bias for all‐cause mortality may be very different from that determined for a patient‐reported pain scale). When information on risk of bias was related to unpublished data or correspondence with a triallist, we noted this in the 'Risk of bias' table.
When we considered treatment effects, we took into account the risk of bias for studies that contributed to those outcomes.
Assessment of bias in conducting the systematic review
We conducted the review according to the published protocol and reported deviations from it in the Differences between protocol and review section of the systematic review.
Measures of treatment effect
We analysed dichotomous data using Mantel‐Haenzsel odds ratios (ORs) with a random‐effects model and 95% confidence intervals (CIs). If we had encountered outcomes with very rare events, we planned to use Peto ORs. If the included trials had reported data as rates or time‐to‐event (e.g. exacerbations), we planned to analyse these as time‐to‐event or rate ratios. We planned to transform reported rate ratios into log rate ratios and to analyse them using a random‐effects model and generic inverse variance (GIV) in RevMan (RevMan 2014). We entered data presented as a scale with a consistent direction of effect.
We analysed continuous outcomes (e.g. ACQ, AQLQ) as mean difference (MD) or standardised mean difference (SMD) values using a random‐effects model and 95% CIs. We used change from baseline scores when available.
We undertook meta‐analyses only where this was meaningful i.e. if the treatments, participants and the underlying clinical question were similar enough for pooling to make sense.
We narratively described skewed data reported as medians and interquartile ranges.
When a single trial reported multiple trial arms, we included only the relevant trial arms. If we combined two comparisons (e.g. intervention A vs usual care and intervention B vs usual care) in one meta‐analysis, we halved the control group to avoid double‐counting.
Unit of analysis issues
We analysed dichotomous data by using participants (rather than events) as the unit of analysis. However, if the included trials had reported exacerbations as rate ratios, we planned to analyse them on this basis. We meta‐analysed data from cluster RCTs only if we could adjust available data to account for clustering.
Dealing with missing data
We contacted investigators or study sponsors to verify key study characteristics and to obtain missing numerical outcome data when possible (e.g. when we identified a study as an abstract only). When this was not possible, and we thought that the missing data introduced serious bias, we took this into consideration in the Grading of Recommendations Assessment, Development and Evaluation (GRADE) rating for affected outcomes.
Assessment of heterogeneity
We used the I² statistic to measure heterogeneity amongst the trials in each analysis. If we identified substantial heterogeneity, we reported this and explored possible causes by performing prespecified subgroup analysis.
Assessment of reporting biases
When we were able to pool more than 10 trials, we created and examined a funnel plot to explore possible small study and publication biases.
Data synthesis
We used a random‐effects model and performed a sensitivity analysis with a fixed‐effect model.
Subgroup analysis and investigation of heterogeneity
We planned the following subgroup analyses.
To whom the intervention is delivered: healthcare provider versus patient/caregiver.
Duration of intervention: one‐off session versus repeated sessions.
We did not pool studies that included children with studies that included adults. If within each of these two populations we found trials that focused on a more narrow age range (e.g. children younger than five years of age), we planned to explore this potential source of heterogeneity.
We suspected that interventions would differ from one another in various ways (e.g. inhaler type, physical demonstration vs no demonstration, remote vs face‐to‐face), which may make exploration through multiple formal subgroup analyses misleading. Instead we summarised intervention characteristics in additional tables (Table 4; Table 5; Table 6).
1. Summary of characteristics of studies in comparisons 1 and 2: inhaler technique education.
| Study ID | Total n |
Study duration (weeks) |
Age | Country | Intervention | Control | Inhaler technique measure | Outcomes |
| Agertoft 1998 | 72 | 2 | Children aged 3 to 5 years | Denmark | Instructional video + individual training; delivered to participant | Instructional video | PIF | PIF, IVC, PEFR, FEV1, FVC |
| Basheti 2005 | 26 | 2 | Adults | Australia | Group B: verbal counselling Group C: verbal counselling + physical demonstration; delivered to participant |
Group A: printed materials | 9‐Step Turbuhaler checklist | Inhaler technique |
| Basheti 2008 | 31 pharmacists, 97 participants | 26 | Adults | Australia | Pharmacist‐participant education + inhaler technique labels; delivered to pharmacist | Peak flow measurement training | 9‐Step checklist | Inhaler technique, asthma severity, peak flow variability, AQOL, perceived control |
| Bynum 2001 | 49 | 4 | Adolescents aged 12 to 19 years | USA | Telepharmacy counselling; delivered to participant | Written instructions only | 8‐Step MDI checklist | Inhaler technique, participant satisfaction |
| Fernandes 2011 | 89 | 12 | Adults | Not reported | Respiratory therapist education; delivered to participant | Rotuine physician education | Not reported | Inhaler technique, asthma control |
| Mehuys 2008 | 201 | 26 | Adults | Belgium | Pharmacist education; delivered to pharmacist | Usual pharmacy care | 10‐Step MDI + spacer checklist/8‐step DPI checklist | Inhaler technique, ACT, exacerbations, ED/hospital visits, adherence, AQLQ, asthma knowledge |
| Nahafizadeh 2010 | 46 | 8.7 | Adults | Iran | Face‐to‐face education; delivered to participant | Usual care (no further details) | Not reported | ACT, FEV1 |
| Ozkaya 2010 | 130 | 12 | Children | Turkey | Face‐to‐face nurse training; delivered to participant | Inhaler package insert only | 10‐Step MDI checklist | Inhaler technique, PAQLQ, spirometry |
| Rahmati 2014 | 90 | 4 | Adults | Iran | Face‐to‐face training (no spacer device); delivered to participant | Usual care (no training) | 11‐Step MDI checklist | Inhaler technique, PEFR |
| Rydman 1999 | 68 | 8 to 20 | Adults | USA | Face‐to‐face training + demonstration; delivered to participant | Inhaler package insert only | Checklist, converted to score out of 1 (0 if any steps missed) | BAI and MDI competency |
| Self 1983 | 29 | 1 to 16 (mean 6) | Adults | USA | Face‐to‐face pharmacist training; delivered to participant | Inhaler package insert only | 10‐Step checklist | Inhaler technique, "effectiveness of instruction" |
| Turgeon 1996 | 96 | 26 | Children and adolescents (max 15 years) | Canada | Interactive nurse training with feedback; delivered to participant | Pictorial nurse training only | Checklist with scores converted to percentages | Inhaler technique, parental perceptions of treatment, asthma morbidity (e.g. no. of exacerbations, ED visits, hospitalisations, days of schools missed) |
ACT: Asthma Control Test; AQLQ: Asthma Quality of Life Questionnaire; AQOL: asthma quality of life; BAI: breath‐activated inhaler; DPI: dry powder inhaler; ED: emergency department; FEV1: forced expiratory volume in one second; FVC: forced vital capacity; IVC: inspiratory vital capacity; MDI: metered dose inhaler; PAQLQ: paediatric AQLQ; PEFR: peak expiratory flow rate; PIF: peak inspiratory flow
2. Summary of characteristics of studies in comparisons 3 and 4: multi‐media training.
| Study ID | Total n | Study duration (weeks) | Age | Country | Intervention | Control | Inhaler technique measure | Outcomes |
| Acosta 2009 | 133 | 4 | Adults | USA | Inhaler technique training video; delivered to participant | Asthma education video | Not reported | "Correct usage" of inhaler |
| Arthurs 2014 | 21 | 13 | Children | Ireland | Inhaler technique DVD; delivered to participant | Individual instruction | New inhaler technique measurement tool | Inhaler technique, self‐efficacy, knowledge acquisition |
| Boone 2002 | 36 | 4.3 | Children | UK | Inhaler technique educational computer software ("Space Inhalers"); delivered to participant | Placebo software | 15‐Step checklist | Inhaler technique, asthma knowledge |
| Carpenter 2015 | 91 | 4.3 | Children and adolescents | USA | Inhaler technique video; delivered to participant | Attention control video (about nutrition) | 8‐Step checklist | Inhaler technique, self‐efficacy, ACT |
| Goodyer 2006 | 69 | Outcomes assessed immediately | Adults | UK (Turkish‐ speaking population) |
Multi‐media touch screen training; delivered to participant | Patient information leaflet plus verbal training | Inhaler checklist | Inhaler technique |
| Lirsac 1991 | 45 | 2.1 | Adults and children (10 to 71 years) | France | Inhaler technique video OR inhaler technique video + spacer; delivered to participant | Patient information sheet | 4‐Step checklist | Inhaler technique, FEV1 |
| Savage 2003 | 110 | Outcomes assessed immediately | Children and adults (12 to 87 years) | UK | Multi‐media touch screen training; delivered to participant | Patient information leaflet | Inhaler checklist, global assessment of technique | Inhaler technique, acceptability |
| Self 1983 | 29 | 1 to 16 (mean 6) | Adults | USA | Video training; delivered to participant | Inhaler package insert only | 10‐Step checklist | Inhaler technique, "effectiveness of instruction" |
| Shah 2014 | 50 | Not reported | Not reported | USA | Computer training; delivered to participant | Written training OR no training | "Fixed rubric" used to give a score | Inhaler technique |
ACT: Asthma Control Test; DVD: digital versatile disc; FEV1: forced expiratory volume in one second
3. Summary of characteristics of studies in comparisons 5 and 6: add‐on/feedback device.
| Study ID | Total n | Study duration (weeks) | Age | Country | Intervention | Control | Inhaler technique measure | Outcomes |
| Al‐Showair 2007 | 108 | 6 | Adults | UK | Verbal training + 2Tone trainer; delivered to participant | Verbal training alone | PIF | PIF, FEV1, AQLQ |
| Ammari 2013 | 56 | 6 | Adults and children (4 to 55 years) |
UK | Verbal training + 2Tone trainer; delivered to participant | Verbal training alone | PIF | PIF, FEV1, AQLQ/PAQLQ |
| Ammari 2015 | 80 | 12 | Children | UK | AeroChamber Plus with Flo‐Vu; delivered to participant | AeroChamber Plus alone | PIF | PIF, PAQLQ, ACQ, parent spacer preference |
| Ammari 2015a | 30 | 6 to 8 | Children | Not reported | Verbal training and use of Trainhaler; delivered to participant | Verbal training alone | PIF | PIF, ACQ |
| Rahmati 2014 | 90 | 4 | Adults | Iran | Face‐to‐face training (with spacer device); delivered to participant | Usual care (no training) | 11‐Step MDI checklist | Inhaler technique, PEFR |
| Schultz 2012 | 132 | 52 | Children | Australia | Funhaler incentive device; delivered to participant | AeroChamber device | Filter used to measure salbutamol deposition | Inhaler technique, asthma control, quality of life |
| Tarsin 2008 | 76 | 4 | Not reported | Libya | Verbal training + 2Tone trainer; delivered to participant | Verbal training alone | PIF | PIF, FEV1, AQLQ, Jones Morbidity Index (JMI) |
| Toumas‐Shehata 2014 | 19 pharmacists (101 participants) | 4 | Adults | Australia | Verbal training + quantitative inhaler feedback; delivered to pharmacist | Verbal training alone | Inhaler checklist/proportion with correct technique | Inhaler technique, ACQ |
| Vitari 2013 | 43 | 4 | Not reported | USA | Face‐to‐face demonstration + In‐Check simulator; delivered to participant | Face‐to‐face demonstration | PIF, inhaler checklist | PIF, inhaler technique |
ACQ: Asthma Control Questionnaire; AQLQ: Asthma Quality of Life Questionnaire; FEV1: forced expiratory volume in one second; MDI: metered dose inhaler; PAQLQ: paediatric AQLQ; PEFR: peak expiratory flow rate; PIF: peak inspiratory flow
We used the following outcomes in subgroup analyses.
Inhaler technique.
Asthma control.
Asthma exacerbations requiring at least OCS.
We used the formal test for subgroup interactions in RevMan (RevMan 2014). When we found insufficient studies to conduct these analyses formally, we displayed in a table summary information regarding each of these variables.
Sensitivity analysis
We planned the following sensitivity analyses.
Exclusion of unpublished data.
Exclusion of studies considered at high risk of selection bias.
Exclusion of studies that did not use a validated tool to assess inhaler technique (from the inhaler technique outcome).
Summary of findings and assessment of the certainty of the evidence
We created a 'Summary of findings' table and included the following outcomes: inhaler technique; asthma control; asthma exacerbations; quality of life; adverse events; unscheduled visit to healthcare provider; and absenteeism from work or school.
We used the five GRADE considerations (study limitations, consistency of effect, imprecision, indirectness and publication bias) to assess the quality of a body of evidence as it related to studies that contributed data to the meta‐analyses for prespecified outcomes. We used methods and recommendations described in Section 8.5 and Chapter 12 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011), and we used GRADEpro Guideline Development Tool (GDT) software (GRADEpro GDT). We justified all decisions to downgrade or upgrade the quality of the evidence by using footnotes. We made comments to aid the reader's understanding of the review when necessary.
Results
Description of studies
Results of the search
We identified a total of 803 unique potentially relevant records, including 718 records from the main electronic database search and 85 additional records from the clinical trial registries ClinicalTrials.gov (n = 76) and the World Health Organization International Clinical Trial Registry Platrform (WHO ICTRP; n = 9). After removing duplicates, we reviewed 791 records and excluded 694 by looking at titles and abstracts alone. We reviewed full‐text articles for the remaining 97 records. Fifty‐seven records related to 46 studies did not meet the inclusion criteria, and we excluded them (with reasons ‐ see Figure 1). We deemed 40 records related to 29 studies eligible for this review.
1.
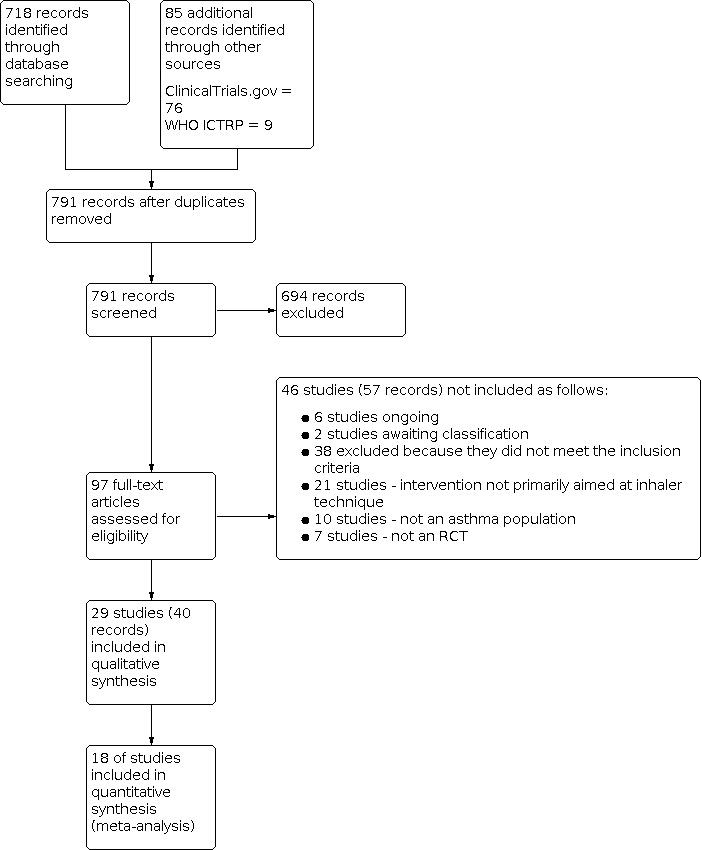
Study flow diagram.
Included studies
Twenty‐nine studies, evaluating 2210 participants (children and adults), met the inclusion criteria for this review (Self 1983; Lirsac 1991; Donateo 1996; Turgeon 1996; Agertoft 1998; Rydman 1999; Bynum 2001; Boone 2002; Savage 2003; Basheti 2005; Goodyer 2006; Al‐Showair 2007; Basheti 2008; Mehuys 2008; Tarsin 2008; Acosta 2009; Nahafizadeh 2010; Ozkaya 2010; Fernandes 2011; Schultz 2012; Ammari 2013; Vitari 2013; Arthurs 2014; Rahmati 2014; Shah 2014; Toumas‐Shehata 2014; Ammari 2015; Ammari 2015a; Carpenter 2015). Detailed descriptions of these studies and risk of bias details can be found in the Characteristics of included studies table.
All included studies were parallel RCTs. The study population in each study ranged from 21 to 201 participants, and the median number of participants was 72. Eleven of the included studies took place in Europe (six in the UK and one in each of the following countries: Belgium; Denmark; France; Ireland; and Italy), seven in USA, four in Australia, three in Asia and one in Africa, and three of the included studies did not report the country of origin. Fourteen studies were hospital based: 11 were conducted in outpatient clinics (Self 1983; Turgeon 1996; Agertoft 1998; Rydman 1999; Al‐Showair 2007; Nahafizadeh 2010; Ozkaya 2010; Schultz 2012; Ammari 2013; Rahmati 2014; Ammari 2015), one took place in a hospital ward (Arthurs 2014) and two did not provide details (Fernandes 2011; Shah 2014). Five studies were conducted in primary care facilities (Bynum 2001; Boone 2002; Savage 2003; Goodyer 2006; Carpenter 2015), four took place in community pharmacies (Basheti 2005; Basheti 2008; Mehuys 2008; Toumas‐Shehata 2014), one was carried out in a comprehensive lung centre (Vitari 2013) and five did not reveal the setting in which they were conducted (Lirsac 1991; Donateo 1996; Tarsin 2008; Acosta 2009; Ammari 2015a).
Population characteristics and inclusion criteria
Seven studies included only children (Agertoft 1998; Boone 2002; Ozkaya 2010; Schultz 2012; Arthurs 2014; Ammari 2015; Ammari 2015a) and 12 only adults (Self 1983; Donateo 1996; Rydman 1999; Goodyer 2006; Al‐Showair 2007; Basheti 2008; Mehuys 2008; Acosta 2009; Nahafizadeh 2010; Fernandes 2011; Rahmati 2014; Toumas‐Shehata 2014). Two of the children's studies also included adolescents (Turgeon 1996; Carpenter 2015), and three included adults and adolescents (Lirsac 1991; Savage 2003; Basheti 2005); these studies were classified as children's and adults' studies, respectively. One study included only adolescents aged 12 to 17 years (Bynum 2001), and one included both children and adults (Ammari 2013). Finally, three studies did not report the age range of participants (Tarsin 2008; Vitari 2013; Shah 2014); none of these three studies contributed to a meta‐analysis. The mean age of the overall population was 28.52 years. The mean ages of adult and children populations were 44.42 and 6.97 years, respectively.
All included studies required a diagnosis of asthma. Other frequently used inclusion criteria were age ranges, type of inhaler used, use of a spacer, absence of recent exacerbations, asthma control, non‐acceptable inhaler technique and specific components of the technique. Two studies did not report inclusion criteria (Nahafizadeh 2010; Shah 2014).
Interventions and comparisons
Interventions assessed in the included trials can be categorised into three broad groups:
Enhanced inhaler technique education, delivered by a trained individual to a healthcare professional (who in turn educated the patient) or directly to the patient (Table 4). Twelve studies implemented face‐to‐face verbal training with or without demonstration of appropriate inhaler technique (Self 1983; Turgeon 1996; Agertoft 1998; Rydman 1999; Bynum 2001; Basheti 2005; Basheti 2008; Mehuys 2008; Nahafizadeh 2010; Ozkaya 2010; Fernandes 2011; Rahmati 2014).
Multi‐media training (Table 5). Four studies used educational computer applications or games (Boone 2002; Savage 2003; Goodyer 2006; Shah 2014). Five studies used instructional videos with or without written information (Self 1983; Lirsac 1991; Acosta 2009; Arthurs 2014; Carpenter 2015).
Training devices providing visual or audio feedback regarding the appropriateness of breathing manoeuvres (Table 6). Patients used these devices for different periods to maintain an acceptable inhaler technique. Three of the included studies used a two‐tone trainer ‐ a training device that looks like an MDI and provides different audio feedback for acceptable versus non‐acceptable inspiratory flow rates (Al‐Showair 2007; Tarsin 2008; Ammari 2013). Trainhaler also provided audible feedback for appropriate breathing manoeuvres with an MDI (Ammari 2015a). AeroChamber Plus with Flow‐Vu (Ammari 2015), a portable hand‐held spirometer, was used to assess breathing manoeuvres associated with the use of different inhaler devices (Toumas‐Shehata 2014), and In‐Check (Vitari 2013) provided visual feedback for appropriateness of breathing manoeuvres with MDI, DPI and different types of inhalers, respectively. Finally Funhaler, a spacer device, provides combined visual and audible feedback for correct inhaler technique with an MDI inhaler (Schultz 2012).
One study used spacer devices to simplify inhalation technique by reducing the need for co‐ordination of actuation and inhalation and increasing deposition in lower airways (Donateo 1996). Another study used a spacer device to implement a complex intervention, which included educational sessions and use of a spacer versus an educational session alone or no intervention (Rahmati 2014).
Comparators used varied among included studies; some used standard inhaler technique verbal instruction; others used written instructions, sham video instructions or no instructions.
Excluded studies
Title and abstract screening of articles identified through our systematic searches revealed 97 potentially relevant records. After reviewing the full texts of these articles, we excluded 57 records describing 46 studies, as described in Figure 1. We classified six studies, described in seven records, as ongoing (ACTRN12610000159055; JPRN‐UMIN000006739; NCT02203266; NCT02283008; NCT02611531; NCT01529697) and two studies as awaiting classification because we did not find adequate details to confirm whether they met the review's inclusion criteria (NCT02062463; Westhus 1998). Finally, we excluded 38 studies (48 citations) because they did not meet the inclusion criteria. Of these, seven studies used the wrong study design for the review (WIlliams 1983; Epstein 2001; Andres Jacome 2003; Schacer 2005; Lee 2010; Sandos Dde 2010; Azouz 2015), 10 studies focused on a wrong study population for the review (McElnay 1989; Verver 1996; Compton 2000; Hesselink 2004; Basheti 2005a; Bosnic‐Anticevich 2010; Jolly 2012; NCT01456494; Jolly 2015; NCT01426581) and 21 studies did not assess the intervention of interest for this review (NCT01641211; NCT02046759; NCT02307669; NCT02363192; NCT02715219; Eriksson 1980; Hodges 1981; Pedersen 1983; Rachelefsky 1986; Reiser 1986; Yoon 1993; Wong 1995; Mulloy 1996; Tuazon 2002; Kritikos 2007; Horner 2008; Garcia‐Cardenas 2013; Fornell 2014; Eakin 2015; Grover 2016; Poureslami 2016).
Risk of bias in included studies
We have presented in Figure 2 an overview of risk of bias in the included studies. We have also provided a summary of possible bias related to each domain. We have given details on the rationale for each judgement of each study's risk in the risk of bias table for each study (see the Characteristics of included studies tables).
2.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Allocation
Most included studies provided very limited information regarding the two selection bias domains. We deemed 12 of the included studies to be at low risk of bias for random sequence generation (Lirsac 1991; Turgeon 1996; Bynum 2001; Savage 2003; Goodyer 2006; Basheti 2008; Mehuys 2008; Schultz 2012; Ammari 2013; Rahmati 2014; Ammari 2015; Carpenter 2015) and only three to be at low risk for allocation concealment (Lirsac 1991; Mehuys 2008; Carpenter 2015). We deemed one study to be at high risk for allocation concealment bias (Shah 2014), and we rated risk of bias of remaining studies in each selection bias domain as unclear.
Blinding
Blinding of participants and personnel to group allocation is challenging because of the nature of the interventions and comparisons; this posed the most significant risk of bias for the evidence in this review. Only one trial reported blinding of participants and personnel (Boone 2002), and we assessed this study as low risk. We judged another trial involving young children, which used a relatively objective measure (lung function), to be at low risk despite lack of blinding (Agertoft 1998). One trial did not report on blinding of participants and personnel; as a result, we rated risk of performance bias for this study as unclear (Fernandes 2011). We deemed all remaining studies as having high risk of performance bias because they were not blinded.
We deemed risk of detection bias to be low in only seven trials (Donateo 1996; Turgeon 1996; Agertoft 1998; Rydman 1999; Savage 2003; Goodyer 2006; Acosta 2009). In the remaining trials, risk of detection bias was high, with the exception of three trials, which we deemed to have unclear risk (Self 1983; Vitari 2013; Shah 2014).
Incomplete outcome data
Sixteen of the included studies had low and balanced attrition across study arms; we deemed these studies to have low risk of bias for incomplete outcome data (Self 1983; Lirsac 1991; Donateo 1996; Agertoft 1998; Rydman 1999; Savage 2003; Basheti 2005; Goodyer 2006; Al‐Showair 2007; Nahafizadeh 2010; Ammari 2013; Vitari 2013; Rahmati 2014; Toumas‐Shehata 2014; Ammari 2015; Carpenter 2015). We rated risk of attrition bias as high in five of the included trials with high or unequal drop‐out (Turgeon 1996; Bynum 2001; Basheti 2008; Mehuys 2008; Schultz 2012) and as unclear in the remaining studies.
Selective reporting
We rated only one study as having low risk of reporting bias (Carpenter 2015) and found 11 of the remaining trials to be at high risk of reporting bias (Lirsac 1991; Turgeon 1996; Basheti 2005; Tarsin 2008; Acosta 2009; Ozkaya 2010; Fernandes 2011; Vitari 2013; Arthurs 2014; Shah 2014; Ammari 2015a). Finally, we were not able to assign a clear risk of bias to the remaining trials, usually because we could not identify a prospective trial registration or a prepublished protocol.
Other potential sources of bias
We did not identify any other potential sources of bias in the included studies.
Effects of interventions
See: Table 1; Table 2; Table 3
Summary of findings 1. Enhanced education compared with control versus usual care for people with asthma.
| Enhanced education compared with control/usual care for people with asthma | |||||||
| Patient or population: adults and children with asthma Setting: primary and secondary care Intervention: enhanced education Comparison: control/usual care | |||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | Number of participants (studies) | Quality of the evidence (GRADE) | Comments | ||
| Risk with control/usual care | Risk with enhanced education | ||||||
|
Correct inhaler technique Follow‐up: 2 to 26 weeks (adults) 12 to 26 weeks (children) |
Adults | 31 per 100 | 69 per 100 (45 to 86) | OR 5.00 (1.83 to 13.65) | 258 (3 RCTs) | ⊕⊕⊕⊝ MODERATEa |
Additional results from technique rating scales could not be combined (Analysis 1.2) |
| Children | 49 per 100 | 55 per 1,00 (40 to 69) | OR 1.29 (0.70 to 2.36) | 175 (2 RCTs) | ⊕⊕⊝⊝ LOWa,b |
One study measured PIF as a marker for inhaler technique and showed benefit (Analysis 2.2; Analysis 2.3) | |
|
Asthma control score 4 to 26 weeks |
Adults | ‐ | Score in the intervention group was 0.48 SDs higher than in the control group (0.29 lower to 1.24 higher) | ‐ | 247 (2 RCTs) | ⊕⊝⊝⊝ VERY LOWa,b,c |
We were not able to calculate a control risk, as the outcome was measured on different scales |
|
Asthma control responders 8 to 12 weeks |
Adults | 42 per 100 | 70 per 100 (52 to 84) | OR 3.18 (1.47 to 6.88) | 134 (2 RCTs) | ⊕⊕⊝⊝ LOWd |
|
|
Exacerbations requiring at least OCS 26 weeks |
Adults | 10 per 100 |
13 per 100 (5 to 28) |
OR 1.32 (0.49 to 3.55) |
158 (1 RCT) |
⊕⊕⊝⊝ LOWa,b |
The same study also reported exacerbations requiring ED/hospitalisation. Events were rare and results imprecise |
|
Quality of life 26 weeks |
Adults | ‐ | Score in the intervention group was 0.52 SDs higher than in the control group (0.04 lower to 1.09 higher) | ‐ | 247 (2 RCTs) | ⊕⊕⊝⊝ LOWa,c,e |
We were not able to calculate a control risk as the outcome was measured on different scales |
| Other outcomes | No results could be analysed for adverse events, unscheduled visits to a healthcare provider or school/work absences | ||||||
| *The risk in the intervention group (and its 95% confidence interval) is based on assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI) CI: confidence interval; ED: emergency department; OCS: oral corticosteroids; OR: odds ratio; PIF: peak inspiratory flow; RCT: randomised controlled trial; RR: risk ratio; SDs: standard deviations | |||||||
| GRADE Working Group grades of evidence High quality: We are very confident that the true effect lies close to the estimate of effect Moderate quality: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of effect but may be substantially different Low quality: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of effect Very low quality: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect | |||||||
aStudies contributing to this outcome were at high risk of bias in several domains (including performance and detection bias). Downgraded once
bWide confidence intervals including possible harm and benefit of intervention. Downgraded once
cHigh level of statistical inconsistency detected. Downgraded once
dThe two small studies contributing to this outcome were identified as abstracts only; it is therefore difficult to assess methodological quality. Studies were considered at high or unclear risk of bias in multiple domains (including selection, performance, detection and reporting biases). Downgraded twice
eConfidence interval includes no difference with random‐effects model, driven by statistical heterogeneity. Fixed‐effect sensitivity analysis yields more precise result. Not downgraded
Summary of findings 2. Multimedia training compared with control versus usual care for people with asthma.
| Multimedia training compared with control/usual care for people with asthma | |||||||
| Patient or population: adults and children with asthma Setting: primary and secondary care Intervention: multi‐media training Comparison: control/usual care | |||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | Number of participants (studies) | Quality of the evidence (GRADE) | Comments | ||
| Risk with control/usual care | Risk with multi‐media training | ||||||
|
Correct inhaler technique Immediately after intervention |
Adults | 30 per 100 | 47 per 100 (26 to 70) | OR 2.15 (0.84 to 5.50) | 164 (2 RCTs) | ⊕⊕⊕⊝ MODERATEa,b |
|
|
Correct inhaler technique 2‐Week follow‐up |
Adults | 43 per 100 | 57 per 100 (23 to 86) | OR 1.78 (0.40 to 7.94) | 28 (1 RCT) | ⊕⊕⊝⊝ LOWa,c |
|
| Inhaler technique score | Adults | Not pooled; narrative summary of evidence provided in data table (Analysis 3.3) | ‐ | 136 (2 RCTs) |
Not graded | Suggests benefit of multi‐media training over control | |
| Children | Not pooled; narrative summary of evidence provided in data table (Analysis 4.1) | ‐ | 127 (2 RCTs) |
Not graded | Suggests benefit of multi‐media training over control | ||
|
Asthma control (ACT) 4 weeks |
Children | Mean change in control group was 1.2 | Mean change was 0.73 better (‐0.99 worse to 2.45 better) |
‐ | 91 (1 RCT) |
⊕⊕⊝⊝ LOWa,c |
|
| Other outcomes | No results could be analysed for quality of life, exacerbations, adverse events, unscheduled visits to a healthcare provider or school/work absences | ||||||
| *The risk in the intervention group (and its 95% confidence interval) is based on assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI) ACT: Asthma Control Test (range 0 to 25; higher is better); CI: confidence interval; OR: odds ratio; RCT: randomised controlled trial; RR: risk ratio; SDs: standard deviations | |||||||
| GRADE Working Group grades of evidence High quality: We are very confident that the true effect lies close to the estimate of effect Moderate quality: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of effect but may be substantially different Low quality: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of effect Very low quality: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect | |||||||
aConfidence intervals include no difference. Downgraded once
bAlthough participants in both studies were unblinded, inhaler technique was rated by a blinded assessor, and both groups received an intervention. Not downgraded
cHigh risk of bias for performance and detection. Downgraded once
Summary of findings 3. Feedback device compared with control versus usual care for people with asthma.
| Feedback device compared with control/usual care for people with asthma | |||||||
| Patient or population: adults and children with asthma Setting: primary and secondary care Intervention: feedback device Comparison: control/usual care | |||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | Number of participants (studies) | Quality of the evidence (GRADE) | Comments | ||
| Risk with control/usual care | Risk with feedback device | ||||||
|
Correct inhaler technique 4‐Week follow‐up |
Adults | 51 per 100 |
83 per 100 (66 to 93) |
OR 4.80 (1.87 to 12.33) | 97 (1 RCT) |
⊕⊕⊝⊝ LOWa,b |
Additional results from technique rating scales could not be combined (Analysis 5.3) |
|
Inhaler technique (PIF) Follow‐up: 6 weeks (adults) 6 to 12 weeks (children) |
Adults | 66 per 100 | 97 per 100 (81 to 100) | OR 18.26 (2.22 to 150.13) | 71 (1 RCT) | ⊕⊕⊝⊝ LOWa,b |
|
| Children | Mean PIF was 51.2 litres/min | Mean PIF was 9.22 litres/min better (33.71 better to 15.27 worse) | ‐ | 98 (2 RCTs) | ⊕⊕⊝⊝ LOWa,c |
||
|
Asthma control (ACQ) 6 to 12 weeks |
Adults | Mean ACQ score was 1.4 | Mean score in the intervention group was 0.1 better (0.46 better to 0.26 worse) |
‐ | 97 (1 RCT) |
⊕⊕⊝⊝ LOWa,c |
|
| Children | Mean ACQ score was 0.7 | Mean score in the intervention group was 0.02 worse (0.35 worse to 0.32 better) | ‐ | 98 (2 RCTs) | ⊕⊕⊕⊝ MODERATEa |
||
|
Quality of life Follow‐up: 6 weeks (adults) 6 to 12 weeks (children) |
Adults | Mean score on the mini‐AQLQ was 4.2 | Mean score in the intervention group was 0.38 better (0.01 worse to 0.77 better) | ‐ | 100 (2 RCTs) | ⊕⊕⊝⊝ LOWa,d |
|
| Children | Mean change in quality of life was 0.07 | Mean change was 0.25 better (0.07 worse to 0.58 better) | ‐ | 91 (2 RCTs) | ⊕⊕⊝⊝ LOWa,d |
One study reported endpoint quality of life (Analysis 6.4) | |
|
Quality of life (responders) 6 weeks |
Adults | 49 per 100 | 83 per 100 (62 to 94) | OR 5.29 (1.76 to 15.89) | 71 (1 RCT) | ⊕⊕⊕⊝ MODERATEa |
|
| Other outcomes | No results could be analysed for exacerbations, adverse events, unscheduled visits to a healthcare provider or school/work absences | ||||||
| *The risk in the intervention group (and its 95% confidence interval) is based on assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI) ACQ: Asthma Control Questionnaire (range 0 to 6; lower is better); CI: confidence interval; OR: odds ratio; PIF: peak inspiratory flow; RCT: randomised controlled trial; RR: risk ratio; SDs: standard deviations | |||||||
| GRADE Working Group grades of evidence High quality: We are very confident that the true effect lies close to the estimate of effect Moderate quality: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of effect but may be substantially different Low quality: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of effect Very low quality: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect | |||||||
aHigh risk of performance and detection bias. Downgraded once
bVery wide confidence intervals based on one study. Downgraded once
cConfidence intervals include possible harm and benefit of the intervention. Downgraded once
dConfidence interval does not exclude no difference, and upper limit exceeds the MCID of 0.5 units. Downgraded once
Structure of the analysis
After examining the data, we found that included studies fell into three main comparisons. As planned, we analysed studies that recruited children (mean age < 12 years) separately from those that recruited adolescents and adults (mean age ≥ 12 years), resulting in six main comparisons.
Comparisons 1 (adults) and 2 (children):enhanced inhaler technique education versus control or usual care. Investigators delivered education directly to the participant or to a healthcare professional (e.g. a pharmacist) and the intervention could be a 'one‐off' intervention or could be repeated one or more times. We explored these differences within comparisons in our prespecified subgroup analyses.
Comparisons 3 (adults) and 4 (children):multi‐media training versus control or usual care. This included videos and computer programmes, which, in the case of our included studies, investigators always delivered directly to the participant. Some studies used a one‐off delivery of the intervention, and in others, participants had ongoing access to the resource. We planned to explore this in our prespecified subgroup analysis, but for all studies in adults, this was a one‐off intervention, and for all studies in children, participants had ongoing access at home.
Comparisons 5 (adults) and 6 (children):feedback device versus control or usual care. Investigators provided devices that gave audio or visual (or both) feedback to the participant on inhaler technique. All but one of the studies that we included in this comparison allowed participants to use the device at home between study visits; thus this prespecified subgroup analysis was not possible.
In the following section, we present results separately for each comparison, with any relevant subgroup or sensitivity analyses described at the end of each comparison section.
Comparisons 1 and 2: enhanced inhaler technique education versus control or usual care
Nine studies in adults (Self 1983; Rydman 1999; Bynum 2001; Basheti 2005; Basheti 2008; Mehuys 2008; Nahafizadeh 2010; Fernandes 2011; Rahmati 2014) and three studies in children (Turgeon 1996; Agertoft 1998; Ozkaya 2010) contributed to this comparison.
Inhaler technique
Contributing studies measured this in several ways and at different time points. Investigators most commonly used a checklist, which resulted in a score reflecting the number of steps performed correctly, but these results were too varied to pool. Another method was to dichotomise participants into those with and those without 'satisfactory' or 'correct' inhaler technique at follow‐up. Study authors usually defined satisfactory or correct as performing all critical steps correctly.
Among adults, more people in the intervention group than in the control group had correct technique at follow‐up, with moderate to substantial heterogeneity (Analysis 1.1; OR 5.00, 95% CI 1.83 to 13.65; 258 participants; three studies; I² = 57%; moderate‐quality evidence). This equates to 31 out of 100 people having correct technique at 2‐ to 26‐week follow‐up in the control group compared with 69 out of 100 (95% CI 45 to 86) in the active intervention group (Figure 3).
1.1. Analysis.

