Abstract
BACKGROUND:
The outcomes from pulmonary vein isolation (PVI) for atrial fibrillation (AF) are suboptimal, but the benefits of additional lesion sets remain unproven. Recent studies propose ablation of AF drivers improves outcomes over PVI, yet with conflicting reports in the literature. We undertook a systematic literature review and meta-analysis to determine outcomes from ablation of AF drivers in addition to PVI or as a stand-alone procedure.
METHODS:
Database search was done using the terms atrial fibrillation and ablation or catheter ablation and driver or rotor or focal impulse or FIRM (Focal Impulse and Rotor Modulation). We pooled data using random effects model and assessed heterogeneity with I2 statistic.
RESULTS:
Seventeen studies met inclusion criteria, in a cohort size of 3294 patients. Adding AF driver ablation to PVI reported freedom from AF of 72.5% (confidence interval [CI], 62.1%−81.8%; P<0.01) and from all arrhythmias of 57.8% (CI, 47.5%−67.7%; P<0.01). AF driver ablation when added to PVI or as stand-alone procedure compared with controls produced an odds ratio of 3.1 (CI, 1.3–7.7; P=0.02) for freedom from AF and an odds ratio of 1.8 (CI, 1.2–2.7; P<0.01) for freedom from all arrhythmias in 4 controlled studies. AF termination rate was 40.5% (CI, 30.6%−50.9%) and predicted favorable outcome from ablation(P<0.05).
CONCLUSIONS:
In controlled studies, the addition of AF driver ablation to PVI supports the possible benefit of a combined approach of AF driver ablation and PVI in improving single-procedure freedom from all arrhythmias. However, most studies are uncontrolled and are limited by substantial heterogeneity in outcomes. Large multicenter randomized trials are needed to precisely define the benefits of adding driver ablation to PVI.
Keywords: ablation, catheter; arrhythmia; atrial fibrillation; cohort studies; freedom; meta-analysis; odds ratio
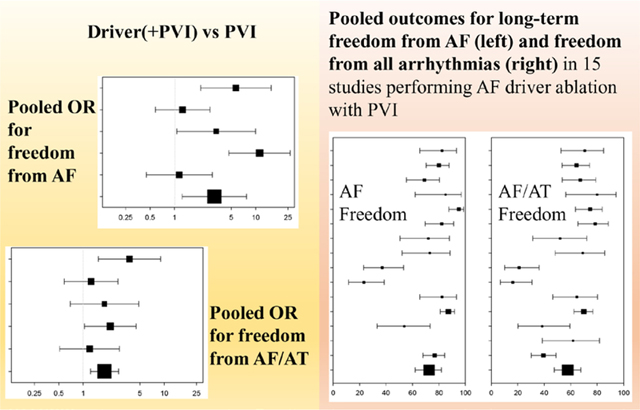
Graphical Abstract
Pulmonary vein isolation (PVI) for atrial fibrillation (AF) improves long-term outcomes compared with antiarrhythmic drugs (AAD) but remains suboptimal particularly for persistent AF.1–3 Unfortunately, attempts to improve outcomes by supplementing PVI with linear lesions or often extensive ablation of electrogram targets have had disappointing results.2–4 Contemporary mapping shows that AF may be sustained by drivers,5,6 whose ablation may be promising.7–9 This has been an increasingly popular area of interest, especially in the last 5 years, with increasing number of bench-to-bedside studies and mostly small-sized, nonrandomized clinical studies with highly variable outcomes in terms of acute impact (AF termination), as well as long-term outcomes. In this study, our intention is to review all the published studies on AF driver ablation to provide some clarity over individual study results, about long-term clinical impact of this approach.
We, therefore, performed a systematic review and meta-analysis to assess the clinical impact of AF driver ablation. AF drivers are defined as electrically mappable mechanisms that sustain, rather than initiate, fibrillatory conduction. Several clinical mapping approaches have been used to reveal potential AF drivers, and we included studies of multiple AF mapping approaches reporting long-term outcomes. This includes dominant frequency analysis,9 FIRM (Focal Impulse and Rotor Modulation),7 and noncontact body surface mapping (ECVUE).8 We also included recent studies mapping AF drivers using electrogram similarity10 and dispersion11 analyses.
Our primary objective was to produce a pooled point estimate and confidence interval (CI) for success rates, defined as freedom from AF or freedom from any atrial arrhythmias at follow-up when AF driver ablation is added to PVI. Our secondary objectives included estimating (1) pooled point estimates and CIs for acute procedural outcomes of AF driver ablation when added to PVI and (2) meta-analysis of pooled results of AF driver ablation compared with a control group. The caveat is that most studies of AF driver ablation to date have been single-arm studies without control arms.
METHODS
Data Sources and Criteria for Selecting Studies
We searched MEDLINE (PubMed) and Cochrane databases (inception to August 1, 2017) using the terms atrial fibrillation and ablation or catheter ablation and driver or rotor or focal impulse or FIRM. In addition, we reviewed the reference lists of retrieved studies and major conference proceedings. Any article that met criteria listed in the following section was retrieved. No language limitations were applied.
Inclusion and exclusion criteria are shown in Figure 1. When groups published multiple reports with overlapping cohorts, the most recent study was included. Definitions of an AF driver vary between studies, including consistent anatomic sites where rotational sites are anchored,8 sites of consistent rotational activation,7 sites of high dominant frequency,9 and sites where dispersion of activation supports driver physiology.11 For the purposes of this analysis, we included each of these studies that targeted ablation at these sites and assessed the long-term outcomes, using definitions used by the author of each study.
Figure 1. Flowchart illustrating study selection methodology.
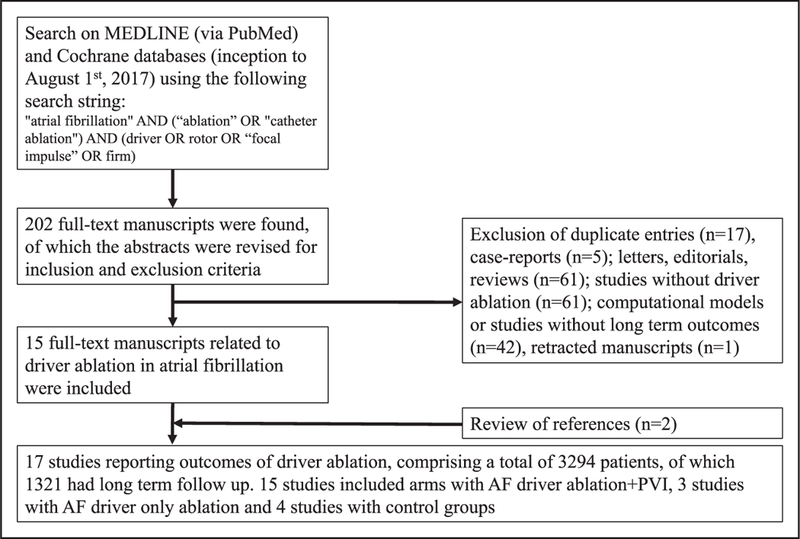
AF indicates atrial fibrillation; and PVI, pulmonary vein isolation.
