Abstract
Background:
The obesity epidemic is a global concern. Standard behavioral treatment (SBT) including increased physical activity, reduced energy intake, and behavioral change counseling is an effective lifestyle intervention for weight loss.
Purpose:
Identify distinct step count patterns among weight loss intervention participants, examine weight loss differences by trajectory group, and examine baseline factors associated with trajectory group membership.
Methods:
Both groups received group-based SBT while the experimental group received up to 31 additional, one-on-one self-efficacy enhancement sessions. Data were analyzed using group-based trajectory modeling, analysis of variance, chi-square tests, and multinomial logistic regression.
Results:
Participants (N=120) were mostly female (81.8%) and white (73.6%) with a mean body mass index (BMI) of 33.2±3.8 kg/m2. Four step count trajectory groups were identified: active (>10,000 steps/day; 11.7%), somewhat active (7,500-10,000 steps/day; 28.3%), low active (5,000-7,500 steps/day; 27.5%), and sedentary (<5,000 steps/day; 32.5%). Percent weight loss at 12 months increased incrementally by trajectory group (5.1±5.7%, 7.8±6.9%, 8.0±7.4%, and 13.63±7.0%, respectively; p=.001). At baseline, lower BMI and higher perceived health predicted membership in the better performing trajectory groups.
Conclusions:
Within a larger group of adults in a weight loss intervention, four distinct trajectory groups were identified and group membership was associated with differential weight loss.
Keywords: health behavior, intervention study, obesity, overweight, physical activity
INTRODUCTION
In the United States, over one-third of adults are obese and the number of adults who are either overweight or obese is increasing globally.1,2 Adults who are obese, defined as a body mass index (BMI) > 30 kilograms divided by meters squared (kg/m2), compared to adults with a healthy weight, have an increased risk for hypertension, dyslipidemia, type 2 diabetes, sleep disordered breathing, coronary heart disease (CHD), certain cancers, and all-cause mortality.3,4 Standard behavioral treatment (SBT) is the recommended lifestyle intervention for weight loss.5 Increased physical activity (PA), a reduced fat and caloric diet, and behavioral therapy are key components of SBT for weight loss.6 The behavioral skills included in SBT are self-monitoring, goal-setting, stimulus control, and behavioral substitution, while the cognitive skills include problem-solving and cognitive restructuring.7
Objective measures of PA are more accurate and reliable than self-report and are being used increasingly in clinical trials.8 Systematic reviews and meta-analyses examining the associations between pedometer use and PA and health outcomes have found that pedometer use is associated with an approximate increase of 2,000 steps/day and significant decreases in BMI and blood pressure compared to baseline values or control groups.9,10 Additionally, given that pedometers, fitness tracking tools, and smartphone applications are becoming less expensive and more accurate, they are being adopted ever more by the general public to self-monitor PA.11
The advantages of objectively measured PA on the improvement of PA and weight loss compared to the absence of such information has been established. However, it should not be assumed that PA changes equally in all participants during the course of an intervention. To date, very little work has been done examining the unique patterns of PA among individuals in an intervention over time. Unlike analysis methods that estimate a single trajectory reflecting the population average, group-based trajectory modeling assumes that the population is composed of distinct groups, each with a different underlying trajectory.12 Group-based trajectory modeling identifies distinct groups of individuals following similar patterns over time.12 Thus, within a large sample with a mean increase in pedometer derived steps, there may be distinct groups of “increasers,” “decreasers,” and “no changers.”12 The identification of these different trajectory groups and the baseline factors associated with membership in a predicted group in the context of a behavioral intervention may result in the detection of individuals requiring additional attention or resources to overcome the barriers preventing behavior change. While the factors associated with less PA include older age, female sex, higher BMI, and worse health, it is not known if these factors are useful in predicting trajectory group membership.13-15
The purpose of this secondary analysis was to: 1) identify distinct temporal patterns (i.e., trajectory groups) for pedometer-derived step counts over the first 12 months of a behavioral weight loss intervention; 2) examine if weight loss varies by trajectory group; and 3) identify baseline factors associated with predicted trajectory group membership.