Comparison 1: Adults: enhanced education versus control/usual care, Outcome 1: Correct inhaler technique (at follow‐up)
3.
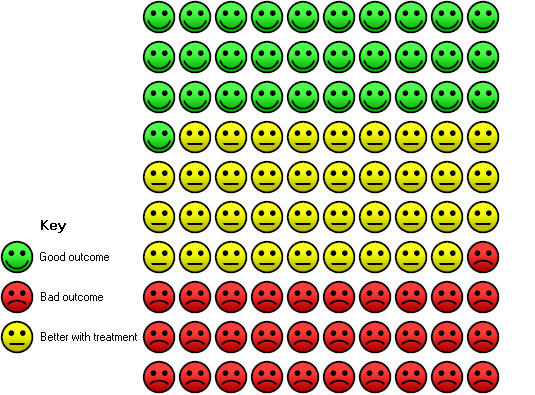
In the control group, 31 out of 100 people had correct inhaler technique after 2 to 26 weeks, compared with 69 (95% CI 45 to 86) out of 100 in the active treatment group.
We considered combining checklist scales using standardised mean difference, but statistical heterogeneity was extremely high and data from individual trials were often heavily skewed. Instead, we have presented effect estimates from the individual studies in data tables. Among adults, when investigators measured performance immediately after delivery of the intervention by using a checklist, they found that inhaler technique education improved inhaler technique over control in most studies (Analysis 1.2). However, these studies have widely different effect estimates and varied precision and provided a similar picture at follow‐up of 2 to 26 weeks (also shown in Analysis 1.2).
1.2. Analysis.
Comparison 1: Adults: enhanced education versus control/usual care, Outcome 2: Inhaler technique score
| Inhaler technique score | |||||
| Study | Time of rating | Intervention mean (SD) | Control mean (SD) | Total N |
Scale (higher score= better technique) |
| Basheti 2008 | Post‐intervention | ‐ | ‐ | ‐ | ‐ |
| Follow‐up (26 wks) | 2.80 (1.60) | 0.90 (1.40) | 100 | Max 9 (change) | |
| Bynum 2001 | Post‐intervention | 7.33 (0.72) | 5.14 (1.62) | 36 | Max 8 |
| Follow‐up (2 to 4 wks) | 6.73 (1.22) | 4.86 (1.10) | 36 | Max 8 | |
| Mehuys 2008 | Post‐intervention | ‐ | ‐ | ‐ | ‐ |
| Follow‐up (26 wks) | 93.2 (10.7) | 83.7 (22.5) | 150 | Max 100 | |
| Rahmati 2014 | Post‐intervention | 10.8 (0.48) | 5.57 (1.20) | 120 | Max 11 |
| Follow‐up (4 wks) | 10.17 (0.91) | 5.48 (1.27) | 90 | Max 11 | |
| Rydman 1999 | Post‐intervention | 0.68 (0.46) | 0.60 (0.49) | 120 | Max 1 |
| Follow‐up (8 to 20 wks) | 0.72 (0.45) | 0.75 (0.43) | 120 | Max 1 | |
| Self 1983 | Post‐intervention | 16.8 (4.1) | 10.7 (5.4) | 19 | Max 20 |
| Follow‐up | ‐ | ‐ | ‐ | ‐ | |
Among children, two studies dichotomised participants to those with and without correct technique at follow‐up (between 12 and 26 weeks) and found no significant differences between groups, with confidence intervals including both potential harm and benefit of the intervention (Analysis 2.1; OR 1.29, 95% CI 0.70 to 2.36; 175 participants; two studies; I² = 0%; low‐quality evidence). One small study measured peak inspiratory flow rate immediately after the intervention to assess inhaler technique. It should be noted that participants in this study were young children (three to five years of age) who were being trained in Turbuhaler use, which requires a rapid, forceful inhalation; thus the applicability of this finding to other populations may be limited. Results showed benefit in favour of the educational intervention (Analysis 2.2; MD 10.00, 95% CI 2.16 to 17.84). The same study measured this again at two‐week follow‐up and reported that benefit was maintained (Analysis 2.3; MD 7.60, 95% CI 1.43 to 13.77).
2.1. Analysis.

Comparison 2: Children: enhanced education versus control/usual care, Outcome 1: Correct inhaler technique (at follow‐up)
2.2. Analysis.

Comparison 2: Children: enhanced education versus control/usual care, Outcome 2: Inhaler technique (PIF immediately after intervention)
2.3. Analysis.

Comparison 2: Children: enhanced education versus control/usual care, Outcome 3: Inhaler technique (PIF at follow‐up)
Asthma control
Among adults, researchers measured asthma control using the ACT ‐ "perceived asthma control" ‐ on a 0 to 55 scale and dichotomised results into complete control versus incomplete control on the ACT. None of the included studies of children in this comparison reported asthma control.
We combined ACT and perceived asthma control scores, both measured at 26 weeks, using SMD. Analysis revealed benefit in favour of the educational intervention but with a lower confidence interval, including no difference and high statistical heterogeneity (Analysis 1.3; SMD 0.48, 95% CI ‐0.29 to 1.24; 247 participants; two studies; I² = 88%; very low‐quality evidence). Two small studies reported "complete control" and meta‐analysis favoured the educational intervention (Analysis 1.4; OR 3.18, 95% CI 1.47 to 6.88; 134 participants; two studies; I² = 0%; low‐quality evidence).
1.3. Analysis.

Comparison 1: Adults: enhanced education versus control/usual care, Outcome 3: Asthma control
1.4. Analysis.

Comparison 1: Adults: enhanced education versus control/usual care, Outcome 4: Asthma control
Exacerbations
Only one study in adults reported asthma exacerbations at 26 weeks (Mehuys 2008). A similar number of participants in each group experienced an exacerbation requiring at least OCS treatment (10 vs 8), and although more participants in the control group experienced an exacerbation requiring an ED visit or hospital admission (1 vs 5), events were too infrequent to allow investigators to draw a conclusion. We considered the evidence of low quality.
Quality of life
Again, for this comparison, only studies involving adults reported quality of life, and both reported this outcome at 26 weeks. One study used asthma‐related quality of life (AQOL) and the other used the AQLQ. We combined both scales using SMD; although results favoured the educational intervention, the lower confidence interval included no difference and heterogeneity was substantial (Analysis 1.7; SMD 0.52, 95% CI ‐0.04 to 1.09; 247 participants; two studies; I2 = 78%; low‐quality evidence).
1.7. Analysis.

Comparison 1: Adults: enhanced education versus control/usual care, Outcome 7: Quality of life
Adverse events
One study involving 97 adults (Basheti 2008) reported that no "clinically important adverse events" occurred during the 26‐week follow‐up.
Investigators reported the following outcomes in a way that did not allow meta‐analysis by any of the studies in this comparison: unscheduled visits to healthcare provider; and absenteeism from work or school.
Subgroup analyses
To whom the intervention was delivered: patient versus healthcare professional
We were unable to perform this subgroup analysis for inhaler technique score, as we chose not to perform a meta‐analysis owing to substantial heterogeneity.
We were able to perform a formal test of subgroup differences for dichotomised inhaler technique and asthma control in adults (Analysis 1.8; Analysis 1.9); for both analyses, the subgroup analysis suggests that it may be more effective to deliver the educational intervention to pharmacists rather than directly to patients. However, very few studies contributed to these analyses, and baseline ACT and AQLQ in Mehuys 2008 (a study in which the intervention was delivered to participants) was high, perhaps limiting the scope for improved control among these participants. Therefore, our confidence in this finding is low.
1.8. Analysis.

Comparison 1: Adults: enhanced education versus control/usual care, Outcome 8: Subgroup analysis: inhaler technique (at follow‐up): to whom intervention is delivered
1.9. Analysis.

Comparison 1: Adults: enhanced education versus control/usual care, Outcome 9: Subgroup analysis: asthma control: to whom intervention is delivered
One‐off versus repeated intervention sessions
As above, we could not perform subgroup analysis for inhaler technique score, as we chose not to combine results, and the only studies reporting asthma control delivered repeated sessions. For dichotomised inhaler technique, the formal test for subgroup differences in both adults and children (Analysis 1.10; Analysis 2.4) did not suggest any impact of repeated versus one‐off sessions of education, but as above, very few studies contributed to these analyses.
1.10. Analysis.

Comparison 1: Adults: enhanced education versus control/usual care, Outcome 10: Subgroup analysis: inhaler technique (at follow‐up): off‐off vs repeated sessions
2.4. Analysis.

Comparison 2: Children: enhanced education versus control/usual care, Outcome 4: Subgroup analysis: inhaler technique (at follow‐up): one‐off vs repeated sessions
Comparisons 3 and 4: multi‐media training versus control or usual care
Five studies in adults (Self 1983; Lirsac 1991; Savage 2003; Goodyer 2006; Acosta 2009) and two studies in children (Boone 2002; Carpenter 2015) contributed to this comparison.
Inhaler technique
Again, investigators usually measured inhaler technique by using a checklist, immediately after the intervention or at follow‐up.
Two further linked studies in separate populations reported "global improvement in technique" dichotomously immediately after the intervention and found benefit in favour of the multi‐media intervention when compared with a patient information leaflet and a verbal explanation, but the lower confidence interval of the effect estimate does not rule out benefit for the control group (Analysis 3.1; OR 2.15, 95% CI 0.84 to 5.50; 164 participants; two studies; I² = 49%; moderate‐quality evidence).
3.1. Analysis.

Comparison 3: Adults: multi‐media training versus control/usual care, Outcome 1: Correct inhaler technique (immediately after intervention)
One study reporting number with correct use after 15 days found no significant differences between groups, although this study included too small a sample to permit firm conclusions (Analysis 3.2; OR 1.78, 95% CI 0.40 to 7.94; low‐quality evidence).
3.2. Analysis.

Comparison 3: Adults: multi‐media training versus control/usual care, Outcome 2: Correct inhaler technique (at follow‐up)
Two studies in adults reported the mean between‐group difference immediately after the intervention or after follow‐up (or both) as "percent correct use" or as a score out of 20. We decided not to combine these results. Both studies demonstrated benefit of multi‐media training versus usual care (Analysis 3.3).
3.3. Analysis.
Comparison 3: Adults: multi‐media training versus control/usual care, Outcome 3: Inhaler technique score
| Inhaler technique score | ||||
| Study | Time of rating | MD (SE) | Total N |
Scale (higher score= better technique) |
| Acosta 2009 | Post‐intervention | 14.77 (2.23) | 116 | % correct use |
| Follow‐up (4 wks) | 13.30 (2.33) | 116 | % correct use | |
| Self 1983 | Post‐intervention | 6.2 (2.33) | 20 | Max 20 |
| Follow‐up (4 wks) | Control not followed‐up | ‐ | Max 20 | |
Two studies in children also reported change from baseline inhaler technique at one‐month follow‐up by using a checklist. We present these effect estimates in a data table and did not include them in a meta‐analysis (Analysis 4.1). Both studies show benefit of multi‐media training.
4.1. Analysis.
Comparison 4: Children: multi‐media training versus control/usual care, Outcome 1: Change in inhaler technique score
| Change in inhaler technique score | |||||
| Study | Time of rating | Intervention mean (SD) | Control mean (SD) | Total N |
Scale (higher score= better technique) |
| Boone 2002 | Post‐intervention | ‐ | ‐ | ‐ | ‐ |
| Follow‐up (4 wks) | 2.60 (0.60) | 0.50 (0.50) | 36 | Max 15 | |
| Carpenter 2015 | Post‐intervention | 1.12 (1.09) | 0.03 (1.07) | 91 | Max 8 |
| Follow‐up (4 wks) | 0.87 (1.09) | 0.32 (1.14) | 91 | Max 8 | |
Asthma control
Only one study in children reported asthma control using the ACT, both as an endpoint score and as change from baseline (Analysis 4.2; Analysis 4.3), and found no significant between‐group differences, with confidence intervals excluding the established minimal clinically important difference (MCID) of 3 (low‐quality evidence).
4.2. Analysis.

Comparison 4: Children: multi‐media training versus control/usual care, Outcome 2: Asthma control (change from baseline)
4.3. Analysis.

Comparison 4: Children: multi‐media training versus control/usual care, Outcome 3: Asthma control (endpoint)
No studies in this comparison reported the following outcomes in a way that allowed meta‐analysis: exacerbations; quality of life; adverse events; unscheduled visits to a health care provider; and absenteeism from work or school.
Subgroup analysis
We were unable to perform either of our prespecified subgroup analyses for this comparison.
Comparisons 5 and 6: feedback device versus control or usual care
Three studies in adults (Al‐Showair 2007; Ammari 2013; Toumas‐Shehata 2014) and four studies in children (Schultz 2012; Ammari 2013; Ammari 2015; Ammari 2015a) contributed to at least one meta‐analysis (Ammari 2013 recruited both adults and children and presented disaggregated results for quality of life).
Inhaler technique
Study authors assessed inhaler technique in both adults and children using peak inspiratory flow (PIF) rate. DPIs require fast, deep inhalation (high PIF rate), and MDIs require a slower, deep inhalation (low PIF rate).
One small study in adults measured this dichotomously at six weeks with participants classified as achieving or not achieving the optimal rate of < 90 L/min. Results showed benefit in favour of the feedback device, but the effect was very imprecise (Analysis 5.1; OR 18.26, 95% CI 2.22 to 150.13; 71 participants; one study; low‐quality evidence). Another study, in which pharmacists in the intervention group used an inhaler device to give quantitative feedback on inhaler technique to participants, dichotomised participants into those with correct technique and those without incorrect technique at four weeks. Use of an inhaler feedback device in addition to verbal training increased the odds of achieving the correct technique (Analysis 5.2: OR 4.80, 95% CI 1.87 to 12.33; 97 participants; one study; low‐quality evidence). This equates to 51 out of 100 people having correct technique at four‐week follow‐up in the control group compared with 83 out of 100 (95% CI 66 to 93) in the active intervention group.
5.1. Analysis.

Comparison 5: Adults: feedback device versus control/usual care, Outcome 1: Inhaler technique (PIF)
5.2. Analysis.

Comparison 5: Adults: feedback device versus control/usual care, Outcome 2: Correct inhaler technique (at follow‐up)
Two small studies in children assessed PIF rate as a continuous variable (L/min) at follow‐up between 6 and 12 weeks. As these studies were assessing MDI technique, slower inhalation (lower PIF rate) was preferred. Combined results do not show clear benefit of the intervention, although the confidence intervals do not rule out benefit or harm (Analysis 6.1; MD ‐9.22, 95% CI ‐33.71 to 15.27; 98 participants; two studies; I² = 42%; low‐quality evidence).
6.1. Analysis.

Comparison 6: Children: feedback device versus control/usual care, Outcome 1: Inhaler technique (PIF)
Asthma control
One study measured asthma control using the ACQ at four weeks and found no differences between groups and confidence intervals, excluding the MCID of 0.5 (Analysis 5.4: MD ‐0.10, 95% CI ‐0.46 to 0.26; 97 participants; one study; low‐quality evidence).
5.4. Analysis.