The systematic review was registered at PROSPERO (International Prospective Register of Systematic Reviews; CRD42017069091). Quality assessment was accomplished with the use of Delphi criteria for randomized studies and the Newcastle-Ottawa scale for nonrandomized studies by 3 reviewers (M.R., G.L.M., and M.A.; Table I in the Data Supplement). Agreement between all 3 reviewers was mandatory for the final classification of the studies.
The data used for the analyses (ie, published articles on AF driver ablation) are specifically referenced within the work and freely available to all researchers. Accordingly, we have not duplicated them. The analytic methods are described herein for other researchers to reproduce our results.
Data Extraction
Three authors (T.B., A.J.R., and G.L.M.) performed database searches independently with agreement on the inclusion of the selected trials. Data extraction and preparation of this article followed recommendations of the PRISMA group.12 Data on demographics, comorbidities, procedural characteristics, and single-procedure outcomes were entered independently by 3 authors and reviewed for discrepancies. In studies permitting repeat ablations, short-and long-term outcomes for the first ablation were extracted. Procedural information collected included driver characteristics, acute AF termination rate, complication rate, fluoroscopy time, total ablation time, and total procedure duration.
Statistical Analysis
Continuous variables are presented as mean±SD. Nominal values are expressed as n (%). Analyses were performed using SPSS, version 19, and MedCalc, version 17.6. Data were pooled using random effects, using DerSimonian and Laird method. Statistical heterogeneity on each outcome of interest was quantified using the P value for the Q statistic and I2. Heterogeneity based on I2 was considered low if <25%, moderate if 25% to 75%, and high if >75%. For pooling single arms, the pooled rate of freedom from AF along with freedom from both AF and atrial tachycardia (AT) was computed along with the 95% CI. For studies including a control group, the odds ratio (OR) and respective 95% CI were used to measure treatment effect. Meta-regression (using the unrestricted maximum likelihood method) was performed to compare associations of potentially confounding variables with the end point of freedom from AF and other arrhythmias.
RESULTS
Search Results
Initial search terms resulted in 202 studies that were retrieved for further analysis (Figure 1). Of these, 187 were excluded because they comprised duplicate populations, did not perform AF driver ablation or provide clinical outcomes with at least 6 months of mean follow-up duration, or were retracted, resulting in 15 studies. Another 2 studies were identified from review of bibliographies for a total of 17 studies.
Study Characteristics
Table 1 presents the 17 studies included in this systematic review, comprised of 1 randomized controlled study, 3 nonrandomized controlled studies, and 13 studies with no control groups.7–11,13–24 Fifteen studies included cohorts that underwent AF driver ablation with PVI, 3 studies included cohorts with AF driver-only ablation, and 4 studies included control groups. Studies are displayed separately to show baseline information in each arm, and so, Atienza et al9 is represented in 3 rows and Narayan et al,7 Lin et al,10 and Seitz et al11 in 2 rows. The enrolled cohort of these studies comprises 3294 patients. Eight hundred sixty-six patients were treated with AF driver ablation in addition to PVI, 187 patients were treated with AF driver ablation without PVI, and 268 patients comprised the control populations. Ninety-one patients were exluded for various reasons (ie, intracardiac thrombus on transesophageal echocardiogram) after enrollment. Forty-seven patients who underwent ablation did not have long-term outcomes reported because of being lost to follow-up or inadequate follow-up duration. Sommer et al13 and Haissaguerre et al8 provided demographics and acute procedural data only for the control groups (n=1800 and n=82, respectively), without long-term outcomes. Details are reported separately in the Appendix in the Data Supplement.
Table 1.
Selected Studies for the Systematic Review: Baseline Information
| Year | Author | Publication Type |
Study Type | Search Database | Study Size, n |
Type of Ablation |
Type of Driver Mapping |
Follow- Up, mo |
Persistent AF |
Redo Ablation |
Age, y | Male Sex |
LA Size, mm |
Ejection Fraction, % |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2012 | Narayan et al7* | Manuscript | Multicenter, controlled | PubMED | 107 | Driver+PVI | FIRM | 9.1 | 0.85 | 0.42 | 63±9 | 0.94 | 48.0±7 | 53±1 5 |
| 2014 | Haissaguerre et al8 | Manuscript | Single center, case series | PubMED | 193 | Driver+PVI | ECVUE | 12.0 | 1.00 | 0.20 | 59±11 | 0.77 | 48.0±7 | 52±13 |
| 2014 | Atienza et al9† | Manuscript | Multicenter, randomized | Cochrane | 232 | Driver+PVI | Dominant frequency |
12.0 | 1.00 | 0 | 55±9 | 0.81 | 45.0±7 | 60 |
| 2015 | Sommer et al13 | Manuscript | Single center, case series | PubMED | 1820 | Driver+PVI | FIRM | … | 0.90 | 0.50 | 61 ±8 | 0.70 | 45.9±5 | 55±8 |
| 2015 | Tomassoni et al14 | Manuscript | Single center, case series | Review of References | 80 | Driver+PVI | FIRM | 16.0 | 0.76 | 0.46 | 62±9 | 0.75 | 55.0±7 | 52 ±8 |
| 2015 | Rashid et al15 | Manuscript | Single center, case series | Review of References | 56 | Driver+PVI | FIRM | 7.7 | 0.77 | 0.48 | 66±9 | 0.75 | … | 56±8 |
| 2015 | Tilz et al16 | Manuscript | Single center, case series | PubMED | 25 | Driver+PVI | FIRM | 13.0 | 0.60 | … | 63±9 | 0.64 | 45.0±5 | 58±7 |