METHODS
Design
We examined data from the first 12 months of the Self Efficacy Lifestyle Focus (SELF) Trial, which focused specifically on the period of weight loss.16 The trial was approved by the University of Pittsburgh Institutional Review Board and was conducted between May 2009 and March 2013. The SELF Trial was an 18-month, randomized clinical trial where participants were randomized with equal allocation to one of two groups: SBT only (the comparison group) or SBT + self-efficacy (SE) enhancement (the experimental group). Both groups received SBT for weight loss that included group sessions, self-monitoring, and daily dietary and weekly PA goals. The SBT + SE group also received 30 supplemental, one-on-one sessions to enhance self-efficacy to reduce fat and calorie intake and to increase PA.16 The intervention for the SELF Trial has been described previously in detail.16 Briefly, group sessions occurred: 1) weekly during month 1; 2) bi-monthly during month 2; 3) monthly during months 3-12; and 4) every 6 weeks during months 13-18, the maintenance of weight loss phase. Content in the group sessions covered nutrition, physical activity and the principles of behavior change, including goal setting, self-monitoring, and feedback.17
Participants in the SBT only group were provided a daily calorie goal that was based on their weight and sex and a fat intake goal of less 25% of their total calories. Additionally, they were given a weekly PA goal of 150 minutes/week at 12 weeks advancing to 180 minutes/week at 6 months and then 210 minutes/week at 12 months. The participants in SBT + SE group received additional 30-minute, individual sessions to enhance self-efficacy.16 The SBT + SE group participants met with an interventionist prior to the first group session to develop individualized calorie and activity goals and a target date for goal achievement. Subsequent meetings occurred bi-monthly through month 12 and at least monthly during the remaining 6 months of the intervention. If there was a lack of progress towards the individualized goals, then possible barriers were explored along with problem-solving to attempt to overcome the barriers.18 All participants were asked to self-monitor calorie and fat intake and record their minutes of PA and number of daily steps. Pedometers were provided starting at week 3 of the intervention.
Sample
Participants were recruited from the southwestern Pennsylvania region. To increase diversity within the sample, mailing lists with Zone Improvement Plan (ZIP) codes that included minority representation were obtained and recruitment postcards were mailed out. Eligibility criteria included: 1) BMI between 27 and 43 kg/m2; 2) presence of a CHD risk factor (e.g., first-degree relative with CHD, hyperlipidemia); and 3) age ≥ 18 years. Exclusion criteria included: 1) physical limitations preventing exercise; 2) presence of an eating disorder; 3) current serious illness or unstable condition; 4) pregnancy; or 5) at-risk alcohol consumption. All participants received medical clearance from their primary care provider.
Measures
Sociodemographic data were collected using a standardized questionnaire developed at the University of Pittsburgh School of Nursing’s Center for Research in Chronic Disorders. To encourage PA self-monitoring, participants were given an Omron HJ-720IT pedometer with 42-day memory in the third week of the intervention. The first two weeks of the intervention focused on the importance of dietary self-monitoring and basic nutrition. As part of the intervention, pedometer use was recommended but not required. Pedometer data were uploaded when participants attended the group sessions. Mean daily step counts were calculated monthly from pedometer data. Days having zero step counts were considered as days when the pedometer was not worn and were coded as missing. Height was measured using a wall-mounted stadiometer. Weight was measured every 6 months on a Tanita digital scale. Baseline BMI and percent weight change from baseline to 12 months ([weight12 months – weightbaseline] / weightbaseline) × 100) were calculated.
Transformed scores from the Medical Outcomes Study Short Form-36, version 2 (MOS SF-36) were used to assess health-related quality of life.19 The MOS SF-36 yields two summary scores, the physical component and mental component summaries, and eight domain scores including: physical functioning, role limitations due to physical problems, bodily pain, general health, vitality, social functioning, role limitations due to emotional problems, and mental health.19 Transformed scores range from 0 to 100, with higher scores indicating greater health-related quality of life.
Analysis
Data were analyzed using SAS version 9.4 (SAS Institute, Cary, NC) and SPSS version 24.0 (IBM, Armonk, NY). The level of statistical significance was set at 0.05 (2-tailed). The sample distributions of socio-demographic and study variables were examined using descriptive statistics. The data were examined for missing data and for any patterns of missing data. Group-based trajectory modeling, using the TRAJ procedure in SAS, was used to identify distinct classes of trajectories of monthly mean daily step counts over 12 months.20 The dependent variable was mean daily step count over the previous month. Since the dependent variable was normally distributed, a normal model was assumed with no censoring. To determine the most appropriate number of groups, the Bayesian information criteria (BIC) for competing models were compared. The model with the largest BIC was considered the best fit using an approximate Bayes factor.21 After the appropriate number of groups was determined, the changes in BIC and the significance of regression coefficients were examined to identify the trajectory shape for each group.