Comparison 5: Adults: feedback device versus control/usual care, Outcome 4: Asthma control
Two studies in children measured this using the ACQ at between 6 and 12 weeks. Investigators noted no between‐group differences, with confidence intervals again excluding the MCID of 0.5 (Analysis 6.2; MD ‐0.02, 95% CI ‐0.35 to 0.32; 98 participants; two studies; I² = 0%; moderate‐quality evidence).
6.2. Analysis.

Comparison 6: Children: feedback device versus control/usual care, Outcome 2: Asthma control
Quality of life
Two studies in adults reported quality of life; both used the mini‐AQLQ and measured this outcome at six weeks. Pooled analysis suggests benefit of device feedback over usual care. However, the mean difference falls below the MCID of 0.5, and the lower confidence interval includes no difference (Analysis 5.5; MD 0.38, 95% CI ‐0.01 to 0.77; 100 participants; two studies; I² = 0%; low‐quality evidence). One of the two studies also reported the mini‐AQLQ as a "responder analysis" (i.e. those experiencing at least a 0.5 point improvement), which shows clear, although imprecise, benefit of the intervention (Analysis 5.6; OR 5.29, 95% CI 1.76 to 15.89; 71 participants; one study; moderate‐quality evidence). This equates to 49 out of 100 people having a greater than 0.5 point improvement at six‐week follow up in the control group compared with 83 out of 100 (95% CI 42 to 94) in the active intervention group (Figure 4).
5.5. Analysis.

Comparison 5: Adults: feedback device versus control/usual care, Outcome 5: Quality of life
5.6. Analysis.

Comparison 5: Adults: feedback device versus control/usual care, Outcome 6: Quality of life (responders)
4.

In the control group, 49 out of 100 people had at least 0.5 unit increase in AQLQ after 6 weeks, compared with 83 (95% CI 42 to 94) out of 100 in the active treatment group.
Among children, three studies reported quality of life ‐ two using the paediatric AQLQ (PAQLQ) and one using the PedsQL Asthma Module. We pooled the two studies reporting PAQLQ as a change from baseline; results show benefit in favour of the feedback device, but the lower confidence interval includes no difference (of note, in one of the studies, reported quality of life deteriorated in both groups, just less so in the feedback device group) (Analysis 6.3; MD 0.25, 95% CI ‐0.07 to 0.58; 91 participants; two studies; I² = 20%; low‐quality evidence). Schultz 2012 reported quality of life on the PedsQL (Asthma Module) at three months and did not detect any significant between‐group differences (Analysis 6.4; MD 41.00, 95% CI ‐76.49 to 158.49; 109 participants; one study), but the result was imprecise.
6.3. Analysis.

Comparison 6: Children: feedback device versus control/usual care, Outcome 3: Quality of life (change from baseline)
6.4. Analysis.

Comparison 6: Children: feedback device versus control/usual care, Outcome 4: Quality of life (endpoint)
Researchers did not report the following outcomes in a way that allowed meta‐analysis in this comparison: exacerbations; adverse events; unscheduled visits to a healthcare provider; and absenteeism from work or school.
Subgroup analysis
We were unable to perform either of our prespecified subgroup analyses for this comparison.
Sensitivity analyses
We did not perform prespecified sensitivity analyses for the following reasons.
We did not obtain any unpublished data.
The only trial deemed at high risk of selection bias (Shah 2014) did not contribute data to any meta‐analysis.
Almost all trials that contributed data on inhaler technique used a standard or validated checklist to assess inhaler technique, or they used an objective measure such as PIF rate. For only one contributing study (Acosta 2009), we could not determine how inhaler technique had been assessed. This information was provided as a conference abstract that reported percentage "correct usage" of inhaler; it is not clear whether this refers to the number of individuals who used the device correctly, or to the mean percentage of correct steps followed by each participant. However, as we decided not to pool checklist scores owing to extremely high statistical heterogeneity and heavily skewed data, we determined that the planned sensitivity analysis was not necessary.
Discussion
Summary of main results
This review includes 29 parallel randomised controlled trials (RCTs; n = 2210), although not all trials reported relevant or useable data. All participants had asthma, and some studies specified use of a particular inhaler or spacer, or required a particular level of asthma control. Follow‐up of analysed studies ranged from 2 to 26 weeks. Studies used a variety of scales and did not always use validated scales. Almost all included studies reported some measure of inhaler technique on a range of different checklists. Most studies were at low or unclear risk of selection and attrition biases and at high risk of biases associated with blinding. We considered most of the evidence to be of low quality owing to these biases and to imprecision in the estimates of effect.
Most studies were classified into three comparisons: those assessing an enhanced face‐to‐face training session(s), those using multi‐media to deliver inhaler training (e.g. a video, computer app or game) and those testing devices that give people visual or audio feedback about technique. Despite the large number of included studies, these differences between interventions, as well as differences in age groups and outcome measures, meant that meta‐analyses often could not be performed. This was particularly true for exacerbations, adverse events, unscheduled visits to a healthcare provider and absenteeism from work or school.
Enhanced inhaler technique education and multi‐media training led to improved technique in most studies immediately after the intervention and at follow‐up, although the variety of checklists used meant that this was difficult to assess reliably. For both adults and children, how and when inhaler technique was assessed appeared to affect whether inhaler technique improved and by how much. Analyses of the numbers of people who demonstrated correct or 'good enough' technique were generally more useful; adult studies of enhanced education showed benefit with this metric (odds ratio (OR) 5.00, 95% confidence interval (CI) 1.83 to 13.65; 258 participants; three studies), as did analyses looking at feedback devices (OR 4.80, 95% CI 1.87 to 12.33; 97 participants; one study), but the benefit of multi‐media training for adults was uncertain (OR 2.15, 95% CI 0.84 to 5.50; 164 participants; two studies; I² = 49%). Evidence tended to be less clear for children, usually because results were based on fewer and smaller studies.
Studies found some benefit for quality of life and asthma control, but results generally did not indicate consistent or important benefits of inhaler technique interventions for adults or children. Confidence intervals included no difference or fell under a range that could be considered clinically important. Responder analyses sometimes showed that more people in the intervention groups saw improvement, even though the mean difference between groups was small.
Overall completeness and applicability of evidence
Most of the studies included in this review showed that an intervention to improve inhaler technique improved technique when assessed by a checklist or dichotomously. This was true for both adults and children with asthma and across the three main types of interventions included in the review. However, interventions used in the included studies were variable, even within the three main comparisons that we have identified. Investigators measured outcomes at different time points and in different ways; thus we have limited confidence in how our findings can be applied to the real‐life setting. A checklist score is not necessarily the most useful measure for clinicians; not all items on the checklist are equally important for achieving medication delivery, and this distinction is not clear when mean scores alone are reported. For example, failing to remove an inhaler cap is a critical error, whereas failing to hold the inhaler upright might not be so critical. A more useful measure, reported by a minority of included studies, is a dichotomous outcome that reports the number of people with (or without) a critical inhaler handling error. We know that critical errors are common, ranging in one study from 12% to 44% of users (depending on inhaler type), and are associated with poorer outcomes (Melani 2011).
In addition, many included studies have treated checklist scores as continuous variables and have used parametric statistical tests, but these measures are clearly skewed, and the wisdom of this analysis choice could be questioned. As a result of the skew and the heterogeneity of the measurement tools used, we chose not to perform meta‐analyses of checklist outcomes and instead reported these outcomes in data tables. Our inability to pool inhaler technique measurements for most of the included studies has considerably limited the conclusions that we can reach.
Another limitation to the applicability of our findings is that we were unable to perform most of our planned subgroup and sensitivity analyses, or, when we were able, our subgroups included very few studies, limiting our confidence in the findings. This means that we cannot comment on whether multiple intervention sessions are superior to one‐off sessions, or whether delivering the intervention to a healthcare professional (e.g. a pharmacist) is more or less effective than delivering the intervention directly to the patient. These are important issues, as the feasibility of larger‐scale implementation would be affected by such intervention design details.
Improvements in inhaler technique observed in many of the included studies did not always translate to any meaningful benefit for patient‐important outcomes, such as exacerbations and quality of life. In some cases, these outcomes were simply not measured; in other cases, studies may not have been powered, or were of insufficient duration, to detect a difference. The maximum duration of follow‐up was only 26 weeks (three studies), and many trials had a much shorter duration. Also, as discussed above, although many participants were performing steps more correctly, they still might have been making critical errors that prevented improved drug delivery and therefore limited clinical improvement.
Another important consideration when the applicability of the evidence is assessed is whether such interventions could be delivered realistically in routine clinical practice. Many healthcare systems are under strain, and healthcare professionals may have only a few minutes to spend with each patient. In view of the time‐consuming nature of many of the interventions investigated in this review, it is even more essential for researchers to demonstrate that clear clinical benefit can be expected from this investment of resources. Of note, only 10 of the 29 studies included in this review were published within the past five years, and of these, only six contributed data to at least one meta‐analysis.
An alternative explanation for the lack of clinical improvement would be that very few of the included studies attempted to address adherence; even a participant who can demonstrate correct technique at follow‐up may not have been adherent to the medication regimen during the follow‐up period. Inadequate adherence to prescribed medication is thought to have contributed to approximately one‐third of asthma deaths in the UK over the course of a year (NRAD 2014). An intervention to improve inhaler technique could be considered incomplete unless it also includes an attempt to address adherence. However, our protocol clearly stated that we would include only studies for which improving inhaler technique was the main aim, and adherence is the topic of another Cochrane Review. This resulted in the exclusion of many studies for which inhaler technique training was just one component of a broader self‐management or asthma education intervention. As a result, we may have excluded studies that would have been informative in a 'real‐world' setting, but their inclusion would have further hampered interpretation of findings. It would be very difficult to assess which element of the intervention had led to any observed clinical benefit.
Some included studies specifically recruited people known to have poor inhaler technique or people with poorly controlled asthma. We did not plan to analyse people with poorly controlled asthma separately from those with better controlled asthma. Greater improvements might have been seen in this group than in a more general asthma population, and this might help in terms of targeting a potentially expensive and time‐consuming intervention in clinical practice. Review authors could consider such a subgroup analysis for future updates of this review.
Quality of the evidence
Most of the evidence that could be combined and graded was related to inhaler technique, asthma control and quality of life. For all of these outcomes, risk of performance and detection bias may have led to an overestimation of treatment effects. Although it was not possible to blind the delivery of behavioural interventions within studies, it would have been possible to control for detection bias by blinding those who assessed inhaler technique at the end of the study; in most cases, this was not done. Across comparisons and outcomes, we downgraded evidence quality for this reason unless it was clear that a particular outcome had been assessed independently (e.g. inhaler technique in Goodyer 2006 and Savage 2003). We were more confident in results from studies in which the control group received additional support or an active control intervention, as this would have minimised the effects of performance bias. For outcomes for which risk of bias was our only concern, we had moderate confidence in the results, meaning that the true effect is likely to be close to that estimated. This was true for inhaler technique in adults given enhanced and multi‐media training, and for responder analyses of asthma control and quality of life.
Our confidence in results was also reduced by imprecision of estimates for which confidence intervals did not exclude the possibility of the effect favouring the control group. This took our confidence in the evidence down to low, which was the most common rating across outcomes. This means that our confidence in the effect estimates is limited, and that the true effect may be substantially different from that estimated from the current evidence. When we noted inconsistency between results, we further downgraded the evidence to very low quality; we did this for the effect of enhanced training on asthma control in adults (comparison 1).
We did not apply GRADE criteria to outcomes for which we could not perform a meta‐analysis, including those for which data were available but we considered it unreasonable to pool results. In these cases, particularly for inhaler technique checklist scores, the results are very difficult to interpret owing to inconsistencies in measurement and non‐parametric properties of the data.
Potential biases in the review process
We followed the methods described in the published protocol (Normansell 2016) and recorded any deviations in the section titled Differences between protocol and review. We made some changes to the division of the workload, but the main deviation from the protocol was result of insufficient data, which prevented several planned meta‐analyses. This is discussed in Overall completeness and applicability of evidence.
We did not know in advance how studies would vary, particularly with regard to interventions delivered and the nature of control groups. As a result, the method of grouping studies into comparisons was iterative and was based on the judgement of the review authors. We stated in the protocol that we would conduct meta‐analyses only "if treatments, participants and the underlying clinical question were similar enough for pooling to make sense". We have been transparent about which studies were included in each comparison but we accept that the post hoc nature of this process could have introduced bias.
Usually we would contact study authors to ask for additional outcome data and to clarify uncertainties about risk of bias, so we could be certain that the evidence is reliable and complete. Owing to the large number of studies identified, we did not contact study authors routinely for this information and contacted teams only if we wished to clarify specific issues related to outcome data. We did not request unpublished data, so analyses may be incomplete if studies did not include all of their outcomes or time points in the published reports. We assessed several studies to be at high risk of bias for selective outcome reporting, but we did not strongly suspect that publication bias compromised the meta‐analyses we were able to perform.
Agreements and disagreements with other studies or reviews
Poor inhaler technique is a common and burdensome problem, and several primary studies previously evaluated interventions to improve inhaler technique among both children and adults with asthma. The variety of interventions assessed and outcomes presented in the primary studies posed significant challenges for our review. Previous relevant systematic reviews identified similar issues. Gillette 2016 evaluated educational interventions to improve inhalation technique among children with asthma on the basis of results obtained from 28 studies. Lavorini 2007 assessed the effect of incorrect use of dry powder inhalers on the treatment of patients with asthma and chronic obstructive pulmonary disease (COPD); this review included 47 relevant primary studies. Both of these reviews identified significant variation in the proportion of patients correctly using their inhalers, which was associated with the use of different inhaler devices and different evaluation methods. In our review, we did not assess differences among devices. Both previous reviews also concluded that appropriate inhaler technique instruction leads to significant but short‐lived improvement in inhalation technique. Our review detected a trend towards prolonged benefit compared with control. However, this finding is based on very limited data, and confirmatory trials are required. In the meantime, as suggested by previous systematic reviews, correct inhaler technique should be reassessed and reinforced regularly. Finally, although Lavorini 2007 describes only incorrect inhaler technique and whether or not patients received adequate instruction, Gillette 2016 identified a variety of educational interventions with different efficacy, which is consistent with our findings.
Authors' conclusions
Implications for practice.
The studies included in this review have examined a variety of interventions, and although many studies report an improvement in checklist score or a greater number of people with correct technique, these results do not clearly translate into clinical benefit; very few studies have reported adverse events. Clinical guidelines consistently recommend that practitioners regularly check that their patients with asthma are using the correct inhaler technique, and evidence suggests that poor technique is associated with worse clinical outcomes. Until larger and longer trials detect consistent improvement in clinical outcomes after a specific inhaler technique intervention, it is reasonable for practitioners to continue following recommended practice to consider ease of use and patient attributes when choosing the type of inhaler to prescribe, ask their patients regularly to demonstrate their inhaler use, correct their technique when necessary, or refer patients for a local inhaler technique intervention.
Implications for research.
Many of the studies included in this review are at least 10 years old, and only 10 have been published within the past five years, suggesting that the evidence base is somewhat dated. Future trials should be adequately powered and of sufficient duration (ideally should last at least six months) to detect clinical improvements and possible harms. Although standardised checklists provide a useful measure, it would be helpful if more triallists report the number of participants achieving an adequate technique, or not performing any critical errors, as this information may serve as a more meaningful measure and would allow increased meta‐analysis. Ideally, inhaler technique should be assessed by a person blind to group allocation, and triallists should clearly report baseline asthma severity and medication use. Given that many of the interventions in this review are likely to be expensive, an economic evaluation would be a useful addition to future studies. Triallists might also consider measuring and reporting adherence to inhaled medication during these trials; this would help to clarify whether improved adherence led to observed benefits, or whether adherence was insufficient for improved technique to have any impact on clinical outcomes.
Issues such as appropriate inhaler choice to best suit patient needs, patient preference, and factors affecting the successful implementation of inhaler technique interventions are all crucial elements of good technique and successful care, but were beyond the scope of this review. A qualitative review investigating how these factors interact with effectiveness would help to inform the application of this study’s findings to real‐life settings.
What's new
| Date | Event | Description |
|---|---|---|
| 7 June 2022 | Amended | Conclusions amended in light of a commenton the review. |
History
Protocol first published: Issue 7, 2016 Review first published: Issue 3, 2017
Acknowledgements
Anne Holland was the Editor for this Cochrane review and commented critically on it.
We based the Background and Methods sections of this protocol on a standard template used by Cochrane Airways.
We would like to thank Kyung‐Hwa Seo and Miyoung Choi, who kindly provided Korean translations for Lee 2010.
Appendices
Appendix 1. Sources and search methods for the Cochrane Airways Group Specialised Register (CAGR)
Electronic searches: core databases
| Database | Search frequency |
| MEDLINE (Ovid) | Weekly |
| EMBASE (Ovid) | Weekly |
| CENTRAL (The Cochrane Library) | Monthly |
| PsycINFO (Ovid) | Monthly |
| CINAHL (EBSCO) | Monthly |
| AMED (EBSCO) | Monthly |
Handsearches: core respiratory conference abstracts
| Conference | Years searched |
| American Academy of Allergy, Asthma and Immunology (AAAAI) | 2001 onwards |
| American Thoracic Society (ATS) | 2001 onwards |
| Asia Pacific Society of Respirology (APSR) | 2004 onwards |
| British Thoracic Society Winter Meeting (BTS) | 2000 onwards |
| Chest Meeting | 2003 onwards |
| European Respiratory Society (ERS) | 1992, 1994, 2000 onwards |
| International Primary Care Respiratory Group Congress (IPCRG) | 2002 onwards |
| Thoracic Society of Australia and New Zealand (TSANZ) | 1999 onwards |
Asthma search
1. exp Asthma/
2. asthma$.mp.
3. (antiasthma$ or anti‐asthma$).mp.
4. Respiratory Sounds/
5. wheez$.mp.
6. Bronchial Spasm/
7. bronchospas$.mp.
8. (bronch$ adj3 spasm$).mp.
9. bronchoconstrict$.mp.
10. exp Bronchoconstriction/
11. (bronch$ adj3 constrict$).mp.
12. Bronchial Hyperreactivity/
13. Respiratory Hypersensitivity/
14. ((bronchial$ or respiratory or airway$ or lung$) adj3 (hypersensitiv$ or hyperreactiv$ or allerg$ or insufficiency)).mp.
15. ((dust or mite$) adj3 (allerg$ or hypersensitiv$)).mp.
16. or/1‐15
Filter to identify randomised controlled trials (RCTs)
1. exp "clinical trial [publication type]"/
2. (randomised or randomised).ab,ti.
3. placebo.ab,ti.
4. dt.fs.
5. randomly.ab,ti.
6. trial.ab,ti.
7. groups.ab,ti.
8. or/1‐7
9. Animals/
10. Humans/
11. 9 not (9 and 10)
12. 8 not 11
We have adapted the MEDLINE strategy and RCT filter (Lefebvre 2011), to enable us to identify trials in other electronic databases.
Appendix 2. Search strategy to identify relevant trials from the CAGR
#1 AST:MISC1
#2 MeSH DESCRIPTOR Asthma Explode All
#3 asthma*:ti,ab
#4 #1 or #2 or #3
#5 MeSH DESCRIPTOR Metered Dose Inhalers Explode All
#6 MeSH DESCRIPTOR Dry Powder Inhalers
#7 MeSH DESCRIPTOR Administration, Inhalation
#8 (#5 or #6 or #7) AND (technique* or train* or instruct* or educat* or teach* or skill*)
#9 (inhaler* or inhalation*) NEAR3 (use or technique* or train* or instruct* or educat* or teach* or skill*)
#10 (inhaler* or inhalation*) NEAR3 (error* or incorrect* or poor* or mishandl*)
#11 inhalation* near3 aid*
#12 #8 or #9 or #10 or #11
#13 #4 AND #12
[Note: in search line #1, MISC1 denotes the field in the record where the reference is coded for condition, in this case, asthma]
Data and analyses
Comparison 1. Adults: enhanced education versus control/usual care.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1.1 Correct inhaler technique (at follow‐up) | 3 | 258 | Odds Ratio (M‐H, Random, 95% CI) | 5.00 [1.83, 13.65] |
| 1.2 Inhaler technique score | 6 | Other data | No numeric data | |
| 1.3 Asthma control | 2 | 247 | Std. Mean Difference (IV, Random, 95% CI) | 0.48 [‐0.29, 1.24] |
| 1.4 Asthma control | 2 | 134 | Odds Ratio (M‐H, Random, 95% CI) | 3.18 [1.47, 6.88] |
| 1.5 Exacerbations requiring at least OCS | 1 | Odds Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 1.6 Exacerbations requiring ED/hospitalisation | 1 | Odds Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 1.7 Quality of life | 2 | 247 | Std. Mean Difference (IV, Random, 95% CI) | 0.52 [‐0.04, 1.09] |
| 1.8 Subgroup analysis: inhaler technique (at follow‐up): to whom intervention is delivered | 3 | 258 | Odds Ratio (M‐H, Random, 95% CI) | 5.00 [1.83, 13.65] |
| 1.8.1 Delivered to participants | 2 | 174 | Odds Ratio (M‐H, Random, 95% CI) | 3.03 [1.61, 5.68] |
| 1.8.2 Delivered to pharmacists | 1 | 84 | Odds Ratio (M‐H, Random, 95% CI) | 12.38 [4.04, 37.90] |
| 1.9 Subgroup analysis: asthma control: to whom intervention is delivered | 2 | 247 | Std. Mean Difference (IV, Random, 95% CI) | 0.48 [‐0.29, 1.24] |
| 1.9.1 Delivered to participants | 1 | 150 | Std. Mean Difference (IV, Random, 95% CI) | 0.10 [‐0.22, 0.42] |
| 1.9.2 Delivered to pharmacists | 1 | 97 | Std. Mean Difference (IV, Random, 95% CI) | 0.88 [0.46, 1.30] |
| 1.10 Subgroup analysis: inhaler technique (at follow‐up): off‐off vs repeated sessions | 3 | 258 | Odds Ratio (M‐H, Random, 95% CI) | 5.00 [1.83, 13.65] |
| 1.10.1 One‐off | 1 | 24 | Odds Ratio (M‐H, Random, 95% CI) | 3.50 [0.50, 24.56] |
| 1.10.2 Repeated | 2 | 234 | Odds Ratio (M‐H, Random, 95% CI) | 5.64 [1.40, 22.66] |
1.5. Analysis.

Comparison 1: Adults: enhanced education versus control/usual care, Outcome 5: Exacerbations requiring at least OCS
1.6. Analysis.