| 2016 | Spitzer et al17 | Manuscript | Single center, case series | PubMED | 58 | Driver+PVI | FIRM | 12.0 | 1.00 | 1.00 | 62±9 | 0.72 | 47.0±6 | 57±9 |
| 2016 | Buch et al18 | Manuscript | Multicenter, case series | PubMED | 43 | Driver+PVI | FIRM | 18.0 | 0.44 | 0.67 | 61 ±11 | 0.74 | … | 59±6 |
| 2016 | Steinberg et al19 | Manuscript | Single center, case series | PubMED | 47 | Driver+PVI | FIRM | 18.7 | 0.83 | 0.72 | 64±11 | 0.79 | 44.0±7 | 54±7 |
| 2016 | Lin et al10‡ | Manuscript | Single center, controlled | Cochrane | 95 | Driver+PVI | Phase+similarity | 17.7 | 1.00 | … | 56±9 | 0.79 | 39.9±7 | 58±7 |
| 2017 | Miller et al25 | Manuscript | Single center, case series | PubMED | 170 | Driver+PVI | FIRM | 15.0 | 0.63 | 0.43 | 59±12 | 0.79 | 52.0± 10 | 47 ±10 |
| 2017 | Balouch et al21 | Manuscript | Single center, case series | PubMED | 27 | Driver+PVI | FIRM | 12.0 | 1.00 | 0.52 | 64±9 | 0.82 | 46.0±8 | 53±7 |
| 2017 | Kis et al22 | Manuscript | Single center, case series | PubMED | 38 | Driver+PVI | FIRM | 12.0 | 1.00 | 0.53 | 63±11 | 0.63 | 46.0±7 | … |
| 2017 | Knecht et al23 | Manuscript | Multicenter, case series | PubMED | 118 | Driver+PVI | ECVUE | 12.0 | 1.00 | 0.00 | 64±8 | 0.74 | 43.0±6 | 60 ±9 |
| 2014 | Atienza et al9† | Manuscript | Multicenter, randomized | Cochrane | 232 | Driver only | Dominant frequency |
12.0 | 0.00 | 0.24 | 54±12 | 0.73 | 40.0±6 | 60 |
| 2016 | Berntsen et al24 | Manuscript | Single center, case series | PubMED | 33 | Driver only | FIRM | 15.2 | 0.00 | 0.15 | 55±12 | 0.93 | 42.0±5 | … |
| 2017 | Seitz et al11§ | Manuscript | Multicenter, controlled | PubMED | 152 | Driver only | Electrogram dispersion |
17.4 | 0.77 | 0.00 | 63±11 | 0.76 | 45.6±8 | 52±11 |
| 2012 | Narayan et al7* | Manuscript | Control | Control | Control | Control | Control | 9.1 | 0.66 | 0.25 | 61 ±8 | 0.96 | 43.0±6 | 55±12 |
| 2014 | Atienza et al9† | Manuscript | Control | Control | Control | Control | Control | 12.0 | 1.00 | 0.26 | 54± 10 | 0.83 | 42.5±7 | 60 |
| 2016 | Lin et al10‡ | Manuscript | Control | Control | Control | Control | Control | 17.7 | 1.00 | … | 54±9 | 0.77 | 39.0±6 | 58±8 |
| 2017 | Seitz et al11§ | Manuscript | Control | Control | Control | Control | Control | 17.4 | 0.81 | 0.00 | 58±11 | 0.74 | 42.4± 12 | 54±12 |
First authors are listed for manuscripts. Persistent AF, redo ablation, and male sex are presented as ratios. Age and LA size and ejection fraction are presented as mean±SD when available. Study size indicates the total cohort enrolled in the study. AF indicates atrial fibrillation; FIRM, Focal Impulse and Rotor Modulation; LA, left atrium; and PVI, pulmonary vein isolation. Study by Atienza et al,
is represented in 3 rows; study by Narayan et al,
Lin et al,
and Seitzet al,
is represented in 2 rows to show baseline information in each arm (ie, driver+PVI, driver only, and control).
The approaches used for mapping and ablation of AF drivers in each study are listed in Table 1. PVI consisted of radiofrequency point-by-point lesions in all studies except for Rashid et al,15 who used cryoballoon ablation in all patients, and Steinberg et al,19 who used cryoballoon in first-time ablation patients but otherwise used point-by-point radiofrequency lesions. Beyond PVI, ablation strategies varied between reports. Narayan et al7 and Tomassoni et al14 included a left atrial roof line ablation in patients with persistent AF. Rashid et al15 performed ablation of the cavotricuspid isthmus in all patients and coronary sinus ablation if AF did not terminate. Steinberg et al19 ablated roof and mitral lines depending on investigator preference. Haissaguerre et al8 and Knecht et al23 performed the stepwise ablation approach if AF persisted after driver ablation and PVI. Studies with control populations treated subjects with PVI only, with the exception of Lin et al10 who added complex fractionated atrial electrogram ablation and Seitz et al11 who performed the stepwise approach if AF persisted after PVI. Details of additional ablation are listed in Table II in the Data Supplement.
The final cohort included 75% patients with persistent or long-standing persistent AF and 25% with paroxysmal AF. Six studies consisted of patients with persistent and long-standing persistent AF only, whereas 9 studies contained a mixed cohort, and 1 study contained only patients with paroxysmal AF.
Mean follow-up duration was ≥12 months in 90% of the studies. All studies monitored patients using ECG or Holter monitoring at 3, 6, and 12 months. Across all articles, AF or AT recurrence was defined as arrhythmias lasting >30 seconds or >1% burden on implanted devices. AAD use was allowed at 1-year follow-up in 11 of the 17 (65%; Table II in the Data Supplement). Three studies13,16,18 allowed AAD use only during the blanking period, and 1 study10 did not clarify whether AAD use was allowed at 12-month follow-up. For this reason, we did not quantify results based on AAD use.
Role of AF Driver Ablation for Long-Term Freedom From AF and AF/AT
Studies With Control Groups
Summary of procedural details is listed in Table 27–11,13 to 24. Three studies (Narayan et al,7 Atienza et al,9 and Lin et al10) compared AF driver ablation with PVI to PVI.7,9,10 Of these 3 studies, Lin et al11 performed additional complex fractionated atrial electrogram ablation in the PVI control group. The significant pooled OR for freedom from AF in these 3 studies using the random effects model was 2.73 (CI, 1.06–7.02 [P=0.037]; I2=66% [P=0.05]). Freedom from AF/AT, compared with PVI alone, yielded an OR of 1.780 (CI, 0.58–5.49 [P=0.32]; I2=79% [P=0.01]).
Table 2.