Analysis of variance (ANOVA) with post hoc pairwise multiple comparisons with Bonferroni adjustment was used to examine the association between the percent mean change in weight from baseline to 12 months and predicted trajectory group membership. Additionally, Cohen’s d effect sizes were calculated comparing the predicted trajectory groups. To identify the bivariate associations for predicted trajectory group membership from the final group-based trajectory model, ANOVA was also applied for continuous variables (age, baseline BMI, MOS SF-36 scores, and years of education) and Pearson’s chi-square test (or Fisher’s exact test if sparse cells were encountered) was used for categorical variables (sex, intervention group, and race). These predictors were selected á priori based on the literature. The significant variables based on the bivariate analyses were included in a multinomial logistic regression model. For the multinomial logistic regression, only data from the individuals who identified their race as white or black (117 of the 120 participants) were included.
RESULTS
Descriptive Characteristics
The SELF Trial had 130 participants; however, 10 participants never used the pedometer and were excluded from the secondary analysis. Therefore, the sample (N=120) was 81.8% female, 73.4% white and 24.2% black with a mean (± standard deviation) age of 53.9 ± 9.0 years, had 15.9 ± 3.1 years of education, and a baseline BMI of 33.2 ± 3.8 kg/m2 (Table 1). Pedometer days, defined as the percent of days used out of all possible days, significantly declined from 72.1% for month 1 through 6 months to 52.6% for months 7 through 12 months (p < .001). Among those who wore the pedometer, there was a non-statistical significant increase in average daily step count, increasing from 6,834 ± 2,618 at month 1 to 6,940 ± 3,199 at 6 months and 7,114 ± 3,596 at 12 months (p = .985).
Table 1.
Baseline characteristics for all participants and by predicted trajectory group
| Characteristic | All Participants N = 120 |
Active group n = 14 |
Somewhat active group n = 34 |
Low active group n = 33 |
Sedentary group n = 39 |
Group differences (p-value) |
|---|---|---|---|---|---|---|
| Treatment group, SBT only | 55.8 (67) | 50.0 (7) | 58.8 (20) | 57.6 (19) | 53.8 (21) | .938 |
| Age, years | 53.9 ± 9.0 | 53.0 ± 10.5 | 55.2 ± 5.7 | 52.4 ± 9.0 | 54.5 ± 10.7 | .588 |
| Sex, female | 81.8 (99) | 85.7 (12) | 82.4 (28) | 87.9 (29) | 77.0 (30) | .682a |
| Education, years | 15.9 ± 2.9 | 15.5 ± 3.4 | 15.7 ± 2.5 | 16.2 ± 3.3 | 15.5 ± 2.9 | .728 |
| Race | ||||||
| White | 73.3 (88) | 50.0 (7) | 76.5 (26) | 87.9 (29) | 66.7(26) | .045a |
| Black | 24.2 (29) | 42.9 (6) | 20.6 (7) | 12.1 (4) | 30.7 (12) | |
| Multi-racial | 0.8 (1) | 0.0 (0) | 0.0 (0) | 0.0 (0) | 2.6 (1) | |
| Other | 0.8 (1) | 7.1 (1) | 0.0 (0) | 0.0 (0) | 0.0 (0) | |
| Not specified | 0.8 (1) | 0.0 (0) | 2.9 (1) | 0.0 (0) | 0.0 (0) | |
| BMI, kg/m2 | 33.2 ± 3.8 | 34.1 ± 3.7 | 31.8 ± 3.3 | 32.6 ± 3.5 | 34.7 ± 3.5 | .007 |
| MOS SF-36 Summary Scores | ||||||
| Physical component | 51.3 ± 7.0 | 52.4 ± 4.6 | 53.9 ± 5.6 | 51.5 ± 5.5 | 48.6 ± 8.9 | .012 |
| Mental component | 49.7 ± 7.3 | 48.3 ± 12.9 | 51.8 ± 7.3 | 50.2 ± 9.0 | 48.0 ± 12.2 | .588 |