Comparison 1: Adults: enhanced education versus control/usual care, Outcome 6: Exacerbations requiring ED/hospitalisation
Comparison 2. Children: enhanced education versus control/usual care.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 2.1 Correct inhaler technique (at follow‐up) | 2 | 175 | Odds Ratio (M‐H, Random, 95% CI) | 1.29 [0.70, 2.36] |
| 2.2 Inhaler technique (PIF immediately after intervention) | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 2.3 Inhaler technique (PIF at follow‐up) | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 2.4 Subgroup analysis: inhaler technique (at follow‐up): one‐off vs repeated sessions | 2 | 175 | Odds Ratio (M‐H, Random, 95% CI) | 1.29 [0.70, 2.36] |
| 2.4.1 One‐off | 1 | 120 | Odds Ratio (M‐H, Random, 95% CI) | 1.37 [0.66, 2.83] |
| 2.4.2 Repeated | 1 | 55 | Odds Ratio (M‐H, Random, 95% CI) | 1.11 [0.37, 3.38] |
Comparison 3. Adults: multi‐media training versus control/usual care.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 3.1 Correct inhaler technique (immediately after intervention) | 2 | 164 | Odds Ratio (M‐H, Random, 95% CI) | 2.15 [0.84, 5.50] |
| 3.2 Correct inhaler technique (at follow‐up) | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 3.3 Inhaler technique score | 2 | Other data | No numeric data |
Comparison 4. Children: multi‐media training versus control/usual care.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 4.1 Change in inhaler technique score | 2 | Other data | No numeric data | |
| 4.2 Asthma control (change from baseline) | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 4.3 Asthma control (endpoint) | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only |
Comparison 5. Adults: feedback device versus control/usual care.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 5.1 Inhaler technique (PIF) | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 5.2 Correct inhaler technique (at follow‐up) | 1 | Odds Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 5.3 Inhaler technique score | 1 | Other data | No numeric data | |
| 5.4 Asthma control | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 5.5 Quality of life | 2 | 100 | Mean Difference (IV, Random, 95% CI) | 0.38 [‐0.01, 0.77] |
| 5.6 Quality of life (responders) | 1 | Odds Ratio (M‐H, Random, 95% CI) | Subtotals only |
5.3. Analysis.
Comparison 5: Adults: feedback device versus control/usual care, Outcome 3: Inhaler technique score
| Inhaler technique score | |||||
| Study | Time of rating | Intervention mean (SD) | Control mean (SD) | Total N |
Scale (higher score= better technique) |
| Toumas‐Shehata 2014 | Follow‐up (4 wks) | 9.50 (1.00) | 8.90 (1.00) | 97 | Max 10 or 11 |
Comparison 6. Children: feedback device versus control/usual care.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 6.1 Inhaler technique (PIF) | 2 | 98 | Mean Difference (IV, Random, 95% CI) | ‐9.22 [‐33.71, 15.27] |
| 6.2 Asthma control | 2 | 98 | Mean Difference (IV, Random, 95% CI) | ‐0.02 [‐0.35, 0.32] |
| 6.3 Quality of life (change from baseline) | 2 | 91 | Mean Difference (IV, Random, 95% CI) | 0.25 [‐0.07, 0.58] |
| 6.4 Quality of life (endpoint) | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Acosta 2009.
| Study characteristics | ||
| Methods |
Design: single‐blind parallel‐group randomised controlled trial Duration: 4 weeks Setting: USA Trial registration: not reported |
|
| Participants |
Population: 133 people with asthma randomised to an MDI inhaler technique training video or an asthma education video (n per group not reported) Age: "adults" Baseline asthma severity: not reported Inclusion criteria: "asthma patients" Exclusion criteria: not reported Percentage withdrawn: not reported per group; 17/133 (13%) did not complete trial Other allowed medication: not reported |
|
| Interventions |
Intervention summary: MDI training video shown at index visit with pre and post assessment of inhaler technique, with follow‐up at 1 month Control summary: asthma education video shown at index visit with pre and post assessment of inhaler technique, with follow‐up at 1 month |
|
| Outcomes |
Outcomes measured: "correct usage" Technique assessment method used: not reported |
|
| Notes |
Type of publication: conference abstract Funding: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Patients were randomized" ‐ no further details of sequence generation |
| Allocation concealment (selection bias) | Unclear risk | No details |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No description of procedures intended to blind participants or personnel to group assignment |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | "The examiner (who assessed inhaler technique) was blinded to the intervention" |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Although 116/133 (87%) participants completed the trial, the drop‐out for each arm is not reported |
| Selective reporting (reporting bias) | High risk | No prospective trial registration identified. Minimal details as reported, as conference abstract only. Unclear how "correct technique" was assessed |
| Other bias | Low risk | None noted |
Agertoft 1998.
| Study characteristics | ||
| Methods |
Design: single‐blind parallel‐group randomised controlled trial Duration: 2 weeks Setting: 1 outpatient clinic in Denmark Trial registration: not reported |
|
| Participants |
Population: 72 children with asthma randomised to hospital and home training (n = 36) or hospital training alone (n = 36) Age: children aged 3 to 5 years; mean age 54 months (range 36 to 71 months) Baseline asthma severity: not reported Inclusion criteria: preschool children aged 3 to 5 years. All had bronchial asthma and were receiving inhaled anti‐inflammatory therapy through a pMDI and spacer Exclusion criteria: children with acute wheeze Percentage withdrawn: 0% of participants withdrew from the intervention group and 3% from the control group Other allowed medication: All children continued their regular antiasthma therapy throughout the course of the study |
|
| Interventions |
Intervention summary: instructional video followed by instructional pamphlet contained in the commercially available Turbuhaler package. Intervention group children then received individual training from a nurse and a placebo inhaler to practice with at home over the next 2 weeks Control summary: instructional video followed by instructional pamphlet contained in the commercially available Turbuhaler package |
|
| Outcomes |
Outcomes measured: lung function measures: peak inspiratory flow (PIF) and inspiratory vital capacity (IVC). Peak expiratory flow rate (PEF), forced expiratory volume in 1 second (FEV1) and forced vital capacity (FVC) were measured "for demographic purposes only" Technique assessment method used: PIF was used as a measure of inhaler technique |
|
| Notes |
Type of publication: single peer‐reviewed journal article Funding: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "At study entry, the children were stratified by age and randomly allocated to one of two study groups". It not clear how the sequence was generated for randomisation after stratification by age |
| Allocation concealment (selection bias) | Unclear risk | No details |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Children, caregivers and personnel could not be blinded owing to nature of intervention. However, given the young age of children and the objective nature of the outcome measures (lung function), it is unlikely that knowledge of group allocation had an impact on their performance, beyond the impact intended by the intervention |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | The trial is described as single‐blind. "The investigator conducting all inspiratory and expiratory lung function testing was unaware of the level of training received by each child after the initial basic clinic training". In addition, lung function measures are relatively objective and are not at high risk of detection bias |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Only 1 child in the control group was withdrawn from the trial by parents |
| Selective reporting (reporting bias) | Unclear risk | No prospective trial registration identified. Baseline characteristics table missing, so unable to assess baseline imbalances objectively, although text states that groups were balanced. All outcomes listed in Methods reported in the text |
| Other bias | Low risk | None noted |
Al‐Showair 2007.
| Study characteristics | ||
| Methods |
Design: parallel‐group randomised controlled trial; blinding not stated Duration: 6 weeks Setting: 1 outpatient clinic, UK Trial registration: not reported |
|
| Participants |
Population: 108 people with asthma randomised to verbal training plus 2Tone Trainer (n = 36) or verbal training alone (n = 36) Age: mean age (SD) in the intervention group 58.3 (13.7) years, and in the control group 52.6 (16.7) years Baseline asthma severity: intervention group: FEV1 % predicted (SD) 71.4 (22.0); mini‐AQLQ (SD) 3.8 (1.1). Control group: FEV1 % predicted (SD) 76.9 (24.1); mini‐AQLQ (SD) 3.9 (1.0) Inclusion criteria: Patients with asthma who were attending an outpatient clinic were invited to take part in this study. Each patient had to be receiving an inhaled corticosteroid from an MDI without a spacer device. Patients with adequate co‐ordination but too rapid inspiratory flow were randomised to 1 of the 2 intervention groups Exclusion criteria: patients who had experienced an acute exacerbation in the past 4 weeks; patients who were deaf or unable to distinguish between 1 and 2 tones with the 2T; patients with poor inhaler co‐ordination who were ineligible for the study and were referred to the asthma nurse for inhaler technique training Percentage withdrawn: 0% of participants withdrew from the intervention group, and 3% from the control group Other allowed medication: "There were no changes to patients' prescriptions" |
|
| Interventions |
Intervention summary: The 2Tone Trainer looks like an MDI but does not have a canister, so that when it is used, the patient does not receive a dose. During use, this training aid provides users with audible feedback according to the patient’s inhalation rate. It makes a 2‐tone sound when the patient is inhaling at 60 L/min, 1 tone when inhaling between 30 and 60 L/min and no sound when inhaling at 30 L/min. Patients are advised to obtain the 1‐tone noise and thus become accustomed to the degree of inspiratory effort they need to make to achieve this rate through an MDI. Participants were given a 2Tone Trainer to use at home and received the same verbal training as the verbal training alone group Control summary: Verbal training participants were trained on the most desirable inhalation technique with emphasis on breathing out slowly as far as comfortable and actuating a dose at or soon after the start of a slow inhalation. A slow inhalation was defined as an inhalation that filled the lungs with air that lasted 5 seconds |
|
| Outcomes |
Outcomes measured: peak inspiratory flow (PIF), FEV1 and quality of life (AQLQ) Technique assessment method used: PIF was used as a measure of inhaler technique |
|
| Notes |
Type of publication: single peer‐reviewed journal article plus 2 conference abstracts Funding: 2Tone Trainers were donated by Canday Medical Ltd. Dr Al‐Showair was financially supported by a scholarship from the Saudi Arabian Government, and the study was part of his PhD thesis |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Subjects in the intervention group were randomly allocated into the verbal training (VT) group or the 2T group" ‐ no further details of sequence generation |
| Allocation concealment (selection bias) | Unclear risk | No details |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No description of procedures intended to blind participants or personnel to group assignment |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No description of procedures intended to blind outcome assessors to group assignment; for outcomes such as AQLQ, the participant/caregiver is the outcome assessor; therefore these outcomes may be at risk of detection bias |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Only 1 participant withdrew from the study |
| Selective reporting (reporting bias) | Unclear risk | No prospective trial registration identified. However, all outcomes listed in Methods clearly reported in paper |
| Other bias | Low risk | None noted |
Ammari 2013.
| Study characteristics | ||
| Methods |
Design: parallel‐group randomised controlled trial; blinding not stated Duration: 6 weeks Setting: 1 outpatient clinic, UK Trial registration: not reported |
|
| Participants |
Population: 56 people with asthma randomised to 2 Tone Trainer (2TT) group (n = 23; 17 adults, 6 children) or verbal counselling (VC) group (n = 23; 17 adults, 6 children). Children with adequate technique at initial assessment formed the "control" group (not of interest in this study, as not randomised) (we have assigned the 2TT as the "intervention" arm and the VC as the "control" arm) Age: 4 to 55 years; mean (SD) age in the intervention group: adults 38.5 (10.8) years, children 11.7 (2.4) years; and in the control group: adults 42.4 (7.2) years, children 11.2 (2.4) years Baseline asthma severity: "Mild‐moderate‐severe asthma, according to GINA 2008" Inclusion criteria: 4 to 55‐year‐old asthmatic patients prescribed at least 1 MDI without spacer Exclusion criteria: experienced an acute exacerbation or received oral prednisolone within 4 weeks before recruitment, other illnesses adversely affecting respiratory system, hearing problems and/or unable to distinguish between 1 and 2 tones produced by the 2TT tool Percentage withdrawn: 12% adults, 0% children withdrew from the intervention (2TT) arm; 18% adults and 17% children withdrew from the "control" (VC) arm Other allowed medication: not reported |
|
| Interventions |
Intervention summary: verbal training plus use of 2 Tone Trainer (2TT) device, which participants were able to take home. 2TT is a training aid with audible feedback when the required slow inhalation flow is used Control summary: verbal training with emphasis on inspiratory flow rate |
|
| Outcomes |
Outcomes measured: lung function measures: change in FEV1; inhalation flow rate; QOL: Juniper's Asthma QOL Questionnaire (AQLQ): adults ‐ Mini AQLQ; children ‐ PAQLQ; PACQLQ by parents of children Technique assessment method used: PIF was used as a measure of inhaler technique |
|
| Notes |
Type of publication: single peer‐reviewed journal article Funding: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "…based on a previously constructed randomization table" |
| Allocation concealment (selection bias) | Unclear risk | No details |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No description of procedures intended to blind participants or personnel to group assignment |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No description of procedures intended to blind outcome assessors to group assignment; for outcomes such as AQLQ, participant/caregiver is the outcome assessor; therefore these outcomes may be at risk of detection bias |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 56 asthmatic patients enrolled and 50 completed the 2 study visits as per protocol. Balanced drop‐out |
| Selective reporting (reporting bias) | Unclear risk | No prospective trial registration identified. No power analysis reported. Outcomes listed in Methods all reported in the text |
| Other bias | Low risk | None noted |
Ammari 2015.
| Study characteristics | ||
| Methods |
Design: parallel‐group randomised controlled trial; blinding not stated Duration: 12 weeks Setting: paediatric respiratory outpatient clinics at NHS teaching hospitals in UK Trial registration: not reported |
|
| Participants |
Population: 80 children with asthma randomised to AeroChamber Plus with Flow‐Vu (FV) (n = 40) or AeroChamber Plus (AC) (n = 40) Age: children aged 1 to 5 years; mean age (SD) in the intervention group 2.8 (0.93) years, and in the control group 3.4 (1.09) years Baseline asthma severity: intervention group: "partly controlled ‐ or uncontrolled asthma"; baseline ACQ (SD): 1.75 (0.54); PAQLQ (total) (SD): 5.34 (0.90). Control group: "partly controlled ‐ or uncontrolled asthma"; baseline ACQ (SD): 1.91 (1.11); PAQLQ (total) (SD): 4.97 (1.05) Inclusion criteria: children aged 1 to 5 years with partially controlled or uncontrolled asthma according to GINA (2008) criteria and receiving parentally supervised inhalation therapy, including an inhaled corticosteroid, via a pMDI plus a spacer device Exclusion criteria: inhalation treatment had been changed over the 4 weeks before enrolment, using a dry powder inhaler or a breath‐activated pMDI, limited physical or mental ability to use a spacer or to follow study procedures, had other chronic disease conditions at study enrolment that might adversely affect their quality of life Percentage withdrawn: No participants withdrew from the trial Other allowed medication: "No change in the asthma medications was recorded for all participants throughout the study period" |
|
| Interventions |
Intervention summary: AeroChamber Plus with Flow‐Vu: designed with a visual feedback reassurance mechanism of an optimal inhalation; 4 visits over 12 weeks; visit 1 training given on correct use of AC. Randomisation occurred at visit 2, during which training on correct use of FV was given. 2 further follow‐up visits at 6 and 12 weeks post randomisation Control summary: currently available AeroChamber device, which does not have the visual feedback indicator; 4 visits over 12 weeks; visit 1 training given on correct use of AC. Randomisation occurred at visit 2, with further training on use of AC provided. 2 further follow‐up visits at 6 and 12 weeks post randomisation |
|
| Outcomes |
Outcomes measured: peak inspiratory flow (PIF), quality of life (PAQLQ), asthma control (ACQ), parent spacer preference on Likert scale Technique assessment method used: PIF was used as a measure of inhaler technique |
|
| Notes |
Type of publication: single peer‐reviewed journal article Funding: Trudell Medical International, Canada: unconditional grant for the use of facilities at clinics used in the study |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "The children were randomised to use the AC or the FV according to a pre‐study designed randomisation table" |
| Allocation concealment (selection bias) | Unclear risk | No details |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No description of procedures intended to blind participants or personnel to group assignment; outcomes such as PAQLQ and ACQ are subjective and may be at risk of performance bias |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No description of procedures intended to blind outcome assessors to group assignment; for outcomes such as PAQLQ and ACQ, participant/caregiver was the outcome assessor; therefore these outcomes may be at risk of detection bias |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No drop‐out |
| Selective reporting (reporting bias) | Unclear risk | No prospective trial registration identified. However, all outcomes listed in Methods clearly reported in paper |
| Other bias | Low risk | None noted |
Ammari 2015a.
| Study characteristics | ||
| Methods |
Design: parallel‐group randomised controlled trial; blinding not stated Duration: 6 to 8 weeks Setting: not reported Trial registration: not reported |
|
| Participants |
Population: 30 children with asthma randomised to Trainhaler (TH) group (n = 9) or verbal counselling (VC) group (n = 9). Children with adequate inhaler technique formed a "control" group (n = 12) (not of interest in this review, as not randomised; we have assigned the TH as the "intervention" arm and the VC as the "control" arm) Age: aged 7 to 17 years; mean age (SD) in the intervention group 9.9 (1.3) years, and in the control group 9.9 (3.3) years Baseline asthma severity: mean (SD) % predicted FEV1 in the intervention group 91.2 (14.6), and in the control group 84.1 (13.9) Inclusion criteria: asthmatic children, aged 7 to 17 years, with an MDI hand‐lung co‐ordination problem including IF > 60 L/min Exclusion criteria: not reported Percentage withdrawn: not reported Other allowed medication: not reported |
|
| Interventions |
Intervention summary: TH group trained on and given TH to practice at home Control summary: VC group received verbal MDI training with emphasis on using a slow and deep inspiratory flow rate |
|
| Outcomes |
Outcomes measured: inhaler technique, peak IF through the inhaler, asthma control (ACQ) Technique assessment method used: 11‐step MDI checklist |
|
| Notes |
Type of publication: conference abstract; does not appear to be a report of the same study as either of the full‐text reports identified for this study author Funding: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomised but no details (conference abstract). As with Ammari 2013 (although different interventions and only child participants), a control group with good technique was not included in the randomisation, and hence was not included in the review |
| Allocation concealment (selection bias) | Unclear risk | No details |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants and personnel to interventions given |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No mention of outcome assessor blinding and some outcomes were self‐rated (e.g. ACQ), so could have been biased by knowledge of group allocation |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No mention of drop‐outs; conference abstract that does not appear to describe the same study as others reported by this study author |
| Selective reporting (reporting bias) | High risk | ACQ data can be extracted from the abstract and included in the review, but lack of a full publication for linking means we have very limited information about the study |
| Other bias | Low risk | None noted |
Arthurs 2014.
| Study characteristics | ||
| Methods |
Design: parallel‐group randomised controlled trial; blinding not stated Duration: 3 months Setting: paediatric ward, Ireland Trial registration: not reported |
|
| Participants |
Population: 21 children with asthma randomised to DVD inhaler instruction or individual instruction (n for each group not reported) Age: not reported Baseline asthma severity: not reported Inclusion criteria: children already using or with newly prescribed inhalers over 3 months in paediatric ward Exclusion criteria: not reported Percentage withdrawn: not reported Other allowed medication: not reported |
|
| Interventions |
Intervention summary: DVD inhaler instruction about valved holding chamber use Control summary: individual instruction equivalent to information in the DVD; delivered by a physiotherapist |
|
| Outcomes |
Outcomes measured: inhaler technique, self‐efficacy and knowledge acquisition Technique assessment method used: "Technique was assessed immediately post and 3 months after education with a new outcome measure. Intra‐rater and inter‐rater reliability of the new measure was examined" |
|
| Notes |
Type of publication: conference abstract Funding: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "21 participants were randomised to DVD or individual education" ‐ no further details |
| Allocation concealment (selection bias) | Unclear risk | No details |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | "Technique was assessed pre‐education in non‐naive participants". Participants and personnel were aware of group allocation |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No mention of blinded outcome assessment, but only a conference abstract available |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not reported |
| Selective reporting (reporting bias) | High risk | Numerical results not reported |
| Other bias | Low risk | None noted |
Basheti 2005.
| Study characteristics | ||
| Methods |
Design: parallel‐group randomised controlled trial; blinding not stated Duration: 2 weeks Setting: community pharmacies, Australia Trial registration: not reported |
|
| Participants |
Population: 26 people with asthma randomised to standard verbal counselling (group A) (n = 8), augmented verbal counselling (group B) (n = 9) or augmented verbal counselling as above, plus a physical demonstration (group C) (n = 9) Age: mean age 42 years; range 11 to 76 years Baseline asthma severity: across groups, at least 65% were using ICS; mild asthma = 15%, moderate asthma = 62%, severe asthma = 23% Inclusion criteria: had asthma, had been dispensed a Turbuhaler by the recruited pharmacist, aged 10 years or older Exclusion criteria: did not self‐administer Turbuhaler medication, did not speak or understand English, this was first Turbuhaler prescription Percentage withdrawn: 13% withdrew from group A, 11% from group B and 0% from group C Other allowed medication: not reported |
|
| Interventions |
Intervention summaries: Group A: instructions on Turbuhaler technique use following the text of 2 standard items of printed material supplied by the manufacturer. One‐off session with follow‐up at 2 weeks Group B: standard verbal counselling as described above plus extra verbal information, which included reinforcing the 4 essential steps. During both standard and augmented verbal counselling, the researcher was careful not to use hand gestures that might act as a surrogate physical demonstration. One‐off session with follow‐up at 2 weeks Group C: verbal counselling as above, plus a physical demonstration by the researcher, using a placebo Turbuhaler. Technique used in the physical demonstration was the same as illustrated in the product information, with the additional component that the Turbuhaler base was placed on a flat surface during loading. One‐off session with follow‐up at 2 weeks |
|
| Outcomes |
Outcomes measured: inhaler technique Technique assessment method used: 9‐step Turbuhaler checklist |
|
| Notes |
Type of publication: peer‐reviewed journal article and conference abstract Funding: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "After assessment, patients were randomly allocated by computer‐generated list to receive one of 3 types of counselling" |
| Allocation concealment (selection bias) | Unclear risk | No details |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No description of procedures intended to blind participants or personnel to group assignment, which may have changed their experience during the study |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No description of procedures intended to blind outcome assessors to group assignment; assessment of inhaler technique may be at risk of detection bias |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Only 2 participants withdrew (1 from group A and 1 from group B) for reasons unrelated to the intervention |
| Selective reporting (reporting bias) | High risk | No prospective trial registration identified. The only outcome listed in the Methods is reported in paper, but some data are presented in only in graphs and cannot be used for meta‐analysis. In addition, baseline characteristics are given for the whole group ‐ not for each arm ‐ so we cannot assess for baseline imbalances, which may have affected response to the intervention |
| Other bias | Low risk | None noted |
Basheti 2008.
| Study characteristics | ||
| Methods |
Design: single‐blind parallel‐group cluster‐randomised controlled trial (i.e. each randomised pharmacist is a 'cluster') Duration: 26 weeks Setting: community pharmacies, Australia Trial registration: not reported |
|
| Participants |
Population: 31 pharmacists randomised; 97 patients with asthma subsequently enrolled. 16 pharmacists (53 patients) randomised to pharmacist–participant educational intervention and inhaler technique labels; 15 pharmacists (44 participants) randomised to peak flow measurement training (control) Age: mean participant age (SD) in the intervention group: Diskus 51.4 (8.3) years and Turbuhaler 45.48 (19.7) years. Mean participant age (SD) in the control group: Diskus 41.1 (20.0) years and Turbuhaler 38.85 (18.4) years Baseline asthma severity: intervention group: mean peak flow variability (Min%Max) (SD) Diskus 71.5 (9.7) and Tubuhaler 74.8 (9.2); control group: mean peak flow variability (Min%Max) (SD) Diskus 76.0 (7.2) and Tubuhaler 71.2 (8.7) Inclusion criteria: aged 14 years, doctor‐diagnosed asthma, use of inhaled corticosteroid by Turbuhaler or Diskus with or without long‐acting beta2‐agonist, no change in asthma medication or dose for 1 month Exclusion criteria: did not self‐administer medication, did not speak or understand English, were not able to return for all visits, were involved in another study Percentage withdrawn: 1 pharmacist withdrew from the intervention group, and 3 from the control group. 16% of participants withdrew across both groups Other allowed medication: not reported |
|
| Interventions |
Intervention summary: Both groups of pharmacists educated participants on measurement of peak expiratory flow (PEF) for assessment of peak flow variability. Active pharmacists also assessed participants' inhaler technique, without giving them feedback. At visit 2, active pharmacists again assessed participants' inhaler technique, then educated participants using a specialised "Show and Tell" Inhaler Technique counselling service, going through each step on the checklist to describe and demonstrate correct use, repeated up to 3 times if necessary, until the participant had correct technique on all steps. The pharmacist then used a highlighter pen to identify incorrect steps from that day’s initial assessment on an "Inhaler Technique Label", which was attached to the highlighted label on the participant's own controller medication inhaler. At each subsequent visit, active pharmacists repeated inhaler technique assessment/education and placed a new label on the participant's replacement inhaler (or on the old one if still in use). If no steps were incorrect on the initial assessment at any visit, the label was attached to the participant's inhaler with no highlighting. Five visits over 6 months Control summary: Both groups of pharmacists educated participants on measurement of peak expiratory flow (PEF) for assessment of peak flow variability. During the run‐in period, 1 researcher independently assessed inhaler technique for all control participants (to establish their baseline inhaler technique without providing information about correct inhaler technique to control pharmacists). No education was provided to participants during these assessments. For control participants, the researcher re‐assessed inhaler technique at the end of the study, then provided inhaler technique counselling |
|
| Outcomes |