Procedural Details and Acute Procedural Outcomes of Included Studies
| Year | Author | Cohort Size for Acute Outcomes, n |
Acute AF Termination |
No. of Localized Drivers |
Procedure Duration, min |
Fluoroscopy Duration, min |
RF Duration, min |
Complication Rate |
|---|---|---|---|---|---|---|---|---|
| 2012 | Narayan et al7* | 36 | 0.56 | 2.1±1 | … | … | 58±23 | 0.06 |
| 2014 | Haissaguerre et al8 | 103 | 0.79 | 4 | … | … | … | … |
| 2014 | Atienza et al9† | 59 | 0.46 | 3 | 239±61 | 67 | 43 | 0.10 |
| 2015 | Sommer et al13 | 20 | 0.05 | 4.2±1.6 | 205±35 | 18±4 | … | 0.00 |
| 2015 | Tomassoni et al14 | 36 | 0.39 | 3.8±1.4 | 280±60 | 36±20 | 76±25 | 0.06 |
| 2015 | Rashid et al15 | 56 | 0.28 | 3.4±1.2 | 221±44 | 20±9 | … | … |
| 2015 | Tilz et al16 | 25 | 0.24 | 3±1.6 | 236±56 | 28±4 | … | 0.04 |
| 2016 | Spitzer et al17 | 58 | 0.09 | 3±1.6 | 199±42 | 26±9 | 30±15 | 0.05 |
| 2016 | Buch et al18 | 43 | 0.26 | 2.6±1.2 | 314±82 | 55±24 | 39±18 | 0.09 |
| 2016 | Steinberg et al19 | 43 | 0.12 | 1.8±0.8 | … | 31±14 | 28±13 | 0.02 |
| 2016 | Lin et al10‡ | 34 | 0.68 | 2.6±0.9 | … | … | … | 0.03 |
| 2017 | Miller et al25 | 170 | 0.39 | 3.5±2.1 | 356±60 | 25±13 | 56±14 | 0.04 |
| 2017 | Balouch et al21 | 27 | 0.30 | 2. ±1.2 | 373±60 | 60±11 | 45±15 | 0 |
| 2017 | Kis et al22 | 38 | 0.68 | 2.1±1.6 | 282±62 | 34±11 | 36±20 | 0.11 |
| 2017 | Knecht et al23 | 118 | 0.72 | 4.9±1 | 231±71 | 31±13 | 75±27 | 0.02 |
| 2014 | Atienza et al9† | 55 | 0.58 | 2.9 | 228±65 | 59 | 29 | 0.06 |
| 2016 | Berntsen et al24 | 27 | 0.30 | 3±1.1 | 397±69 | 74±34 | 25±10 | 0 |
| 2017 | Seitz et al11§ | 105 | 0.95 | 5±1.5 | 168±42 | 15±13 | 49±21 | 0.03 |
| 2012 | Narayan et al7* | 71 | 0.09 | Control | 52±18 | … | … | 0.8 |
| 2014 | Atienza et al9† | 116 | 0.32 | Control | 209±62 | 63 | 36.5 | 0.10 |
| 2016 | Lin et al10‡ | 34 | 0.26 | Control | 154±41 | … | 141±47 | … |
| 2017 | Seitz et al11§ | 47 | 0.60 | Control | 230±67 | 78±15 | 85±35 | … |
Acute AF termination includes termination to AT or sinus rhythm and is presented as ratio. Number of localized drivers, procedure duration, fluoroscopy duration, and RF duration are presented as mean±SD when available. AF indicates atrial fibrillation; AT, atrial tachycardia; PVI, pulmonary vein isolation; and RF, radiofrequency. Study by Atienza et al
is represented in 3 rows; study by Narayan et al,
Lin et al,
and Seitz et al,
is represented in 2 rows to show baseline information in each arm (ie, driver+PVI, driver only, and control).
Two other studies (Seitz et al11 and Atienza et al9) compared AF driver-only ablation to PVI.9,11 If these 2 studies are included with the 3 reported above, the OR for AF freedom is 3.10 (CI, 1.25–7.71 [P=0.02]; I2=79% [P<0.01]; Figure 2, top). Freedom from AF/AT produced an OR of 1.83 (CI, 1.23–2.73; P<0.01), with minimal heterogeneity between studies (I2=13%; P=0.33; Figure 2, bottom).7,9–11
Figure 2. Meta-analysis of studies with control groups.
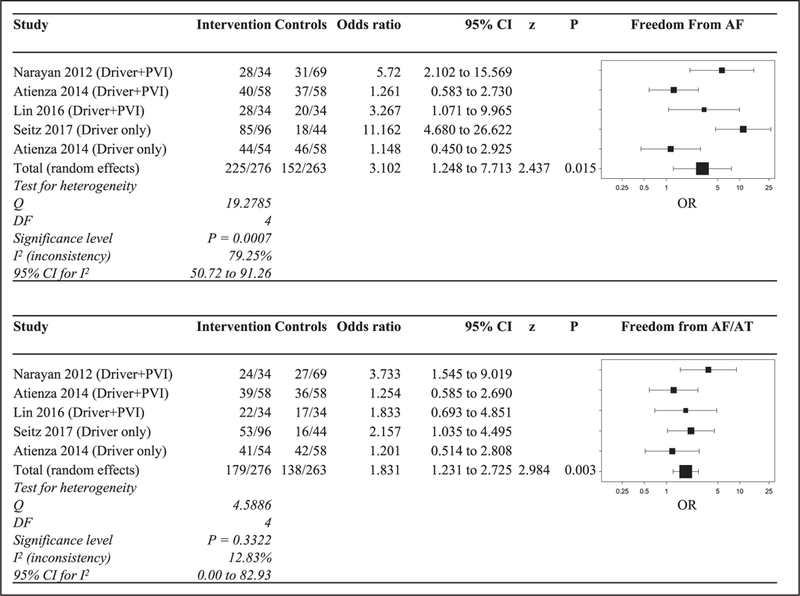
Top, Table demonstrates pooled odds ratio (OR) for freedom from atrial fibrillation (AF). Bottom, Table demonstrates pooled OR for freedom from AF/atrial tachycardia (AT) of 3 studies with driver ablation with pulmonary vein isolation (PVI) and 2 studies with driver-only ablation, compared with PVI. The study by Atienza et al9 is represented in 2 rows to reflect driver ablation with PVI and driver-only ablation cohorts. CI indicates confidence interval.
In 3 controlled studies, the termination rates were reported for both driver ablation with PVI (n=129) and PVI alone (n=156). The pooled OR comparing these groups is 5.23 (CI, 1.97–13.93; P<0.01). Because of the small number of available series, attempts were not made to identify sources of heterogeneity using metaregression in these controlled studies, but differences among study characteristics that affect outcomes can be identified in Table III in the Data Supplement.