| MOS SF-36 Domain Scores | ||||||
| Physical functioning | 86.0 ± 15.5 | 86.8 ± 16.8 | 89.6 ± 13.7 | 87.9 ± 9.8 | 81.0 ± 19.0 | .090 |
| Role physical | 86.1 ± 17.9 | 88.8 ± 18.0 | 91.5 ± 16.1 | 86.6 ±16.0 | 80.0 ± 19.5 | .042 |
| Bodily pain | 74.3 ± 19.3 | 72.0 ± 9.9 | 80.1 ± 18.1 | 75.2 ± 17.1 | 69.3 ± 23.3 | .115 |
| General health perception | 70.6 ± 20.7 | 72.8 ± 19.5 | 79.2 ± 15.1 | 70.8 ± 18.8 | 62.1 ± 23.9 | .005 |
| Vitality | 58.5 ± 17.3 | 64.0 ± 12.9 | 56.3 ± 17.0 | 54.8 ± 17.7 | 54.8 ± 17.7 | .106 |
| Social functioning | 86.7 ± 19.8 | 84.0 ± 27.0 | 92.6 ± 14.1 | 88.3 ± 15.3 | 81.1 ± 23.1 | .080 |
| Role emotional | 86.6 ± 21.3 | 81.6 ± 27.0 | 90.0 ± 17.9 | 91.2 ± 16.8 | 81.6 ± 26.2 | .153 |
| Mental health | 75.5 ± 16.6 | 74.6 ± 24.8 | 79.0 ± 12.8 | 75.0 ± 15.7 | 73.2 ± 17.0 | .520 |
Descriptive statistics are reported as means ± standard deviation or percent (n)
p-value based on Fisher’s Exact test.
Predicted trajectory groups of step counts
Four distinct trajectory groups were identified (Table 2): active (intercept = 10,886, slope = 140; n = 14, 11.7%), somewhat active (intercept = 8,836, slope = −55; n = 34, 28.3%), low active (intercept = 5,953; n = 33, 27.5%), and sedentary (intercept = 4,583, slope = −120; n = 39, 32.5%). Over the 12 months, the active group increased their daily step counts, as evidenced by a positive slope, while the other groups either maintained (low active group) or decreased (somewhat active and sedentary groups) their step counts as evidenced by a zero or negative slope, respectively. Only the active group had a mean daily step count greater than 10,000 steps/day (Figure 1).
Table 2.
Group-based trajectory modeling results for pedometer-based monthly mean daily step counts (N = 120)
| Trajectory Group |
Parameter | Estimate | Standard Error |
t-value | p-value |
|---|---|---|---|---|---|
| Active | Intercept Linear |
10886.00 139.54 |
306.14 44.96 |
35.56 3.10 |
< .001 .002 |
| Somewhat active | Intercept Linear |
8836.27 −55.64 |
225.74 28.19 |
39.14 −1.97 |
< .001 .048 |
| Low active | Intercept | 5953.24 | 157.90 | 37.70 | < .001 |
| Sedentary | Intercept Linear |
4582.53 −119.96 |
197.56 29.66 |
23.20 −4.04 |
< .001 < .001 |
Figure 1:
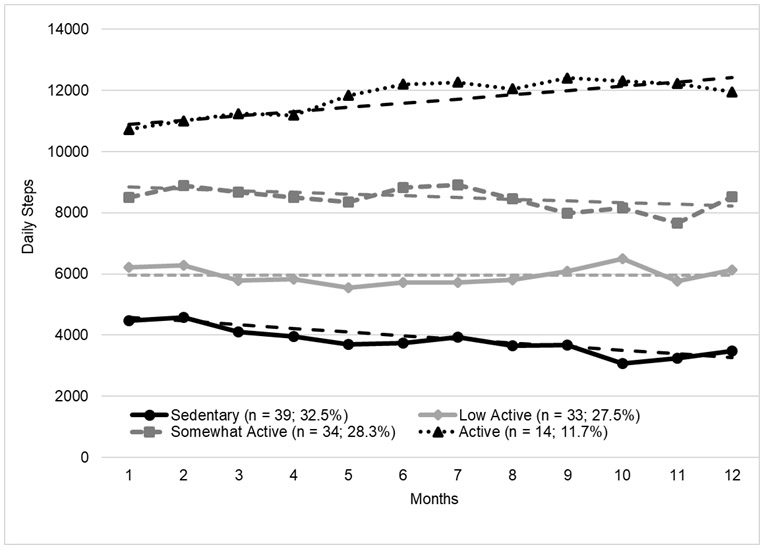
Predicted (dashed lines) and observed (with line markers) mean daily step count per month by trajectory group
Percent weight change by trajectory group
Overall, mean percent weight loss at 12 months was −7.7 ± 7.0%. Mean percent weight loss at 12 months tended to increase incrementally as step counts increased: 5.1 ± 5.7% in sedentary group, 7.8 ± 6.9% in low active group, 8.0 ± 7.4% in somewhat active group, and 13.63 ± 7.0% in active group, respectively (F = 12.3, p=.001; Figure 2). Post-hoc multiple pairwise comparisons with a Bonferroni correction showed that the active group had significantly greater weight loss compare to the sedentary group (p = .001). All other comparisons were not statistically significant. The Cohen’s d effect sizes for the active group compared to the other groups were: 1.23 for the sedentary group, 0.81 for the low active, and 0.77 for the somewhat active group.