Outcomes measured: peak flow variability, calculated as Min%Max (lowest morning PEF over 2 weeks, as percentage of highest PEF over the same period), Inhaler Technique Score, categorisation of asthma severity based on Australian Asthma Management Handbook, asthma‐related quality of life (AQOL), perceived control (PC) Technique assessment method used: 9‐step inhaler technique checklist |
|
| Notes |
Type of publication: 1 conference abstract, 1 peer‐reviewed journal article, 1 letter to the editor Funding: funded by the Faculty of Pharmacy, University of Sydney. HK Reddel was funded by the Asthma Foundation of NSW |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "After arrival, pharmacists were allocated randomly by computer‐generated list to Active or Control groups" |
| Allocation concealment (selection bias) | Unclear risk | No details |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participating pharmacists could not be blinded to group allocation. It is unclear whether participants were aware of their group allocation, although the trial is reported as 'single‐blind', and control participants did not have their inhaler technique assessed at 3 months "in order to avoid drawing their attention to inhaler technique" |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No description of procedures intended to blind outcome assessors to group assignment, although the study is reported as 'single‐blind'. Patient‐reported outcomes may have been affected by knowledge of group assignment. It is not clear whether the unblinded participating pharmacist, or a blinded researcher, assessed objective outcomes such as inhaler technique |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Although only 5 pharmacists dropped out, report states that 116 participants were enrolled, but only 97 returned from the second visit, at which the first intervention was delivered. It is not clear how many participants were initially enrolled into each arm. It is also unclear how many participants were assessed at 6 months for each outcome. Although it is stated that 97 'completed the study', the total n for those with correct technique at the end equals 84. It is not clear on what number the continuous outcomes were based |
| Selective reporting (reporting bias) | Unclear risk | No prospective trial registration identified. All outcomes listed in Methods appear to be reported in a peer‐reviewed publication and a letter to the editor |
| Other bias | Low risk | None noted |
Boone 2002.
| Study characteristics | ||
| Methods |
Design: parallel‐group randomised controlled trial; blinding not stated Duration: 1 month Setting: primary care, UK Trial registration: not reported |
|
| Participants |
Population: 36 children with asthma randomised to an educational software intervention (n = 17) or placebo software (control) (n = 19) Age: children aged 7 to 11 years; mean age not given Baseline asthma severity: not reported Inclusion criteria: children aged 7 to 11 with asthma and with access to a personal computer Exclusion criteria: not reported Percentage withdrawn: not reported Other allowed medication: not reported |
|
| Interventions |
Intervention summary: an educational computer game called "Space Inhalers", containing educational material about inhaler technique and asthma information Control summary: the same "Space Inhalers" game as in the intervention arm, but without educational material |
|
| Outcomes |
Outcomes measured: inhaler technique, asthma knowledge Technique assessment method used: measured out of 15. No other details |
|
| Notes |
Type of publication: conference abstract Funding: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "subjects were randomised", but no further details |
| Allocation concealment (selection bias) | Unclear risk | No details |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Although it is not clear whether participants or their caregivers were aware of whether they were receiving the active or placebo intervention, it seems unlikely that children in the 7 to 11 year age range were likely to be substantially affected by performance bias as a result of this knowledge. The intervention took place at home, so knowledge of allocation by trial personnel was also unlikely to introduce bias |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No description of procedures intended to blind outcome assessors to group allocation; therefore assessment of inhaler technique and asthma knowledge may be at risk of detection bias |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Drop‐out not reported |
| Selective reporting (reporting bias) | Unclear risk | No prospective trial registration identified, and trial reported only as a conference abstract, so minimal details given. However, both planned outcomes ‐ asthma knowledge and inhaler technique ‐ are clearly reported |
| Other bias | Low risk | None noted |
Bynum 2001.
| Study characteristics | ||
| Methods |
Design: parallel‐group randomised controlled trial; blinding not stated Duration: 4 weeks Setting: recruited from rural junior high and high schools in southeastern Arkansas. Intervention delivered in health clinics in USA Trial registration: |
|
| Participants |
Population: 49 adolescents with asthma randomised to tele‐pharmacy counselling (n = 24) or written instructions only (n = 25) (control) Age: across both groups: 12 to 14 years = 43%, 15 to 17 years = 50%, 18 to 19 years = 7% Baseline asthma severity: not reported Inclusion criteria: diagnosis of asthma, previous MDI use, male or female adolescents in grades 7 to 12, access to a local health clinic with interactive compressed video equipment Exclusion criteria: not reported Percentage withdrawn: 38% of participants withdrew from the intervention group, and 12% from the control group Other allowed medication: not reported |
|
| Interventions |
Intervention summary: Participants in the tele‐pharmacy counselling group demonstrated MDI technique at baseline (pretest) during the first session. A pharmacist scored each performance using the MDI Technique Checklist. Participants received counselling that included verbal instructions and demonstrations by the pharmacist of any needed corrections to their MDI technique. Reassessment for MDI technique immediately followed counselling (post test). MDI technique was assessed a third time 2 to 4 weeks later (follow‐up). After the final assessment session, additional counselling by the pharmacist was provided for participants who needed corrections to their MDI technique or for those who had specific questions about asthma Control summary: The control group also demonstrated pretest, post‐test and follow‐up MDI technique. After completing the pretest assessment, this group received the "Patient’s Instructions for Use of the Metered‐Dose Inhaler" with written instructions for use of the MDI on a package insert provided with their placebo inhaler. These written instructions were reproduced from a patient inhaler package insert that included diagrams demonstrating proper MDI technique and instructions printed in small type. Counselling on correct MDI technique was not provided by the pharmacist during this assessment period. After reviewing the inhaler package insert, participants were immediately reassessed for MDI technique by the pharmacist. After completion of the final assessment, verbal instructions and demonstrations by the pharmacist were given to correct improper MDI technique. Participants in the control group were asked if they had any questions about asthma at this final session and were instructed accordingly |
|
| Outcomes |
Outcomes measured: MDI inhaler technique, patient satisfaction with intervention measured using a "Telepharmacy Metered‐Dose Inhaler Technique Evaluation instrument" (not previously validated) Technique assessment method used: MDI Technique Checklist (validated) evaluated 8 skills for proper MDI technique, including preparation of inhaler equipment, position of the mouth on the inhaler mouthpiece and breathing techniques. Maximum score = 8 |
|
| Notes |
Type of publication: single peer‐reviewed journal article Funding: funded by a grant from the Office for the Advancement of Telehealth in the Department of Health Resources and Services Administration |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | '"The participants in the study were assigned to either a tele‐pharmacy counselling group or a control group using a random number chart" |
| Allocation concealment (selection bias) | Unclear risk | No details |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No description of procedures intended to blind participants or personnel to group assignment |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No description of procedures intended to blind outcome assessors to group allocation; therefore assessment of inhaler technique may be at risk of detection bias |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Unbalanced drop‐out (38% in the intervention group and 12% in the control group) may have introduced bias. In addition, no flow diagram was presented, and reasons for drop‐out were not given, apart from 8 participants who were excluded as they had never used an MDI ("Three students did not attend any visit, 8 students had never used an MDI in the past (and, therefore, did not meet the inclusion criteria), and 2 students did not attend the follow‐up visit for comparison") |
| Selective reporting (reporting bias) | Unclear risk | No prospective trial registration identified. However, all outcomes listed in Methods clearly reported in paper |
| Other bias | Low risk | None noted |
Carpenter 2015.
| Study characteristics | ||
| Methods |
Design: open‐label parallel‐group randomised controlled trial Duration: 1 month Setting: 2 paediatric practices in a medium‐sized metropolitan county in North Carolina, USA Trial registration: NCT01641211 |
|
| Participants |
Population: 91 children and adolescents with asthma randomised to inhaler technique video (n = 46) or an attention control video (n = 45) Age: mean age (SD) in the intervention group was 10.9 (2.6) years, and in the control group 10.8 (2.9) years Baseline asthma severity: intervention group: mild persistent asthma = 52% moderate/severe asthma = 44%; control group: mild persistent asthma = 49% moderate/severe asthma = 51% Inclusion criteria: 7 to 17 years old, could speak English or Spanish, could read the assent form, were present at the visit with an adult (> 18 years old) caregiver (parent or legal guardian) who could speak English or Spanish, used an MDI, missed or incorrectly performed at least 1 step on an inhaler technique assessment, had mild, moderate or severe persistent asthma Exclusion criteria: not reported Percentage withdrawn: 7% of children withdrew from the intervention arm, and 13% from the control arm Other allowed medication: not reported |
|
| Interventions |
Intervention summary: 3‐minute video in English or Spanish. Separate videos were available for an MDI with or without a spacer; children who indicated that they had used an MDI with a spacer and without a spacer watched both MDI videos. Each inhaler video provided an overview of the device and specific instructions for how to use the device correctly. Children watched the videos on a laptop computer and were given a wallet card with a web address and login information, so they could watch the video again after leaving the clinic Control summary: control group: children allocated to an attention control group in which they watched a 3‐minute video about nutrition in English or Spanish. The nutrition video discussed the importance of balancing protein, carbohydrates and lipids in one’s diet |
|
| Outcomes |
Outcomes measured: inhaler technique, child inhaler self‐efficacy, asthma control (ACT) Technique assessment method used: MDI technique was measured as the number of steps (out of 8 possible steps) that the child performed correctly. The RA used an inhaler technique checklist to document whether each step was performed correctly |
|
| Notes |
Type of publication: single peer‐reviewed journal article Funding: This pilot project was supported by Award Number ULTR000083 from the National Center for Advancing Translational Sciences. Dr Carpenter’s salary was supported in part by the National Center for Research Resources and the National Center for Advancing Translational Sciences, National Institutes of Health, through Grant KL2TR000084 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The randomisation sequence was prepared ahead of time by a statistician who used computer‐generated random numbers. Randomisation was stratified by clinic |
| Allocation concealment (selection bias) | Low risk | Immediately after the child’s medical visit, the RA opened a sequentially numbered, sealed envelope to determine whether the child had been allocated to the experimental or control group |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | The study RA was not blinded to children’s experimental group assignment. All children and caregivers were informed that the study was about how children use their asthma devices |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | The study RA was not blinded to children’s experimental group assignment. All children and caregivers were informed that the study was about how children use their asthma devices |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Less than 15% of participants were lost to follow‐up. All randomised participants were included in the adjusted intention‐to‐treat primary analysis |
| Selective reporting (reporting bias) | Low risk | The study was prospectively registered as NCT01641211; outcomes were reported as planned at all time points |
| Other bias | Low risk | None noted |
Donateo 1996.
| Study characteristics | ||
| Methods |
Design: parallel‐group randomised controlled trial; blinding not stated Duration: 1 week Setting: Italy; setting not reported Trial registration: not reported |
|
| Participants |
Population: 36 older adults with asthma randomised to MDI with Jet spacer (n = 18) or MDI without spacer (n = 18) Age: aged 65 years and older; mean age (SD) years in the intervention group 67.9 (1.6), and in the control group 67.6 (1.8) Baseline asthma severity: mean (SD) PEFR % predicted = 65.4(6) in the intervention group, and in the control group 65.5 (5) Inclusion criteria: aged 65 and older, imperfect inhaler technique at baseline, moderate asthma (PEFR 60% to 80% predicted), reversibility (15%+ increase in FEV1 30 minutes post 200 mcg salbutamol), ability to co‐operate and to be instructed on use of inhalers Exclusion criteria: airway infection, serious comorbidity, inability to abstain from theophylline or LABA use during study Percentage withdrawn: 0% of participants withdrew from the intervention group, and 6% from the control group Other allowed medication: inhaled steroids, inhaled sodium cromoglycate and nedocromil were allowed if patients were already receiving these drugs. LABA, oral bronchodilators and anticholinergics were not allowed |
|
| Interventions |
Intervention summary: small (approx. 10 cm diameter) spacer device used with MDI. Intended to reduce need for co‐ordination of actuation and inhalation, to reduce oropharyngeal deposition and to increase deposition in lower airways Control summary: standard MDI without spacer device |
|
| Outcomes |
Outcomes measured: FEV1, PEFR, patient‐reported acceptability of device, adverse events Technique assessment method used: technique not measured or reported |
|
| Notes |
Type of publication: single peer‐reviewed journal article Funding: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Described as 'randomised' but no other details |
| Allocation concealment (selection bias) | Unclear risk | No details |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No description of procedures intended to blind participants or personnel to group assignment |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Although no description of procedures intended to blind participants or personnel to group assignment, outcomes measured in this study unlikely to be prone to detection bias and not included in meta‐analysis |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Only 1 participant withdrew from the study; reason for withdrawal given |
| Selective reporting (reporting bias) | Unclear risk | No prospective trial registration identified. However, all outcomes listed in Methods clearly reported in paper |
| Other bias | Low risk | None noted |
Fernandes 2011.
| Study characteristics | ||
| Methods |
Design: parallel‐group randomised controlled trial; blinding not stated Duration: 12 weeks Setting: "hospital" based, country not stated Trial registration: not reported |
|
| Participants |
Population: 89 people with asthma randomised to an education intervention group (n = 43) or a control group (n = 46) (n not stated explicitly for each group; these numbers are calculated from the percentage female given per group) Age: mean age (SD) in the intervention group 41 (14) years, and in the control group 41 (12) years Baseline asthma severity: "uncontrolled" asthma Inclusion criteria: non‐smoking patients with new, uncontrolled asthma reporting to hospital Exclusion criteria: not reported Percentage withdrawn: not reported Other allowed medication: not reported |
|
| Interventions |
Intervention summary: inhaler technique education delivered by respiratory therapist (no further details) Control summary: routine inhaler technique instruction delivered by physician (no further details) |
|
| Outcomes |
Outcomes measured: inhaler technique and asthma control (ACT) Technique assessment method used: not described |
|
| Notes |
Type of publication: conference abstract Funding: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Described as 'randomised', but no details of sequence generation |
| Allocation concealment (selection bias) | Unclear risk | No details |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No description of procedures intended to blind participants or personnel to group assignment |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No description of procedures intended to blind participants or personnel to group assignment; for patient‐reported outcomes, such as ACT, the participant was the outcome assessor |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Drop‐out not reported |
| Selective reporting (reporting bias) | High risk | No prospective trial registration identified. Minimal details, as reported as conference abstract only. Unclear what "asthma control" percentage refers to. Number of participants included in analysis unclear |
| Other bias | Low risk | None noted |
Goodyer 2006.
| Study characteristics | ||
| Methods |
Design: single‐blind parallel‐group randomised controlled trial Duration: intervention and assessment on the same day Setting: GP surgeries in Camden followed by 'snowball' convenience sampling method was therefore used; contacts in social clubs and informal networks in Tower Hamlets and Camden, UK Trial registration: not reported |
|
| Participants |
Population: 69 Turkish‐speaking people with asthma randomised to a multi‐media touch screen system (MTS) (n = 34) or translated patient information leaflet (PIL) plus support from a translator (PIL + verbal) (n = 35) (PIL + supported treatment as control) Age: mean (SD) age across both groups 41 (17.5) years Baseline asthma severity: not reported Inclusion criteria: Turkish‐speaking people with asthma who use an MDI Exclusion criteria: not reported Percentage withdrawn: not drop‐out Other allowed medication: not reported |
|
| Interventions |
Intervention summary: MTS system covered key steps in correct inhaler use and additional information on posture. Participant could interact with the programme by selecting to replay a step, or could move on to the next one. Participants were allowed to use the programme for as long as they wished before repeating the demonstration. The researcher/translator identified areas where technique could be improved, then spent up to 15 minutes discussing this with the user Control summary: Leaflet was produced by one of the trial authors (fluent in Turkish) and was an exact translation of the current version of Allen and Hanbury’s PIL for the Ventolin MDI. Participants were allowed to study the leaflet for as long as they wished before repeating the demonstration. The researcher/translator identified areas where technique could be improved, then spent up to 15 minutes discussing this with the user |
|
| Outcomes |
Outcomes measured: inhaler technique Technique assessment method used: Participants were videotaped while using their inhaler before and after the intervention. Blinded assessor rated their technique first as a 'quick check', then using a checklist |
|
| Notes |
Type of publication: single peer‐reviewed journal article Funding: funded by the Department of Health and the North London Primary Care Research Network (Nocten) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | '"Patient allocation was done using random number tables" |
| Allocation concealment (selection bias) | Unclear risk | '"Patients did not know in advance which information method they would receive" but no description of concealing allocation from investigators |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants and personnel were aware of group allocation |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | "These assessors (of the inhaler technique videos) did not attend experimental sessions and had no contact with patient volunteers. They were therefore blind as to the information format" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Study was completed in 1 session, with technique assessed before and after instruction. No drop‐out |
| Selective reporting (reporting bias) | Unclear risk | No prospective trial registration identified. Only outcome described in Methods (inhaler technique) is clearly reported, but baseline characteristics per arm not given, so not able to objectively assess for baseline imbalance |
| Other bias | Low risk | None noted |
Lirsac 1991.
| Study characteristics | ||
| Methods |
Design: parallel‐group randomised controlled trial; blinding not stated Duration: 15 days Setting: France; setting not reported Trial registration: not reported |
|
| Participants |
Population: 45 people with asthma randomised to patient information sheet (group 1) (n = 14) or video group (group 2) (n = 14) or video + spacer (group 3) (n = 17) Age: 10 to 71 years; mean (SD) age in group 1: 48 (17) years, in group 2: 35 (19) years and in group 3: 26 (20) years Baseline asthma severity: mean (SD) baseline FEV1 (L): group 1: 2.03 (0.65), group 2: 1.89 (0.61), group 3: 1.77 (0.66) Inclusion criteria: asthma characterised by attacks of paroxysmal dyspnoea with wheezing and a reversible airway obstruction demonstrated in the year preceding inclusion; using daily MDI, but with imperfect technique; had to speak and understand French, be cooperative with the study procedure and not be using a spacer device. Treatment of patients must be stable for 15 days before the start of the study and during the 15 days of the study Exclusion criteria: not reported Percentage withdrawn: no drop‐out Other allowed medication: not reported, although 22 patients were using ICS, and 22 theophylline |
|
| Interventions |
Intervention summaries: Group 1: Participants received MDI use education by reading an information sheet, which included a statement by the doctor and diagrams, for 3 to 4 minutes Group 2: Participants viewed a 5‐minute video describing correct use of the MDI Group 3: Participants viewed the same film as the video group but extended by 2 minutes to describe the use of a spacer device. Participants were also given a spacer device. This group was intended to act as a positive control with optimal inhalation technique |
|
| Outcomes |
Outcomes measured: FEV1, inhalation technique score Technique assessment method used: 4‐item checklist |
|
| Notes |
Type of publication: single peer‐reviewed journal article (in French) Funding: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants were allocated to 1 of 3 groups according to a randomisation code, revealed, for each participant, just before the education |
| Allocation concealment (selection bias) | Low risk | "Revealed, for each patient, just before the education" suggests that this was kept concealed in advance |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No description of procedures intended to blind participants or personnel to group assignment |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No description of procedures intended to blind outcome assessors to group allocation; therefore assessment of inhaler technique may be at risk of detection bias |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Appears all participants completed follow‐up |
| Selective reporting (reporting bias) | High risk | No prospective trial registration identified. All outcomes listed in Methods appear to be reported, but some in graphs, so unable to extract. Inhaler technique data for positive control group also not given, but likely because use of the spacer device made this group incomparable with the other 2 groups |
| Other bias | Low risk | None noted |
Mehuys 2008.
| Study characteristics | ||
| Methods |
Design: parallel‐group randomised controlled trial; blinding not stated Duration: 26 weeks Setting: 66 community pharmacies, Belgium Trial registration: not reported |
|
| Participants |
Population: 201 adults with asthma randomised to a pharmacist education intervention (n = 107) or to usual pharmacy care (n = 94) Age: mean age (range) in the intervention group 35.2 (19 to 51) years, and in the control group 36.3 (17 to 51) years Baseline asthma severity: in the intervention group, 5.6% had an ACT score < 15 (indicating poor control), and in the control group 8.5% had a score < 15 Inclusion criteria: required to carry a prescription for asthma medication. In consecutive order, patients visiting the pharmacy were invited to participate in the study when they fulfilled the following inclusion criteria: aged between 18 and 50 years; being treated for asthma for > 12 months; 3) ‘‘using’’ controller medication; and 4) regular visitor to the pharmacy Exclusion criteria: smoking history of .10 pack‐years, suffering from another severe disease (e.g. cancer) and with an ACT score at screening of,15 (indicating seriously uncontrolled asthma; for ethical reasons, patients were immediately referred to their general practitioner (GP) or respiratory specialist) or equalling 25 (indicating complete asthma control; no room for improvement) Percentage withdrawn: 25% of participants withdrew from the intervention group, and 26% from the control group Other allowed medication: not reported |
|
| Interventions |
Intervention summary: Before the start of the present study, participating pharmacists had a training session about asthma (pathophysiology), its non‐pharmacological and pharmacological treatment (GINA guidelines) and use of the study protocol. Participants in the intervention group received a protocol‐defined intervention at the start of the study and at 1‐ and 3‐month follow‐up visits Control summary: Participants in the control group received usual pharmacist care |
|
| Outcomes |
Outcomes measured: asthma control (ACT), patient diary (nocturnal awakenings due to the number of inhalations of rescue medication; the best of 3 measurements of peak expiratory flow), severe asthma exacerbations (defined as those requiring treatment with oral glucocorticoids (individually recorded in computerised pharmacy records) or an emergency department visit or hospital admission due to asthma), adherence to medication (prescription refill rates and self‐reporting), AQLQ, asthma knowledge inhaler technique Technique assessment method used: 10‐point checklist for MDI + spacer and 8‐point checklist for DPI (1 point for each correct step, but total score of 0 given in major error made, e.g. failure to remove cap) |
|
| Notes |
Type of publication: single peer‐reviewed journal article Funding: funding not reported but study authors thank GlaxoSmithKline (GSK) Belgium for permission to use the Asthma Control Test |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "The sequence of allocation to either control or intervention group was predetermined by the investigators based on a randomisation table" |
| Allocation concealment (selection bias) | Low risk | "Serially numbered, closed envelopes were made for each participating pharmacy. The envelope with the lowest number was opened by the pharmacist upon inclusion of a new patient" |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | It was not possible to blind participants, so some outcomes such as ACT and AQLQ are subject to potential performance bias, as participants knew to which group they were assigned |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Blinding of outcome assessors is not described, and it appears that inhalation technique was assessed by the pharmacist delivering the intervention. Other patient‐reported outcomes (such as ACT and AQLQ) are also at risk because the participant was the outcome assessor |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Approximately 25% of participants dropped out of each arm of the trial. Although reasons were similar and baseline characteristics of those completing and not completing did not differ significantly, rate of drop‐out still high; we cannot be sure this did not affect the results. Secondary outcomes were analysed per protocol rather than by ITT |
| Selective reporting (reporting bias) | Unclear risk | No prospective trial registration identified, although all outcomes listed in Methods reported in text/tables |
| Other bias | Low risk | None noted |
Nahafizadeh 2010.
| Study characteristics | ||
| Methods |
Design: parallel‐group randomised controlled trial; blinding not stated Duration: 2 months Setting: "outpatients", Iran Trial registration: not reported |
|
| Participants |
Population: 46 people with asthma randomised to inhaler technique education (n = 25) or no education/usual care (n = 20) Age: mean age (SD) across both group 48 (13) years Baseline asthma severity: "According to ACT score, none of patients were in complete asthma control at the beginning" Inclusion criteria: not reported Exclusion criteria: not reported Percentage withdrawn: not reported Other allowed medication: not reported |
|
| Interventions |
Intervention summary: face‐to‐face education about proper use of inhalers (no further details) Control summary: usual care (no further details) |
|
| Outcomes |
Outcomes measured: asthma control (ACT) and FEV1 Technique assessment method used: inhaler technique not reported |
|
| Notes |
Type of publication: conference abstract Funding: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "randomly placed"; no further details |