Pooling Single Arms
There were 15 studies where AF driver ablation was performed with PVI. Of these, 14 studies with 816 patients reported long-term freedom from AF. The pooled AF freedom was 72.5% (CI, 62.1–81.8; heterogeneity I2=90.0%; P<0.01). Fifteen studies with 837 patients reported long-term freedom from AF/AT. The pooled rate was 57.8% (CI, 47.5–67.7; I2=85.6%; P<0.01). The pooled results for freedom from AF and AF/AT are shown in Figure 3.7–10,13–23
Figure 3. Forest plot diagrams showing pooled outcomes for long-term freedom from atrial fibrillation (AF; left) and freedom from all arrhythmias (right) in 15 studies that performed AF driver ablation with pulmonary vein isolation.

AT indicates atrial tachycardia; and CI, confidence interval.
Three studies reported long-term outcomes with AF driver-only ablation, without PVI. Freedom from AF after driver only, reported in 177 patients in 3 studies, was 63.6% (CI, 25.5–94.8; I2=96.53%; P<0.01).9,11,24 Freedom from AF/AT, reported in 150 patients in 2 studies, was 65.2% (CI, 44.4–83.4; I2=84.7%; P<0.01).9,11
Of these 15 studies that reported outcomes on AF driver ablation with PVI, acute procedural outcomes were reported in n=865 patients. Figure 4 includes pooled acute termination rates of AF to sinus rhythm or AT as 39.6% (CI, 27.0–52.9; I2=92%; P<0.01) during AF driver ablation with PVI. In 3 studies (n=188) with AF driver ablation only, the termination rate was 64.5% (CI, 0.22–0.96; I2=97%; P<0.01).7–10,13–23
Figure 4. Forest plot diagrams demonstrating acute termination rates of atrial fibrillation (AF) in 15 studies that performed AF driver ablation with pulmonary vein isolation.

CI indicates confidence interval.
Figure I in the Data Supplement reflects the pooled outcomes of AF driver ablation when added to PVI in 20 studies, when the outcomes of 5 abstracts presented in major meetings, including the abstract of the retracted manuscripts, are included.
Possible Sources of Heterogeneity, Risk of Bias Across Studies
Univariate meta-regression analysis was used to examine variables that may have impacted success rates in AF driver ablation with PVI, when potential confounder values were available. Results of the examined variables are presented in Table III in the Data Supplement. Larger left atrium size (P<0.01), longer ablation times (P<0.01), and termination or slowing of AF during ablation (P<0.01) were associated with greater freedom from AF, with larger study size showing a trend toward significance (P=0.08) in this direction. Heterogeneity was largely driven by 2 series18,19 that lay outside of the funnel plot of all series and reported lower success rates than expected for their sample sizes (Figure II in the Data Supplement). On sensitivity analysis, exclusion of these 2 series yielded a pooled estimate of 78.3% AF freedom (CI, 72.59–83.47; I2=67.9%; P<0.01).
Larger left atrium size also related to freedom from AF/AT (P<0.01), with longer follow-up duration trended to show lower rates of AF/AT freedom (P=0.05).
DISCUSSION
We performed a systematic review and meta-analysis of studies on AF driver ablation as an approach to improve the success of PVI or as a stand-alone ablation strategy in some studies. In the limited number of controlled studies, AF driver ablation may offer greater arrhythmia freedom over conventional ablation alone, with acceptable heterogeneity in the analyses of freedom from AF/ AT. Single-arm studies were characterized by substantial heterogeneity. In a single-arm analysis of all studies, AF driver ablation with PVI produced a single-procedure freedom from AF of 72.5% and freedom from all arrhythmias of 57.8% freedom from all arrhythmias in a population of 75% with nonparoxysmal AF.
Despite the limitations of included studies, several notable features are evident from this meta-analysis. First, targeted AF driver ablation as a stand-alone procedure or when added to PVI may increase acute procedural termination of AF over PVI alone. It remains to be determined whether this supports the mechanistic importance of drivers, but AF termination in this analysis was associated with increased long-term arrhythmia freedom. Second, heterogeneity in long-term outcomes was substantial but driven by poor outcomes in 2 studies18,19 that lay outside the funnel plot, with lower results than expected by their sample sizes. Sensitivity analysis removing these 2 studies yielded low heterogeneity. The reasons for this remain unclear. Third, AF driver ablation seems to produce more favorable results when combined with conventional ablation (PVI) compared with studies in which it was used alone. It is unclear whether this reflects the cumulative effect of eliminating concomitant triggers by PVI, eliminating additional drivers by PVI, or some atrial debulking effect of greater ablation area.
Interest in human AF drivers is motivated by their potential to improve ablation beyond PVI alone,2,26 based on mechanisms translated from optical mapping of human AF,6 AF in animal studies,5 and modeling studies. The challenge is that this translation has been at times unclear, with mixed acute results of AF driver ablation and varying long-term data as quantified in this systematic review and meta-analysis. Fundamental debate still exists on the mechanisms of human AF. Although many studies show localized AF rotational or focal drivers by many methods listed in this article, historical AF mapping studies show disorganized waves with no (or few) drivers.27 Some studies have also shown drivers that may be unstable28,29 and hence less amenable to ablation. It remains undetermined whether conflicting results reflect patient selection, mapping methodology in AF, or other factors. Some data suggest that multiple mapping approaches may produce similar results when applied to the same patients,30 but further studies are needed to understand these discrepancies. Studies included in this systematic review were insufficiently powered to compare outcomes between different AF mapping approaches.
Limitations
This study has limitations. The quality of evidence is moderate with only 1 randomized controlled trial meeting inclusion criteria, and so the results of ongoing multicenter randomized studies are needed to supplement these data (eg, REAFFIRM, Randomized Evaluation of Atrial Fibrillation Treatment With Focal Impulse and Rotor Modulation Guided Procedures, NCT02274857; RECONFIRM, Randomized Evaluation of Conventional Ablation With or Without Focal Impulse and Rotor Modulation to Eliminate Human Atrial Fibrillation NCT02456233; and REDO-FIRM, Randomized Evaluation of Redo Ablation Procedures of Atrial Fibrillation With Focal Impulse and Rotor Modulation Guided Procedures, NCT02799043).