Figure 2. Percent weight change from baseline to 12 months by predicted trajectory group.
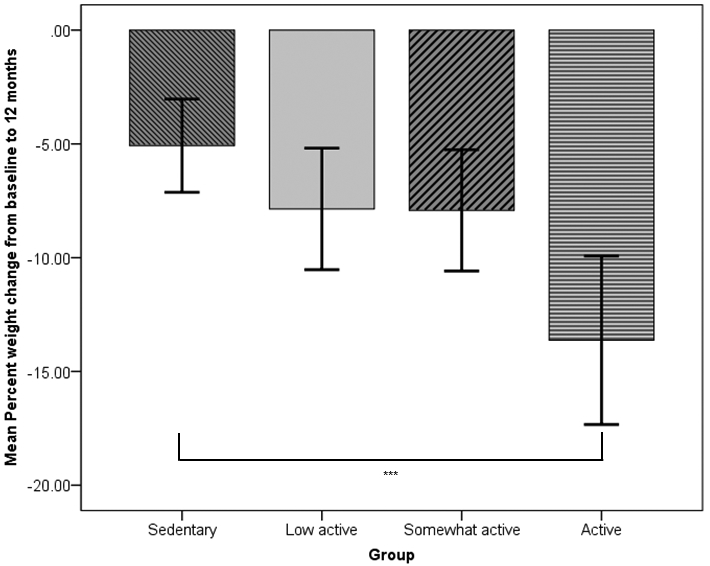
Error bars: 95% Confidence Interval
*** = p ≤ 0.001
Predictors of group membership of step counts
When examining the bivariate associations of group membership of step counts, race (p = .045), BMI (p = .007), MOS SF-36 physical component summary score (p = .012), and the MOS SF-36 role physical and general health perception domain scores (p = .042 and p = .005, respectively) were statistically significant (Table 1). Since the MOS SF-36 physical component summary score consisted, in part, of the MOS SF-36 role physical and general health perception domain scores, it was not included in the multinomial logistic regression model. When the remaining variables were entered into the model, only BMI and the general health perception domain score were statistically significant (Table 3). Compared to the sedentary group, the reference group for the analyses, each one-unit increase in BMI predicted a 13.7% (odds ratio [OR] = 0.86 and 95% confidence interval [95% CI]; 0.75, 0.99) lower odds of membership in the low active group and a 19% (OR = 0.81; 95% CI = 0.67, 0.94) lower odds of membership in the somewhat active group. For the general health perception domain score, each one-point increase in the score predicted a 9.0% (OR = 1.09; 95% CI = 1.02, 1.17) higher odds of membership in the somewhat active group compared to the sedentary group.