| Allocation concealment (selection bias) | Unclear risk | No details |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No description of procedures intended to blind participants or personnel to group assignment |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No description of procedures intended to blind outcome assessors to group assignment; for patient‐reported outcomes, such as ACT, participant was the outcome assessor |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No description of drop‐outs but numbers reported and related percentages suggest that only 1 person did not complete the study |
| Selective reporting (reporting bias) | Unclear risk | No prospective trial registration identified. Minimal details, as reported as conference abstract only. Unclear how "complete control" is defined. Unclear how many participants were included in the analyses at each time point |
| Other bias | Low risk | None noted |
Ozkaya 2010.
| Study characteristics | ||
| Methods |
Design: single‐blind parallel‐group randomised controlled trial Duration: 12 weeks Setting: allergy outpatient clinic in the urban area of Istanbul, Turkey Trial registration: not reported |
|
| Participants |
Population: 130 children with asthma randomised to face‐to‐face nurse training (n = 66 completed) or no training (package insert) (n = 54 completed). NB: n randomised to each arm not reported Age: mean (SD) age in intervention group 8.2 (1.7) years, and in control group 7.7 (0.9) years Baseline asthma severity: in the intervention group 51 classified as mild asthma, 15 as moderate; in the control group 42 classified as mild asthma; 12 as moderate Inclusion criteria: mild to moderate asthma and attending outpatient allergy clinic. Diagnosis and severity of asthma defined according to GINA 2005 Exclusion criteria: not reported Percentage withdrawn: not reported Other allowed medication: Participants were permitted to take salbutamol or terbutaline as needed for relief of symptoms."None of the patients had previously received an MDI with spacer, and none had taken oral steroids in the past 1‐month" |
|
| Interventions |
Intervention summary: At the beginning of the study, the active group was educated at home on correct use of the MDI spacer by 2 paediatric nurse specialists certified in allergy‐pulmonology. All of the children in this study group received instruction. All participants were prescribed fluticasone propionate 125 mg 1 puff by an MDI with a small‐volume Aerochamber spacer twice daily for 12 weeks. Educational pamphlets, such as those on asthma management, prophylactic measures and trigger avoidance, were also distributed to both groups Control summary: The control group was left as a baseline, meaning that group members did not receive any formal education on correct use of the MDI spacer. However, all study participants received the Aerochamber package insert, which includes information on how to use the device. All participants were prescribed fluticasone propionate 125 mg 1 puff by an MDI with a small‐volume Aerochamber spacer twice daily for 12 weeks. Educational pamphlets, such as those on asthma management, prophylactic measures and trigger avoidance, were also distributed to both groups |
|
| Outcomes |
Outcomes measured: inhalation skill, health‐related quality of life (PAQLQ), spirometry. All participants were asked to keep an asthma diary on the presence of asthma symptoms and on the use of main and additional antiasthmatic drugs Technique assessment method used: Inhalation skill scoring was done using the standardised MDI spacer checklist. Summation of 10 item scores not weighted equally |
|
| Notes |
Type of publication: single peer‐reviewed journal article Funding: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Our subjects were randomly classified into study and control groups at the beginning of therapy" ‐ no further details |
| Allocation concealment (selection bias) | Unclear risk | No details |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No description of procedures intended to blind participants or personnel to group assignment |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | "At the end of the 12 weeks, a paediatric allergist blinded to the results of the pulmonary function parameters (PFPs), rated each child’s MDI spacer skills after asking the child to demonstrate how he or she used the MDI spacer at home". However, it is not clear if this outcome assessor was blinded to group allocation, and for patient‐reported outcomes, such as AQLQ, the un‐blinded participant was the outcome assessor |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Drop‐out not clearly reported (130 children were randomised and 120 are included in the analyses because 10 dropped out. eAlthough this represents fairly low drop‐out overall of 7.7%, it is not clear to which groups the drop‐outs were randomised) |
| Selective reporting (reporting bias) | High risk | No prospective trial registration identified, and the PAQLQ is reported only as a correlation with the MDI checklist, not as means per group |
| Other bias | Low risk | None noted |
Rahmati 2014.
| Study characteristics | ||
| Methods |
Design: open‐label parallel‐group randomised controlled trial Duration: 4 weeks Setting: "clinics", Iran Trial registration: IRCT2013091514666N1 |
|
| Participants |
Population: 90 adults with asthma randomised to face‐to‐face training: non‐spacer group (n = 30) or face‐to‐face training: spacer group (n = 30) or no training (control) (n = 30) Age: mean age (SD) in the non‐spacer group was 41.5 (9.1), in the spacer group 42.7 (13.8) and in the control group 44.7 (10.8) Baseline asthma severity: not reported; however, mean duration of asthma ranged from 2.6 to 2.8 years across groups (with SD < 1.0), which is surprisingly short given the age of participants Inclusion criteria: asthmatic patients who had been referred to the clinics affiliated with Shiraz University of Medical Science, Shiraz. 18 to 60 years old, with a past history of using salbutamol MDI for at least 3 months, and not participating in similar interventional programmes Exclusion criteria: smoking, having an asthmatic attack and not willing to continue co‐operation in the study Percentage withdrawn: no withdrawals Other allowed medication: salbutamol |
|
| Interventions |
Non‐spacer group: Three educational sessions, both theoretical and practical, were held for the 2 intervention groups. Inhalation techniques with and without spacer were taught in the spacer group and the non‐spacer group, respectively. Educational classes included presenting a lecture, showing a PowerPoint, holding a question and answer session and evaluating participants at the end of the session. The content of instructional sessions in the non‐spacer group included the principles of asthma, the importance and advantages of correct inhalation technique, training on inhalation technique without using a spacer and repetition and reinforcement of training presented in 3 sessions Spacer group: as for non‐spacer group but amended to teach correct use of MDI with a spacer Control group: Control group did not receive any interventions |
|
| Outcomes |
Outcomes measured: PEFR and inhalation skills Technique assessment method used: two 11‐item checklists for checking MDI usage skills scored by 0 and 1 (double‐rated in advance on 10 participants showing correlation of 0.95). A separate checklist was used for MDI with and without spacer, and the control group was assessed on both |
|
| Notes |
Type of publication: single peer‐reviewed journal article Funding: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "The subjects were randomly divided into two intervention groups and a control group using block randomization with a random sequence of 6 block sizes." |
| Allocation concealment (selection bias) | Unclear risk | No details |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | "It should be noted that the patients were aware of the reasons of the interventions and the research was not thus blinded" |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No description of procedures intended to blind outcome assessors to group allocation; therefore assessment of inhaler technique may be at risk of detection bias |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No drop‐out, no exclusions from the analysis |
| Selective reporting (reporting bias) | Unclear risk | Prospectively registered trial (IRCT2013091514666N1); all listed outcomes reported |
| Other bias | Low risk | None noted |
Rydman 1999.
| Study characteristics | ||
| Methods |
Design: single‐blind parallel‐group randomised controlled trial Duration: 8 to 20 weeks Setting: 1 inner city asthma clinic, part of Cook County Hospital, Illinois Trial registration: not reported |
|
| Participants |
Population: 68 people with asthma randomised to face‐to‐face verbal training + demonstration (n = 36) or written training (package insert) (n = 32) Age: mean (SD) age in the intervention group 49.5 (16.5) years, and in the control group 43.6 (13.5) years Baseline asthma severity: baseline FEV1 (SD) (L) in the intervention group 2.18 (0.95), and in the control group 2.05 (0.75) Inclusion criteria: diagnosed, stable asthmatic patients who had been in the Pulmonary/Asthma clinic for 6 months Exclusion criteria: missed more than 25% of appointments in the previous 6 months, had an ED visit in the month before entry or 2 or more visits in the prior 6 months, taking more than 10 mg of oral prednisolone daily or 30 mg every other day, unable to read or understand English Percentage withdrawn: 11% of participants withdrew from the intervention arm, and 13% from the control arm Other allowed medication: All participants had access to albuterol in an MDI and pirbuterol in BAI |
|
| Interventions |
Intervention summary: Experimental group received verbal instructions and demonstration on breath actuated inhaler technique. Participants were asked to demonstrate their inhalation technique to the instructor, who counselled them until their technique was deemed proper. Also were given written instructions (package insert). Both experimental and control group participants demonstrated their MDI technique to the instructor upon enrolment (baseline MDI). The instructor then gave them a demonstration of MDI technique and counselled them on correct use of the MDI Control summary: Control group received written instruction only on breath actuated inhaler use. After receiving instructions, participants also demonstrated their technique to the instructor, who did not correct them or give feedback if incorrect. Both experimental and control group participants demonstrated their MDI technique to the instructor upon enrolment (baseline MDI). The instructor then gave them a demonstration of MDI technique and counselled them on correct use of the MDI |
|
| Outcomes |
Outcomes measured: BAI and MDI competency Technique assessment method used: Scoring was based on competency features repeated in scientific literature. Participants had to complete all steps successfully for each of the respective inhalers to be given a score of 1. If any steps were missed, participants were given an overall score of zero for that inhaler technique |
|
| Notes |
Type of publication: single peer‐reviewed journal article Funding: funded in part by a grant from 3M Pharmaceuticals, St. Paul, Minnesota, USA |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Patients were randomized either to an experimental group or control group in order to evaluate two different teaching methods" ‐ no further details (although randomisation reported to be 'successful' owing to lack of baseline imbalance) |
| Allocation concealment (selection bias) | Unclear risk | No details |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No description of procedures intended to blind participants or personnel to group assignment |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | "Patients demonstrated their BAI and MDI techniques to an independent physician who was blinded as to their group assignment" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 68 participants were randomised (36 and 32 in experimental and control groups) and 60 were included in the analyses (32 and 28). Hence, 4 participants dropped out of each group, which was 11.1% and 12.5% drop‐out in intervention and control groups. These people were not included in the analysis, but drop‐out was low and balanced |
| Selective reporting (reporting bias) | Unclear risk | No prospective trial registration identified, although all outcomes listed in Methods reported |
| Other bias | Low risk | None noted |
Savage 2003.
| Study characteristics | ||
| Methods |
Design: single‐blind parallel‐group randomised controlled trial Duration: intervention and assessment on the same day Setting: 4 GP surgeries in North London, UK Trial registration: not reported |
|
| Participants |
Population: 110 adults and adolescents with asthma randomised to a multi‐media touch screen system (MTS) (n = 57) or written training (package insert) (n = 48) Age: aged 12 to 87 years, mean (SD) not given Baseline asthma severity: 44% of participants in the intervention group BTS step 3 and above; 38% in the control group Inclusion criteria: Patients over 12 years old, recorded as using a bronchodilator MDI in the past 6 months, were identified from surgery repeat medication records by the practice manager. Exclusion criteria: problem patients, those known not to speak English well Percentage withdrawn: 9% of participants dropped out from the intervention arm, and 10% from the control arm Other allowed medication: not reported |
|
| Interventions |
Intervention summary: The demonstration on the multi‐media touch screen computer (MTS) covered key information points contained in pictures 1 to 6 of the ‘How to use your inhaler’ section of the Ventolin patient information leaflet. Key messages given in the voice‐over were reinforced as on‐screen text. After each step, the participant could choose whether to proceed, or to replay a section. At the end, the participant could choose to repeat a section, or the whole demonstration. This could be done as many times as the participant wished. Participants were asked to demonstrate how they used their inhaler, and this was videotaped before and after the participant received information. Remaining technique errors were discussed and documented, and participants were referred on to the practice nurse or GP if required Control summary: The patient information leaflet used was a laminated copy of the 1996 version of the Ventolin pack leaflet. Both MTS and PIL used white male models as demonstrators. Participants were asked to demonstrate how they used their inhaler, and this was videotaped before and after the participant received information. Remaining technique errors were discussed and documented, and participants were referred on to the practice nurse or GP if required |
|
| Outcomes |
Outcomes measured: global inhaler technique, co‐ordination of inspiration and inhaler actuation, breathing in time, information acceptability and usefulness (agree, neutral, disagree to a series of 18 statements about information format and content) Technique assessment method used: Videotaped demonstrations were assessed ‘blind’ by an assessor who did not attend experimental sessions and had no contact with participant volunteers. Global technique was rated as poor, adequate or good, and individual steps were scored as correct/incorrect with the use of a checklist. Inhaler shaking (counts) and length of inspiration (seconds) were assessed directly from videotaped recordings |
|
| Notes |
Type of publication: single peer‐reviewed journal article Funding: funded by the Department of Health and the North London Primary Care Research Network |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Patient allocation was done using random number tables, and was stratified by age" |
| Allocation concealment (selection bias) | Unclear risk | "Patients did not know in advance which information method they would receive", but no description of concealing allocation from investigators |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No description of procedures intended to blind participants or personnel to group assignment |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | "They (videos of participants using the inhaler) were subsequently assessed ‘blind’ by an assessor who did not attend experimental sessions and had no contact with patient volunteers" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Less than or equal to 10% drop‐out in both groups |
| Selective reporting (reporting bias) | Unclear risk | No prospective trial registration identified. Only outcome described in Methods (inhaler technique) is clearly reported |
| Other bias | Low risk | None noted |
Schultz 2012.
| Study characteristics | ||
| Methods |
Design: parallel‐group randomised controlled trial; blinding not stated Duration: 52 weeks Setting: research clinic at Princess Margaret Hospital for Children, Perth, Australia Trial registration: not reported |
|
| Participants |
Population: 132 children with asthma randomised to the Funhaler incentive device (n = 64) or Aerochamber control (n = 68) Age: median (range) age in the intervention group 4.25 (2 to 7) years, and in the control group 4.25 (2.1 to 6.9) years Baseline asthma severity: 100% were receiving ICS at baseline (reduced to 67% in intervention group and 70% in control group by end of study) Inclusion criteria: asthma diagnosed by a doctor, prescribed inhaled steroids for treatment of their asthma Exclusion criteria: known immunodeficiency, chronic lung disease other than asthma, known allergy to study medication, had been administered systemic steroids in the 2 months before the baseline study visit Percentage withdrawn: 27% of participants withdrew from the intervention arm, and 6% from the control arm Other allowed medication: none mentioned as excluded. Participants were allowed to continue to take salmeterol |
|
| Interventions |
Intervention summary: 1‐month run‐in: Children were switched to fluticasone if on a different ICS. Those using a spacer with face mask were instructed to use the mouthpiece instead. Spacer technique was checked and corrected if necessary. Children then received regular inhaled fluticasone through a Funhaler Control summary: 1‐month run‐in: Children were switched to fluticasone if on a different ICS. Those using a sacer with face mask were instructed to use the mouthpiece instead. Spacer technique was checked and corrected if necessary. Children then received regular inhaled fluticasone through a conventional valved spacer (Aerochamber) |
|
| Outcomes |
Outcomes measured: asthma control defined as daytime asthma symptoms less than twice a week and night‐time awakenings less than once a month. For 1 week before every study visit, parents documented symptoms of cough and wheeze and bronchodilator use on diary cards. Quality of life (QOL) was measured with the PedsQL 3.0 Asthma Module questionnaire, based on parental response at each study visit Technique assessment method used: Proficiency in spacer technique was measured at the first 4 visits by measuring the amount of salbutamol inhaled from spacer onto a filter interposed between participant and spacer. Five separate doses of salbutamol were administered to ensure that a measurable amount of drug was deposited onto the filters |
|
| Notes |
Type of publication: single peer‐reviewed journal article Funding: funded in part by a grant from the NIH: R01 HL70967. The fluticasone used in the study was supplied by GlaxoSmithKline, Australia. The Funhaler devices used in the study were sponsored by Visiomed, Australia. Sponsors did not have access to the data and played no part in analyses or in interpretation of the data NB: As data were not normally distributed, samples were compared using the Mann–Whitney U‐test |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "After the 1‐month run‐in period, at the baseline study visit, subjects were randomised, using the block randomisation method" |
| Allocation concealment (selection bias) | Unclear risk | No details |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No description of procedures intended to blind participants or personnel to group assignment |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | ''No description of procedures intended to blind participants or personnel to group assignment and for patient reported outcomes, such as PedsQL, the participant/career is the outcome assessor" |
| Incomplete outcome data (attrition bias) All outcomes | High risk | "Significantly more subjects dropped out of the Funhaler group (17 vs 4; P < 0.01)", which may have impacted the results. In addition, it is not always clear how many participants were included in the analysis at each time point for quality of life |
| Selective reporting (reporting bias) | Unclear risk | No prospective trial registration identified; although all outcomes listed in Methods are reported, it is not always clear how many participants were included in the analysis |
| Other bias | Low risk | None noted |
Self 1983.
| Study characteristics | ||
| Methods |
Design: parallel‐group randomised controlled trial; blinding not stated Duration: 1 to 16 weeks (mean 6) but no training (control group); not followed up after initial assessment Setting: allergy clinic in Memphis, Tennessee, USA Trial registration: not reported |
|
| Participants |
Population: 29 adults with asthma randomised to face‐to‐face pharmacist training (n = 9) or video training (n = 10) or no training (package insert) (n = 10) Age: mean age 39 years across all 3 groups Baseline asthma severity: 4 participants in each group had previously used the devices ‐ most were not taking/did not need MDIs Inclusion criteria: mildly asthmatic adults ‐ "mildly asthmatic" Exclusion criteria: not reported Percentage withdrawn: no drop‐out Other allowed medication: not reported |
|
| Interventions |
Face‐to‐face training: personal instruction by 1 of 2 pharmacists on use of the inhaler while in the physician's office Video training: Participants watched a videotaped programme of instruction produced by investigators No training: received only an information sheet reflecting the manufacturer's direction and the current literature |
|
| Outcomes |
Outcomes measured: inhaler technique/effectiveness of instruction Technique assessment method used: 10‐point checklist with equal weight items assessed by the physician |
|
| Notes |
Type of publication: single peer‐reviewed journal article Funding: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "We randomly assigned 29 mildly asthmatic adults" ‐ no further details |
| Allocation concealment (selection bias) | Unclear risk | No details |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No description of procedures intended to blind participants or personnel to group assignment |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Inhaler technique was assessed by a "specially trained technician". This was not the person who delivered the intervention, but it is not clear if this person knew to which group each participant belonged |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No drop‐out |
| Selective reporting (reporting bias) | Unclear risk | No prospective trial registration identified. Only outcome described in Methods (inhaler technique) is clearly reported, although control group is not followed up |
| Other bias | Low risk | None noted |
Shah 2014.
| Study characteristics | ||
| Methods |
Design: open‐label randomised trial; design not clearly reported Duration: not reported Setting: 1 hospital, Evanston, Illinois, USA Trial registration: not reported |
|
| Participants |
Population: 50 people with asthma randomised to computer training, written training or no training (n in each group not reported) Age: not reported Baseline asthma severity: not reported Inclusion criteria: not reported Exclusion criteria: not reported Percentage withdrawn: not reported Other allowed medication: not reported |
|
| Interventions |
Computer training: Participants completed a "computer based training solution" such as those at www.use‐inhalers.com Written training: "traditional written instruction on inhaler technique" No training: "our controls were patients without any training and patients given written training" |
|
| Outcomes |
Outcomes measured: inhaler technique Technique assessment method used: "videotapes of patients using their inhalers before and after training were created and analysed by a fixed rubric and given a score" |
|
| Notes |
Type of publication: conference abstract Funding: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "patients were recruited in a randomized, unblinded enrolment process." ‐ no further details |
| Allocation concealment (selection bias) | High risk | "randomized, unblinded enrolment process" ‐ implies that allocation was not concealed |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Described as 'unblinded' |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Described as 'unblinded', although 'Inhaler technique was assessed by "fixed rubric", which may have controlled for some bias, depending on who was making the assessment and whether they knew what sort of training the participant had received |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Drop‐out not reported |
| Selective reporting (reporting bias) | High risk | No prospective trial registration identified. Minimal details reported as conference abstract only |
| Other bias | Low risk | None noted |
Tarsin 2008.
| Study characteristics | ||
| Methods |
Design: parallel‐group randomised controlled trial; blinding not stated Duration: 4 weeks Setting: Tripoli, Libya. Setting not reported Trial registration: not reported |
|
| Participants |
Population: 76 people with asthma randomised to face‐to‐face verbal training + 2Tone training aid (n = 26) or face‐to‐face verbal training alone (n = 25) (those with correct MDI technique were used as a control group; others were randomised to 2 training groups relevant to this review) Age: not reported Baseline asthma severity: not reported Inclusion criteria: patients with asthma using MDI Exclusion criteria: not reported Percentage withdrawn: not reported Other allowed medication: not reported |
|
| Interventions |
Intervention summary: face‐to‐face verbal training + 2Tone training aid (no further details) Control summary: face‐to‐face verbal training alone (no further details) |
|
| Outcomes |
Outcomes measured: inhalation flow rate, FEV1, Jones Morbidity Index (JMI) and Juniper AQLQ Technique assessment method used: inhalation flow rate through MDI |
|
| Notes |
Type of publication: conference abstract Funding: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Described as 'randomised' but no details of sequence generation |
| Allocation concealment (selection bias) | Unclear risk | No details |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No description of procedures intended to blind participants or personnel to group assignment |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No description of procedures intended to blind participants or personnel to group assignment; for patient‐reported outcomes, such as QOL, the participant was the outcome assessor |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Drop ‐out not reported |
| Selective reporting (reporting bias) | High risk | No prospective trial registration identified. Minimal details reported as conference abstract only |
| Other bias | Low risk | None noted |
Toumas‐Shehata 2014.
| Study characteristics | ||
| Methods |
Design: parallel‐cluster repeated‐measures randomised controlled trial; blinding not stated Duration: 4 weeks Setting: 1 community pharmacy, Australia Trial registration: not reported |
|
| Participants |
Population: 19 pharmacists (101 adult patients) randomised to pharmacist training + quantitative inhaler feedback (51 patient participants) or to pharmacist training no quantitative feedback (50 patient participants) (control) Age: mean age not reported; age categories given (18 to > 60 years) Baseline asthma severity: mean (SD) ACQ score in intervention group: 1.6 (0.96), and in control group 1.7 (1.01) Inclusion criteria: diagnosis of asthma and aged 18 years or over; currently using a Turbuhaler (TH) or Accuhaler (ACC) for delivery of preventer asthma medication; having been on the same asthma medication and dose regimen for a minimum of 1 month Exclusion criteria: medication not self‐administered; inability to speak or understand English; inability to return for follow‐up visit; and/or involved in another clinical trial/study Percentage withdrawn: 6% of patient participants withdrew from the intervention group, and 2% from the control group Other allowed medication: not reported |
|
| Interventions |
Intervention summary: combination of qualitative and quantitative visual feedback for DPI inhalers. Training of community pharmacists occurred on an individual basis with the researcher delivering a 2‐hour 1‐on‐1 training session to each pharmacist in their own community pharmacy. Intervention group pharmacists were also trained as per a train‐the‐trainer approach and an established pharmacist‐training programme with an additional quantitative feedback process. Quantitative feedback involved the use of a portable hand‐held spirometer, which has been developed with the ability to assess breathing manoeuvres associated with the use of different inhaler devices. It is a preprogrammed device that can measure breathing manoeuvres and provides feedback in both numerical and visual/graphic forms. Actual breathing manoeuvres are then compared with optimal manoeuvres for a particular inhaler. This allows patients to see exactly where they are making errors and to what extent. A DVD showing HCPs delivering inhaler technique education to people with asthma was used to consolidate the training of pharmacists. Pharmacists also received an update on basic asthma management and inhaled medications Control summary: current best practice DPI inhaler technique education utilising qualitative visual feedback. Training of community pharmacists occurred on an individual basis, with the researcher delivering a 2‐hour 1‐on‐1 training session to each pharmacist in their own community pharmacy. Control group pharmacists were trained as per a train‐the‐trainer approach and an established pharmacist‐training programme. A DVD showing HCPs delivering inhaler technique education to people with asthma was used to consolidate the training of pharmacists. Pharmacists also received an update on basic asthma management and inhaled medications |
|
| Outcomes |
Outcomes measured: asthma control (ACQ), inhaler technique Technique assessment method used: The inhaler technique was assessed according to manufacturer‐approved checklists. Individuals were considered to use the correct technique if they were able to perform all steps in the checklist correctly. Inhaler technique data were represented in 2 ways: proportion of participants with correct technique and mean number of steps performed correctly for each device |