One major limitation is that ablation approach was heterogeneous between component trials, as is true for many ablation strategies for AF We have tried to clarify in depth the differences in ablation approaches in the Data Supplement. Especially controlled studies in this meta-analysis had variable procedures in the control limb (ie, additional lines, complex fractionated atrial electrogram, posterior wall ablation), although this has been a feature of many randomized trials of PVI ablation. As with all meta-analyses, the statistical analysis was limited by variable reporting of follow-up, AAD, and other factors in each parent article. The control cohorts were also limited in number, with a slightly lower rate of redo ablation (25%−30% versus 35%−40%) that was not statistically significant. Redo ablation also did not predict freedom from AF or AF/AT in metaregression analyses (Table III in the Data Supplement).
It was not always clearly stated in successive articles by the same authors whether the same subjects were used as in prior studies. We took a diligent and conservative approach to avoid including duplicate subjects. For this reason, the study by Miller et al20 using FIRM was not analyzed because it included patients subsequently presented in the study by Buch et al,18 Miller et al,25 and Steinberg et al19 who are analyzed separately. We did not include the article by Gianni et al31 because it reported <6 months of follow-up, nor did we include its earlier abstract report or related retracted article in which this limb was described as 30 consecutive nonrandomized patients.32 Studies such as those by Narayan et al33,34 and Baykaner et al35 were also not included because these substudies reflected subjects who were included in earlier included studies.7
Finally, we acknowledge that heterogeneity was high. However, this may be part of the landscape of emerging questions for which study outcomes are heterogeneous, as noted by Higgins et al,36 in which ≈25% of meta-analyses in Cochrane Database had I2 values of >50%, or by a few smaller studies which amplified this heterogeneity.
Conclusions
This systematic review and meta-analysis supports the possible benefit of a combined approach of AF driver ablation and PVI in improving freedom from all arrhythmias compared with conventional ablation alone. Outcomes of single-arm studies were significantly limited by high heterogeneity. This systematic review and meta-analysis provides a summary of currently available data on AF driver ablation and motivates further large multicenter randomized trials of AF driver ablation.
Supplementary Material
WHAT IS KNOWN?
Contemporary mapping shows that atrial fibrillation (AF) may be sustained by drivers, whose ablation may be promising.
Acute impact and long-term outcomes of AF driver ablation have been reported in small-sized, nonrandomized clinical studies with highly variable outcomes.
WHAT THE STUDY ADDS?
This systematic review and meta-analysis provides a summary of currently available data on AF driver ablation and motivates further large multicenter randomized trials of AF driver ablation.
AF driver ablation and pulmonary vein isolation, in a small number of controlled studies, seem to improve freedom from all arrhythmias compared with pulmonary vein isolation alone.
Outcomes of single-arm studies are significantly limited by high heterogeneity.
Footnotes
Disclosures
Dr Narayan receives compensation from Up to Date, Abbott Laboratories, and American College of Cardiology Foundation; consulting fees from Medtronic and St. Jude Medical; equity interests from Topera; intellectual property rights from U.C. Regents; and research grants from the National Institutes of Health (R01 HL85537 and K24 HL103800). Dr Wang receives honoraria from Janssen, St. Jude Medical, Amgen, and Medtronic; fellowship support from Biosense Webster, Boston Scientific, Medtronic, and St. Jude Medical; clinical studies from Medtronic, Siemens, Cardiofocus, and ARCA; and stock options from Vy-tronus.
The other authors report no conflicts.
The Data Supplement is available at http://circep.ahajournals.org/lookup/suppl/doi:10.1161/CIRCEP117.006119/-/DC1.
REFERENCES
- 1.Calkins H, Hindricks G, Cappato R, Kim YH, Saad EB, Aguinaga L, Akar JG, Badhwar V, Brugada J, Camm J, Chen PS, Chen SA, Chung MK, Nielsen JC, Curtis AB, Davies DW, Day JD, d’Avila A, de Groot NMSN, Di Biase L, Duytschaever M, Edgerton JR, Ellenbogen KA, Ellinor PT, Ernst S, Fenelon G, Gerstenfeld EP, Haines DE, Haissaguerre M, Helm RH, Hylek E, Jackman WM, Jalife J, Kalman JM, Kautzner J, Kottkamp H, Kuck KH, Kumagai K, Lee R, Lewalter T, Lindsay BD, Macle L, Mansour M, Marchlinski FE, Michaud GF, Nakagawa H, Natale A, Nattel S, Okumura K, Packer D, Pokushalov E, Reynolds MR, Sanders P, Scanavacca M, Schilling R, Tondo C, Tsao HM, Verma A, Wilber DJ, Yamane T. 2017 HRS/EHRA/ECAS/APHRS/SOLAECE expert consensus statement on catheter and surgical ablation of atrial fibrillation. Heart Rhythm. 2017;14:e275–e444. doi: 10.1016/j.hrthm.2017.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Verma A, Jiang CY, Betts TR, Chen J, Deisenhofer I, Mantovan R, Macle L, Morillo CA, Haverkamp W, Weerasooriya R, Albenque JP, Nardi S, Menardi E, Novak P, Sanders P; STAR AF II Investigators. Approaches to catheter ablation for persistent atrial fibrillation. N Engl J Med. 2015;372:1812–1822. doi: 10.1056/NEJMoa1408288. [DOI] [PubMed] [Google Scholar]
- 3.Vogler J, Willems S, Sultan A, Schreiber D, Lüker J, Servatius H, Schäffer B, Moser J, Hoffmann BA, Steven D. Pulmonary vein isolation versus defragmentation: the CHASE-AF clinical trial. J Am Coll Cardiol. 2015;66:2743–2752. doi: 10.1016/j.jacc.2015.09.088. [DOI] [PubMed] [Google Scholar]