Table 3:
Multinomial logistic regression model for the predictors of trajectory group membership (n=117)
| Trajectory Groupa |
Predictor | b | 95% CI of b |
OR | 95% CI of OR |
p-value |
|---|---|---|---|---|---|---|
| Low Active |
BMIb | −0.147 | −0.288, −0.006 | 0.863 | 0.751, 0.991 | .037 |
| SF-36: General Healthb | 0.027 | −0.028, 0.082 | 1.028 | 0.972, 1.086 | .334 | |
| Somewhat Active |
BMIb | −0.214 | −0.371, −0.057 | 0.808 | 0.692, 0.943 | .007 |
| SF-36: General Healthb | 0.088 | 0.021, 0.155 | 1.092 | 1.021, 1.168 | .010 | |
| Active | BMIb | −0.008 | −0.194, 0.178 | 0.993 | 0.825, 1.193 | .936 |
| SF-36: General Healthb | 0.061 | −0.007, 0.129 | 1.063 | 0.981, 1.153 | .136 |
Sedentary group is reference;
At baseline; SE, standard error; OR, odds ratio; CI, confidence interval; BMI, body mass index
Adjusted for race and SF-36: Role Physical domain score
DISCUSSION
In this secondary analysis, we identified four distinct trajectory groups for mean daily step counts over the course of the first 12 months of a weight loss intervention. An examination of the mean daily step counts among all participants who used the pedometer suggests an increase of approximately 280 steps/day from baseline to 12 months. However, by examining the slopes of the four predicted trajectory groups, it was clear that only the active trajectory group increased their step counts. Additionally, membership in the more active groups (the groups with a higher mean daily step counts) was associated with significantly greater weight losses. Finally, we identified baseline BMI and general health perception as predictors of trajectory group membership.
This is the first study, to our knowledge, to examine pedometer derived trajectory groups among participants in a weight loss intervention. Based on the BIC for the competing models (two vs. three vs. four groups) the four group model had the largest BIC (data not shown) and was best fit.2 In addition to the four group model being the best fit statistically, the model mirrored Tudor-Locke’s pedometer-determined classifications of physical activity.22
Previous studies of PA among the general population and healthy adults have reported associations between older age, female sex, higher BMI, and worse health and less PA.13-15 The associations among education, income and PA are less clear with studies reporting mixed results. Specifically, The America On the Move study,13 found that females compared to males took, on average, 400 fewer steps/day (p=.03), which decreased by age (p<.001), and that individuals who were overweight or obese took fewer steps/day compared to individuals with a healthy weight (5,200 and 4,330, respectively, vs. 5,864, p<.001). Our study did not find that sex or age predicted trajectory group membership. The study by Bassett and colleagues did not find differences in mean steps/day by education level or race, which is consistent with our findings.13
Dai and colleagues examined eight cycles of health survey data between 1994-1995 and 2008-2009 to examine the predictors of decreased PA level over time.14 Among females, becoming or remaining overweight/obese compared to maintaining a healthy weight (OR = 1.24; 95% CI 1.08, 1.43 and OR = 1.18; 95% CI = 1.06, 1.32, respectively) and becoming or remaining unhealthy compared to remaining healthy (OR = 1.72; 95% CI = 1.41, 2.10 and OR = 1.82; 95% = 1.41, 2.35, respectively) predicted reduced leisure-time PA.14 Among males, becoming or remaining unhealthy compared to remaining healthy (OR = 1.41; 95% CI = 1.13, 1.74 and OR = 1.55; 95% CI = 1.18, 2.05, respectively) predicted reduced leisure-time PA.14 These findings support our results related to the role of BMI and general health on PA. Income or changes in income did not predict changes in leisure-time PA. Interestingly, completing more education, compared to education level remaining the same, predicted increase leisure-time PA in both females (OR = 0.42; 95% CI = 0.36, 0.46) and males (OR = 0.44; 95% CI = 0.37, 0.52).14
In an examination of accelerometer derived patterns of PA from the 2003-2004 National Health and Nutrition Examination Survey (NHANES) dataset, Kao and colleagues found that intensity of PA decreased with increased age and increased BMI.15 Compared to the reference group of adults 20-29 years old, adults greater than 40 years old had a decrease in moderate and intense activities. Individuals with obesity spent 6-33% less time engaged in moderate and 37-80% less time engaged in intense PA compared to individuals with a healthy weight. Furthermore, females compared to males spent a greater proportion of time engaged in sedentary and light activity and less time engaged in more strenuous (moderate and intense) PA.15 Unlike the findings of our study and the study by Basset and colleagues,13 Kao and colleagues found that a greater then a high school education and an income greater than $45,000/year were associated with a complex pattern of PA. The individuals who completed a greater than high school education spent more time engaged in sedentary and moderate to intense activities, while spending less time engaged in light activities compared to the individuals with less education.15 Individuals with a higher income spent more time in sedentary activities and less time engaged in light activity compared to individuals with a lower income. The type of employment and amount of work-related PA could be responsible for these findings. One notable difference in Kao’s study compared to our study is the use of accelerometer derived patterns of PA compared to pedometer derived step counts.