|
| Notes |
Type of publication: peer‐reviewed journal article Funding: This study was funded by the Australian Postgraduate Award. The DVD was funded through Australian Research Council Linkage Project LP LP0882737. Checklists were developed in collaboration with the National Prescribing Service, Sydney, Australia, through funding from the Australian Research Council Linkage Project LP LP0882737 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "19 community pharmacists were recruited and randomised" ‐ no further details |
| Allocation concealment (selection bias) | Unclear risk | No details |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No description of procedures intended to blind participants or personnel to group assignment |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | 'No description of procedures intended to blind outcome assessors to group allocation; therefore assessment of inhaler technique and asthma control may be at risk of detection bias |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Less than 10% drop‐out in both groups |
| Selective reporting (reporting bias) | Unclear risk | No prospective trial registration identified; all outcomes listed in methods reported |
| Other bias | Low risk | None noted |
Turgeon 1996.
| Study characteristics | ||
| Methods |
Design: single‐blind parallel‐group randomised controlled trial Duration: 26 weeks Setting: 1 asthma clinic in a paediatric hospital, Canada Trial registration: not reported |
|
| Participants |
Population: 96 children and adolescents with asthma randomised to nurse training: interactive with feedback (n = 47) or nurse training: pictorial only (n = 49) Age: median (range) age in the intervention group was 4.5 (0.75 to 15) years, and in the control group 5.75 (0.75 to 15) years Baseline asthma severity: in the intervention group: 57% mild; 32% moderate; 11% severe asthma; in the control group: 55% mild; 35% moderate; 10% severe asthma Inclusion criteria: children between 1 and 18 years of age starting aerosol therapy for the first time Exclusion criteria: younger than 1 year or older than 18 years, previous teaching session of technique of aerosol administration, language other than French or English, if another member of the family suffered from asthma and was using inhalers Percentage withdrawn: 43% of participants withdrew from both intervention and control arms Other allowed medication: not reported |
|
| Interventions |
Intervention summary: Experimental participants received an interactive teaching session from the asthma clinic nurse that lasted about 15 minutes. Instruction was given with picture diagrams provided with inhalation devices by pharmaceutical companies. This was followed by interactive teaching consisting of immediate correction of faulty technique displayed by the child and/or parent. All participants received 2 teaching sessions at initial and 1‐month visits. Devices were MDIs with an Aerochamber, Nebuhaler or Venthaler and DPIs with Diskhaler or Turbuhaler Control summary: Control participants received instruction only by picture diagrams (didactic teaching) given by another nurse, who had no contact with the experimental group. All participants received 2 teaching sessions at initial and 1‐month visits |
|
| Outcomes |
Outcomes measured: technical ability in inhalation and Likert scales for parental perceptions of treatment at 1, 3 and 6 months (end of study); morbidity assessed at baseline and at 6 months; morbidity evaluated by a questionnaire derived from Beck et al, including number of asthma attacks, number of hospitalisations and duration of stay, number of ED visits, numbers of missed school days and disability days (unable to perform usual activities) Technique assessment method used: assessed by research assistant through direct observation of the child and/or parent administering a placebo aerosol. Score was calculated by using a checklist of essential steps of the technique ‐ 1 point for each correct step. Number of steps differed between devices, so scores were converted into percentages |
|
| Notes |
Type of publication: single peer‐reviewed journal article Funding: supported by the 'Fondation de l'Hopital Sainte‐Justine' through special funding from the Fonds de la Recherche en Sante de Quebec (FRSQ) and the Interservice Club Council (Telethon of Stars) granted to the Group in Evaluative, Clinical and Epidemiologic Research at the Ste‐Justine Hospital Research Center |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Patients were randomised into experimental and control groups using a computer generated list of random numbers" |
| Allocation concealment (selection bias) | Unclear risk | No details |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No description of procedures intended to blind participants or personnel to group assignment |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Participants were evaluated by a research assistant who was blind to the teaching assignment group at baseline and follow‐up visits, and inhalation technique assessed by this person was the main outcome reported. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | More than 40% dropped out from both arms; although they are reported to not differ significantly from those who completed in terms of baseline demographics, reason for drop ‐out is not given and no flow diagram is presented. No ITT analysis/adjustment for attrition is described |
| Selective reporting (reporting bias) | High risk | No prospective trial registration identified. 'Morbidity indices' were collected during follow ‐up (e.g. number of attacks, hospitalisation and days of school missed) but were not fully reported, so could not be included in the meta‐analysis |
| Other bias | Low risk | None noted |
Vitari 2013.
| Study characteristics | ||
| Methods |
Design: parallel‐group randomised controlled trial; blinding not stated Duration: 4 weeks Setting: Comprehensive Lung Center, Pittsburgh, Pennsylvania, USA Trial registration: not reported |
|
| Participants |
Population: 43 people with asthma randomised to face‐to‐face demonstration + in‐check simulator (n = 22) or face‐to‐face demonstration (n = 21) Age: not reported Baseline asthma severity: not reported Inclusion criteria: people with asthma new to the Comprehensive Lung Center Exclusion criteria: not reported Percentage withdrawn: 5% of participants withdrew from the intervention arm, and 10% from the control arm Other allowed medication: not reported |
|
| Interventions |
Intervention summary: usual teaching with demonstrator models plus In‐Check to simulate resistance and measure inspiratory flow for each specific inhaler used Control summary: usual teaching with demonstrator models |
|
| Outcomes |
Outcomes measured: inspiratory flow, number of correct steps met Technique assessment method used: In‐Check inspiratory flow |
|
| Notes |
Type of publication: conference abstract Funding: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Twenty‐one subjects were randomized to traditional teaching (control arm) while 22 received In‐Check" ‐ no further details |
| Allocation concealment (selection bias) | Unclear risk | No details |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No description of procedures intended to blind participants or personnel to group assignment |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | 'No description of procedures intended to blind outcome assessors to group allocation but the IN‐CHECK device provides an objective measure of inhalation technique" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Less than 10% drop ‐out in both groups |
| Selective reporting (reporting bias) | High risk | No prospective trial registration identified. Minimal details as reported as conference abstract only |
| Other bias | Low risk | None noted |
ACQ: Asthma Control Questionnaire; ACT: Asthma Control Test; AQLQ: Asthma Quality of Life Questionnaire; AQOL: asthma quality of life; BAI: breath‐activated inhaler; BTS:British Thoracic Society; DPI: dry powder inhaler; ED: emergency department; FEV1: forced expiratory volume in one second; FVC: forced vital capacity; GINA: Global Initiative for Asthma; HCP: healthcare practitioner; ICS: inhaled corticosteroids; IF: inspiratory flow; ITT: intention‐to‐treat; IVC: inspiratory vital capacity; JMI: Jones Morbidity Index; LABA: long‐acting beta2‐agonist; MDI: metered dose inhaler; MTS: multi‐media touch screen system; PACQLQ: PAQLQ completed by parents of children; PAQLQ: Paediatric Asthma Quality of Life Questionnaire; PEFR: peak expiratory flow rate; PIF: peak inspiratory flow; PIL: patient information leaflet; pMDI: pressurised metered dose inhaler; QOL: quality of life; RA: research assistant; SD: standard deviation; TH: Trainhaler; VC: verbal counselling.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Andres Jacome 2003 | Not an RCT |
| Azouz 2015 | Cross‐over study performed during 1 clinic visit. Participants used 2 different inhaler types in a randomised order before and after normal, and then enhanced training with the IN‐CHECK device. Before‐and‐after data presented only |
| Basheti 2005a | Intervention delivered to pharmacists; focus was pharmacists' knowledge rather than participant outcomes |
| Bosnic‐Anticevich 2010 | Mixed population with asthma and COPD; no disaggregated data presented |
| Compton 2000 | Healthy participants |
| Eakin 2015 | Preliminary observational findings from a complex educational intervention. Primary focus of intervention not inhaler technique |
| Epstein 2001 | Not an RCT |
| Eriksson 1980 | Trial of impact of spacer delivery on bronchodilatation outcomes |
| Fornell 2014 | Primary focus of intervention not inhaler technique |
| Garcia‐Cardenas 2013 | Primary focus of intervention not inhaler technique |
| Grover 2016 | Primary focus of intervention not inhaler technique |
| Hesselink 2004 | Mixed population with asthma and COPD; no disaggregated data presented |
| Hodges 1981 | Trial of impact of spacer delivery on bronchodilatation outcomes |
| Horner 2008 | Primary focus of intervention not inhaler technique |
| Jolly 2012 | Not stated that participants had asthma; likely mixed population with asthma and COPD judging by age and sex of participants |
| Jolly 2015 | Mixed population with asthma and COPD; no disaggregated data |
| Kritikos 2007 | Primary focus of intervention not inhaler technique |
| Lee 2010 | Not an RCT |
| McElnay 1989 | Randomised portion of trial involved healthy volunteers |
| Mulloy 1996 | Primary focus of intervention not inhaler technique |
| NCT01426581 | Mixed population with asthma and COPD; no disaggregated data |
| NCT01456494 | Mixed population with asthma and COPD; no disaggregated data |
| NCT01641211 | Subanalysis of a larger trial investigating a multi‐faceted intervention to improve asthma management in older adults. Primary focus of intervention not inhaler technique |
| NCT02046759 | Primary focus of intervention not inhaler technique |
| NCT02307669 | Primary focus of intervention not inhaler technique |
| NCT02363192 | Primary focus of intervention not inhaler technique |
| NCT02715219 | Primary focus of intervention not inhaler technique |
| Pedersen 1983 | Primary focus of intervention not inhaler technique |
| Poureslami 2016 | Primary focus of intervention not inhaler technique |
| Rachelefsky 1986 | Cross‐over study of spacer drug delivery |
| Reiser 1986 | Cross‐over study primarily assessing impact of spacer delivery on lung function |
| Sandos Dde 2010 | Not an RCT |
| Schacer 2005 | Control group but no mention of random allocation |
| Tuazon 2002 | Primary focus of intervention not inhaler technique |
| Verver 1996 | Mixed population with asthma and COPD; no disaggregated data |
| WIlliams 1983 | Not an RCT ‐ children used as their own controls |
| Wong 1995 | Trial of impact of spacer delivery on bronchodilatation outcomes |
| Yoon 1993 | Primary focus of intervention not inhaler technique |
COPD: chronic obstructive pulmonary disease; RCT: randomised controlled trial.
Characteristics of studies awaiting classification [ordered by study ID]
NCT02062463.
| Methods | Open‐label parallel‐group randomised controlled trial |
| Participants | Adults with asthma aged 18 to 75 years receiving step 3 or 4 therapy for asthma as defined by British Thoracic Society (BTS) guidelines (daily doses of BDP‐equivalent ICS ≥ 800 mcg to 2000 mcg as part of fixed or free combinations with long‐acting beta‐agonists (LABAs)) |
| Interventions | Comparison of inhaler technique mastery of Spiromax vs Symbicort Turbohaler |
| Outcomes | Critical and number of errors, adherence, patient satisfaction, exacerbations, change in asthma treatment, adverse events |
| Notes | Study reported as completed in March 2015, but no study results posted on clinicaltrial.gov; we are unable to link record to a full‐text publication |
Westhus 1998.
| Methods | Quasi‐experimental study; a convenience sample of children were "randomly assigned to one of two equal groups" |
| Participants | Children (7 to 12 years of age) with asthma; sample included 154 children (African American and Caucasian) |
| Interventions | Mnemonic device to assist in learning to use the MDI (3 colourful cards with keywords and animated pictures representing MDI use) |
| Outcomes | At 2 points in time, participants answered demographic and medical history questions, had their inhaler technique evaluated, received mnemonic or standard instructions and performed pulmonary function tests. An inhaler checklist measured skill in MDI use |
| Notes | Not clear from the abstract whether this is a truly randomised study. Attempted to contact NK Westhus (lead author) via the University of St Louis; email sent on 26 August 2016; no response received at the time of publication |
BDP: beclomethasone dipropionate; BTS: British Thoracic Society; ICS inhaled corticosteroids; LABA: long‐acting beta‐agonist; MDI: metered dose inhaler.
Characteristics of ongoing studies [ordered by study ID]
ACTRN12610000159055.
| Study name | Assessing the effectiveness of Inhaler Technique Labels on asthma patients' inhaler technique |
| Methods | Parallel‐group randomised controlled trial |
| Participants | People aged 14 to 85 years with a doctor diagnosis of asthma, currently using inhaled corticosteroids with or without long‐acting beta‐agonists via Turbuhaler or Diskus, who have been on the same asthma medication and dose for a minimum of 1 month before study enrolment. Planned recruitment 214 participants |
| Interventions | Inhaler technique labels used as part of inhaler technique education (verbal plus physical demonstration) compared with inhaler technique education alone |
| Outcomes | Inhaler technique, asthma control (using Asthma Control Test) |
| Starting date | 01/08/2009 |
| Contact information | Dr Iman Amin Basheti
940344
Amman
11194
Jordan Email: ibasheti@usyd.edu.au |
| Notes | Listed as 'active but not recruiting'. Unable to link to a full‐text publication |
JPRN‐UMIN000006739.
| Study name | The relationship between asthma management and inhaler technique training |
| Methods | Parallel‐group randomised controlled trial |
| Participants | Adults with asthma aged 20 years and older with an ACT score under 24. Planned recruitment 90 participants |
| Interventions | No inhaler technique training vs inhaler technique training vs inhaler technique training and education |
| Outcomes | Adherence, ACT, FEV1, FeNO |
| Starting date | 01/11/2011 |
| Contact information | Kumiya Sugiyama 880 Kita‐kobayashi Mibu Tochigi 321‐0293 Japan Email: sugiyama@dokkyomed.ac.jp |
| Notes | Status listed as 'enrolling by invitation'. Unable to link to a full‐text publication |
NCT01529697.
| Study name | A protocol for a randomised clinical trial of the effect of providing feedback on inhaler technique and adherence from an electronic device in patients with poorly controlled severe asthma |
| Methods | Single‐blind prospective parallel‐group randomised clinical trial |
| Participants | Patients with partially controlled or uncontrolled severe asthma who have also had at least 1 severe asthma exacerbation in the prior year are eligible to participate. Planned recruitment 220 participants |
| Interventions | Active group will receive feedback on their inhaler technique and adherence with the new device over a 3‐month period. Control group will also receive training in inhaler technique and strategies to promote adherence, but no feedback from the device |
| Outcomes | Adherence, inhaler technique, number who remain poorly controlled despite appropriate technique |
| Starting date | 2011 |
| Contact information | Imran Sulaiman Email: imransulaiman@rcsi.ie |
| Notes |
NCT02203266.
| Study name | A randomised, parallel‐group, multi‐centre trial using a novel 'INCA' Tracker Device to measure and monitor compliance and technique of Seretide Diskus inhaler in a community pharmacy setting |
| Methods | Open‐label parallel‐group randomised controlled trial |
| Participants | Adults with asthma or COPD aged 18 years or older with a valid prescription for Seretide Diskus inhaler or currently using a Seretide Diskus inhaler. Planned recruitment 200 participants |
| Interventions | Feedback on the participant's own inhaler use, with personalised information on participant technique and timing of use of the Diskus inhaler as recorded on the INCA device, will be provided to participants in the feedback group after 1, 2 and 6 months vs current best practice inhaler technique education |
| Outcomes | Adherence, inhaler technique, rescue inhaled medication use, rescue antibiotic/steroid use, quality of life |
| Starting date | February 2014 |
| Contact information | Richard Costello Royal College of Surgeons Clinical Research Centre Beuamont Hospital Email: rcostello@rcsi.ie |
| Notes |
NCT02283008.
| Study name | Evaluating the efficacy of 2 different educational strategies for improving and maintaining inhaler technique |
| Methods | Open‐label parallel‐group randomised controlled trial |
| Participants | Adults aged 35 to 90 years whose regular treatment requires inhaled medication. They will be included regardless of age, disease, inhaler device used or cognition |
| Interventions | Structured education on the use of inhalers vs usual standard informal education |
| Outcomes | Inhaler technique |
| Starting date | December 2014 |
| Contact information | Steven Hickey, Respiratory Nurse Specialist Northampton General Hospital NHS Trust |
| Notes |
NCT02611531.
| Study name | Video vs Teach‐To‐Goal Respiratory Inhaler Technique Assessment and InstructioN (V‐TRaIN) |
| Methods | Single‐blind (outcomes assessor) parallel‐group randomised controlled trial |
| Participants | Adults aged 18 years and older, admitted to the inpatient medical service and surgical service with physician‐diagnosed COPD or asthma. We will enrol patients even if the primary reason for admission is not COPD or asthma (e.g. patients admitted for heart failure but with a physician diagnosis of COPD are eligible) |
| Interventions | Those in the TTG condition will be provided with an intensive, iterative education and evaluation strategy. Those in the video module education condition will be provided with a tablet device and instructions on how to complete video training and self‐assessment |
| Outcomes | Inhaler technique, symptoms, quality of life, self‐efficacy, healthcare utilisation, lung function |
| Starting date | November 2015 |
| Contact information | Susannah Butters Email: sbutters@medicine.bsd.uchicago.edu |
| Notes |
ACT: Asthma Control Test; COPD: chronic obstructive pulmonary disease; FeNO: fractional exhaled nitric oxide; FEV1: forced expiratory volume in one second; TTG: teach‐to‐goal.
Differences between protocol and review
As described, we were unable to perform most of our planned subgroup and sensitivity analyses owing to data paucity.
We planned to contact trial authors to ask for missing information, but owing to the number of included studies and the relatively small size of individual studies, we did not do so.
Contributions of authors
RN drafted the Background and Methods text, and KK provided substantial input and revisions. KK screened all references, and RN and AM screened half, each in duplicate. All review authors contributed to finalising the list of included studies through discussion. RN, KK and AM contributed to extraction of study characteristics, data and risk of bias assessments. RN entered characteristics and data into the review, and KK checked the data for accuracy. RN and KK interpreted results together and applied GRADE. RN, KK and AM contributed to writing sections of the Results and Discussion, and all review authors approved the final version of the manuscript.
Sources of support
Internal sources
-
St George's, University of London, UK
Kayleigh Kew and Rebecca Normansell received support in the form of salaries
External sources
-
National Institute of Health Research, UK
Evidence to guide care in adults and children with asthma, 13/89/14
This project was supported by the National Institute for Health Research (NIHR), via Cochrane Infrastructure, Cochrane Programme Grant or Cochrane Incentive funding to the Airways Group. The views and opinions expressed therein are those of the review authors and do not necessarily reflect those of the Systematic Reviews Programme, NIHR, NHS or the Department of Health
-
National Institute of Health Research, UK
AGM was funded by an NIHR Academic Clinical Fellowship in Respiratory Medicine
Declarations of interest
RN is the deputy co‐ordinating editor of Cochrane Airways and is a qualified general practitioner.
KK is funded to prepare Cochrane Reviews by a Programme Grant awarded by the NIHR to the Cochrane Airways Group.
AM is a clinician working in the area of respiratory medicine. He is funded by an Academic Clinical Fellowship in Respiratory Medicine from the NIHR.
Edited (no change to conclusions)
References
References to studies included in this review
Acosta 2009 {published data only}
- Acosta JF, Eckardt P, Negron D, Rubin D. Educational intervention in adult asthma: a randomized clinical trial to determine if adult patients with asthma can learn how to use a metered dose inhaler. Annals of Emergency Medicine 2009;54(3):S50. [1097-6760] [Google Scholar]
Agertoft 1998 {published data only}
- Agertoft L, Pedersen S. Importance of training for correct Turbuhaler use in preschool children. Acta Paediatrica 1998;87(8):842-7. [DOI] [PubMed] [Google Scholar]
Al‐Showair 2007 {published data only}
- Al-Sahowair RAM, Pearson SB, Chrystyn H. Two-tone trainer maintains a slow inhalation rate when using a metered dose inhaler (MDI) [Abstract]. European Respiratory Journal 2005;26:Abstract No. 416. [Google Scholar]
- Al-Showair RAM, Pearson SB, Chrystyn H. Maintenance of good inhalation technique for metered dose inhalers (MDIs) by using a two-tone trainer [Abstract]. In: American Thoracic Society 2005 International Conference; 2005 May 20-25; San Diego, California. 2005:[C33] [Poster: F28].
- Al-Showair RAM, Pearson SB, Chrystyn H. The potential of a 2Tone trainer to help patients use their metered-dose inhalers. Chest 2007;131(6):1776-82. [DOI] [PubMed] [Google Scholar]
Ammari 2013 {published data only}
- Ammari WG, Chrystyn H. Optimizing the inhalation flow and technique through metered dose inhalers of asthmatic adults and children attending a community pharmacy. Journal of Asthma 2013;50(5):505-13. [0277-0903] [DOI] [PubMed] [Google Scholar]
Ammari 2015 {published data only}
- Ammari WG, Toor S, Chetcuti P, Stephenson J, Chrystyn H. Evaluation of asthma control, parents' quality of life and preference between AeroChamber Plus and AeroChamber Plus Flow-Vu spacers in young children with asthma. Journal of Asthma 2015;52(3):301-7. [0277-0903] [DOI] [PubMed] [Google Scholar]
Ammari 2015a {published data only}
- Ammari WG, Al-Hyari NK, Obeidat N, Khater M, Sabouba A, Sanders M. Improving paediatrics' pressurised metered dose inhaler technique and asthma control: Inhaler verbal counselling vs. trainhaler. Thorax 2015;70:A125-6. [Google Scholar]
Arthurs 2014 {published data only}
- Arthurs S, Khan R, Yasin F, Cahalane E, Cournane J, Browne B, O'Shea R et al. Comparison of two methods of inhaler technique instruction in children. Irish Journal of Medical Science 2014;183(11):S522-3. [0021-1265] [Google Scholar]
Basheti 2005 {published data only}
- Basheti I, Armour CL, Reddel HK, Bosnic Anticevich SZ. A pilot study of the effect of three educational interventions on Turbuhaler technique in community pharmacy. Respirology 2002;7:A37 Abstract number (P91). [1440-1843] [Google Scholar]
- Basheti IA, Reddel HK, Armour CL, Bosnic-Anticevich SZ. Counseling about turbuhaler technique: needs assessment and effective strategies for community pharmacists. Respiratory Care 2005;50(5):617-23. [PubMed] [Google Scholar]
Basheti 2008 {published data only}
- Basheti IA, Armour CL, Bosnic-Anticevich SZ, Reddel HK. Evaluation of a novel educational strategy, including inhaler-based reminder labels, to improve asthma inhaler technique. Patient Education and Counseling 2008;72(1):26-33. [DOI] [PubMed] [Google Scholar]
- Basheti IA, Reddel HK, Armour CL, Bosnic-Anticevich SZ. Impact of inhaler technique: improved asthma outcomes with a simple intervention by community pharmacists. Respirology 2006;11:Abstract no. 212. [1440-1843] [DOI] [PubMed] [Google Scholar]
- Basheti IA, Reddel HK, Armour CL, Bosnic-Anticevich SZ. Improved asthma outcomes with a simple inhaler technique intervention by community pharmacists. Journal of Allergy and Clinical Immunology 2007;119(6):1537-8. [DOI] [PubMed] [Google Scholar]
- Reddel HK, Basheti IA, Armour CL, Bosnic-Anticevich SZ. The impact of correcting inhaler technique: improved asthma outcomes with a simple intervention by community pharmacists [Abstract]. In: American Thoracic Society International Conference; 2006 May 19-24; San Diego. 2006:A269. [1943-5665]
Boone 2002 {published data only}
- Boone D, Counsell P, Dobson C, Baker EH. Effect of computer-assisted education on inhaler technique and knowledge in children with asthma [abstract]. European Respiratory Journal 2002;20:331s. [Google Scholar]
Bynum 2001 {published data only}
- Bynum A, Hopkins D, Thomas A, Copeland N, Irwin C. The effect of telepharmacy counseling on metered-dose inhaler technique among adolescents with asthma in rural Arkansas. Telemedicine Journal and e-health 2001;7(3):207-17. [DOI] [PubMed] [Google Scholar]
Carpenter 2015 {published data only}
- Carpenter D, Geryk L, Blalock S, Lee C, Weaver M, Reuland D et al. Using videos to improve children's inhaler technique: a randomized controlled trial. Journal of the American Pharmacists Association 2014;54(2):e99-e100. [1544-3191] [Google Scholar]
- Carpenter DM, Lee C, Blalock SJ, Weaver M, Reuland D, Coyne-Beasley T et al. Using videos to teach children inhaler technique: a pilot randomized controlled trial. Journal of Asthma 2015;52(1):81-7. [0277-0903] [DOI] [PMC free article] [PubMed] [Google Scholar]
Donateo 1996 {published data only}
- Donateo L, Gerardi R, Cantini L. A new spacer device for administration of inhaled salbutamol: use in elderly asthmatics. Advances in Therapy 1996;13(5):292-300. [0741-238X] [PubMed] [Google Scholar]
Fernandes 2011 {published data only}
- Fernandes L, Mesquita A. Improving asthma control with therapeutic education intervention [Abstract]. European Respiratory Journal 2011;38(55):913s [P4997]. [CN-00833621] [Google Scholar]
Goodyer 2006 {published data only}
- Goodyer L, Savage I, Dikmen Z. Inhaler technique in Turkish people with poor English: a case of information discrimination? Pharmacy World and Science 2006;28(2):107-14. [0928-1231] [DOI] [PubMed] [Google Scholar]
Lirsac 1991 {published data only}
- Lirsac B, Braunstein G. Randomised evaluation of two teaching methods using aerosol dosers (French). Revue des Maladies Respiratoires 1991;8(6):559-65. [1776-2588] [PubMed] [Google Scholar]
Mehuys 2008 {published data only}
- Mehuys E, Van Bortel L, De Bolle L, Van Tongelen I, Remon J-P, Annemans L et al. [Does pharmacist intervention lead to appropriate use of asthma medication and improved asthma control?]. Farmaceutisch Tijdschrift voor Belgie 2008;85(1):1-9. [0771-2367] [Google Scholar]
- Mehuys E, Van Bortel L, De Bolle L, Van Tongelen I, Remon J-P, Annemans L et al. Effectiveness of pharmacist intervention for asthma control improvement. European Respiratory Journal 2008;31(4):790-9. [DOI] [PubMed] [Google Scholar]
Nahafizadeh 2010 {published data only}
- Najafizadeh K, Rostami SK, Ghorbani F, Khoddami HR. The effect of face to face education about proper use of metered dose inhaler on asthma control [Abstract]. In: European Respiratory Society Annual Congress, Barcelona, Spain, 2010 September 18-22. 2010:[P3992].
Ozkaya 2010 {published data only}
- Ozkaya E, Samanci N, Guler N. Evaluation of the standardized MDI-spacer checklist on pediatric asthma management. Journal of Asthma and Allergy Educators 2010;1(4):144-9. [Google Scholar]
Rahmati 2014 {published data only}
- Rahmati H, Ansarfard F, Ghodsbin F, Ghayumi MA, Sayadi M. The effect of training inhalation technique with or without spacer on maximum expiratory flow rate and inhaler usage skills in asthmatic patients: a randomized controlled trial. International Journal of Community Based Nursing and Midwifery 2014;2(4):211-9. [2322-2476] [PMC free article] [PubMed] [Google Scholar]
Rydman 1999 {published data only}
- Rydman RJ, Sonenthal K, Tadimeti L, Butki N, McDermott MF, Laksminarayana T et al. Evaluating the outcome of two teaching methods of breath actuated inhaler in an inner city asthma clinic. Journal of Medical Systems 1999;23(5):349-56. [1573-689X] [DOI] [PubMed] [Google Scholar]
Savage 2003 {published data only}
- Savage I, Goodyer L. Providing information on metered dose inhaler technique: is multimedia as effective as print? Family Practice 2003;20(5):552-7. [DOI] [PubMed] [Google Scholar]
Schultz 2012 {published data only}
- Schultz A, Sly PD, Zhang G, Venter A, Le Souef PN, Devadason SG. Incentive device improves spacer technique but not clinical outcome in preschool children with asthma. Journal of Paediatrics and Child Health 2012;48(1):52-6. [1440-1754] [DOI] [PMC free article] [PubMed] [Google Scholar]
Self 1983 {published data only}
- Self TH, Brooks JB, Lieberman P, Ryan MR. The value of demonstration and role of the pharmacist in teaching the correct use of pressurized bronchodilators. Canadian Medical Association Journal 1983;128(2):129-31. [PMC free article] [PubMed] [Google Scholar]
Shah 2014 {published data only}
- Shah R, Shah R. Effectiveness of computer based interactive training on inhaler technique and clinical outcomes in asthma patients (Abstract). American Journal of Respiratory and Critical Care Medicine 2014;189:A6707. [Google Scholar]