- 4.Wong KC, Paisey JR, Sopher M, Balasubramaniam R, Jones M, Qureshi N, Hayes CR, Ginks MR, Rajappan K, Bashir Y, Betts TR. No benefit of complex fractionated atrial electrogram ablation in addition to circumferential pulmonary vein ablation and linear ablation: benefit of complex ablation study. Circ Arrhythm Electrophysiol. 2015;8:1316–1324. doi: 10.1161/CIRCEP.114.002504. [DOI] [PubMed] [Google Scholar]
- 5.Pandit SV, Jalife J. Rotors and the dynamics of cardiac fibrillation. Circ Res. 2013;112:849–862. doi: 10.1161/CIRCRESAHA.111.300158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hansen BJ, Zhao J, Csepe TA, Moore BT, Li N, Jayne LA, Kalyanasundaram A, Lim P, Bratasz A, Powell KA, Simonetti OP, Higgins RS, Kilic A, Mohler PJ, Janssen PM, Weiss R, Hummel JD, Fedorov VV. Atrial fibrillation driven by micro-anatomic intramural re-entry revealed by simultaneous sub-epicardial and sub-endocardial optical mapping in explanted human hearts. EurHeartJ. 2015;36:2390–2401. doi: 10.1093/eurheartj/ehv233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Narayan SM, Krummen DE, Shivkumar K, Clopton P, Rappel WJ, Miller JM. Treatment of atrial fibrillation by the ablation of localized sources: CONFIRM (Conventional Ablation for Atrial Fibrillation With or Without Focal Impulse and Rotor Modulation) trial. J Am Coll Cardiol. 2012;60:628–636. doi: 10.1016/j.jacc.2012.05.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Haissaguerre M, Hocini M, Denis A, Shah AJ, Komatsu Y, Yamashita S, Daly M, Amraoui S, Zellerhoff S, Picat MQ, Quotb A, Jesel L, Lim H, Ploux S, Bordachar P, Attuel G, Meillet V, Ritter P, Derval N, Sacher F, Bernus O, Cochet H, Jais P, Dubois R. Driver domains in persistent atrial fibrillation. Circulation. 2014;130:530–538. doi: 10.1161/CIRCULATI0NAHA.113.005421. [DOI] [PubMed] [Google Scholar]
- 9.Atienza F, Almendral J, Ormaetxe JM, Moya A, Martinez-Alday JD, Hernandez-Madrid A, Castellanos E, Arribas F, Arias MÂ, Tercedor L, Peinado R, Arcocha MF, Ortiz M, Martinez-Alzamora N, Arenal A, Fernandez-Avilés F, Jalife J; RADAR-AF Investigators. Comparison of radiofrequency catheter ablation of drivers and circumferential pulmonary vein isolation in atrial fibrillation: a noninferiority randomized multicenter RADAR-AF trial. J Am Coll Cardiol. 2014;64:2455–2467. doi: 10.1016/j.jacc.2014.09.053. [DOI] [PubMed] [Google Scholar]
- 10.Lin YJ, Lo MT, Chang SL, Lo LW, Hu YF, Chao TF, Chung FP, Liao JN, Lin C, Kuo HY, Chang YC, Lin C, Tuan TC, Young V, Suenari K, Do V, Raharjo S, Hyuand NE, Chen S. Benefits of atrial substrate modification guided by electrogram similarity and phase mapping techniques to eliminate rotors and focal sources versus conventional defragmentation in persistent atrial fibrillation. JACC Clin Electrophysiol. 2016;2:667–678. [DOI] [PubMed] [Google Scholar]
- 11.Seitz J, Bars C, Théodore G, Beurtheret S, Lellouche N, Bremondy M, Ferracci A, Faure J, Penaranda G, Yamazaki M, Avula UM, Curel L, Siame S, Berenfeld O, Pisapia A, Kalifa J. AF ablation guided by spatiotemporal electrogram dispersion without pulmonary vein isolation: a wholly patient-tailored approach. J Am Coll Cardiol. 2017;69:303–321. doi: 10.1016/j.jacc.2016.10.065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol. 2009;62:1006–1012. doi: 10.1016/j.jclinepi.2009.06.005. [DOI] [PubMed] [Google Scholar]
- 13.Sommer P, Kircher S, Rolf S, John S, Arya A, Dinov B, Richter S, Bollmann A, Hindricks G. Successful repeat catheter ablation of recurrent longstanding persistent atrial fibrillation with rotor elimination as the procedural endpoint: a case series. J Cardiovasc Electrophysiol. 2016;27:274–280. doi: 10.1111/jce.12874. [DOI] [PubMed] [Google Scholar]
- 14.Tomassoni G, Duggal S, Muir M, Hutchins L, Turner K, McLoney AM, Hesselson A. Long-term follow-up of FIRM-guided ablation of atrial fibrillation: a single-center experience. J Innovations Card Rhythm Management. 2015;6:2145–2151. [Google Scholar]
- 15.Rashid H, Sweeney A. Approaches for focal impulse and rotor mapping in complex patients: a US private practice perspective. J Innovations Card Rhythm Management. 2015;6:2193–2198. [Google Scholar]
- 16.Tilz RR, Lin T, Rillig A, Heeger CH, Scholz L, Wohlmuth P, Bucur T, Metzner A, Mathew S, Wissner E, Ouyang F, Kuck KH. Focal impulse and rotor modulation for the treatment of atrial fibrillation: locations and 1 year outcomes of human rotors identified using a 64-electrode basket catheter. J Cardiovasc Electrophysiol. 2017;28:367–374. doi: 10.1111/jce.13157. [DOI] [PubMed] [Google Scholar]
- 17.Spitzer SG, Karolyi L, Ràmmler C, Scharfe F, Weinmann T, Zieschank M, Langbein A. Treatment of recurrent nonparoxysmal atrial fibrillation using focal impulse and rotor mapping (FIRM)-guided rotor ablation: early recurrence and long-term outcomes. J Cardiovasc Electrophysiol. 2017;28:31–38. doi: 10.1111/jce.13110. [DOI] [PubMed] [Google Scholar]
- 18.Buch E, Share M, Tung R, Benharash P, Sharma P, Koneru J, Mandapati R, Ellenbogen KA, Shivkumar K. Long-term clinical outcomes of focal impulse and rotor modulation for treatment of atrial fibrillation: a multicenter experience. Heart Rhythm. 2016;13:636–641. doi: 10.1016/j.hrthm.2015.10.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Steinberg JS, Shah Y, Bhatt A, Sichrovsky T, Arshad A, Hansinger E, Musat D. Focal impulse and rotor modulation: acute procedural observations and extended clinical follow-up. Heart Rhythm. 2017;14:192–197. doi: 10.1016/j.hrthm.2016.11.008. [DOI] [PubMed] [Google Scholar]