From the time when the pedometers were provided to participants (week three) to 12 months, mean daily steps among the individuals who used the pedometers increased by approximately 280 steps/day (6,834 ± 2,618 to 7,114 ± 3,596). This change was driven by the active group. The aforementioned systematic review by Bravata and colleagues reported a mean increase from baseline of 2,183 steps/day in observational pedometer-based studies.9 While the increase seen in our study was much less, daily step counts were not collected until week 3 of the study. If daily steps were collected before the initiation of the intervention, a greater increase may have been observed. Furthermore, at three weeks our participants had a mean of 6,834 steps/day. This was higher than the mean steps/day for adults who are overweight, 5200 steps/day, and adults with obesity, 4330 steps/day, reported by Basset and colleague.13
In the SELF Trial, neither the SBT nor the SBT + SE group were given a daily step goal. Instead, participants were given minutes of PA/week goals. Bravata and colleagues reported that a greater mean increase in daily steps was seen in studies where a step goal was provided with the greatest increase in daily steps seen with a goal of 10,000 steps/day.9 It is possible that individuals in the active and somewhat active trajectory groups created their own daily step goals that contributed to their success.
Like previous studies, our results support that a higher BMI and worse perceived general health negatively affects PA and PA changes over the course of an intervention. These represent substantial barriers that individuals must overcome when attempting to increase their PA and lose weight. In the context of an SBT intervention, individuals with these baseline characteristics may require more time and support to acquire or improve the behavioral and cognitive skills included in SBT. Without this additional time and support, they may fail at overcoming the barriers resulting in little or no improvements in their PA. Unlike the previously published literature, we found no sex or age differences by trajectory groups. However, the sample of the SELF trial consisted primarily of middle-aged females, which may explain our findings.
This study had several limitations. Pedometer use was encouraged, but not required; thus, results may be a reflection of groups with different levels of motivation for self-monitoring. Additionally, overall pedometer use steadily declined during the intervention. It is unknown if those who failed to use the pedometer were more or less active than the other members of their predicted trajectory group. Another weakness of this secondary analysis was the relatively small, mostly homogenous sample. This is especially of note with the active group that was limited to 14 participants and may negatively affect the validity of the results. The study had several strengths including the good retention rate of the SELF trial, the usage of Group Based Trajectory Modeling, and a sample that had a 25% minority (black) representation.
The study highlights that group-based trajectory modeling can be used to identify distinct sub-groups within a weight-loss intervention trial that may require additional strategies to improve their level of PA as part of the lifestyle that supports weight loss. Moreover, the findings suggest that less active individuals may have difficulty increasing steps even when using a pedometer and that individuals with a higher BMI and poorer general health may face additional physical and environmental barriers that limit daily walking and warrant additional assistance. While a large portion of the study participants did not achieve the recommended step count of 10,000 steps/day, the striking difference in weight losses by the trajectory group cannot be overlooked. These findings provide data to demonstrate to individuals how much additional weight loss can be achieved by simply increasing daily step counts. Furthermore, the early identification of less active individuals may allow for additional interventions to specifically target their low-activity lifestyle, potentially leading to improved weight loss. While this study was able to identify distinct step count trajectories and BMI and perceived general health as a predictors of trajectory group membership, additional work is needed. Future studies need to build on these findings and also further examine trajectories using other objective measures in larger, even more diverse samples.
Acknowledgments
Funding Sources: This work was supported by National Institutes of Health National Institute of Nursing Research P01NR010949 and by National Institutes of Health National Institute of Nursing Research K24NR010742 (L.E. Burke, MidCareer Mentorship Award). This study is registered at www.clinicaltrials.gov (NCT00896194).