- Shah R, Velez L. Effectiveness of software-based patient education on inhaler technique: a clinical study [Abstract]. European Respiratory Journal 2014;44:4824. [Google Scholar]
Tarsin 2008 {published data only}
- Tarsin W, Hshad NE, lshamli I, Soussi M, Chrystyn H. Training patients on how to use metered dose inhaler (MDI) by using the 2Tone will improve asthma quality of life (AQOL) [Abstract]. In: European Respiratory Society Annual Congress, Berlin, Germany, 2008 October 4-8. 2008:[E4638].
Toumas‐Shehata 2014 {published data only}
- Toumas-Shehata M, Price D, Basheti I, Bosnic-Anticevich S. Exploring the role of feedback in inhaler technique education [Abstract]. Respirology 2014;19(S2):25 [TO 037]. [1440-1843] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toumas-Shehata M, Price D, Basheti I, Bosnic-Anticevich S. Exploring the role of quantitative feedback in inhaler technique education: a cluster-randomised, two-arm, parallel-group, repeated-measures study. NPJ Primary Care Respiratory Medicine 2014;24:14071. [ES:2055-1010: IL:2055-1010] [DOI] [PMC free article] [PubMed] [Google Scholar]
Turgeon 1996 {published data only}
- Turgeon JP, St-Laurent-Gagnon T, Chabot G, Allard-Dansereau C, Gaudreault P, Thivierge RL et al. Teaching inhalation techniques to asthmatic children: a randomized clinical trial. Ambulatory Child Health 1996;1(3):205-13. [Google Scholar]
Vitari 2013 {published data only}
- Vitari CA, Holguin F, Wenzel SE, Landsittel D. Pilot study to evaluate inhaler technique using the in-check™. American Journal of Respiratory and Critical Care Medicine 2013;187:A1279. [Google Scholar]
References to studies excluded from this review
Andres Jacome 2003 {published data only}
- Andres JJ, Inesta GA. Prospective study about the impact of a community pharmaceutical care service in patients with asthma. [Spanish]. Revista Espanola de Salud Publica 2003;77(3):393-403. [PubMed] [Google Scholar]
Azouz 2015 {published data only}
- Azouz W, Chetcuti P, Hosker H, Saralaya D, Chrystyn H. Enhanced training on how to use a dry powder inhaler (DPI) improves the inhalation manoeuvre (IM) of patients with asthma (child 6â□“17 yrs and adult >17 yrs) or COPD and in healthy adults (HA) when they use a Spiromax® (S) and Turbuhaler® (T) DPI [Abstract]. In: European Respiratory Society Annual Congress; 2013 Sept 7-11; Barcelona. Vol. 42. 2013:126s [P693].
- Azouz W, Chetcuti P, Hosker H, Saralaya D, Chrystyn H. Inhalation characteristics of asthma patients, COPD patients and healthy volunteers with the Spiromax(R) and Turbuhaler(R) devices: a randomised, cross-over study. BMC Pulmonary Medicine 2015;15(1):47. [1471-2466] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chrystyn H, Azouz W, Chetcuti P, Hosker H, Saralaya D. Inhalation characteristics with spiromax® and turbuhaler® dry powder inhalers (DPI) in healthy adults and patients with asthma or chronic obstructive pulmonary disease (COPD): before and after enhanced training [Abstract]. In: 7th International Primary Care Respiratory Group (IPCRG) World Conference; 2014 May 21-24; Athens. Vol. 0. 2014:OR-079.
- Chrystyn H, Azouz W, Chetcuti P, Hosker H. Inhalation characteristics with spiromax® and turbuhaler® dry powder inhalers (DPI) in healthy adults and patients with asthma or chronic obstructive pulmonary disease (COPD): before and after enhanced training [Abstract]. Thorax 2013;0:A178 [P226]. [Google Scholar]
Basheti 2005a {published data only}
- Basheti I, Reddel H, Armour C, Bosnic-Anticevich S. Educating community pharmacists correct PFM and inhaler technique for two different inhaler devices [Abstract]. Respirology 2005;10:A37. [1440-1843] [Google Scholar]
Bosnic‐Anticevich 2010 {published data only}
- Bosnic-Anticevich SZ, Sinha H, So S, Reddel HK. Metered-dose inhaler technique: the effect of two educational interventions delivered in community pharmacy over time. Journal of Asthma 2010;47(3):251-6. [DOI] [PubMed] [Google Scholar]
Compton 2000 {published data only}
- Crompton GK, Dewar MH, Allbutt H, MInnes JA. Inhaler preference and technique in inhaler naive subjects; a comparison of HFA and conventional devices. Thorax 2000;55:A61. [Google Scholar]
Eakin 2015 {published data only}
- Eakin MN, Ruvalcaba E, Rand CS, Riekert KA. Poor asthma medication management among urban preschool children. American Journal of Respiratory and Critical Care Medicine 2015;191:A3632. [Google Scholar]
Epstein 2001 {published data only}
- Epstein S, Maidenberg A, Hallett D, Khan K, Chapman KR. Patient handling of a dry-powder inhaler in clinical practice. Chest 2001;120(5):1480-4. [DOI] [PubMed] [Google Scholar]
Eriksson 1980 {published data only}
- Eriksson NE, Haglind K, Hidinger KG. A new inhalation technique for freon aerosols. Terbutaline aerosol with a tube extension in a 2-day cross-over comparison with salbutamol aerosol. Allergy 1980;35(7):617-22. [DOI] [PubMed] [Google Scholar]
Fornell 2014 {published data only}
- Fornell LL, Escriche XF, Álvarez SÁ, Francitorra ME, Fernández EA, Manrique CA et al. Can we improve the follow up of asthmatic patients with asthma educational program (PAMA)? [Abstract]. European Respiratory Journal 2014;44:P3021. [Google Scholar]
Garcia‐Cardenas 2013 {published data only}
- Garcia-Cardenas V, Sabater-Hernandez D, Kenny P, Martinez-Martinez F, Faus MJ, Benrimoj SI. Effect of a pharmacist intervention on asthma control. A cluster randomised trial. Respiratory Medicine 2013;107(9):1346-55. [DOI] [PubMed] [Google Scholar]
Grover 2016 {published data only}
- Grover C, Goel N, Armour C, Van Asperen PP, Gaur SN, Moles RJ et al. Medication education program for Indian children with asthma: a feasibility study. Nigerian Journal of Clinical Practice 2016;19(1):76-84. [1119-3077] [DOI] [PubMed] [Google Scholar]
Hesselink 2004 {published data only}
- Hesselink AE, Penninx BW, Windt DA, Duin BJ, Vries P, Twisk JW et al. Effectiveness of an education programme by a general practice assistant for asthma and COPD patients: results from a randomised controlled trial. Patient Education and Counseling 2004;55(1):121-8. [0738-3991] [DOI] [PubMed] [Google Scholar]
Hodges 1981 {published data only}
- Hodges IG, Milner AD, Stokes GM. Assessment of a new device for delivering aerosol drugs to asthmatic children. Archives of Disease in Childhood 1981;56(10):787-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Horner 2008 {published data only}
- Horner SD, Fouladi RT. Improvement of rural children's asthma self-management by lay health educators. Journal of School Health 2008;78(9):506-13. [0022-4391] [DOI] [PMC free article] [PubMed] [Google Scholar]
Jolly 2012 {published data only}
- Jolly GP, Mahmood A, Mohan A, Pandey RM. Evaluation of inhaler usage technique and response to educational training in a tertiary health care centre [Abstract]. American Journal of Respiratory and Critical Care Medicine 2012;185:A3328. [Google Scholar]
Jolly 2015 {published data only}
- Jolly GP, Mohan A, Guleria R, Poulose R, George J. Evaluation of metered dose inhaler use technique and response to educational training. Indian Journal of Chest Diseases and Allied Sciences 2015;57(1):17-20. [PubMed] [Google Scholar]
Kritikos 2007 {published data only}
- Kritikos V, Armour CL, Bosnic-Anticevich SZ. Interactive small-group asthma education in the community pharmacy setting: a pilot study. Journal of Asthma 2007;44(1):57-64. [0277-0903] [DOI] [PubMed] [Google Scholar]
Lee 2010 {published data only}
- Lee JK, Yang YH. [Evaluation of an education program for patients with asthma who use inhalers]. [Korean]. Journal of Korean Academy of Nursing 2010;40(2):202-12. [2005-3673] [DOI] [PubMed] [Google Scholar]
McElnay 1989 {published data only}
- McElnay JC, Scott MG, Armstrong AP, Stanford CF. Audiovisual demonstration for patient counselling in the use of pressurised aerosol bronchodilator inhalers. Journal of Clinical Pharmacy and Therapeutics 1989;14(2):135-44. [DOI] [PubMed] [Google Scholar]
Mulloy 1996 {published data only}
- Mulloy E, Donaghy D, Quigley C, McNicholas WT. A one-year prospective audit of an asthma education programme in an out-patient setting. Irish Medical Journal 1996;89(6):226-8. [PubMed] [Google Scholar]
NCT01426581 {published data only}
- NCT01426581. Effectiveness of interventions to teach respiratory inhaler techNique (E-TRaIN). clinicaltrials.gov/show/NCT01426581 (first received 29 August 2011).
- Press VG, Arora V, Constantine KL, Naureckas ET, White SR, Krishnan J. Forget me not: a randomized trial of the durability of hospital-based education on inhalers for patients with COPD or asthma. Journal of General Internal Medicine 2014;29:S102. [0884-8734] [Google Scholar]
- Press VG, Arora VM, Constantine K, Naureckas E, White SR, Krishnan JA. Effectiveness of teaching respiratory inhaler technique (E-TRaIN): a randomized trial. American Journal of Respiratory and Critical Care Medicine 2013;187:A5022. [Google Scholar]
- Press VG, Arora VM, Trela KC, Adhikari R, Zadravecz FJ, Liao C et al. Effectiveness of interventions to teach metered-dose and Diskus(R) inhaler technique: a randomized trial. In: Annals of the American Thoracic Society. Vol. 0. 2016. [---: - 2325-6621 (Electronic) - 2325-6621 (Linking)] [DOI] [PMC free article] [PubMed]
NCT01456494 {published data only}
- NCT01456494. Teaching use of respiratory inhalers (TURI). clinicaltrials.gov/show/NCT01456494 (first received 14 October 2011).
- Press VG, Arora VM, Shah LM, Lewis SL, Charbeneau J, Naureckas ET et al. Teaching the use of respiratory inhalers to hospitalized patients with asthma or COPD: a randomized trial. Journal of General Internal Medicine 2012;27(10):1317-25. [0884-8734] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Press VG, Naureckas E, Shah LM, Lewis SL, Charbeneau JT, Starkey J et al. A randomized clinical trial testing teach-to-goal vs. brief intervention for teaching hospitalized patients with asthma or chronic obstructive lung disease (COPD) effective inhaler use [Abstract]. American Journal of Respiratory and Critical Care Medicine 2011;183(1):A2263. [Google Scholar]
NCT01641211 {published data only}
- Crane MA, Douglass JA, Goeman DP, Jenkins CR. Inhaler technique education for older people [Abstract]. Respirology 2012;17:47. [1440-1843] [Google Scholar]
- Crane MA, Jenkins CR, Goeman DP, Douglass JA. Inhaler device technique can be improved in older adults through tailored education: findings from a randomised controlled trial. NPJ Primary Care Respiratory Medicine 2014;24:14034. [ES:2055-1010: IL:2055-1010] [DOI] [PMC free article] [PubMed] [Google Scholar]
- NCT01641211. ENLaCE pilot study [Using MEDUCATION to improve asthma medication device technique]. clinicaltrials.gov/show/NCT01641211 (first received 9 July 2012).
NCT02046759 {published data only}
- NCT02046759. A comparative study of an integrated pharmaceutical care plan and a routine care in bronchial asthma. clinicaltrials.gov/show/NCT02046759 (first received 24 January 2014).
NCT02307669 {published data only}
- NCT02307669. Inhaler adherence in severe unstable asthma (INCA-SUN) [A study on inhaler adherence to improve poor asthma control]. clinicaltrials.gov/show/NCT02307669 (first received 21 April 2014).
NCT02363192 {published data only}
- NCT02363192. Effectiveness of pharmacist interventions in difficult asthma [The effectiveness of pharmacist interventions in improving asthma control and quality of life in patients with difficult asthma]. clinicaltrials.gov/show/NCT02363192 (first received 9 February 2015).
NCT02715219 {published data only}
- NCT02715219. Effectiveness of an AEP on patient's knowledge, medication adherence and inhaler technique [Effectiveness of an asthma education programme on patient's knowledge, medication adherence and inhaler technique: randomized control trial]. clinicaltrials.gov/show/NCT02715219 (first accessed 25 February 2016).
Pedersen 1983 {published data only}
- Pedersen S. Aerosol treatment of bronchoconstriction in children, with or without a tube spacer. New England Journal of Medicine 1983;308(22):1328-30. [CN-00469229] [DOI] [PubMed] [Google Scholar]
Poureslami 2016 {published data only}
- Poureslami I, Shum J, Nimmon L, FitzGerald JM. Culturally specific evaluation of inhaler techniques in asthma. Respiratory Care 2016;61(12):1588-96. [PMID: ] [DOI] [PubMed] [Google Scholar]
Rachelefsky 1986 {published data only}
- Rachelefsky GS, Rohr AS, Wo J, Gracey V, Spector SL, Siegel SC et al. Use of a tube spacer to improve the efficacy of a metered-dose inhaler in asthmatic children. American Journal of Diseases of Children (1960) 1986;140(11):1191-3. [0002-922X] [DOI] [PubMed] [Google Scholar]
Reiser 1986 {published data only}
- Reiser J, Frame MH, Warner JO. The potential value of a 750-ml spacer for the administration of inhaled corticosteroids to children. Pediatric Pulmonology 1986;2(4):237-43. [DOI] [PubMed] [Google Scholar]
Sandos Dde 2010 {published data only}
- Santos Dde O, Martins MC, Cipriano SL, Pinto RM, Cukier A, Stelmach R. Pharmaceutical care for patients with persistent asthma: assessment of treatment compliance and use of inhaled medications. Jornal Brasileiro de Pneumologia 2010;36(1):14-22. [---: - 1806-3756 (Electronic) - 1806-3713 (Linking)] [DOI] [PubMed] [Google Scholar]
Schacer 2005 {published data only}
- Schacer C, Kraftt J, Karg M, Worth H. Role of a computer supported peak inspiratory flow guided inhalation training in patient education of adult asthmatics [Abstract]. In: American Thoracic Society 2005 International Conference; 2005 May 20-25; San Diego, California. Vol. 0. 2005:[A26] [Poster: 529].
Tuazon 2002 {published data only}
- Tuazon JA. Two years follow-up effects of asthma education programs on inhaler technique, health locus of control, self-efficacy and self-care behaviours. American Journal of Respiratory and Critical Care Medicine 2002;165:A420. [Google Scholar]
Verver 1996 {published data only}
- Verver S, Poelman M, Bögels A, Chisholm SL, Dekker FW. Effects of instruction by practice assistants on inhaler technique and respiratory symptoms of patients. A controlled randomized videotaped intervention study. Family Practice 1996;13(1):35-40. [DOI] [PubMed] [Google Scholar]
WIlliams 1983 {published data only}
- Williams RI Jr. Chamber assisted inhalant treatment (CAIR). Annals of Allergy 1983;51(3):371-3. [PubMed] [Google Scholar]
Wong 1995 {published data only}
- Wong C, Ayson M, Rajasingham S, Burgess C, Crane J. Efficacy of a simple DIY spacer with a metered dose inhaler in asthma. New Zealand Medical Journal 1995;108(1002):256-7. [ES:1175-8716: IL:0028-8446] [PubMed] [Google Scholar]
Yoon 1993 {published data only}
- Yoon R, McKenzie DK, Bauman A, Miles DA. Controlled trial evaluation of an asthma education programme for adults. Thorax 1993;48(11):1110-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
References to studies awaiting assessment
NCT02062463 {published data only}
- NCT02062463. Study to evaluate the mastery of inhaler technique for budesonide formoterol (BF) SPIROMAX® as compared to SYMBICORT® TURBOHALER® as treatment for adult patients with asthma (ELIOT) [A 12 week, randomized, open-label, parallel group study to evaluate the mastery of inhaler technique for budesonide formoterol (BF) SPIROMAX® (160/4.5 and 320/9 mcg) as compared to SYMBICORT® TURBOHALER® (200/6 and 400/12 mcg) as treatment for adult patients with asthma]. clinicaltrials.gov/show/NCT02062463 (first received 12 February 2014).
Westhus 1998 {published data only}
- Westhus NK. The test of a mnemonic device to help children with asthma learn to use a metered-dose inhaler [Dissertation]. Saint Louis University, Saint Louis, Missouri, 1998. [Google Scholar]
References to ongoing studies
ACTRN12610000159055 {published data only}
- ACTRN12610000159055. Improving health outcomes for Jordanian outpatients with asthma Improving health outcomes for Jordanian outpatients with asthma [Assessing the effectiveness of inhaler technique labels on asthma patients' inhaler technique]. apps.who.int/trialsearch/Trial2.aspx?TrialID=ACTRN12610000159055 (first received 18 February 2010).
JPRN‐UMIN000006739 {published data only}
- JPRN-UMIN000006739. The relationship between asthma management and inhaler technique training. apps.who.int/trialsearch/Trial2.aspx?TrialID=JPRN-UMIN000006739 (first received 17 November 2011).
NCT01529697 {published data only}
- NCT01529697. Prospective study of the feedback from an adherence monitor on asthma control. clinicaltrials.gov/show/NCT01529697 (first received 7 February 2012).
- Sulaiman I, Hale EM, Holmes M, Hughes C, D'Arcy S, Taylor T et al. A protocol for a randomised clinical trial of the effect of providing feedback on inhaler technique and adherence from an electronic device in patients with poorly controlled severe asthma. BMJ Open 2016;6(1):e009350. [2044-6055] [DOI] [PMC free article] [PubMed] [Google Scholar]
NCT02203266 {published data only}
- NCT02203266. Teaching inhaler use with the INCA device in a community pharmacy setting [A randomised, parallel-group, multi-centre trial using a novel INCA tracker device to measure and monitor compliance and technique of Seretide Diskus inhaler in a community pharmacy setting]. clinicaltrials.gov/show/NCT02203266 (first received 27 July 2014).
NCT02283008 {published data only}
- NCT02283008. Inhaler technique training [Evaluating the efficacy of 2 different educational strategies for improving and maintaining inhaler technique]. clinicaltrials.gov/show/NCT02283008 (first received 31 October 2014).
NCT02611531 {published data only}
- NCT02611531. Video vs. TTG respiratory inhaler technique assessment and InstructioN (V-TRaIN). clinicaltrials.gov/show/NCT02611531 (first received 18 November 2015).
Additional references
ADMIT 2016
- The Aerosol Drug Management Improvement Team. ADMIT. http://www.admit-online.info/index.php?id=342&L=0 (accessed 20 May 2016).
Al‐Jahdali 2013
- Al-Jahdali H, Ahmed A, Al-Harbi A, Khan M, Baharoon S, Bin Salih S et al. Improper inhaler technique is associated with poor asthma control and frequent emergency department visits. Allergy Asthma and Clinical Immunology 2013;9(1):8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Alotabi 2011
- Alotaibi S, Hassan WM, Alhashimi H. Concurrent use of metered dose inhalers without spacer and dry powder inhalers by asthmatic children adversely affect proper inhalation technique. Internet Journal of Pediatrics and Neonatology 2011;13(1):29. [DOI] [PMC free article] [PubMed] [Google Scholar]
Armour 2013
- Armour CL, Reddel HK, LeMay KS, Saini B, Smith LD, Bosnic-Anticevich SZ et al. Feasibility and effectiveness of an evidence-based asthma service in Australian community pharmacies: a pragmatic cluster randomized trial. Journal of Asthma 2013;50(3):302-9. [DOI] [PubMed] [Google Scholar]
Asher 2006
- Asher M, Montefort S, Björkstén B, Lai C, Strachan D, Weiland S et al. Worldwide time trends in the prevalence of symptoms of asthma, allergic rhinoconjunctivitis, and eczema in childhood: ISAAC Phases One and Three repeat multicountry cross-sectional surveys. Lancet 2006;368:733-43. [DOI] [PubMed] [Google Scholar]
Barnes 2003
- Barnes PJ, Adcock IM. How do corticosteroids work in asthma? Annals of Internal Medicine 2003;139(5 Pt 1):359-70. [DOI] [PubMed] [Google Scholar]
Bårnes 2015
- Barnes CB, Ulrik SC. Asthma and adherence to inhaled corticosteroids: current status and future perspectives. Respiratory Care 2015;60(3):455-68. [DOI] [PubMed] [Google Scholar]
Basheti 2009
- Basheti IA, Armour CL, Reddel HK, Bosnic-Anticevich SZ. Long-term maintenance of pharmacists' inhaler technique demonstration skills. American Journal of Pharmaceutical Education 2009;73(2):32. [DOI] [PMC free article] [PubMed] [Google Scholar]
BNF 2016
- Joint Formulary Committee. British National Formulary (online). London: BMJ Group and Pharmaceutical Press. http://www.medicinescomplete.com (accessed 17 February 2016).
Brocklebank 2001
- Brocklebank D, Ram F, Wright J, Barry P, Cates C, Davies L et al. Comparison of the effectiveness of inhaler devices in asthma and chronic obstructive airways disease: a systematic review of the literature. Health Technology Assessment 2001;5(26):1-149. [DOI] [PubMed] [Google Scholar]
BTS/SIGN 2014
- British Thoracic Society and Scottish Intercollegiate Guidelines Network. British guideline on the management of asthma. A national clinical guideline. https://www.brit-thoracic.org.uk/guidelines-and-quality-standards/asthma-guideline/ (accessed 24 February 2016).
Capanoglu 2015
- Capanoglu M, Dibek Misirlioglu E, Toyran M, Civelek E, Kocabas CN. Evaluation of inhaler technique, adherence to therapy and their effect on disease control among children with asthma using metered dose or dry powder inhalers. Journal of Asthma 2015;52(8):838-45. [DOI] [PubMed] [Google Scholar]
Crompton 2006a
- Crompton G. A brief history of inhaled asthma therapy over the last fifty years. Primary Care Respiratory Journal 2006;15(6):326-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
Crompton 2006b
- Crompton GK, Barnes PJ, Broeders M, Corrigan C, Corbetta L, Dekhuijzen R et al. The need to improve inhalation technique in Europe: a report from the Aerosol Drug Management Improvement Team. Respiratory Medicine 2006;100(9):1479-94. [DOI] [PubMed] [Google Scholar]
Deerojanawong 2009
- Deerojanawong J, Promsaka na Sakolnakorn V, Prapphal N, Hanrutakorn C, Sritippayawan S. Evaluation of metered-dose inhaler administration technique among asthmatic children and their caregivers in Thailand. Asian Pacific Journal of Allergy and Immunology 2009;27(2-3):87-93. [PubMed] [Google Scholar]
Dekhuijzen 2007
- Dekhuijzen PN, Crompton GK. Issues in inhalation therapy: a new series of papers from the ADMIT Working Group. Primary Care Respiratory Journal 2007;16(6):335-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Erikson 2003
- Erickson SR, Chang A, Johnson CE, Gruppen LD. Lecture versus Web tutorial for pharmacy students' learning of MDI technique. Annals of Pharmacotherapy 2003;37(4):500-5. [DOI] [PubMed] [Google Scholar]
Fink 2005
- Fink JB, Rubin BK. Problems with inhaler use: a call for improved clinician and patient education. Respiratory Care 2005;50(10):1360-74; discussion 1374-5. [PubMed] [Google Scholar]
Gillette 2016
- Gillette C, Rockich-Winston N, Kuhn JA, Flesher S, Shepherd M. Inhaler technique in children with asthma: a systematic review. Academic Pediatrics 2016;16(7):605-15. [EMBASE: 610628205] [DOI] [PubMed] [Google Scholar]
GINA 2016
- Global Initiative for Asthma (GINA). Global Initiative for Asthma. Global Strategy for Asthma Management and Prevention, 2016. http://ginasthma.org/gina-reports/ (accessed 17 February 2016).
Giraud 2001
- Giraud V, Roche N. Misuse of corticosteroid metered-dose inhaler is associated with decreased asthma stability. European Respiratory Journal 2001;19(2):246-51. [DOI] [PubMed] [Google Scholar]
Global Asthma Network 2014
- Global Asthma Network. The Global Asthma Report 2014. www.globalasthmareport.org/index.php (accessed 12 July 2016).
GRADEpro GDT [Computer program]
- GRADE Working Group, McMaster University GRADEpro GDT. Version accessed 13 January 2017. Hamilton (ON): GRADE Working Group, McMaster University, 2014.
Haughney 2010
- Haughney J, Price D, Barnes NC, Virchow JC, Roche N, Chrystyn H. Choosing inhaler devices for people with asthma: current knowledge and outstanding research needs. Respiratory Medicine 2010;104(9):1237-45. [DOI] [PubMed] [Google Scholar]
Hedlin 2010
- Hedlin G, Bush A, Lødrup Carlsen K, Wennergren G, De Benedictis FM, Melén E et al. Problematic severe asthma in children, not one problem but many: a GA2LEN initiative. European Respiratory Journal 2010;36(1):196-201. [DOI] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1 [updated March 2011]. The Cochrane Collaboration, 2011. www.cochrane-handbook.org.
Inhaler Error Steering Committee 2013
- Inhaler Error Steering Committee, Price D, Bosnic-Anticevich S, Briggs A, Chrystyn H, Rand C et al. Inhaler competence in asthma: common errors, barriers to use and recommended solutions. Respiratory Medicine 2013;107(1):37-46. [DOI] [PubMed] [Google Scholar]
Kamps 2000
- Kamps AW, Ewijk B, Roorda RJ, Brand PL. Poor inhalation technique, even after inhalation instructions, in children with asthma. Pediatric Pulmonology 2000;29(1):39-42. [DOI] [PubMed] [Google Scholar]
Kemp 2010
- Kemp L, Haughney J, Barnes N, Sims E, Ziegenweidt J, Hillyer EV et al. Cost-effectiveness analysis of corticosteroid inhaler devices in primary care asthma management: a real world observational study. ClinicoEconomics and Outcomes Research 2010;2:75-85. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kim 2009
- Kim SH, Kwak HJ, Kim TB, Chang YS, Jeong JW, Kim CW et al. Inappropriate techniques used by internal medicine residents with three kinds of inhalers (a metered dose inhaler, Diskus, and Turbuhaler): changes after a single teaching session. Journal of Asthma 2009;46(9):944-50. [DOI] [PubMed] [Google Scholar]
Lavorini 2007
- Lavorini F, Magnan A, Dubus JC, Voshaar T, Corbetta L, Broeders M et al. Effect of incorrect use of dry powder inhalers on management of patients with asthma and COPD. Respiratory Medicine 2007;102:593-604. [DOI] [PubMed] [Google Scholar]
Lavorini 2010
- Lavorini F, Levy ML, Corrigan C, Crompton G, ADMIT Working Group. The ADMIT series - issues in inhalation therapy. 6) Training tools for inhalation devices. Primary Care Respiratory Journal 2010;19(4):335-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lefebvre 2011
- Lefebvre C, Manheimer E, Glanville J. Chapter 6: Searching for studies. In: Higgins JPT, Green S. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. www.cochrane-handbook.org.
Levy 2013
- Levy ML, Hardwell A, McKnight E, Holmes J. Asthma patients' inability to use a pressurised metered-dose inhaler (pMDI) correctly correlates with poor asthma control as defined by the global initiative for asthma (GINA) strategy: a retrospective analysis. Primary Care Respiratory Journal 2013;22(4):406-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lewis 2016
- Lewis A, Torvinen S, Dekhuijzen PRN, Chrystyn H, Watson AT, Blackney M et al. The economic burden of asthma and chronic obstructive pulmonary disease and the impact of poor inhalation technique with commonly prescribed dry powder inhalers in three European countries. BMC Health Services Research 2016;16:251. [DOI] [PMC free article] [PubMed] [Google Scholar]
Masoli 2004
- Masoli M, Fabian D, Holt S, Beasley R, Global Initiative for Asthma (GINA) Program. The global burden of asthma: executive summary of the GINA Dissemination Committee report. Allergy 2004;59(5):469-78. [DOI] [PubMed] [Google Scholar]
McFadden 1995
- McFadden ER Jr. Improper patient techniques with metered dose inhalers: clinical consequences and solutions to misuse. Journal of Allergy and Clinical Immunology 1995;96(2):278-83. [DOI] [PubMed] [Google Scholar]
Melani 2011
- Melani AS, Bonavia M, Cilenti V, Cinti C, Lodi M, Martucci P et al. Inhaler mishandling remains common in real life and is associated with reduced disease control. Respiratory Medicine 2011;105(6):930-8. [DOI] [PubMed] [Google Scholar]
Moher 2009
- Moher D, Liberati A, Tetzlaff J, Altman D. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Medicine 2009;6(7):e1000097. [DOI: 10.1371/journal.pmed.1000097] [DOI] [PMC free article] [PubMed] [Google Scholar]
Navarre 2007
- Navarre M, Patel H, Johnson CE, Durance A, McMorris M, Bria W et al. Influence of an interactive computer-based inhaler technique tutorial on patient knowledge and inhaler technique. Annals of Pharmacotherapy 2007;41(2):216-21. [DOI] [PubMed] [Google Scholar]
Nelson 2011
- Nelson P, Young HN, Knobloch MJ, Griesbach SA. Telephonic monitoring and optimization of inhaler technique. Telemedicine Journal and e-health 2011;17(9):734-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
NRAD 2014
- National Review of Asthma Deaths. Why asthma still kills: the national review of asthma deaths. https://www.rcplondon.ac.uk/sites/default/files/why-asthma-still-kills-full-report.pdf (accessed 7 April 2016).
Poureslami 2012
- Poureslami I, Nimmon L, Doyle-Waters M, Rootman I, Schulzer M, Kuramoto L et al. Effectiveness of educational interventions on asthma self-management in Punjabi and Chinese asthma patients: a randomized controlled trial. Journal of Asthma 2012;49(5):542-51. [DOI] [PubMed] [Google Scholar]
Price 2002
- Price D, Duerden M. Inhalers: education and training needs. Current Therapeutics 2002;43(5):21-6, 28-9. [Google Scholar]
RevMan 2014 [Computer program]
- The Nordic Cochrane Centre, The Cochrane Collaboration Review Manager (RevMan). Version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Rootmensen 2010
- Rootmensen GN, Keimpema ARJ, Jansen HM, Haan RJ. Predictors of incorrect inhalation technique in patients with asthma or COPD: a study using a validated videotaped scoring method. Journal of Aerosol Medicine and Pulmonary Drug Delivery 2010;23(5):323-8. [DOI] [PubMed] [Google Scholar]
Roy 2011
- Roy A, Battle K, Lurslurchachai L, Halm EA, Wisnivesky JP. Inhaler device, administration technique, and adherence to inhaled corticosteroids in patients with asthma. Primary Care Respiratory Journal 2011;20(2):148-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sanchis 2013
- Sanchis J, Corrigan C, Levy ML, Viejo JL, ADMIT Group. Inhaler devices - from theory to practice. Respiratory Medicine 2013;107(4):495-502. [DOI] [PubMed] [Google Scholar]
Toumas 2009
- Toumas M, Basheti IA, Bosnic-Anticevich SZ. Comparison of small-group training with self-directed internet-based training in inhaler techniques. American Journal of Pharmaceutical Education 2009;73(5):85. [DOI] [PMC free article] [PubMed] [Google Scholar]
van Beerendonk 1998
- Beerendonk I, Mesters I, Mudde AN, Tan TD. Assessment of the inhalation technique in outpatients with asthma or chronic obstructive pulmonary disease using a metered-dose inhaler or dry powder device. Journal of Asthma 1998;35(3):273-9. [DOI] [PubMed] [Google Scholar]
van der Palen 1999
- Palen J, Klein JJ, Herwaarden CL, Zielhuis GA, Seydel ER. Multiple inhalers confuse asthma patients. European Respiratory Journal 1999;14(5):1034-7. [DOI] [PubMed] [Google Scholar]
Westerik 2016
- Westerik JA, Carter V, Chrystyn H, Burden A, Thompson SL, Ryan D et al. Characteristics of patients making serious inhaler errors with a dry powder inhaler and association with asthma-related events in a primary care setting. Journal of Asthma 2016;53(3):321-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
References to other published versions of this review
Normansell 2016
- Normansell R, Kew KM. Interventions to improve inhaler technique for people with asthma. Cochrane Database of Systematic Reviews 2016, Issue 7. Art. No: CD012286. [DOI: 10.1002/14651858.CD012286] [DOI] [PMC free article] [PubMed] [Google Scholar]