- 20.Miller JM, Kowal RC, Swarup V, Daubert JP, Daoud EG, Day JD, Ellenbogen KA, Hummel JD, Baykaner T, Krummen DE, Narayan SM, Reddy VY, Shivkumar K, Steinberg JS, Wheelan KR. Initial independent outcomes from focal impulse and rotor modulation ablation for atrial fibrillation: multicenter FIRM registry. J Cardiovasc Electrophysiol. 2014;25:921–929. doi: 10.1111/jce.12474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Balouch M, Gucuk Ipek E, Chrispin J, Bajwa RJ, Zghaib T, Berger RD, Ashikaga H, Nazarian S, Marine JE, Calkins H, Spragg DD. Impact of rotor temperospatial stability on acute and one-year atrial fibrillation ablation outcomes. Clin Cardiol. 2017;40:383–389. doi: 10.1002/clc.22674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kis Z, Theuns DA, Bhagwandien R, Wijchers S, Yap SC, Szili-Torok T. Type and rate of atrial fibrillation termination due to rotational activity ablation combined with pulmonary vein isolation. J Cardiovasc Electrophysiol. 2017;28:862–869. doi: 10.1111/jce.13240. [DOI] [PubMed] [Google Scholar]
- 23.Knecht S, Sohal M, Deisenhofer I, Albenque JP, Arentz T, Neumann T, Cauchemez B, Duytschaever M, Ramoul K, Verbeet T, Thorsten S, Jadidi A, Combes S, Tavernier R, Vandekerckhove Y, Ernst S, Packer D, Rostock T. Multicentre evaluation of non-invasive biatrial mapping for persistent atrial fibrillation ablation: the AFACART study. Europace. 2017;19:1302–1309. doi: 10.1093/europace/euw168. [DOI] [PubMed] [Google Scholar]
- 24.Berntsen RF, Hâland TF, Skårdal R, Holm T. Focal impulse and rotor modulation as a stand-alone procedure for the treatment of paroxysmal atrial fibrillation: a within-patient controlled study with implanted cardiac monitoring. Heart Rhythm. 2016;13:1768–1774. doi: 10.1016/j.hrthm.2016.04.016. [DOI] [PubMed] [Google Scholar]
- 25.Miller JM, Kalra V, Das MK, Jain R, Garlie JB, Brewster JA, Dandamudi G. Clinical benefit of ablating localized sources for human atrial fibrillation: the Indiana University FIRM Registry. J Am Coll Cardiol. 2017;69:1247–1256. doi: 10.1016/j.jacc.2016.11.079. [DOI] [PubMed] [Google Scholar]
- 26.Kuck KH, Brugada J, Fürnkranz A, Metzner A, Ouyang F, Chun KR, Elvan A, Arentz T, Bestehorn K, Pocock SJ, Albenque JP, Tondo C; FIRE AND ICE Investigators. Cryoballoon or radiofrequency ablation for paroxysmal atrial fibrillation. N Engl J Med. 2016;374:2235–2245. doi: 10.1056/NEJMoa1602014. [DOI] [PubMed] [Google Scholar]
- 27.Allessie MA, de Groot NM, Houben RP, Schotten U, Boersma E, Smeets JL, Crijns HJ. Electropathological substrate of long-standing persistent atrial fibrillation in patients with structural heart disease: longitudinal dissociation. Circ Arrhythm Electrophysiol. 2010;3:606–615. doi: 10.1161/CIRCEP.109.910125. [DOI] [PubMed] [Google Scholar]
- 28.Lee S, Sahadevan J, Khrestian CM, Cakulev I, Markowitz A, Waldo AL. Simultaneous biatrial high-density (510–512 Electrodes) epicardial mapping of persistent and long-standing persistent atrial fibrillation in patients: new insights into the mechanism of its maintenance. Circulation. 2015;132:2108–2117. doi: 10.1161/CIRCULATI0NAHA.115.017007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cuculich PS, Wang Y, Lindsay BD, Faddis MN, Schuessler RB, Damiano RJ Jr, Li L, Rudy Y. Noninvasive characterization of epicardial activation in humans with diverse atrial fibrillation patterns. Circulation. 2010;122:1364–1372. doi: 10.1161/CIRCULATI0NAHA.110.945709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Alhusseini M, Vidmar D, Meckler GL, Kowalewski CA, Shenasa F, Wang PJ, Narayan SM, Rappel WJ. Two independent mapping techniques identify rotational activity patterns at sites of local termination during persistent atrial fibrillation. J Cardiovasc Electrophysiol. 2017;28:615–622. doi: 10.1111/jce.13177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gianni C, Mohanty S, Di Biase L, Metz T, Trivedi C, Gökoğlan Y, Güneş MF, Bai R, Al-Ahmad A, Burkhardt JD, Gallinghouse GJ, Horton RP, Hranitzky PM, Sanchez JE, Halbfaβ P, Müller P, Schade A, Deneke T, Tomassoni GF, Natale A. Acute and early outcomes of focal impulse and rotor modulation (FIRM)-guided rotors-only ablation in patients with nonparoxysmal atrial fibrillation. Heart Rhythm. 2016;13:830–835. doi: 10.1016/j.hrthm.2015.12.028. [DOI] [PubMed] [Google Scholar]
- 32.Gianni C, Di Biase L, Deneke T, Tami Metz T, Halbfass P, Muller P, Schade A, Mohanty S, Trivedi C, Bai R, Al-Ahmad A, Burkhardt JD, Gallinghouse GJ, Horton RP, Hranitzky PM, Sanchez JE, Tomassoni GF, Natale A. Acute and short-term outcomes in persistent and long-standing persistent patients undergoing rotors only ablation (abstract). Heart Rhythm. 2015;12:PO01–PO58. [Google Scholar]
- 33.Narayan SM, Baykaner T, Clopton P, Schricker A, Lalani GG, Krummen DE, Shivkumar K, Miller JM. Ablation of rotor and focal sources reduces late recurrence of atrial fibrillation compared with trigger ablation alone: extended follow-up of the CONFIRM trial (Conventional Ablation for Atrial Fibrillation With or Without Focal Impulse and Rotor Modulation). J Am Coll Cardiol. 2014;63:1761–1768. doi: 10.1016/j.jacc.2014.02.543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Narayan SM, Krummen DE, Clopton P, Shivkumar K, Miller JM. Direct or coincidental elimination of stable rotors or focal sources may explain successful atrial fibrillation ablation: on-treatment analysis of the CONFIRM trial (Conventional ablation for AF with or without focal impulse and rotor modulation). J Am Coll Cardiol. 2013;62:138–147. doi: 10.1016/j.jacc.2013.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Baykaner T, Clopton P, Lalani GG, Schricker AA, Krummen DE, Narayan SM; CONFIRM Investigators. Targeted ablation at stable atrial fibrillation sources improves success over conventional ablation in high-risk patients: a substudy of the CONFIRM Trial. Can J Cardiol. 2013;29:1218–1226. doi: 10.1016/j.cjca.2013.07.672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