REFERENCES
- 1.Imes CC, Burke LE. The obesity epidemic: The United States as a cautionary tale for the rest of the world. Curr Epidemiol Rep. 2014; 1(2), 82–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ogden CL, Carroll MD, Fryar CD, Flegal KM. NCHS data brief, no 219 Prevalence of obesity among adults and youth: United States, 2011–2014. Hyattsville, MD: National Center for Health Statistics; 2015. [PubMed] [Google Scholar]
- 3.Flegal KM, Graubard BI, Williamson DF, Gail MH. Cause-specific excess deaths associated with underweight, overweight, and obesity. JAMA. 2007; 298(17), 2028–2037. [DOI] [PubMed] [Google Scholar]
- 4.Brown WV, Fujioka K, Wilson PW, Woodworth KA. Obesity: why be concerned? Am J Med. 2009; 122(4 Suppl), S4–S11. [DOI] [PubMed] [Google Scholar]
- 5.Webb VL, Wadden TA. Intensive lifestyle intervention for obesity: principles, practices, and results. Gastroenterology. 2017; 152(7), 1752–1764. [DOI] [PubMed] [Google Scholar]
- 6.Butryn ML, Webb V, Wadden TA. Behavioral treatment of obesity. Psychiatr Clin North Am. 2011; 34(4), 841–859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fabricatore AN. Behavior therapy and cognitive-behavioral therapy of obesity: is there a difference? J Am Diet Assoc. 2007; 107(1), 92–99. [DOI] [PubMed] [Google Scholar]
- 8.Strath SJ, Kaminsky LA, Ainsworth BE, et al. Guide to the assessment of physical activity: clinical and research applications: a scientific statement from the American Heart Association. Circulation. 2013; 128(20), 2259–2279. [DOI] [PubMed] [Google Scholar]
- 9.Bravata DM, Smith-Spangler C, Sundaram V, et al. Using pedometers to increase physical activity and improve health: a systematic review. JAMA. 2007; 298(19), 2296–2304. [DOI] [PubMed] [Google Scholar]
- 10.Kang M, Marshall SJ, Barreira TV, Lee JO. Effect of pedometer based physical activity interventions: a meta-analysis. Res Q Exerc Sport. 2009; 80(3), 648–655. [DOI] [PubMed] [Google Scholar]
- 11.Jee H Review of researches on smartphone applications for physical activity promotion in healthy adults. J Exerc Rehabil. 2017; 13(1), 3–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nagin DS. Analyzing developmental trajectories: A semiparametric, group-based approach. Psychol Methods. 1999; 4(2), 139–157. [DOI] [PubMed] [Google Scholar]
- 13.Bassett DR Jr, Wyatt HR, Thompson H, Peters JC, Hill JO. (2010) Pedometer-measured physical activity and health behaviors in U.S. adults. Med Sci Sports Exerc. 2010; 42(10), 1819–1825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dai S, Wang F, Morrison H. Predictors of decreased physical activity level over time among adults: a longitudinal study. Am J Prev Med. 2014; 47(2), 123–130. [DOI] [PubMed] [Google Scholar]
- 15.Kao MC, Jarosz R, Goldin M, Patel A, Smuck M. Determinants of physical activity in America: a first characterization of physical activity profile using the National Health and Nutrition Examination Survey (NHANES). PM R. 2014; 6(10), 882–892. doi: 10.1016/j.pmrj.2014.03.004. [DOI] [PubMed] [Google Scholar]
- 16.Burke LE, Ewing LJ, Ye L, et al. The SELF trial: A self-efficacy-based behavioral intervention trial for weight loss maintenance. Obesity. 2015; 23(11), 2175–2182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wing RR. Behavioral approaches to the treatment of obesity In Bray GA, Bourchard C, James WPT, eds. Handbook of obesity: Clinical applications. 2nd ed. New York, NY: Marcel Dekker; 2004:147–167. [Google Scholar]
- 18.D’Zurilla TJ, Goldfried MR. Problem solving and behavior modification. J Abnorm Psychol. 1971; 78(1), 107–126. [DOI] [PubMed] [Google Scholar]
- 19.McHorney CA, Ware JE Jr, Lu JF, Sherbourne CD. MOS 36-item Short-Form Health Survey (SF-36): III. Tests of data quality, scaling assumptions, and reliability across diverse patient groups. Med Care. 1994; 32(1), 40–66. [DOI] [PubMed] [Google Scholar]
- 20.Jones BL, Nagin NS, Roeder K. A SAS procedure based on mixture models for estimating developmental trajectories. Sociol Method Res. 2001; 29(3), 373–393. [Google Scholar]
- 21.Nagin DS. Group-based modeling of development. Cambridge, MA: Harvard University Press; 2005. [Google Scholar]
- 22.Tudor-Locke C, Bassett DR Jr. How many steps/day are enough? Preliminary pedometer indices for public health. Sports Med. 2004; 34(1):1–8. [DOI] [PubMed] [Google Scholar]


